Summary
Background
Despite calls for gender transformative family planning interventions to increase male engagement and female reproductive agency, there is limited research involving rigorous evaluation of the integration of these approaches. CHARM2 (counseling Husbands and wives to Achieve Reproductive Health and Marital Equity) builds upon a prior three-session male engagement intervention by integrating female-focused sessions emphasizing women's choice and agency (i.e., gender synchronization). We hypothesized that CHARM2 participants will be more likely to report marital contraceptive use and communication and women's contraceptive agency, and less likely to report unintended pregnancy, relative to participants in the control condition.
Methods
We conducted a two-armed cluster randomized controlled trial evaluating the effects of CHARM2 on marital contraceptive use, communication, decision-making; women's contraceptive agency, and pregnancy among young married couples in rural Maharashtra, India (ClinicalTrials.gov #NCT03514914, complete). 40 geographic clusters, defined based on the catchment areas of subcenter health facilities (the most proximal level of community health care within India's public health system) were randomized to control (n = 20) and intervention (n = 20). We assigned all participants within that geographic cluster to the corresponding cluster treatment condition; participants, investigators, and study staff were not masked to treatment assignment. Eligibility criteria included wife aged 18–29, couple residing together for at least six months with no plan for migration, and neither spouse sterilized or infertile. The CHARM2 intervention included five provider-delivered sessions on gender equity and family planning, two delivered in parallel to husbands and wives separately by gender-matched providers, and one final joint session, delivered within the four months subsequent to baseline survey. We conducted surveys and pregnancy testing at baseline and 9-month and 18-month follow-up. We used difference-in-differences multilevel mixed effects logistic regressions to assess CHARM2 effects on marital contraceptive use and communication, and women's contraceptive agency; we used single time point mixed effects logistic regressions for pregnancy outcomes. All analyses used an intention-to-treat approach.
Findings
1201 couples were recruited between September 2018 and June 2019; 600 intervention and 601 control. All couples were included in outcome analyses. Full couple retention was 90·2% (n = 1083) at 9-month follow-up and 90·5% (n = 1087) at 18-month follow-up. Modern contraceptive use was higher among intervention participants at 9-month but not 18-month follow-up (9-month adjusted ratio of odds ratio [AROR] 1·5, 95% CI 1·03–2·3; 18-month AROR 0·8, 95% CI 0·4–1·4). Communication (9-month AROR 1·9, 95% CI 1·0–3·6; 18-month AROR 2·7, 95% CI 1·5–4·8) and agency (9-month AROR 5·1, 95% CI 1·2–22·4; 18-month AROR 8·1, 95% CI 1·4–48·2) both improved at both time points. There was no significant difference in pregnancy between groups over the 18-month period (AOR 0·8, 95% CI 0·7–1.1) However, for women who expressed fertility ambivalence at baseline, unintended pregnancy was marginally less likely among intervention participants (47% vs 19%) (p = 0·07). There were no reported adverse events.
Interpretation
The CHARM2 intervention offers a scalable model to improve contraceptive use, communication, and agency and possibly decrease unplanned pregnancies for couples in rural India.
Keywords: Family planning, Cluster randomized controlled trial, Contraceptive use, Gender equity
Research in Context.
Evidence before this study
We systematically reviewed clinical trials evaluating gender-equity focused and gender-transformative family planning interventions to assess the approach and impact of these on contraceptive uptake and pregnancy outcomes. In August of 2020 and January of 2021, we searched PubMed using the following MeSH search terms: (“family planning” OR “contraception”) AND (“gender-transformative” or “gender equity”) OR (“male engagement”) with the following filters “clinical trial” (Phases I-IV and Pragmatic, excluded veterinary), “randomized controlled trial”, “evaluation study”, “meta-analysis”, “observational study” (excluded veterinary), “review”, and “systematic review”. We also limited our search to articles published in the past 10 years. We identified 39 papers. We additionally obtained papers known to and recommended by our co-authors on this paper, as well as via reviewer recommendations.
Evidence indicates that addressing gender norms in family planning counseling may be effective at increasing contraceptive use, but gender-synchronized interventions addressing gender norms, male engagement, and female agency are limited. Further, more intensive interventions- longer duration with more points of contact – remain the norms for these types of programs, impeding their scale up.
Added value of this study
This study involves a two-armed cluster evaluation of CHARM2, a gender synchronized, gender equity-focused family planning intervention. CHARM2 is a briefer intervention built upon the three-session (two male-only sessions and one couple session) counseling Husbands to Achieve Reproductive Health and Marital Equity (CHARM) intervention, which employed male health providers to engage and counsel husbands on gender equity and family planning (GE + FP). CHARM2 added two women-focused sessions delivered by a female provider, a broader array of contraceptive options, and evaluation measures on women's agency as potential outcomes. Evaluation results indicate significant effects of CHARM2 on marital contraceptive use and communication and women's contraceptive agency at 9-month follow-up, as well as on contraceptive communication, women's reproductive agency, and a trend in pregnancy planning at 18-month follow-up. We also found high intervention participation and satisfaction with the intervention. The 18-month follow-up period overlapped with the COVID-19 pandemic, which may have affected access to modern contraceptives and thus contraceptive use.
Implications of all the available evidence
Results of this study indicate that CHARM2 is a scalable model with high receptivity from couples that can increase male engagement in family planning and female contraceptive agency, in tandem, with impacts on contraceptive use and potentially pregnancy planning. Study findings related to this briefer intervention inclusive of both members of a married couple have broad implications for an approach to FP intervention at scale for low resource settings in India and elsewhere.
Alt-text: Unlabelled box
Introduction
The prevalence of modern contraceptive use in India has remained largely unchanged for almost two decades, with most contraceptive use occurring in the form of sterilization.1,2 Family planning (FP) services in India emphasize and incentivize female sterilization, and reversible contraceptive methods, which can support healthy birth spacing and delaying first births, receive less attention.1 Even within more highly resourced Indian states such as Maharashtra, 59% of women who use a modern contraceptive report never receiving counseling on other contraceptive options,3 and 78% of married women reporting non-use of a contraceptive report never received FP counseling from a health provider.2 Findings highlight the need for strengthening evidence-based FP services in India with greater emphasis on women's reproductive choice and agency.
Research posits that gender equity in FP interventions is important to support women's reproductive choice and agency and to increase modern contraceptive use, particularly in contexts where traditional gender norms prevail.4 Gender transformative interventions that aim to alter traditional gender roles and normative practices, particularly as relates to male engagement in FP and the unacceptability of male violence against women, have proven effective in improving contraceptive uptake among young married couples.5, 6, 7 Importantly, many of these male engagement interventions focus on respectful marital communication and joint contraceptive decision-making, which is in itself require a shift in norms. Prior research from India involved evaluation of such an approach, the CHARM (counseling Husbands to Achieve Reproductive health and Marital equity) intervention, a three-session gender equity and family planning (GE+FP) counseling intervention delivered by male health care providers to married men, both alone and with their wives. CHARM session attendance by men was high (91%), and a randomized controlled trial evaluating CHARM found significant impacts on contraceptive use and men's gender role ideologies over an 18-month follow-up period.8,9 However, despite the effectiveness of the intervention, and high male participation, impact on contraception was largely limited to condoms, and only half of women participated in couple sessions.8 Inadequate focus on women may have impeded their participation and uptake of female-controlled reversible contraceptive methods. Further, low engagement of women in an FP program can impede women's reproductive agency.
