Abstract
Prurigo pigmentosa (PP) is a rare inflammatory dermatosis of unknown etiology that primarily affects adolescents and young adults. It is typically characterized by a pruritic eruption of erythematous papules on the trunk and neck that evolves into reticulate hyperpigmentation upon resolution of the inflammatory phase of the rash. It has been associated with various triggers, including the metabolic state of ketosis. Interestingly, the recent increase in popularity of the ketogenic diet for weight loss has led to an increased number of PP cases reported in the literature. We present a case of PP in a 21-year-old Hispanic man, which erupted during strict adherence to a ketogenic diet. We conducted a literature review and identified 19 other cases of PP related to ketogenic diet. While PP has historically been reported primarily in Asia, we found cases occurring in patients of Middle Eastern, Caucasian, Hispanic, Asian, and African descent. On average, the rash presented 31 days after initiating the diet and subsided 18 days after diet cessation. Most cases were treated with an oral tetracycline and resolved with residual hyperpigmentation. We present this information to highlight the increasing association of PP with the ketogenic diet so that early diagnosis and treatment and optimal patient outcomes may be achieved. Dermatologists should be aware of the timing of rash onset and resolution in relation to the diet.
Prurigo pigmentosa (PP) is a rare inflammatory dermatosis that has historically been reported in Japanese patients. It is characterized by an initial inflammatory stage with pruritic papules in a reticulate distribution, which later evolves into a hyperpigmented stage with corresponding changes on histopathology. While the etiology is unknown, various mechanical, hormonal, and metabolic triggers have been identified, including ketosis. With the rise in popularity of the ketogenic diet in recent years, there has been an emergence of PP cases worldwide. The ketogenic diet is a very low-carbohydrate, moderate-protein, high-fat diet that restricts carbohydrate intake to under 50 grams daily. The goal of this diet is to induce a metabolic state that mimics starvation and promotes the breakdown of fat into ketone bodies as an alternative energy source, resulting in the purported benefits of weight loss and reduced risk of cardiovascular disease and Type 2 diabetes mellitus.1 We present a case of ketogenic diet-induced PP in a Hispanic patient and review the literature on this interesting diagnosis.
CASE REPORT
A 21-year-old otherwise healthy Hispanic man presented to dermatology clinic with a pruritic rash on his central chest and upper back, which had been present for three weeks. He was not on any medications and denied using any new topical products prior to rash onset. He had been on a ketogenic diet for two months with a resultant weight loss of 20 pounds. He stopped dieting three days prior to presentation and noted a slight improvement in the appearance of the rash.
On exam, he had erythematous to hyperpigmented papules coalescing into reticulated thin plaques on his central chest and upper back (Figures 1 and 2). He reported extreme pruritus and was actively scratching during the skin exam. Skin biopsy showed spongiosis, superficial perivascular infiltrate of eosinophils, lymphocytes, and rare neutrophils, as well as rare melanophages in the papillary dermis (Figure 3). A diagnosis of PP was made, and the patient was treated with oral doxycycline 100mg twice daily and instructed to avoid resuming a ketogenic diet. Within two weeks, the pruritus resolved and the erythematous plaques evolved into asymptomatic, hyperpigmented, reticulated patches.
FIGURE 1.
Erythematous to hyperpigmented papules and reticulated thin plaques on the central chest
FIGURE 2.
