Abstract
Background
the ageing global population is living longer with complex health conditions addressed by multiple medications. Little is known about how older people manage these medications and associated packaging at home.
Objectives
to explore how older people manage the use of multiple medication and associated packaging in their process of self-care.
Methods
fifteen older, home-dwelling participants (mean age = 76.2 years) participated in this study. All participants used three or more daily medications and resided in Southern Sweden. Data were collected using photographs and written diaries completed by each participant over seven consecutive days, complemented by researcher-led interviews. Interviews and diary data were analysed using thematic analysis.
Results
six major themes emerged and are discussed: systematic organisation of medication, design of medication packaging, design of tablets, ease of package opening, emotional response to the need for medication, and environmental waste.
Conclusion
packaging plays an important role in protecting products and enabling easy storage, product longevity and transportation. Medication packaging is no exception. However, the design of medication packaging poses challenges for older people managing medications for their chronic health conditions at home. There is a need to facilitate the systematic management of multiple medications, especially for new medication regimes or changes in treatment. Design of both packaging and medication should be consistent for older users to avoid potential errors; difficulties opening packaging can potentially hinder adherence to treatment. This study highlights the need for patient-centred solutions and involvement of older people in a co-design process for medication and packaging design.
Keywords: Medication adherence, medication packaging, older people, packaging design, solicited diaries, qualitative research
Key Points
Greater attention should be given to patient-centred medication packaging to support self-care of older people with multiple medications at home.
Medication packaging should be designed with a systematic approach to reduce potential medication errors.
Practitioners can support older people by facilitating medication routines within the complexity of the home environment.
Co-designing with older people to promote patient-centred packaging design and improve understanding and use of medications.
Introduction
Life expectancy has increased globally. The world will see a shift from 703 million people aged 65 years and over in 2019 to 1.5 billion by 2050 [1]. Older age comes with the likelihood of experiencing multiple health conditions such as high blood pressure, diabetes and arthritis, [2, 3]. Consequently, polypharmacy (i.e. the use of five or more medications concomitantly [4],) tends to prevail in about 40–50% of the older people [5, 6], with an increased risk of poor health outcomes [7]. Multiple chronic conditions are predominantly managed by the older person in their home environment, highlighting concerns about how people cope with self-care and use numerous medications [8], their adherence to treatment [9] and the occurrence of medication errors [10, 11].
One important factor related to the management of medications by older patients is how these medications are packed. Packaging and older people have been investigated for accessibility for food and drink [12, 13] and for medication [14–16]. Medication packaging is traditionally designed with an emphasis on its protective functions to preserve the drug, in a highly regulated context with limited marketing functions [17]. This design approach is mostly not patient-centred and fails to comprehensively understand the patient’s needs [18]. Although attempts have been made to improve medication packaging accessibility [19], the lack of patient-centricity applied to packaging has historically perpetuated problems in medication use [20].
To date, studies examining older people and medication packaging design have favoured data collection methods based on physician/investigator observations and questionnaires about patient preferences [21]. Although these methods provide relevant data about which packaging designs tend to fail in terms of accessibility to medication, they do not investigate the complexity experienced by people when handling a multitude of packaging and dosage methods in their own homes. One study has been identified describing the use of medications in the home setting, providing a case study of medication packaging format and user experiences for terminally ill patients [22]. Yet, little is known about the daily habits older people follow to take their medication and the implications of using multiple medication packaging to manage chronic diseases to a person’s life and general well-being. A way forward is to look closely at the lived experiences of older people with their medication and its packaging and rethink these experiences with a patient-centred approach.
Therefore, this study aims to explore how older people experience the use of multiple medication and its packaging in their process of self-care. Findings from this study are particularly relevant when considering an ageing population that is increasingly responsible for self-care at home.
Materials and methods
Participants and recruitment strategy
This study included a non-probability convenience sample of older home-dwelling participants living in Southern Sweden. Those interested registered by providing their contact details, or by directly contacting the researcher via email or telephone. Criteria for joining the study were: being 65 years of age or over, using three or more different medications daily, being interested in taking pictures and completing a solicited diary for seven consecutive days.
Ten participants were recruited through an invitation letter sent electronically to coordinators of the Southern healthcare region and community facilities where older people gather for social activities. Three participants were recruited in a patient education centre at a local hospital, where patients and their relatives learn about their illness. Two further participants engaged in the study through snowballing. Each participant signed a form giving consent to voluntarily participate in the study and received a voucher card valued 200 SEK in recognition of their contribution.
Study design
The study follows a qualitative research design. Study participants were asked to report their experiences with self-care and medication packaging through a diary-interview method combined with photo-elicitation [23–25]. One pilot trial was conducted with one participant to test the diary-interview method. Amendments were made to the interview guide and instructions to the diary. The pilot data were not included in the final sample for analysis. A consistent single researcher met each participant to introduce the protocol and conduct the interviews. The study was approved by The Regional Swedish Ethical Review Authority.