Building upon this work, we developed the gender-synchronized CHARM2 (counseling Husbands and wives to Achieve Reproductive health and Marital equity) intervention. CHARM2 is a five session GE+FP counseling intervention, which added two female-only sessions (delivered by female health providers) in parallel with the two male-only sessions provided in the original CHARM intervention, followed by a joint session for the couples.10 CHARM2 built upon the original CHARM intervention by offering a broader array of contraceptives (e.g., intrauterine devices (IUDs), and oral contraceptive pills (OCPs)) directly to women by a gender-matched provider across the multiple sessions. We use a person-centered care approach, a proven model that places women at the center of FP decision-making, relative to the provider and the male partner.11, 12, 13, 14, 15 This approach, which borrowed from prior reproductive coercion-focused clinical interventions with women,16,17 was designed to ensure that the intervention did not just emphasize male engagement but also female reproductive agency.4
The CHARM2 model is a briefer intervention than most evaluated interventions with demonstrated effectiveness in reproductive and sexual health outcomes in low and middle income countries (LMICs), which tend to be community-based rather than provider-delivered, and are ongoing via mass media or groups rather than individual or couple focused care.18,19 We found couple-level interventions lacking in the literature. The local provider-delivered CHARM2 model offers only three required points of contact for men and women, respectively, with the last point of contact for the couple jointly. This approach allows for a more personally tailored approach and greater ease for participation, given the localized access combined with low required number of contacts. Fewer contact requirements can facilitate uptake and scale of this intervention. This approach requires more contact that the World Health Organization-recommended brief intervention approach, which involves one session for less than 60 min,20,21 but a one-session intervention would be difficult to carry out with coverage of sensitive gender equity issues, such as son preference and intimate partner violence (IPV), in conjunction with FP counseling. Nonetheless, our approach included strategies used in brief sexual and reproductive health interventions with proven effectiveness, including education on social and health consequences, behavioral demonstration and feedback, and use of a credible source.22
Methods
Study design
We conducted a two-arm cluster randomized controlled trial to evaluate the impact of the CHARM2 GE+FP intervention, relative to standard of care, on modern contraceptive use, marital contraceptive communication and joint decision-making (male engagement outcomes), women's contraceptive agency (contraceptive self-efficacy and equal control over decision-making), and pregnancy. The complete study protocol is published elsewhere and included as an appendix (see Supplemental Document 1).10 Briefly, married couples were recruited from households in the rural Pune district of Maharashtra, India. The study area was selected due to lower than state-level modern spacing contraceptive use and higher male to female sex ratio (indicating strong son preference).10
We collected data from couples at three time points: baseline (September 2018–June 2019), nine-month (July 2019–March 2020), and 18-month (June-December 2020) follow-up. There was a gap between the follow-up surveys due to the COVID-19 pandemic and state-wide shutdowns. Our team administered surveys with additional protections during COVID-19, including masking and social distancing.
Cluster randomization, sampling, and recruitment
We randomized 20 geographic clusters within the Junnar taluka (region) of Pune district to receive either the CHARM2 intervention or the standard of care. We created clusters based on the catchment area of subcenter (SC) health facilities, the most proximal level of community health care within India's public health system. Cluster randomization ensured that providers were consistent in offering either intervention or control services to assigned participants, reducing risk for contamination. Neither participants nor research staff were masked to the treatment assignment.
Total sample size of 1200 was determined based on expected treatment effects detectable with 80% power given the two-arm design with 20 equally sized clusters of 48 couples. We recruited 60 couples per cluster to account for 80% retention; full detail on sample size calculation has been published.10 First, research staff screened all households in a cluster for married couples meeting the inclusion criteria: residing together for at least six months with no plan for migration, wife aged 18–29 years, and neither spouse sterilized or infertile. Second, we selected eligible couples using random number generation to obtain 60 couples per cluster. Study staff used random number generation to assign clusters to treatment status and to determine which eligible couples to approach.
Study procedure and retention
Gender-matched research staff obtained written informed consent from participants and conducted one-on-one surveys in private settings with wives and husbands separately. A gender-matched interviewer met with each spouse separately and privately, and obtained written consent immediately prior to survey implementation. If either partner refused consent, the couple was no longer eligible. Staff administered interviews and directly entered the responses into an electronic tablet system. Research staff conducted the 30–60 min interviews in the local language (Marathi).
Standard of FP care in Maharashtra, India
The Indian government has a long-standing public FP program, dating back to 1952.23 They continue to renew their commitments to this issue, with a US$2 billion commitment to expand contraceptive options and FP counseling availability in 2012, and establishment of the Mission Parivar Vikas Programme in 2016 with additional funds and support to improve these same services in high fertility districts in seven states (not including Maharashtra).24,25 Analysis of funding distribution indicates that more than two-thirds of this funding went to support services and incentives for female sterilization.25 Hence, while the Government of India covers IUDs, OCPs, condoms, and male sterilization, as well as injectable contraceptives in some contexts,23 these continue to receive less focus and support from the public health system.25
As part of the country's 2012 commitments to improved contraceptive access,24 the government of India revised their guidelines for SCs to support rural areas across India. Each SC serves a population of 3000–5000, depending on the terrain for ease of outreach, and each must include at least one female auxiliary nurse midwife (ANM) (preferably two) and one male health worker. SCs provide contraceptives and FP counseling within villages, and support accredited social health activists (ASHAs) to provide contraceptives and FP counseling as well.26 Per policy, community-based as well as SC-based clinical efforts should include education and motivation on contraceptives and the social and health benefits of FP, as well as maintaining supply and provision of condoms, OCPs, emergency contraceptives, and IUDs.26 SC facilities must have all necessary materials and conditions for IUD insertion, including a trained ANM. ANMs also offer counseling and referral for safe abortion services and follow-up for any complications from abortion,26 and they also maintain records of households regarding reproductive, maternal, and child health needs, including information regarding contraceptive practices of married household members. They outreach to couples as well as women to support contraceptive uptake and provide follow-up for contraceptive acceptors to address any side effects or concerns related to continuation of contraceptive use.26 The public health system trains ANMs and ASHAs in FP counseling and monitors their provision of services and quality of care.26
The State Government of Maharashtra additionally has two gender equity schemes to reduce son preference.27 The Majhi Kanya Bhagyashree provides payment of IRs.50,000 (approximately US$715) toward one girl child and IRs.25,000 (approximately US$360) for each of two girls. The Beti Bachao Beti Padhao Scheme supports community engagement to build norms and practices that improve the value of the girl child. While there is not clarity on the effectiveness of these schemes, their existence does indicate a policy environment supportive of shifts on the issue of son preference, an issue known to affect contraceptive use in India.25,28,29
Intervention
The CHARM2 intervention involves five sessions of FP+GE counseling delivered over four to six months, with one month between sessions. Two sessions were delivered separately to husbands and wives (i.e., gender-synchronized) by gender-matched health providers, and a final session for couples provided by either the male or female provider who delivered the individual sessions for either spouse, based on availability or participants’ preference. Providers included the ANM attached to the SC as well as local private health providers of both genders, both allopathic and non-allopathic (ayurvedic and homeopathic) doctors. CHARM2 providers, including ANMs and physicians, received a two-day training on gender equity issues, person-centered FP, and the CHARM2 intervention in addition to receipt of standard government FP training. The public health system provided training on IUD insertion to all ANMs in the CHARM2 program, and they made available their IUD insertion training available for allopathic physicians providing CHARM2. We gave all providers in the intervention clusters a visual flip chart covering the themes of CHARM2 content as well as cards with FP methods to facilitate counseling sessions inclusive of contraceptive choice.
CHARM2 FP content for both spouses included exploration of fertility goals and counseling on contraceptive options to achieve these goals including education regarding efficacy, risks, non-contraceptive benefits, and side effects of different types of contraceptives, and skills training and practice related to contraceptive communication and joint decision-making. For women, counseling also assessed for reproductive coercion from partners or family and used a person-centered care approach11, 12, 13, 14 in which women's choice and fertility goals were central to contraceptive decision-making, including discussion about the potential for covert contraceptive use. For men, counseling emphasized the importance of male engagement and respectful communication with wives. GE elements of the program included dialogue on the importance of respect for women and girls, risks of social norms related to son preference, and the effect male dominance and marital violence can have on healthy and positive marital dynamics and the health of women and children (Appendix Table 1).
The provider offered contraceptive methods on the same day if desired and available. We maintained a supply of condoms, pills, and IUDs for providers to distribute to CHARM2 intervention participants at no cost, and these were available at all sessions, though the IUD was only offered and provided to women if a trained ANM or physician was available for insertion. If the women preferred an IUD and there was no trained provider available, the provider scheduled a follow up visit with a trained provider for this service. While we hoped to provide CHARM2 to women through ANMs within the public health system and at the cluster-based SCs, in practice, we often found ANM vacancies at SCs. In these cases, ANMs from other SCs offered coverage. (See Supplemental Document 2.) This offered inconsistent coverage, so trained private and public female physicians provided CHARM2 to women in these clusters.
