Abstract
Purpose
(I) To determine the incidence of periprosthetic tibial fractures in cemented and cementless unicompartmental knee arthroplasty (UKA) and (II) to summarize the existing evidence on characteristics and risk factors of periprosthetic fractures in UKA.
Methods
Pubmed, Cochrane and Embase databases were comprehensively searched. Any clinical, laboratory or case report study describing information on proportion, characteristics or risk factors of periprosthetic tibial fractures in UKA was included. Proportion meta-analysis was performed to estimate the incidence of fractures only using data from clinical studies. Information on characteristics and risk factors was evaluated and summarized.
Results
A total of 81 studies were considered to be eligible for inclusion. Based on 41 clinical studies, incidences of fractures were 1.24% (95%CI 0.64–2.41) for cementless and 1.58% (95%CI 1.06–2.36) for cemented UKAs (9451 UKAs). The majority of fractures in the current literature occurred during surgery or presented within 3 months postoperatively (91 of 127; 72%) and were non-traumatic (95 of 113; 84%). Six different fracture types were observed in 21 available radiographs. Laboratory studies revealed that an excessive interference fit (press fit), excessive tibial bone resection, a sagittal cut too deep posteriorly and low bone mineral density (BMD) reduce the force required for a periprosthetic tibial fracture to occur. Clinical studies showed that periprosthetic tibial fractures were associated with increased body mass index and postoperative alignment angles, advanced age, decreased BMD, female gender, and a very overhanging medial tibial condyle.
Conclusion
Comparable low incidences of periprosthetic tibial fractures in cementless and cemented UKA can be achieved. However, surgeons should be aware that an excessive interference fit in cementless UKAs in combination with an impaction technique may introduce an additional risk, and could therefore be less forgiving to surgical errors and patients who are at higher risk of periprosthetic tibial fractures.
Level of evidence
V.
Keywords: Periprosthetic fractures, Tibial plateau fractures, Complications, Failure modes, Unicompartmental knee arthroplasty, Partial knee replacement, UKA, PKR
Introduction
Unicompartmental knee arthroplasty (UKA) is a well-established treatment for patients with isolated compartmental knee arthritis. Advantages of UKA over total knee arthroplasty (TKA) include reduced morbidity and mortality, preservation of normal knee kinematics and faster recovery [35, 49, 59]. However, national registry data have shown lower revision rates after TKA in comparison to UKA [49, 66]. Reasons for UKA revision include aseptic loosening, malalignment, progression of osteoarthritis, instability, infection and periprosthetic fractures [49, 66].
Periprosthetic fractures represent a complex complication with serious consequences in UKA and have been associated with increased mortality and morbidity [26]. The periprosthetic fractures in UKA are most commonly reported on the tibial side (approximately 87%) [66]. Although these periprosthetic tibial fractures are relatively rare compared to other complications in UKA, recent registry-based studies have shown an increased rate of periprosthetic fractures in cementless UKAs compared to cemented UKAs [49, 63]. Since the interest of cementless fixation for UKAs is expected to increase, the rate of periprosthetic fractures may increase as well [49, 63]. However, registry-based studies may not provide reliable information about all fractures, as some periprosthetic fractures are internally fixed and the components are not revised or are treated conservatively. Another common limitation of registry-based studies is that tibial and femoral periprosthetic fractures are not reported separately. This stresses the need for a thorough evaluation of the incidence of periprosthetic tibial fractures in cemented and cementless UKAs using clinical studies. Furthermore, there is a lack of studies providing an overview of the available evidence on characteristics and risk factors of periprosthetic tibial fractures in UKA to gain a better understanding and awareness.
Therefore, the primary study aim was to estimate the incidence of periprosthetic tibial fractures in cemented and cementless UKA using clinical studies. Secondarily, relevant studies were systematically reviewed to summarize characteristics and risk factors of periprosthetic tibial fractures in UKA. Based on earlier large case series of both cemented and cementless UKAs reporting no non-traumatic periprosthetic tibial fractures [62, 68], it was hypothesized that comparable low incidences of periprosthetic tibial fractures can be achieved as long as surgeons are aware of factors that could increase the risk.
Methods
Search strategy
This systematic review with meta-analysis was conducted according to the PRISMA guidelines [65]. Medline, Cochrane and Embase databases were comprehensively searched on 28 May 2020. The database search included several combinations of key terms: “unicompartmental”, “knee”, “arthroplasty”, “failure”, “complication”, “survival”, “survivorship”, “revision”, “reoperation”, “fracture” and “collapse”. The search was, however, limited to English language studies published since 2000.
After duplicates were excluded, titles and abstracts were screened by two independent reviewers (*** & ***). Subsequently, full texts of the potential studies were carefully assessed by the two reviewers to confirm study eligibility. To be eligible, the study needed to contain information on proportion, characteristics and/or risk factors of periprosthetic tibial fractures in UKA. Clinical studies with information on fixation type and proportion were used to estimate incidences. For information regarding characteristics and/or risk factors, any study design was considered eligible, including case reports and laboratory studies. Although case reports and laboratory studies constitute low-level evidence, a systematic review of such studies can provide a better understanding and awareness of tibial plateau fractures in UKA. Studies were excluded if they reported on bicompartmental UKAs, used the same database, were reviews, registry-based studies, commentaries or abstracts. References of the included studies were checked for any missing studies. Any disagreements on study eligibility were resolved through consultation of the third reviewer (***).
Data collection and analysis
Data extraction was entered in predefined spreadsheets by two independent reviewers. First author, publication year and study design were reported for each study. Total number of UKAs, number of fractures and fixation type were collected only from clinical studies for the analysis of incidence. To identify potential risk factors, characteristics of patients with and without periprosthetic tibial fractures were collected from clinical studies and compared. For example, body mass index (BMI) of patients with and without fractures were compared. Both clinical studies and case reports were used to evaluate characteristics of periprosthetic tibial fractures (time of fracture in relation to UKA, fracture mechanism [traumatic or non-traumatic], fracture type, type of treatment). Time of fracture in relation to UKA was classified into the following time-points: during surgery, within 3 months postoperatively, between 4 and 12 months postoperatively and after 1 year postoperatively. Schematic drawings were used to present the fracture types found on available radiographs. Causes of fractures considered by authors from each study were evaluated and summarized. Finally, conclusions of laboratory studies were presented.
Methodological quality assessment
Different tools for methodological quality assessment were used depending on study design.
The National Institutes of Health (NIH) checklist was used for all clinical studies [67],The Case Report (CARE) checklist was used for case reports [29],and the Quality Appraisal for Cadaveric Studies (QUACS) checklist [90] was used for cadaveric studies. A score was provided for each article (poor, fair or good). The assessment was performed by two independent reviewers (*** & ***) and disagreements of the level of study quality were resolved through consultation of the third reviewer (***).
Statistical analyses
Incidence of periprosthetic tibial fractures was calculated as the number of fractures divided by the total number of UKAs from each clinical study. These data were combined via proportion meta-analysis [94]. This is a tool to calculate an overall proportion from studies reporting a single proportion. Combined proportions were determined for cementless and cemented UKAs. A subgroup analysis was performed for cementless and cemented Oxford Partial Knee Implants. Effect sizes and 95% Confidence Intervals (CI) were determined using a random-effects model by the back-transformation of the weighted mean of the logit-transformed proportions with Dersimonian weights. Characteristics between patients with and without periprosthetic tibial fractures were compared using the chi-square test for categorical variables and independent t test for continuous variables. All analyses were performed with R version 4.0.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
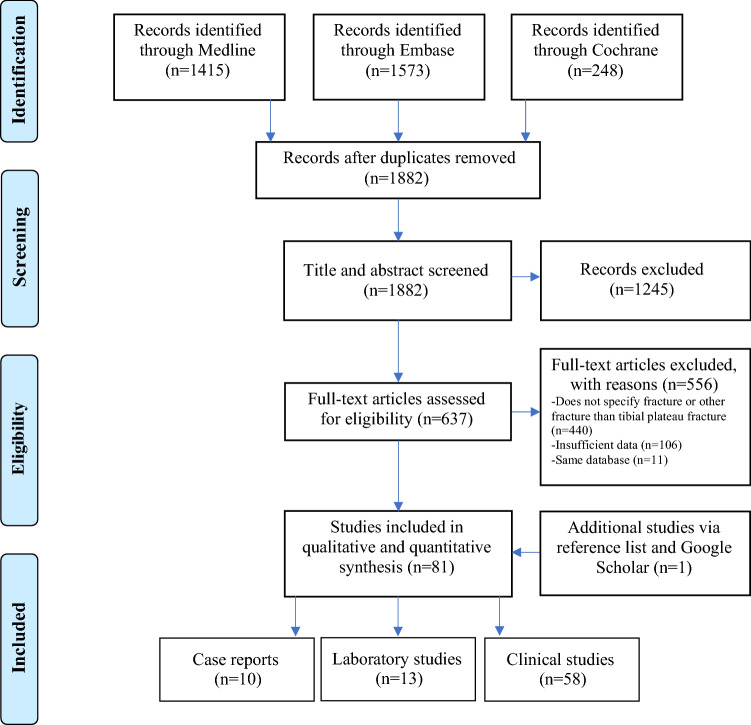
A total of 81 studies were included (Fig. 1). Fifty-eight (72%) were clinical studies consisting of 30 retrospective case series (52%) [1–6, 8–11, 14, 27, 31, 36, 37, 43–45, 47, 48, 53, 54, 70, 73, 83, 85, 88, 91, 93, 96], 14 prospective case series (26%) [7, 17, 18, 32, 51, 55–58, 61, 77, 78, 86, 95], seven retrospective cohort studies (12%) [13, 24, 25, 46, 50, 59, 72], four prospective cohort studies (7%) [28, 30, 84, 89] and three randomized controlled trials (5%) [22, 23, 33]. Ten (12%) studies were case reports [15, 40, 52, 60, 69, 74, 81, 82, 87, 92]. Thirteen (16%) were laboratory studies, of which four (31%) used sawbones [16, 20, 39, 64], four (31%) finite element models [41, 42, 75, 76], three (23%) human cadavers [21, 79, 80] and two (15%) a combination of finite element models with sawbones [19, 71]. The quality of studies was considered to be good in 54 (67%) studies, fair in 26 (32%) studies, and poor in one (1%) study. Table 1 summarizes the conclusions and quality assessment of the laboratory studies. Appendix 1 and 2 summarize the data extraction and quality assessment of the case reports and clinical studies, respectively.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram
Table 1.