Solicited diaries and photo-elicitation
Solicited diaries are written with awareness of the researcher and for a limited amount of time—different from unsolicited diaries, where an individual takes personal notes for their own reflection without a timeframe or intention of sharing its content to others. A solicited diary technique was selected as it is advantageous in research to track routines that could be difficult or not practical to observe for extended periods of time, or that would be altered in the presence of the researcher [25–27]. In addition to written text, solicited diaries were complemented with photography taken by the diarists. Photos can evoke ‘deeper elements of human consciousness’ than when only using words [28], helping the diarists to create a meaningful narrative of daily events and contributing to the familiarisation of the researcher with the lived experiences narrated [29].
In our study, participants were invited to complete a solicited diary for seven consecutive days. Seven consecutive days covered all the medication routines the participants usually follow and avoided loss of interest and monotony in participation [30]. Each participant received a diary kit containing: one instant-photo camera filled with film to take pictures of the medication and their routines to follow their prescribed treatment; one step-by-step manual with instructions about how to operate the instant-photo camera; a glue stick; a personal copy of the signed consent form and a diary. The diary was composed of one cover page and seven double-sided A4-sheets with prompt questions and a space to paste a picture for each day. Examples of prompt questions are: How do I feel today? Did I do anything today to solve a problem with one or more of my medication packaging? I took this picture because. . . The participants were not contacted while keeping their diary.
Interviews
Each participant was interviewed face-to-face on two occasions by the researcher: before and after the diary completion, either at the home of each participant or at the university facilities as preferred by the participant.
In the first interview, the participant received further information about the study and answered a series of set questions about their living circumstances and daily medication routines. Each participant was also instructed on the diary-keeping process and received the diary kit. Participants were given a demonstration about how to operate the instant camera at the end of the interview. The second interview was booked within 3 weeks of completing the diary. The purpose of this follow up interview was to: (i) to collect the diary; (ii) to ask participants about their experience of completing the diary and (iii) to allow the participants to discuss their note-taking process and the meaning of the photos [24].
Data management and analysis
Data analysis followed the six steps for qualitative thematic analysis [31]. For the diaries, all pictures taken by the diarists were scanned and stored digitally. Text from the diaries was typed into one spreadsheet, together with a short description of each picture, helping two researchers to read and code independently the entire diary data. The two researchers then compared their themes in an iterative process. A third researcher worked as a critical auditor, questioning the themes and subthemes. After several rounds of discussion, final coding descriptors emerged. All researchers have considerable training and more than 5 years of experience in qualitative methods and research of how packaging is handled by older people.
For the interviews, the audio was recorded and transcribed verbatim. The interview transcripts were imported in NVivo (QSR International), read entirely at least once and coded by one researcher based on the themes from the diaries.
Quality assessment
This study follows quality criteria for qualitative research to assure its trustworthiness [32]. The design of the study was based on data triangulation using multiple sources of evidence (interviews, diary notes, field notes and photographs) to provide credibility to the findings. The study was pilot-tested and could be replicated by using the detailed description of the study setup and participants’ selection criteria, as well as the pre-formatted diary with prompt questions. To reduce researcher bias, participants were responsible for taking the photos and making notes in the diaries, with a follow-up interview to assure participants they were allowed to explain their insertions in the diary. Findings were based on the digitalised content of diaries, followed by a coding scheme linked with data and illustrative quotes.
Results
Participants
Fifteen participants volunteered for this research, 10 women and 5 men (mean age = 76.2 years; range = 65–88 years). At the time of the study, 10 respondents used up to 7 different medications every day, whereas 5 respondents had up to 15 daily medications. Medication regimens included prescribed tablets taken for an array of health issues, for example, high-blood pressure, blood thinning, pain, cholesterol, diabetes. For further detailed data, see Supplementary Table 1.
Themes and sub-themes from interviews and diaries
The collation of participant data from the interviews and diaries fell into six key themes with several sub-themes (Table 1 and Supplementary Table 2).
Table 1.