Control
As described above in our description of standard of care in the country and state, ASHAs provided women in the control group FP brochures, OCPs, and condoms via standard home visits. Our research team also referred women and couples to the locally available public health services at each point of data collection. Local public health services provide FP counseling and select contraceptive methods, as noted above. These services were equivalently available across the treatment and control conditions.
Measures
Outcomes
Outcomes included modern contraceptive use, type of contraceptive use, male engagement in contraceptive use (contraceptive communication and joint decision-making), contraceptive agency (self-efficacy and equal decision-making control), and pregnancy (any pregnancy and pregnancy intention) (Definitions, Table 1).
Table 1.
Outcome measure definitions.
| Construct | Outcome | Definition |
|---|---|---|
| Modern contraceptive use | Any modern use | We asked participants whether they had done anything to prevent or delay a pregnancy within the past three months. If they answered ‘yes’, they were asked which method(s) they had used. Modern methods available in the project area were condoms (male condoms are widely available and there is limited availability of female condoms), combined hormonal and progestin-only oral contraceptive pills, Copper IUDs, emergency contraceptive pills, and sterilization (male and female). Injectable contraceptives were available in a limited number of locations. We excluded currently pregnant women from this outcome. We categorized participants as using a modern method in the past three months or not. Lactational amenorrhea (LAM) was not included as a modern method, per prior research.1 |
| Use by type | The categorical method type outcome included no method use in past three months, rhythm and/or withdrawal use only, condom use, pill use, IUD use, or (at 9-month and 18-month follow-up only) female sterilization use. We excluded currently pregnant women from this outcome. We excluded women exclusively using LAM, emergency contraceptives, and injectable contraceptives from this outcome due to low prevalence (n<10). | |
| Male engagement in contraceptive use | Contraceptive communication | We assessed contraceptive communication by asking women “Did you have a discussion with your husband on contraceptive use in the past three months?”, with response options yes/no. |
| Joint decision-making | We assessed male engagement in contraceptive decision-making via the DHS India measure3: “Would you say that using or not using contraception is mainly your decision, your husband's, joint decision by both, your mother, mother in law, elderly head of household, your sibling, your husband's sibling or someone else?” We dichotomized this as joint decision vs not, to indicate male participation but not unilateral male-decision-making control. | |
| Contraceptive agency | Self-efficacy items 1, 2, & 3 | We used three distinct items to assess wife's contraceptive self-efficacy; these were kept as independent variables rather than combined into a scale due to insufficient intercorrelation. The items were: “How sure are you that you could tell your husband that you wanted to use family planning?”, “How sure are you that you could use family planning?”, and “How sure are you that you could use family planning, even if your husband did not want to?”, with response options ranging from 1 (completely unsure that I could) to 5 (completely sure that I could). Responses to all three items were highly skewed, so we dichotomized responses to completely/somewhat sure (4 or 5) vs not (1, 2, or 3). |
| Decision-making control | We used a single item to assess women's equal control with husband over contraceptive decision-making. We asked: “In the past three months, did you feel that you had equal right (as your husband) to choose a family planning method?” with response options yes/no. | |
| Pregnancy | Any pregnancy | At both 9-month and 18-month follow-up, we asked women if they were currently pregnant and how many times they were pregnant in the prior 9 months (e.g. time since prior survey). Women also took a urine pregnancy test at each time point. We categorized women has having a pregnancy during follow-up if a woman reported a current pregnancy, reported a pregnancy in the prior 9 months, or had a positive pregnancy test, at either follow-up time point. |
| Unintended pregnancy | Women were asked for each pregnancy ‘when you got pregnant, did you want to get pregnant at that time?’. Women who answered ‘no’ to this item (indicating either mistimed or unwanted pregnancy) for any pregnancy at either 9-month or 18-month survey were considered to have an unintended pregnancy during follow-up. |
References:
1. Hubacher D, Trussell J. A definition of modern contraceptive methods. Contraception 2015; 92(5): 420–1.
2. IIPS & ICF. National Family Health Survey (NFHS-4) 2015–16. Mumbai, India, 2017.
Covariates
We assessed wife's age, age at marriage, religion, caste, parity, having a living son, and co-residence with mother-in-law via single item measures using wife's responses. We assessed husband's age and household below poverty line (BPL) card ownership [a proxy for low-income] using husband's responses.
Data analyses
First, we assessed descriptive statistics, including baseline demographics and outcomes at each time point, overall and by treatment. We used Fisher's exact tests to compare categorical items and t-tests to compare continuous items across treatment group; mean and standard deviation are reported for continuous measures.
Next, we assessed intervention effects on current modern FP use, contraceptive communication, joint contraceptive decision-making, contraceptive self-efficacy, and equal contraceptive decision-making control outcomes using an intent-to-treat design and difference-in-differences logistic regression approach, including mixed-effects models with nested random effects to account for cluster randomization. We first constructed unadjusted models, accounting only for time (baseline, nine-month follow-up, 18-month follow-up), treatment status, and time-treatment interaction. We then constructed adjusted models, including baseline demographic characteristics as fixed effects if associated with treatment or with female loss to follow-up in Fisher's exact tests at p<0·20 (if categorical) or t-tests at p<0·20 (if continuous). We used female rather than male loss to follow-up because we used female data to define outcome measures. Demographics included in models as covariates were tested for multicollinearity and were excluded if highly collinear. Fixed effects in these models thus included baseline indicators of religion and of wife living in the same household as her mother-in-law, as well as wife and husband age, wife age at marriage, wife parity, having a living son, scheduled tribe/scheduled caste designation, and BPL card ownership. All models, unadjusted and adjusted, included couple nested within subcenter as random intercepts.
We assessed pregnancy and pregnancy intention during the follow-up period via three single-time-point analyses:
-
(a)
mixed effects logistic regression of any pregnancy during the follow-up time period vs no pregnancy during follow-up, unadjusted and adjusted, with subcenter random effect;
-
(b)
mixed effects logistic regression of unintended pregnancy vs intended pregnancy during follow-up, unadjusted and adjusted, with subcenter random effect; and
-
(c)
multinomial logistic regression of unintended vs intended vs no pregnancy during follow-up, unadjusted and adjusted, with subcenter clustering variance estimation specification.
In unadjusted models, we included only treatment condition as a fixed effect. For adjusted models, we also included the same demographics as models for outcomes above. As an additional post-hoc exploratory analysis, we present ex post facto pregnancy intention stratified by baseline fertility intention, with treatment differences assessed via chi-squared test. Fertility intention at baseline was assessed via a single item asking “Would you like to have (a/another) child, or would you prefer not to have any (more) children?”, with response options ‘Have a/another child; No more/none; Undecided/Don't know’. Due to small cell sizes, we present only unadjusted bivariate analyses.
We also examined contraceptive method mix at each time point as an exploratory analysis. We assessed differences by treatment status at each time point via multinomial regression models, accounting for subcenter clustering and covariates accounted for in primary outcome models.
As a pre-specified sensitivity analysis, we replicated the current use models using generalized estimating equations (GEE) with an exchangeable working correlation matrix. As an additional post-hoc sensitivity analysis, we also replicated the current contraceptive use models using a per-protocol rather than intent-to-treat approach.
To assess acceptability of the intervention, we also conducted basic frequency responses to a participant satisfaction survey, with gender-stratified data presented for each item.
Significance was set at p<0·05 for all comparisons including adjusted odds ratios (AORs) and adjusted ratios of odds ratios (ARORs); conditional (individual) odds ratios (ORs) and 95% confidence intervals (CIs) reported throughout. All analyses were conducted using STATA 15·1.
We used CONSORT guidelines24 for reporting on our cluster randomized controlled trial.
Ethical review
The institutional review boards of the University of California, San Diego, Population Council, and the National Institute for Research in Reproductive Health in India approved the protocol and all participants provided written consent prior to enrollment.
Role of the funding source
The funder had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. All authors had full access to the data in the study; NJ, FV, SA and AR verified data presented. All authors approved of the decision to submit for publication.
