Abstract
Study Design:
Cross-sectional observational cohort study.
Objective:
To investigate preparation, response, and economic impact of COVID-19 on private, public, academic, and privademic spine surgeons.
Methods:
AO Spine COVID-19 and Spine Surgeon Global Impact Survey includes domains on surgeon demographics, location of practice, type of practice, COVID-19 perceptions, institutional preparedness and response, personal and practice impact, and future perceptions. The survey was distributed by AO Spine via email to members (n = 3805). Univariate and multivariate analyses were performed to identify differences between practice settings.
Results:
A total of 902 surgeons completed the survey. In all, 45.4% of respondents worked in an academic setting, 22.9% in privademics, 16.1% in private practice, and 15.6% in public hospitals. Academic practice setting was independently associated with performing elective and emergent spine surgeries at the time of survey distribution. A majority of surgeons reported a >75% decrease in case volume. Private practice and privademic surgeons reported losing income at a higher rate compared with academic or public surgeons. Practice setting was associated with personal protective equipment availability and economic issues as a source of stress.
Conclusions:
The current study indicates that practice setting affected both preparedness and response to COVID-19. Surgeons in private and privademic practices reported increased worry about the economic implications of the current crisis compared with surgeons in academic and public hospitals. COVID-19 decreased overall clinical productivity, revenue, and income. Government response to the current pandemic and preparation for future pandemics needs to be adaptable to surgeons in all practice settings.
Keywords: COVID-19, coronavirus, spine; surgeons, private practice, global, impact
Introduction
The COVID-19 pandemic has swiftly become the defining global health crisis of our time.1-3 Patients infected with COVID-19 have placed a colossal strain on health care systems and medical practices across the world. 4 Epidemiologic models forecast ongoing demands on hospital resources and staff across the world.5-8 Fulfilling these demands in severely affected regions has proven daunting for many health care systems. 9 To ensure appropriate availability of health care resources, most governments and hospitals enacted policies leading to restrictions on clinical activities, postponement of all elective surgeries, and reductions in staffing. 10 The future impact of these government, local, and hospital policies remains relatively unknown.
With low back pain ranking as the most disabling condition worldwide and neck-related issues ranked as the fourth leading cause of disability globally, there is a major demand for spine providers.11,12 A recent study by Louie et al 13 emphasized, in over 900 spine surgeons worldwide, that COVID-19 had extensive clinical, personal, and financial impacts; however, such impact varied. However, it remains unknown whether the practice setting played a role in preparedness, response, and economic impact. Previous studies have focused on the effect of COVID-19 on emergency room, critical care, and internal medicine specialties.14,15 Nonetheless, the impact of preparedness on subspecialty spine surgery remains a topic that has not been well elucidated.10,13,16,17
The COVID-19 pandemic comes amid a period of change in health care economics.18,19 Over the past decade, the United States has seen a precipitous decline in physician private practice, from 62% in 2008 to 35% in 2014. 20 Coinciding with the shift in practice types, is the transition away from fee-for-service reimbursement toward alternative payment models.21,22 In an era of increased financial stress on surgeons and health systems, the COVID-19 pandemic has the potential to exponentiate the problem.
With the drastic reduction in elective surgeries and in-person clinic visits occurring during COVID-19-related shutdowns, surgeons who rely on clinical productivity as a major source of revenue may see a reduction in income. The American Medical Association issued guidance on how private medical practices could adapt to the financial and logistical stresses of this global pandemic. 23 However, what is not known, is how spine surgeons in various practice settings prepared for, and responded to, COVID-19. The current study addresses the perceived preparation of private, public, academic, and privademic spine surgeons for COVID-19. This study also defines the varied responses experienced by these providers and outlines the potential economic implications for spine surgeons worldwide.
Methods
Study Design
The AO Spine COVID-19 and Spine Surgeon Global Impact Survey was developed by an international working group of spine surgeons, epidemiologists and surgical trainees who are experts in spinal disorders. Question selection was based on a Delphi methodology24,25 to achieve consensus through numerous rounds of review. Domains of the survey included surgeon demographics, location of practice, type of practice, COVID-19 perceptions, institutional preparedness and response, personal and practice impact, and future perceptions. Specific demographics obtained include age, gender, country of practice, region of practice, population of city of practice, specialty, fellowship experience, year in practice, and practice type. For the purpose of this study, practice type was either private, academic, privademic, or public. Privademic refers to a hybrid practice model whereby physicians work within a private practice at an academic institution enabling them to contribute to high-quality literature, discoveries, and innovation. 26
Survey Distribution
The 73-item, English language survey was distributed via email to the AO Spine membership who previously agreed to receive surveys for research purposes (n = 3805). AO Spine provided the largest available international network of spine surgeons (www.aospine.org). The survey recipients were asked to complete the questionnaire during a predefined 9-day period (March 27, 2020 to April 4, 2020). Respondents were informed that their participation was voluntary, that they could end their participation at any time, and that all data would be kept confidential. Participants were informed that findings from the study would be disseminated in peer-reviewed journals, websites, and social media.
Statistical Analyses
All statistical analyses were performed with SAS (SAS Institute). Graphical representation of survey responses was performed using Excel (Microsoft Inc). Percentages and means were made for count data and rank-order questions, respectively. All means were presented with standard deviations (mean ± standard deviation). Respondents were not required to answer all questions, thus, the number of responses for each question varies. Statistical analyses were performed to assess significant differences in count data using a combination of Fisher’s exact and chi-square tests, where applicable. For variables with significance on 4-way chi-square tests, post hoc 2-way chi-square was performed for direct comparison between groups. Differences in continuous variables between groups were assessed using analysis of variance (ANOVA).
A nominal multivariate regression analysis was performed to control for baseline demographic differences between the groups (gender, home city population, region, fellowship training, and practice breakdown). Outcome variables with P < .200 on univariate analysis were assessed in the multivariate model. Variables with dichotomous categorical outcomes are presented as odds ratios (ORs) and 95% confidence intervals (CIs) were also noted. An OR > 1 indicated increased occurrence of outcome. An OR < 1 indicated decreased occurrence of outcome. Variables with numerous categorical outcomes were presented as likelihood ratios (LRs). The threshold for statistical significance for all tests was P < .05.
Results
Overall, 902 spine surgeons from 91 countries completed the survey representing all 7 predefined global regions (Africa, Asia, Australia, Europe, the Middle East, North America, and South America/Latin America) (Figure 1). However, only 892 surgeons provided information on their practice setting and were included in the final analysis. Most surgeons were from Europe (242/881; 27.5%), followed by Asia (213/881; 24.2%) and North America (152/881; 17.3%). By country, the most survey responses were from the United States (128/902; 14.2%), China (73/902; 8.1%), and Egypt (66/902; 7.3%).
Figure 1.
Distribution of survey responses by country. World map depicting number of survey responses received internationally. Color-filled countries indicate at least one survey was received. Green = Under 10 surveys received. Teal = 11 to 25. Red = 26 to 50. Orange = 51 to 100. Dark blue = Over 100. Light blue = No surveys received.
The majority of respondents were male (826/881; 93.8%), ranging in age from 35 to 44 years (344/895; 38.4%), and orthopedic surgeons by residency training (637/902; 70.6%). When stratified by practice type, most surgeons reported working in an academic setting (405/892; 45.4%), followed by privademics (204/892; 22.9%), private practice (144/892; 16.1%), or public hospitals (139/892; 15.6%) (Table 1). There were baseline differences in demographics between practice settings (Table 1). Gender (P = .0013), home city population (P < .0001), region (P < .0001), fellowship training (P = .0039), and practice breakdown (ie, research, clinical, teaching) (P = .0003, P = .011, P = .0009, respectively) varied by practice setting.
Table 1.
