Abstract
Primary lymphoma originating from the lacrimal drainage system is a rare disease. Such lymphomas are mostly B-cell in origin and present nonspecific symptoms. The treatment of malignant lymphoma of the lacrimal drainage system is slightly different. We present the case of a 71-year-old woman with a painless mass below the medial canthus. Computed tomography (CT) scan of the orbit revealed a mass invading the right lacrimal sac. An incision biopsy was obtained, and the pathologic findings suggested a diagnosis of primary diffuse large B-cell lymphoma of the lacrimal sac. The patient was treated with chemotherapy and intrathecal methotrexate. After completing eight cycles of chemotherapy, the patient was followed up by a CT scan, which revealed nearly total resolution of an ill-defined enhancing mass. At the time of this case report writing, the patient is in complete remission at six months with no other complications.
Keywords: Case reports, Diffuse large B-cell lymphoma, Nasolacrimal sac, Lacrimal sac, Lymphoma
INTRODUCTION
Tumors of the lacrimal drainage system are rare, which can be classified into two types: epithelial and non-epithelial neoplasms. Epithelial tumors are more commonly found, with an incidence of 90%. Lacrimal sac lymphomas are even more rare and usually occur secondary to systemic lymphoma metastasis. Patients commonly present with epiphora, recurrent dacryocystitis, lacrimal sac mass and epistaxis. Early diagnosis and management can reduce the risk of disease recurrence and visual loss. Even though the lacrimal drainage system is located near the nasal area, the treatment of a malignant lymphoma of the lacrimal drainage system is slightly different from other tumors that located near the nasal area.
CASE REPORT
A 71-year-old woman presented with a painless mass below the right medial canthal area for 6 months. She was asymptomatic. The patient had no history of fever, malaise, significant weight loss, or family history malignancy. Ocular examination showed a firm, mild-tender, mild erythematous mass measuring 2× 3 cm in the right lacrimal fossa. The tear meniscus height was 0.6 mm for the right eye and 0.3 mm for the left eye. There was no fluid reflux upon lacrimal sac compression. Irrigation tests showed a partial lower canalicular obstruction but otherwise drainage system patency with blood-stained fluid passing into the nose. In addition, there were multiple enlarged lymph nodes in the cervical area. Rhinoscopic examination showed a mass at the right nasolacrimal duct opening below the right inferior turbinate, with no contact bleeding. Neck examination showed a right cervical lymphadenopathy level II sized 1.5 cm.
A computed tomography (CT) scan of the head and neck showed an ill-defined enhancing mass, sized 1.8× 1.6× 2.9 cm, located at the right lacrimal sac extending to the right extraconal fat, right nasal cavity, and right maxillary sinus involving the medial maxillary wall. There were multiple cervical lymph nodes, sizes up to 1.7 cm (Fig. 1).
Fig. 1.
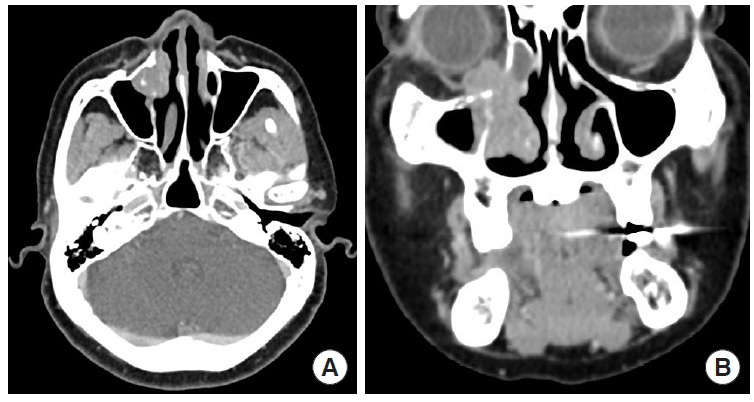
Enhanced computed tomographic image of a 71-year-old woman shows ill-defined enhancing mass located at the right lacrimal sac extending to the right extraconal fat, right nasal cavity and right maxillary sinus involving the medial site eyeball. (A) Axial and (B) coronal views.