Results
Characteristics of the sample at baseline
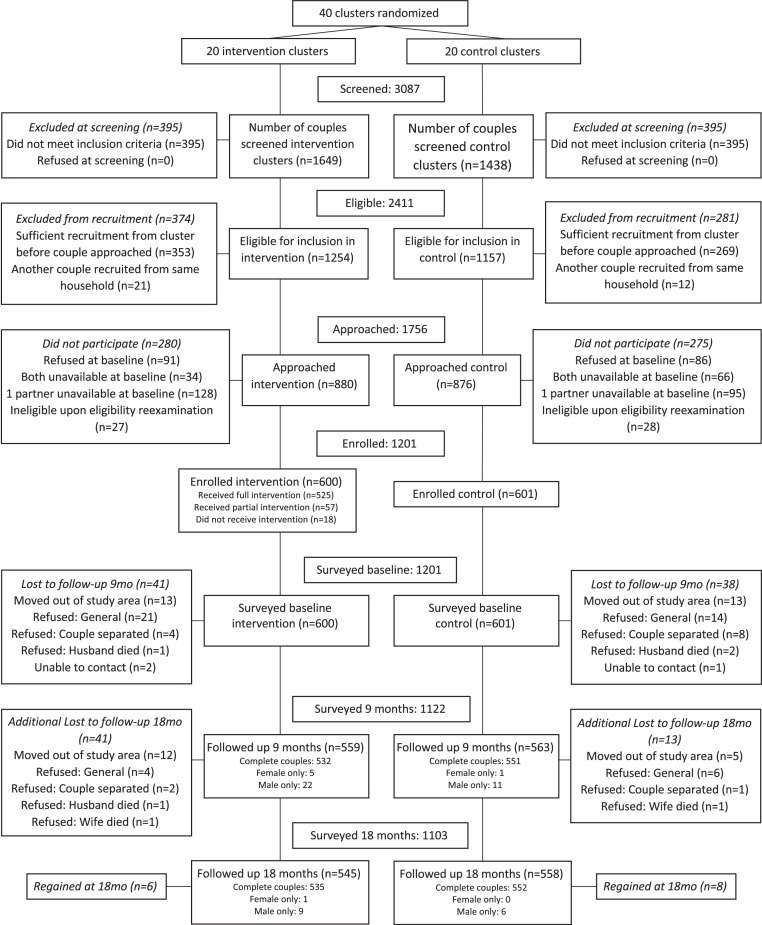
We screened 3087 couples and identified 2411 couples eligible for inclusion in the study (78%) (Figure 1). We then re-approached 1756 of the eligible couples for recruitment. Of the 880 couples and 876 couples approached in the intervention and control clusters, 600 (68·2%), and 601(68·6%) were enrolled; 1201 couples were included in total.
Figure 1.
CHARM2 recruitment and retention CONSORT flow diagram.
At baseline, women averaged 24 (23·9, SD 3·0) and men averaged 29 (29·4, SD 3·8) years old (Table 2). Average monthly household income was 25,182 rupees (approx. $352), most did not hold a BPL card (indicating low income; 75%), had at least secondary education (86% women, 86% men), were not of a scheduled tribe/caste (68% women, 67% men). About half of women (54%) and all men (100%) had worked for pay within the past year. One in six women were nulliparous (16%), 54% had given birth once, and 30% had given birth two or more times.
Table 2.
Characteristics of CHARM2 participants at baseline, by treatment status (n = 1201).
| Overall | Control | Intervention | p-value1 | |
|---|---|---|---|---|
| N | 1201 | 601 | 600 | |
| Wife age, mean (SD) | 23.9 (3.0) | 23.9 (3.0) | 23.9 (2.9) | 0.96 |
| Husband age, mean (SD) | 29.4 (3.8) | 29.4 (3.7) | 29.4 (3.9) | 0.80 |
| Wife age at marriage, mean (SD) | 19.4 (2.3) | 19.4 (2.4) | 19.5 (2.3) | 0.55 |
| Child marriage (wife married <18) | 0.50 | |||
| No | 987 (82.2%) | 489 (81.4%) | 498 (83.0%) | |
| Yes | 214 (17.8%) | 112 (18.6%) | 102 (17.0%) | |
| Couple age difference H-W, mean (SD) | 5.6 (3.2) | 5.5 (3.1) | 5.6 (3.3) | 0.80 |
| Wife parity | 0.31 | |||
| 0 | 197 (16.4%) | 92 (15.3%) | 105 (17.5%) | |
| 1 | 644 (53.6%) | 324 (53.9%) | 320 (53.3%) | |
| 2 | 315 (26.2%) | 157 (26.1%) | 158 (26.3%) | |
| 3+ | 45 (3.7%) | 28 (4.7%) | 17 (2.8%) | |
| Wife highest education completed | 0.24 | |||
| Primary or No education (0–8) | 169 (14.1%) | 93 (15.5%) | 76 (12.7%) | |
| Secondary (9–10) | 345 (28.7%) | 163 (27.1%) | 182 (30.3%) | |
| Higher secondary (11–12) | 321 (26.7%) | 169 (28.1%) | 152 (25.3%) | |
| Post secondary(13+) | 366 (30.5%) | 176 (29.3%) | 190 (31.7%) | |
| Husband highest education completed | 0.94 | |||
| Primary or No education (0–8) | 174 (14.5%) | 86 (14.3%) | 88 (14.7%) | |
| Secondary (9–10) | 368 (30.6%) | 188 (31.3%) | 180 (30.0%) | |
| Higher secondary (11–12) | 305 (25.4%) | 154 (25.6%) | 151 (25.2%) | |
| Post secondary(13+) | 354 (29.5%) | 173 (28.8%) | 181 (30.2%) | |
| Wife worked in past year | 0.27 | |||
| No | 556 (46.3%) | 288 (47.9%) | 268 (44.7%) | |
| Yes | 645 (53.7%) | 313 (52.1%) | 332 (55.3%) | |
| Husband worked in past year | – | |||
| No | 0 (0%) | 0 (0%) | 0 (0%) | |
| Yes | 1201 (100%) | 601 (100%) | 600 (100%) | |
| Religion | <0.001 | |||
| Hindu | 1110 (92.4%) | 529 (88.0%) | 581 (96.8%) | |
| Muslim/Buddhist/Jain/Christian/Other | 91 (7.6%) | 72 (12.0%) | 19 (3.2%) | |
| SCST designation | 0.29 | |||
| None/other | 818 (68.1%) | 418 (69.6%) | 400 (66.7%) | |
| SC/ST/OBC | 383 (31.9%) | 183 (30.4%) | 200 (33.3%) | |
| Husband-reported avg mo income Rs, mean (SD) | 25,182 (51,131) | 27,046 (64,613) | 23,315 (32,384) | 0.21 |
| Household has BPL card | 0.84 | |||
| No | 902 (75.2%) | 453 (75.5%) | 449 (75.0%) | |
| Yes | 297 (24.8%) | 147 (24.5%) | 150 (25.0%) | |
| Has living son | 0.52 | |||
| No | 645 (53.7%) | 317 (52.7%) | 328 (54.7%) | |
| Yes | 556 (46.3%) | 284 (47.3%) | 272 (45.3%) | |
| Mother-in-law lives in same household | 0.097 | |||
| No | 240 (20.0%) | 132 (22.0%) | 108 (18.0%) | |
| Yes | 961 (80.0%) | 469 (78.0%) | 492 (82.0%) |
Fisher's exact test (categorical) or t-test (continuous), control versus intervention.
The full intervention (five CHARM2 counseling sessions) was received by 87·5% of participating couples; an additional 7·3% of women and 5·3% of men received at least one session. Only 3% of couples received no sessions (Figure 1).
At nine-month follow-up, 1083 couples provided surveys, and an additional six women and 33 men responded while their partner did not (Figure 1). Full-couple retention at nine months was 90·2% (88·7% intervention, 91·7% control couples) (p = 0·08). At 18-month follow-up, 1087 couples provided surveys, and an additional one woman and 15 men responded while their partner did not. Full-couple retention at 18 months was 90·5% (89·2% intervention, 91·8% control couples) (p = 0·11).
Differences between treatment groups at baseline
Women in the intervention clusters were more likely to be Hindu (96·8% vs 88·0%, p<0·001) and to live in the same household as their mother-in-law (82·0% vs 78·0%, p = 0·10) (Table 2). No other sociodemographic characteristics differed significantly at p<0·20 between groups.
