Abstract
Background
Medical students' mental health is a public health problem that has worsened with COVID 19's pandemic. There is a lack of French data. The principal aim was to assess French medical students' mental health.
Methods
An online cross-sectional survey was performed between May 27 and June 27, 2021. An anonymous questionnaire was sent via academic email addresses by medical faculties and secondly on social media. We assessed 7-day anxiety and depressive symptoms were evaluated with the Hospitalization Anxiety and Depression scale, 12-month major depressive episode (MDE) with the Composite International Diagnostic Interview- Short Form, burnout with the Maslach Burnout Inventory, 12-month suicidal ideation, humiliation, sexual harassment, and sexual aggression during their curriculum. Multivariable logistic regression was performed to identify main MDE associated factors.
Outcomes
11,754 participants (response rate: 15.3%) were included. Prevalence of 7-day anxiety symptoms, 7-day depressive symptoms, 12-month MDE, and 12-month suicidal thoughts were 52%, 18%, 25%, and 19% respectively. Burnout syndrome concerned 67% of clinical students and residents and 39% of preclinical students. Prevalence of humiliation, sexual harassment, and sexual abuse during their curriculum were 23%, 25%, and 4%, respectively. Having important (OR = 1.44, IC 95 [1.31–1.58], p < 0.001) or very important financial issues (OR = 2.47, IC 95 [2.15–2.85], p < 0.001), experienced humiliation (OR = 1.63, IC 95 [1.46–1.81], p < 0.001), sexual harassment (OR = 1.43, IC 95 [1.28–1.59], p < 0.001) and sexual abuse (OR = 1.52, IC 95 [1.24–1.85], p < 0.001) were associated with an increased risk of MDE.
Interpretation
This is the largest study on French medical students' mental health. These results point to very particular conditions in French students environment that need to be addressed to improve their mental health.
Keywords: Depression, Anxiety, Burnout, Suicidal ideation, Medical students, Mistreatments
1. Introduction
Medical students' mental health was already a public health issue before COVID19's pandemic. In 2016, a meta-analysis found that 27.2% of medical students experienced depression or depressive symptoms and 11.1% suicidal ideation. Prevalence did not differ between preclinical and clinical students [1]. Among the 183 studies included, only one was French.
In 2016 in France, a national study on students included 19,000 students, of which 2400 medical students. Prevalence in medical students was 15% for 12-month major depressive episode (MDE), assessed by Composite International Diagnostic Interview-Short Form (CIDI-SF) [2], and 9% for suicidal thoughts [3]. In the general population, the prevalence in 2017 was 10% and 5%, respectively, according to the National French health barometer (FHB) using the same questionnaire 4, 5. In 2017, a survey was conducted by medical students associations to measure anxiety and depressive symptoms prevalence among medical students and young doctors using the Hospital Anxiety and Depressive scale (HAD). They found 66.2% of subjects presented a high level of anxiety symptoms and 27.7% a high level of depressive symptoms during the last week (with a >7 cut-off). Furthermore, the study also sought suicidal thoughts in the previous month reported for 23.7% of participants [6]. However, this survey wasn't published. More recently, in 2019, a study on 2000 medical students and young medical doctors using HAD (cut-off >10) found high levels of anxiety and depressive symptoms: 32.3% and 8.7%, respectively [7].
Both studies 6, 7 used the same scale (HAD) but with a different cut-off, rendering difficult the comparison of prevalence without access to the data. Cut-off variability was a problem highlighted by Rotenstein's meta-analysis as well as scales variability [1]. Indeed, there are more than 200 scales to assess depression and even restraining to the 7 common rating scales for depression evaluating 52 different symptoms, only 12% of symptoms are common in all 7 scales [8]. This is why it is important to distinguish between diagnostic questionnaires, using DSM (Diagnostic and Statistical Manual of Mental Disorders) or ICD (International Classification of Diseases) criteria, from scales. In the systematic review on the global prevalence and burden of depressive and anxiety disorders in 2020 (Supplementary data Section 4), the authors found only 3 studies using diagnostic instruments: 2 the CIDI and 1 the Mini International Neuropsychiatric Interview (MINI) [9]. However, even if such tools use the same set of symptoms criteria to determine the presence or the absence of MDE, symptoms heterogeneity can be significant [8]. Other variables can also impact prevalence results such as considering the impairment criteria or not, the period of study, the response rate, handling of missing data (prevalence calculated based on the respondent or the whole sample of participants)… [10].
Another issue in medical students' health is burnout, a syndrome usually defined by the combination of three categories of symptoms: Emotional Exhaustion (EE), Depersonalization (DP), and Personal Accomplishment (PA) [11]. In medical students before residency [12], a meta-analysis estimated burnout's prevalence to 44.2%. In residents, burnout was estimated between 18 and 82% [13]. COVID19's pandemic has considerably impacted mental health, especially for medical students (increased workload, exposition to death, …) [14]. French medical students' associations decided to conduct a new national study. The principal aim was to evaluate French medical students' mental health. Secondary aims were to assess workload, humiliation, and sexual violence (harassment and aggression) elements.