Summary of laboratory studies
| Study | Country | Study type | Implant | Summary | Study quality * |
|---|---|---|---|---|---|
| Campi et al. [16] | UK | Sawbone | Oxford (Biomet) | This study suggests that decreasing the press fit of the tibial keel of the cementless UKA would significantly decrease the push-in force required to insert the tibial component (and so decrease the risk of fracture), without reducing the pull-out force and therefore ensuring the same level of primary stability | Good |
| Chang et al. [19] | Taiwan | FE model & Sawbone | Miller-Galante II, cemented (Zimmer) | This study suggests that in UKA, rounding the resection corner during preparation of the tibial plateau decreases the strain on tibial bone and avoid degenerative remodeling, in comparison to a standard rectangular corner. This modified surgical technique using a predrilled tunnel through the tibia prior to cutting could avoid extended vertical saw cutting errors | Good |
| Clarius et al. [20] | Germany | Sawbone | Oxford (Biomet) | This study suggests several sawing errors can occur during preparation of the tibial plateau (extended vertical cuts which may reduce the stability of the medial tibial plateau, extended horizontal cuts, perforation of the posterior cortex) and femoral condyle (ascending cut at the posterior femoral condyle) in UKA, especially with inexperienced surgeons | Good |
| Clarius et al. [21] | Germany | Cadaver | Oxford UKA (Biomet) | This study suggests that extended sagittal saw cuts in UKA weaken the tibial bone structure and increase the risk of periprosthetic tibial plateau fractures. In addition, this study showed that UKA patients with low BMD are at higher risk, as the fracture load is dependent on the bone density | Good |
| Iesaka et al. [41] | Japan | FE model | NR | In UKA, placing the tibial component in slight valgus inclination is preferred to varus or square inclination as it results in more even stress distributions | Fair |
| Inoue et al. [42] | Japan | FE model | Metal-backed tibia, cemented | This study suggests that the risk of medial tibial condylar fractures in UKA increases with increasing valgus inclination of the tibial component and with increased extension of the sagittal cut in the posterior tibial cortex | Good |
| Mohammad et al. 2018 | UK | Sawbone | Oxford, cementless (Zimmer Biomet) | This study suggests to use a new wider and deeper keel cut saw blade in UKA as it decreases the risk of tibial fracture compared to the standard keel cut saw blade, with no compromise in fixation | Good |
| Sasatani et al. 2019 | Japan | FE model | Persona (Zimmer Biomet) | This study suggests that the optimal alignment of the tibial implant in UKA is the middle position the coronal plane and the original posterior inclination in the sagittal plane | Good |
| Sawatari et al. 2005 | Japan | FE model | SCR UKA, metal-backed tibia, cemented (Stryker) | This study suggests that in UKA, placing the tibial component in slight valgus inclination is recommended due to reduced stress on tibial cancellous bone, in comparison with varus or square inclination. However, excessive posterior slope should be avoided | Good |
| Seeger et al. [79] | Germany | Cadaver | Oxford cemented & cementless (Biomet) | The risk for periprosthetic tibial plateau fractures is higher with cementless UKA than cemented UKA, especially in patients with poor bone quality | Good |
| Seeger et al. [80] | Germany | Cadaver | Oxford (Biomet) | Concerning the treatment of periprosthetic tibial plateau fractures in UKA, angle-stable plates provides better initial stability than fixation with cannulated screws | Good |
| Pegg et al. [71] | UK | FE model and Sawbone | Oxford (Biomet) | This study suggests that excessive resection depth and making the vertical cut too deep posteriorly increase the risk for periprosthetic tibial fractures in UKA | Good |
| Houskamp et al. [39] | USA | Sawbone | Metal-backed fixed-bearing (Stryker) | In UKA, tibial resections beyond 5.82 mm increase the risk of periprosthetic fractures | Good |
UKA unicompartmental knee arthroplasty; NR not reported
*Quality Appraisal for Cadaveric Studies (QUACS) Scale was used as a quality assessment tool
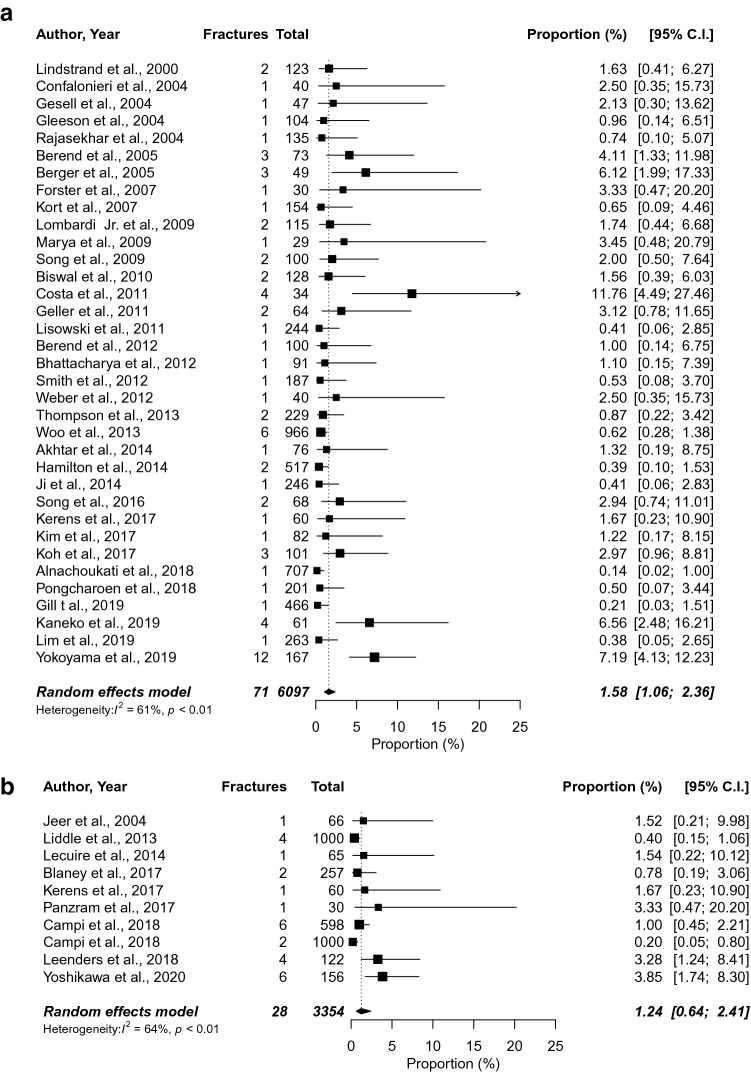
Incidence of fixation type
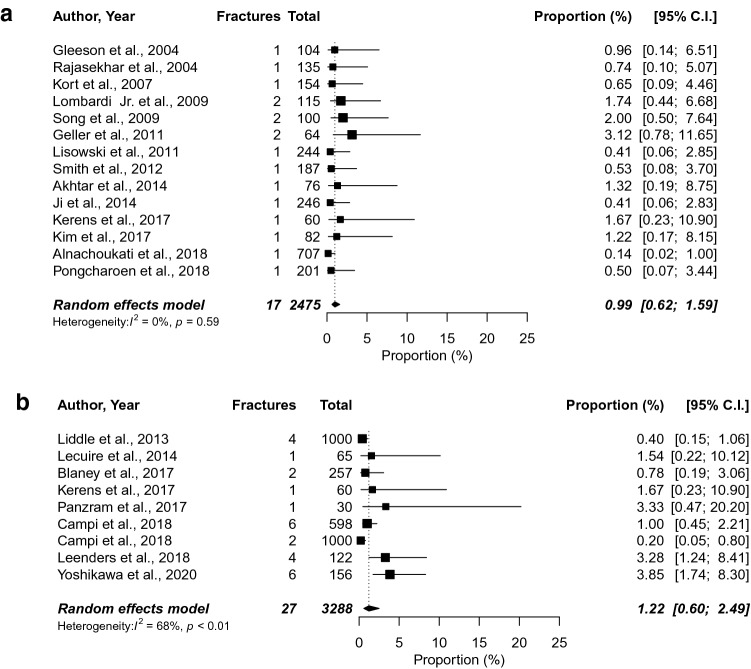
The incidence of each fixation type was determined using 44 clinical studies [1, 3, 5–10, 17, 18, 22, 23, 28, 30–33, 36, 43–46, 48, 50, 51, 53–59, 61, 70, 72, 73, 83–86, 89, 91, 93, 96], leading to a incidence of 1.24% (95% CI 0.64–2.41) for cementless and 1.58% (95% CI 1.06–2.36) for cemented UKAs (Fig. 2). Subgroup analysis for the Oxford Partial Knee implants was performed using 21 clinical studies [1, 3, 10, 17, 18, 30, 33, 44, 46, 48, 51, 53–55, 58, 59, 70, 72, 73, 83, 85, 96], resulting in an incidence of 1.22% (95% CI 0.60–2.49) for cementless and 0.99% (95% CI 0.62–1.59) for cemented fixation (Fig. 3).
Fig. 2.
Proportion meta-analysis to estimate the incidence of fractures in cemented (a) and cementless (b) unicompartmental knee arthroplasty
Fig. 3.
Proportion meta-analysis to estimate the incidence of fractures in cemented (a) and cementless (b) Oxford Partial Knee unicompartmental knee arthroplasty
Characteristics
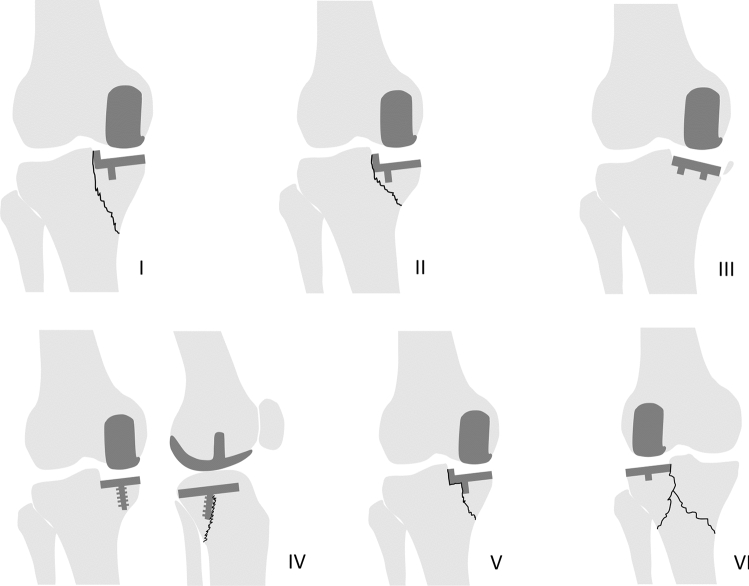
A total of 202 periprosthetic tibial fractures in UKA were reported in 58 clinical studies [1–4, 6–11, 13, 14, 17, 18, 22–25, 27, 28, 30–33, 36, 37, 43–48, 50, 51, 53–59, 61, 70, 72, 73, 77, 78, 83–86, 88, 89, 91, 93, 95, 96] and ten case reports [15, 40, 52, 60, 69, 74, 81, 82, 87, 92]. The time of fracture was noted for 127 fractures. Twenty-three fractures (18%) occurred during the operation, 68 (54%) presented within 3 months postoperatively, 19 (15%) presented between 4 and 12 months postoperatively, and 17 (13%) presented after 1 year postoperatively. Fracture mechanism was reported for 113 fractures with 95 (84%) being non-traumatic.