Fine needle aspiration of an enlarged cervical lymph node (right neck IIA level) was performed, and the pathologic studies showed polymorphous lymphoid cells, but were inconclusive.
Pathologic findings from the trans-nasal biopsy of the lacrimal sac mass showed atypical round cells (Figs. 2, 3). Immunohistochemistry studies found positive expressions for BCL-2, BCL-6, MUM1, c-MYC; negative for AE1/AE3, CD10, CD23, Cyclin D-1; CD3 of scattered small T-cell, CD20 of sheets of large atypical B-cells, Ki-67 of 80% proliferation index (Fig. 4). From these findings, the mass was concluded as being a “diffuse large B-cell lymphoma (DLBCL) with non-germinal center phenotype.” However, the double expression of BCL-2 and c-MYC with a high proliferation index might indicate a poor prognosis.
Fig. 2.
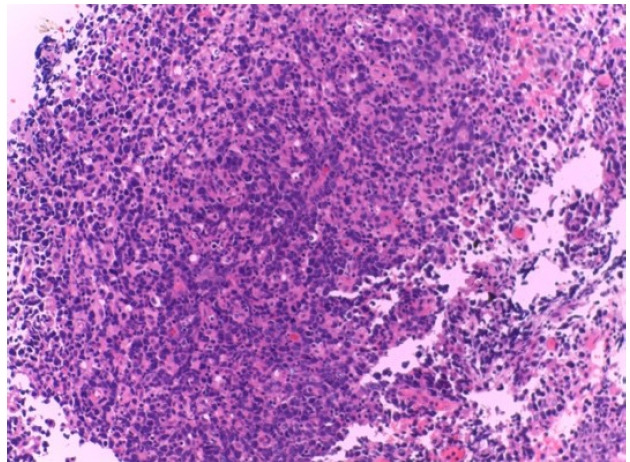
Lacrimal sac mass. Section showing fragments of the lacrimal glands and tumor cell clusters. The tumor cells are arranged in diffuse sheets without structure or nodular formation (H&E, ×200).
Fig. 3.
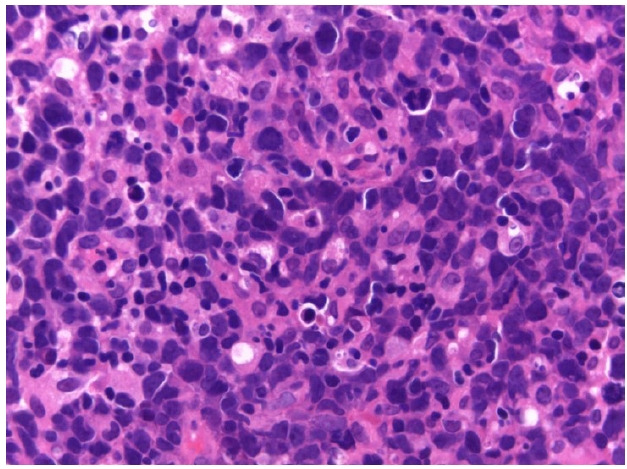
Lacrimal sac mass. The tumor cells contain irregular-shaped nuclei with rather fine nuclear chromatin. The lesion also contains tingible body macrophages (H&E, ×400).
Fig. 4.
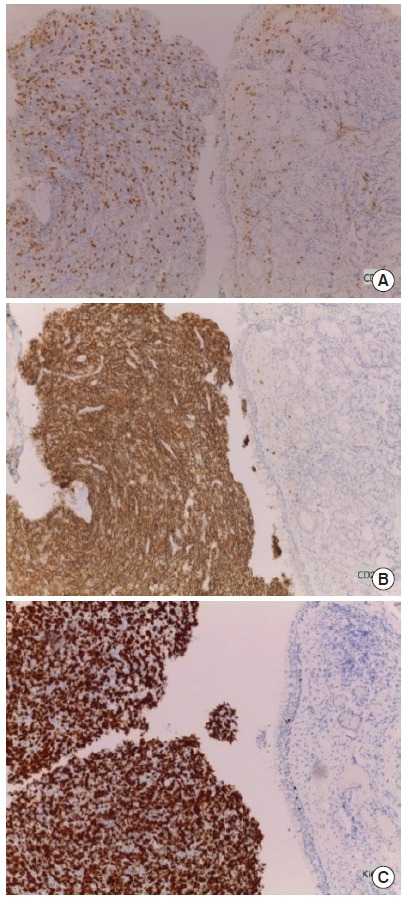
Lacrimal sac mass with immunohistochemical stain. (A) CD3 was negative (×100). (B) CD20 was diffuse positive (×100). (C) Ki-67 showing a high proliferation index (up to 80%–90%) (×200).