2. Methods
2.1. Overview of the survey and participants
The study was conducted between May 27 and June 27, 2021, using the Qualtrics© platform. An invitation to an anonymous online questionnaire was sent via academic email addresses by medical faculties to all their students. Inclusion criteria were medical students second and the third medical year (preclinical); between the fourth year and the sixth year of medicine (clinical); and medical residents; over 18 years old, registered in a French medical faculty.
A reminder email was sent to all French medical students once a week for three weeks. Because some faculties didn't send at least one email after 2 weeks, a different survey link was also put on social media (Twitter, Facebook, Instagram) by medical students' associations.
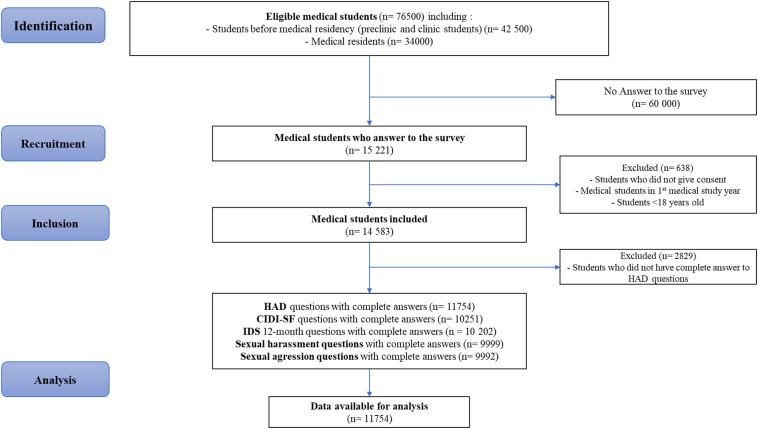
According to public data, 76,500 French medical students were eligible for the survey. Among them, 15,221 answered the survey, and 14,583 were included. We removed from the statistical analysis 2829 participants who did not fulfill HAD (e.g., who stopped answering the questionnaire before completing the HAD). A total of 11,754 participants (response rate: 15.3%) were included for statistical analysis. Concerning the participants, 9159 answers to the questionnaire were obtained from email links and 2595 from social media links. This study was conducted according to the STROBE guidelines and presented as a flowchart (Fig. 1 ).
Fig. 1.
Flowchart of the study according to STROBE guidelines.
2.2. Questionnaire
The survey was designed to ensure comparisons with previous French national surveys on the general population [4] or student population [15], and the survey questions were derived from these studies. The questionnaire was structured in 4 specific sections. Items answering were mandatory to progress to the following questions (“I don't know” or “refuse to answer” were considered as an answer). The first section was related to socio-demographic characteristics (gender, age, familial situation, subjective financial difficulties). The second section concerned the medical curriculum (year of study, work conditions). The third section examined mental health. HAD was used to assess anxiety and depressive symptoms in the last 7 days (cut-off: >10 to compare with general population survey [16] and cut-off>7 to compare with previous national survey on medical students [6]). The Maslach Burnout Inventory (MBI) was used to measure burnout. Two different versions of MBI were proposed to answer: the MBI Student Survey “SS” [17] for students in the preclinical stage (years 2 and 3) and MBI Human Service Survey “HSS” [11] for clinical students (years 4 to 6) or residents (years 7 and more). The CIDI-SF [2] was used to assess MDE with a similar algorithm used in FHB. Suicidal thoughts were also measured. The fourth section contained questions about humiliation, sexual harassment, and aggression during the curriculum. Finally, medical students could write free comments.
CIDI-SF is relatively commonly used as a diagnostic instrument to detect the presence of depression according to ICD criteria [2]. See Supplementary data 1 for details.
2.3. Statistics analysis
Data analysis was performed using R4.0 software. According to our knowledge, there is no agreement for a clear cut-off for HAD nor MBI scales 1, 18 since they were primarily designed as dimensional measurement tools. HAD is commonly used with 2 subscales: (i) for depression (HAD-D) and (ii) anxiety (HAD-A) measures. A recent individual participant data meta-analysis compared HAD-D scores to odds of major depression classification and concluded that compared to CIDI, the HAD-D may misclassify MDE cases and be less sensitive to increases in depressive symptoms. When the CIDI was used as a reference diagnostic tool of MDE, a HAD-D cut off >7 detected 60% of all cases and only 25% with a cut-off >10 [19]. For MBI-HSS, burnout is defined as subscales scores EE > 26 and DP > 9, which is one of the most used in previous surveys according to Rotenstein's meta-analysis [18]. For MBI-SS, burnout is defined as subscales scores EE >14 and CY > 6 and professional/academic efficacy (the equivalent of PA) <23 [20].
Data analysis was performed, including missing responses on MDE, Burnout, suicidal thoughts, humiliation, sexual harassment, and abuse outcome, by recoding them as zero. Missing data were mainly due to participants included in the panel that didn't fully complete the survey. Considering CIDI-SF as a skip structure questionnaire (if screening questions criteria are not met, further questions on secondary symptoms are not asked), all panel members were considered with no condition before applying CIDI-SF algorithm. For predictors variables, answers I don't know, refuse to answer, or missing were included as an unknown response category.