Erythematous to hyperpigmented papules coalescing into reticulated thin plaques on the central back
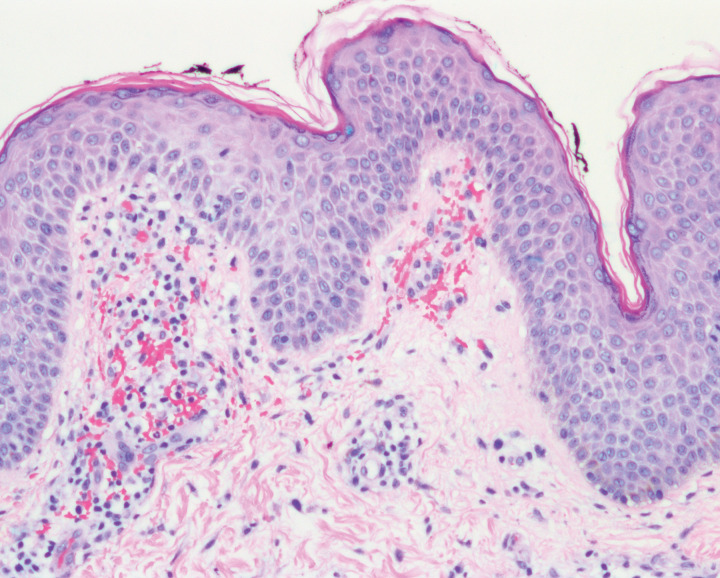
FIGURE 3.
Histologic section showing spongiosis, superficial perivascular infiltrate of eosinophils, lymphocytes, and rare neutrophils
DISCUSSION
PP was first described by Nagashima et al2 in 1971 as an eruption of erythematous pruritic papules coalescing in a reticular pattern that later resolved with postinflammatory hyperpigmentation (PIH). Most cases were reported in the Japanese population, occurring in female patients twice as commonly as male patients, with an average age of 24 years at presentation.3,4 The histopathologic features of PP depend on the timing of the biopsy, with early stages showing superficial perivascular neutrophilic infiltrate and later stages characterized by spongiosis and necrotic keratinocytes, followed by eosinophilic and lymphocytic infiltrate with melanophages in the papillary dermis.3 Our patient presented with a later stage of PP based on clinicopathologic correlation, likely due to the termination of his ketogenic diet three days prior to biopsy.
The pathogenesis of PP is unknown but proposed triggers include sweating,2,3 friction from clothing, rubbing,4 acupuncture, atopic dermatitis,5 diabetes mellitus,6 anorexia nervosa,7 rapid weight loss, contact dermatitis,8 pregnancy,9 Helicobacter pylori (H. pylori) infection,10 and ketosis.4,5,6 Ketosis may be precipitated by a ketogenic diet, fasting, insulin-dependent diabetes mellitus,11or bariatric surgery.12 Researchers have postulated that ketone bodies might induce perivascular neutrophilic inflammation and play a role in the development of PP.12 First-line treatment is oral minocycline or doxycycline, which are thought to be effective due to their inhibition of neutrophil chemotaxis and function.13
A review of the literature identified 19 cases of PP induced by a ketogenic diet from the years 2015 to 2021 (Table 1).14-27 Patients ranged in age from 16 to 43 years, with a mean age at diagnosis of 24 years. There was a strong female predominance (79%), which could be due to higher prevalence of dieting behaviors among young women compared to young men. The majority of patients were Asian (32%) and Middle Eastern (32%), followed by Caucasian (11%). Most patients were otherwise healthy, with the exception of two cases, one of whom was diagnosed with asthma two weeks after the eruption of PP and the other of whom was on a ketogenic diet for management of intractable seizures. These comorbidities were not thought to be associated with the development of PP.
TABLE 1.
