Abstract
Introduction and importance
Retrocaval ureter (RCU) is a rare congenital anomaly usually associated with upper urinary tract stasis, in which the ureter itself passes behind the inferior vena cava. RCU is often misdiagnosed and can lead to serious complications related to the upper urinary tract stasis.
Case presentation
We report the case of a 57-year-old female who presented with 1-year history of intermittent right flank pain, of gradual onset. She was diagnosed with right RCU, with advanced functional deterioration of the kidney, managed by nephrectomy. The postoperative course was uneventful.
Clinical discussion
RCU results in varying degrees of hydronephrosis and thus, in a non-specific clinical presentation. Most cases are asymptomatic, discovered only during imaging or surgery for unrelated conditions or at autopsy. A late diagnosis can lead to an obstructive nephropathy which can be very harmful to the kidney.
Conclusion
RCU is a very rare entity. The diagnosis can sometimes be late in under-medicalized settings, and must be taken into consideration in front of any hydronephrosis associated or not with intermittent flank pain. RCU-related complications can be very serious. Fish hook sign may be absent in case of nonfunctional kidney and must not exclude the diagnosis. Emphasis should be placed on prenatal diagnosis and routine abdominal ultrasound for early detection.
Keywords: Retrocaval ureter, Late diagnosis, Kidney functional deterioration, Case report
Highlights
-
•
Retrocaval ureter (RCU) is a very rare congenital anomaly.
-
•
Most cases are asymptomatic and late diagnosis can lead to an obstructive nephropathy which can be very harmful to the kidney.
-
•
This paper highlights difficulties in diagnosis and management of a case of RCU, late diagnosed, with functional deterioration of the kidney, in a ressource-poor setting in Africa.
-
•
We describe the most complex case of RCU reported in the medical literature in sub-Sahara Africa.
1. Introduction
Retrocaval ureter (RCU), also known as postcaval ureter, circumcaval ureter, deilected ureter or preureteric vena cava inferior, is a rare congenital anomaly usually associated with upper urinary tract stasis and an “S” or “fishhook” deformity of the ureter, in which the ureter itself passes behind the inferior vena cava [1], [2]. RCU is an obstructive uropathy whose symptomatology is sometimes nonspecific and whose evolution can be sometimes redoubtful. Several terms used appear to be somewhat misleading, as this configuration is more considered as developmental anomaly of the inferior vena cava (IVC) [3], [4]. IVC anomalies are rare, occurring in up to 8.7% of the population, as left renal vein anomalies are considered [3]. RCU usually presents in the third to the fourth decade of life [5]. However, cases have been reported in the first decade and after the fourth decade [6], [7], [8], [9]. The incidence is 0.06-0.17% worldwide [8], [10], [11]. Most cases are diagnosed post-mortem, during autopsies. Thus, the post mortem incidence varies between 1 in 1500 cases and 2 in 1000 cases [2], [6], [12], [13], [14], [15]. There is a male preponderance with overall reported male to female ratio ranging from 2.8:1 to 4:1 [6], [7], [12], [13], [14], [15], [16], [17], [18].
Most of the cases occur on right side except in situs inversus/duplication of IVC or persistent left subcardinal vein [6], [8], [19], [20], [21]. However, Gladstone reported the condition bilaterally in 1905 [22]. Since RCU can be associated with multiple congenital anomalies, one should also look for them. A total of 20% of cases of RCU present with concomitant anomalies, mainly from cardiovascular system and genitourinary tract [6], [23]. Associated anomalies are numerous, including right double inferior cava, ipsilateral ureterocele, glandular hypospadias, supernumerary lumbar vertebrae, syndactylia, partial situs inversus, solitary kidney, contralateral renal hypoplasia or ectopia, horseshoe kidney, aberrant renal artery, cardiac defects, Turner's syndrome, Goldenhar syndrome, retroperitoneal fibrosis and polycystic disease of the kidneys [6], [7], [24], [23], [25], [26], [27], [28], [29], [30], [31], [32], [33]. Vesicoureteric reflux may also be associated [6]. Historically, the first recorded case of RCU was seen on autopsy and was described by Hochstetter in 1893 [7], [34]. In 1935, Kimbrough reported the first case examined by urography and performed the first successful surgical correction [2], [35], [36]. In 1940 Harrill was the first to diagnose the condition preoperatively [36], [38]. The youngest and the oldest cases of RCU, a still-born acardiac infant and a male of 84 years, were reported by Gladstone [2]. Both were autopsy cases.
A little over 200 cases have been reported worldwide since Hochstetter's first report in 1893 [8], [34], [37]. There are very few reported cases from Sub Saharan Africa countries, including Nigeria, Ghana, Tchad, Cameroon, Mali, Ivory Coast, Togo and Senegal [8], [15], [38], [39], [40], [41]. But, to the best of our knowledge, no cases have been reported with a very severe complication in Sub Saharan Africa medical literature. We report a case of very late diagnosed RCU, with kidney functional deterioration, in Cameroon. The work has been reported in line with the SCARE criteria [42].