Current modern contraceptive use
Current modern contraceptive use increased over the study time period for the total study population, from 37·9% at baseline, to 49·6% at nine-month, and 55·7% at 18-month follow-up (Appendix Table 2). Modern contraceptive use was equivalent at baseline (37·6% intervention vs 38·1% control, p = 0·89), marginally higher among intervention participants at nine-month follow-up (52·7% vs 46·6%, p = 0·06), and somewhat lower among intervention participants at 18-month follow-up relative to controls, though this difference was not statistically significant (53·1% vs 58·3%, p = 0·21). In unadjusted difference-in-difference models, significant treatment effects were present at nine-month follow-up (ROR 1·6, 95% CI 1·1–2·4), but not 18-month follow-up (ROR 0·8, 95% CI 0·4–1·4) (Table 3). The magnitude and significance of findings were nearly identical in adjusted models (nine-month AROR 1·5, 95% CI 1·03–2·3; 18-month AROR 0·8, 95% CI 0·4–1·4). As a sensitivity analysis, adjusted GEE analyses produced similar findings, though marginal population treatment effects were slightly attenuated from individual effects observed in logistic regression models (results not shown). As a post-hoc sensitivity analysis, effects from per-protocol analyses were somewhat stronger than those from intention-to-treat analyses at nine months (AROR 1.80, 95% CI 1.20–2.69) though remained not statistically significant at 18-month follow-up (AROR 0.76, 95% CI 0.45–1.28) (results not shown).
Table 3.
Difference-in-differences logistic regression time-treatment interaction effects, assessing CHARM2 impact on modern contraceptive use, contraceptive communication, joint contraceptive decision-making, and contraceptive agency.
| Outcome | Interaction | Simple2 |
Adjusted3 |
|||||
|---|---|---|---|---|---|---|---|---|
| ROR | 95% CI | p-value | AROR | 95% CI | p-value | ICC4 | ||
| Current modern contraceptive use1 | Intervention # 9mo follow-up | 1.59 | [1.07,2.37] | 0.022 | 1.54 | [1.03,2.29] | 0.035 | 0.0081 |
| Intervention # 18mo follow-up | 0.79 | [0.44,1.41] | 0.42 | 0.78 | [0.44,1.39] | 0.40 | ||
| Contraceptive communication | Intervention # 9mo follow-up | 1.96 | [1.06,3.60] | 0.057 | 1.93 | [1.04,3.58] | 0.037 | 0.0111 |
| Intervention # 18mo follow-up | 2.67 | [1.47,4.84] | 0.032 | 2.66 | [1.46,4.84] | 0.001 | ||
| Joint contraceptive decision-making | Intervention # 9mo follow-up | 1.48 | [0.90,2.42] | 0.12 | 1.45 | [0.89,2.36] | 0.14 | 0.0057 |
| Intervention # 18mo follow-up | 1.46 | [0.78,2.75] | 0.23 | 1.46 | [0.77,2.78] | 0.25 | ||
| Contraceptive self-efficacy: How sure are you that you could tell your husband that you wanted to use family planning? | Intervention # 9mo follow-up | 5.13 | [1.17,22.42] | 0.030 | 5.12 | [1.17,22.44] | 0.030 | <0.0001 |
| Intervention # 18mo follow-up | 8.25 | [1.37,49.59] | 0.021 | 8.08 | [1.35,48.19] | 0.022 | ||
| Contraceptive self-efficacy: How sure are you that you could use family planning? | Intervention # 9mo follow-up | 2.64 | [1.17,5.96] | 0.020 | 2.56 | [1.15,5.70] | 0.021 | 0.0435 |
| Intervention # 18mo follow-up | 1.46 | [0.54,3.97] | 0.46 | 1.41 | [0.53,3.75] | 0.49 | ||
| Contraceptive self-efficacy: How sure are you that you could use family planning, even if your husband did not want to? | Intervention # 9mo follow-up | 1.20 | [0.76,1.91] | 0.43 | 1.20 | [0.76,1.89] | 0.44 | 0.0156 |
| Intervention # 18mo follow-up | 1.23 | [0.72,2.12] | 0.45 | 1.22 | [0.71,2.11] | 0.46 | ||
| Equal right to choose contraceptive method | Intervention # 9mo follow-up | 2.55 | [1.04,6.25] | 0.041 | 2.52 | [1.03,6.16] | 0.044 | 0.0046 |
| Intervention # 18mo follow-up | 1.74 | [0.72,4.17] | 0.22 | 1.75 | [0.73,4.21] | 0.21 | ||
Limited to non-pregnant women.
Simple models include time (baseline, 9-month follow-up, 18-month follow-up), treatment status, and time-treatment interaction, with individual nested within subcenter random intercepts to account for repeated measures over time and subcenter clustering.
Adjusted models include same specifications as simple models, as well as baseline indicators of religion, wife living in the same household as her mother-in-law, wife and husband age, wife age at marriage, wife parity, having a living son, scheduled tribe/scheduled caste designation, and BPL card ownership.
Intracluster correlation coefficient, adjusted model.
Types of contraceptives used differed over time. At baseline, 25·4% of women were using condoms, 3·2% pills, 8·9% IUDs, 23·4% withdrawal or rhythm method, and 39·1% were using no method; this did not differ by treatment group (Appendix Table 2). Due to inclusion criteria, no participants were sterilized at baseline. At nine-month follow-up, condom use increased significantly more for intervention compared to control participants (35·3% vs 26·5%, p = 0·004). Female sterilization occurred but did not differ significantly different between groups (5·2% intervention vs 6·9% control, p = 0·37). At 18-month follow-up, condom use was equivalent across groups (32·5% intervention vs 32·2% control, p = 0·94), but pill use was significantly lower among intervention participants (1·8% vs 4·4%, p = 0·02). In multinomial regression models, there were no statistically significant associations between any specific method use (relative to no use) and treatment at baseline (Appendix Table 3). At nine-month follow-up, there was significantly greater condom use (relative to no method use) among participants in the treatment group (AOR 1·8, 95% CI 1·1–2·8). At 18-month follow-up, there was no longer a significant association between condom use (relative to no method use) and treatment, and no other significant association was found between treatment and any other specific method.
Contraceptive communication
At baseline, 35% of women reported having had a conversation about contraceptive use with their husbands within the past three months; this did not differ by group (p = 0·69) (Appendix Table 2). At nine-month follow-up, this had increased to 48% (55% intervention vs 41% control, p = 0·010) and at 18-month follow-up, 40% reported a recent discussion (50% intervention vs 30% control, p<0·001). In both unadjusted and adjusted regression models, women in the treatment clusters were significantly more likely to report this item at both follow-ups (fully adjusted model nine-month AROR 1·9, 95% CI 1·0–3·6; 18-month 2·7, 95% CI 1·5–4·8) (Table 3).
Joint contraceptive decision-making
Male participation in contraceptive decision-making with the female partner was assessed as joint contraceptive decision-making; 79% of women reported this at baseline, and there was no difference by group (p = 0·78) (Appendix Table 2). At nine-month follow-up, this had increased to 87% (89% intervention vs 85% control, p = 0·10) and by 18-month follow-up, 88% of women reported joint contraceptive decision-making (90% intervention vs 86% control, p = 0·04). In both unadjusted and adjusted regression models there was no statistically significant difference between groups in women reporting joint-decision making (fully adjusted model nine-month AROR 1·5, 95% CI 0·9–2·4; 18-month AROR 1·5, 95% CI 0·8–2·8) (Table 3).
Contraceptive agency
An affirmative answer to “How sure are you that you could tell your husband that you wanted to use family planning?” was high at baseline. Almost all women (98%) reported that they were somewhat or completely sure that they could do so (98% intervention vs 99% control, p = 0·22) (Appendix Table 2). This remained true at nine-month (99% intervention vs 98% control, p = 0·11) and 18-month follow-up (99% intervention vs 97% control, p = 0·02). In both unadjusted and adjusted regression models assessing treatment effect, women in the treatment clusters were significantly more likely to report this item (fully adjusted model nine month AROR 5·1, 95% CI 1·2–22·4; 18-month AROR 8·1, 95% CI 1·4–48·2) (Table 3).
