Abstract
Background
The mechanism of fat reduction from radiofrequency occurs via the thermal stimulation of adipocyte metabolism, causing a lipase-mediated triglyceride enzyme degradation, apoptosis, and adipocyte rupture. Ultracavitation promotes fat reduction using adipose cell destruction through mechanical stimulus. The literature on the combination of these two physical agents, named ultrafrequency, is still scarce and requires consistent analysis of the effects of this therapy combination.
Objective
The objective of this study was to investigate the effects of radiofrequency associated with ultracavitation in the treatment of abdominal subcutaneous tissue of women.
Methods
This was a prospective, randomized clinical trial in which 45 participants were divided into three distinct groups: the control group (no treatment); ultracavitation group; and ultracavitation and radiofrequency (UCV+RF) group, each with 15 volunteers. The following variables were evaluated: weight, perimetry, plicometry, ultrasonography, treatment reactions, and patient satisfaction.
Results
The participants in the UCV+RF group presented a more significant decrease in adipose tissue, which was verified through all the evaluation methods.
Conclusion
Based on our results, the simultaneous application of ultracavitation and radiofrequency generated a reduction in localized adiposity superior to the isolated use of ultracavitation.
Keywords: Fat, subcutaneous tissue, ultrafrequency, adiposity, abdomen, ultracavitation, radiofrequency
Currently, many resources are used to attenuate and treat localized adiposity, including invasive (e.g., liposuction) and noninvasive procedures (e.g., carboxytherapy, endermotherapy, cryolipolysis, ultrasound, ultracavitation, radiofrequency). Ultracavitation (UCV) and radiofrequency (RF) are highlights among noninvasive procedures, as they have been shown to yield good aesthetic treatment results in clinical practice.1–3
Ultracavitation refers to a piece of equipment that emits sound waves of varied frequency and high intensity. These ultrasonic waves promote the formation of gas or vapor microbubbles that are subject to the considerable negative or positive pressure that is generated in the ultrasonic field. With the same way it occurs with microbubbles, the subcutaneous tissue will also respond to the ultrasound frequency, and through unstable cavitation, after the implosion of the microbubbles, the adipocyte membrane may be ruptured, promoting extravasation of the fat. The elimination of this fat occurs through physiological pathways; the triglycerides of fat cells that have been cavitated are eliminated in the interstitial fluid where they are successively taken through the lymphatic or venous system to the liver, where they are metabolized again.4
The radiofrequency uses high-frequency electromagnetic waves to produce heat at the cutaneous and the subcutaneous levels. The mechanism of action, through the vibration of water molecules, transforms the electromagnetic energy into thermal. The heat generated by conversion occurs under 30 kHz to 300 MHz, and the most frequently used frequency is set between 0.5 and 1.5 MHz.5 The RF mechanism of fat reduction occurs by the generation of thermal stimulation of adipocyte metabolism, occurring through enzymatic degradation by lipase-mediated triglycerides, apoptosis, and adipocyte rupture.6
The application of the two therapeutic modalities at the same time and in the same area is called ultrafrequency. It is suggested that the effects of the two intervention modalities overlap.7 Thus, the potentiation of these combined techniques may favor the reduction of localized adiposity through mechanical waves. Furthermore, radiofrequency modulates the fibroblasts and collagen functions, and consequently, minimizes flaccidity.8
In the present study, we sought to investigate possible advantages in the of ultracavitation combined with radiofrequency for the treatment of localized adiposity. The literature on this combination is still scarce, which requires consistent analysis of the effects of this combination therapy.
METHODS
This was a prospective, randomized clinical trial. The study population of this study consisted of women with localized adiposity in the subcutaneous infraumbilical region. The sample consisted of 45 women aged 20 to 40 years.
The inclusion criteria included body mass index (BMI) between 18.5 and 29.99 (normal to overweight); infraumbilical localized fat thickness greater than 1cm and smaller than 4cm (identified by ultrasonographic image); nulliparous women; no use of drugs of lipolytic and/or thermogenic effects up to a week before treatment; subjects not affected by severe metabolic diseases. The exclusion criteria included the following: participants who did not carry out the proposed evaluations, missed consecutive treatment sessions, with excessive weight increase during the research, or who presented severe dermal reactions and decreased sensitivity.
