Abstract
This study evaluates diabetes self-management mobile health applications available from European app stores with respect to quality, concordance with recommended self-management tasks and implementation of persuasive system design principles. The European Play Store and Apple App Store were systematically searched and relevant apps were tested. Two raters independently assessed app quality using the Mobile Application Rating Scale and conducted a content analysis of provided persuasive system design principles and self-management tasks. A total of 2,269 mobile health applications were identified and 120 could be included in the evaluation. The overall quality was rated as moderate M = 3.20 (SD = 0.39, min = 2.31, max = 4.62), with shortcomings in the subcategories of engagement (M = 2.80, SD = 0.67) and information quality (M = 2.26, SD = 0.48). Scientific evidence is available for 8% of the apps. The reviewed apps implemented a median of three persuasive system design principles (range 0–15) and targeted a median of 4.5 (range 1–8) self-management tasks, however, with a lack of information about psychosocial coping strategies. Most available diabetes self-management apps lack a scientific evidence base. Persuasive system design features are underrepresented and may form a promising tool to improve app quality. Furthermore, the interaction of physical and behavioral health should be improved in existing diabetes self-management mobile health applications.
Subject terms: Psychology, Endocrinology
Introduction
In Europe, about 60 million people are diagnosed with diabetes, and the prevalence and incidence rates are rising1,2. Diabetes care requires the performance of multiple essential self-management tasks by affected individuals. A best possible performance of diabetes self-management task, as recommended by the American Association of Diabetes Educators3, is decisive for the course of diabetes including lower risks of acute and long-term complications, significantly lower morbidity and mortality and higher mental well-being and quality of life4. Accordingly, diabetes self-management education and support are key elements for the successful self-management of the condition5. However, self-management education and support may be underutilized in diabetes care3, thus applications supporting people to better self-manage their diabetes may be useful. Mobile health applications (MHA) have been found to be a promising technological approach to help people perform better self-managements3,6–10. Studies support that MHA might have positive impacts on quality of life, diabetes outcomes and patient-provider communication6,11. In addition, MHA offer a low-threshold, cost-effective and flexible support opportunity in the everyday lives of users12.
Due to the often unregulated and rapidly growing nature of app stores, numerous commercial diabetes MHA are available. Since user ratings do not constitute a reliable or valid indicator of app quality13, it is important to systematically evaluate the quality of the available MHA in order to support health care providers, educators and users in their search for appropriate and secure apps13,14. For this purpose, several studies have been conducted in recent years13,15,16.
Hood et al.13 conducted a meta-review of international available MHA quality rating studies published between 2010 and 2014. Overall, the results indicate security concerns, lack of content founded upon validated theories, deficient educational information and limited implementation of behavior change techniques13.
In more recent quality rating studies, Gong et al.16 and Chavez et al.17 assessed the quality of diabetes self-management MHA in the largest app stores in China and the US, respectively, using the mobile application rating scale (MARS), a reliable and valid measurement of MHA quality18. Both studies reported suboptimal overall quality of the MHA, with the information and engagement domains scoring the worst.
To optimize engagement with MHA it is crucial to leverage technical capabilities19,20. The framework of the persuasive system design (PSD) model encompasses various technical principles to optimize human–machine interaction to support users in achieving their personal target behavior, thereby influencing their attitudes and behavior21,22. The positive impact of PSD on adherence to and effectiveness of MHA has been demonstrated in various studies19,23,24. Previously reported technical features in diabetes MHA include disease-related reminders, social networking features, feedback on self-monitoring and the possibility of sharing data with health care providers, with self-monitoring being the most frequently implemented feature13,25.
The findings by Hood et al. suggesting a substantial lack of educational information are of paramount concern as users are exposed to the risk of misinformation. Since clinical studies on the usefulness or effectiveness are often not available, the recommendations should, as a minimum standard, follow established clinical guidelines4,5. In this context, it is important that the focus of education is not limited to individual aspects of self-management. Areas such as coping and problem solving should also be targeted26.
Therefore, this study aims to systematically search and evaluate diabetes self-management MHA which are available in the European commercial app stores in English or German language to answer the following research questions:
What is the quality rating according to the MARS of diabetes self-management MHA available in European commercial app stores in terms of engagement, functionality, aesthetics and information?
Which persuasive system design features do diabetes self-management MHA include?
Do persuasive system design features predict the quality rating of diabetes self-management MHA?
Which of the self-management tasks recommended by the American Association of Diabetes Educators do diabetes self-management MHA address?
Materials and methods
Search strategy
The search was limited until December 2020, we searched the European Google Play Store and the Apple App Store using diabetes-related terms via a web-crawler of the Mobile Health App Database (MHAD) project27. This approach has been evaluated in several previous studies [e.g.28–30]. MHA were screened and downloaded if they (1) addressed people with diabetes or parents of children with diabetes; (2) contained educational or supporting information on diabetes self-management; (3) were available in English or German language. MHA were eligible for inclusion if they were accessible and enabled assessment. In the case of MHA which required further information for access (e.g., login data provided by physician), MHA developers were contacted and asked for access. Dead links were retrieved three times during a period of two weeks before final exclusion.
Quality rating
Two independent raters assessed MHA quality using the German version of the Mobile App Rating Scale (MARS-G;18,31). All reviewers were graduates of clinical and health psychology supervised by a licensed psychotherapist with extensive psycho-somatic expertise. Before the reviewing process, reviewers underwent an online training for using the MARS. To capture interrater reliability between reviewers, initially five MHA were rated by all four reviewers, and the ratings were compared. Interrater reliability in both reviewer teams was excellent (Team 1: 2-way mixed ICC = 0.94, 95% CI 0.94 to 0.95; Team 2: 2-way mixed ICC = 0.88, 95% CI 0.81 to 0.92). Through the MARS, MHA quality can be evaluated using four subscales: 1) engagement (five items: fun, interest, individual adaptability, interactivity, target group); 2) functionality (four items: performance, usability, navigation, gestural design); 3) aesthetics (three items: layout, graphics, visual appeal); and 4) information quality (seven items: accuracy of app description, goals, quality of information, quantity of information, quality of visual information, credibility, evidence base). Each item can be rated on a 5-point scale. The MARS sum score is determined from the four subscales18.