Twenty-one fractures (10%) had good-quality radiographs to assess the location of the fracture line [6, 14, 33, 40, 45, 48, 52, 69, 74, 81, 85, 87, 88, 92]. Schematic drawings of the different fracture types are displayed in Fig. 4.
Fig. 4.
Periprosthetic tibial fracture types in unicompartmetnal knee arthroplasty (UKA) seen on radiographs. I–II: Fracture line extending from the corner of the tibial resection to the medial cortex, resulting in a large (I) or small (II) medial plateau fracture. These fracture lines were identified on the anteroposterior (AP) view in patients with different implant designs. III: Varus subsidence or anterior subsidence of the tibia component, resulting in a small medial fragment fracture. These fractures were identified on the AP view. IV: Fracture line extending from the screw fixation to the posterior cortex, resulting in a posteromedial plateau fracture. The fracture line could not be identified on the AP view but only on the lateral view in a patient with a cementless fixed-bearing UKA with screw fixation. V: Fracture line extending from the tibial keel to the medial cortex, resulting in a medial plateau fracture. These fracture lines were identified on the AP view in patients with Oxford Partial Knee implants. VI: Two fracture lines extending from the corner of the tibial resection to the medial and lateral cortex after traumatic event six years postoperatively, resulting in a bicondylar plateau fracture. The fracture line was identified on the AP view in a patient with a lateral UKA
Based on information from 167 fractures, 85 (51%) periprosthetic tibial fractures were treated with TKA (with metal augmentation and/or tibial stem extension), 38 (23%) with ORIF, and 44 (26%) with conservative treatment. Authors reported that eight fractures, initially treated conservatively, underwent a subsequent TKA; six fractures, initially treated with ORIF, underwent a subsequent TKA; one fracture, initially treated conservatively, underwent ORIF; and one fracture, initially treated conservatively, underwent ORIF and eventually needed a TKA.
Risk factors
Factors related to periprosthetic tibial fractures in UKA were analyzed using 23 clinical studies Table 2 [1, 8–10, 13, 18, 23–25, 28, 31, 32, 37, 43, 47, 48, 57, 61, 86, 89, 91, 93, 96]. Fractures were associated with increased BMI (p = 0.017), advanced age (p = 0.003), decreased bone mineral density (BMD) (p = 0.030), female gender (p = 0.011), increased postoperative tibia-femoral alignment (p = 0.0120) and a very overhanging medial tibial condyle (< 0.001). The definition of a very overhanging medial tibial condyle was based on the medial eminence line (MEL) described by Yoshikawa et al. [96]. The MEL is a line drawn on preoperative radiographs, that is parallel to the tibial axis passing through the tip of medial intercondylar eminence. If this line passes medial to the medial cortex of the tibia, knees were classified as having a very overhanging medial tibial condyle. Fractures were not associated with the postoperative level of patient activity (p = 0.976) or with the tibial component alignment angle in the coronal plane (p = 0.130).
Table 2.
Results of the comparison between UKAs without and with fractures
| No. of clinical studies | Group | No. of knees | Mean ± SD or % | P value§ | |
|---|---|---|---|---|---|
| Body mass index (kg/m2) | 4 | UKAs without fractures | 1379 | 26.3 ± 6.8* | 0.017 |
| UKAs with fractures | 12 | 31.0 ± 6.8 | |||
| Age (yrs) | 14 | UKAs without fractures | 2701 | 64.4 ± 9.2* | 0.003 |
| UKAs with fractures | 24 | 70.0 ± 9.2 | |||
| Bone mineral density (g/m2) | 1 | UKAs without fractures | 155 | 0.73 ± 0.10 | 0.030 |
| UKAs with fractures | 12 | 0.65 ± 0.16 | |||
| Tibial component angle (°) | 1 | UKAs without fractures | 155 | 4.19 ± 2.94 | 0.130 |
| UKAs with fractures | 12 | 2.83 ± 2.69 | |||
| Postoperative Tibia-femoral Angle (°) | 1 | UKAs without fractures | 155 | 176.5 ± 3.6 | 0.012 |
| UKAs with fractures | 12 | 179.3 ± 3.3 | |||
| Gender (Female/Male) | 20 | UKAs without fractures | 5910 | 67%/33% | 0.011 |
| UKAs with fractures | 58 | 83%/17% | |||
| Activity level (High/Low) # | 1 | UKAs without fractures | 566 | 20%/80% | 0.976 |
| UKAs with fractures | 10 | 20%/80% | |||
| Very overhanging medial tibial condyle (Yes/No) † | 1 | UKAs without fractures | 150 | 12%/88% | < 0.001 |
| UKAs with fractures | 6 | 67%/33% |
§Chi square test was used for categorical variables and the independent t test for continuous variables
#Patients with an UCLA (University of California Los Angeles) activity score > 6 were classified as high
*The weighted mean of the overall UKA population with the same standard deviation as the tibial plateau fracture cases was used to allow for a fair comparison. This means this is an estimation and not the exact mean with standard deviation of the UKAs without fractures
†Very overhanging medial tibial condyle was defined as a medial eminence line outside the medial cortex of the tibial shaft as described by Yoshikawa et al.[95]
Authors considerations
Authors reported their considerations of cause of fracture in 36 clinical studies [1, 2, 4–11, 13, 14, 17, 18, 23, 30, 31, 33, 36, 37, 43–45, 54, 55, 57, 61, 70, 84, 85, 88, 89, 91, 93, 95, 96] and nine case reports [15, 40, 52, 60, 69, 74, 81, 82, 87, 92] (Table 3).
Table 3.
Factors associated with periprosthetic tibial fractures considered by authors
| Implant and surgical factors |
|---|
| Excessive postoperative alignment angle |
| Pin placement (excessive pins, not predrilled, too close to medial tibial cortex) |
| Excessive tibial bone resection |
| Vertical saw cut too distal in posterior tibial cortex |
| Excessive posterior slope |
| Error in keel preparation |
| Learning curve/introduction of new implant |
| Limited instrumentation |
| Not enough medialization of the tibial component to tibial spine |
| Tibial peg hole drilled too deeply |
| All-polyethylene design |
| Tibial subsidence or collapse |
| Undersizing or oversizing of tibia component |
| Forceful impaction |
| Patient factors |
| Infection |
| Osteoporosis |
| Overweight |
| Small tibial size |
| Very overhanging medial tibial condyles |
| Trauma |
| Rehabilitation factor |
| Weightbearing too early |
Discussion
The main study finding was that the incidence of periprosthetic tibial fractures in cemented and cementless UKA was comparable. However, experimental evidence showed that excessive interference fit (press fit), excessive resection depth, making the sagittal cut too deep posteriorly, and low BMD reduces the load required for a periprosthetic tibial fracture to occur. Furthermore, clinical studies revealed that patients with fractures were more often female, of older age, exhibited higher BMI and postoperative alignment angles, had lower BMD and had very overhanging medial tibial condyles.
Contrarily to the main finding of this study, two recent registry-based studies showed higher rates of periprosthetic fractures in cementless compared to cemented Oxford Partial Knee implants [49, 63], raising some concerns regarding a keel design in cementless techniques. Campi et al. demonstrated that fixation of the cementless mobile-bearing Oxford UKA is ensured by the interference fit [18]. However, an excessive interference increases the assembly load required to push-in the component potentially introducing a splitting force during impaction (type V fracture) [16]. As this interference fit, combined with an impaction technique, could introduce an additional risk factor for fractures, the cementless Oxford Partial Knee implant may be less forgiving to surgical errors and patients who are at higher risk of periprosthetic tibial fractures.
Several surgical errors have been proposed by authors to cause periprosthetic tibial fractures in UKA Table (3). Only a few authors have supported their conclusion with experimental evidence. Laboratory studies showed a vertical saw cut too distal in the posterior tibial cortex and excessive tibial bone resection reduces the load required for a fracture to occur [20, 21, 39, 71]. Additionally, laboratory studies on the role of tibial component alignment suggested valgus alignment and an excessive posterior slope should be avoided [41, 42, 76]. Other authors based their conclusions on radiographic or intraoperative findings. Radiographs revealed that fracture lines went through multiple pinholes of the extramedullary tibial guide (type II fracture) [15]. One author reported that a fracture occurred due to breaching the posterior cortex while using a tibial gouge for keel preparation in Oxford Partial Knee implants (type V fracture) [82]. Furthermore, one fracture occurred after breaching the tibial cortex with the screw to fixate a cementless fixed-bearing UKA (type VI) [87]. These findings indicate that surgical actions that weaken cortical bone or reduce the bony area under the tibial component increase the risk of fracture. However, more studies evaluating fractures under different conditions in UKA are necessary to understand the main pathologic elements of periprosthetic tibial fractures.
It was further noted that female gender, higher BMI and age, osteoporosis, excessive postoperative alignment angles and a very overhanging medial tibial condyle could contribute to the occurrence of periprosthetic tibial fractures in UKA. The relationship with greater age and osteoporosis is not surprising as fractures have been directly linked to these factors [12]. The higher proportion of periprosthetic tibial fractures in females compared to males may be due to higher rate of osteoporosis[12], the smaller average size of tibial plateaus [97] and the higher likelihood of having very overhanging medial tibial condyles [38, 96] in females. The two latter reasons reduce the bone volume to support the tibial component which may increase the risk of fracture. As such, surgeons should avoid large tibial resections as well as peripheral positioning [39], especially in those with already little bone volume to support the tibial component. Further, the relationship of higher BMI and excessive postoperative alignment angles with periprosthetic tibial fractures may be explained by the excessive loads placed on the small tibial surface [40, 74, 84]. In addition, small medial femoral condyles needing small components might also be a risk factor leading to overload because of smaller contact areas at the medial tibial surface [34].
Despite surgeons should be aware of potential risk factors, current evidence underlines developments in instrumentation and implants can minimize fracture risk. Chang et al. showed a modified technique using a predrilled tunnel through the tibia prior to cutting could avoid extended vertical saw cut errors [19]. Campi et al. suggested the optimal interference fit for good implant stability and minimal risk of fracture is between 0.5 mm and 0.7 mm [16]. Mohammad et al. reported improvements in instrumentation that widen the keel slot could reduce the risk of tibial fractures in cementless Oxford Partial Knee implants without compromising fixation [64]. Some authors suggested to change the depth of the tibial keel in very small cementless Oxford Partial Knee components as the depth of the keel is currently the same in all components, increasing the risk of fracture [38]. Vardi et al. reported that a change was made to the shape and size of the tibial keel of the Alphanorm implant due to high rates of periprosthetic tibial fractures [88].