This study was submitted to the Research Ethics Committee and approved by the Research Ethics Committee of Universidade Potiguar. Participants were instructed on the procedures that would be performed and signed an informed consent form.
The instruments that were used to collect data included the following: an ultrasound imaging device for analysis and measurement of adipose tissue (MSLPU35 Linear Wireless Probe Ultrasound Scanner 10 MHz; Guangzhou Medsinglong Medical Equipment, Co™ South Korea), a retractable tape measure (Fibe™), a plicometer (Sanny™); a digital scale (Glicomed™). Skin temperature was measured and/or controlled through thermographic imaging.
The ultrafrequency device used for the procedures was the NARNIAH™ (Medical San™, Brasil) for a 4-MHz ultracavitation with a power of 90 W (5.6 W/cm2), bipolar, multi-frequency (650, 1200, and 2400 kHz) resistive radiofrequency with a power of 120 W.
The study participants were submitted to three evaluations throughout the treatment: initial evaluation (before treatment), intermediate (after two weeks of treatment), and final (after the end of the study) using perimetry, plicometry, and body weight measurement. Ultrasound analysis was performed at the initial and the final evaluations only. The participants were divided into three distinct groups, composed of 15 volunteers each group: control group; ultracavitation (UCV); and ultracavitation and radiofrequency (UCV+RF).
The perimetry was performed with the participants standing, with the tape measure positioned 5cm above and 5cm below the navel. The plicometry was performed with the participants standing, with the manual "pinch" fold being performed on the left and right lateral region of the navel; the bodyweight measurement was performed with the participants standing on the digital scale. The ultrasonography was performed on the central infra-umbilical region at two different spots, and the distance between these spots was approximately 7cm. The marking of the points of analysis and the accomplishment of the ultrasonography were done with the participants in dorsal decubitus, and the measurements were collected from participants. The Global Aesthetic Improvement Scale (GAIS) questionnaire from Narins9 and the Adapted Satisfaction Questionnaire from Segot-Chicq et al10 were also applied. The subjects from the treated groups had their infra-umbilical area treated with UCV and UCV+RF, one application each week for four weeks. The treated region received appropriate marking to delimit the specific site of the application.
Each volunteer underwent a 15-minute session of each therapeutic resource as follows: the UCV group received intervention with ultracavitation only; the UCV+RF group received intervention using ultracavitation and radiofrequency simultaneously. The control group received a simulated session simulation of the treatment application, using the equipment off in the application region.
The applied ultracavitation dosimetry modulation parameters were 4 MHz wave frequency and 5 W/cm2, both for the UCV group and in the RF+UCV group. The radiofrequency was adjusted at a 650 kHz with the dosimetry required to produce intense heat on the skin surface within the range of 40 to 43° C, according to the of treated subjects’ tolerance levels, with the use of a digital thermometer and a thermographic camera.
After reaching the therapeutic temperature of 40ºC, the radiofrequency device was used for 15 minutes, while the temperature was controlled with the aid of a digital thermometer. The same length of time was used for ultracavitation.
The data collected during the evaluations were recorded in an Excel spreadsheet and then submitted to the descriptive statistical analysis of the Service Statistical Package for Social Science (SPSS) (version 22.0) for Windows. For the analysis of the obtained data, the mixed ANOVA was applied, along with the Tukey post hoc test. The level of significance was 95 percent with p<0.05.
RESULTS
The evaluation procedures were performed as mentioned. However, some volunteers did not follow guidelines, and some withdrew during the procedures, which led to their exclusion. A total of 36 volunteers remained for the duration of the treatment and until the end of the study. The sample was divided into the same three groups, each with 12 volunteers. Table 1 shows the results of the mean and standard deviation of variables. In the anthropometric analysis, no significant statistical difference (p=0.96, p=0.91, p=0.87) was observed in the body weight in the comparison among groups.