According to the categorical nature of the variables, analyses were presented as a frequency distribution. Specificity, sensitivity, positive predictive value, and negative predictive value for HAD-depression were computed using CIDI-SF as a reference for 12-month MDE cases. Lastly, univariate and multivariate binary logistic regressions were performed with 12-month MDE as the dependent variable and gender, age, familial status, level of study, financial issues, humiliation, sexual harassment, and sexual aggression as explicative variables. Material, code and synthetic data based on original data are available at https://osf.io/9qvb8/.
2.4. Ethics
This study ensures patient information and informed consent regarding the different approved studies through a transparency portal following European Regulation on data protection (GDPR) and was registered to National Commission for Information Technology and Civil Liberties (CNIL) (no. 2220683). The project was accepted by University Paris Saclay's ethics committee: CER-Paris-Saclay-2021-022.
3. Results
3.1. Population
Medical students were mainly women (71%), in a relationship (54%), and having no subjective financial difficulties (54%). There were more men in medical residents (32%) than in preclinical (27%) or clinical (28%) students. They were less single (32% versus 63% and 46%) and had fewer financial issues (62% had very low economic issues versus 50% and 51%), p < 0.001 for all (Table 1 ). There was significant heterogeneity regarding the number of respondents by faculty (17 to 1599) and repartition between official email and social networks (0 to 94%) answers (Supplementary data 2). Social network responders were older, more in a relationship, had more anxiety and depression symptoms, experienced more humiliation and sexual harassment than official email respondents (Supplementary data 3).
Table 1.
Demographic characteristics of the study population.
| Characteristics | Overall (N = 11,754a) | Preclinical level (N = 3167) | Clinical level (N = 4785) | Medical residents (N = 3764) | p-Valueb |
|---|---|---|---|---|---|
| Gender | <0.001 | ||||
| Male | 3387 (29%) | 855 (27%) | 1345 (28%) | 1187 (32%) | |
| Female | 8268 (71%) | 2292 (73%) | 3418 (72%) | 2558 (68%) | |
| Unknown | 61 | 20 | 22 | 19 | |
| Age (years) | <0.001 | ||||
| 18–20 | 1638 (14%) | 1590 (50%) | 47 (1.0%) | 1 (<0.1%) | |
| 21–23 | 4178 (36%) | 1398 (44%) | 2752 (58%) | 28 (0.7%) | |
| 24–26 | 3502 (30%) | 88 (2.8%) | 1709 (36%) | 1705 (45%) | |
| ≥27 | 2371 (20%) | 82 (2.6%) | 267 (5.6%) | 2022 (54%) | |
| Unknown | 27 | 9 | 10 | 8 | |
| Familial situation | <0.001 | ||||
| Single | 5340 (46%) | 1956 (63%) | 2199 (46%) | 1185 (32%) | |
| In a relationship | 6226 (54%) | 1167 (37%) | 2533 (54%) | 2526 (68%) | |
| Unknown | 150 | 44 | 53 | 53 | |
| Financial difficulties | <0.001 | ||||
| Very low | 6289 (54%) | 1555 (50%) | 2400 (51%) | 2334 (62%) | |
| Moderate | 4164 (36%) | 1197 (39%) | 1780 (38%) | 1187 (32%) | |
| Serious | 1126 (9.7%) | 351 (11%) | 561 (12%) | 214 (5.7%) | |
| Unknown | 137 | 64 | 44 | 29 | |
| Anxiety on the last 7 days (HAD > 10) | <0.001 | ||||
| Yes | 6092 (52%) | 1637 (52%) | 2920 (61%) | 1535 (41%) | |
| Depressive symptoms on the last 7 days (HAD > 10) | <0.001 | ||||
| Yes | 2100 (18%) | 531 (17%) | 1058 (22%) | 511 (14%) | |
| MDE on the last 12 months (CIDI-SF) | <0.001 | ||||
| Yes | 2909 (25%) | 835 (26%) | 1272 (27%) | 802 (21%) | |
| Suicidal thoughts on the last 12 months | <0.001 | ||||
| Yes | 2229 (19%) | 523 (17%) | 991 (21%) | 715 (19%) | |
| Burnout on the last 12 months (MBI-HSS) | <0.001 | ||||
| Yes | 5749 (49%) | 0 (0%) | 3277 (68%) | 2472 (66%) | |
| Humiliation during studies | <0.001 | ||||
| Yes | 2652 (23%) | 288 (9.1%) | 1289 (27%) | 1075 (29%) | |
| Sexual harassment during studies | <0.001 | ||||
| Yes | 2901 (25%) | 334 (11%) | 1344 (28%) | 1223 (32%) | |
| Sexual aggression during studies | <0.001 | ||||
| Yes | 515 (4.4%) | 88 (2.8%) | 205 (4.3%) | 222 (5.9%) |
Overall include 38 subjects for whom the level of education is not specified.