Clinical characteristics of patients with ketogenic diet-induced prurigo pigmentosa
| CASE | SEX/AGE | ETHNICITY | RASH DISTRIBUTION | RASH ONSET AFTER DIET INITIATION | TREATMENT | OUTCOME |
|---|---|---|---|---|---|---|
| 114 | M/17 | Caucasian | Trunk | 2 weeks | Doxycycline 100mg BID x 2 months, D/C diet | Resolution in 1 week with minimal PIH |
| 215 | F/16 | Middle Eastern | Trunk, neck | 1 month | Doxycycline 100mg QD x 2 months | Resolution in 10 days with PIH |
| 316 | F/43 | Chinese | Trunk | 3 weeks | Diphenhidramine, loratadine, topical steroids, D/C diet | Eventual resolution after D/C diet |
| 416 | M/18 | Japanese | Trunk, neck | 9 days | Increased carbohydrate intake to 90gm/d | Resolution in 18 days with PIH |
| 517 | F/25 | Middle Eastern | Trunk | 3 weeks | Clobetasol propionate BID, topical antibiotic, topical antifungal, D/C diet | Resolution in 2 months with PIH |
| 618 | F/26 | Middle Eastern | Trunk | 3 months | Doxycycline 100mg QD x 1 month, D/C diet | Resolution in 2 weeks with PIH |
| 718 | M/20 | Middle Eastern | Neck | 2 months | Doxycycline 100mg QD x 1 month, D/C diet | Resolution in 2 weeks with PIH |
| 818 | F/22 | Middle Eastern | Trunk, neck | 4 months | Doxycycline 100mg QD x 1 month, D/C diet | Resolution in 2 weeks with PIH |
| 919 | M/37 | N/A | Trunk | 3 weeks | Triamcinolone 0.1% cream QD, loratadine 10mg QD, D/C diet | Resolution in 1 month with PIH |
| 1020 | F/26 | N/A | Trunk | 3 weeks | D/C diet | Resolution in 2 days with PIH |
| 1121 | F/37 | Chinese | Trunk | 2 weeks | Doxycycline 100mg BID x 6 weeks, D/C diet | Resolution in 3 weeks |
| 1221 | F/19 | Chinese | Trunk | 2 weeks | Doxycycline 100mg QD x 6 weeks, D/C diet | Resolution in 2 weeks |
| 1321 | F/19 | Chinese | Trunk, suprapubic | 1 month | Doxycycline 100mg QD x 4 weeks, D/C diet | Resolution in 2 weeks |
| 1421 | F/22 | Hispanic | Trunk, arms | 2 weeks | Minocycline PO x 2 weeks, D/C diet | Resolution in 2 weeks with PIH |
| 1523 | F/21 | Chinese | Trunk, mons pubis, sacrum | 2 weeks | Topical steroids, D/C diet | Resolution in 1 week with PIH |
| 1624 | F/20s | N/A | Trunk, neck, face, scalp | 2 months | Doxycycline x 2 weeks, D/C diet | Resolution in 2 weeks |
| 1725 | F/24 | Black | Trunk, face | 2 weeks | Prednisolone 40mg taper x 2 weeks, minocycline 100mg BID x 4 weeks, D/C diet | Resolution in 1 month with PIH |
| 1826 | F/32 | Middle Eastern | Trunk | 3 weeks | Doxycycline 100mg QD x 1 month, D/C diet | Resolution in 4 weeks with PIH |
| 1927 | F/19 | Caucasian | Trunk, neck | 6 days | Minocycline 100mg QD x 3 weeks, prednisone 0.5 mg/kg/d taper, D/C diet | Resolution in 1 month with PIH |
M: male; F: female; N/A: not available; D/C: discontinue; PIH: postinflammatory hyperpigmentation
The onset of the rash ranged from six days to four months after initiating a ketogenic diet. On average, lesions erupted 31 days after starting the diet. The skin lesions predominantly occurred on the trunk and neck. Involvement of atypical locations (e.g., face, scalp, suprapubic region) were described in five cases. The vast majority of the case reports described the rash as erythematous papules or vesicles coalescing into a reticulated pattern. Patients presented with hyperpigmentation in 42 percent of cases.
Treatment included cessation of the ketogenic diet in all cases. Over half the patients were treated with oral doxycycline, ranging from 100 to 200 milligrams daily for two weeks to two months. Other treatments included oral minocycline, topical steroids, topical antibiotics, oral antihistamines, oral prednisolone, and topical antifungals. Active rash lesions resolved after an average of 18 days of treatment. The majority of patients (68%) experienced residual hyperpigmentation.