The MARS sum score showed excellent psychometric properties (ICC [Intra Class Correlation] = 0.82, 95% CI: 0.81 to 0.82; internal consistency: ω = 0.93)32. The four subcategories demonstrated acceptable to excellent internal consistencies (ω = 0.79 to 0.90)32. In accordance with the MARS, three further categories were assessed: (5) therapeutic gain (four items: gain for patients, gain for therapists, risks and side effects, ease of implementation into routine healthcare); (6) subjective quality (four items: recommendation, frequency of use, willingness to pay, overall star rating); and (7) perceived impact (six items: awareness, knowledge, attitudes, intention to change, help seeking, behavioral change).
User rating
Ratings of user satisfaction with the MHA (from 1 to 5 “stars”, higher score = higher satisfaction), which were available in the app stores, were extracted for comparison with the quality ratings according to the MARS.
General characteristics
The description section of MARS was modified to collect the following information for each MHA: (1) app name; (2) platform; (3) language; (4) specific target group (if any); (5) cost; (6) technical aspects of potential tracking features (export possibilities; manual tracking; CGM connection); (7) data protection and privacy; (8) user rating; and (9) available scientific studies. Irrespective of whether relevant studies were referenced in the MHA app store descriptions, we searched the app developers’ websites and Google Scholar to identify available studies for each MHA.
Persuasive system design features
We assessed the included MHA for 24 of the 28 PSD features as recommended by Oinas-Kukkonen and Harjumaa21. The features are divided into four subcategories: (1) primary task support; (2) dialogue support; (3) social support; and (4) system credibility. We focused on design features provided through the technical system itself. Therefore, we excluded the principle of liking (subcategory dialogue support), surface credibility, expertise, trustworthiness of content (subcategory trustworthiness). Principles were defined according to Oinas-Kukkonen and Harjumaa21 and Kelders et al.19. Examples for each principle are incorporated in Table 3.
Table 3.
Number of apps incorporating a particular PSD principle.
| Implemented principles (%) | Example | |
|---|---|---|
| System credibility | ||
| Real-world feel | 98.3 | Providing contact data of developers |
| Authority | 14.2 | Citations of clinicians |
| Third-party endorsements | 28.3 | Recommendations of diabetes institutions |
| Verifiability | 22.5 | Providing source of information and links to it |
| Dialogue support | ||
| Praise | 23.3 | Feedback/compliments on tracked data |
| Rewards | 2.5 | Collecting stars for engaging in lessons |
| Reminders | 16.7 | System based daily pop-up messages |
| Suggestion | 85.8 | Recipes for healthy nutrition |
| Similarity | 4.2 | Stories of other diabetes patients |
| Social role | 7.5 | Guidance by an avatar |
| Primary task support | ||
| Reduction | 16.7 | Dividing tracking in small simple steps |
| Tunneling | 6.7 | Implementing sequential lessons |
| Tailoring | 25.0 | Adapting information according to type of diabetes |
| Personalization | 10.0 | Possibility to customize interface |
| Self-monitoring | 28.3 | Feature for glucose tracking |
| Simulation | 0.8 | Calculator how glucose level changes during the day |
| Rehearsal | 5.0 | Knowledge quiz |
| Social support | ||
| Social learning | 2.5 | Board showing activity of other app users |
| Social comparison | 0 | Comparison of user’s response to others’ responses |
| Normative influence | 13.3 | Comparing glucose values to healthy peers |
| Social facilitation | 7.5 | Online discussion forum |
| Cooperation | 1.7 | Giving advice in small peer groups |
| Competition | 0 | Leader boards on daily activity level |
| Recognition | 7.5 | Liking and posting achievements |
System credibility, dialogue support, primary task support and social support are the four categories of persuasive system design. Each category consists of seven principles.
Concordance with recommended self-management tasks
The American Association of Diabetes Educators recommends eight tasks as important for successful diabetes self-management and education3: (1) diabetes pathophysiology and treatment options; (2) healthy nutrition; (3) physical activity; (4) medication usage; (5) monitoring; (6) preventing, detecting and treating acute and chronic complications; (7) healthy coping with psychosocial issues and concerns; and (8) problem solving. We conducted a content analysis and systematically rated which of these tasks were addressed in each MHA’s educational content. Educational content could be delivered as text, video/audio, games, or forums. We calculated the median number of self-management tasks addressed by each MHA’s content.
Statistical analyses
Means (M) and standard deviations (SD) for the MARS sum score and all subscales were calculated. Frequency of implemented general characteristics, PSD principles and self-management tasks are reported. Furthermore, bivariate correlations and hierarchical regression analysis were performed to evaluate a potential association between PSD subcategories and MARS sum score or subcategories. Additionally, correlations between user ratings and the MARS scales scores were estimated.