Description of themes and sub-themes
| Themes | Sub-Themes | Description |
|---|---|---|
| Systematic organisation of medication | • Routine | Having a regular routine to systematically manage medication |
| • Dosing box | Use of dosing box (i.e. dosette) to organize medication | |
| • Visual cues | Using visual cues as reminders to take medication | |
| • Auditory cues | Using auditory cues as reminder to take medication | |
| • Assistance | Help from spouse to access and manage medication | |
| Design of medication packaging | • Variety of packaging design | Same medication can be presented in different package formats |
| • Cues on medication use | Poor intuitive design leading to confusion about how to open or use medication | |
| Design of tablets | • Shape and colour | Consistent shape and colour assist recognition of medication |
| • Size | Annoyance regarding inappropriate size of tablet (too big or too small) | |
| • Embossing | Identification on the tablet as a useful attribute | |
| Ease of package opening | • Child-resistant closures (CRCs) | Difficulty opening CRCs |
| • Preference for bottles over blister packages | Bottles easier to access than pushing tablets out of blister packages | |
| • Strategies and tools to open packages and access medication | Variety of household tools are used to open and access medication | |
| Emotional response to need for medication | • Treatment concerns | Distress about treatment – difficulty renewing prescriptions; communication difficulties with and between health providers; medications that cannot be taken together |
| • Side effects | Need to understand side effects; side effects impact on quality of life | |
| • Impact on perception of self | Need to take medication distresses participants; seeing self as a ‘patient’ | |
| • Empathy for others taking medication | Concern for other people needing greater amount of medication | |
| Environmental waste | • Concern about waste | Waste from medication packaging as a concern for participants |
| • Wasted space in bottle | ‘Empty’ bottle space could be used for tablets rather than using more containers |
Systematic organisation of medication
Routines
All participants reported they had established a system to manage their medication, mostly based on routines embedded in their daily living routines:
I take [the medications] when I give food to the cat, I sit down for coffee and pick up the newspaper, so when I have done that, I take my breakfast and then in connection with it I eat my tablets. (P8)
In the morning, I take them [the medications] before I eat breakfast. And, in the evening, before I have dinner. (P12)
Dosing box
All but two participants reported using a dosing box (i.e. dosette) to organize their medications (Supplementary Figure 1). The dosette is usually made of hard plastic, with cavities for each day of the week, where tablets can be placed. Participants commented organising their dosettes usually on Sundays to get ready for the next 1 or 2 weeks. Setting up the dosette gave confidence with the medication management, avoiding any additional burden to handle multiples packages along the week:
I have a dosette. […] Morning, noon, and evening. Every Sunday, in the morning, I sort everything, and then it's easier every day [to take the medications]. (P10)
However, the dosette was not always optimal with the daily dosage, being considered unnecessary for just a few medications or too small to contain too many tablets. P15, for instance, felt organising a dosette was difficult and instead placed the daily dose in another container. Even though convenient, P10 thought organising the dosette was time consuming (‘It takes me about one hour to sort and divide up all the weekly medications’). Participants also used other boxes to store the medications in their original packaging in a safe place, as packaging occupied a lot of space when medications were not in the dosette.
Visual cues
Participants noted that it was important to have visual cues associated with daily routines to manage their medication (Figure 1). A common example was to place their medication on the breakfast table. Another example was placing the medication close to toothbrush in a cabinet in the bathroom for evening routines:
Figure 1.

Use of cues. Diary notes: Top left: ‘I always remember the medications I should take in the evening when I prepare to brush my teeth’ (P11). Top right: ‘Weekly dosette filled and serving glass which I fill afterwards’ (P14). Bottom left: ‘A medication I take together with another one. It tastes bad, so I take it with juice.’ (P5). Bottom right: ‘It [the picture] shows how I dose my medications daily’ (P2).
I pour medication the night before into a glass. Then I know I'll take them in the morning. I always put the dose in a small glass, so that I do not forget it. (P14)
Auditory cues
Those participants with more complex routines (e.g. multiple medications at different times during the day) reported using an alarm on their mobile phones. However, as commented by P3, using the alarm was not always optimal as while it signals the time to take the medication, it does not provide information about which medication to take. Furthermore, if she were not proximal to her medications when the alarm sounded, she could easily forget to take the medication. P7 mentioned about using a smart watch set to vibrate when it was time for one of her Parkinson’s medications. No other technological devices or any mobile applications were reportedly used as cues for medication use.
Assistance
No participants received external home health care to manage their medication. Pharmacists were mentioned as a source of instruction when starting a treatment or a new medication. However, most of the assistance came from other family members, mainly the spouse. Findings indicated a difference between how male and female participants asked for assistance at home. For male participants P1 and P14, the wife had a quality control role, helping to organize the medications into the dosette or reassuring the medications were taken correctly. For female participants, spouses were asked to remove tablets from hard-to-open/hard-to-press packaging.
Design of medication packaging
Variety of packaging design
Participants’ medications were mainly packed in either a hard plastic bottle, push-through blister pack or peel-off blister pack. To lesser extent, participants had medications administered as creams packed in metallic tubes, or eye-drop medication in multi-dose plastic container closure. Packaging design varied from being a source of recognition of the medication by participants or a source of confusion.
One common problem mentioned was medication substitution by the pharmacy for another manufacturer/brand—so that participants received an equivalent medication with a different packaging design and most likely different name to the brand to which they were accustomed.