This study revealed that most of periprosthetic tibial fractures occurred intraoperatively or within 3 months of surgery and were non-traumatic. Studies of intraoperative fractures described that operative damage in combination with the impaction of the tibial component caused the tibial bone to fracture. The postoperative fractures within 3 months may be associated with operative damage and repetitive stress on the bone during daily activities such as walking and stair climbing. Fractures that presented after 3 months were mostly associated with traumatic events, excessive weight, osteoporosis, infection, all-polyethylene designs and tibial component malposition.
Furthermore, a classification of periprosthetic tibial fracture types was presented. As only 10% of all fractures could be used in the classification, the incidence and completeness of fracture types in UKA remain unknown. However, presented paths of fractures could explain the high-risk fracture regions. For example, the type I fracture not only suggest that an extended sagittal cut posteriorly can initiate a fracture, but indicate that risk of fracture propagation can be increased by placing pins from the extramedullary tibial guide within fracture line regions.
Some limitations of this study should be noted. First, the pooled estimated incidences of fractures were not adjusted for the follow-up period. However, almost all clinical studies had a minimum follow-up of one year and thus included the period when the majority of fractures occurred. Second, poor reporting on characteristics of fractures may have biased the results. Third, not all risk factors for fractures in UKA mentioned by authors have been verified with clinical data, and therefore might be subjective. Also, it cannot be clarified which risk factors verified with clinical data were independently related to periprosthetic tibial fractures as the findings were based on unadjusted analyses. Fourth, to analyze whether increased BMI and age were related to fracture cases, the weighted mean of the overall UKA population was used with the same standard deviation as those of the periprosthetic tibial fracture cases. Although this approach can be considered a fair approximation, the statistical difference for BMI and age between UKAs with and without fractures may have been underestimated. Finally, this study did not focus on the diagnostics and treatment of periprosthetic tibial fracture in UKA. However, based on the current search, three studies have currently evaluated the management of periprosthetic tibial fractures in UKA [14, 80, 91]. Treatments of the included fracture cases were reported to give a complete overview. Despite the aforementioned limitations, this is the first study evaluating the incidence of periprosthetic tibial fractures in cemented and cementless UKAs and providing an overview of the available evidence on periprosthetic tibial fracture in UKA.
Conclusion
The incidence of periprosthetic tibial fractures in cementless UKAs can be similar to those seen in cemented UKAs. However, surgeons should be aware that an excessive interference fit for cementless UKAs in combination with an impaction technique may introduce an additional risk, and may, therefore, be less forgiving to surgical errors and patients who are at higher risk of periprosthetic tibial fractures. While findings of this study raise awareness about periprosthetic tibial fractures in UKA, this study also highlights the importance of improvements in instrumentation and implants to prevent periprosthetic tibial fractures in future practices.
Appendix
Table 4.
Summary of case reports
| Study | Country | No. cases | Time point | UKA Laterality | Trauma | Gender | BMI (kg/m2) |
Osteop | Age (year) | Implant | Cement | Treatment | Study Quality* |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brumby et al. [15] | Australia / USA | 4 |
6 wks 3 mo 3 mo 3 wks |
Medial Medial Medial Medial |
No No No No |
Female Female Male Female |
NR NR NR NR |
Yes NR NR NR |
72 57 65 62 |
NR, Fixed bearing NR NR NR |
Yes Yes Yes Yes |
Conservative > TKA Conservative > TKA Conservative > TKA TKA |
Fair |
| Rudol et al. [74] | UK | 1 | 2 wks | Medial | No | Male | NR | NR | 80 | Oxford Phase 3 (Biomet) | Yes | ORIF | Fair |
| Lu et al. 2019 | China | 2 |
3 wks 2 wks |
Medial Medial |
No No |
Male Female |
NR NR |
Yes Yes |
70 72 |
NR NR |
NR NR |
ORIF Conservative |
Fair |
| Seon et al. [81] | South Korea | 2 |
3 wks 5 wks |
Medial Medial |
No No |
Female Female |
29.6 32.1 |
Yes Yes |
65 68 |
Miller Galante (Zimmer) Miller Galante (Zimmer) |
Yes Yes |
ORIF TKA |
Fair |
| Sloper et al. [82] | UK | 1 | Intraop | Medial | No | Male | NR | No | 58 | Oxford (Biomet) | -Yes | -ORIF | Fair |
| Kumar et al. [52] | Canada | 1 | 6 years | Lateral | Yes | Female | NR | Yes | 70 | NR | Yes | TKA | Good |
| Van Loon et al. [87] | Belgium | 3 |
6 days Intraop Intraop |
Medial Medial Medial |
No No No |
Female Female Female |
NR NR NR |
NR NR NR |
62 57 45 |
Accuris (Smith & Nephew) NR Profix (Smith & Nephew) |
NR NR NR |
ORIF > TKA Conservative > TKA TKA |
Fair |
| Yang et al. [92] | Singapore | 2 |
5 mo 3 mo |
Medial Medial |
No No |
Female Male |
NR NR |
NR NR |
60 71 |
PFC Sigma (Johnson Johnson) PFC Sigma (Johnson Johnson) |
NR NR |
TKA Conservative |
Fair |
| Pandit et al. [69] | UK | 8 |
Intraop 6 wks 10 wks Intraop 4 wks 12 wks 24 wks 16 wks |
Medial Medial Medial Medial Medial Medial Medial Medial |
No No No No No No No No |
Female Male Female Female Male Male Female Female |
NR NR NR NR NR NR NR NR |
NR NR NR NR NR NR NR NR |
72 65 55 73 82 67 76 67 |
Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) |
NR NR NR NR NR NR NR NR |
Conservative Conservative ORIF Conservative > ORIF > TKA Conservative > TKA Conservative > TKA TKA TKA |
Fair |
| Yuk Wah et al. 2018 | China | 1 | 4 wks | Medial | No | F emale | NR | yes | 75 | ZUK (Zimmer Biomet) | Yes | ORIF > TKA | Good |
UKA unicompartmental knee arthroplasty; BMI body mass index; ORIF open reduction internal fixation; NR not reported; TKA total knee arthroplasty
*Quality Appraisal for Cadaveric Studies (QUACS) checklist was used as a quality assessment tool
Table 5.
Summary of clinical studies
| Study | Country | UKA population | Fracture cases | Study design | Quality* | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (Knees) | Mean BMI | Mean Age | Female (%) | No. cases | Time point | UKA Laterality | Trauma | Gender | BMI (kg/m2) | Osteop | Age (yrs) | Implant | Cement | Treatment | ||||
| Akhtar et al. [1] | UK | 76 | 30 | 64 | 58 | 1 | -2 mo | -Medial | -Yes | -Male | -29.8 | -NR | -78 | -Oxford (Biomet) | -Yes | -ORIF | Case series, retrospective | Good |
| Aleto et al. [2] | USA | NR | NR | NR | NR | 15 |
-16 mo -14 NR |
-15 Medial | -15 NR | -15 NR | -15 NR | - 15 NR | - 15 NR | -15 NR | -15 NR | -15 TKA | Case series, retrospective | Fair |
| Alnachoukati et al. [3] | USA | 707 | 32 | 64 | 45 | 1 | -9.6 yrs | -Medial | -NR | -NR | -NR | -NR | -NR | -Oxford Phase 3 (Biomet) | -Yes | -NR | Case series, retrospective | Good |
| Argenson et al. [4] | France | 38 | 26 | 61 | 62 | 1 | -11 mo | -Lateral | -No | -NR | -NR | -NR | -NR | -Fixed-bearing, metal-backed | -Yes | -TKA | Case series, retrospective | Good |
| Berend et al. [5] | USA | 100 | 30 | 68 | 70 | 1 | -2 yrs | -Lateral | -Yes | -NR | -NR | -NR | -NR | -Repicci II/VanguardM (Biomet) | -Yes | -ORIF | Case series, retrospective | Good |
| Berend et al. [6] | USA | 73 | 32 | 66 | 77 | 3 |
-1 mo -NR -NR |
-Medial -Medial -Medial |
-No -No -No |
-Female -NR -NR |
-24.9 -NR -NR |
-NR -NR -NR |
-72 -NR -NR |
-Fixed-bearing -Fixed-bearing -Fixed-bearing |
-Yes -Yes -Yes |
-NR -NR -NR |
Case series, retrospective | Good |
| Berger et al. [7] | USA | 49 | NR | 68 | 67 | 3 |
-Intraop -Intraop -Intraop |
-Medial -Medial -NR |
-No -No -No |
-NR -NR -NR |
-NR -NR -NR |
-NR -NR -NR |
-NR -NR -NR |
-Miller-Galante (Zimmer) -Miller-Galante (Zimmer) -Miller-Galante (Zimmer) |
-Yes -Yes -Yes |
-Conservative -ORIF -Conservative |
Case series, prospective | Good |
| Bhattacharya et al. [8] | UK | 91 | NR | 68 | 58 | 1 | -31 mo | -Medial | -Yes | Male | -NR | -NR | -65 | -Preservation (DePuy) | -Yes | TKA | Case series, retrospective | Good |
| Biswal et al. [9] | Australia | 128 | 29 | 68 | 49 | 2 |
-10 mo -50 mo |
-Medial -Medial |
-No -Yes |
-NR -NR |
-36.0 -40.1 |
-No -Yes |
-58 -57 |
-Allegretto (Zimmer) -Allegretto (Zimmer) |
-Yes -Yes |
-TKA -TKA |
Case series, retrospective | Good |
| Blaney et al. [10] | UK | 257 | 30 | 65 | 48 | 2 |
-2 wks -13 mo |
-Medial -Medial |
-No -Yes |
-Female -Male |
-NR -NR |
-NR -NR |
-NR -NR |
-Oxfort (Biomet) -Oxfort (Biomet) |
-No -No |
-ORIF -ORIF |
Case series, retrospective | Good |
| Bohm et al. [11] | Austria | 278 | NR | NR | NR | 1 | -1 wk | -Medial | -No | -NR | -NR | -NR | -NR | -NR | -NR | -TKA | Case series, retrospective | Good |
| Bonutti et al. [13] | USA | 80 | 33 | 66 | 45 | 1 | -9 mo | -Medial | -No | -Male | -NR | -NR | -NR | -Fixed-bearing | -NR | -TKA | Cohort study, retrospective | Good |
| Brown et al. [14] | USA | 2464 | NR | NR | NR | 16 | -Mean: 35 dys |
-15 Medial -1 Lateral |
-2 No -14 NR |
-11 Female -5 Male |