Results
Search
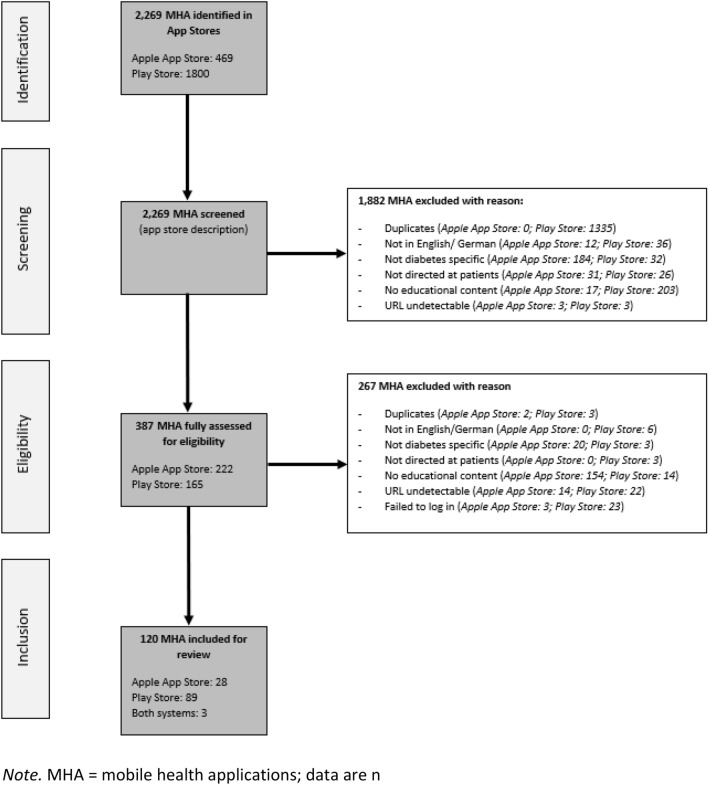
120 MHA were finally included in the app rating. Of these, 89 (74%) were available in the Play Store, 28 (23%) in the Apple App Store and three (3%) in both systems (Fig. 1).
Figure 1.
Flow-chart showing selection of MHA.
General characteristics
Thirteen of the included MHA (10.8%) specifically targeted type 1 diabetes, eight (6.7%) type 2 diabetes and two (1.7%) gestational diabetes. Type of diabetes was not specified for 97 (80.8%) of the MHA. One hundred and three MHA (85.8%) were available free of charge. The fees for the 14.2% of MHA charging fees varied between 0.59€ and 64.99€. Two of the MHA (“myDiabetes”, “X-Pert”) could only be accessed via a code to be provided by the user’s treating physician. All 120 MHA were available in English, however, 22 (18.3%) of them were additionally available in German. Nine of the MHA (7.5%) were designed for parents of children with Type 1 Diabetes (“DIABETES TREATEMENT App”; “Diabetes Type 1”; “Diabetes Care”; “Diabetes treatment”; “Diabetes–Diabetes Diet Tips”; “Hypo Program”; “Broteinheiten”; “KE-Finder”; “Our Journey with Diabetes”). In addition, three of the MHA were specifically designed for children (“Jerry the Bear”) and/or adolescents and young adults with diabetes (“Invincible”; “Kids and Teens Diabetes”). Regarding user privacy and data security, ten of the MHA (8.3%) were password-protected, 20 (16.7%) had a login page, 96 (80.0%) provided information on a privacy policy and 119 (99.2%) incorporated a contact or legal notice. Furthermore, 35 of the MHA (29.2%) offered a tracking feature. Among these, 23 (19.2%) offered manual tracking, while twelve (10.0%) offered automatic tracking by connecting to a CGM system; a function to export tracking data was available in 17 MHA. With regard to the evidence base of MHA, seven of the MHA (5.8%) (“Diabetes Forum”; “Hypo Program”; “myDiabetes”; “Dario”; “RapidCalc Diabetes Manager”; “Diabetes Tracker by MyNetDiary”; “iHealth Gluco Smart”;33–36) had been evaluated in usability or non-controlled studies and two of them (2%; “One Drop Diabetes Management”; “X-Pert”;37,38) in randomized controlled trials.
Quality rating
The MARS subcategory functionality revealed the highest scores (M = 4.10, SD = 0.30), followed by aesthetics (M = 3.64, SD = 0.50) and engagement (M = 2.80, SD = 0.67). Information quality had the lowest rating scores (M = 2.26, SD = 0.48). Detailed information on the MARS sum scores and subcategory scores for the ten best-rated MHA per app store are given in Table 1. MARS ratings for all reviewed MHA are reported in Supplementary Table S1.
Table 1.
MARS ratings for the ten highest ranking apps per app store in descending order (MARS ratings for all 120 apps in Supplementary Table S1).