Respondent Demographics by Practice Setting.a
| Academic (n = 405), n (%) | Privademic (n = 204), n (%) | Private (n = 144), n (%) | Public (n = 139), n (%) | P | |
|---|---|---|---|---|---|
| Age (years) | n = 405 | n = 203 | n = 144 | n = 139 | .25 |
| 25-34 | 66 (16.3) | 27 (13.3) | 18 (12.5) | 19 (13.7) | |
| 35-44 | 133 (32.8) | 91 (44.8) | 57 (39.6) | 61 (43.9) | |
| 45-54 | 120 (29.6) | 47 (23.2) | 39 (27.1) | 37 (26.6) | |
| 55-64 | 75 (18.5) | 34 (16.7) | 23 (16) | 18 (12.9) | |
| 65+ | 11 (2.7) | 4 (2.0) | 7 (4.9) | 4 (2.9) | |
| Male sex | 372 (91.9) | 196 (96.1) | 137 (95.1) | 117 (84.2) | .0013 |
| Estimated home city population | n = 403 | n = 203 | n = 144 | n = 139 | <.0001 |
| <100 000 | 14 (3.5) | 3 (1.5) | 6 (4.2) | 22 (15.8) | |
| 100 000-500 000 | 79 (19.6) | 33 (16.3) | 30 (20.8) | 43 (30.9) | |
| 500 000-1 000 000 | 71 (17.6) | 29 (14.3) | 21 (14.6) | 15 (10.8) | |
| 1 000 000-2 000 000 | 54 (13.4) | 47 (23.2) | 23 (16) | 20 (14.4) | |
| >2 000 000 | 185 (45.9) | 91 (44.8) | 64 (44.4) | 39 (28.1) | |
| Geographic region | n = 400 | n = 198 | n = 142 | n = 137 | <.0001 |
| Africa | 20 (5.0) | 13 (6.6) | 7 (4.9) | 4 (2.9) | |
| Asia | 127 (31.8) | 29 (14.6) | 26 (18.3) | 30 (21.9) | |
| Australia | 1 (0.3) | 4 (2.0) | 1 (0.7) | 2 (1.5) | |
| Europe | 115 (28.9) | 47 (23.7) | 20 (14.1) | 59 (43.1) | |
| Middle east | 23 (5.8) | 28 (14.1) | 15 (10.6) | 11 (8.0) | |
| North America | 91 (22.8) | 23 (11.6) | 30 (21.1) | 7 (5.1) | |
| South/Latin America | 23 (5.8) | 54 (27.3) | 43 (30.3) | 24 (17.5) | |
| Specialty | n = 401 | n = 202 | n = 140 | n = 138 | .63 |
| Neurosurgery | 100 (24.9) | 55 (27.2) | 41 (29.3) | 36 (26.1) | |
| Orthopedics | 294 (73.3) | 145 (71.8) | 97 (69.3) | 99 (71.7) | |
| Pediatric surgery | 0 (0) | 1 (0.5) | 1 (0.7) | 0 (0) | |
| Trauma | 7 (1.7) | 1 (0.5) | 1 (0.7) | 3 (2.2) | |
| Fellowship trained | 282 (69.3) | 158 (77.5) | 112 (77.8) | 86 (61.9) | .0039 |
| Years since training completion | n = 279 | n = 158 | n = 109 | n = 84 | .23 |
| <5 | 64 (22.9) | 38 (24.1) | 33 (30.3) | 4 (28.6) | |
| 5-10 | 53 (19) | 41 (26) | 24 (22) | 19 (22.6) | |
| 10-15 | 53 (19) | 25 (15.8) | 13 (11.9) | 13 (15.5) | |
| 15-20 | 63 (22.6) | 19 (12) | 20 (18.4) | 15 (17.9) | |
| >20 | 46 (16.5) | 35 (22.2) | 19 (17.4) | 13 (15.5) | |
| Percent research | n = 404 | n = 204 | n = 143 | n = 138 | .0003 |
| 0%-25% | 306 (75.7) | 167 (81.9) | 129 (90.2) | 126 (91.3) | |
| 26%-50% | 78 (19.3) | 29 (14.2) | 13 (9.1) | 8 (5.8) | |
| 51%-75% | 10 (2.5) | 6 (2.9) | 1 (0.7) | 4 (2.9) | |
| 76%-100% | 10 (2.5) | 2 (1) | 0 (0) | 0 (0) | |
| Percent clinical | n = 404 | n = 204 | n = 143 | n = 139 | .011 |
| 0%-25% | 13 (3.2) | 3 (1.5) | 4 (2.8) | 2 (1.4) | |
| 26%-50% | 47 (11.6) | 19 (9.3) | 10 (7) | 10 (7.2) | |
| 51%-75% | 96 (23.8) | 53 (26) | 16 (11.2) | 29 (20.9) | |
| 76%-100% | 248 (61.4) | 129 (63.2) | 113 (79) | 98 (70.5) | |
| Percent teaching | n = 404 | n = 203 | n = 143 | n = 138 | .0009 |
| 0%-25% | 292 (72.3) | 135 (66.5) | 124 (86.7) | 114 (82.6) | |
| 26%-50% | 70 (17.2) | 49 (24.1) | 15 (10.5) | 17 (12.3) | |
| 51%-75% | 28 (6.9) | 14 (6.9) | 2 (1.4) | 6 (4.4) | |
| 76%-100% | 14 (3.5) | 5 (2.5) | 2 (1.4) | 1 (0.7) |
a Demographic data presented as number of respondents (n) and percent of total respondents for specific question (%). For privacy reasons, respondents were not required to answer all demographic questions.
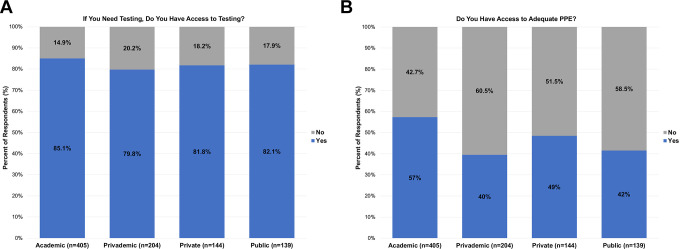
There were no differences in access to COVID testing by practice setting (p = 0.42), with 82.9% of respondents reporting adequate access (Table 2; Figure 2a). Surgeons reported having adequate personal protective equipment (PPE) at a rate of 49.6%; there was significant variation in PPE availability by practice setting (P = .0002) (Table 2). Comparison between surgeons at academic versus public hospitals revealed a significant difference in the availability of adequate PPE (217/379; 57.6% vs 51/123; 41.5%, P = .0023) (Figure 2b). On multivariate analysis, surgeons in academic practice were more likely to have adequate PPE compared to surgeon in privademic practice (OR 1.72, 95% CI 1.16-2.56, P = .0086) (Table 3). There was significant variation in the availability of N-95 masks (P = .018), face shields (P < .0001), gowns (P = .001), and full-face respirators (P = .0007) between the various practice settings (Table 2). On multivariate analysis, practice setting was independently associated with these variations in PPE (Table 3). On univariate analysis, there was significant variation in availability of ventilators (P = .0024) with 47.2% of surgeons at academic hospitals reporting adequate access to ventilators. On multivariate analysis, academic practice setting was independently associated with better ventilator supply compared to privademic practice (OR 1.59, 95% CI 1.04-2.38, P = .031) (Table 3).
Table 2.