Characteristic chi-square test of independence. For psychiatrics symptoms, humiliation and sexual violence, statistical tests performed between variables “yes” (presence of the symptom) and “no” (absence of the symptom).
3.2. Prevalence of psychiatric symptoms
Prevalence of 7-day anxiety and depressive symptoms, 12-month MDE, and 12-month suicidal thoughts were 52%, 18%, 25%, and 19% respectively. Residents showed less anxiety and depressive symptoms and less MDE than younger medical students. Burnout concerned 67% of clinical students and residents and 39% of preclinical students (Table 1).
3.3. HAD-D properties compare to CIDI-SF
With >10 cut-off for HAD-D had worse sensitivity (37,8% vs. 64,5%) and better specificity (89,3% vs. 70,6%) than with >7 cut-off to detect MDE cases measured with CIDI-SF. Using >10 cut-off gave better positive predictive value (57,9% vs. 46,1%) and similar negative predictive value (79,0% vs. 83,7%) (Supplementary data 4).
3.4. Prevalence of humiliation, sexual harassment, and sexual aggression during the curriculum
Prevalence of humiliation, sexual harassment, and sexual abuse were 23%, 25%, and 4.4%, respectively, and increased as students advanced with their curricula (Table 1). Students' mistreatments occurred mainly at the hospital (76%). Aggressors were mostly men (95%) and graduate doctors (60%) but also residents (13%), non-doctor caregivers (12%), and medical students (10%). Student victims mainly told relatives about their situation (51%), fewer to student's union (14%). Less than 10% shared with hospital/university staff, and 18% didn't speak to anyone about those events (Supplementary data 5 to 7).
3.5. Major depressive episode's associated variables
In univariate binary logistic regression, female gender, being single, financial issues, preclinical level, having experienced humiliation, sexual harassment, and sexual abuse were associated with an increased risk of MDE (Table 2 ).
Table 2.
Binary logistic regression model for a major depressive episode (MDE).
| Presence of a MDE during the last 12-months |
Univariate binary logistic regression |
Multivariate binary logistic regression |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | OR | 95% CI |
p-Value | OR | 95% CI |
p-Value | |||
| Lower | Upper | Lower | Upper | |||||||
| Variables | ||||||||||
| Model 0: Only socio demographics variables | ||||||||||
| Gender | ||||||||||
| Male | 2601 (76.5%) | 797 (23.5%) | – | – | – | – | – | – | – | – |
| Female | 6195 (74.7%) | 2100 (25.3%) | 1.11 | 1.01 | 1.22 | 0.034 | 1.14 | 1.04 | 1.26 | 0.007 |
| Medical course | ||||||||||
| Preclinical level | 2332 (73.6%) | 835 (26.4%) | – | – | – | – | – | – | – | – |
| Clinical level | 3513 (73.4%) | 1272 (26.6%) | 1.01 | 0.91 | 1.12 | 0.830 | 1.03 | 0.90 | 1.18 | 0.637 |
| Medical resident | 2962 (78.7%) | 802 (21.3%) | 0.76 | 0.68 | 0.85 | 0.001 | 0.83 | 0.69 | 1.00 | 0.045 |
| Age (years) | ||||||||||
| 18–20 | 1217 (74.3%) | 422 (25.7%) | – | – | – | – | – | – | – | – |
| 21–23 | 3092 (74.0%) | 1087 (26.0%) | 1.01 | 0.89 | 1.16 | 0.837 | 0.97 | 0.83 | 1.14 | 0.704 |
| 24–26 | 2669 (76.1%) | 839 (23.9%) | 0.91 | 0.79 | 1.04 | 0.155 | 1.01 | 0.83 | 1.23 | 0.915 |
| ≤27 | 1835 (76.4%) | 566 (23.6%) | 0.89 | 0.77 | 1.03 | 0.115 | 1.07 | 0.86 | 1.33 | 0.560 |
| Familial situation | ||||||||||
| Single | 3928 (73.4%) | 1423 (26.6%) | – | – | – | – | – | – | – | – |
| In a relationship | 4789 (76.6%) | 1464 (23.4%) | 0.84 | 0.78 | 0.92 | <0.001 | 0.84 | 0.76 | 0.91 | <0.001 |
| Financial difficulties | ||||||||||
| Very low | 5029 (79.7%) | 1280 (20.3%) | – | – | – | – | – | – | – | – |
| Moderate | 3028 (72.4%) | 1152 (27.6%) | 1.49 | 1.36 | 1.64 | 0.001 | 1.49 | 1.36 | 1.63 | <0.001 |
| Serious | 667 (59.1%) | 461 (40.9%) | 2.72 | 2.38 | 3.10 | 0.001 | 2.73 | 2.37 | 3.13 | <0.001 |
| Model 1 (M0 + humiliation) | ||||||||||
| No | 7089 (78.0%) | 1998 (22.0%) | – | – | – | – | – | – | – | – |
| Yes | 1746 (65.5%) | 921 (34.5%) | 1.87 | 1.70 | 2.06 | <0.001 | 1.86 | 1.68 | 2.06 | <0.001 |
| Model 2 (M0 + sexual harassment) | ||||||||||
| No | 6878 (77.8%) | 1964 (22.2%) | – | – | – | – | – | – | – | – |
| Yes | 1957 (67.2%) | 955 (32.8%) | 1.71 | 1.56 | 1.87 | <0.001 | 1.75 | 1.58 | 1.94 | <0.001 |
| Model 3 (M0 + sexual aggression) | ||||||||||
| No | 8526 (75.9%) | 2712 (24.1%) | – | – | – | – | – | – | – | – |
| Yes | 309 (59.9%) | 207 (40.1%) | 2.11 | 1.75 | 2.52 | <0.001 | 2.06 | 1.70 | 2.49 | <0.001 |