TABLE 1.
Mean and standard deviation of the anthropometric variables and thickness of the adipose layer in ultrasound for the control, UCV, and UCV+RF groups
| VARIABLES | CONTROL | UC | UC+RF |
|---|---|---|---|
| Starting Weight | 65.6±6.56 | 65.31±8.8 | 66.82±10.6 |
| Weight 15 days | 65.7±6.22 | 64.7±8.0 | 66.44±10.5 |
| Weight 30 days | 66.44±8.78 | 64.97±7.8 | 66.44±10.7 |
| Initial Right Plicometry | 2.76±0.53 | 2.8±0.65 | 2.7±0.53 |
| Right Plicometry 15 Days | 2.68±0.89 | 2.5±0.63 | 2.6±0.52 |
| Right Plicometry 30 Days | 2.7±0.53 | 2.0±0.65 | 1.6±0.5 |
| Initial Left Plicometry | 2.88±0.13 | 2.83±0.16 | 2.79±0.1 |
| Left Plicometry, 15 days | 2.87±0.52 | 2.78±0.63 | 2.87±0.52 |
| Left Plicometry, 30 days | 2.7±0.8 | 2.00±0.79 | 1.7±0.82 |
| Initial Perimetry | 88.44±5.5 | 88.56±4.9 | 87.48±5.3 |
| Perimetry 15 days | 86.3±5.5 | 86.1±5.9 | 85.9±6.1 |
| Perimetry 30 days | 86.1±5.1 | 80.0±4.8 | 78.0±5.9 |
| US Initial Left | 2.3±0.67 | 2.0±0.68 | 1.9±0.73 |
| US Final Left | 2.1±0.69 | 1.78±0.7 | 1.5±0.7 |
| US Initial Right | 2.2±0.73 | 2.2±0.68 | 2.2±0.73 |
| US Final Right | 1.9±0.65 | 1.7±0.71 | 1.6±0.64 |
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency; US: ultrasound
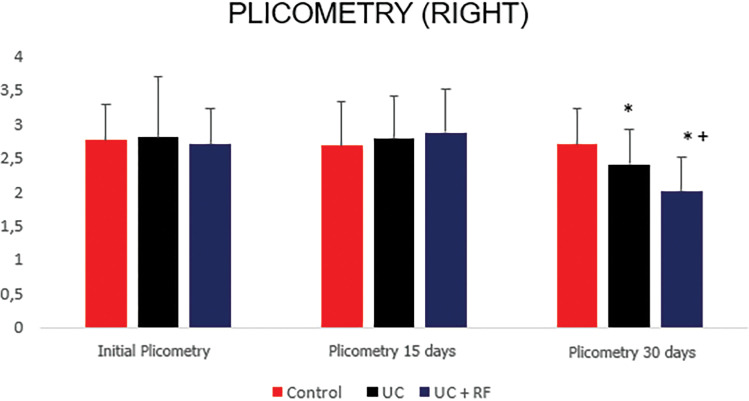
Figure 1 shows the plicometry of the right lateral region, and it was verified that in the comparison among groups, there was a significant difference between the final evaluation in the UCV group (p=0.04) and the UCV+RF (p=0.02) when compared to control. In the comparison between the UCV+RF and the UCV group, a reduction in plicometry measurements was observed in the final evaluation (p=0.001).
FIGURE 1.
Right side plicometry analysis. *There was some difference between the UC and the control group (0.04), the UCV+RF and The control group (0.02). *There was some difference between the UCV+RF group and the UCV group (0.001).