| Name | Developer | Total score | Quality rating | Additional subscales | |||||
|---|---|---|---|---|---|---|---|---|---|
| Engagement | Functionality | Aesthetics | Information Quality | Therapeutic Gain | Subjective Quality | Perceived Impact | |||
| Available from Play Store | |||||||||
| myDiabetes* | my mhealth | 4.62 | 4.80 | 4.75 | 5.00 | 3.93 | 4.75 | 4.38 | 4.58 |
| Invincible * | Invincible Corp | 4.02 | 4.30 | 4.38 | 4.84 | 2.58 | 2.25 | 3.63 | 3.75 |
| BD Diabetes Care App | BD-Digital Health | 4.01 | 4.20 | 4.38 | 4.67 | 2.79 | 2.25 | 3.75 | 2.50 |
| Glucose Buddy Diabetes Tracker * | Azumio Inc | 3.95 | 4.3 | 4.25 | 4.17 | 3.07 | 2.50 | 3.88 | 3.92 |
| Hypo Program | Diabetes Digital Media | 3.90 | 3.80 | 4.38 | 4.34 | 3.08 | 2.13 | 3.38 | 2.42 |
| Jerry the Bear | Sproutel. Inc | 3.88 | 3.80 | 4.25 | 4.67 | 2.79 | 2.00 | 3.13 | 2.25 |
| GLUCOSEZONE | Fitscript | 3.82 | 4.40 | 3.75 | 4.00 | 3.15 | 2.38 | 3.75 | 3.58 |
| Diabetes Words | LES LABORATOIRES SERVIER | 3.74 | 3.30 | 4.38 | 4.84 | 2.43 | 2.13 | 3.38 | 2.50 |
| DiabTrend-Diabetes Assistant | DiabTrend AI Analytics Kft | 3.71 | 4.10 | 4.25 | 4.00 | 2.50 | 2.50 | 3.50 | 3.25 |
| My DiabetesConnect | Dr Ryzian Nizar MD MRCPUK | 3.65 | 3.60 | 4.38 | 3.84 | 2.79 | 2.13 | 3.00 | 3.42 |
| Available from Apple App Store | |||||||||
| myDiabetes* | My mhealth | 4.62 | 4.80 | 4.75 | 5.00 | 3.93 | 4.75 | 4.38 | 4.58 |
| X-PERT | Pulse Digital | 4.61 | 4.60 | 4.50 | 4.84 | 4.50 | 4.13 | 4.38 | 4.67 |
| Invincible * | Invincible Corp | 4.02 | 4.30 | 4.38 | 4.84 | 2.58 | 2.25 | 3.63 | 3.75 |
| Glucose Buddy Diabetes Tracker* | Azumio Inc | 3.95 | 4.3 | 4.25 | 4.17 | 3.07 | 2.50 | 3.88 | 3.92 |
| One Drop Diabetes Management | Informed Data Systems. Inc | 3.93 | 4.00 | 4.38 | 4.00 | 3.36 | 2.88 | 3.50 | 3.75 |
| Dario | LabStyle Innovation Ltd | 3.78 | 4.00 | 4.25 | 4.17 | 2.72 | 3.13 | 3.13 | 3.42 |
| Diabetes Tracker by MyNetDiary | MyNetDiary Inc | 3.70 | 3.80 | 4.13 | 4.17 | 2.72 | 2.25 | 2.75 | 3.25 |
| iHealth Gluco Smart | iHealth Labs Inc | 3.67 | 3.90 | 4.00 | 3.84 | 2.93 | 2.38 | 3.50 | 3.08 |
| Diabetes App: BD Diabetes Care | Becton. Dickinson. and Company | 3.62 | 3.60 | 4.25 | 4.00 | 2.64 | 2.25 | 3.50 | 3.67 |
| DMP | TLC Platforms Inc | 3.61 | 4.00 | 4.00 | 4.17 | 2.29 | 1.88 | 3.50 | 3.09 |
*MHA rated in both systems; numbers represent mean score.
User rating
Sixty-two (51.7%) of MHA had been rated by users at the time of review. The mean user satisfaction rating was 4.14 points on a five-point scale (SD = 0.74). Forty-four (71%) MHA received a mean satisfaction rating of 4 points or higher. There was a significant correlation between the user ratings and the MARS sum scores (r = 0.31, p = 0.015) as well as between the user ratings and the subcategory functionality (r = 0.37, p = 0.003). No significant correlations with further subcategories were found (information quality: r = 0.23; p = 0.070; engagement: r = 0.23, p = 0.073; aesthetics: r = 0.22, p = 0.081).
Implementation of persuasive system design features
A median of three PSD principles were implemented in the MHA. The most frequently implemented principles were: system credibility (M = 1.62, SD = 0.87), dialogue support (M = 1.42, SD = 0.98), primary task support (M = 0.83, SD = 1.25) and social support (M = 0.27, SD = 0.69). Table 2 shows how many principles of each PSD category were implemented per MHA. Table 3 provides the percentages of the MHA incorporating a particular PSD principle. The MARS sum score showed significant correlations with system credibility (r = 0.23, p = 0.010), dialogue support (r = 0.64, p < 0.001), primary task support (r = 0.54, p < 0.001) and social support (r = 0.41, p < 0.001). Dialogue support and social support significantly predicted the MARS sum score. Overall, PSD subcategories can explain a significant proportion of variance in the MARS sum score (R2 = 0.44, p < 0.001; see Table 4). PSD principles per MHA are shown in detail in Supplementary Table S2.
Table 2.
Proportion of apps implementing principles of one of the four persuasive system design categories.
| Number of implemented principles | ||||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | |
| System credibility (%) | 1.7 | 56.7 | 22.5 | 16.7 | 2.5 | – |
| Dialogue support (%) | 11.7 | 55.0 | 17.5 | 11.7 | 4.2 | – |
| Primary task support (%) | 59.2 | 16.7 | 13.3 | 5 | 4.2 | 1.7 |
| Social support (%) | 81.7 | 12.5 | 3.3 | 1.7 | 0.8 | – |
Numbers represent how many apps implemented which amount of the seven principles of each persuasive system design category.
Table 4.
Hierarchical regression analysis for persuasive system design categories predicting MARS sum score.