COVID-19 Preparedness by Practice Setting.
| Academic, n (%) | Privademic, n (%) | Private, n (%) | Public, n (%) | P | |
|---|---|---|---|---|---|
| Access to COVID testing | 326 (85.1) | 158 (79.8) | 112 (81.8) | 101 (82.1) | .42 |
| Formal hospital guidelines | 227 (66.8) | 103 (58.9) | 60 (50.9) | 60 (53.1) | .0048 |
| Adequate PPE | 217 (57.3) | 77 (39.5) | 66 (48.5) | 51 (41.5) | .0002 |
| Forms of PPE | |||||
| N-95 mask | 226 (55.8) | 91 (44.6) | 63 (43.8) | 68 (48.9) | .018 |
| Surgical mask | 344 (84.9) | 169 (82.8) | 113 (78.5) | 108 (77.7) | .15 |
| Face shield | 223 (55.1) | 72 (35.3) | 54 (37.5) | 63 (45.3) | <.0001 |
| Gown | 249 (61.5) | 107 (52.5) | 63 (43.8) | 69 (49.6) | .001 |
| Full-face respirator | 61 (15.1) | 11 (5.4) | 12 (8.3) | 10 (7.2) | .0007 |
| Adequate ventilators | 180 (47.2) | 61 (31.3) | 53 (39.6) | 46 (37.7) | .0024 |
Abbreviation: PPE, personal protective equipment.
Figure 2.
COVID-19 Preparedness by Practice Setting. (a) Bar graph comparing access to COVID-19 testing stratified by practice setting. (b) Bar graph comparing access to adequate personal protective equipment (PPE) stratified by practice setting.
Table 3.
Multivariate Analysis.a
| Academic vs Private (ref), OR (95% CI) [P] | Academic vs Privademic (ref), OR (95% CI) [P] | Academic vs Public (ref), OR (95% CI) [P] | Private vs Privademic (ref), OR (95% CI) [P] | Private vs Public (ref), OR (95% CI) [P] | Privademic vs Public (ref), OR (95% CI) [P] | |
|---|---|---|---|---|---|---|
| Hospital formal guidelines | 1.56 (0.98, 2.5) [.06] | 1.11 (0.72, 1.72) [.61] | 1.54 (0.93, 2.5) [.095] | 0.71 (0.42, 1.17) [.19] | 0.97 (0.55, 1.72) [.93] | 1.37 (0.79, 2.38) [.26] |
| Adequate PPE | 1.33 (0.85, 2.08) [.21] | 1.72 (1.16, 2.56) [.0068] | 1.56 (0.97, 2.5) [.065] | 1.29 (0.81, 2.08) [.29] | 1.16 (0.68, 2.0) [.58] | 0.90 (0.54, 1.52) [.69] |
| Forms of PPE provided | ||||||
| N-95 mask | 1.94 (1.24, 3.06) [.004] | 1.43 (0.96, 2.13) [.075] | 1.2 (0.77, 1.87) [.42] | 0.74 (0.45, 1.2) [.22] | 0.62 (0.36, 1.05) [.076] | 0.84 (0.51, 1.37) [.48] |
| Surgical mask | 1.40 (0.8, 2.43) [.24] | 1.00 (0.59, 1.69) [.99] | 1.71 (0.98, 2.99) [.06] | 0.71 (0.39, 1.29) [.24] | 1.22 (0.65, 2.92) [.53] | 1.71 (0.93, 3.17) [.086] |
| Face shield | 2.05 (1.31, 3.19) [.0016] | 1.90 (1.28, 2.83) [.0016] | 1.36 (0.87, 2.12) [.18] | 0.92 (0.57, 1.52) [.77] | 0.66 (0.87, 2.12) [.18] | 0.72 (0.43, 1.18) [.19] |
| Gown | 2.33 (1.5, 3.62) [.0002] | 1.38 (0.93, 2.04) [.11] | 1.8 (1.15, 2.82) [.011] | 0.59 (0.37, 0.95) [.03] | 0.77 (0.46, 1.31) [.34] | 1.31 (0.8, 2.14) [.29] |
| Full-face respirator | 2.29 (1.11, 4.7) [.024] | 2.62 (1.28, 5.37) [.0086] | 2.14 (0.99, 4.63) [.054] | 1.14 (0.47, 2.78) [.77] | 0.93 (0.37, 2.35) [.88] | 0.82 (0.32, 2.09) [.67] |
| Adequate ventilators | 1.20 (0.76, 1.89) [.43] | 1.59 (1.04, 2.38) [.031] | 1.47 (0.9, 2.38) [.12] | 1.31 (0.79, 2.17) [.28] | 1.22 (0.69, 2.17) [.49] | 0.92 (0.54, 1.61) [.79] |
| Very worried about outbreak (score of 4 or 5) | 0.84 (0.54, 1.32) [.46] | 0.71 (0.47, 1.07) [.1] | 0.87 (0.54, 1.41) [.58] | 0.84 (0.51, 1.38) [.5] | 1.03 (0.59, 1.81) [.9] | 1.23 (0.72, 2.08) [.45] |
| Greatest stressors | ||||||
| Hospital ability to treat COVID-19 positive patients | 2.34 (1.46, 3.73) [.004] | 1.55 (1.05, 2.29) [.029] | 0.62 (0.38, 1.02) [.058] | 0.66 (0.4, 1.1) [.11] | 0.41 (0.24, 0.71) [.0014] | 0.61 (0.38, 1.02) [.058] |
| Economic issues | 0.49 (0.32, 0.75) [.0011] | 0.56 (0.29, 0.81) [.0025] | 1.22 (0.77, 1.91) [.4] | 1.13 (0.71, 1.78) [.6] | 2.47 (1.47, 4.16) [.0007] | 2.19 (1.34, 3.57) [.0018] |
| Hospital restrictions | ||||||
| Limitations on domestic travel | 3.1 (2, 4.81) [<.0001] | 1.9 (1.29, 2.8) [.0011] | 1.99 (1.28, 3.1) [.0021] | 0.61 (0.38, 0.98) [.041] | 0.64 (0.38, 1.08) [.095] | 1.05 (0.65, 1.7) [.85] |
| Cancellation of all education activities | 2.36 (1.45, 3.84) [.0005] | 1.13 (0.7, 1.82) [.62] | 2.53 (1.52, 4.24) [.0004] | 0.48 (0.28, 0.81) [.0061] | 1.07 (0.61, 1.88) [.8] | 2.25 (1.28, 3.94) [.0047] |
| Nonessential staff to work from home | 2.31 (1.47, 3.6) [.0002] | 1.08 (0.48, 1.38) [.45] | 1.88 (1.19, 2.97) [.0067] | 0.47 (0.29, 0.76) [.002] | 0.82 (0.48, 1.38) [.45] | 1.74 (1.06, 2.87) [.03] |
| Performing elective spine surgeries | 2.32 (1.17, 4.6) [.016] | 1.75 (0.99, 3.07) [.053] | 1.12 (0.59, 2.14) [.73] | 0.75 (0.22, 0.86) [.47] | 0.48 (0.21, 1.11) [.087] | 0.64 (0.31, 1.35) [.24] |
| Performing essential/emergent spine cases | 3.06 (1.58, 5.94) [.0009] | 1.72 (0.9, 3.28) [.1] | 3.19 (1.6, 6.36) [.001] | 0.56 (.29, 1.09) [.087] | 1.04 (0.51, 2.12) [.91] | 1.85 (0.92, 3.73) [.085] |
| Impact on patient care in 1 year | ||||||
| No change | 1.22 (0.67, 2.24) [.52] | 1.41 (0.8, 2.49) [.24] | 0.68 (0.39, 1.18) [.17] | 1.15 (0.58, 2.31) [.69] | 0.56 (0.28, 1.1) [.092] | 0.48 (0.25, 0.93) [.031] |
| Heightened awareness of hygiene | 1.09 (0.71, 1.67) [.68] | 0.67 (0.46, 0.99) [.042] | 1.46 (0.94, 2.28) [.094] | 0.62 (0.39, 0.98) [.04] | 1.34 (0.79, 2.25) [.79] | 2.17 (1.33, 2.54) [.0019] |
| Will increase use of PPE | 1.27 (0.81, 1.98) [.3] | 0.69 (0.47, 1) [.055] | 1.11 (0.71, 1.74) [.64] | 0.54 (0.34, 0.87) [.012] | 0.88 (0.51, 1.5) [.63] | 1.61 (0.99, 2.62) [.054] |
Abbreviation: PPE, personal protective equipment.
a Nominal multivariate logistic regression controlling for gender (P = .0013), home city population (P < .0001), region (P < .0001), fellowship training (P = .0039), and practice breakdown (ie, research, clinical, and teaching) (P = .0003, P = .011, and P = .0009, respectively). Odds ratios (ORs) presented as first group in reference to second group (ie, academic surgeons had 1.56 times likelihood of reporting formal hospital guidelines compared with private surgeons).