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency
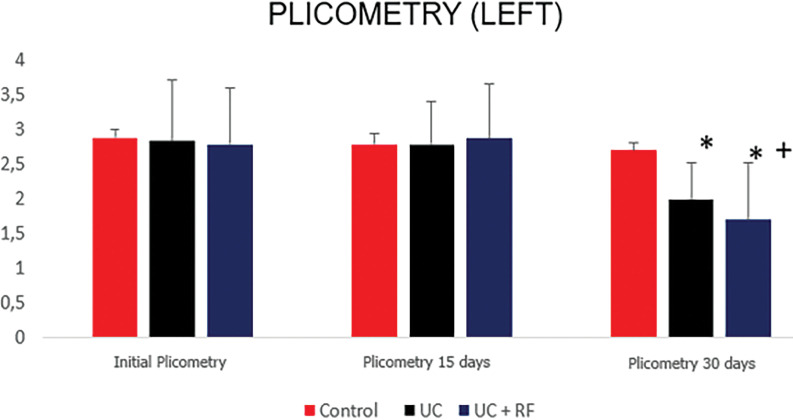
Figure 2 shows the plicometry of the left lateral region and found that in the comparison among groups, there was a significant difference between the final evaluation in the UCV group (p=0.03) and UCV+RF group (p=0.01) when compared to control. In the comparison between the UCV+RF and the UCV group, a reduction in plicometry measurements was observed in the final evaluation (p=0.01).
FIGURE 2.
Left side plicometry analysis. *There was some difference between the UCV+RF groups and the UCV group (0.01). *There was some difference between the UCV and the control group (0.03), the UCV+RF and the control group (0.01).
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency
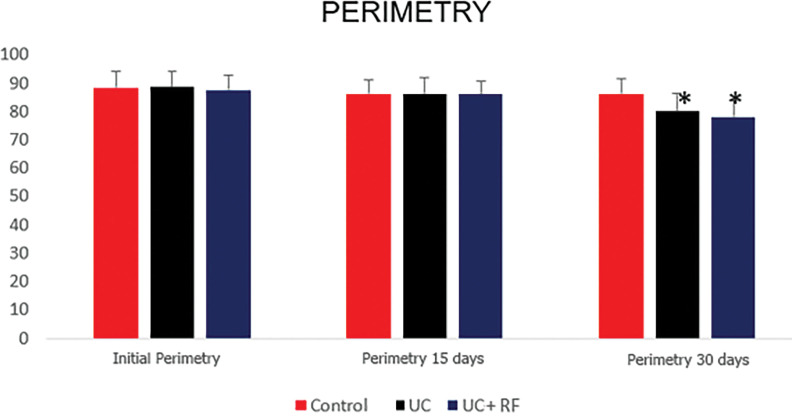
Figure 3 presents the perimetry and verified that in the comparison between the groups, there was a significant difference between the final evaluation in the UCV group (p=0.02) and the UCV+RF (p=0.02) when compared to the control group.
FIGURE 3.
Perimetry analysis *Difference against control. There was some difference between the UCV group and the control group (0.02), and the UCV+RF and the control (0.02).
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency
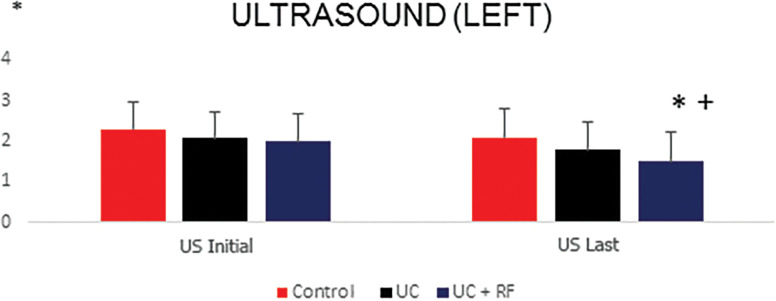
Figure 4 shows the distribution of infraumbilical adipose tissue through ultrasonography in the left lateral region. Greater decrease of the adipose tissue was observed in the UCV+RF group when compared to the control (p=0.02) and when compared to the UCV group (p=0.01).
FIGURE 4.
US analysis of the left side. *There was some difference between the UCV+RF versus Control (0.02). When the UCV groups were compared to the UCV+RF group, it was possible to verify that *some difference was identified (p=0.01). Greater decrease of the greasy contingent in the UCV+RF group was verified.