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β |
| Dialogue support | 0.26 | 0.03 | 0.64*** | 0.22 | 0.04 | 0.55*** | 0.21 | 0.04 | 0.52*** | 0.20 | 0.04 | 0.50*** |
| Primary task support | 0.04 | 0.04 | 0.12 | 0.02 | 0.03 | 0.07 | 0.02 | 0.03 | 0.06 | |||
| Social support | 0.11 | 0.04 | 0.20* | 0.11 | 0.04 | 0.20* | ||||||
| System credibility | 0.04 | 0.03 | 0.10 | |||||||||
| R2 | .41 | .41 | .44 | .44 | ||||||||
| ∆R2 | 0.000 | 0.028 | 0.004 | |||||||||
***p < 0.001; **p < 0.01; *p < 0.05; B, unstandardized regression coefficient; β, standardized regression coefficient.
Concordance with recommended self-management tasks
The evaluated MHA addressed a median of 4.5 of the eight recommended self-management tasks. Ninety-three MHA (77.5%) provided educational content on pathophysiology of and treatment options for diabetes. Furthermore, healthy nutrition (n = 92, 77%), physical activity (n = 79, 66%), monitoring (n = 67, 56%), as well as preventing, detecting and treating acute and chronic complications (n = 69, 58%) were frequently addressed. Problem solving (n = 31, 26%), medication usage (n = 45, 38%) as well as healthy coping with psychosocial issues and concerns (n = 44, 37%) were less often addressed. Twenty-four MHA (20%) targeted 1–2 tasks, 36 (30%) 3–4 tasks, 38 (32%) 5–6 tasks and 15 (12%) seven tasks; all eight self-management tasks were addressed in seven MHA (6%). A detailed overview of the implemented self-management tasks in each MHA is provided in Supplementary Table S3.
Discussion
In this systematic evaluation of 120 commercially available diabetes self-management MHA, we observed an average overall quality (MARS rating) of the MHA (M = 3.20, SD = 0.39) with a median of three implemented PSD principles per MHA. Notably, implemented PSD principles predict MHA quality ratings and the potential of PSD is not exploited yet.
Previous studies on quality using MARS of US-American (M = 2.99, SD = 0.64)17 and Chinese diabetes MHA (M = 3.42, SD = 0.66)16 yielded similar results to our study. Notably, in this study the MARS sum score as well as the subscale functionality were correlated significantly with the user ratings. This is in contradiction to previous evaluations reporting that MARS ratings were not correlated with user ratings28–30,39,40. Given that users commonly rely on user ratings when choosing a MHA for download41, it is an encouraging finding that there are correlations between user ratings and MARS quality ratings in the context of diabetes self-management MHA.
In line with previous studies, the reviewed MHA had higher scores in the functionality and aesthetics subcategories, but lower scores in the engagement and information quality domains16,17. A potential solution to improve engagement is to implement PSD features. The concept of PSD was taken into account in the development of the MARS18 and our results support that the PSD principles of dialogue support and social support, in particular, predict MHA quality ratings and may strengthen the perceived quality of the MHA.
According to the present findings, the least commonly implemented PSD features are social support features. Peer support has been shown to be highly relevant for reducing diabetes distress, diabetes self-care and clinical outcomes, such as mortality42–44. Although online discussion forums are the most frequently implemented social support feature in the MHA examined in the present study, this type of support is often associated with ethical concerns. For instance, there may be counterproductive exchanges between individuals or the anonymity of individuals may not be guaranteed45. Research on the effectiveness of alternative social support principles, which could avoid some of these issues, is still limited and new approaches of social support in MHA should be evaluated46. A further strategy could be to implement multimodal support. For example, the use of MHA could be complemented by telehealth support by peers or clinical staff members47. Notably, the highest rating MHA in this study allows interaction with clinical staff members, suggesting different possibilities of personal interaction.
Regarding the PSD principle dialogue support, we found reminders and suggestions to be the most commonly used principles. Reminders, in particular, seem to be a key app component for supporting successful diabetes management48. An overarching aim of dialogue support features is enhancing the users’ impression that the system is a real person. This can be maintained through the use of avatars which guide the user through the MHA49. Recent studies demonstrated that a virtual avatar providing diabetes treatment information could improve the users’ diabetes self-management50,51.
Principles of system credibility features are widely implemented in the reviewed MHA by providing contact information of MHA developers. In this respect, other principles could be exploited to a greater extent. For instance, incorporating authority figures or offering opportunities for verification (e.g., literature links) could encourage users to perceive the information as more credible and could therefore increase their engagement52.
Finally, in terms of primary task support principles, self-monitoring was found to be most commonly addressed (e.g., apps requesting regular entries of measured glucose values). However, manual entries can be demanding for people with diabetes. Especially for people living with type 1 diabetes, the compactness and ease of use of glucose monitoring could be improved by implementation of an automated MHA-to-sensor connection. Yet, only 10% of evaluated MHA offered this option. Based on the technological possibilities, improvements should be made to facilitate glucose monitoring options53. Another crucial principle of primary task support is tailoring the content to people with diabetes’ needs54. MHA content regulation by diabetes care providers could be an innovative and effective approach to this. For instance, some MHA can be directly used for physician–patient interaction and treatment adjustment wherein the treating physician can set and change the treated person’s goals based on the monitored data (e.g., “myDiabetes”). Tailoring may also be particularly important with regard to age appropriateness (e.g., MHA appealing to younger people). With only three MHA targeting the needs of children and adolescents, the present study findings suggest major shortcomings in this area. Children are only able to understand and comply with self-management recommendations if the provided information is appropriate to their level of cognitive development55. Furthermore, children and adolescents are confronted with age-specific disease-related concerns (e.g., peer-group and diabetes, alcohol and diabetes), for which appropriate content need to be established56,57. Devising age-appropriate MHA could thus help improve diabetes-related outcomes particularly in children and adolescents58,59.
Aside from the technical support by MHA through PSD, this review also focused on the incorporated self-management tasks. The median of 4.5 targeted self-management tasks per MHA suggests significant improvements in the content of diabetes self-management MHA since the findings of Hood et al.13, who reported that MHA contained too little educational information. However, the self-management tasks of problem solving and coping with psychosocial issues are only addressed in one third of the MHA. Given the great importance of mental health in people with diabetes and the lack of time in routine clinical care for discussing mental health problems with concerned persons60–62, eHealth apps could serve as an important low-threshold entry point to these topics63,64.