CONCLUSION
Given the growing popularity of the ketogenic diet, cases of PP appear to be on the rise. However, ketogenic diet-induced PP might be an underdiagnosed entity due to lack of clinical inquiry regarding patients’ dietary habits and/or the potential to confuse this historically rare dermatosis with more common conditions, such as eczema, contact dermatitis, and confluent and reticulated papillomatosis. Therefore, a high index of suspicion is required for prompt diagnosis and management. It is important to recognize that ketogenic diet-induced PP can affect patients of diverse ethnicities worldwide, as demonstrated in this literature review. The prognosis is excellent after resuming a normal diet and initiating treatment, typically with oral doxycycline.
In conclusion, dermatologists should review dietary habits of all patients presenting with a pruritic erythematous papular reticulated rash on the trunk, and consider PP at the top of their differential for any patient presenting with a cutaneous eruption after initiating a ketogenic diet.
References
- Paoli A, Rubini A, Volek JS, Grimaldi KA. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr. 2013;67(8):789–96. doi: 10.1038/ejcn.2013.116. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagashima M. A peculiar pruriginous dermatosis with gross reticular pigmentation. Jpn J Dermatol. 1971;81:38–39. doi: 10.1111/j.1440-0960.1992.tb00060.x. [DOI] [PubMed] [Google Scholar]
- Boer A, Misago N, Wolter M et al. Prurigo pigmentosa: a distinctive inflammatory disease of the skin. Am J Dermatopathol. 2003;25(2):117–129. doi: 10.1097/00000372-200304000-00005. [DOI] [PubMed] [Google Scholar]
- Oh YJ, Lee MH. Prurigo pigmentosa: a clinicopathologic study of 16 cases. J Eur Acad Dermatol Venereol. 2012;26(9):1149–1153. doi: 10.1111/j.1468-3083.2011.04263.x. [DOI] [PubMed] [Google Scholar]
- Cota C, Donati P, Amantea A. Prurigo pigmentosa associated with an atopic diathesis in a 13-year-old girl. Pediatr Dermatol. 2007;24:277–279. doi: 10.1111/j.1525-1470.2007.00402.x. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Kawada A, Hiruma M et al. Prurigo pigmentosa, ketonemia and diabetes mellitus. Dermatology. 1996;192:78–80. doi: 10.1159/000246324. [DOI] [PubMed] [Google Scholar]
- Nakada T, Sueki H, Iijima M. Prurigo pigmentosa (Nagashima) associated with anorexia nervosa. Clin Exp Dermatol. 1998;23:25–27. doi: 10.1046/j.1365-2230.1998.00249.x. [DOI] [PubMed] [Google Scholar]
- Kim MH, Choi YW, Choi HY, Myung KB. Prurigo pigmentosa from contact allergy to chrome in detergent. Contact Dermatitis. 2001;44:289–92. doi: 10.1034/j.1600-0536.2001.440507.x. [DOI] [PubMed] [Google Scholar]
- Hanami Y, Yamamoto T. Bullous prurigo pigmentosa in a pregnant woman with hyperemesis gravidarum. J Dermatol. 2015;42(4):436–437. doi: 10.1111/1346-8138.12795. [DOI] [PubMed] [Google Scholar]
- Erbagci Z. Prurigo pigmentosa in association with Helicobacter pyroli infection in a Caucasian Turkish woman. Acta Derm Venereol. 2002;82:302–3. doi: 10.1080/000155502320323324. [DOI] [PubMed] [Google Scholar]
- Ohnishi T, Kisa H, Ogata E et al. Prurigo pigmentosa associated with diabetic ketoacidosis. Acta Derm Venereol. 2000;80:447–448. doi: 10.1080/000155500300080447448. [DOI] [PubMed] [Google Scholar]