There were no differences in the rate of COVID-19 diagnosis (P = .53) or quarantine (P = .16) among surgeons by practice setting. Surgeons in various practice settings did not report a significant difference in the rate of performing medical duties outside their normal scope (P = .19). There was significant variation in the presence of formal hospital guidelines for pandemic response on univariate analysis (P = .0048) with surgeons at academic institutions reporting the presence of hospital guidelines at a greater rate than private practice surgeons (227/405; 66.8% vs 60/144; 50.9%, P = .0021).
Respondents overall reported a moderate to high level of concern regarding the COVID-19 outbreak, with a mean score of 3.7 ± 1.2 on a scale of 1 to 5. On univariate analysis, there was significant variation between respondents from various practice settings (P = .019) (Table 4). Respondents from privademic practices reported higher mean worry compared to those at academic institutions (3.9 ± 1.1 vs 3.6 ± 1.2, P = .013) and surgeons from academic institutions reported lower overall mean worry compared with all other respondents (3.6 ± 1.2 vs 3.83 ± 1.1, P = .0025). Multivariate analysis did not reveal practice setting to be independently associated with mean worry (P > .05) (Table 3).
Table 4.
COVID-19 Impact and Response by Practice Setting.
| Academic, n (%) | Privademic, n (%) | Private, n (%) | Public, n (%) | P | |
|---|---|---|---|---|---|
| Diagnosed with COVID-19 | 4 (1) | 3 (1.5) | 0 (0) | 2 (1.6) | .53 |
| Personally quarantined | 81 (21.3) | 53 (26.8) | 35 (25.7) | 21 (17.1) | .16 |
| Performed medical duties outside of normal scope | 92 (24.9) | 39 (20.9) | 21 (16.5) | 30 (25.9) | .19 |
| Mean worry (1 = not worried at all to 5 = very worried), mean ± SD | 3.6 ± 1.2 | 3.9 ± 1.1 | 3.8 ± 1.1 | 3.8 ± 1.1 | .019 |
| 3 greatest stressors | |||||
| Personal health | 161 (39.8) | 86 (42.2) | 52 (36.1) | 57 (41) | .71 |
| Family health | 287 (70.9) | 153 (75) | 101 (70.1) | 95 (68.4) | .55 |
| Community health | 160 (39.5) | 97 (47.6) | 61 (42.4) | 51 (36.7) | .17 |
| Hospital ability to treat COVID-19 positive patients | 170 (42) | 73 (5.8) | 37 (25.7) | 70 (50.4) | .0001 |
| Timeline to resume regular clinic work | 170 (42) | 92 (45.1) | 66 (45.8) | 49 (35.3) | .24 |
| Government/leadership | 75 (18.5) | 28 (13.7) | 26 (18.1) | 25 (18) | .48 |
| Return to nonessential activities | 59 (14.6) | 19 (9.3) | 21 (14.6) | 16 (11.5) | .27 |
| Economic issues | 148 (36.5) | 106 (52) | 82 (56.9) | 47 (33.8) | <.0001 |
| Hospital restrictions | |||||
| Quarantine on return from international travel | 244 (60.3) | 112 (54.9) | 71 (49.3) | 77 (55.4) | .13 |
| Limitations on domestic travel | 260 (64.2) | 98 (48) | 56 (38.9) | 66 (47.5) | <.0001 |
| Cancellation of all education activities | 328 (81) | 162 (79.4) | 97 (67.4) | 98 (70.5) | .0018 |
| Nonessential staff to work from home | 270 (66.7) | 132 (64.7) | 74 (51.4) | 78 (56.1) | .004 |
| Cancellation of hospital meetings | 311 (76.8) | 159 (77.9) | 101 (70.1) | 99 (71.2) | .21 |
| Cancellation of elective surgeries | 320 (79) | 170 (83.3) | 110 (76.4) | 110 (79.1) | .43 |
| Satisfaction with hospital response | .0046 | ||||
| Appears in disarray/disorganized | 241 (67.7) | 94 (51.7) | 79 (64.8) | 61 (53) | |
| Taken some action but not enough | 9 (2.5) | 2 (1.1) | 4 (3.3) | 2 (1.7) | |
| Acceptable/appropriate | 24 (6.7) | 20 (11) | 8 (6.6) | 16 (13.9) | |
| Actions are excessive and unnecessary | 82 (23) | 66 (36.3) | 31 (25.4) | 36 (31.3) |
Economic issues (P < .0001) and ability to treat COVID-19 patients (P < .0001) as sources of stress differed by practice setting (Table 4). On multivariate analysis, respondents from private practice settings were 2.04 times more likely to report economic issues as a source of stress compared with academic surgeons (OR 2.04, 95% CI 1.33-3.13, P = .0011) and 2.47 times as likely compared with surgeons at public hospitals (OR 2.47, 95% CI 1.47-4.16). Surgeons at private hospitals were independently less likely to report concern regarding their hospital’s ability to treat COVID-19 patients compared with the public hospitals (OR 0.41, 95% CI 0.24-0.71, P = .0014) (Table 3).
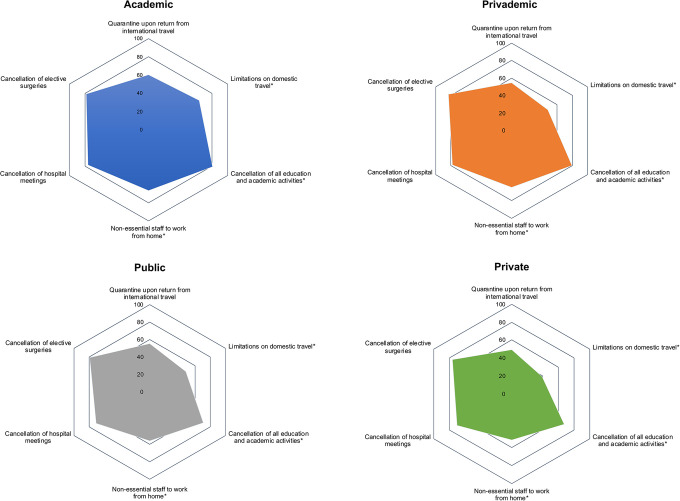
Respondents reported differences in their hospital-mandated limitations on travels (P < .0001), cancellation of educational activities (P = .0018), and work-from-home orders (P = .004) (Table 4). There was no variation in the cancellation of elective surgeries by practice setting (P = .43) (Figure 3). Overall, 59.2% of respondents reported that their hospital’s response to COVID-19 was “acceptable.” This had significant variation by practice setting with 67.7% (241/405) of respondents in academic institutions reporting an “acceptable” response compared with 55.8% (234/419) of respondents from other practice settings (P = .0044).
Figure 3.
Radar chart depictions of current COVID-19 hospital policies by practice setting. Six-sided (hexagon) radar charts visually depicting cumulative percentage of responses verifying the enactment of a given COVID-19 hospital policy at the time of survey distribution. Queried policies are listed at the vertex of a given figure, whereby points falling on a vertex of the innermost pentagon correspond to a cumulative total of 0% of survey responses received. Each subsequent pentagon corresponds to a 20% increase in responses for a given category. *Indicates difference significant at the 95% confidence level (P < .05).