Limitations
Some limitations must be considered when interpreting the findings of this study. First, we only searched MHA available in European app stores in English or German language. Therefore, the findings cannot be generalized to apps available in other countries or languages. Second, due to the fast-paced nature of MHA development, it is conceivable that the content of some MHA may change or be no longer available on short to medium term13. Third, we used the MARS because it is a standard tool for systematic evaluation of MHA quality. Future studies could use different evaluating instruments which have other specific emphases, such as the APA app evaluation framework65 or the ENLIGHT tool66. Fourth, we only assessed privacy and security on a descriptive level. An assessment of privacy and security practice in smoking cessation and depression MHA with a more elaborated procedure showed that present privacy policies often lack adequate and sufficient information67. Future studies regarding MHA for diabetes could build on this procedure and assess whether data protection is still guaranteed under attack.
Conclusions
At present, the potential of PSD principles implementation in diabetes self-management MHA may not be exploited optimally. PSD principles predict quality ratings of MHA and may play a crucial role in improving the engagement with MHA. Therefore, improvements in the implementation of PSD features in MHA should be achieved. Future studies should evaluate the engagement of real users with specific PSD principles to determine which features and functions work best in real life and thus contribute to the targeted improvement of diabetes self-management MHA. Finally, this study demonstrates an on average moderate quality of MHA with educational content targeting diabetes self-management available in European app stores, with deficits in information quality and engagement. As the more important it seems to establish databases such as mhad.science, psyberguide.org or mindapps.org in order to inform patients and healthcare providers about quality proven MHA in the vast quantity of available but most often not recommendable MHA for diabetes and beyond.
Supplementary Information
Acknowledgements
The article processing charge was funded by the University of Freiburg in the funding program Projekt DEAL.
Author contributions
L.B.S. and A.G. initiated this study and contributed to the study design. A.G. drafted the manuscript and ran the analysis. A.G., C.M., M.S. and M.W., rated apps. A.S. and H.B. assisted the project with their psychodiabetological expertise. All authors revised the manuscript and approved the final version.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was self-funded by the participating institutes. Open Access funding enabled and organized by Projekt DEAL.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
Competing interests
E.M.M., Y.T., L.B.S., H.B. developed and run the German Mobile Health App Database project. The MHAD is a self-funded project at Ulm University with no commercial interests. H.B., L.B.S. and E.M.M. received payments for talks and workshops in the context of e-mental-health. All other authors declare no conflicts of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-07544-2.
References
- 1.Tamayo T, et al. Diabetes in Europe: an update. Diabetes Res. Clin. Pract. 2014;103:206–217. doi: 10.1016/j.diabres.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Data and statistics. https://www.euro.who.int/en/health-topics/noncommunicable-diseases/diabetes/data-and-statistics.
- 3.Beck, J., Greenwood, D. A., Blanton, L., Bollinger, S. T., Butcher, M. K. & Condon, J. E. National Standards for Diabetes Self-Management Education and Support (2017).
- 4.Peyrot M, Peeples M, Tomky D, Charron-Prochownik D, Weaver T. Development of the American association of diabetes educators' diabetes self-management assessment report tool. Diabetes Educ. 2007;33:818–826. doi: 10.1177/0145721707307614. [DOI] [PubMed] [Google Scholar]
- 5.Lange K, Swift P, Pańkowska E, Danne T. ISPAD clinical practice consensus guidelines 2014. Diabetes education in children and adolescents. Pediatr. Diabetes. 2014;15(Suppl 20):77–85. doi: 10.1111/pedi.12187. [DOI] [PubMed] [Google Scholar]
- 6.Kitsiou S, Paré G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes: an overview of systematic reviews. PLoS ONE. 2017;12:e0173160. doi: 10.1371/journal.pone.0173160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cui M, Wu X, Mao J, Wang X, Nie M. T2DM self-management via smartphone applications: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0166718. doi: 10.1371/journal.pone.0166718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonoto BC, et al. Efficacy of mobile apps to support the care of patients with diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. JMIR mHealth uHealth. 2017;5:e4. doi: 10.2196/mhealth.6309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang Z, Soljak M, Boehm BO, Car J. Clinical relevance of smartphone apps for diabetes management: a global overview. Diabetes Metab. Res. Rev. 2018;34:e2990. doi: 10.1002/dmrr.2990. [DOI] [PubMed] [Google Scholar]
- 10.Moumtzoglou A. Mobile Health Applications for Quality Healthcare Delivery. IGI Global; 2019. [Google Scholar]
- 11.Whitehead L, Seaton P. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J. Med. Internet Res. 2016;18:e97. doi: 10.2196/jmir.4883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klonoff DC. The current status of mHealth for diabetes: will it be the next big thing? J. Diabetes Sci. Technol. 2013;7:749–758. doi: 10.1177/193229681300700321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hood M, et al. What do we know about mobile applications for diabetes self-management? A review of reviews. J. Behav. Med. 2016;39:981–994. doi: 10.1007/s10865-016-9765-3. [DOI] [PubMed] [Google Scholar]