- Abbass M, Abiad F, Abbas O. Prurigo Pigmentosa After Bariatric Surgery. JAMA Dermatol. 2015;151(7):796–797. doi: 10.1001/jamadermatol.2015.0247. [DOI] [PubMed] [Google Scholar]
- Gironi LC, Farinelli P, Giacalone A, Colombo E. The efficacy of minocycline in inflammatory dermatoses: a case of prurigo pigmentosa of prepubescent onset in Western world. Dermatol Ther. 2015;28(4):239–42. doi: 10.1111/dth.12216. Jul. [DOI] [PubMed] [Google Scholar]
- Michaels JD, Hoss E, DiCaudo DJ, Price H. Prurigo pigmentosa after a strict ketogenic diet. Pediatr Dermatol. 2015;32(2):248–51. doi: 10.1111/pde.12275. Mar. [DOI] [PubMed] [Google Scholar]
- Onaygil E, Songur A, Kutlubay Z, Demirkesen C. Early Stage Prurigo Pigmentosa: A Case Report. Turk Patoloji Derg. 2018;34(2):182–5. doi: 10.5146/tjpath.2015.01333. May 1. [DOI] [PubMed] [Google Scholar]
- Miki Wong MA, Lee E, Wu Y, Lee R. Treatment of prurigo pigmentosa with diet modification: a medical case study. Hawaii J Med Public Health. 2018;77(5):114. May. [PMC free article] [PubMed] [Google Scholar]
- Alkeraye S, AlMuqrin A, AlQahtani SM et al. Twenty-five year-old female with sudden onset itchy skin eruption over her upper back and chest three weeks after starting a ketogenic diet. Ann Saudi Med. 2019;39(6):444–5. doi: 10.5144/0256-4947.2019.444. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshaya MA, Turkmani MG, Alissa AM. Prurigo pigmentosa following ketogenic diet and bariatric surgery: A growing association. JAAD Case Rep. 2019;5(6):504–7. doi: 10.1016/j.jdcr.2019.03.011. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au J, Jaros J, Wang S, Flischel A. Prurigo pigmentosa: A case of the” keto rash”. J Am Acad Dermatol. 2019;81(4):AB260–AB260. Oct 1. [Google Scholar]
- Croom D, Barlow T, Landers JT. Pruritic rash on chest and back. J Fam Pract. 2019;68(2):113–6. Mar. [PubMed] [Google Scholar]
- Goh SW, Adawiyah J, Md Nor N et al. Skin eruption induced by dieting - an underdiagnosed skin disease in Malaysia. Malays Fam Physician. 2019;14(1):42–46. Apr 30. [PMC free article] [PubMed] [Google Scholar]
- Lonowski S, Levins P. A unique case of prurigo pigmentosa related to ketogenic diet. Dermatol Online J. 2020;26:2. Feb 15. [PubMed] [Google Scholar]
- Mao DD, Chen X, Zhang H, Jin J, Chen X, Wen GD. Bullous prurigo pigmentosa following a ketogenic diet. Chin Med J (Engl). 2021;134(13):1632–1633. doi: 10.1097/CM9.0000000000001322. Jan 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delaleu J, Grynberg-Laloum E, Moguelet P et al. Prurigo pigmentosa induced by ketosis (“keto rash”): a demonstrative case and internet search results. Int J Dermatol. 2020;59(7):876–877. doi: 10.1111/ijd.14873. Jul. [DOI] [PubMed] [Google Scholar]
- Salam A, Peleva E, Cowper SE, Leventhal JS. Pruritic reticulation: don’t ‘fiddle’ around. Clin Exp Dermatol. 2020;45(4):501–504. doi: 10.1111/ced.14135. Jun. [DOI] [PubMed] [Google Scholar]
- Hamouda MB, Fetoui NG, Ghariani N et al. Prurigo Pigmentosa Following Ketogenic Diet. Am J Med. 2021;134(4):e291–e292. doi: 10.1016/j.amjmed.2020.10.016. Apr. [DOI] [PubMed] [Google Scholar]
- Partarrieu-Mejías F, Martínez-Domenech Á, Ríos-Viñuela E et al. Acute pruritic rash on a young woman after a restrictive diet. J Dtsch Dermatol Ges. 2021;19(6):926–928. doi: 10.1111/ddg.14427. Jun. [DOI] [PubMed] [Google Scholar]