-Mean: 32 |
-2 yes -14 NR |
-92 -87 -14 NR |
-16 NR | -16 NR |
-2 conservative -7 ORIF -2 ORIF > TKA -6 TKA |
Case series, retrospective | Good |
| Campi et al. [16] | South Africa |
522 cem 598 cem. less |
NR | 65 | 49 | 6 | -NR | -6 Medial | -6 NR | -6 Female | -6 NR | -6 NR | -6 NR | -6 Oxford (Biomet) | -6 No |
-4 ORIF -2 TKA |
Case series, prospective | Good |
| Campi et al. [16] | UK / New Zealand | 1000 | NR | 66 | 45 | 2 |
-1 mo -2 mo |
-Medial -Medial |
-No -No |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-Oxford (Biomet) -Oxford (Biomet) |
-No -No |
-TKA -TKA |
Case series, prospective | Good |
| Confalonieri et al. [22] | Italy | 40 | NR | 70 | 53 | 1 | -Intraop | -Medial | -No | -NR | -NR | -NR | -NR | -AMC (Corin) | -Yes | -ORIF | RCT, prospective | Fair |
| Costa et al. [23] | USA | 34 | 30 | 73 | 44 | 4 |
-2 mo -3 mo -6 mo -18 mo |
-Medial -Medial -Medial -Medial |
-No -No -No -No |
-Female -Female -Female -Male |
-NR -NR -NR -NR |
-Yes -Yes -Yes -No |
-64 -78 -61 -NR |
-EIUS (Stryker) -EIUS (Stryker) -EIUS (Stryker) -EIUS (Stryker) |
-Yes -Yes -Yes -Yes |
-TKA -TKA -TKA -TKA |
RCT, prospective | Fair |
| Crawford et al. [24] | USA | 576 | 32 | 62 | 59 | 10 | -10 NR | - 10 Medial | -10 NR | -10 NR | -10 NR | -10 NR | -10 NR | -10 Oxford (Zimmer) | -10 NR | -10 TKA | Cohort study, retrospective | Fair |
| Darrith et al. [25] | USA | 178 | 31 | 55 | 37 | 1 | -NR | -NR | -NR | -Male | -NR | -NR | -68 | -NR | -NR | -Conservative | Cohort study, retrospective | Fair |
| Epinette et al. [27] | France | NR | NR | NR | NR | 15 | -15 NR | -15 NR |
-5 yes -10 No |
-15 NR | -15 NR | -15 NR | -15 NR | -15 NR | -15 NR | -15 NR | Case series, retrospective | Fair |
| Forster et al. [28] | Australia | 30 | NR | 67 | 53 | 1 | -Intraop | -Lateral | -No | -Female | -NR | -Yes | -80 | -Fixed-bearing | -Yes | -Conservative | Cohort study, prospective | Fair |
| Geller et al. [30] | USA | 64 | 31 | 67 | 59 | 2 |
-NR -1 yr |
-Medial -Medial |
-No -Yes |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-Fixed-bearings -Fixed-bearings |
-Yes -Yes |
-TKA -TKA |
Cohort study, prospective | Good |
| Gesell et al. [31] | USA | 47 | NR | 68 | 59 | 1 | -10 dys | -Medial | -NR | -Medial | -NR | -NR | -NR | -Miller-Galante (Zimmer) | -Yes | -Conservative | Case series, retrospective | Good |
| Gill et al. [32] | UK | 466 | 29 | 67 | 49 | 1 | -3 mo | -Medial | -No | -Female | -NR | -NR | -77 | -Physica ZUK (LIMA) | -Yes | -TKA | Case series, prospective | Good |
| Gleeson et al. [33] | UK | 104 | NR | 66 | 50 | 1 | -8 mo | -Medial | -No | -NR | -NR | -NR | -NR | -NR | -Yes | -TKA | RCT, prospective | Poor |
| Hamilton et al. [36] | USA | 517 | 29 | 66 | 62 | 2 |
-5 mo -2 yrs |
-Medial -Medial |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-Preservation (DePuy) -Preservation (DePuy) |
-Yes -Yes |
-TKA -TKA |
Case series, retrospective | Good |
| Hamilton et al. [37] | USA | 221 | 29 | 66 | 59 | 3 |
-2 mo -3 mo -14 mo |
-Medial -Medial -Medial |
-No -No -No |
-Female -Male -Male |
-33 -37 -27 |
-NR -NR -NR |
-64 -61 -69 |
-Preservation (DePuy) -Preservation (DePuy) -Preservation (DePuy) |
-NR -NR -NR |
-TKA -TKA -TKA |
Case series, retrospective | Good |
| Jeer et al. [43] | Australia | 66 | NR | 69 | NR | 1 | -2 wks | -Medial | -No | -Female | -NR | -NR | -64 | -LCS (Depuy) | -No | -Consrevative > TKA | Case series, retrospective | Good |
| Ji et al. [44] | South Korea | 246 | NR | 64 | 84 | 1 | -Intraop | -Medial | -No | -NR | -NR | -NR | -NR | -Oxford (Biomet) | -Yes | -Consrevative > TKA | Case series, retrospective | Good |
| Kaneko et al. [45] | Japan | 61 | NR | 74 | 73 | 4 |
-6 mo -7 mo -2 yr -5 yr |
-Medial -Medial -Medial -Medial |
-Yes -No -No -No |
-Female -NR -NR -NR |
-NR -NR -NR -NR |
-NR -NR -NR -NR |
-74 -NR -NR -NR |
-Physica ZUK (LIMA) -Physica ZUK (LIMA) -Physica ZUK (LIMA) -Physica ZUK (LIMA) |
-Yes -Yes -Yes -Yes |
-TKA -Conservative -Conservative -Conservative |
Case series, retrospective | Good |
| Kerens et al. [46] | Holland |
60 cem. less 60 cem |
30 | 63 | 51 | 2 |
-1 mo -2 mo |
-Medial -Medial |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-Oxford (Biomet) -Oxford (Biomet) |
-Yes -No |
-TKA -NR |
Cohort study, retrospective | Fair |
| Kim et al. [47] | South Korea | 1576 | NR | 62 | 90 | 5 |
-Intraop -NR -NR -NR -NR |
-Medial -Medial -Medial -Medial -Medial |
-No -No -Yes -Yes -Yes |
-Female -Female -Female -Female -Female |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-ORIF -ORIF -ORIF -ORIF > TKA -TKA |
Case series, retrospective | Good |
| Kim et al. [48] | South Korea | 82 | 26 | 55 | 95 | 1 | -7 yrs | -Medial | -NR | -Female | -NR | -NR | -60 | -Oxford Phase 3 (Biomet) | -Yes | -TKA | Case series, retrospective | Good |
| Koh et al. [50] | South Korea | 101 | 26 | 62 | 89 | 3 |
-NR -NR -NR |
-Medial -Medial -Medial |
-NR -NR -NR |
-NR -NR -NR |
-NR -NR -NR |
-NR -NR -NR |
-NR -NR -NR |
-Fixed-bearing -Fixed-bearing -Fixed-bearing |
-Yes | -NR | Cohort study, retrospective | Fair |
| Kort et al. [51] | Holland | 154 | NR | 56 | 67 | 1 | -4 wks | -Medial | -Yes | -NR | -NR | -NR | -NR | -Oxford Phase 3 (Biomet) | -Yes | -Conservative | Case series, prospective | Good |
| Lecuire et al. [53] | France | 65 | 28 | 72 | 72 | 1 | -Intraop | -Medial | -No | -NR | -NR | -NR | -NR | -Alpina (Biomet) | -No | -ORIF | Case series, retrospective | Good |
| Leenders et al. [54] | Holland | 122 | 29 | 63 | 70 | 4 |
-1 mo -1.5 mo -4 mo -5 mo |
-Medial -Medial -Medial -Medial |
-NR -NR -NR -NR |
-NR -NR -NR -NR |
-NR -NR -NR -NR |
-NR -NR -NR -NR |
-NR -NR -NR -NR |
-Oxford Phase3 (Biomet) -Oxford Phase3 (Biomet) -Oxford Phase3 (Biomet) -Oxford Phase3 (Biomet) |
-No -No -No -No |
-ORIF -Conservative -TKA -TKA |
Case series, retrospective | Fair |
| Liddle et al. [55] | UK | 1000 | NR | 66 | 43 | 4 |
-Intraop -Intraop -Intraop -Intraop |
-Medial -Medial -Medial -Medial |
-No -No -No -No |
-Male -NR -NR -NR |
-NR -NR -NR -NR |
-NR -NR -NR -NR |
-62 -NR -NR -NR |
Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) Oxford (Biomet) |
-No -No -No -No |
-Conservative -TKA -TKA -ORIF |
Case series, prospective | Good |
| Lim et al. [56] | Singapore | 263 | 26 | 63 | 72 | 1 | 18 mo | Medial | NR | -NR | NR | NR | NR | Fixed-bearing | -Yes | -TKA | Case series, prospective | Fair |
| Lindstrand et al. [57] | Sweden | 123 | NR | 72 | 70 | 2 |
9 mo 13 mo |
-Medial -Medial |
-No -Yes |
-Female -Female |
-NR -NR |
-NR -NR |
-71 -77 |
-Fixed-bearing |
-Yes -Yes |
-NR -NR |
Case series, prospective | Good |
| Lisowski et al. [58] | Holland | 244 | 28 | 72 | NR | 1 | -Intraop | -Medial | -No | -NR | -NR | -NR | -NR | -Oxford Phase 3 (Biomet) | -Yes | -Conservative | Case series, prospective | Good |
| Lombardi Jr et al. [59] | USA | 115 | 31 | 61 | 63 | 2 |
-7 mo -22 mo |
-Medial -Medial |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-Oxford Phase 3 (Biomet) -Oxford Phase 3 (Biomet) |
-Yes -Yes |
-TKA -TKA |
Cohort study, retrospective | Good |
| Marya et al. [61] | India | 29 | NR | 83 | 16 | 1 | -Intraop | -Medial | -No | -Male | -NR | yes | 87 | -Allegretto (Zimmer) | -Yes | -ORIF | Case series, prospective | Good |
| Panzram et al. [70] | Germany | 30 | 28 | 63 | 44 | 1 | -1 mo | -Medial | -No | -NR | -NR | NR | NR | -Oxford (Biomet) | -No | -ORIF&UKA | Case series, retrospective | Good |
| Pongcharoen et al. [72] | Thailand | 201 | 27 | 64 | 75 | 1 | -3 mo | -Medial | -NR | -NR | -NR | NR | NR | -Oxford (Zimmer-Biomet) | -Yes | NR | Cohort study, retrospective | Good |
| Rajasekhar et al. [73] | UK | 135 | NR | 70 | 57 | 1 | -Intraop | -Medial | -No | -NR | -NR | NR | NR | -Oxford Phase 2 (Biomet) | -Yes | -ORIF | Case series, retrospective | Fair |
| Saxler et al. [77] | Germany | 361 | NR | 70 | 67 | 1 | -Intraop | -Medial | -No | -NR | -NR | NR | NR | -AMC (Corin) | -NR | -ORIF | Case series, prospective | Good |
| Schotanus et al. [54] | Holland | NR | NR | NR | NR | 1 | -7.1 yrs | -Medial | -NR | -Female | -NR | NR | 58 | -NR | -NR | -TKA | Case series, prospective | Good |
| Smith et al. 2012 | UK | 187 | NR | 65 | 68 | 1 | -Intraop | -Medial | -NR | -NR | -NR | -NR | -NR | -Oxford Phase 3 (Biomet) | -Yes | -TKA | Case series, retrospective | Good |
| Song et al. [44] | South Korea | 68 | 26 | 64 | 96 | 2 |
-5 wks -7 wks |
-Medial -Medial |
-No -No |
-NR -Female |
-NR -NR |
-NR -Yes |
-NR -76 |
-Miller-Galante (Zimmer) -Miller-Galante (Zimmer) |
-Yes -Yes |
-Conservative -TKA |
Cohort study, prospective | Good |
| Song et al [85] | South Korea | 100 | 26 | 66 | 87 | 2 |
-4 wks -NR |
-Medial -Medial |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-NR -NR |
-Oxford Phase 3 (Biomet) -Oxford Phase 3 (Biomet) |
-Yes -Yes |
-TKA -TKA |
Case series, retrospective | Fair |
| Thompson et al. [86] | USA | 229 | 29 | 66 | 60 | 2 |
-18 dys -28 dys |
-Medial -Lateral |
-NR -NR |
-Female -Female |
-NR -NR |
-NR -NR |
-81 -68 |
-NR -NR |
-Yes -Yes |
-TKA -TKA |
Case series, prospective | Fair |
| Vardi et al. [88] | UK | 206 | NR | 64 | 37 | 5 |
-Intraop -6 wks -6 wks -6 wks -6 mo |
-Lateral -NR -NR -NR -NR |
-No -No -No -No -No |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-NR -NR -NR -NR -NR |
-ORIF > TKA -TKA -TKA -TKA -Conservative |