Respondents endorsed various economic impacts by practice setting (Table 5). Surgeons reported variations in performance of elective (P = .0011) and emergent spine surgeries (P = .0001) by practice setting (Figure 4a). On univariate analysis, private and privademic surgeons were performing elective spine surgeries at a lower rate compared with surgeons in academic or public hospitals (39/348; 11.2% vs 109/544; 20.0%, P = .006). On multivariate analysis, surgeons in academic practice were 2.32 times more likely to report performing elective surgeries (OR 2.32, 95% CI 1.17-4.6, P = .016) and 3.06 times more likely to report performing emergent surgeries (OR 3.06, 95% CI 1.58-5.94, P = .0009) compared with private practice surgeons (Table 3). Surgeons reported variation in the decrease in case volume by practice setting (P = .0006). Private and privademic surgeons reported a >75% decrease in case volume at a higher rate compared with academic or public surgeons (233/348; 66.9% vs 304/544; 55.9%, P = .0010).
Table 5.
Economic Impact of COVID-19 by Practice Setting.
| Academic, n (%) | Privademic, n (%) | Private, n (%) | Public, n (%) | P | |
|---|---|---|---|---|---|
| Performing elective spine cases | 89 (24.2) | 25 (13.2) | 14 (11.2) | 20 (17) | .0011 |
| Performing essential/emergent spine cases | 342 (92.9) | 162 (85.7) | 101 (80.8) | 94 (80.3) | .0001 |
| Decrease in case volume | .0095 | ||||
| ≤25% | 40 (10.8) | 10 (5.3) | 12 (9.6) | 10 (8.6) | |
| 26%-50% | 40 (10.8) | 12 (6.3) | 8 (6.4) | 18 (15.5) | |
| 51%-75% | 65 (17.6) | 32 (16.8) | 8 (6.4) | 18 (15.5) | |
| >75% | 224 (60.7) | 136 (71.6) | 97 (77.6) | 80 (69) | |
| Time spent performing clinical duties | .31 | ||||
| Increased | 19 (5.1) | 14 (7.4) | 6 (4.8) | 7 (6) | |
| Stayed the same | 44 (11.9) | 15 (18.1) | 8 (6.4) | 16 (13.8) | |
| Decreased | 307 (83) | 161 (84.7) | 111 (88.8) | 93 (80.2) | |
| Impact on income | <.0001 | ||||
| Planned reduction—on salary | 63 (18.2) | 39 (22) | 18 (14.9) | 18 (15.7) | |
| No impact—on salary | 151 (43.6) | 32 (18.1) | 15 (12.4) | 45 (39.1) | |
| Planned reduction—productivity-based income | 30 (8.7) | 10 (5.7) | 11 (9.1) | 13 (11.3) | |
| No impact—productivity-based income | 5 (1.5) | 1 (0.6) | 1 (0.8) | 0 (0) | |
| Losing income | 97 (28) | 95 (53.7) | 76 (62.8) | 39 (33.9) | |
| Impact on personal revenue | <.0001 | ||||
| ≤25% | 141 (41) | 24 (13.6) | 12 (9.8) | 42 (37.2) | |
| 26%-50% | 108 (31.4) | 53 (29.9) | 28 (23) | 37 (32.7) | |
| 51%-75% | 61 (17.7) | 39 (22) | 25 (20.5) | 17 (15) | |
| >75% | 34 (9.9) | 61 (34.5) | 57 (46.7) | 17 (15) | |
| Impact on hospital revenue | <.0001 | ||||
| ≤25% | 93 (26.9) | 29 (16.4) | 9 (7.6) | 38 (33.6) | |
| 26%-50% | 96 (27.8) | 53 (29.9) | 19 (16) | 31 (27.4) | |
| 51%-75% | 100 (28.9) | 39 (22) | 40 (33.6) | 26 (23) | |
| >75% | 57 (16.5) | 56 (31.6) | 51 (42.9) | 18 (15.9) |
Figure 4.
COVID-19 economic impact by practice setting. (a) Bar graph comparing performance of elective and emergent spine case during the COVID-19 pandemic stratified by practice setting. (b) Bar graph comparing self-reported impact on surgeon income stratified by practice setting.
Impact on income (P < .0001), personal revenue (P < .0001), and hospital revenue (P < .0001) also varied significantly between practice settings (Table 5). In total, 62.8% (76/144) of private practice surgeons and 53.7% (95/204) of privademic surgeons reported losing income due to COVID-19 (Figure 4b). Surgeons from private or privademic practice settings were 2.9 times more likely to report losing income compared with surgeons at academic or public institutions (OR 2.9, 95% CI 2.18-3.83, P < .0001). On multivariate analysis, practice setting was independently associated with impact on income (LR 51.3, P < .0001), loss of personal revenue (LR 83.3, P < .0001), and impact on hospital revenue (LR 43.8, P < .0001). The long-term effects of COVID-19 also differed by practice setting (Table 6).
Table 6.
Long-Term Impacts of COVID-19 by Practice Setting.
| Academic, n (%) | Privademic, n (%) | Private, n (%) | Public, n (%) | P | |
|---|---|---|---|---|---|
| Impact on patient care in 1 year | |||||
| No change | 60 (14.8) | 21 (10.3) | 20 (13.9) | 31 (22.3) | .022 |
| Heightened awareness of hygiene | 203 (50.1) | 116 (58.9) | 65 (45.1) | 51 (38.7) | .0023 |
| Will increase use of PPE | 154 (38) | 97 (47.6) | 45 (31.3) | 48 (34.5) | .011 |
| Ask patient to reschedule if they feel sick | 128 (31.6) | 67 (32.8) | 45 (31.3) | 45 (33.4) | .99 |
| Pursue increased nonoperative measures prior to surgery | 68 (16.8) | 40 (19.6) | 18 (12.5) | 24 (17.3) | 0.38 |
| Growth in digital options for communication | 153 (37.8) | 76 (37.3) | 39 (27.1) | 45 (32.4) | .1 |
| Likelihood to attend conference in 1 year | .33 | ||||
| Likely | 215 (63.2) | 119 (68) | 85 (71.4) | 76 (67.9) | |
| Unsure | 101 (29.7) | 46 (26.3) | 26 (21.9) | 24 (21.4) | |
| Not likely | 24 (7.1) | 10 (5.7) | 8 (6.7) | 12 (10.7) | |
| Need for formal guidelines | 320 (97.9) | 168 (100) | 114 (99) | 106 (100) | .1 |
Abbreviation: PPE, personal protective equipment.
Discussion
COVID-19 is a defining global health crisis for the current generation of spine surgeons. In a cohort of 900 spine surgeons around the globe, Louie et al 13 highlighted that COVID-19 had a sizeable impact on their patient care, practice, and personal lives; however, the impact was nuanced. Understanding the variations in COVID-19 preparation, response, and economic impact will help mitigate the effect of future crises on the spine community.
The COVID-19 pandemic comes amid a period of change in healthcare economics.18,19 Over the past decade, the United States has seen a precipitous decline in physician private practice, likely driven by health care policy that operates on the theory that large health care organizations are more data driven, more efficient, and more effective than their small, private-practice counterparts. 20 Our study presents critical data on the variation in preparation, response, and financial impact of COVID-19 on spine surgeons around the world primarily based on the practice setting.
Preparedness by Practice Type
The World Health Organization (WHO) and the global health community made pandemic preparedness one of their main missions,27,28 and research on pandemic preparedness is abundant.9,29-31 However, it remains unknown how surgeons in various practice settings interpret these guidelines and prepare for global health crises.
Limitations in access and availability of testing have been cited as a major shortcoming in the media.32,33 Our results indicate that access to testing is no longer a major limitation for surgeons, with over 82% of surgeons reporting access to a COVID-19 test. Furthermore, there were no differences in testing availability reported by surgeons at academic, privademic, private, or public institutions. While the overall availability of testing for surgeons is encouraging, prior studies reported that health care workers have accounted for anywhere between 10% and 30% of total positive COVID-19 tests in various regions.34,35 Surgeons in all practice settings need to improve testing availability and guarantee testing is accessible for their staff and patients before a return to normal operations.