2. Case presentation
A 57-year-old female patient, housewife, presented at the outpatient department of our institute on the 25th September 2020, with 1-year history of intermittent right flank pain. Her pain was of gradual onset, spasmodic, without specific radiation, of increasing intensity, relieved by antispasmodics and non-steroidal anti-inflammatory drugs. Her pain was evaluated at 5/10 when she consulted. She had no history of chronic illnesses such as diabetes mellitus or tuberculosis. Her general condition was good, with no fever. Her vital signs were normal. She had a normal body mass index. Her abdomen was soft and the right renal angle showed mild tenderness. The remaining physical examination findings were unremarkable. Our working diagnosis was right calculous renal colic. Our differential diagnoses were pyelonephritis, retroperitoneal fibrosis, retroperitoneal abscess, retroperitoneal hematoma, musculoskeletal disorders or various etiologies of ureteropelvic junction obstruction among which RCU.
All laboratory findings including renal function tests and urinalysis were within normal ranges. Urine culture was sterile. Abdomen ultrasound revealed right-sided hydronephrosis, right proximal ureteral (29.6 mm) and pyelocalic dilatation with paper-thin renal parenchyma, classified as Rad-V or SFU-IV according to the Radiology hydronephrosis grading system (Rad) and to the Society for Fetal Urology grading system (SFU) respectively [43]. The cause of the hydronephrosis was not found. Computed tomography urography revealed an enlarged right kidney with very marked hydronephrosis and significant architectural changes (Fig. 1). The right kidney exhibited no contrast visualization in the collecting duct system. Renal scan using Tc-99m diethylene-triamine-pentaacetate (DTPA) according to GATES's method was performed and revealed decreased perfusion in the right kidney (split renal function of 18%) with obstruction to urine outflow (Fig. 2). The split renal function was 82% on the left. The mean glomerular filtration rate was 99 mL/min. No associated congenital malformations were found.
Fig. 1.

Computed tomography urography showing an enlarged right kidney with very marked hydronephrosis and thinning of the renal parenchyma.
Fig. 2.
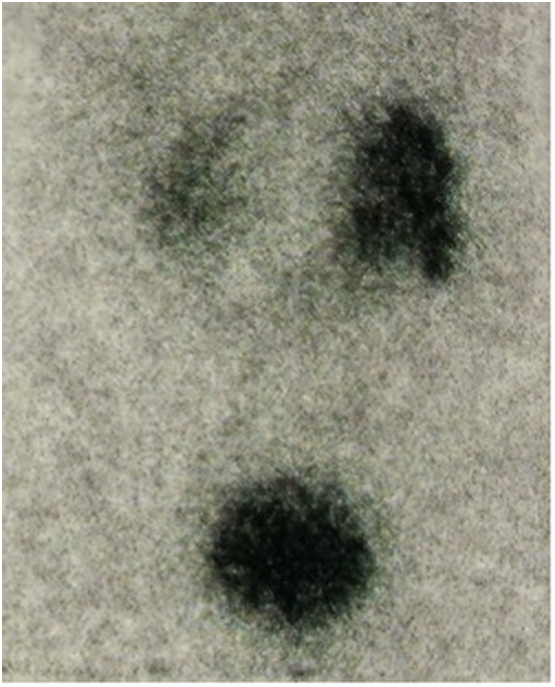
Renal scan after injection of 5 mCi of Tc-99m diethylene-triamine-pentaacetate (DTPA) with injection of furosemide at the twentieth minute revealing a fairly good left renal function and weak right renal function with no transit and incomplete emptying despite the diuretic.
The patient was admitted in the surgical department of our institute. Then, the patient and her relatives were counselled for surgery and a full informed consent was obtained. Pre-operative work up was within normal ranges. We carried out a surgical procedure under general anesthesia, two days after admission. The patient was installed in the lateral position. We proceeded with an open approach by right subcostal incision. On exploration, there was a globular renal enlargement, with important macroscopic architectural remodeling (Fig. 4). The right renal pelvis was dilated, with lumbar ureter retrocrossing the inferior vena cava (Fig. 3), reappearing on its left edge (giving a “water under the bridge” aspect) and continuing its normal course. The ureter was dilated upstream of its retrocaval course. The retrocaval part of the ureter was atretic and the lumen returned to a normal calibre beyond its retrocaval course. A diagnosis of Type 1 RCU with hydronephrosis of the right kidney was made intraoperatively. We proceeded with simple right nephrectomy. The postoperative course was uneventful. The patient was discharged on postoperative day 5. The patient and her relatives were counselled about nephrotoxic substances, medications and various other products. The possibility of a future kidney transplant was also discussed with them. Histopathological examination of specimen revealed very advanced obstructive nephropathy with advanced disruption of the renal architecture, significant kidney damage, end-stage nephrons, epithelial necrosis, tubular atrophy, inflammation and fibrosis. There was intense inflammatory infiltrate and no malignancy. The patient is still followed up. Actually, fourteen months after surgery, she is healthy, with no complaints and normal renal function tests.