Case series, retrospective | Fair |
| Weber et al. [89] | Germany | 40 | 30 | 69 | 52 | 1 | -6 wks | -Medial | -No | -Female | -NR | -Yes | -89 | -Univation (Aesculap) | -Yes | -TKA | Cohort study, prospective | Good |
| Woo et al. [91] | Singapore | 966 | 25 | 62 | 75 | 6 |
-1 mo -1 mo -1 mo -1 mo -1 mo -5 mo |
-Medial -Medial -Medial -Medial -Medial -Medial |
-No -No -No -No -No -Yes |
-Female -Female -Female -Female -Female -Female |
-19.3 -29.5 -24.3 -33 -22.5 -40.1 |
-Yes -Yes -No -No -No -No |
-62 -58 -76 -67 -77 -65 |
-Fixed-bearing -Fixed-bearing -Fixed-bearing -Fixed-bearing -Fixed-bearing -Fixed-bearing |
-Yes -Yes -Yes -Yes -Yes -Yes |
-Conservative -Conservative -Conserative > ORIF -Conservative -Conservative -TKA |
Case series, retrospective | Good |
| Yokoyama et al. [93] | Japan | 167 | NR | 77 | 73 | 12 | -12 NR | -12 Medial | -12 NR | -12 Female | -12 NR | -12 Yes | mean 79,4 | -12 Fixed-bearings | -Yes |
-11 Coservative -1 TKA |
Case series, retrospective | Fair |
| Yoshida et al. [95] | Japan | 1279 | NR | 77 | 82 | 3 |
-0.17 yrs -0.25 yrs -0.67 yrs |
-Medial -Medial -Medial |
-No -No -No |
-NR -NR -NR |
-NR -NR -NR |
-Yes -Yes -No |
-NR -NR -NR |
-Oxford Phase 3 (Biomet) -Oxford Phase 3 (Biomet) -Oxford Phase 3 (Biomet) |
-NR -NR -NR |
-TKA -TKA -TKA |
Case series, prospective | Good |
| Yoshikawa et al. [96] | Japan | 156 | NR | 73 | 70 | 6 | NR | -6 Medial | -6 NR | -6 Female | -6 NR | -6 NR | -6 NR | -Oxford (Biomet) | -6 No | -6 NR | Case series, retrospective | Fair |
UKA unicompartmental knee arthroplasty; BMI body mass index; ORIF open reduction internal fixation; NR not reported; TKA total knee arthroplasty
*Consensus-based Clinical Case Reporting (CARE) checklist was used as a quality assessment tool
Author contributions
JAB performed the literature search, scanned all abstracts and full texts, determined the quality of the studies and wrote the manuscript. TJ screened all abstracts, full texts and determined the quality of the studies as a second author and revised the manuscript. MSD checked data extraction, study quality and revised the manuscript. HAZ, GMMJK and ADP participated in the design of the study and revised manuscript. All authors read and approved the final manuscript.
Funding
There is no funding source.
Compliance with ethical standards
Conflict of interest
Author ADP report consultancy fees from Stryker (Mahwah, NJ, USA) and he has ownership interest in Engage Surgical (Orlando, FL, USA). The other authors (JAB, TJ, MSD, HAZ, GMMJK) report no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Akhtar KS, Somashekar N, Willis-Owen CA, Houlihan-Burne DG. Clinical outcomes of bilateral single-stage unicompartmental knee arthroplasty. Knee. 2014;21:310–314. doi: 10.1016/j.knee.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 2.Aleto TJ, Berend ME, Ritter MA, Faris PM, Meneghini RM. Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty. 2008;23:159–163. doi: 10.1016/j.arth.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 3.Alnachoukati OK, Barrington JW, Berend KR, Kolczun MC, Emerson RH, Lombardi AV, Jr, et al. Eight hundred twenty-five medial mobile-bearing unicompartmental knee arthroplasties: the first 10-Year US multi-center survival analysis. J Arthroplasty. 2018;33:677–683. doi: 10.1016/j.arth.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 4.Argenson JN, Parratte S, Bertani A, Flecher X, Aubaniac JM. Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res. 2008;466:2686–2693. doi: 10.1007/s11999-008-0351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berend KR, Kolczun MC, 2nd, George JW, Jr, Lombardi AV., Jr Lateral unicompartmental knee arthroplasty through a lateral parapatellar approach has high early survivorship. Clin Orthop Relat Res. 2012;470:77–83. doi: 10.1007/s11999-011-2005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berend KR, Lombardi AV, Jr, Mallory TH, Adams JB, Groseth KL. Early failure of minimally invasive unicompartmental knee arthroplasty is associated with obesity. Clin Orthop Relat Res. 2005;440:60–66. doi: 10.1097/01.blo.0000187062.65691.e3. [DOI] [PubMed] [Google Scholar]
- 7.Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, et al. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87:999–1006. doi: 10.2106/JBJS.C.00568. [DOI] [PubMed] [Google Scholar]
- 8.Bhattacharya R, Scott CE, Morris HE, Wade F, Nutton RW. Survivorship and patient satisfaction of a fixed bearing unicompartmental knee arthroplasty incorporating an all-polyethylene tibial component. Knee. 2012;19:348–351. doi: 10.1016/j.knee.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 9.Biswal S, Brighton RW. Results of unicompartmental knee arthroplasty with cemented, fixed-bearing prosthesis using minimally invasive surgery. J Arthroplasty. 2010;25:721–727. doi: 10.1016/j.arth.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 10.Blaney J, Harty H, Doran E, O'Brien S, Hill J, Dobie I, et al. Five-year clinical and radiological outcomes in 257 consecutive cementless Oxford medial unicompartmental knee arthroplasties. Bone Joint J. 2017;99:623–631. doi: 10.1302/0301-620X.99B5.BJJ-2016-0760.R1. [DOI] [PubMed] [Google Scholar]
- 11.Bohm I, Landsiedl F. Revision surgery after failed unicompartmental knee arthroplasty: a study of 35 cases. J Arthroplasty. 2000;15:982–989. doi: 10.1054/arth.2000.9841. [DOI] [PubMed] [Google Scholar]
- 12.Bonnick SL. Osteoporosis in men and women. Clin Cornerstone. 2006;8:28–39. doi: 10.1016/s1098-3597(06)80063-3. [DOI] [PubMed] [Google Scholar]
- 13.Bonutti PM, Goddard MS, Zywiel MG, Khanuja HS, Johnson AJ, Mont MA. Outcomes of unicompartmental knee arthroplasty stratified by body mass index. J Arthroplasty. 2011;26:1149–1153. doi: 10.1016/j.arth.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Brown NM, Engh G, Fricka K. Periprosthetic fracture following partial knee arthroplasty. J Knee Surg. 2019;32:947–952. doi: 10.1055/s-0038-1672204. [DOI] [PubMed] [Google Scholar]
- 15.Brumby SA, Carrington R, Zayontz S, Reish T, Scott RD. Tibial plateau stress fracture. J Arthroplasty. 2003;18:809–812. doi: 10.1016/s0883-5403(03)00330-9. [DOI] [PubMed] [Google Scholar]
- 16.Campi S, Mellon SJ, Ridley D, Foulke B, Dodd CAF, Pandit HG, et al. Optimal interference of the tibial component of the cementless Oxford Unicompartmental Knee Replacement. Bone Joint Res. 2018;7:226–231. doi: 10.1302/2046-3758.73.BJR-2017-0193.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campi S, Pandit H, Hooper G, Snell D, Jenkins C, Dodd CAF, et al. Ten-year survival and seven-year functional results of cementless Oxford unicompartmental knee replacement: a prospective consecutive series of our first 1000 cases. Knee. 2018;25:1231–1237. doi: 10.1016/j.knee.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 18.Campi S, Pandit HG, Oosthuizen CR. The Oxford medial unicompartmental knee arthroplasty: the South African experience. J Arthroplasty. 2018;33:1727–1731. doi: 10.1016/j.arth.2018.01.035. [DOI] [PubMed] [Google Scholar]
- 19.Chang TW, Yang CT, Liu YL, Chen WC, Lin KJ, Lai YS, et al. Biomechanical evaluation of proximal tibial behavior following unicondylar knee arthroplasty: modified resected surface with corresponding surgical technique. Med Eng Phys. 2011;33:1175–1182. doi: 10.1016/j.medengphy.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 20.Clarius M, Aldinger PR, Bruckner T, Seeger JB. Saw cuts in unicompartmental knee arthroplasty: an analysis of Sawbone preparations. Knee. 2009;16:314–316. doi: 10.1016/j.knee.2008.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Clarius M, Haas D, Aldinger PR, Jaeger S, Jakubowitz E, Seeger JB. Periprosthetic tibial fractures in unicompartmental knee arthroplasty as a function of extended sagittal saw cuts: an experimental study. Knee. 2010;17:57–60. doi: 10.1016/j.knee.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 22.Confalonieri N, Manzotti A, Pullen C. Comparison of a mobile with a fixed tibial bearing unicompartimental knee prosthesis: a prospective randomized trial using a dedicated outcome score. Knee. 2004;11:357–362. doi: 10.1016/j.knee.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Costa CR, Johnson AJ, Mont MA, Bonutti PM. Unicompartmental and total knee arthroplasty in the same patient. J Knee Surg. 2011;24:273–278. doi: 10.1055/s-0031-1280970. [DOI] [PubMed] [Google Scholar]
- 24.Crawford DA, Adams JB, Lombardi AV, Jr, Berend KR. Activity level does not affect survivorship of unicondylar knee arthroplasty at 5-year minimum follow-up. J Arthroplasty. 2019;34:1364–1368. doi: 10.1016/j.arth.2019.03.038. [DOI] [PubMed] [Google Scholar]
- 25.Darrith B, Frisch NB, Tetreault MW, Fice MP, Culvern CN, Della Valle CJ. Inpatient versus outpatient arthroplasty: a single-surgeon, matched cohort analysis of 90-day complications. J Arthroplasty. 2019;34:221–227. doi: 10.1016/j.arth.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 26.Della Rocca GJ, Leung KS, Pape HC. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011;25:S66–70. doi: 10.1097/BOT.0b013e31821b8c28. [DOI] [PubMed] [Google Scholar]