Multivariate binary logistic regression identified the same associations. Being a woman (OR = 1.14, IC 95 [1.04;1.26], p = 0.007), single (OR = 1.20, IC 95 [1.10–1.32], p < 0.001), preclinical level (OR = 1.43, IC 95 [1.19–1.72] p < 0.001), having important (OR = 1.44, IC 95 [1.31–1.58], p < 0.001) or very important financial issues (OR = 2.47, IC 95 [2.15–2.85], p < 0.001), having experienced humiliation (OR = 1.63, IC 95 [1.46–1.81], p < 0.001), sexual harassment (OR = 1.43, IC 95 [1.28–1.59], p < 0.001) or sexual abuse (OR = 1.52, IC 95 [1.24–1.85], p < 0.001) during the curriculum were associated with an increased risk of MDE (Table 2).
4. Discussion
Our study found high levels of prevalence of psychiatric symptoms and violence. In the last year, 1 in 4 students suffered from MDE, and 1 in 5 had suicidal thoughts. In agreement with previous data, having financial difficulties [21] and being confronted with humiliation and sexual violence [22] were associated with an increased risk of MDE.
4.1. Comparison with other French studies
Prevalence of 12-month MDE and suicidal thoughts were higher in our study than in medical students in 2016 (15% and 9%, respectively) [3]. In 2016, the prevalence was also more important in younger students: 18% in premed (not included in our study), 14% in preclinical, 13.5% in clinical, and 13% in residents [3]. Prevalence of 7 day depressive and anxiety symptoms were higher in 2021 than in 2017 (75% vs. 66.2% and 39% vs. 27.2% with a 7 cut-off score) [6]. In the French general population, 18–24 years prevalence of anxiety and depressive symptoms (with a 10 cut-off score) were estimated between 33,9% (May 2021) and 28,5% (June 2021) for anxiety and between 26,1% (May 2021) and 22,6% (June 2021) for depressive symptoms [16]. So medical students have more anxiety symptoms but fewer depressive symptoms.
In the French general population aged 18–24, the 12-month prevalence of suicidal thoughts was estimated between 15,7% (May 2021) and 20,1% (June 2021), which was in range with health students (19%) [16].
Prevalence of burnout in preclinical students is consistent with a previous French study conducted at the University of Caen [23]. There is no French data available for clinical students. Before the pandemic, studies found 52% of burnout for digestive surgery residents [24], and 40% for anesthesia and intensive care residents [25].
Humiliation and sexual violence (harassment or abuse) in French medical students were previously described [26]. A study on clinical students, residents, and young doctors found a 16% prevalence of sexual harassment [26]. More recently, a survey on preclinical and clinical students has found a 30% prevalence of sexual harassment [27], slightly higher than us.
4.2. COVID 19 and depression assessment: comparison between studies methodological considerations
A French public organization has assessed a panel of 2000 French adults every few weeks since the first lockdown using the HAD scale. Data for 18–24 year old subjects show huge variations for 7-day depressive symptoms prevalence: from 29% in 28–30 April 2020 to 6% in 24–26 August 2020 and an increase to 32% in 23–25 November 2020 [16]. It highlights HAD's potential utility to monitor for mental health with repetitive measures in an idiographic perspective. However, with a nomothetic consideration of monitoring depression and anxiety in the general population, prevalence could be highly dependent on a short-term context (here, the evolution of pandemic and restraining measures) combined with possible variability induced by different panel participants at each assessment. Furthermore, as observed in a previous study [28], we have found low sensitivity and specificity for last week's depression measured with HAD compared to last year's depression measured with CIDI-SF.
Since the pandemic beginning, students' mental health has been of concern for many countries [29] and has made some headlines in the press. A meta-analysis that included studies published only in 2020 found a prevalence of depressive and anxiety symptoms to be 34% and 32%, respectively [30]. These results should be interpreted with caution. For instance, many studies used Patient Health Questionnaire 9 (PHQ9) [31]: 15 studies used a cut-off ≥5 with a mean prevalence of 49% IC 95 [39–58], whereas 7 studies used a cut-off ≥10 with a mean prevalence of 28% IC 95 [13–46] [30]. Different observed prevalence depends on different chosen cut-off to delineate between normal and pathologic cases. This leads sometimes to a false impression of deterioration or improvement between two studies that could otherwise be explained by different used cut-offs.