Choosing a yes answer to the second contraceptive self-efficacy item, “How sure are you that you could use family planning?” was also high at baseline; 95% of women reported that they were somewhat to completely sure that they could do so (95% intervention vs 95% control, p = 0·89); this went down somewhat over time, to 92% at nine-month follow-up (95% intervention vs 89% control, p = 0.005) and 78% at 18-month follow-up (81% intervention vs 76% control, p = 0·34) (Appendix Table 2). In both unadjusted and adjusted regression models, women in the treatment clusters were significantly more likely to answer that they were somewhat or completely sure on this item at nine-month follow-up (fully adjusted AROR 2·6, 95% CI 1·2–5·7), but not at 18-month follow-up (AROR 1·4, 95% CI 0·5–3·8) (Table 3).
Answering yes to the third contraceptive self-efficacy item, “How sure are you that you could use family planning, even if your husband did not want to?” was less common at baseline; 44% of women reported that they were somewhat to completely sure that they could do so (46% of intervention vs 42% of control, p = 0·21) (Appendix Table 2). This also declined over time, to 37% at nine-month (40% intervention vs 33% control, p = 0·19) and 22% at 18-month follow-ups (24% intervention vs 19% control, p = 0·10). In unadjusted and adjusted regression models, there was no significant treatment effect (fully adjusted nine-month AROR 1·2, 95% CI 0·8–1.9; 18-month AROR 1·2, 95% CI 0·7–2·1) (Table 3).
We assessed whether a woman felt she had as equal right as her husband to decide what contraceptive method to use in the prior three months; 78% of women reported this baseline, and there was no difference by treatment group (p = 0·98) (Appendix Table 2). At nine-month follow-up, this had increased to 90% (94% intervention vs 86% control, p = 0·001) and at 18-month follow-up, 89% reported equal decision-making as their husband (81% intervention vs 86% control, p = 0·048). In both unadjusted and adjusted regression models assessing treatment effect, women in the treatment clusters were significantly more likely to report this item (fully adjusted nine-month AROR 2·5, 95% CI 1·03–6·2; 18-month AROR 1·7, 95% CI 0·7–4·2) (Table 3).
Pregnancy, pregnancy intention, and fertility intention
We found that 48% of women reported a pregnancy at some point during the 18-month study follow-up period, and this was similar between treatment groups (46% intervention vs 50% control, p = 0·23) (Appendix Table 2). This difference remained not statistically significant in unadjusted and adjusted regression models (AOR 0·8, 95% CI 0·7–1.1) (Table 4).
Table 4.
Regression model treatment effects assessing effects of CHARM2 intervention on pregnancy and pregnancy intention in the follow-up period.
| Outcome | Intervention vs control, unadjusted |
Intervention vs control, adjusted4 |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | AOR | 95% CI | p-value | |
| Any pregnancy in the follow-up time period1 | 0.86 | [0.70,1.07] | 0.18 | 0.83 | [0.65,1.06] | 0.13 |
| Unintended pregnancy in the follow-up time period1,2 | 0.89 | [0.58,1.38] | 0.62 | 0.93 | [0.56,1.55] | 0.79 |
| Three-level pregnancy outcome3 | ||||||
| No pregnancy | Ref | Ref | Ref | Ref | Ref | Ref |
| Intended pregnancy(ies) only | 0.90 | [0.73,1.11] | 0.34 | 0.81 | [0.52,1.26] | 0.23 |
| Unintended pregnancy(ies) | 0.85 | [0.64,1.11] | 0.35 | 0.83 | [0.54,1.27] | 0.39 |
Mixed-effects logistic regression, accounting for clustering using subcenter random intercepts.
Limited to women with a pregnancy in in the follow-up time period.
Multinomial logistic regression, accounting for clustering using clustering variance estimation specifications on subcenter.
Adjusted models include baseline indicators of religion, wife living in the same household as her mother-in-law, wife and husband age, wife age at marriage, wife parity, having a living son, scheduled tribe/scheduled caste designation, and BPL card ownership.
Among pregnancies in the follow-up period, approximately one quarter were reported to be unintended (26%, 25% intervention vs 27% control, p = 0·61) (Appendix Table 2). There was no significant association between unintended pregnancy with treatment group in unadjusted (OR 0·9, 95% CI 0·6–1·4) or adjusted regression models (AOR 0·9, 95% CI 0·6–1·6) (Table 4). In multinomial logistic regression models [no pregnancy, intended pregnancy(ies) only, unintended pregnancy(ies)], we found no significant differences by treatment group.
As a post-hoc exploratory analysis, we also examined unintended pregnancy stratified by baseline fertility intention. At baseline, 58% of women reported wanting a/another child, 34% reported wanting no more/none, and 8% expressed ambivalence, as indicated by an ‘undecided/don't know’ response (Appendix Table 4). These responses did not differ by treatment status). For women who expressed fertility ambivalence at baseline, unintended pregnancy was marginally more likely in the follow-up period for control participants (47% vs 19%) (p = 0·07) (Appendix Table 5).
Participant satisfaction
Most participants in the treatment group indicated satisfaction with the CHARM2 program; 76% of women and 75% of men indicated the program has helped daily life very much, 23% of women and 22% of men indicated it helped somewhat, and 1% of women and 4% of men indicated it did not help at all (Table 5). To the question, ‘Do you think this program should be continued beyond the study period?’ 77% of women and 75% of men agreed very much that it should continue, 23% of women and 23% of men agreed somewhat that it should continue, 1% of women and 2% of men responded that it should not continue.
Table 5.
Participant satisfaction - summary items. Intervention participants only.
| Total | Wife |
Husband |
||||
|---|---|---|---|---|---|---|
| 537 | 100% | 100% | 554 | 100% | 100% | |
| N | % | % nonmissing | N | % | % nonmissing | |
| Do you think this program has helped you in your daily life? | ||||||
| Very much | 396 | 73.7 | 75.6 | 387 | 69.9 | 74.0 |
| Somewhat | 123 | 22.9 | 23.5 | 117 | 21.1 | 22.4 |
| Not at all | 5 | 0.9 | 1.0 | 19 | 3.4 | 3.6 |
| Declined | 13 | 2.4 | – | 31 | 5.6 | – |
| Do you think this program should be continued beyond the study time period? | ||||||
| Very much | 405 | 75.4 | 76.6 | 394 | 71.1 | 75.1 |
| Somewhat | 120 | 22.4 | 22.7 | 118 | 21.3 | 22.5 |
| Not at all | 4 | 0.7 | 0.8 | 13 | 2.4 | 2.5 |
| Declined | 8 | 1.5 | – | 29 | 5.2 | – |
| How responsive was the health provider to you about your health and marital concerns? | ||||||
| Very much | 401 | 74.7 | 78.5 | 396 | 71.5 | 79.5 |
| Somewhat | 110 | 20.5 | 21.5 | 100 | 18.1 | 20.1 |
| Not at all | 0 | 0 | 0 | 2 | 0.4 | 0.4 |
| Declined | 26 | 4.8 | – | 56 | 10.1 | – |
Discussion
We conducted this study to assess whether our gender synchronized GE+FP intervention was effective in increasing contraceptive use and communication and women's contraceptive agency, and in reducing unintended pregnancy, among young married couples in rural India. Findings suggest significant short-term impacts on contraceptive use, communication, and agency, as well as some longer-term positive impacts on contraceptive communication and agency in the form of contraceptive self-efficacy and a possible effect on unplanned pregnancies. We also found high intervention participation and satisfaction with the CHARM2 intervention, supporting population receptivity to the program.