- 27.Epinette JA, Brunschweiler B, Mertl P, Mole D, Cazenave A, French Society for H, et al Unicompartmental knee arthroplasty modes of failure: wear is not the main reason for failure: a multicentre study of 418 failed knees. Orthop Traumatol Surg Res. 2012;98:124–130. doi: 10.1016/j.otsr.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 28.Forster MC, Bauze AJ, Keene GC. Lateral unicompartmental knee replacement: fixed or mobile bearing? Knee Surg Sports Traumatol Arthrosc. 2007;15:1107–1111. doi: 10.1007/s00167-007-0345-5. [DOI] [PubMed] [Google Scholar]
- 29.Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D, et al. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014;67:46–51. doi: 10.1016/j.jclinepi.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Geller JA, Yoon RS, McKean J, Macaulay W. Does a high-flexion design affect early outcome of medial unicondylar knee arthroplasty? Clinical comparison at 2 years. J Arthroplasty. 2011;26:1468–1474. doi: 10.1016/j.arth.2011.03.040. [DOI] [PubMed] [Google Scholar]
- 31.Gesell MW, Tria AJ., Jr MIS unicondylar knee arthroplasty: surgical approach and early results. Clin Orthop Relat Res. 2004;428:53–60. [PubMed] [Google Scholar]
- 32.Gill JR, Nicolai P. Clinical results and 12-year survivorship of the physica ZUK unicompartmental knee replacement. Knee. 2019;26:750–758. doi: 10.1016/j.knee.2019.02.016. [DOI] [PubMed] [Google Scholar]
- 33.Gleeson RE, Evans R, Ackroyd CE, Webb J, Newman JH. Fixed or mobile bearing unicompartmental knee replacement? a comparative cohort study. Knee. 2004;11:379–384. doi: 10.1016/j.knee.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 34.Grammens J, Van Haver A, Danckaers F, Booth B, Sijbers J, Verdonk P. Small medial femoral condyle morphotype is associated with medial compartment degeneration and distinct morphological characteristics: a comparative pilot study. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06218-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gupta V, Kejriwal R, Frampton C. Revision following cemented and uncemented Oxford-III primary medial unicompartmental knee replacements: a 19-Year analysis from the New Zealand joint registry. J Bone Joint Surg Am. 2020;102:1777–1783. doi: 10.2106/JBJS.19.01443. [DOI] [PubMed] [Google Scholar]
- 36.Hamilton WG, Ammeen DJ, Hopper RH., Jr Mid-term survivorship of minimally invasive unicompartmental arthroplasty with a fixed-bearing implant: revision rate and mechanisms of failure. J Arthroplasty. 2014;29:989–992. doi: 10.1016/j.arth.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 37.Hamilton WG, Collier MB, Tarabee E, McAuley JP, Engh CA, Jr, Engh GA. Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2006;21:98–107. doi: 10.1016/j.arth.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 38.Hiranaka T, Yoshikawa R, Yoshida K, Michishita K, Nishimura T, Nitta S, et al. Tibial shape and size predicts the risk of tibial plateau fracture after cementless unicompartmental knee arthroplasty in Japanese patients. Bone Joint J. 2020;102:861–867. doi: 10.1302/0301-620X.102B7.BJJ-2019-1754.R1. [DOI] [PubMed] [Google Scholar]
- 39.Houskamp DJ, Tompane T, Barlow BT. What is the critical tibial resection depth during unicompartmental knee arthroplasty? A biomechanical study of fracture risk. J Arthroplasty. 2020 doi: 10.1016/j.arth.2020.04.005. [DOI] [PubMed] [Google Scholar]
- 40.Hung Y-W, Chi-Ho Fan J, Ka-Bon Kwok C, Lok-Fai Wong E, Ka-Man Lo C. Delayed tibial-platform periprosthetic stress fracture after unicompartmental knee arthroplasty: uncommon and devastating complication. J Orthop Trauma Rehabilitation. 2018;25:29–33. [Google Scholar]
- 41.Iesaka K, Tsumura H, Sonoda H, Sawatari T, Takasita M, Torisu T. The effects of tibial component inclination on bone stress after unicompartmental knee arthroplasty. J Biomech. 2002;35:969–974. doi: 10.1016/s0021-9290(01)00244-5. [DOI] [PubMed] [Google Scholar]
- 42.Inoue S, Akagi M, Asada S, Mori S, Zaima H, Hashida M. The valgus inclination of the tibial component increases the risk of medial tibial condylar fractures in unicompartmental knee arthroplasty. J Arthroplasty. 2016;31:2025–2030. doi: 10.1016/j.arth.2016.02.043. [DOI] [PubMed] [Google Scholar]
- 43.Jeer PJ, Keene GC, Gill P. Unicompartmental knee arthroplasty: an intermediate report of survivorship after the introduction of a new system with analysis of failures. Knee. 2004;11:369–374. doi: 10.1016/j.knee.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 44.Ji JH, Park SE, Song IS, Kang H, Ha JY, Jeong JJ. Complications of medial unicompartmental knee arthroplasty. Clin Orthop Surg. 2014;6:365–372. doi: 10.4055/cios.2014.6.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaneko T, Kono N, Sunakawa T, Okuno Y, Ikegami H, Musha Y. Reliable patient-reported outcome measure and survivorship of UKA for primary spontaneous osteonecrosis. Eur J Orthop Surg Traumatol. 2019;29:119–124. doi: 10.1007/s00590-018-2296-6. [DOI] [PubMed] [Google Scholar]
- 46.Kerens B, Schotanus MGM, Boonen B, Boog P, Emans PJ, Lacroix H, et al. Cementless versus cemented Oxford unicompartmental knee arthroplasty: early results of a non-designer user group. Knee Surg Sports Traumatol Arthrosc. 2017;25:703–709. doi: 10.1007/s00167-016-4149-3. [DOI] [PubMed] [Google Scholar]
- 47.Kim KT, Lee S, Lee JI, Kim JW. Analysis and treatment of complications after unicompartmental knee arthroplasty. Knee Surg Relat Res. 2016;28:46–54. doi: 10.5792/ksrr.2016.28.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim YJ, Kim BH, Yoo SH, Kang SW, Kwack CH, Song MH. Mid-Term results of Oxford medial unicompartmental knee arthroplasty in young asian patients less than 60 years of age: a minimum 5-year follow-up. Knee Surg Relat Res. 2017;29:122–128. doi: 10.5792/ksrr.16.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Knifsund J, Reito A, Haapakoski J, Niinimaki T, Eskelinen A, Leskinen J, et al. Short-term survival of cementless Oxford unicondylar knee arthroplasty based on the finnish arthroplasty register. Knee. 2019;26:768–773. doi: 10.1016/j.knee.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 50.Koh IJ, Suhl KH, Kim MW, Kim MS, Choi KY, In Y. Use of all-polyethylene tibial components in unicompartmental knee arthroplasty increases the risk of early failure. J Knee Surg. 2017;30:807–815. doi: 10.1055/s-0036-1597979. [DOI] [PubMed] [Google Scholar]
- 51.Kort NP, van Raay JJ, Cheung J, Jolink C, Deutman R. Analysis of Oxford medial unicompartmental knee replacement using the minimally invasive technique in patients aged 60 and above: an independent prospective series. Knee Surg Sports Traumatol Arthrosc. 2007;15:1331–1334. doi: 10.1007/s00167-007-0397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kumar A, Chambers I, Wong P. Periprosthetic fracture of the proximal tibia after lateral unicompartmental knee arthroplasty. J Arthroplasty. 2008;23:615–618. doi: 10.1016/j.arth.2007.04.036. [DOI] [PubMed] [Google Scholar]
- 53.Lecuire F, Berard JB, Martres S. Minimum 10-year follow-up results of ALPINA cementless hydroxyapatite-coated anatomic unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol. 2014;24:385–394. doi: 10.1007/s00590-013-1192-3. [DOI] [PubMed] [Google Scholar]
- 54.Leenders AM, Schotanus MGM, Wind RJP, Borghans RAP, Kort NP. A high rate of tibial plateau fractures after early experience with patient-specific instrumentation for unicompartmental knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2018;26:3491–3498. doi: 10.1007/s00167-018-4956-9. [DOI] [PubMed] [Google Scholar]
- 55.Liddle AD, Pandit H, O'Brien S, Doran E, Penny ID, Hooper GJ, et al. Cementless fixation in Oxford unicompartmental knee replacement: a multicentre study of 1000 knees. Bone Joint J. 2013;95:181–187. doi: 10.1302/0301-620X.95B2.30411. [DOI] [PubMed] [Google Scholar]
- 56.Lim JW, Chen JY, Chong HC, Pang HN, Tay DKJ, Chia SL, et al. Pre-existing patellofemoral disease does not affect 10-year survivorship in fixed bearing unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27:2030–2036. doi: 10.1007/s00167-018-5169-y. [DOI] [PubMed] [Google Scholar]
- 57.Lindstrand A, Stenstrom A, Ryd L, Toksvig-Larsen S. The introduction period of unicompartmental knee arthroplasty is critical: a clinical, clinical multicentered, and radiostereometric study of 251 Duracon unicompartmental knee arthroplasties. J Arthroplasty. 2000;15:608–616. doi: 10.1054/arth.2000.6619. [DOI] [PubMed] [Google Scholar]