Unsurprisingly, practice setting was independently associated with the availability of personal protective equipment. Across all practice settings, access to personal protective equipment was concerningly low, at 49%. The media in the United States and across the world has highlighted the critical lack of PPE that frontline health care workers faced in the early days of the COVID-19 outbreak.7,8,36-38 Our results indicate that public and privademic hospitals face worse PPE shortages than academic medical centers. The issues with PPE availability for public hospitals are likely driven by public safety-net hospitals in the United States, where resource and funding shortages were well established before COVID-19.39,40 Further research is needed to elucidate the reason for PPE shortages among privademic practices.
Along with PPE shortages, physicians faced the possibility of difficult decisions surrounding allocation of ventilators,41,42 and operating room anesthesia machines were reallocated to intensive care units, closing operating rooms for surgeon use. 43 A disturbingly low 41% of respondents reported adequate ventilator supplies during the COVID-19 pandemic. While there was a significant difference in ventilator availability on univariate analysis, this was likely confounded by regional differences, as only privademic practice setting was independently associated with ventilator availability on multivariate analysis. Once again, further research into the shortcomings of privademic practice preparedness is needed.
Despite numerous health departments across of the world recommending formal institutional guidelines for pandemic preparedness,44-46 an unexpectedly low 60% of respondents reported guidelines in place at their institutions prior to COVID-19. We postulate that countries with prior infectious disease epidemics likely had guidelines in place or were quick to adopt formal guidelines while countries with little infectious disease experience were slow to respond. Also, surgeons in academic institutions reported formal guidelines at a greater rate than private practice surgeons; however, practice setting alone was not associated with the presence of guidelines. Future guidelines for crisis preparedness need to be applicable and adaptable to all practice settings to maximize adoption.
COVID-19 Response by Practice Type
As COVID-19 continued to spread despite numerous interventions, there were a variety of responses to the growing threat. Many of the variations in response have been attributed to geopolitical differences between nations around the world.47-51 However, our results indicate that independent of global region, spine surgeons in different practice types experienced distinctive responses to COVID-19.
Surgeons in practice settings more reliant on clinical productivity for income (eg, private practice, privademic practice) were more worried about the impact of COVID-19. This likely stemmed from private and privademic surgeons increased stress around economic issues. The high level of stress among surgeons at public hospitals likely stems from their concerns about resource availability and ability to adequately care for COVID-19 patients.
Based on our survey results, academic institutions appeared to respond more robustly to COVID-19 compared with private, privademic, and public institutions. Academic respondents reported more domestic travels bans, cancellation of educational activities, and more work-from-home orders compared with surgeons at private, privademic, and public institutions. Overall, a disappointing 61.4% of respondents rated their hospital responses as “acceptable,” while 27.7% rate their hospital’s action as “not enough.” Surgeons in academic institutions were satisfied at a higher rate compared to other practice settings.
These large academic institutions tend to have the infrastructure and human resources in place to respond to new guidelines. Smaller private practices and privademic institutions operate with less ancillary staff and possibly lack the resources to develop comprehensive response plans that can be quickly disseminated to their staff. This presents an opportunity for leadership in the spine community to develop crisis guidelines that are easily adaptable to all practice settings. A comprehensive preparedness and response plan could be developed that applies to all practice settings with more individualized plans then developed for each practice setting to specifically address unique concerns by practice type. Given the enormous public health impact of COVID-19, a multidisciplinary effort is needed to develop these guidelines to minimize the impact of future outbreaks.
Economic Impact by Practice Type
COVID-19 occurred during a period of major changes in healthcare economics. Alongside the swift shift in practice types, is the transition away from fee-for-service reimbursement toward alternative payment models.21,22 These models were designed to shift financial risk from insurers to providers in an attempt to improve quality and outcomes.52,53 However, these models still require clinical productivity to generate revenue.
Prior research across numerous specialties has compared the compensation of surgeons in academic practices versus private practices.19,54,55 Private practice surgeons tend to be compensated based on clinical productivity, and tend to have higher overall income.19,54 Academic surgeons tend to have inputs into their income, including base salary, clinical productivity, and academic productivity. 56 Surgeons at public or government-run hospitals tend to be salaried employees. 57 Therefore, providers in various practice settings have differing incentives on clinical productivity.
Despite the guidance issued by professional societies and spine leadership, our survey indicates that a small percent of surgeons continued to perform elective spine surgeries throughout the pandemic.10,16,58 However, contrary to what we predicted, private and privademic surgeons performed elective spine surgeries at a lower rate compared with surgeons in academic or public hospitals. Thus, despite increased monetary incentive to continue elective surgeries, private and privademic surgeons heeded the governmental recommendations and stopped operating during the pandemic. We postulate that perhaps the greater resource availability and multidisciplinary approach of academic and public hospitals allowed them to continue some elective cases at a greater rate. Because of the fact that private practice models exist only in some countries, it is also conceivable that the result is confounded by unequal distribution of practice types around the world.
With the drastic reduction in elective case volume occurring during COVID-19, surgeons who rely on clinical productivity as a major source of revenue are reporting a decrease in revenue and income. Our survey further outlines that surgeons in private and privademic practices are reporting that their hospitals are experiencing greater financial hardship compared to academic and public hospitals. The American Medical Association issued guidance on how private medical practices could adapt to financial and logistical stresses of this global pandemic. 23 However, surgeons may be even more affected. The American Academy of Orthopaedic Surgeons recently released guidance to support private practice surgeons during COVID-19 and is lobbying congress for specific government programs to assist private practice surgeons. 59 While our survey results echo the sentiment that private and privademic surgeons are at risk for the greatest financial impact, the Department of Health and Human Services is obligated to assist all spine providers in surviving this pandemic so we can continue to ensure care is accessible to all patients.
Long-Term Impacts
While the COVID-19 pandemic is ongoing, we must start looking toward the future. Spine practices must adapt to the post-COVID-19 era in order to keep patients and providers safe while ensuring the survival of all practice types. Our respondents identified heightened awareness of hygiene, increased PPE use, and a rise in digital communication options as changes to patient care over the next year. However, many questions remain. Over the past several years, private equity firms have started to see private surgical practices as potential investment opportunities. 60 These firms specialize in improving the financial performance of struggling or unprofitable companies, and selling them for a profit. This raises concern that practices facing financial difficulty in the post-COVID-19 era will be bought up by private equity firms, accelerating the transition away from surgeon-controlled practices.
We believe spine surgeons and spine societies must lead our healthcare system into the post-COVID-19 era. We must ensure that governments do not use COVID-19 as an opportunity to transition away from private or privademic practice. COVID-19 highlighted the need for future formal guidelines to consider the stresses that pandemics cause for different practice types.
Limitations
As with many survey-based studies, there are clear limitations. The survey distribution was limited to the current AO Spine surgeon members network. The survey was sent out to 3,805 spine surgeons worldwide; however, only 902 surgeons responded (23.7%). This likely introduces a response bias as subjects with strong opinions are more inclined to respond. Previous studies have described that low response rate is a risk factor for low validity, but does not dictate low validity. 61 Response rates are important to assess, but should not be considered a proxy for study validity.
Our study relied on respondents’ self-classification of practice type. Given that our study included international respondents, there may be different definitions of private, privademic, academic, and public around the world. Furthermore, we attempted to control for differences in the distribution of practice types throughout the world by including geographic region in our multivariate model, however, we lacked sufficient power to control for individual countries. Given the limit of survey length due to fatigue, we were not able to explore all the possible domains related to COVID-19.