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency; US: ultrasound
Figure 3 presents the perimetry and verified that in the comparison between the groups, there was a significant difference between the final evaluation in the UCV group (p=0.02) and the UCV+RF (p=0.02) when compared to the control group.
Figure 4 shows the distribution of infraumbilical adipose tissue through ultrasonography in the left lateral region. Greater decrease of the adipose tissue was observed in the UCV+RF group when compared to the control (p=0.02) and when compared to the UCV group (p=0.01).
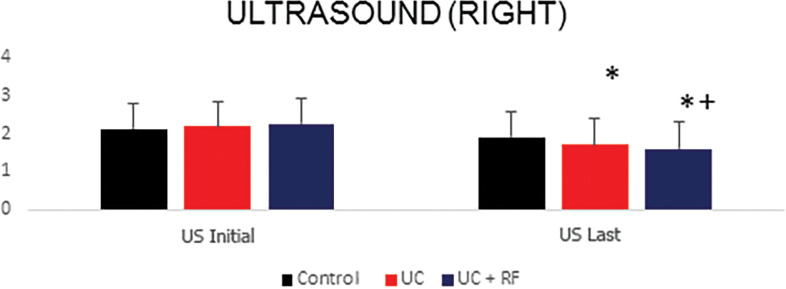
Figure 5 shows the distribution of infraumbilical adipose tissue through ultrasonography on the right side. It was observed that in the UCV+RF group, there was a greater decrease in the adipose tissue when compared to control (p=0.04) and when compared to the UCV group (p=0.04).
FIGURE 5.
Right side ultrasonographic (US) analysis. *There was some difference between the UCV+RF group and The control group (0.04). When UCV groups were compared with the UCV+RF groups, it was verified that *there was some difference between these groups (p=0.01), and a more significant decrease of the fat contingent in the UCV+RF group was identified.
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency
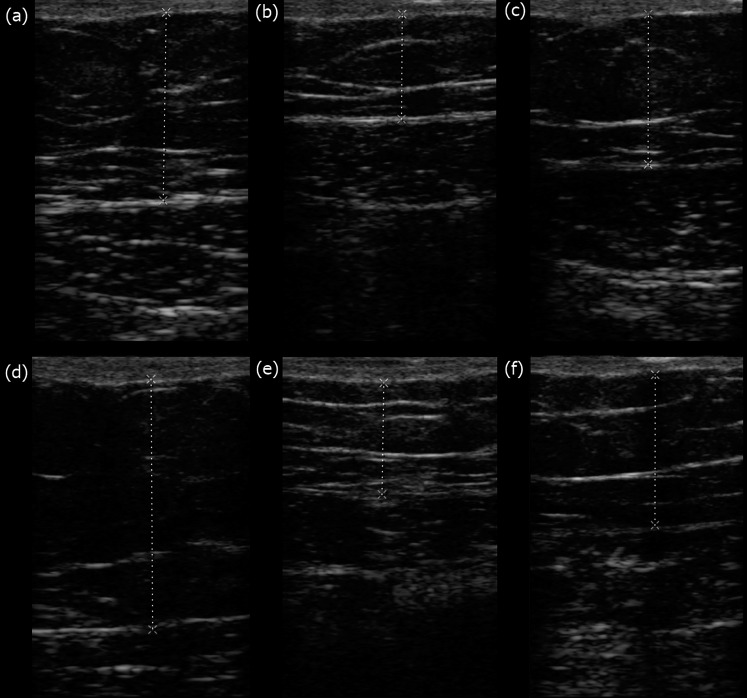
Figure 6 shows a representation of the ultrasonography results.
FIGURE 6.
Ultrasonography images: Figures A, B, and C correspond to ultracavitation and radiofrequency, ultracavitation, and control groups, respectively, before treatment. The values of the ultrasonography are 2.92cm, 1.30cm, and 1.74cm. After treatment (Figures D, E, and F), the values of the ultrasonography were 2.18cm, 1.22cm, and 1.75cm.
Tables 2 and 3 present the results of the questionnaires. The values are distributed in absolute frequency (AF) and relative frequency (RF).
TABLE 3.