Fig. 4.

Right nephrectomy specimen with marked macroscopic architectural remodeling and pyeloureteral dilatation upstream of the retrocaval ureter.
Fig. 3.
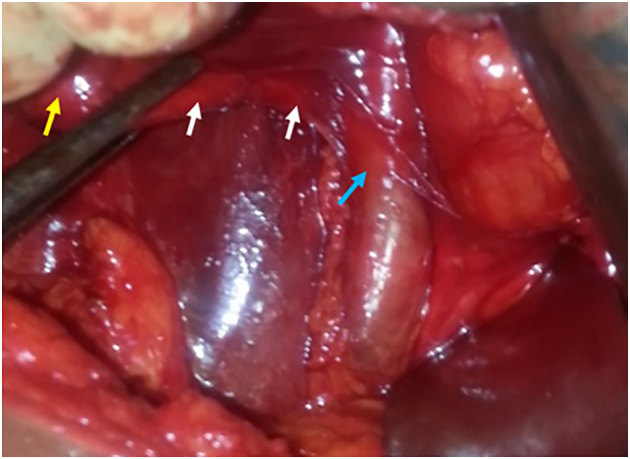
Intraoperative picture showing dilated right pyelon (yellow arrow) with ureter (white arrows) retrocrossing the inferior vena cava (blue arrow) and becoming retrocaval. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
RCU is very rare. Its underhanded evolution is one of the main reasons why its diagnosis is often very late and sometimes post mortem. Although congenital, RCU usually becomes symptomatic in the third or fourth decade of life due to hydronephrosis from compression of the ureteral segment by the IVC against the psoas muscle, ureteral kinking or from an adynamic retrocaval ureteral segment [8], [44], [45]. RCU results in varying degrees of hydronephrosis and thus, in non-specific clinical presentation [17]. In fact, symptoms depend on the degree of ureteral obstruction or the presence of complications. Symptoms include flank or abdominal pain and haematuria. Urinary infection, stone formation, and renal dysfunction may complicate the ureteral obstruction [8], [46]. In extreme cases, when the diagnosis is very late, the obstruction can lead to a nonfunctional kidney. Some patients may present with symptoms earlier than the third or fourth decade of life.
Most cases are asymptomatic, discovered only during imaging or surgery for unrelated conditions or at autopsy [8], [46]. Imaging holds the key to the diagnosis. Two types of RCU have been described based on the classic imaging findings. Bateson adopted in 1969, a classification of surgical interest considering that the obstruction mechanism is different for the two types of RCU: Type 1 in which the obstructive syndrome is due to an intrinsic anomaly in the development of the retrocaval segment of the ureter requiring surgical resection; Type 2 in which the obstruction is due to extrinsic compression of a normal ureter in its retrocaval portion, and for which the plasty is possible without resection [47], [48]. Intravenous urogram (IVU) classically depicts a fishhook-shaped or S-shaped deformity of the ureter in type 1 or the low loop variety of RCU [3], [49]. In type 2, also known as the high loop variety, the retrocaval segment is at the same level as the renal pelvis; the sickle-shaped appearance of the involved ureter can be identified on IVU [3], [49]. Type 1 is the more prevalent variety (90%) and generally causes marked hydronephrosis [15], [48]. Type 2 is generally associated with mild hydronephrosis. RCU is one of the various etiologies of ureteropelvic junction obstruction (UPJO) [50]. Type 1 RCU realises an intrinsic UPJO and type 2, an extrinsic one.
The diagnosis of RCU can sometimes be late in low-income countries [8], [9]. In fact, in low-income countries, patients use to consult very late because they cannot usually afford for hospital bills, since most of those countries lack adequate health coverage system. Ureteral obstruction usually leads to functional deterioration of the kidney in adulthood [15]. Imaging holds the key to the diagnosis and ultrasound is generally the imaging modality that first shows the dilated collecting system. Antegrade or retrograde pyelography can confirm the diagnosis preoperatively. Abdominal ultrasound can at best demonstrate the presence of hydronephrosis since it poorly delineates the ureter, while IVU readily demonstrates hydroureteronephrosis with upward curving and abrupt termination of the ureter and non-visualization of the middle and distal thirds of the ureter as seen in Type I [38]. Spiral computerised tomography (CT), which can delineate both the ureter and IVC, is considered the investigation of choice compared to IVU. Magnetic Resonance Imaging (MRI) can delineate the course of the entire ureter and may be better than CT because it is not associated with radiation exposure, unlike IVU or CT [38]. Renal scan using Tc-99m diethylene-triamine-pentaacetate (DTPA) or mercaptoacetyltriglycine can assess the level of obstruction and determine the best therapeutic modality [51]. RCU is classically characterised by a fishhook-shaped or S-shaped deformity of the ureter on IVU in type 1, also known as fish hook sign [3], [49]. However, this sign may be absent in non-functioning kidneys, exhibiting no contrast visualization in the collecting duct system. The absence of fish hook sign should not exclude the diagnosis of RCU. All these imaging investigations are relatively very expensive in poor countries where the minimum wage ranges between 50 and 200 US Dollars. Poverty is a real barrier to early diagnosis and appropriate management of diseases, especially in settings where there is no adequate health coverage system.