- 14.Eng DS, Lee JM. The promise and peril of mobile health applications for diabetes and endocrinology. Pediatr. Diabetes. 2013;14:231–238. doi: 10.1111/pedi.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J. Med. Internet Res. 2014;16:e104. doi: 10.2196/jmir.2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gong E, et al. Quality, functionality, and features of Chinese mobile apps for diabetes self-management: systematic search and evaluation of mobile apps. JMIR mHealth uHealth. 2020;8:e14836. doi: 10.2196/14836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chavez S, et al. Mobile apps for the management of diabetes. Diabetes Care. 2017;40:e145–e146. doi: 10.2337/dc17-0853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stoyanov SR, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR mHealth uHealth. 2015;3:e27. doi: 10.2196/mhealth.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelders SM, Kok RN, Ossebaard HC, van Gemert-Pijnen JEWC. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J. Med. Internet Res. 2012;14:e152. doi: 10.2196/jmir.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ryan JC, et al. Identifying critical features of type two diabetes prevention interventions: a Delphi study with key stakeholders. PLoS ONE. 2021;16:e0255625. doi: 10.1371/journal.pone.0255625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oinas-Kukkonen H, Harjumaa M. Persuasive system design: key issues, process model, and system features. CAIS. 2009;24:28. [Google Scholar]
- 22.Baumeister H, Kraft R, Baumel A, Pryss R, Messner EM. Persuasive e-health design for behavior change. In: Baumeister H, Montag C, editors. Digital phenotyping and mobile sensing. Springer Nature; 2019. [Google Scholar]
- 23.Wozney L, et al. How do eHealth programs for adolescents work? A realist review of persuasive system design components in internet-based psychological therapies. J. Med. Internet Res. 2017;19:e266. doi: 10.2196/jmir.7573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Radomski AD, et al. Design and delivery features that may improve the use of internet-based cognitive behavioral therapy for children and adolescents with anxiety: a realist literature synthesis with a persuasive systems design perspective. J. Med. Internet Res. 2019;21:e11128. doi: 10.2196/11128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Priesterroth L, Grammes J, Holtz K, Reinwarth A, Kubiak T. Gamification and behavior change techniques in diabetes self-management apps. J. Diabetes Sci. Technol. 2019;13:954–958. doi: 10.1177/1932296818822998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu Y, et al. A comparison of functional features in Chinese and US mobile apps for diabetes self-management: a systematic search in app stores and content analysis. JMIR mHealth uHealth. 2019;7:e13971. doi: 10.2196/13971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stach, M. et al. Mobile health app database: a repository for quality ratings of mHealth apps, 427–432.
- 28.Terhorst Y, et al. Systematic evaluation of content and quality of English and German pain apps in European app stores. Internet Interv. 2021;24:100376. doi: 10.1016/j.invent.2021.100376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sander LB, et al. 'Help for trauma from the app stores?' A systematic review and standardised rating of apps for Post-Traumatic Stress Disorder (PTSD) Eur. J. Psychotraumatol. 2020;11:1701788. doi: 10.1080/20008198.2019.1701788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Terhorst Y, Rathner E-M, Baumeister H, Sander L. «Hilfe aus dem App-Store?»: Eine systematische Übersichtsarbeit und Evaluation von Apps zur Anwendung bei Depressionen. Verhaltenstherapie. 2018;28:101–112. [Google Scholar]
- 31.Messner E-M, et al. The German version of the mobile app rating scale (MARS-G): development and validation study. JMIR mHealth uHealth. 2020;8:e14479. doi: 10.2196/14479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Terhorst Y, et al. Validation of the mobile application rating scale (MARS) PLoS ONE. 2020;15:e0241480. doi: 10.1371/journal.pone.0241480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu, P. F. & Bernardi, R. Community attachment and emotional well-being: an empirical study of an online community for people with diabetes. ITP ahead-of-print (2020).
- 34.Hershcovitz Y, Dar S, Feniger E. Continuous reduction of blood glucose average during one year of glucose monitoring using a digital monitoring system in a high-risk population. Diabetes. 2018;67:78-LB. [Google Scholar]
- 35.Quinn CC, et al. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934–1942. doi: 10.2337/dc11-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fu HNC, Rizvi RF, Wyman JF, Adam TJ. Usability evaluation of four top-rated commercially available diabetes apps for adults with type 2 diabetes. Comput. Inform. Nurs. CIN. 2020;38:274–280. doi: 10.1097/CIN.0000000000000596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Osborn CY, et al. One drop mobile: an evaluation of hemoglobin A1c improvement linked to app engagement. JMIR Diabetes. 2017;2:e21. doi: 10.2196/diabetes.8039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deakin T. The diabetes pandemic: Is structured education the solution or an unnecessary expense? Pract. Diabetes. 2011;28:1–14. [Google Scholar]
- 39.Portenhauser AA, et al. Mobile apps for older adults: systematic search and evaluation within online stores. JMIR Aging. 2021;4:e23313. doi: 10.2196/23313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Domhardt M, et al. Mobile-based interventions for common mental disorders in youth: a systematic evaluation of pediatric health apps. Child Adolesc. Psychiatry Mental Health. 2021;15:49. doi: 10.1186/s13034-021-00401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mudambi SM, Schuff D. What makes a helpful online review? A study of customer reviews on amazon.com. MIS Q. 2010;34:185–200. [Google Scholar]
- 42.Ju C, et al. Effect of peer support on diabetes distress: a cluster randomized controlled trial. Diabetic Med. J. Br. Diabetic Assoc. 2018;35:770–775. doi: 10.1111/dme.13625. [DOI] [PubMed] [Google Scholar]
- 43.Song Y, Nam S, Park S, Shin I-S, Ku BJ. The impact of social support on self-care of patients with diabetes: what is the effect of diabetes type? Systematic review and meta-analysis. Diabetes Educ. 2017;43:396–412. doi: 10.1177/0145721717712457. [DOI] [PubMed] [Google Scholar]
- 44.Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr. Diabetes Rep. 2012;12:769–781. doi: 10.1007/s11892-012-0317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sharkey S, et al. Ethical practice in internet research involving vulnerable people: lessons from a self-harm discussion forum study (SharpTalk) J. Med. Ethics. 2011;37:752–758. doi: 10.1136/medethics-2011-100080. [DOI] [PubMed] [Google Scholar]
- 46.Vlahu-Gjorgievska, E., Alkorbi, A. S., Nushayli, M. M. & Win, K. W. Persuasive social support features in diabetes self-management mHealth applications.