Finally, our targeted demographic was spine surgeons that are members associated with AO Spine. This is one group of subspecialty surgeons and the results may not be generalizable to other medical specialties. Despite these limitations, this survey remains the largest, international effort to assess multiple domains of the impact of COVID-19 on spine surgeons.
Conclusions
The COVID-19 pandemic has impacted spine surgeons across the world. As health systems and government agencies look to generate policies for mitigating current and future outbreaks, understanding the differential impact on various practice settings is critical. The current study indicates that surgeons entered COVID-19 with varying levels of preparedness based on practice setting. Furthermore, apart from the obvious impact on elective case volume, COVID-19 has triggered a massive decrease in overall clinical productivity, revenue, and income. This has caused disproportionate financial stress in private and privademic settings. As we move through this COVID-19 crisis and into the postpandemic era, we are hopeful for a return to some level of normalcy. Spine surgeons and our professional societies must urge the governments around the world to assist all spine providers in surviving this pandemic so we can continue to ensure care is accessible to all patients.
Acknowledgments
The authors would especially like to thank Kaija Kurki-Suonio and Fernando Kijel from AO Spine (Davos, Switzerland) for their assistance with circulating the survey to AO Spine members.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Joseph A. Weiner, MD  https://orcid.org/0000-0001-7566-7764
https://orcid.org/0000-0001-7566-7764
Philip K. Louie, MD  https://orcid.org/0000-0002-4787-1538
https://orcid.org/0000-0002-4787-1538
Michael H. McCarthy, MD, MPH  https://orcid.org/0000-0003-2766-6366
https://orcid.org/0000-0003-2766-6366
Jason P. Y. Cheung, MBBS, MS, MD  https://orcid.org/0000-0002-7052-0875
https://orcid.org/0000-0002-7052-0875
Mohammad El-Sharkawi, MD  https://orcid.org/0000-0001-6177-7145
https://orcid.org/0000-0001-6177-7145
Daniel M. Sciubba, MD  https://orcid.org/0000-0001-7604-434X
https://orcid.org/0000-0001-7604-434X
Dino Samartzis, DSc  https://orcid.org/0000-0002-7473-1311
https://orcid.org/0000-0002-7473-1311
References
- 1.Munster VJ, Koopmans M, van Doremalen N, et al. A novel coronavirus emerging in China—key questions for impact assessment. N Engl J Med. 2020;382:692–694. doi:10.1056/NEJMp2000929 [DOI] [PubMed] [Google Scholar]
- 2.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi:10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gates B. Responding to Covid-19—a once-in-a-century pandemic? N Engl J Med. 2020;382:1677–1679. doi:10.1056/NEJMp2003762 [DOI] [PubMed] [Google Scholar]
- 4.Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382:2368–2371. doi:10.1056/nejmms2009984 [DOI] [PubMed] [Google Scholar]
- 5.Moghadas SM, Shoukat A, Fitzpatrick MC, et al. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci U S A. 2020;117:9122–9126. doi:10.1073/pnas.2004064117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weissman GE, Crane-Droesch A, Chivers C, et al. Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann Intern Med. 2020;173:21–28. doi:10.7326/M20-1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Sullivan ED. PPE guidance for covid-19: be honest about resource shortages. BMJ. 2020;369:m1507. doi:10.1136/bmj.m1507 [DOI] [PubMed] [Google Scholar]
- 8.Rimmer A. Covid-19: third of surgeons do not have adequate PPE, royal college warns. BMJ. 2020;369:m1492. doi:10.1136/bmj.m1492 [DOI] [PubMed] [Google Scholar]
- 9.Kandel N, Chungong S, Omaar A, et al. Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. Lancet. 2020;395:1047–1053. doi:10.1016/S0140-6736(20)30553-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donnally CJ, 3rd, Shenoy K, Vaccaro AR, et al. Triaging spine surgery in the COVID-19 era. Clin Spine Surg. 2020;33:129–130. doi:10.1097/bsd.0000000000000988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.GBD 2013 DALYs and HALE Collaborators; Murray CJL, Barber RM, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–2191. doi:10.1016/S0140-6736(15)61340-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi:10.1016/S0140-6736(15)60692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Louie PK, Harada GK, McCarthy MH, et al. The impact of COVID-19 pandemic on spine surgeons worldwide. Glob Spine J. 2020;10:534–552. doi:10.1177/2192568220925783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenland JR, Michelow MD, Wang L, London MJ. COVID-19 infection: implications for perioperative and critical care physicians. Anesthesiology. 2020;132:1346–1361. doi:10.1097/aln.0000000000003303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Indini A, Aschele C, Cavanna L, et al. Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: a nationwide Italian survey. Eur J Cancer. 2020;132:17–23. doi:10.1016/j.ejca.2020.03.024 [DOI] [PubMed] [Google Scholar]
- 16.Wright RW, Armstrong AD, Azar FM, et al. The American Board of Orthopaedic Surgery response to COVID-19. J Am Acad Orthop Surg. 2020;28:e465–e468. doi:10.5435/JAAOS-D-20-00392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi:10.1016/j.amjsurg.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kazberouk A, Mcguire K, Landon BE. A survey of innovative reimbursement models in spine care. Spine (Phila Pa 1976). 2016;41:344–352. doi:10.1097/BRS.0000000000001212 [DOI] [PubMed] [Google Scholar]
- 19.Baimas-George M, Fleischer B, Korndorffer JR, Jr, Slakey D, DuCoin C. The economics of private practice versus academia in surgery. J Surg Educ. 2018;75:1276–1280. doi:10.1016/j.jsurg.2018.03.006 [DOI] [PubMed] [Google Scholar]
- 20.Capital Flows. Why private practice is dying. Accessed April 25, 2020. https://www.forbes.com/sites/realspin/2016/09/07/why-private-practice-is-dying/#1303d76b27c8
- 21.Dietz N, Sharma M, Alhourani A, et al. Bundled payment models in spine surgery: current challenges and opportunities, a systematic review. World Neurosurg. 2019;123:177–183. doi:10.1016/j.wneu.2018.12.001 [DOI] [PubMed] [Google Scholar]
- 22.Ugiliweneza B, Kong M, Nosova K, et al. Spinal surgery: variations in health care costs and implications for episode-based bundled payments. Spine (Phila Pa 1976). 2014;39:1235–1242. doi:10.1097/BRS.0000000000000378 [DOI] [PubMed] [Google Scholar]
- 23.American Medical Association. AMA announces private practice resources during COVID-19 pandemic. Published March 27, 2020. Accessed April 25, 2020. https://www.ama-assn.org/press-center/press-releases/ama-announces-private-practice-resources-during-covid-19-pandemic
- 24.Hohmann E, Brand JC, Rossi MJ, Lubowitz JH. Expert opinion is necessary: Delphi panel methodology facilitates a scientific approach to consensus. Arthrosc J Arthrosc Relat Surg. 2018;34:349–351. doi:10.1016/j.arthro.2017.11.022 [DOI] [PubMed] [Google Scholar]
- 25.Linstone HA, Turoff M, eds. The Delphi Method Techniques and Applications. 1st ed. Addison-Wesley; 2002:4–6. [Google Scholar]
- 26.Shi WJ, Murphy HA, Sebastian AS, Schroeder GD, West M, Vaccaro AR. Privademics: the best of both worlds. Neurosurgery. 2017;64(CN_suppl_1):83–86. doi:10.1093/neuros/nyx291 [DOI] [PubMed] [Google Scholar]
- 27.Harvard Global Health Institute. Global monitoring of disease outbreak preparedness: preventing the next pandemic. Accessed July 28, 2020. https://globalhealth.harvard.edu/wp-content/uploads/2020/07/GlobalMonitoring_summary_report.pdf