Treatment options include observation for those who are asymptomatic, reconstructive surgery for those with hydronephrosis or nephrectomy if there is cortical atrophy [52]. In cases of complete obstruction of the urinary tract, a timely intervention to release the obstruction is critical for preserving kidney function. RCU is treated surgically either by laparoscopic, robotic or open surgery [17], [53], [54]. Based on European Association of Urology (EAU) and European Society for Pediatric Urology (ESPU) 2019 Guidelines on pediatric urology, surgical indications for Ureteropelvic Junction Type Hydronephrosis (UPJHN) are impaired renal function (<40%), significant renal functional decrease (>10%) in control scans, poor drainage after furosemide injection, increased anteroposterior (AP) diameter, and SFU-III/IV [55]. All of these indications are problematic. The surgical management include division of the dilated renal pelvis with transposition (the ureter is transposed anterior to the IVC) and reanastomosis, ureteroureteral reanastomosis over a double-J stent with or without resection of the stenotic retrocaval segment and ligation or transection of the IVC with or without reanastomosis [16]. Hence, there are many options, including pyeloplasty, ureteropyeloplasty and ureteroureterostomy. Distal strictures may be approached with ureteroneocystotomy [56]. Transperitoneal or retroperitoneal laparoscopic or robotic ureterolysis and reconstruction of the RCU are widely practiced worlwide, but remain very difficult to access for low-income countries [16], [56], [57], [58]. Occasionally nephrectomy may be required in the presence of cortical atrophy or a nonfunctional kidney [16], [52], [59]. A non-functioning kidney was defined as one having paper-thin parenchyma on urinary ultrasound or computed tomography, exhibiting no contrast visualization in the collecting duct system on intravenous urography and having a split renal function of <10% on nuclear renal function studies [60]. In our case, there was a cortical atrophy. The right kidney had a paper-thin parenchyma on urinary ultrasound as well as on computed tomography and exhibited no contrast visualization in the collecting duct system, despite a split renal function of 18% on renal scan using Tc-99m diethylene-triamine-pentaacetate.
Histopathological examination of nephrectomy specimen remains crucial, since squamous metaplasia of the ureter has been reported in RCU [7]. Persistence of hydronephrosis can result in tubular atrophy, inflammation and fibrosis [61]. Disruption of the renal architecture usually correlates with the increased severity of fibrosis [62]. Elevated hydrostatic pressure associated with obstruction results in radial dilatation of the tubules and ducts, leading to increased epithelial apoptosis and tubular atrophy, and causes a reduction in the glomerular filtration rate. RCU is a clinical entity to be very wary of. Renal transplantation remains an indispensable therapeutic option. However, in our country, as in many poor countries, there is still no comprehensive national policy on kidney transplantation. The implementation of such a policy is fundamental and must be encouraged.
RCU is an embryologic anomaly commonly known to urologists as retrocaval or circumcaval ureter. These terms are anatomically descriptive but misleading in regards to development. The anomaly is not the result of an abnormality in ureteral development but rather an anomaly in the development of the inferior vena cava. The term preureteral vena cava may thus emphasize that the circumcaval ureter results from altered vascular, rather than ureteral development [63]. Embryonic folding during the fourth week of development marks the beginning of the urinary tract with the formation of a longitudinal mass known as the urogenital ridge. The collecting duct, major and minor calyces, renal pelvis, and ureters arise from the ureteric bud which originates from the mesonephric duct during the fifth week [64]. The ureters develop from the mesonephros, which travels with the kidney through the lumbar venous ring [7]. Six venous channels in the lumbosacral region are noted in the embryo. The IVC develops from the sixth to the eighth gestational weeks, originating from three paired embryonic veins, namely the subcardinal, supracardinal and postcardinal veins [3]. In man, atrophy of the posterior cardinal vein, which is one of the six veins, should occur in early fetal development. The anomaly occurs between the fourth and eight weeks of intrauterine development and is due to failure of the lumbar segment of right subcardinal vein to get atrophied [6], [24]. If the posterior cardinal vein persists, RCU results [7]. RCU is thus an anomaly of embryologic development of the IVC in which the ventral infrarenal subcardinal vein persists, forcing the more dorsally placed ureter to pass behind it [7], [65]. This anomaly is also called postcaval ureter, circumcaval ureter, deilected ureter or preureteric vena cava inferior, the last mentioned name being aetiologically the most correct one [2].