Another common problem was to have too similar packaging design, making differentiation between medication and strengths of medication difficult, increasing the risk of medication errors, as highlighted by one participant:
It's 4 mg that I should have now, and 8 mg that I should not have. So, I went to the closet, fetched a box and looked at it and saw properly which one I should take and re-marked it then in the pack with a large pen: 4 mg. Colours are the same on the small tablets, the colour is blue just the same, and the jar is just the same. You have to be super clever to remember and fix everything. You need to be healthy to be sick. You have to be super healthy; you must not have even a little touch of stroke. (P9)
Cues on medication use
Notes in the diaries showed that packaging could facilitate medication use when cues were provided in a simplified manner. Figure 2 presents a collection of photos where use of packaging and medication were perceived differently. The photo on the left depicts instructions printed on the outer box simplifying medication use. Conversely, the photo in the centre shows a multitude of leaflets, whereas the photo on the right outlines the many steps necessary just to open the packaging. The lack of cues on use irritated participants, as commented:
Figure 2.

Cues on medication use. Diary notes: Left: ‘It is an exemplary list of important tasks about the content and handling. Easy to find, easy to read and to grasp. This should be a standard for all types of medications’ (P2). Centre: ‘How much a person reads, comprehends, continuity, credibility, necessity, identification etc. Is that too much information in the current accelerated information flow? How to follow that up?’ (P1). Right: ‘Such a long description. Just to open the lid you need 1, 2, 3, 4 pictures plus text. I think it’s bad’ (P5).
The leaflet you don’t know in which side it is. It's annoying. Sometimes I do this [He makes a cross on the packaging with a pencil, to identify which side the leaflet is]. (P2)
Design of tablets
Shape and colour
Participants with stable medication regimes commented they ‘knew’ their tablets by shape and colour, highlighting the importance of consistent tablet design. Difficulties were noted when a medication was changed by the doctor or substituted for a different brand by the pharmacy, with participants reporting uncertainty that they were taking the correct medication:
This [medication] used to be round and white, now they are oblong and blue. I do not like when they change colour and shape, or name. Sometimes, they say [at the pharmacy], ‘Do you want to switch to one that is cheaper?’, And then you ask: ‘How much is the difference between them?’. It can be between 3 Kr or 50 Kr. (…) It may be better to stick to what you had before. (P10)
Size
Comments also emerged from participants about the size of medication—large tablets being difficult to swallow and small tablets difficult to locate and very difficult to break in half with tablets disintegrating when half doses were required:
This is my calcium tablet. They are difficult to swallow. […] I took this picture because these tablets are so big. Huge. I think they [manufacturers] could do it smaller. (P3)
Embossing
Some medication is embossed, assisting in medication recognition. One participant commented that the embossing helped him identify the medication and avoid mixing it with other medication when the medication was already removed from the packaging. He suggested also that the packaging should clearly depict the tablet with the embossing, so patients could easily identify and recognize their medications.
Ease of package opening
Child-resistant containers
Child-resistant containers (CRCs) were commonly considered difficult and frustrating to open by participants, demanding extra hand strength or additional steps to open the package (e.g. press and turn):
When you open, you have to press and you have to screw. You know, before I got sick, I did everything with the right hand. Now, those fingers are asleep and I am weak in my hands and arm. I cannot open. Therefore, my husband helps me to open it. Then, once it has been opened you cannot screw it on. (P6)
Preference for bottles over blister packages
Many of the participants photographed their preferred packaging format, with bottles with no child-resistant closures strongly preferred over blister packages. Bottles allowed easier access to the medication and for redistributing tablets into the dosettes. Participants also reported keeping alternative (preferred) packaging or even older medication packaging to substitute for those they considered difficult to deal with daily:
When I get a blister, I push them in(to) the jar right away, altogether, and sometimes it can take half a morning on Sunday. (P10)
Strategies and tools to open packages and access medication
Participants diarised a range of strategies to overcome difficulties opening the packaging and accessing the tablets it contained. For example, participants reported purposefully not closing the CRC containers completely so they could access it easily.
Another participant had several tools to overcome the difficulties accessing her 15 medications, using nutcrackers to turn and open plastic bottles (Figure 3) and pliers to remove plastic rings when opening medication bottles for the first time:
Figure 3.
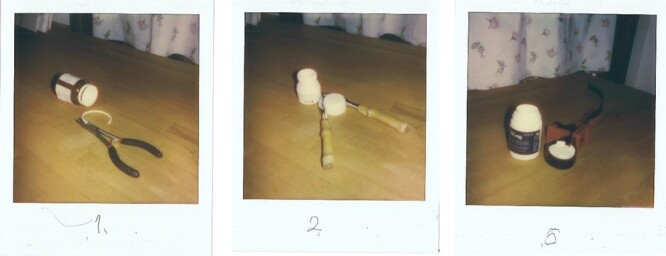
Examples of tools used to open the packaging.