4.3. Improving medical student's health
If we cannot rule out that the pandemic has played a part in a higher declaration of symptoms by the study participants, medical students' working conditions are still a matter of concern. The 2017 study [6] was a wake-up call, and several reforms of French medical studies were initiated. French government created in 2019 a dedicated national institution: the National Support Center for health students (and canceled it only two years later). But our results have highlighted the insufficiency of the measures currently in place. Some recommendations have been proposed to improve medical students' mental health [32].
Furthermore, some factors associated with mental health status such as financial difficulties, humiliation, sexual harassment, and sexual abuse could be potential targets to improve the situation. A recent meta-analysis included 84 studies only on psychological interventions for the prevention and treatment of mental health disorders in university students [33]. But institutional interventions are also important [32]. This pandemic is an opportunity to change things. A narrative review on student support systems for undergraduate medical students during the COVID-19 pandemic found 10 studies: the two main themes were academic support and mental health support [34]. French medical universities had a critical gap compared to some countries. In Canada, they created a “National Standard for Mental Health and Well-Being for Post-Secondary Students”. The Quebec government announced a $60 million plan over 5 years for student mental health. As a recent psychiatrist said: it's time to “Creating Space for Well-Being in Medical School and Beyond” [35].
4.4. Limitations and strength
The response rate was under 20%, similar to the previous national study OVE [3] but much higher than a recent national student survey (4.3%) [36]. A few suggestions can be made to improve response rate: financial incentive, better involvement of university staff and reducing number of studies to avoid student's over-solicitation. We did not explore the impact of COVID-19 on the prevalence of anxiety and depression. However, the association between COVID-19 diagnosis and depression and anxiety disorder incidence is not clear 37, 38. Burnout assessment was made with two different scales to be adapted to students' reality, but it limits the ability to compare preclinical and other medical students. Including missing data and recoding them at 0 could underestimate prevalence. Using both emails and social networks reduces bias linked to one-way diffusion [39]; however, we cannot exclude that some participated more than once. Using CIDI-SF allows a 12-month prevalence, which is better if we want to reproduce the survey in the future and compare the prevalence, especially with the French general population [4]. Using both HAD and CIDI-SF allows us to assess sensibility and specificity but only for HAD depression. Lastly, to avoid the Table 2 fallacy 40, 41 (e.g. suggesting implicitly that all of the risk factor estimates can be interpreted similarly), it's important to consider factors identified in this study only as factors associated with medical student mental health that we suppose are involved in a broader complex system.
5. Conclusion
Four years after the first national study about medical students' mental health and one year after COVID19's pandemic beginning, we found an increased prevalence of anxiety and depressive symptoms compared to previous studies. In the last year, 1 student in 4 has had a major depressive episode, and 1 in 5 has had suicidal thoughts. Prevalence of humiliation and sexual harassment are also high, with 1 in 4 medical student victims of such behaviors. Because we used CIDI-SF and the 2 versions of MBI, our study could allow more reliable comparisons and serve as a baseline for future studies. Our study results highlight the urgent need for targeted political actions against violence in hospitals but more broadly to improve student mental health on many different levels of intervention of its complex system.
Research in context
Evidence before this study: Medical students' mental health was already a public health problem [1] that might have worsened with COVID 19's pandemic. COVID19's pandemic has considerably impacted mental health, especially for medical students [14]. Only few studies really assessed the presence of a major depressive episode (MDE) [9].
Added value of this study: This is the first nationwide study to assess MDE in medical students and to seek for associated factors. Depression scale, 12-month major depressive episode (MDE) with the Composite International Diagnostic Interview-Short Form, burnout with the Maslach Burnout Inventory, 12-month suicidal ideation, humiliation, sexual harassment, and sexual aggression during their curriculum. Multivariable logistic regression was performed to identify main MDE associated factors. We found elevated level of MDE, burnout and mistreatment among students. Having important or very important financial issues, experiencing humiliation, sexual harassment, and sexual abuse were associated with an increased risk of MDE.
Implications of all the available evidence: Many medical students had a MDE on the last year. Some risk factors are modifiable. These results highlight the importance of important institutional actions to improve the mental health of medical students. This study can be used as a reference to evaluate the effectiveness of the actions undertaken.
Information on author access to data
Yannick Morvan and Ariel Frajerman had full access to the data.
Funding
None.
CRediT authorship contribution statement
Franck Rolland and Nawale Hadouiri did the ethic submission (French regulator and ethic committee), they contributed to the non psychiatric questions of the survey, the distribution of the questionnaire and the redaction of the manuscript.
Adrien Haas-Jordache, Evan Gouy, Loona Mathieu and Anne Goulard contributed to the non psychiatric questions of the survey, the distribution of the questionnaire and the redaction of the manuscript.
Yannick Morvan and Ariel Frajerman selected the psychiatric tools, programmed the questionnaire, did the statistical analysis and contributed to the redaction of the manuscript. They had access to all the data.
Conflict of interest
F.R., N.H. and E.G. are members of the ISNI's board. A.H. and A.G. are members of the ISNAR-IMG's board. L.M. is a member of the ANEMF board's.