4. Conclusion
RCU is a very rare entity. The diagnosis can sometimes be late in under-medicalized settings, and must be taken into consideration in front of any hydronephrosis associated or not with intermittent flank pain. RCU-related complications can be very serious. Fish hook sign may be absent in case of nonfunctional kidney and must not exclude the diagnosis. Emphasis should be placed on prenatal diagnosis and routine abdominal ultrasound for early detection.
Funding
No funding sources.
Ethical approval
Our study is exempt from ethical approval by the ethics committee of the Faculty of Medicine and Pharmaceutical Sciences of the University of Douala (Cameroon).
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
N/A.
Guarantor
Arthur ESSOMBA, M.D., Professor of Surgery, General Surgery, Head of Department of Surgery of the Faculty of Medicine and Biomedical Sciences of the University of Yaounde I (Cameroon). email: artgessomba@gmail.com.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
The patient was admitted and operated under the care of Armel Quentin ESSOMBA who concepted the study with Olivier KOPONG FOLA. Frantz Guy NGALLE EPOUPA, Forban AKO and Olivier KOPONG FOLA collected data. From there, the paper was written. Arthur ESSOMBA reviewed the paper and gave the final approval.
Declaration of competing interest
The authors declare no conflict of interest.
References
- 1.Lesma A., Bocciardi A., Rigatti P. Circumcaval ureter: embryology. Eursup. J. 2006;5(5):444–448. doi: 10.1016/j.eursup.2006.02.008. [DOI] [Google Scholar]
- 2.Nielsen P.B. Retrocaval ureter. Report of a case. Acta Radiol. 1959;51(3):179–188. doi: 10.3109/00016925909171095. [DOI] [PubMed] [Google Scholar]
- 3.Bass J.E., Redwine M.D., Kramer L.A., Huynh P.T., Harris J.H. Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. RadioGraphics. 2000;20(3):639–652. doi: 10.1148/radiographics.20.3.g00ma09639. [Pubmed] [DOI] [PubMed] [Google Scholar]
- 4.Cardoza F., Shambhulinga C.K., Rajeevan A.T. Retrocaval ureter and contra lateral renal agenesis – a case report and review of literature. Int. Braz. J. Urol. 2016;42(4):842–844. doi: 10.1590/S1677-5538.IBJU.2015.0549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dudekula, Prabhu S.D. A rare case of right retrocaval ureter with duplication of infrarenal IVC. Case Rep. Radiol. 2014 doi: 10.1155/2014/345712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arya M.C., Kumar L., Kumar R., Mittal R. Retrocaval ureter with vesicoureteric reflux, a very rare entity. Afr. J. Urol. 2017;23:5–8. doi: 10.1016/j.afju.2016.04.005. [DOI] [Google Scholar]
- 7.Hung-Yu L., Yii-Her C., Shu-Pin H., Yung-Chin L., Hsiu-Nan T., Hao-Shuoh J., et al. Retrocaval ureter: report of two cases and literature review. Kaohsiung J. Med. Sci. 2003;19:127–131. doi: 10.1016/S1607-551X(09)70460-7. [DOI] [PubMed] [Google Scholar]
- 8.Atawurah H., Maison P.O.M., Owusu-Ansah M., Asante-Asamani A. Retrocaval ureter: report of two cases. Case Rep. Urol. 2019 doi: 10.1155/2019/2815748. [Pumed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Hajjaj M., Tallaa M. Retrocaval ureter: a case report. J. Surg. Case Rep. 2021;(1) doi: 10.1093/jscr/rjaa596. PMID: 33569165, PMCID: PMC7852603 [Pubmed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uthappa M.C., Anthony D., Allen C. Case report: retrocaval ureter: MR appearances, e. Br. J. Radiol. 2002;75(890):177–179. doi: 10.1259/bjr.75.890.750177. [DOI] [PubMed] [Google Scholar]
- 11.Hostiuc S., Rusu M.C., Negoi I., Grigoriu M., Hostiuc M. Retrocaval ureter: a meta-analysis of prevalence. Surg. Radiol. Anat. 2019;41(11):1377–1382. doi: 10.1007/s00276-019-02269-w. November. Epub (june (14)) (2019), PMID: 31201483 [Pubmed] [DOI] [PubMed] [Google Scholar]
- 12.Resnick M.I., Kurush E.D. In: Campbells Urology. 6th ed. Walsh P., Retic A.B., Stamey T.A., Vaughan E.D., editors. W.B. Saunders; Philadelphia: 1992. Extrinsic obstruction of the ureter; pp. 533–569. [Google Scholar]
- 13.Schlussel R.N., Relik A.B. In: Campbells Urology. 6th ed. Walsh P.C., Retik A.B., Vaughan E.D., editors. W.B. Saunders; Philadelphia: 1998. Anomalies of upper urinary tract-anomalies of ureteric position; pp. 1850–1857. [Google Scholar]
- 14.Heslin J.E., Mamonas C. Retrocaval ureter, report of four cases and review of literature. J. Urol. 1951;65:212–222. doi: 10.1016/S0022-5347(17)68477-5. [DOI] [PubMed] [Google Scholar]