I have no medication that I can get in without tools. Of the fifteen I have, there is only one I can get into (P3).
When reflecting about all the difficulties faced with her medication packaging, she added:
[…] Someone with rheumatism or arthritis in the fingers should be together from the start in the design of packaging (P3).
Removing tablets from blister packages also led to use of tools and specific techniques. Participants reported using their fingernails, thumb, or a household tool to break the foil and remove the tablet, often decanting the tablets into an easier to open bottle:
I also have blisters. And I usually press my thumbs there. Thumbs and nails. And I do it all at once, fourteen (tablets) at a time. (P13)
Emotional response to need for medication
Treatment concerns
Participants reported distress when they could not get a prescription renewed automatically. One participant noted the lack of communication between different healthcare providers, which resulted in the patient unable to obtain the prescribed medication:
It feels that care providers, such as primary care, sometimes do not know if a medication is sold out, they have not received any information, [they] write up the medication even though it is over. The pharmacy knows nothing either and knows nothing about delivery time. And the patient... the patient can have a time delay; they cannot follow up the treatment. I feel that there is not a real routine in that communication, therefore I call for three different groupings. So, I wrote that I experienced it badly sometimes that caregivers don’t know if medication is sold out and what is the replacement. […] How should the care patient then act? (P1)
Side effects
Participants with recent new medication regimes were disturbed by the side effects of their medications. Their concern was amplified by not knowing which of their multiple medications was the one causing the issues. This situation not only affected their treatment, but their daily routine and general well-being. The narratives on the diaries showed the distress caused, with an indication of relief once the situation was restored:
I could not go anywhere, the only time I felt good, I slept. And I woke up and it itched. […] I did not want any clothes; a fleece sweater was good. Soft. So that's why I could not get started. (P9)
Participants noted that although established medication regimes rarely changed, when changes did occur, there were concerns about medication interactions and potential side effects:
I have a system when it comes to medications. If I receive two different medications, I first start with one and see how it reacts. Seems good. I follow the doctor's prescription. If it did not work, I make contact [with healthcare provider]. If it goes well, I will take the next prescription and then put it together […] Otherwise, I cannot find out what is wrong because I get side effects so easily. (P5)
Impact on perception of self
Most of the participants in the study with established medication regimens expressed sadness about the quantity of medications they needed, reporting they wished to use less medication in the future. A few participants with recent cerebrovascular accidents (CVAs) described their transition to a ‘new me’. Seeing and dealing with the medication and its packaging seemed to be an important part of this process to gain maximum recovery and prevent further CVAs. Despite that, P6 found it depressing to see all the medication she needed to take, writing in her diary: ‘I have not thought health was the most important thing in life before my stroke.’ Frustration also emerged when medication packaging was hindering participants in their self-care. An outstanding example was P13, who took a self-portrait and described:
Me. 83 years and capable of taking care of our household without help. So why should I need help with medication packaging?
Empathy for others taking medication
When participants reflected on their own difficulties, they often expressed concern and empathy for even older patients with more severe conditions or more complex regimens:
I am not the weakest. There are many at my age that are much worse. If you have less strength [in the hands, to open the medication packaging]; and most of the people at my age take a lot of medications. Why do they do it like that? ["They" refers to the companies producing the packaging] (P13).
Environmental waste
Concern about waste
Concerns about the environmental waste from the large amount of medication packaging was noted in the diaries, even though there were no specific questions asked in the study (Figure 4). Participants expressed annoyance with too many packages; concerns about the extensive use of plastics; and difficulties in recycling packaging with combined materials (e.g. blister packages made of aluminium foil and plastic):
Figure 4.

Packaging waste photographed by participants. Diary notes: Left: ‘Lots of rubbish! Many medications that you do not know how to sort the waste. I think medication packaging should tell how they should be sorted’ (P9). Centre: ‘Pile of rubbish after I have sorted my medications into the dosette’ (P10). Right: ‘My medication packaging in plastics. The plastic bottles are filled just to 1/3, so unnecessary!’ (P6).
I think paper is the best. It feels better. There's too much plastic, the lid and so on. There are a lot of thoughts now that you should not have so much plastic. (P6)
Wasted space in bottle
Participants also commented on the wasted space in medication bottles and how it led to increased environmental waste as well as taking up space in their medication cupboards:
The doctor prescribes 300 [tablets] each time, but sometimes I get 6 small jars with 50 [tablets] in each. And then when I get home, I open them all, because there's room for 100 in these jars. (P10)
Discussion
With a rapidly ageing population relying on medication for their longevity and independence, multiple medication regimens are commonplace [33]. This study focused on the experiences of older people managing multiple medications and associated packaging in their process of self-care.
