Dr. Wei and colleagues present a thorough examination of percutaneous gastrostomy techniques, including indications and contraindications for gastrostomy tube placements in An overview of percutaneous endoscopic gastrostomy tube placement in the intensive care unit. This is an important overview as research demonstrates critically ill patients benefit from aggressive timely care, and the critical care patient population represents over 50% of gastrostomy tubes placed in the USA (1,2). One percutaneous gastrostomy technique in the review, Percutaneous Ultrasound Gastrostomy (PUG), is a relatively new technique designed specifically for the ICU bedside. This technique has rapidly evolving implementation and outcomes research. Understandably, the authors requested more rigorous outcomes data on PUG, “further studies are needed to explore the safety and efficacy of the PUMA-G (PUG) technique in comparison to standard PEG technique”, but excluded the latest PUG literature available at the time of the review’s publication date. Therefore, an updated review of PUG literature is detailed below.
Most importantly, PUG is at least as safe as percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG). Two prospective studies (n=50) have shown an equivalent safety profile compared to matched retrospective cohorts (3,4). Critical care teams have demonstrated decreased time to gastrostomy placement for their patients when compared to PEG, decreased ICU length of stay (LOS) and immense utility in the COVID-19 pandemic (5-7). Furthermore, no visceral injuries, such as colon or liver injuries seen in PEG, have been reported in PUG because proceduralists have real-time ultrasound needle visualization throughout gastrostomy tract formation, as compared to the blind nature of transillumination in PEG. Visceral injury was described as an “unavoidable risk” when PEG was developed and first critiqued in the early 1980s (8). Ultrasound guidance via PUG now makes visceral injuries avoidable in percutaneous gastrostomy. For example, Figure 1 shows clear tissue planes and the internal balloon catheter under magnetic gastropexy. Data from 300 PUG cases were compiled and submitted as clinical evidence supporting CE Mark, which was granted in May 2021. This data from US (under US FDA clearance) and Canadian cases reported no visceral injuries while using the PUMA-G System, the device used in PUG.
Figure 1.
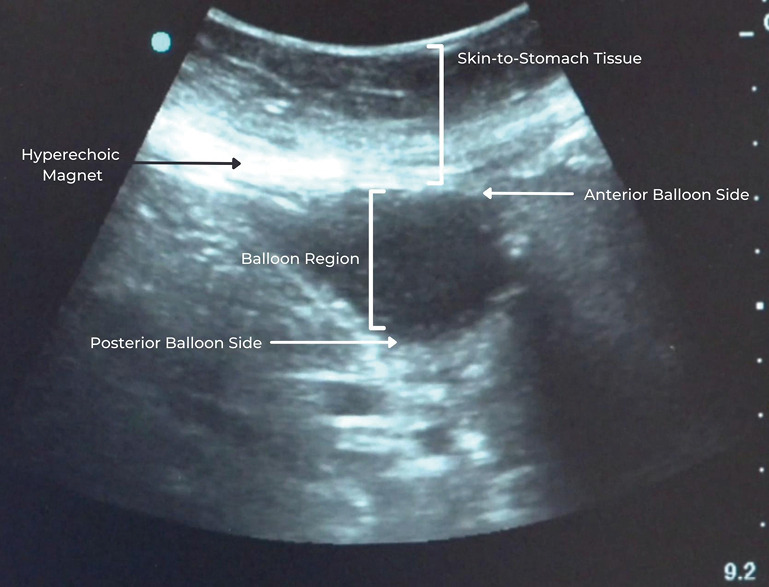
Real-time ultrasound of internal balloon catheter under magnetic gastropexy and clear gastrostomy tract.
Dr. Wei and colleagues describe concomitant tracheostomy and gastrostomy as the future of advanced critical care medicine—“the next logical evolution would be for interventional pulmonologists to perform both procedures at the same time when indicated. This would minimize the risks associated with sedation and paralytics as the two procedures can be merged into a single coordinated procedure performed by the same physician.” However, this presents significant training and credentialing hurdles for critical care physicians without endoscopy training. In contrast, any critical care physician can be trained and credentialed in percutaneous dilation tracheostomy (PDT) and PUG using existing skill sets. Concomitant PDT and PUG, otherwise known as TPUGTM, has shown to be safe and efficient, and have been performed by critical care physicians, pulmonary critical care physicians, interventional pulmonary critical care physicians and neuro-critical care physicians (6,7).