- 15.Rimtebaye K., Mpah H.E.M., Silong F.D., Tashkand A.Z.A., Kaboro M., Niang L., et al. The usage of ultrasound in diagnosing retrocaval ureter. Open J. Urol. 2017;7:212–218. doi: 10.4236/oju.2017.711025. [DOI] [Google Scholar]
- 16.Schlussel R.N., Retik A.B. In: Campbell’s Urology. 7th ed. Walsh P.C., Retik A.B., Vaughan E.D., Wein A.J., editors. Springer; Philadelphia: 1982. Anomalies of the ureter; p. 1850. [Google Scholar]
- 17.Bhattacharjee S., Sanga S., Gupta P., George R.A. Retrocaval ureter or preureteral vena cava: lest we forget this rare cause of hydronephrosis. Med. J. Armed Forces India. 2016;72(1):S77–S79. doi: 10.1016/j.mjafi.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lesma A., Bocciardi A., Rigatti P. Circumcaval ureter: embryology. Eur. Urol. 2006;(5):444–448. [Google Scholar] [Google Scholar]
- 19.Watanabe M., Kawamura S., Nakada T., Ishii N., Hirano K., Numasawa K. Left preureteral vena cava (retrocaval or circumcaval ureter) associated with partial situs inversus. J. Urol. 1991;145:1047–1048. doi: 10.1016/s0022-5347(17)38528-2. [DOI] [PubMed] [Google Scholar]
- 20.Rubinstein I., Calvacanti A.G., Canalini A.F., Freitas M.A., Accioly P.M. Left retrocaval ureter associated with inferior vena cava duplication. J. Urol. 1999;162:1373–1374. [PubMed] [Google Scholar]
- 21.Shin M., Lee J.B., Park S.B., Park H.J., Kim Y.S. Right double inferior vena cava associated with retrocaval ureter: computed tomographic findings in two cases. Clin. Imaging. 2014;38(3):353–356. doi: 10.1016/j.clinimag.2013.12.012. May-Jun. Epub 2014 Jan 6, PMID: 24513316 [Pubmed] [DOI] [PubMed] [Google Scholar]
- 22.Gladstone R.J. Acardiac fetus (acephalus omphalositicus) J. Anat. Physiol. 1905;40:71. [PubMed] [Google Scholar] [PMC free article] [PubMed] [Google Scholar]
- 23.Perimenis P., Gyftopopoulos K., Athanasopoulos A., Pastromas V., Barbalis G. Retrocaval ureter and associated abnormalities. Int. Urol. Nephrol. 2002;33(1):19–22. doi: 10.1023/a:1014436432109. [DOI] [PubMed] [Google Scholar]
- 24.Lin H.Y., Chou Y.H., Huang S.P., Li Y.C., Tsai H.N., Jeng H.S., et al. Retrocaval ureter: report of two cases and literature review, Kaohsiung. J. Med. Sci. 2003;19:127–131. doi: 10.1016/S1607-551X(09)70460-7. [DOI] [PubMed] [Google Scholar]
- 25.Liu E., Sun X., Guo H., Li F., Liu S., Wang K. Retroperitoneoscopicureteroplasty for retrocaval ureter: report of nine cases and literature review. Scand. J. Urol. 2016;50(4):319–322. doi: 10.1080/21681805.2016.1177589. [Pubmed] [DOI] [PubMed] [Google Scholar]
- 26.Ding G.Q., Xu L.W., Li X.D., Li G.H., Yu Y.L., Yu D.M. Pure transperitoneal laparoscopic correction of retrocaval ureter. Chin. Med. J. 2012;125(13):2382–2385. [Pubmed] [PubMed] [Google Scholar]
- 27.Brito R.R., Zulian R., Albuquerque J., Borges H.J. Retrocaval ureter. Br. J. Urol. 1973;45:144–152. doi: 10.1111/j.1464-410x.1973.tb12131.x. [DOI] [PubMed] [Google Scholar]
- 28.Fernandes M., Scheuch J., Seebode J.S. Horseshoe kidney with a retrocaval ureter: a case report. J. Urol. 1988;140:362–363. doi: 10.1016/s0022-5347(17)41608-9. [DOI] [PubMed] [Google Scholar]
- 29.Fuyii Y., Sasabe S., Araki T. Retrocaval ureter treated by division and reanastomosis of the IVC. Acta Urol. Jpn. 1966;12:422–426. [PubMed] [Google Scholar]
- 30.Cleeve D.M., Older R.A., Cleeve L.K., Bredael J.J. Retrocaval ureter in turner syndrome. Urol. 1979;13:544–545. doi: 10.1016/0090-4295(79)90469-2. [DOI] [PubMed] [Google Scholar]
- 31.Ishitoya S., Arai Y., Waki K., Okubo K., Suzuki Y. Left retrocaval ureter associated with the Goldenhar syndrome (branchial arch syndrome) J. Urol. 1997;158(2):572–573. (August) PMID: 9224364 [Pubmed] [PubMed] [Google Scholar]
- 32.Arriola P.M., el-Droubi H., Dahlen C.P. Combined retrocaval ureter and retroperitoneal fibrosis: report of a case. J. Urol. 1979;121:107–108. doi: 10.1016/s0022-5347(17)56682-3. [DOI] [PubMed] [Google Scholar]
- 33.Fujii Y., Sasabe S., Araki T. Retrocaval ureter associated with polycystic disease of the kidneys: treated by division and reanastomosis of the vena cava. Hinyokika Kiyo. 1966;12:1422–1428. [PubMed] [Google Scholar]
- 34.F. Hochstetter , Beitrage zur Entwicklungsgeschichte des Venensystems der Amniten: II. Reptilien (Lacerta, Tropidonotus), Morphol. Jahrb. (Leipzig), 19 (1892–1893) 428–501.