Y.M. is a member of the scientific committee of the “Observatoire de la Vie Etudiante”.
Acknowledgment
The authors thank the medical student associations: ANEMF (“Association nationale des étudiants en médecine de France”), ISNAR-IMG (“InterSyndicale Nationale Autonome Représentative des Internes de Médecine Générale”) and ISNI (“InterSyndicale Nationale des Internes”), and the Conference of Deans of Medical Schools. They also thank Pr Bruno Falissard for his support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.03.001.
Appendix A. Supplementary data
Supplementary material
References
- 1.Rotenstein L.S., Ramos M.A., Torre M., et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler R.C., Andrews G., Mroczek D., Ustun B., Wittchen H.U. The World Health Organization composite international diagnostic interview short-form (CIDI-SF) Int. J. Methods Psychiatr. Res. 1998;7(4):171–185. doi: 10.1002/mpr.47. [DOI] [Google Scholar]
- 3.Frajerman A., Chevance A., Chaumette B., Morvan Y. European Psychiatry. Vol 63. CAMBRIDGE UNIV PRESS EDINBURGH BLDG; SHAFTESBURY RD, CB2 8RU CAMBRIDGE, ENGLAND: 2020. Are medical students really more affected by depression than other students? results from a national survey of 18,875 students in France. S138-S138. [Google Scholar]
- 4.C. Léon La Dépression en France Chez Les 18-75 Ans : Résultats du Baromètre Santé 2017 / Depression in France Among the 18-75 Year-olds: Results from the 2017 Health Barometer. :8.
- 5.C Léon . Baromètre de Santé Publique France 2017 : Tentatives de Suicide etPensées Suicidaires Chez Les 18-75 ANS / Santé Publique France Health Barometer 2017: Suicidal Attempts and Suicidal IdeationAmong the 18-75 Years-old. :10.
- 6.Fuhrman J. Enquête santé mentale des jeunes médecins. ANEMF.org, le site officiel des étudiants en médecine. 2017. https://www.anemf.org/blog/2017/06/13/enquete-sante-mentale-des-jeunes-medecins-2/ Accessed February 3, 2020.
- 7.Fond G., Boulangeat C., Messiaen M. Anxiety and depression in young physicians: prevalence and associated factors. The MESSIAEN national study. Encephale. 2021 doi: 10.1016/j.encep.2021.02.005. Published online April 20. S0013-7006(21)00084-1. [DOI] [PubMed] [Google Scholar]
- 8.Fried E.I. The 52 symptoms of major depression: lack of content overlap among seven common depression scales. J. Affect. Disord. 2017;208:191–197. doi: 10.1016/j.jad.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 9.COVID-19 Mental Disorders Collaborators Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021 doi: 10.1016/S0140-6736(21)02143-7. Published online October 8. S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morvan Y., Frajerman A. La santé mentale des étudiants : mieux prendre la mesure et considérer les enjeux. L’Encéphale. 2021 doi: 10.1016/j.encep.2020.10.009. Published online March 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maslach C., Jackson S.E. The measurement of experienced burnout. J. Organ. Behav. 1981;2(2):99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 12.Frajerman A., Morvan Y., Krebs M.O., Gorwood P., Chaumette B. Burnout in medical students before residency: a systematic review and meta-analysis. Eur. Psychiatry. 2019;55:36–42. doi: 10.1016/j.eurpsy.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Prins J.T., Gazendam-Donofrio S.M., Tubben B.J., Van Der Heijden F.M.M.A., Van De Wiel H.B.M., Hoekstra-Weebers J.E.H.M. Burnout in medical residents: a review. Med. Educ. 2007;41(8):788–800. doi: 10.1111/j.1365-2923.2007.02797.x. [DOI] [PubMed] [Google Scholar]
- 14.Magklara E., Angelis S., Solia E. The role of medical students during COVID-19 era. A review. Acta Biomed. 2021;92(1) doi: 10.23750/abm.v92i1.10873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Enquête sur les conditions de vie des étudiant·e·s. OVE : Observatoire de la vie Étudiante. 2021. http://www.ove-national.education.fr/enquete/enquete-conditions-de-vie/ Accessed August 25.
- 16.CoviPrev une enquête pour suivre l’évolution des comportements et de la santé mentale pendant l’épidémie de COVID-19. 2021. https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquete-pour-suivre-l-evolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie-de-covid-19 Accessed August 23.