- 28.Global Preparedness Monitoring Board. A world at risk annual report on global preparedness for health emergencies. Sales Mark Manag. 2019;151(9 pt 1):44. doi:10.2307/40153772 [Google Scholar]
- 29.Gates B. Innovation for pandemics. N Engl J Med. 2018;378:2057–2060. doi:10.1056/NEJMp1806283 [DOI] [PubMed] [Google Scholar]
- 30.Moon S, Sridhar D, Pate MA, et al. Will Ebola change the game? Ten essential reforms before the next pandemic. the report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Lancet. 2015;386(10009):2204–2221. doi:10.1016/S0140-6736(15)00946-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fineberg H V. Global health: pandemic preparedness and response—lessons from the H1N1 influenza of 2009. N Engl J Med. 2014;370:1335–1342. doi:10.1056/NEJMra1208802 [DOI] [PubMed] [Google Scholar]
- 32.Madrigal AC, Meyer R. Private labs are Fueling a new coronavirus testing crisis. Accessed April 25, 2020. https://www.theatlantic.com/health/archive/2020/03/next-covid-19-testing-crisis/609193/
- 33.Aubrey A. Which states are doing enough testing? This benchmark helps settle the debate. Accessed April 25, 2020. https://www.npr.org/sections/health-shots/2020/04/22/840526338/is-the-u-s-testing-enough-for-covid-19-as-debate-rages-on-heres-how-to-know
- 34. The Lancet . COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi:10.1016/S0140-6736(20)30644-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stobbe M.Health care workers are 10%-20% of US coronavirus cases. Accessed July 28, 2020. https://apnews.com/daeaccea8ed06a54df4ba39d41776bc2
- 36.World Health Organization. Shortage of personal protective equipment endangering health workers worldwide. Accessed April 28, 2020. https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide
- 37.Schlanger Z. Begging for thermometers, body bags, and gowns: US health care workers are dangerously ill-equipped to fight COVID-19. Accessed April 28, 2020. https://time.com/5823983/coronavirus-ppe-shortage/
- 38.Connolly K. German doctors pose naked in protest at PPE shortages. Accessed April 28, 2020. https://www.theguardian.com/world/2020/apr/27/german-doctors-pose-naked-in-protest-at-ppe-shortages
- 39.Felland L, Cunningham P, Doubleday A, Warren C. Effects of the Affordable Care Act on safety net hospitals. Accessed July 28, 2020. https://www.mathematica.org/our-publications-and-findings/publications/effects-of-the-affordable-care-act-on-safety-net-hospitals
- 40.Institute of Medicine (US) Committee on the Changing Market, Managed Care, and the Future Viability of Safety Net Providers; Lewin ME, Altman S, eds. The core safety net and the safety net system. America’s Health Care Safety Net: Intact but Endangered. National Academies Press; 2000. Accessed July 28, 2020. https://www.ncbi.nlm.nih.gov/books/NBK224521/
- 41.Vergano M, Bertolini G, Giannini A, et al. Clinical ethics recommendations for the allocation of intensive care treatments in exceptional, resource-limited circumstances: the Italian perspective during the COVID-19 epidemic. Crit Care. 2020;24:165. doi:10.1186/s13054-020-02891-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mawer C. Covid-19: we need to be open about rationing ventilators. BMJ. 2020;369:m1542. doi:10.1136/bmj.m1542 [DOI] [PubMed] [Google Scholar]
- 43.Bowers J. FDA Emergency Use Authorization for OR Anesthesia Machines. 2020. Accessed April 28, 2020. https://www.fda.gov/media/136423/download
- 44.Government of Canada. COVID-19 pandemic guidance for the health care sector. Accessed April 28, 2020. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/covid-19-pandemic-guidance-health-care-sector.html
- 45.Toner E, Waldhorn R. What US hospitals should do now to prepare for a COVID-19 pandemic. Accessed April 28, 2020. https://www.centerforhealthsecurity.org/cbn/2020/cbnreport-02272020.html
- 46.Nicoll A, Brown C, Karcher F, et al. Developing pandemic preparedness in Europe in the 21st century: experience, evolution and next steps. Bull World Health Organ. 2012;90:311–317. doi:10.2471/BLT.11.097972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kupferschmidt K, Cohen J. China’s aggressive measures have slowed the coronavirus. They may not work in other countries. Science. Published online March 2, 2020. Accessed July 28, 2020. https://www.sciencemag.org/news/2020/03/china-s-aggressive-measures-have-slowed-coronavirus-they-may-not-work-other-countries
- 48.World Health Organization Europe. China shows COVID-19 responses must be tailored to the local context. Published April 3, 2020. Accessed April 28, 2020. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/4/china-shows-covid-19-responses-must-be-tailored-to-the-local-context
- 49.Cyranoski D. What China’s coronavirus response can teach the rest of the world. Nature. 2020;579:479–480. doi:10.1038/d41586-020-00741-x [DOI] [PubMed] [Google Scholar]
- 50.Beaubien J. How South Korea reined in coronavirus without shutting everything down. Accessed April 28, 2020. https://www.npr.org/sections/goatsandsoda/2020/03/26/821688981/how-south-korea-reigned-in-the-outbreak-without-shutting-everything-down
- 51.Song JY, Yun JG, Noh JY, Cheong HJ, Kim WJ. Covid-19 in South Korea—challenges of subclinical manifestations. N Engl J Med. 2020;382:1858–1859. doi:10.1056/nejmc2001801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Greenwald AS, Bassano A, Wiggins S, Froimson MI. Alternative reimbursement models: bundled payment and beyond: AOA critical issues. J Bone Joint Surg Am. 2016;98:e45. doi:10.2106/JBJS.15.01174 [DOI] [PubMed] [Google Scholar]
- 53.Siddiqi A, White PB, Mistry JB, et al. Effect of bundled payments and health care reform as alternative payment models in total joint arthroplasty: a clinical review. J Arthroplasty. 2017;32:2590–2597. doi:10.1016/j.arth.2017.03.027 [DOI] [PubMed] [Google Scholar]
- 54.Prakash S, Satiani B. Analysis of compensation disparities between junior academic and private practice vascular surgeons. Ann Vasc Surg. 2017;39:236–241. doi:10.1016/j.avsg.2016.05.127 [DOI] [PubMed] [Google Scholar]
- 55.Watts SH, Promes SB, Hockberger R. The Society for Academic Emergency Medicine and Association of Academic Chairs in Emergency Medicine 2009-2010 emergency medicine faculty salary and benefits survey. Acad Emerg Med. 2012;19:852–860. doi:10.1111/j.1553-2712.2012.01400.x [DOI] [PubMed] [Google Scholar]
- 56.LeMaire SA, Trautner BW, Ramamurthy U, et al. An academic relative value unit system for incentivizing the academic productivity of surgery faculty members. Ann Surg. 2018;268:526–533. doi:10.1097/SLA.0000000000002921 [DOI] [PubMed] [Google Scholar]
- 57.Office of Human Resources Management. Final approved pay ranges for physicians and dentists effective January 8, 2017. Accessed July 28, 2020. https://www.va.gov/OHRM/Pay/2017/PhysicianDentist/FinalAnnualPayRanges.pdf
- 58.North American Spine Society. NASS Guidance Document on elective, emergent and urgent procedures. Accessed July 28, 2020. https://www.spine.org/Portals/0/assets/downloads/Publications/NASSInsider/NASSGuidanceDocument040320.pdf
- 59.American Academy of Orthopaedic Surgeons. Private practice COVID-19 support. Accessed May 10, 2020. https://www.aaos.org/advocacy/advocacy-action-center/private-practice-relief
- 60.Lundy DW. A day at the office: private practice and private equity. Clin Orthop Relat Res. 2019;477:955–957. doi:10.1097/CORR.0000000000000758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sivo S, Saunders C, Chang Q, et al. How low should you go? Low response rates and the validity of inference in IS Questionnaire research. J Assoc Inf Syst. 2006;7:351–414. doi:10.17705/1jais.00093 [Google Scholar]