The main findings highlight participant development of individual systems to manage multiple medications, aided by visual/auditory cues and use of dosettes. Although dosettes are intuitive to use and easy to access, they have limitations [34]. To use dosettes effectively, patients must have reasonable cognitive and organisational skills, memory recall, problem-solving abilities and dexterity. In a British report [22], the terminally ill patient required his medication to be decanted from the dosette by his wife due to difficulty handling the tablets with the dosette. In addition, dosettes replace the original medication packaging, meaning it can be difficult to obtain further information about the medication. Dosettes also may not work for medication that is sensitive to moisture or other conditions that only the original packaging can provide.
This study is consistent with previous laboratory work, finding participants had recurrent difficulty opening containers to access their medication. This was particularly true for older females and patients with physical restrictions, such as rheumatoid arthritis [35, 36]. To overcome hindrances imposed by a life full of medications, participants adopted a series of coping strategies, which come with a range of risks from moderate discomfort (e.g. pain in the hands) to more severe consequences (e.g. injuring themselves) [37].
Consistent packaging and tablet design were identified as important for patients with several medications to manage, as this allowed them to become familiar and confident with their medication intake. Conversely, variations in tablet formats and packages created confusion, for example when different strengths of the same medication were not clearly differentiated by the packaging design. These results are also consistent with previous research, which found that similar packaging and medication design for distinct medication led patients to take the wrong medication [38]. What was new and, quite particular to this study, was that participants could and did comment on how these difficulties impacted on their perception of self. In their diaries and interviews, our diarists reflected on the dissonance created by difficult medication packaging, as while participants felt otherwise fit and capable in their lives, the issues posed by the medication packaging left them feeling vulnerable.
In addition, the diary commentary covered social, environmental and economic concerns with medication packaging use. For example, participants revealed their concerns about ‘other older patients’, who they felt would have even greater accessibility issues than themselves. Waste generated by sub-optimal packaging design (blister packages; wasted space in bottles) was widely discussed as undesirable. Economic issues of cost saving by the pharmacy providing alternate packaging created usability issues for the participants. These findings highlight the complexity that surrounds medication adherence [39], and the emotional efforts self-care and long-term treatment demand from patients.
Implications for health care practice and packaging development
Healthcare practitioners need to be aware of the routines established by patients with multiple medications to support these systems and reduce the risk of errors. Researchers have suggested that home visits might be necessary to identify medication issues [7], especially for ‘brand new’ patients undertaking a process of accepting the need for medication. This is not only a matter of taking the medication correctly, but also of incorporating the treatment into personal and daily life for better patient outcomes.
Our study shows a series of preferences by older patients that are not always fulfilled by their current medication packaging. One strong preference was for bottles over blisters. Pharmaceutically, blisters offer individualized protection and good shelf-life for medications. However, blisters are a well-known source of frustration and challenge for older patients, especially peel-off blister packages [40, 41]. Another preference was for consistent packaging and tablet design. Our participants had good cognitive ability and no major visual impairments, which allowed them to rely on visual aspects of the medication and its packaging to differentiate and recognize discrete medications. Currently, pharmaceutical manufacturers can freely decide shape, colour and size attributes for their medications. The study findings suggest that older people’s needs can be used as the platform for medication packaging development, based on the principle that by meeting the needs of this population, a wider range of patients will be able to use the packaging designs [42]. To achieve optimal outcomes, it is essential that older people be part of the packaging design process in both a consultative role assessing packaging concepts, as well as in the generation of early concepts and ideas that fit their daily routines [43].
Finally, packaging has received attention in the community for the extensive use of materials and the waste generated after household products are consumed [44]. Participants’ feedback in this study underlines the level of concern in the community around sustainable packaging practices and the opportunity for pharmaceutical manufacturers to modify packages, and for regulators to develop and review guidance in this area.
Limitations
There are limitations to this study. Study participants were purposively recruited and represent a convenience sample. As such, they may not be representative of the wider population or vulnerable population groups. The study was conducted in the participant’s home and no controls were in place for potential damage to medication or packaging, for example with the use of scissors or ambient storage temperature/humidity. In addition, this is a small sample of older adults, limiting the transferability of these findings. However, due to the exploratory nature of this research, the findings of this study provide a basis for further research and methodology development that considers the complexities of medication use at home.
Conclusion
This study undertaken with older people reporting their use of medication in their homes indicates the need for patient-centred solutions for medication and packaging design and highlights the importance of involvement of older people in a co-design process. Development of medication packaging demands a systematic approach, underpinned by the understanding of the context of medication use by older people. Consideration about the complexity of the home environment, the use of established routines for managing medications, as well as packaging preferences, has the potential to reduce the risk of medication errors and increase adherence for these patients—a vital point for clinicians and practitioners coordinating treatment for older patients. This is a topic where further exploration is necessary, and research can be expanded to a larger group of older adults, ideally in a co-design approach.