- 17.Schaufeli W.B., Martinez I.M., Pinto A.M., Salanova M., Bakker A.B. Burnout and engagement in university students: a cross-national study. J. Cross-Cult. Psychol. 2002;33(5):464–481. [Google Scholar]
- 18.Rotenstein L.S., Torre M., Ramos M.A., et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Y., Levis B., Sun Y., et al. Probability of major depression diagnostic classification based on the SCID, CIDI and MINI diagnostic interviews controlling for hospital anxiety and depression scale - depression subscale scores: an individual participant data meta-analysis of 73 primary studies. J. Psychosom. Res. 2020;129 doi: 10.1016/j.jpsychores.2019.109892. [DOI] [PubMed] [Google Scholar]
- 20.Kajjimu J., Kaggwa M.M., Bongomin F. Burnout and associated factors among medical students in a public University in Uganda: a cross-sectional study. Adv. Med. Educ. Pract. 2021;12:63–75. doi: 10.2147/AMEP.S287928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajapuram N., Langness S., Marshall M.R., Sammann A. Medical students in distress: the impact of gender, race, debt, and disability. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0243250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cook A.F., Arora V.M., Rasinski K.A., Curlin F.A., Yoon J.D. The prevalence of medical student mistreatment and its association with burnout. Acad. Med. 2014;89(5):749–754. doi: 10.1097/ACM.0000000000000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Breton P., Morello R., Chaussarot P., Delamillieure P., Le Coutour X. Burnout syndrome among third year medical students in Caen: prevalence and associated factors. Rev. Epidemiol. Sante Publique. 2019;67(2):85–91. doi: 10.1016/j.respe.2019.01.119. [DOI] [PubMed] [Google Scholar]
- 24.Chati R., Huet E., Grimberg L., Schwarz L., Tuech J.J., Bridoux V. Factors associated with burnout among french digestive surgeons in training: results of a national survey on 328 residents and fellows. Am. J. Surg. 2017;213(4):754–762. doi: 10.1016/j.amjsurg.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Jaulin F., Nguyen D.P., Marty F., et al. Perceived stress, anxiety and depressive symptoms among anaesthesia and intensive care residents: a French national survey. Anaesth. Crit. Care Pain Med. 2021;40(3) doi: 10.1016/j.accpm.2021.100830. [DOI] [PubMed] [Google Scholar]
- 26.Duba A., Messiaen M., Boulangeat C., et al. Sexual harassment exposure and impaired mental health in medical students. The MESSIAEN national study. J. Affect. Disord. 2020;274:276–281. doi: 10.1016/j.jad.2020.05.100. [DOI] [PubMed] [Google Scholar]
- 27.Enquête VSS DP Final.pdf. Google Docs. 2021. https://drive.google.com/file/d/18D_7w2qSuUmNaLLDFerCqs_MF9YHn6gp/view?usp=embed_facebook Accessed September 14.
- 28.Roberge P., Doré I., Menear M., et al. A psychometric evaluation of the french Canadian version of the hospital anxiety and depression scale in a large primary care population. J. Affect. Disord. 2013;147(1–3):171–179. doi: 10.1016/j.jad.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 29.Australian Medical Association; 2020. Joint Statement - COVID-19 impact likely to lead to increased rates of suicide and mental illness.https://www.ama.com.au/media/joint-statement-covid-19-impact-likely-lead-increased-rates-suicide-and-mental-illness Accessed June 28, 2021. [Google Scholar]
- 30.Deng J., Zhou F., Hou W., et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frajerman A. Which interventions improve the well-being of medical students? A review of the literature. Encéphale. 2020;46(1):55–64. doi: 10.1016/j.encep.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 33.Barnett P., Arundell L.L., Saunders R., Matthews H., Pilling S. The efficacy of psychological interventions for the prevention and treatment of mental health disorders in university students: a systematic review and meta-analysis. J. Affect. Disord. 2020;280(Pt A):381–406. doi: 10.1016/j.jad.2020.10.060. [DOI] [PubMed] [Google Scholar]
- 34.Ardekani A., Hosseini S.A., Tabari P., et al. Student support systems for undergraduate medical students during the COVID-19 pandemic: a systematic narrative review of the literature. BMC Med. Educ. 2021;21(1):352. doi: 10.1186/s12909-021-02791-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bagby-Stone S. Creating space for well-being in medical school and beyond. Mol. Med. 2021;118(1):50–54. [PMC free article] [PubMed] [Google Scholar]
- 36.Wathelet M., Duhem S., Vaiva G., et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gasnier M., Choucha W., Radiguer F., et al. Acute objective severity of COVID-19 infection and psychiatric disorders 4 months after hospitalization for COVID-19. J. Clin. Psychiatry. 2021;83(1) doi: 10.4088/JCP.21br14179. [DOI] [PubMed] [Google Scholar]
- 38.Jacob L., Koyanagi A., Smith L., Bohlken J., Haro J.M., Kostev K. No significant association between COVID-19 diagnosis and the incidence of depression and anxiety disorder? A retrospective cohort study conducted in Germany. J. Psychiatr. Res. 2022;147:79–84. doi: 10.1016/j.jpsychires.2022.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pierce M., McManus S., Jessop C., et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7(7):567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Westreich D., Edwards J.K., van Smeden M., Comment on Williamson (OpenSAFELY): the table 2 fallacy in a study of COVID-19 mortality risk factors. Epidemiology. 2021;32(1) doi: 10.1097/EDE.0000000000001259. [DOI] [PubMed] [Google Scholar]
- 41.Westreich D., Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am. J. Epidemiol. 2013;177(4):292–298. doi: 10.1093/aje/kws412. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material