There was no abnormal finding on the CT scan of her chest with whole abdomen and bone marrow aspiration. Thus, the patient was diagnosed with primary DLBCL of the lacrimal sac stage II.
The patient was treated with chemotherapy because the tumor was DLBCL that categorized as stage II. The patient received one cycle of CVP regimen, comprising cyclophosphamide, vincristine, and prednisolone, and eight cycles of R-CHOP regimen, comprising rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone. Also, intrathecal methotrexate was given to prevent the recurrence of neurological complications.
After completing eight cycles of chemotherapy, the follow-up CT scan revealed nearly total resolution of the mass. There was an overall decrease in size of the cervical nodes (Fig. 5). Rhinoscopic examination showed no mass at the right nasal cavity and no palpable cervical lymph node upon neck examination. At the time of writing this report, the patient is in complete remission for 6 months with no other complications.
Fig. 5.

Enhanced computed tomographic image of lacrimal sac lymphoma (posttreatment) show nearly total resolution of the mass, which could be seen as a small soft tissue density involving the right lacrimal sac and extraconal fat at the medial aspect of the right orbit. There was an overall decrease in size of the cervical nodes, sized up to 0.5 cm.
DISCUSSION
Lacrimal sac tumors are rare [1-4]. Approximately 55% of lacrimal sac tumors are malignant, and 71% originate from epithelial cells [1]. Malignant lymphomas account for approximately 6% of all lacrimal sac tumors [5]. They are commonly secondary occurrence due to lymphatic metastasis from other areas, with primary lacrimal lymphomas rarely found [6]. Primary lacrimal sac lymphomas are found primarily in older patients [1,6]. The median age is 71 years (range, 45–95 years), with 80% of patients older than 60 years.
The clinical signs and symptoms of lacrimal sac tumors are nonspecific [7], but include medial canthal swelling [4], epiphora [3]. Therefore, some may be initially misdiagnosed or the diagnosis may be delayed [7-9]. Tumors of the lacrimal sac can originate directly from the lacrimal sac or adjacent organs [10-12].
Imaging such as CT scan or magnetic resonance imaging (MRI) can help guide the diagnosis, staging, and treatment plans [13]. CT scan is preferred over MRI for viewing the extent of the tumor and bone metastasis [3]. A CT scan should be done if the patient presents with the following findings: a hard consistency mass at the lacrimal sac, palpable mass over the medial canthal ligament, or orbital deformities due to the effect of the mass [14].
Diagnosis can be made by a tissue biopsy of the tumor [13,14]. Specific laboratory tests for primary lacrimal drainage system lymphoma are still not available due to the lack of data and as only a few cases have been reported to date. As a consequence, flow cytometry, molecular studies, and immunophenotyping are used to examine the ocular adnexal lymphoid proliferative lesion along with the presented signs and symptoms to differentiate the type of tumor and to make the diagnosis [15].
The most common cell type of non-Hodgkin’s lymphoma of the ocular and ocular adnexal is B-cell. T-cell lymphoma of the ocular and adnexa is uncommon. Therefore, most lacrimal sac lymphomas are from B-cell and the common subtypes are mucosa-associated lymphoid tissue lymphoma, extranodal marginal B-cell lymphoma, or DLBCL [10].