We find that the CHARM2 intervention had a significant impact on modern contraceptive use at nine months, largely in the form of increased condom use, but this impact dissipated by the 18-month follow-up. However, these findings should be interpreted with caution, particularly given that data collection at 18-months occurred during the COVID-19 pandemic, when access to the public health system, including some FP services, may have been constrained due to state-wide shutdowns and public health resources re-focused on COVID-19. Additional data collection is likely required to assess longer-term impacts of the intervention, as well as potential impediments to impact attributable to the pandemic, though safety measures such as phone interviews may be required due to the ongoing nature of the pandemic. The emphasis on condom use among CHARM2 participants may be, at least in part, because of our focus on male engagement, but also because this remains the most common method of reversible contraception in the country and state, as was noted in our original CHARM intervention study.8 This has been seen in a number of other male engagement-focused FP evaluation studies, as well.30
We found significant effects of the CHARM2 intervention on contraceptive communication at nine-month and 18-month follow-ups, as was seen in our original CHARM study, as well as sustained effects on women's agency in terms of self-efficacy related to both contraceptive use and contraceptive communication. However, we did not see sustained intervention effect on women's perceptions that they had an equal right as their husband to decide what contraceptive to use, which was seen at 9-month follow-up but lost at 18-month follow-up. This loss of effect, which corresponds with loss of effect on contraceptive use, may indicate need for booster session to sustain intervention effects; prior research shows that FP interventions likely require booster sessions for sustained impact.18 Loss of effect on women's perception of their equal right in contraceptive decision-making may also be due to the COVID-19 pandemic, which resulted in gender regressive practices in households, reinforcing male dominance and authority,31 as well as impeding mobility and contraceptive access for women.31,32 With regard to women's perceptions that they could use contraception even if their husband did not want to, findings are more complex. We saw no intervention effect and in fact, we found a steady decline in women's reports of this form of agency over time, from 44% at baseline to 22% at 18-month follow-up for sample as a whole (Appendix Table 2). Possibly, male engagement itself, in the study and program, may affect a woman's ability to use contraception independently of their husband, even while it increases her involvement and support from him for contraceptive use and FP. Taken together, these findings suggest that male engagement efforts may be more easily achieved and sustained than are women's agency impacts for these types of GE interventions. Further data is needed to understand how to create and sustain gendered impacts in gender-synchronized FP interventions with regard to women's contraceptive behaviors independent of their male partners. The paucity of FP interventions that include evaluation of effects on female agency outcomes hinders understanding of these issues, but this work offers some insight, which can be built upon in future research.
We found that approximately half of all participants, regardless of group, were pregnant at some point over our 18-month follow-up period. This is unsurprising given that our sample is young couples and there are strong pro-fertility norms in this context. Importantly, about one-quarter of these pregnancies were unintended, where women reported that they did not want the pregnancy then or wanted no more pregnancies at all; we found no significant difference in this outcome by treatment group (Appendix Table 4). However, when we further assessed the pregnancies in the follow-up period based on baseline report of whether they wanted no more children, another child, or were unsure, we found a marginal difference by treatment status among the subsample of participants who were unsure and subsequently had a pregnancy in the follow-up period (47% of control vs 19% of intervention participants; p = 0·07) (Appendix Table 5). These findings suggest that while the intervention was not associated with a statistically significant reduction in unintended pregnancy overall, it did potentially affect likelihood of pregnancy among those who were uncertain of their fertility goals at baseline. Ultimately, these findings relied on a small number of observations and should be interpreted with caution, but these exploratory findings support future research to better understand pregnancy intention and ambivalence in FP interventions.
Because we embedded the CHARM2 intervention into the local health system, training and overseeing local providers to deliver the gender equity and FP intervention to couples, findings from this study not only show intervention effects but also the capacity for local providers to deliver the intervention. We found that participants enjoy and, largely, complete all program sessions. These findings support sustainability and scale-up of the CHARM2 intervention. Further indicating support for scale up are responses from key stakeholders in the community, including leadership in the health system and community leaders, as seen from our report on stakeholder interviews and mapping of local providers. (See Supplemental Document 2). These providers and stakeholders indicated that the local system and communities could manage the program and that they believe it should be continued. An additional important finding for scale up is that the intervention likely requires a context with competent and available private providers, particularly given vacancies in the public health system, but these providers can include allopathic as well as non-allopathic practitioners. However, regardless of type of provider and whether they are private or public providers, they must be well trained, have clear values regarding women's agency in FP and gender equity, and provide high-quality care, as recommended from prior research.14 Further examination of data from CHARM2 should assess the provider-client counseling relationship, given the importance of these issues, and given that too few FP evaluation studies from LMICs include data on counseling interactions.33
The CHARM2 model advances the state of the field, which has largely seen effective FP interventions focus solely on women and unmarried adolescents, rather than couples and men, and measure contraceptive use but not women's contraceptive agency as outcomes.18,19 Focus on men and couples remains under-researched and under-utilized at scale, despite decades of calls for male engagement in FP.34 Prior FP interventions with men are largely community-based, much lengthier, and do not include female partners,18,19,34 where the briefer CHARM2 model builds on the health system, facilitating implementation at scale. Further, while previously evaluated male engagement FP interventions include gender equity issues, such as IPV and son preference, they typically do not include feminist theory and female partners, impeding a woman-centered focus on FP with male engagement.35 CHARM2 provides woman-centered care as part of gender-synchronized counseling for couples, personalized risk assessment, and ease of implementation. It uses key elements of proven FP interventions, including education on social and health consequences, behavioral demonstration and feedback, and use of a credible source,22 as well as social and behavioral change approaches proven to affect key gender equity issues in India, such as IPV and son preference and couple communication.25,29 These findings extend on prior research documenting the value of Prachar, a more intensive gender synchronized family intervention for young couples in Bihar, India,36 and our original CHARM FP intervention, which was also brief and able to engage husbands in rural Maharashtra,8 highlighting CHARM2 as brief and effective with couples. Findings should be considered in context of study limitations. Outcomes were largely reliant on self-report and collected by interview, and are, therefore, vulnerable to recall and social desirability biases. We found slight but statistically significant differences between treatment groups at baseline in terms of religion and residence with mother-in-law despite randomization. Additionally, while study retention was high, there were some small differences between participants retained and not retained in the study over time. We conducted the study in a single rural district in India among non-sterilized and married women, limiting generalizability. Finally, data collection at follow-up encompassed the period of the COVID-19 pandemic and subsequent lockdown periods in India, and the pandemic may have affected access to contraceptives as well as women's agency,37,38 potentially affecting our study outcomes at 18-month follow-up. Longer-term follow-up after the pandemic will offer greater insight into potential sustained intervention effects.
Overall, these findings suggest that the gender synchronized GE+FP CHARM2 intervention supports women's reproductive agency, joint contraceptive decision-making, and contraceptive use among young married couples in rural Maharashtra. Over time, there was a loss of effects in contraceptive use and agency, but not male participation. These losses in impact over time may be, at least in part, due to the COVID-pandemic; the pandemic may have affected access to modern contraceptives and women's autonomy generally in the country.37,38 Nonetheless, these findings offer an important contribution to the field highlighting the value of GE focused interventions that increase male engagement and partner communication in FP while simultaneously supporting women's reproductive agency. At the same time, the study reveals that FP intervention effects on women's agency may be more tenuous than effects on male engagement, and thus may require greater support over time, such as booster sessions, for sustained impact. Findings also suggest the potential value of GE+FP interventions to support planned pregnancies among women who are undecided about their fertility goals. Overall, these findings suggest the value of gender synchronized GE+FP interventions but highlight those effects can be tenuous in the context of crisis such as the COVID-19 pandemic.
Declaration of interests
The authors have nothing to disclose.
Acknowledgments
Funding
This work was supported by the National Institutes of Health, Grant R01HD084453.
Authors contributions
SA, SB, NS, JS, and MB are co-Investigators on the study and contributing to the design and implementation of the study and interpretation of the result. FV and NJ are respectively the co-Investigator biostatistician and data analyst on the study and contributed to the power calculations and study design and completed data management and analysis. MG led implementation of the study and AD led development of the survey instruments. AR is the Principal Investigator of the study and led the conceptualization and design; oversaw the implementation and created the first draft this paper. SA and AR oversaw all substantive revisions of the work. All authors contributed to substantive review and revision of the final manuscript.
Data sharing statement
Data used for presented analyses and analytic code are available upon reasonable request from the corresponding author.
Acknowledgments
The authors thank the CHARM2 participants, health providers, and research staff who provided the data and feedback for this study, as well as the communities, health systems, and community leaders that supported and housed this work. We also want to thank our Data Safety and Monitoring Board members, as well as the members of the IRBs who reviewed our work in progress and helped ensure adherence to the highest principles of safe and ethical research.
Footnotes
Trial Registration number: ClinicalTrials.gov Identifier: NCT03514914.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101334.