Supplementary Material
Acknowledgements
The authors thank all the participants who agreed to take part in the study.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
Kamprad Family Foundation for the research grants received for the project Patient-centred pharmaceutical packaging design for enhanced life quality of older people (reference number: 20180091). The funder played no role in the design, execution, analysis and interpretation of data, or writing of the study.
References
- 1. United Nations (Department of Economic and Social Affairs Population Division) . World Population Ageing 2019: Highlights. New York: United Nations, 2019. [Google Scholar]
- 2. World Health Organization . Ageing and health: Key facts 2018. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- 3. Denton FT, Spencer BG. Chronic health conditions: changing prevalence in an aging population and some implications for the delivery of health care services. Can J Aging 2010; 29: 11–21. [DOI] [PubMed] [Google Scholar]
- 4. Jyrkka J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S. Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons. Drugs Ageing 2009; 26: 493–503. [DOI] [PubMed] [Google Scholar]
- 5. Gao L, Maidment I, Matthews FE, Robinson L, Brayne C. Medication usage change in older people (65+) in England over 20 years: findings from CFAS I and CFAS II. Age Ageing 2018; 47: 220–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Charlesworth CJ, Smit E, Lee DSH, Alramadhan F, Odden MC. Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Gerontol 2015; 70: 989–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sorensen L, Stokes JA, Purdie DM, Woodward M, Roberts MS. Medication management at home: medication-related risk factors associated with poor health outcomes. Age Ageing 2005; 34: 626–32. [DOI] [PubMed] [Google Scholar]
- 8. Wong AKC, Wong FKY, Chang K. Effectiveness of a community-based self-care promoting program for community-dwelling older adults: a randomized controlled trial. Age Ageing 2019; 48: 852–8. [DOI] [PubMed] [Google Scholar]
- 9. Menditto E, Cahir C, Aza-Pascual-Salcedo Met al. Adherence to chronic medication in older populations: application of a common protocol among three European cohorts. Patient Prefer Adherence 2018; 12: 1975–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Patton DE, Cadogan CA, Ryan Cet al. Improving adherence to multiple medications in older people in primary care: selecting intervention components to address patient-reported barriers and facilitators. Health Expect 2018; 21: 138–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization . Medication errors: Technical Series on Safer Primary Care. Geneva: World Health Organization, 2016. [Google Scholar]
- 12. Bell AF, Walton K, Chevis JSet al. Accessing packaged food and beverages in hospital. Exploring experiences of patients and staff. Appetite 2013; 60: 231–8. [DOI] [PubMed] [Google Scholar]
- 13. Yoxall A, Bell A, Gee K, Lecko C. Single portion packaging and the use of user test protocols to determine patient accessibility. J Nutr Gerontol Geriatr 2019; 38: 387–96. [DOI] [PubMed] [Google Scholar]
- 14. Atkin PA, Finnegan TP, Ogle SJ, Shenfield GM. Functional ability of patients to manage medication packaging: a survey of geriatric inpatients. Age Ageing 1994; 23: 113–6. [DOI] [PubMed] [Google Scholar]
- 15. Braun-Münker M, Ecker F. Ease of opening of blistered solid dosage forms in a senior citizens target group. Int J Pharm 2016; 512: 412–5. [DOI] [PubMed] [Google Scholar]
- 16. Philbert D, Notenboom K, Bouvy ML, Geffen ECG. Problems experienced by older people when opening medicine packaging. Int J Pharm Pract 2014; 22: 200–4. [DOI] [PubMed] [Google Scholar]
- 17. Lockhart H, Paine FA. Packaging of Pharmaceuticals and Healthcare Products. London: Chapman and Hall, 1996. [Google Scholar]
- 18. Lorenzini GC, Olsson A. Towards patient-centered packaging design: an industry perspective on processes, functions, and constraints. Packag Technol Sci 2018; 32: 59–73. [Google Scholar]
- 19. Rowson J, Sangrar A, Rodriguez-Falcon Eet al. Rating accessibility of packaging: a medical packaging example. Packag Technol Sci 2014; 27: 577–89. [Google Scholar]
- 20. Lorenzini GC, Hellström D. Medication packaging and older patients: a systematic review. Packag Technol Sci 2017; 30: 525–58. [Google Scholar]