There are multiple prognostic factors of ocular non-Hodgkin’s lymphoma. Factors that suggest a poor prognosis are age (> 59 years old), elevated lactate dehydrogenase levels, stage IV, high-grade histological subgroup, presence of B symptoms (fever, night sweats, and weight loss) [16], and metastasis to the bone marrow [17]. They found that most woman patients with lacrimal drainage system lymphoma have more severe symptoms and a higher rate of disease recurrence [7,12,14]. To date, multiple published studies have shown conflicting data regarding the 5-year survival rate, ranging from < 30% to 75% [18]. Although this patient has factors that indicate a poor prognosis, including the double expression of BCL-2 and c-MYC with a high proliferation index, woman, and old age, bone marrow metastasis was not found and the patient has lymphoma stage II, without B symptoms. Moreover, most lacrimal drainage system lymphomas are the B-cell type, which has a good response to radiotherapy or chemotherapy [2], and therefore the prognosis appears favorable.
For primary lacrimal sac lymphoma, chemotherapy or radiotherapy is considered the primary treatment [19]. Extensive surgical interventions should be avoided to preserve the function and aesthetic of the eye [2]. In DLBCL, systemic chemotherapy that is CHOP regimens, which include cyclophosphamide, doxorubicin, vincristine, prednisolone, and adjunct immunotherapy therapy that is rituximab, are the treatment of choice. For DLBCL cells that have the CD20 antigen on the cell surface, immunotherapy with rituximab, which is a chimeric monoclonal anti-CD20 antibody, combined with chemotherapy has a significant advantage over chemotherapy alone in terms of overall survival and response rate [20]. As a result, we treated the patient with CHOP regimen chemotherapy, rituximab for adjunct immunotherapy and intrathecal methotrexate for preventing the recurrence of neurological complications.
In conclusion, primary lacrimal sac lymphoma is rare, with minimal and nonspecific signs and symptoms. In this case report, we present a patient with primary lacrimal sac DLBCL who showed a good response to R-CHOP regimens.
Abbreviations
- CT
computed tomography
- DLBCL
diffuse large B-cell lymphoma
- MRI
magnetic resonance imaging
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Human Ethics Committee of Srinakharinwirot University (SWUEC/X-144/2564).
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Author contribution
Project administration: Somtaporn Ueathaweephol. Writing - original draft: Somtaporn Ueathaweephol. Writing - review & editing: Somtaporn Ueathaweephol, Panuwat Wongwattana. Supervision: Panuwat Wongwattana, Waruttaporn Chanlalit, Therdkiat Trongwongsa, Sirilak Sutthinont. All authors read and approved the final manuscript.
REFERENCES
- 1.Tsao WS, Huang TL, Hsu YH, Chen N, Tsai RK. Primary diffuse large B cell lymphoma of the lacrimal sac. Taiwan J Ophthalmol. 2016;6:42–4. doi: 10.1016/j.tjo.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gao HW, Lee HS, Lin YS, Sheu LF. Primary lymphoma of nasolacrimal drainage system: a case report and literature review. Am J Otolaryngol. 2005;26:356–9. doi: 10.1016/j.amjoto.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Kumar VA, Esmaeli B, Ahmed S, Gogia B, Debnam JM, Ginsberg LE. Imaging features of malignant lacrimal sac and nasolacrimal duct tumors. AJNR Am J Neuroradiol. 2016;37:2134–7. doi: 10.3174/ajnr.A4882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venkitaraman R, George MK. Primary non Hodgkin’s lymphoma of the lacrimal sac. World J Surg Oncol. 