- 35.Carrion H. In: The Ureter. Bergman H., editor. Springer; New York, NY: 1981. Retrocaval ureter: diagnosis and management. [DOI] [Google Scholar]
- 36.Kimbrough J.C. Surgical treatment of hydronephrosis. J. Urol. 1935;33:97. [Google Scholar] [Google Scholar]
- 37.Harrill H.C. Retrocaval ureter: report of a case with operative correction of the defect. J. Urol. 1940;44:459. [Google Scholar] [Google Scholar]
- 38.Ahmed M., Alhassan A., Sadiq M.A., Lawal A.T., Bello A., Maitama H.Y. Variable presentation of retrocaval ureter: report of four cases and review of literature. Niger. Postgrad. Med. J. 2017;24(2):126–197. doi: 10.4103/npmj.npmj_48_17. [DOI] [PubMed] [Google Scholar]
- 39.Tengue K., Botcho G., Kpatcha T.M., Adabra K., Sewa E., Leloua E., et al. Management of the retrocaval ureter in Togo about 3 cases. Afr. J. Urol. 2016;22(4):279–283. doi: 10.1016/j.afju.2016.03.008. [DOI] [Google Scholar]
- 40.Coulibaly N., Koffi D., Sanou B., Sangare I.S., Bi N.B.Gnanazan. Retrocaval ureter : diagnosis and management, a report of three cases. Afr. J. Urol. 2003;9(3):138–142. PMID: 33569165, PMCID: PMC7852603 [Pubmed] [Google Scholar]
- 41.Tembely A., Diarra A., Berthé H., Diakité M.L., Ouattara K. Retocaval ureter : two new observations at Point GA hospital in Bamako. Afr. J. Urol. 2014;20(2):104–107. November. Epub (june (14)) (2019), PMID: 31201483 [Pubmed] [Google Scholar]
- 42.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 43.Onen A. Grading of Hydronephrosis: An Ongoing Challenge. Vol. 8. 2020. p. 458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang K.H., Chang S.C., Huang C.Y., Pu Y.S., Huang J.C. Retrocaval ureter: report of 12 cases and literature review. JTUA. 2005;16(4):163–167. [Google Scholar]
- 45.Hyseni N., Llullaku S., Berisha M., Sheiu A., Grajqevci S., Jashari H. Case presentation of preureteral vena cava and review of the literature. Open J. Urol. 2013;3(5):206–209. [Google Scholar]
- 46.Yarmohammadi A., MohamadzadehRezaei M., Feizzadeh B., Ahmadnia H. Retrocaval ureter: a study of 13 cases. Urol. J. 2006;3(3):175–178. [PubMed] [Google Scholar]
- 47.Hassan R., Aziz A.A., Mohamed S.K. Retrocaval ureter: the importance of intravenous urography. Malays. J. Med. Sci. 2011;18(4):84–87. [Pubmed] [PMC free article] [PubMed] [Google Scholar]
- 48.Bateson E.M., Atkinson D. Circumcaval ureter: a new classification. Clin. Radiol. 1969;20:173–177. doi: 10.1016/s0009-9260(69)80166-2. May-Jun. Epub 2014 Jan 6, PMID: 24513316 [Pubmed] [DOI] [PubMed] [Google Scholar]
- 49.Fadil Y., Bai W., Dakir M., Debbagh A., Aboutaieb R. Retrocaval ureter: a case report and review of the literature. Urol. Case Rep. 2020;35(28) doi: 10.1016/j.eucr.2020.101556. December. PMID: 33437649, PMCID: PMC7787943 [pubmed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grasso M.I.I.I., Caruso R.P., Phillips C.K. UPJ obstruction in the adult population: are crossing vessels significant? Rev. Urol. 2001;3(1):42–51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1476031/ (Winter) [PMC free article] [PubMed] [Google Scholar]
- 51.Gallart R.Méndez, Nieto D.Vela, Tellado M.Gómez, Sánchez M.Montero, E. Paí s.Piñ eiro, Alonso J.Candal. Retrocaval ureter in children: surgical approach based on the obstructive pattern in the diuretic renogram with 99mTc DTPA. Actas Urol. Esp. 1998;22:789–792. [PubMed] [Google Scholar]