- 21. Drumond N, Riet-Nales DA, Karapinar-Çarkit F, Stegemann S. Patients’ appropriateness, acceptability, usability and preferences for pharmaceutical preparations: results from a literature review on clinical evidence. Int J Pharm 2017; 521: 294–305. [DOI] [PubMed] [Google Scholar]
- 22. Pollock K, Latif A, Wilson E, Crosby V, Caswell A, Avery A, et al. Managing medicines for patients with serious illness being cared for at home. HS&DR Researcher Led; 2021, [15/70/101].https://www.journalslibrary.nihr.ac.uk/hsdr/hsdr09140#/abstract. [PubMed] [Google Scholar]
- 23. Alaszewski A. Using Diaries for Social Research. London: Sage, 2006. [Google Scholar]
- 24. Barlett R. Modifying the diary interview method to research the lives of people with dementia. Qual Health Res 2012; 22: 1717–26. [DOI] [PubMed] [Google Scholar]
- 25. Zimmerman DH, Wieder DL. The diary interview method. Urban Life 1977; 5: 479–99. [Google Scholar]
- 26. Milligan C, Bingley A, Gatrell A. Digging deep: using diary techniques to explore the place of health and well-being amongst older people. Soc Sci Med 2005; 61: 1882–92. [DOI] [PubMed] [Google Scholar]
- 27. Verbrugge LM. Health diaries. Med Care 1980; 18: 73–95. [DOI] [PubMed] [Google Scholar]
- 28. Harper D. Talking about pictures: a case for photo elicitation. Visual Studies 2002; 17: 13–26. [Google Scholar]
- 29. Kantrowitz-Gordon I, Vandermause R. Metaphors of distress: photo-elicitation enhances a discourse analysis of parents’ accounts. Qual Health Res 2016; 26: 1031–43. [DOI] [PubMed] [Google Scholar]
- 30. Jacelon CS, Imperio K. Participant diaries as a source of data in research with older adults. Qual Health Res 2005; 15: 991–7. [DOI] [PubMed] [Google Scholar]
- 31. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 32. Stenfors T, Kajamaa A, Bennett D. How to… assess the quality of qualitative research. Clin Teach 2020; 17: 596–9. [DOI] [PubMed] [Google Scholar]
- 33. Wise J. Polypharmacy: a necessary evil. BMJ 2013; 347: f7033. [DOI] [PubMed] [Google Scholar]
- 34. Levings B, Szep S, Helps SC. Towards the safer use of dosettes. J Qual Clin Pract 1999; 19: 69–72. [DOI] [PubMed] [Google Scholar]
- 35. Beckman A, Bernsten C, Parker MG, Thorslund M, Fastbom J. The difficulty of opening medicine containers in old age: a population-based study. Pharm World Sci 2005; 27: 393–8. [DOI] [PubMed] [Google Scholar]
- 36. Sormunen E, Nevala N, Sipilä S. Critical factors in opening pharmaceutical packages: a usability study among healthcare workers, women with rheumatoid arthritis and elderly women. Packag Technol Sci 2014; 27: 559–76. [Google Scholar]
- 37. Notenboom K, Beers E, Riet-Nales DAet al. Practical problems with medication use that older people experience: a qualitative study. J Am Geriatr Soc 2014; 62: 2339–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ward J, Buckle P, Clarkson PJ. Designing packaging to support the safe use of medicines at home. Appl Ergon 2010; 41: 682–94. [DOI] [PubMed] [Google Scholar]
- 39. Yap AF, Thirumoorthy T, Kwan YH. Systematic review of the barriers affecting medication adherence in older adults. Geriatr Gerontol Int 2016; 16: 1093–101. [DOI] [PubMed] [Google Scholar]
- 40. Mühlfeld L, Langguth P, Häusler H, Hagels H. Influence of blister package design on usability among older adults. Int J Clin Pharm 2012; 34: 553–60. [DOI] [PubMed] [Google Scholar]
- 41. Geffen EC, Meuwese E, Philbert D, Bouvy ML. Problems with medicine packages: experiences reported to a Dutch medicine reporting system. Ann Pharmacother 2010; 44: 1104–9. [DOI] [PubMed] [Google Scholar]
- 42. Goodman-Deane J, Waller S, Bradley M, Yoxall A, Wiggins D, Clarkson PJ. Designing inclusive packaging. In: Burgess P, ed. Woodhead Publishing Series in Food Science, Technology and Nutrition: Integrating the Packaging and Product Experience in Food and Beverages. Woodhead Publishing, 2016; 37–57. [Google Scholar]
- 43. Lorenzini GC, Olsson A, Larsson A. Listening to current practice: patient involvement in the pharmaceutical packaging design process. J Appl Packag Res 2021; 13: Article 4. [Google Scholar]
- 44. Nemat B, Razzaghi M, Bolton K, Rousta K. The role of food packaging design in consumer recycling behavior: a literature review. Sustainability 2019; 11: 4350. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