2007;5:127. doi: 10.1186/1477-7819-5-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stefanyszyn MA, Hidayat AA, Pe’er JJ, Flanagan JC. Lacrimal sac tumors. Ophthalmic Plast Reconstr Surg. 1994;10:169–84. doi: 10.1097/00002341-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Sjo LD, Ralfkiaer E, Juhl BR, Prause JU, Kivela T, Auw-Haedrich C, et al. Primary lymphoma of the lacrimal sac: an EORTC ophthalmic oncology task force study. Br J Ophthalmol. 2006;90:1004–9. doi: 10.1136/bjo.2006.090589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Palma P, Ravalli L, Modestino R, Grisanti F, Casillo F, Marzola A. Primary lacrimal sac B-cell immunoblastic lymphoma simulating an acute dacryocystitis. Orbit. 2003;22:171–5. doi: 10.1076/orbi.22.3.171.15620. [DOI] [PubMed] [Google Scholar]
- 8.De Stefani A, Lerda W, Usai A, Cavalot A, Riella P, Bussi M. Squamous cell carcinoma of the lacrimal drainage system: case report and literature review. Tumori. 1998;84:506–10. doi: 10.1177/030089169808400414. [DOI] [PubMed] [Google Scholar]
- 9.Palamar M, Midilli R, Ozsan N, Egrilmez S, Sahin F, Yagci A. Primary diffuse large B-cell lymphoma of the lacrimal sac simulating chronic dacryocystitis. Auris Nasus Larynx. 2011;38:643–5. doi: 10.1016/j.anl.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Jordan DR, Nerad JA. Diffuse large-cell lymphoma of the nasolacrimal sac. Can J Ophthalmol. 1988;23:34–7. [PubMed] [Google Scholar]
- 11.Saccogna PW, Strauss M, Bardenstein DS. Lymphoma of the nasolacrimal drainage system. Otolaryngol Head Neck Surg. 1994;111:647–51. doi: 10.1177/019459989411100517. [DOI] [PubMed] [Google Scholar]
- 12.Erickson BA, Massaro BM, Mark LP, Harris GJ. Lacrimal collecting system lymphomas: integration of magnetic resonance imaging and therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1994;29:1095–103. doi: 10.1016/0360-3016(94)90406-5. [DOI] [PubMed] [Google Scholar]
- 13.Montalban A, Lietin B, Louvrier C, Russier M, Kemeny JL, Mom T, et al. Malignant lacrimal sac tumors. Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:165–72. doi: 10.1016/j.anorl.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Parmar DN, Rose GE. Management of lacrimal sac tumours. Eye (Lond) 2003;17:599–606. doi: 10.1038/sj.eye.6700516. [DOI] [PubMed] [Google Scholar]
- 15.Sharara N, Holden JT, Wojno TH, Feinberg AS, Grossniklaus HE. Ocular adnexal lymphoid proliferations: clinical, histologic, flow cytometric, and molecular analysis of forty-three cases. Ophthalmology. 2003;110:1245–54. doi: 10.1016/S0161-6420(03)00330-0. [DOI] [PubMed] [Google Scholar]
- 16.Meunier J, Lumbroso-Le Rouic L, Vincent-Salomon A, Dendale R, Asselain B, Arnaud P, et al. Ophthalmologic and intraocular non-Hodgkin’s lymphoma: a large single centre study of initial characteristics, natural history, and prognostic factors. Hematol Oncol. 2004;22:143–58. doi: 10.1002/hon.741. [DOI] [PubMed] [Google Scholar]
- 17.Rasmussen PK, Ralfkiaer E, Prause JU, Sjo LD, Toft PB, Siersma VD, et al. Diffuse large B-cell lymphoma of the ocular adnexal region: a nation-based study. Acta Ophthalmol. 2013;91:163–9. doi: 10.1111/j.1755-3768.2011.02337.x. [DOI] [PubMed] [Google Scholar]
- 18.Zarrabi K, Desai V, Yim B, Gabig TG. Primary diffuse large Bcell lymphoma localized to the lacrimal sac: a case presentation and review of the literature. Case Rep Hematol. 2016;2016:5612749. doi: 10.1155/2016/5612749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keleti D, Flickinger JC, Hobson SR, Mittal BB. Radiotherapy of lymphoproliferative diseases of the orbit. Surveillance of 65 cases. Am J Clin Oncol. 1992;15:422–7. [PubMed] [Google Scholar]
- 20.Decaudin D, de Cremoux P, Vincent-Salomon A, Dendale R, Rouic LL. Ocular adnexal lymphoma: a review of clinicopathologic features and treatment options. Blood. 2006;108:1451–60. doi: 10.1182/blood-2006-02-005017. [DOI] [PubMed] [Google Scholar]