- 52.Batura D., Saxena V.K. Retrocaval ureter - a rare cause of hydronephrosis (a case report) Med. J. Armed Forces India. 1997;53(3):223–225. doi: 10.1016/S0377-1237(17)30722-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gupta R., Kesar A., Mahajan A., Mehta A., Masood S. Transperitoneal laparoscopic ureteropyeloplasty of retrocaval ureter: single surgeon experience and review of literature. Asian J. Endosc. Surg. 2021;(28) doi: 10.1111/ases.12970. [DOI] [PubMed] [Google Scholar]
- 54.Inoue Y., Naitoh Y., Ajiki J., Fukui A., Yamada T., Fujihara A. Robot-assisted laparoscopic pyeloplasty for ureteropelvic junction obstruction due to aberrant blood vessel with ipsilateral retrocaval ureter. IJU Case Rep. 2021;4(5):273–276. doi: 10.1002/iju5.12304. ((june) (3)) PMID: 34497981, PMCID: PMC8413217 [Pubmed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Radmayr C., Bogaert G., Dogan H.S., Kocvara R., Nijman J.M., Stein R. European Society for Paediatric Urology and European Association of Urology. EAU Guidelines Office; Arnhem: 2019. EAU guidelines on pediatric urology; pp. 55–59. [Google Scholar]
- 56.Drain A., Jun M.S., Zhao L.C. Robotic ureteral reconstruction. Urol. Clin. N. Am. 2021;48(1):91–101. doi: 10.1016/j.ucl.2020.09.001. (february) Epub ((November) (5)) (2020), PMID: 33218597 [Pubmed] [DOI] [PubMed] [Google Scholar]
- 57.Li H.Z., Ma X., Qi L., Shi T.P., Wang B.J., Zhang X. Retroperitoneal laparoscopic ureteroureterostomy for retrocaval ureter: report of 10 cases and literature review. Urology. 2010;76:873–876. doi: 10.1016/j.urology.2009.12.056. (february) Epub ((November) (5)) (2020), PMID: 33218597 [Pubmed] [DOI] [PubMed] [Google Scholar]
- 58.Tobias-Machado M., Lasmar M.T., Wroclawski E.R. Retroperitoneoscopic surgery with extracorporeal uretero-ureteral anastomosis for treating retrocaval ureter. Int. Braz. J. Urol. 2005;31:147–150. doi: 10.1590/s1677-55382005000200009. [DOI] [PubMed] [Google Scholar]
- 59.Silverman S.G., Leyendecker J.R., Amis E.S. What is the current role of CT Urography and MR Urography in the evaluation of the urinary tract? Radiology. 2009;250(2):309–323. doi: 10.1148/radiol.2502080534. (February) [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 60.Zengin K., Tanik S., Sener N.C., Albayrak S., Ekici M., Bozkurt I.H. Incidence of renal carcinoma in non-functioning kidney due to renal pelvic stone disease. Mol. Clin. Oncol. 2015;3(4):941–943. doi: 10.3892/mco.2015.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chevalier R.L., Thornhill B.A., Forbes M.S., Kiley S.C. Mechanisms of renal injury and progression of renal disease in congenital obstructive nephropathy. Pediatr. Nephrol. 2010;25(4):687–697. doi: 10.1007/s00467-009-1316-5. (April) Epub ((October) (21)) (2009), PMID: 19844747 [Pubmed] [DOI] [PubMed] [Google Scholar]
- 62.LeBleu V.S., Taduri G., O'Connell J., Teng Y., Cooke V.G., Woda C. Origin and function of myofibroblasts in kidney fibrosis. Nat. Med. 2013;19(8):1047–1053. doi: 10.1038/nm.3218. (August) Epub ((June) (30)) (2013), PMID: 23817022, PMCID: PMC4067127 [Pubmed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pick J.W., Anson B.J. Retrocaval ureter: report of a case with discussion of its clinical significance. J. Urol. 1940;43:672. [Google Scholar]
- 64.Aaraj M.S.Al, Badreldin A.M. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2021. Ureteropelvic junction obstruction, ((july) (19)) (2021) (january) PMID: 32809575 [Pubmed] [PubMed] [Google Scholar]
- 65.Fletcher E.W., Lecky J.W. Retrocaval ureter obstructed by an aberrant renal artery. J. Urol. 1971;106:184–185. doi: 10.1016/s0022-5347(17)61256-4. [DOI] [PubMed] [Google Scholar]