There are limitations and learning curves to PUG, as Dr. Wei and colleagues noted based on early PUG literature, but these limitations and learning curves are no different than other percutaneous gastrostomy techniques. When choosing appropriate cases, PUG users are trained to anticipate gastrostomy tract depth instead of BMI, as BMI is a poor predictor of gastrostomy tract depth. Pre-existing abdominal CAT scans can help estimate gastrostomy tract depth, otherwise real-time ultrasound can measure gastrostomy tract depth during a PUG procedure when magnetic gastropexy is achieved. Importantly, the FDA-cleared indications for use do not rely on BMI, instead focusing on tract depths <4.5 cm. These depths are achievable in the obese population with gastric insufflation, and PUG cases have been successfully performed in morbidly obese patients of 50+ BMIs. With respect to learning curves, critical care physicians with PUG experience (and PDT) have reported bedside PUG procedure times as short as 8 minutes and TPUG procedure times as short as 30 minutes. PUG has also been reduced to the minimal staffing level it was designed for, shown effective with one physician and one nurse at the bedside. TPUGs do require a third provider, typically a respiratory therapist and/or second physician (6).
Over 200,000 gastrostomy tubes are placed in the USA every year and 50% of gastrostomies placed are in the critically ill patient population (1). Meeting this care demand requires a safe approach, ubiquitous to all critical care environments and critical care physicians. Point of care ultrasound is the optimal choice, as it has been safely utilized in both bedside tracheostomy and gastrostomy (3,4,6,7,9). When appropriately indicated, based upon current literature, PUG or TPUG can serve as a primary option for safe and timely care for your critically ill patients.
Supplementary
The article’s supplementary files as
Acknowledgments
The author would like to thank the dedicated professionals who aided in the development of coaptive ultrasound technologies and their transformation into PUMA System applications for better patient care.
Funding: None.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Provenance and Peer Review: This article was a standard submission to the journal. The article has not undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-1576/coif). SPT is the inventor of PUG, and has developed several patents on coaptive ultrasound and specialized guidewires, and is the CMO and partial owner of CoapTech Inc, the only manufacturer of PUMA-G System. The author has no other conflicts of interest to declare.
References
- 1.Law AC, Stevens JP, Walkey AJ. Gastrostomy Tube Use in the Critically Ill, 1994-2014. Ann Am Thorac Soc 2019;16:724-30. 10.1513/AnnalsATS.201809-638OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doig GS, Heighes PT, Simpson F, et al. Early enteral nutrition, provided within 24 h of injury or intensive care unit admission, significantly reduces mortality in critically ill patients: a meta-analysis of randomised controlled trials. Intensive Care Med 2009;35:2018-27. 10.1007/s00134-009-1664-4 [DOI] [PubMed] [Google Scholar]
- 3.Accorsi F, Chung J, Mujoomdar A, et al. Percutaneous ultrasound gastrostomy (PUG): first prospective clinical trial. Abdom Radiol (NY) 2021;46:5377-85. 10.1007/s00261-021-03200-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reis SP, Brejt SZ, Weintraub JR, et al. Percutaneous Ultrasound Guided Gastrostomy Tube Placement: A Prospective Cohort Trial. J Intensive Care Med 2021. [Epub ahead of print]. doi: . 10.1177/08850666211015595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olivieri PP, Abdulmahdi M, Heavner JJ. Bedside percutaneous ultrasound gastrostomy tube placement by critical care physicians. J Clin Ultrasound 2021;49:28-32. 10.1002/jcu.22895 [DOI] [PubMed] [Google Scholar]
- 6.Olivieri P, Heavner J, Abdulmahdi M. Concomitant percutaneous dilatation tracheostomy and percutaneous ultrasound gastrostomy: methods to ensure safe practice standards during the COVID-19 pandemic. Chest 2020;158:A2470. 10.1016/j.chest.2020.09.047 [DOI] [Google Scholar]
- 7.Neurocritical Care Society Virtual 19th Annual Meeting October 26-29, 2021. Neurocrit Care 2021;35:177-461. 10.1007/s12028-021-01352-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ponsky JL, Gauderer MW, Stellato TA. Percutaneous endoscopic gastrostomy. Review of 150 cases. Arch Surg 1983;118:913-4. 10.1001/archsurg.1983.01390080021006 [DOI] [PubMed] [Google Scholar]
- 9.Rudas M, Seppelt I, Herkes R, et al. Traditional landmark versus ultrasound guided tracheal puncture during percutaneous dilatational tracheostomy in adult intensive care patients: a randomised controlled trial. Crit Care 2014;18:514. 10.1186/s13054-014-0514-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