- 47.Tang, P. Y. et al. Complementarity of digital health and peer support: “This Is What’s Coming”. Front. Clin. Diabetes Healthc.2 (2021). [DOI] [PMC free article] [PubMed]
- 48.Jimenez G, et al. Reminders for medication adherence in type 2 diabetes management apps. J. Pharm. Pract. Res. 2020;50:78–81. [Google Scholar]
- 49.Duncan-Carnesciali J, Wallace BC, Odlum M. An evaluation of a diabetes self-management education (DSME) intervention delivered using avatar-based technology: certified diabetes educators' ratings and perceptions. Diabetes Educ. 2018;44:216–224. doi: 10.1177/0145721718769474. [DOI] [PubMed] [Google Scholar]
- 50.Faddoul G. & Chatterjee, S. The virtual diabetician: a prototype for a virtual avatar for diabetes treatment using persuasion through storytelling. Proceedings of the 25th Americas Conference on Information Systems (AMCIS’2019), Cancún, Mexico, 15–17 August 2019.
- 51.Wonggom P, Kourbelis C, Newman P, Du H, Clark RA. Effectiveness of avatar-based technology in patient education for improving chronic disease knowledge and self-care behavior: a systematic review. JBI Database Syst. Rev. Implement. Rep. 2019;17:1101–1129. doi: 10.11124/JBISRIR-2017-003905. [DOI] [PubMed] [Google Scholar]
- 52.Oinas-Kukkonen, H. Persuasive technology, in Third International Conference, PERSUASIVE 2008, Oulu, Finland, June 4–6, 2008 Proceedings 5033 (2008).
- 53.Cappon G, Acciaroli G, Vettoretti M, Facchinetti A, Sparacino G. Wearable continuous glucose monitoring sensors: a revolution in diabetes treatment. Electronics. 2017;6:65. [Google Scholar]
- 54.Kim MT, et al. Motivating people to sustain healthy lifestyles using persuasive technology: a pilot study of Korean Americans with prediabetes and type 2 diabetes. Patient Educ. Couns. 2019;102:709–717. doi: 10.1016/j.pec.2018.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Christie D. How do children and adolescents understand their diabetes? Pract. Diab. 2019;36:117. [Google Scholar]
- 56.Geirhos A, et al. Involving patients' perspective in the development of an internet- and mobile-based CBT intervention for adolescents with chronic medical conditions: findings from a qualitative study. Internet Interv. 2021;24:100383. doi: 10.1016/j.invent.2021.100383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Miller KM, Beck RW, Foster NC, Maahs DM. HbA1c levels in type 1 diabetes from early childhood to older adults: a deeper dive into the influence of technology and socioeconomic status on HbA1c in the T1D exchange clinic registry findings. Diabetes Technol. Ther. 2020;22:645–650. doi: 10.1089/dia.2019.0393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Swartwout E, El-Zein A, Deyo P, Sweenie R, Streisand R. Use of gaming in self-management of diabetes in teens. Curr. Diabetes Rep. 2016;16:59. doi: 10.1007/s11892-016-0754-2. [DOI] [PubMed] [Google Scholar]
- 59.Domhardt M, Schröder A, Geirhos A, Steubl L, Baumeister H. Efficacy of digital health interventions in youth with chronic medical conditions: a meta-analysis. Internet Interv. 2021;24:100373. doi: 10.1016/j.invent.2021.100373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hermanns N, Ehrmann D, Finke-Groene K, Kulzer B. Trends in diabetes self-management education: where are we coming from and where are we going? A narrative review. Diabetic Med. J. Br. Diabetic Assoc. 2020;37:436–447. doi: 10.1111/dme.14256. [DOI] [PubMed] [Google Scholar]
- 61.Zhang Y, et al. Exploration of users' perspectives and needs and design of a type 1 diabetes management mobile app: mixed-methods study. JMIR mHealth uHealth. 2018;6:e11400. doi: 10.2196/11400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baptista S, et al. What do adults with type 2 diabetes want from the "perfect" app? Results from the second diabetes MILES: Australia (MILES-2) study. Diabetes Technol. Ther. 2019;21:393–399. doi: 10.1089/dia.2019.0086. [DOI] [PubMed] [Google Scholar]
- 63.Bendig E, et al. Internet-based interventions in chronic somatic disease. Deutsches Arzteblatt Int. 2018;115:659–665. doi: 10.3238/arztebl.2018.0659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lunkenheimer F, et al. Effectiveness and cost-effectiveness of guided Internet- and mobile-based CBT for adolescents and young adults with chronic somatic conditions and comorbid depression and anxiety symptoms (youthCOACHCD): Study protocol for a multicentre randomized controlled trial. Trials. 2020;21:253. doi: 10.1186/s13063-019-4041-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Torous JB, et al. A hierarchical framework for evaluation and informed decision making regarding smartphone apps for clinical care. Psychiatr. Serv. 2018;69:498–500. doi: 10.1176/appi.ps.201700423. [DOI] [PubMed] [Google Scholar]
- 66.Baumel A, Faber K, Mathur N, Kane JM, Muench F. Enlight: A comprehensive quality and therapeutic potential evaluation tool for mobile and web-based eHealth interventions. J. Med. Internet Res. 2017;19:e82. doi: 10.2196/jmir.7270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huckvale K, Torous J, Larsen ME. Assessment of the data sharing and privacy practices of smartphone apps for depression and smoking cessation. JAMA Netw. Open. 2019;2:e192542. doi: 10.1001/jamanetworkopen.2019.2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).