- 58.Lisowski LA, van den Bekerom MP, Pilot P, van Dijk CN, Lisowski AE. Oxford Phase 3 unicompartmental knee arthroplasty: medium-term results of a minimally invasive surgical procedure. Knee Surg Sports Traumatol Arthrosc. 2011;19:277–284. doi: 10.1007/s00167-010-1213-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lombardi AV, Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res. 2009;467:1450–1457. doi: 10.1007/s11999-009-0731-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lu C, Ye G, Liu W, Wu H, Wu G, Chen J. Tibial plateau fracture related to unicompartmental knee arthroplasty: two case reports and literature review. Medicine (Baltimore) 2019;98:e17338. doi: 10.1097/MD.0000000000017338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marya S, Thukral R. Unicompartmental knee arthroplasty for tricompartment osteoarthritis in octogenarians. Indian J Orthop. 2009;43:361–366. doi: 10.4103/0019-5413.54970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mohammad HR, Kennedy JA, Mellon SJ, Judge A, Dodd CA, Murray DW. Ten-year clinical and radiographic results of 1000 cementless Oxford unicompartmental knee replacements. Knee Surg Sports Traumatol Arthrosc. 2020;28:1479–1487. doi: 10.1007/s00167-019-05544-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mohammad HR, Matharu GS, Judge A, Murray DW. Comparison of the 10-year outcomes of cemented and cementless unicompartmental knee replacements: data from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Acta Orthop. 2020;91:76–81. doi: 10.1080/17453674.2019.1680924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mohammad HR, Matharu GS, Judge A, Murray DW. New surgical instrumentation reduces the revision rate of unicompartmental knee replacement: a propensity score matched comparison of 15,906 knees from the National Joint Registry. Knee. 2020;27:993–1002. doi: 10.1016/j.knee.2020.02.008. [DOI] [PubMed] [Google Scholar]
- 65.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.New Zealand Arthroplasty Registry (2019) NZJR 20 Year Report. https://nzoa.org.nz/nzoa-joint-registry. (Accessed 10 Jan 2020)
- 67.NIH study quality assessment tool (2015). https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. (Accessed 17 Jul 2020)
- 68.Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011;93:198–204. doi: 10.1302/0301-620X.93B2.25767. [DOI] [PubMed] [Google Scholar]
- 69.Pandit H, Murray DW, Dodd CA, Deo S, Waite J, Goodfellow J, et al. Medial tibial plateau fracture and the Oxford unicompartmental knee. Orthopedics. 2007;30:28–31. [PubMed] [Google Scholar]
- 70.Panzram B, Bertlich I, Reiner T, Walker T, Hagmann S, Gotterbarm T. Cementless Oxford medial unicompartimental knee replacement: an independent series with a 5-year-follow-up. Arch Orthop Trauma Surg. 2017;137:1011–1017. doi: 10.1007/s00402-017-2696-9. [DOI] [PubMed] [Google Scholar]
- 71.Pegg EC, Walter J, D'Lima DD, Fregly BJ, Gill HS, Murray DW. Minimising tibial fracture after unicompartmental knee replacement: a probabilistic finite element study. Clin Biomech. 2020;73:46–54. doi: 10.1016/j.clinbiomech.2019.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pongcharoen B, Chanalithichai N. Clinical outcomes of patients with residual medial osteophytes following mobile bearing unicompartmental knee arthroplasty. PLoS ONE. 2018;13:e0205469. doi: 10.1371/journal.pone.0205469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rajasekhar C, Das S, Smith A. Unicompartmental knee arthroplasty. 2- to 12-year results in a community hospital. J Bone Joint Surg Br. 2004;86:983–985. doi: 10.1302/0301-620x.86b7.15157. [DOI] [PubMed] [Google Scholar]
- 74.Rudol G, Jackson MP, James SE. Medial tibial plateau fracture complicating unicompartmental knee arthroplasty. J Arthroplasty. 2007;22:148–150. doi: 10.1016/j.arth.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 75.Sasatani K, Majima T, Murase K, Takeuchi N, Matsumoto T, Oshima Y, et al. Three-dimensional finite analysis of the optimal alignment of the tibial implant in unicompartmental knee arthroplasty. J Nippon Med Sch. 2020;87:60–65. doi: 10.1272/jnms.JNMS.2020_87-202. [DOI] [PubMed] [Google Scholar]
- 76.Sawatari T, Tsumura H, Iesaka K, Furushiro Y, Torisu T. Three-dimensional finite element analysis of unicompartmental knee arthroplasty–the influence of tibial component inclination. J Orthop Res. 2005;23:549–554. doi: 10.1016/j.orthres.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 77.Saxler G, Temmen D, Bontemps G. Medium-term results of the AMC-unicompartmental knee arthroplasty. Knee. 2004;11:349–355. doi: 10.1016/j.knee.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 78.Schotanus MGM, Thijs E, Boonen B, Kerens B, Jong B, Kort NP. Revision of partial knee to total knee arthroplasty with use of patient-specific instruments results in acceptable femoral rotation. Knee Surg Sports Traumatol Arthrosc. 2018;26:1656–1661. doi: 10.1007/s00167-017-4674-8. [DOI] [PubMed] [Google Scholar]
- 79.Seeger JB, Haas D, Jager S, Rohner E, Tohtz S, Clarius M. Extended sagittal saw cut significantly reduces fracture load in cementless unicompartmental knee arthroplasty compared to cemented tibia plateaus: an experimental cadaver study. Knee Surg Sports Traumatol Arthrosc. 2012;20:1087–1091. doi: 10.1007/s00167-011-1698-3. [DOI] [PubMed] [Google Scholar]
- 80.Seeger JB, Jaeger S, Rohner E, Dierkes H, Wassilew G, Clarius M. Treatment of periprosthetic tibial plateau fractures in unicompartmental knee arthroplasty: plates versus cannulated screws. Arch Orthop Trauma Surg. 2013;133:253–257. doi: 10.1007/s00402-012-1649-6. [DOI] [PubMed] [Google Scholar]
- 81.Seon JK, Song EK, Yoon TR, Seo HY, Cho SG. Tibial plateau stress fracture after unicondylar knee arthroplasty using a navigation system: two case reports. Knee Surg Sports Traumatol Arthrosc. 2007;15:67–70. doi: 10.1007/s00167-006-0097-7. [DOI] [PubMed] [Google Scholar]
- 82.Sloper PJ, Hing CB, Donell ST, Glasgow MM. Intra-operative tibial plateau fracture during unicompartmental knee replacement: a case report. Knee. 2003;10:367–369. doi: 10.1016/s0968-0160(03)00003-6. [DOI] [PubMed] [Google Scholar]
- 83.Smith TO, Chester R, Glasgow MM, Donell ST. Accelerated rehabilitation following Oxford unicompartmental knee arthroplasty: five-year results from an independent centre. Eur J Orthop Surg Traumatol. 2011;22:151–158. [Google Scholar]
- 84.Song EK, Lee SH, Na BR, Seon JK. Comparison of outcome and survival after unicompartmental knee arthroplasty between navigation and conventional techniques with an average 9-year follow-up. J Arthroplasty. 2016;31:395–400. doi: 10.1016/j.arth.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 85.Song MH, Kim BH, Ahn SJ, Yoo SH, Lee MS. Early complications after minimally invasive mobile-bearing medial unicompartmental knee arthroplasty. J Arthroplasty. 2009;24:1281–1284. doi: 10.1016/j.arth.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 86.Thompson SA, Liabaud B, Nellans KW, Geller JA. Factors associated with poor outcomes following unicompartmental knee arthroplasty: redefining the “classic” indications for surgery. J Arthroplasty. 2013;28:1561–1564. doi: 10.1016/j.arth.2013.02.034. [DOI] [PubMed] [Google Scholar]
- 87.Van Loon P, de Munnynck B, Bellemans J. Periprosthetic fracture of the tibial plateau after unicompartmental knee arthroplasty. Acta Orthop Belg. 2006;72:369–374. [PubMed] [Google Scholar]
- 88.Vardi G, Strover AE. Early complications of unicompartmental knee replacement: the Droitwich experience. Knee. 2004;11:389–394. doi: 10.1016/j.knee.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 89.Weber P, Utzschneider S, Sadoghi P, Pietschmann MF, Ficklscherer A, Jansson V, et al. Navigation in minimally invasive unicompartmental knee arthroplasty has no advantage in comparison to a conventional minimally invasive implantation. Arch Orthop Trauma Surg. 2012;132:281–288. doi: 10.1007/s00402-011-1404-4. [DOI] [PubMed] [Google Scholar]
- 90.Wilke J, Krause F, Niederer D, Engeroff T, Nurnberger F, Vogt L, et al. Appraising the methodological quality of cadaveric studies: validation of the QUACS scale. J Anat. 2015;226:440–446. doi: 10.1111/joa.12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Woo YL, Chin PL, Lo NN, Chia S-L, Tay DKJ, Yeo SJ. Management of periprosthetic fracture in unicompartmental knee arthroplasty patients: a case series. Proc Singapore Health. 2013;22:267–272. [Google Scholar]
- 92.Yang KY, Yeo SJ, Lo NN. Stress fracture of the medial tibial plateau after minimally invasive unicompartmental knee arthroplasty: a report of 2 cases. J Arthroplasty. 2003;18:801–803. doi: 10.1016/s0883-5403(03)00332-2. [DOI] [PubMed] [Google Scholar]
- 93.Yokoyama M, Nakamura Y, Egusa M, Doi H, Onishi T, Hirano K, et al. Factors related to stress fracture after unicompartmental knee arthroplasty. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2019;15:1–5. doi: 10.1016/j.asmart.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yoon BH, Park JW, Cha YH, Won SH, Lee YK, Ha YC, et al. Incidence of ceramic fracture in contemporary ceramic-on-ceramic total hip arthroplasty: a meta-analysis of proportions. J Arthroplasty. 2020;35:1437–e1433. doi: 10.1016/j.arth.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 95.Yoshida K, Tada M, Yoshida H, Takei S, Fukuoka S, Nakamura H. Oxford phase 3 unicompartmental knee arthroplasty in Japan–clinical results in greater than one thousand cases over ten years. J Arthroplasty. 2013;28:168–171. doi: 10.1016/j.arth.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 96.Yoshikawa R, Hiranaka T, Okamoto K, Fujishiro T, Hida Y, Kamenaga T, et al. The medial eminence line for predicting tibial fracture risk after unicompartmental knee arthroplasty. Clin Orthop Surg. 2020;12:166–170. doi: 10.4055/cios19011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G. Differences of knee anthropometry between Chinese and white men and women. J Arthroplasty. 2011;26:124–130. doi: 10.1016/j.arth.2009.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]