Appendix. Supplementary materials
References
- 1.IIPS & ICF . IIPS & ICF; 2017. National Family Health Survey (NFHS-4) 2015-16. Mumbai, India. [Google Scholar]
- 2.International Institute for Population Sciences (IIPS) International Institute for Population Sciences (IIPS); 2020. National Family Health Survey (NFHS-5). Key Indicators for 22 States/UTs from Phase-1. [Google Scholar]
- 3.IIPS. National Family Health Survey (NFHS 5) India 2019–2020: Maharashtra. Mumbai, India, IIPS.
- 4.Bhan N., Raj A. From choice to agency in family planning services. Lancet. 2021;398(10295):99–101. doi: 10.1016/S0140-6736(21)00990-9. [DOI] [PubMed] [Google Scholar]
- 5.Hay K., McDougal L., Percival V., et al. Disrupting gender norms in health systems: making the case for change. Lancet. 2019;393(10190):2535–2549. doi: 10.1016/S0140-6736(19)30648-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heymann J., Levy J.K., Bose B., et al. Improving health with programmatic, legal, and policy approaches to reduce gender inequality and change restrictive gender norms. Lancet. 2019;393(10190):2522–2534. doi: 10.1016/S0140-6736(19)30656-7. [DOI] [PubMed] [Google Scholar]
- 7.Kraft J.M., Wilkins K.G., Morales G.J., Widyono M., Middlestadt S.E. An evidence review of gender-integrated interventions in reproductive and maternal-child health. J Health Commun. 2014;19(sup1):122–141. doi: 10.1080/10810730.2014.918216. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raj A., Ghule M., Ritter J., et al. Cluster randomized controlled trial evaluation of a gender equity and family planning intervention for married men and couples in rural India. PLoS One. 2016;11(5) doi: 10.1371/journal.pone.0153190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fleming P.J., Silverman J., Ghule M., et al. Can a gender equity and family planning intervention for men change their gender ideology? Results from the CHARM intervention in rural India. Stud Fam Plann. 2018;49(1):41–56. doi: 10.1111/sifp.12047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dixit A., Averbach S., Yore J., et al. A gender synchronized family planning intervention for married couples in rural India: study protocol for the CHARM2 cluster randomized controlled trial evaluation. Reprod Health. 2019;16(1):88. doi: 10.1186/s12978-019-0744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diamond-Smith N., Warnock R., Sudhinaraset M. Interventions to improve the person-centered quality of family planning services: a narrative review. Reprod Health. 2018;15(1):144. doi: 10.1186/s12978-018-0592-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diamond-Smith N., McDonell C., Sahu A.B., Roy K.P., Giessler K. A mixed-methods evaluation of the impact of a person-centered family planning intervention for community health workers on family planning outcomes in India. BMC Health Serv Res. 2020;20(1):1139. doi: 10.1186/s12913-020-05995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brittain A.W., Loyola Briceno A.C., Pazol K., et al. Youth-friendly family planning services for young people: a systematic review update. Am J Prev Med. 2018;55(5):725–735. doi: 10.1016/j.amepre.2018.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Danna K., Angel A., Kuznicki J., Lemoine L., Lerma K., Kalamar A. Leveraging the client-provider interaction to address contraceptive discontinuation: a scoping review of the evidence that links them. Glob Health Sci Pract. 2021;9(4):948–963. doi: 10.9745/GHSP-D-21-00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holt K., Dehlendorf C., Langer A. Defining quality in contraceptive counseling to improve measurement of individuals' experiences and enable service delivery improvement. Contraception. 2017;96(3):133–137. doi: 10.1016/j.contraception.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Miller E., Decker M.R., McCauley H.L., et al. A family planning clinic partner violence intervention to reduce risk associated with reproductive coercion. Contraception. 2011;83(3):274–280. doi: 10.1016/j.contraception.2010.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller E., Tancredi D.J., Decker M.R., et al. A family planning clinic-based intervention to address reproductive coercion: a cluster randomized controlled trial. Contraception. 2016;94(1):58–67. doi: 10.1016/j.contraception.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mwaikambo L., Speizer I.S., Schurmann A., Morgan G., Fikree F. What works in family planning interventions: a systematic review. Stud Fam Plann. 2011;42(2):67–82. doi: 10.1111/j.1728-4465.2011.00267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma A.E., Frederiksen B.N., Malcolm N.M., Rollison J.M., Carter M.W. Community education and engagement in family planning: updated systematic review. Am J Prev Med. 2018;55(5):747–758. doi: 10.1016/j.amepre.2018.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO . WHO; 2015. Brief Sexuality-Related Communication: Recommendations for a Public Health Approach. Geneva, Switzerland. [PubMed] [Google Scholar]
- 21.Toskin I., Cooper B., Troussier T., et al. WHO guideline for brief sexuality-related communication: implications for STI/HIV policy and practice. Reprod Health Matters. 2015;23(46):177–184. doi: 10.1016/j.rhm.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 22.De Vasconcelos S., Toskin I., Cooper B., et al. Behaviour change techniques in brief interventions to prevent HIV, STI and unintended pregnancies: a systematic review. PLoS One. 2018;13(9) doi: 10.1371/journal.pone.0204088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.GoI . GoI; 2018. National Health Mission: Family Planning. Delhi, India. [Google Scholar]
- 24.FP2030. India: commitment maker since 2012. 2021. https://fp2030.org/india.
- 25.Muttreja P., Singh S. Family planning in India: the way forward. Indian J Med Res. 2018;148(Suppl):S1–s9. doi: 10.4103/ijmr.IJMR_2067_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.GoI . GoI; 2012. Indian Public Health Standards (IPHS) Guidelines for Sub-Centres Revised 2012. [Google Scholar]
- 27.GoM . GoM; 2021. Women Corner: Schemes. [Google Scholar]
- 28.Parsekar S.S., Hoogar P., Dhyani V.S., Yadav U.N. The voice of Indian women on family planning: a qualitative systematic review. Clin Epidemiol Glob Health. 2021;12 [Google Scholar]
- 29.Hoogar P., Pujar A., Dhyani V.S., Parsekar S.S. The voice of Indian women on family planning: a qualitative systematic review and meta-synthesis. Int J Epidemiol. 2021;50(Supplement_1) [Google Scholar]
- 30.Adamou B.M., Iskarpatyoti B.S., Agala C.B., Mejia C. Exploring gaps in monitoring and evaluation of male engagement in family planning. Gates Open Res. 2019;3:1114. doi: 10.12688/gatesopenres.12927.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chauhan P. Gendering COVID-19: impact of the pandemic on women's burden of unpaid work in India. Gender Issues. 2021;38(4):395–419. doi: 10.1007/s12147-020-09269-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Islahi F., Musavi A. Disaster caused by COVID-19 pandemic and lockdown: an overview of Indian women's condition. Disaster Adv. 2021;14(2):65–71. [Google Scholar]
- 33.Ganle J.K., Baatiema L., Ayamah P., et al. Family planning for urban slums in low- and middle-income countries: a scoping review of interventions/service delivery models and their impact. Int J Equity Health. 2021;20(1):186. doi: 10.1186/s12939-021-01518-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hook C., Hardee K., Shand T., Jordan S., Greene M.E. A long way to go: engagement of men and boys in country family planning commitments and implementation plans. Gates Open Res. 2021;5:85. doi: 10.12688/gatesopenres.13230.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robinson M., Aventin Á., Hanratty J., et al. Nothing so practical as theory: a rapid review of the use of behaviour change theory in family planning interventions involving men and boys. Reprod Health. 2021;18(1):126. doi: 10.1186/s12978-021-01173-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Subramanian L., Simon C., Daniel E.E. Increasing contraceptive use among young married couples in Bihar, India: evidence from a decade of implementation of the PRACHAR project. Glob Health Sci Pract. 2018;6(2):330–344. doi: 10.9745/GHSP-D-17-00440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vora K.S., Saiyed S., Natesan S. Impact of COVID-19 on family planning services in India. Sexual Reprod Health Matters. 2020;28(1) doi: 10.1080/26410397.2020.1785378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Agarwal B. Livelihoods in COVID times: gendered perils and new pathways in India. World Dev. 2021;139 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.