Results of the treatment satisfaction questionnaire.
| CONTROL | UC | UC+RF | ||||
|---|---|---|---|---|---|---|
| AF | RF | AF | RF | AF | RF | |
| Satisfaction | ||||||
| Yes | 3 | 25.0 | 3 | 25.0 | 12 | 100 |
| No | 9 | 75.0 | 9 | 75.0 | ||
| Treatment Evaluation | ||||||
| Weak treatment | 4 | 33.3 | 2 | 15 | 1 | 4 |
| Good treatment | 8 | 66.7 | 10 | 75 | 1 | 8 |
| Very good treatment | 5 | 41.7 | ||||
| Excellent treatment | 5 | 41.7 | ||||
| Improvement in Aesthetics | ||||||
| Unchanged | 10 | 83.3 | 3 | 26.7 | 1 | 8.3 |
| Better | 2 | 16.7 | 9 | 73.3 | 6 | 50.0 |
| Much better | 2 | 16.7 | ||||
| Very much better | 3 | 25.0 | ||||
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency; AF: absolute frequency; RF: relative frequency
TABLE 2.
Presentation of the results of the adverse response questionnaires
| CONTROL | UCV | UCV+RF | |||||
|---|---|---|---|---|---|---|---|
| AF | RF | AF | RF | AF | RF | ||
| Pain | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
| Numbness | No | 12 | 100.0 | 11 | 91.7 | 12 | 100.0 |
| Yes, for a few minutes | 1 | 8.3 | |||||
| Hypersensitivity | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
| Edema | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
| Erythema | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
| Bruise | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
| Burn | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
| Adverse effects | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
| Medical care | No | 12 | 100.0 | 12 | 100.0 | 12 | 100.0 |
UCV: ultracavitation; UC+RF: ultracavitation and radiofrequency; AF: absolute frequency; RF: relative frequency
Regarding the reactions immediately after the sessions, none of the volunteers presented redness, marks, and felt no shocks on the skin. In the control group, 100 percent of the volunteers reported not noticing loose clothing. In the analysis of the presence of loose clothing within the other groups, the UCV group about 75 percent of the volunteers presented loose clothing on the first week; however, after four weeks, only 25 percent of the participants reported loose clothing. Within the UCV+RF group, 75 percent of the volunteers reported their clothes seemed loose after four weeks.
In the skin texture analysis, the control and the UC groups did not show modifications. Only the UCV+RF group showed skin alteration, whereas 33.3 percent reported firmer skin. However, 58.4 percent reported that the skin appeared much firmer.
Among the volunteers from the control group, 100 percent did not report being satisfied with the treatment outcome. However, 50 percent of the volunteers in the UCV group reported being satisfied, whereas, in the UCV+RF group, there was 100 percent satisfaction at the end of treatment. Regarding the evaluation of the treatment quality, 41.7 percent of the volunteers from the UCV+RF group rated it as an excellent treatment.
DISCUSSION
In the analysis of the anthropometric measures, no variation of body weight between the studied groups was observed, in any of the comparisons, which demonstrates the sample homogeneity and the standardisation of a localized adiposity analysis. Some volunteers were excluded from the study, as they presented excessive body weight variation, with a gain of adipose mass. Thus, three individuals from each group (control, UCV, and UCV+RF) were excluded to ensure volunteers-related data reliability analysis.
In the plicometry analysis, the right and left sides of the umbilical line presented similar behaviour. On both sides, the reduction of the skinfold measurement was observed in the treatment groups when compared to control. However, there was a more significant reduction in the UCV+RF group when compared to the group that received UCV alone.
In the perimetry evaluation, a reduction of the measurements in the UCV+RF and UCV groups was observed when compared to control, but no visually perceived difference was evidenced.
In the ultrasound evaluation, it was observed that in the group that the UCV+RF group, there was a greater adipose tissue decrease when compared to control and the UCV groups.
The fat thickness reduction in the treated area without concomitant weight reduction characterises a response that is indicative of the treatment applied to localized adiposity. This behaviour is similar to the one verified in this study, in which there was no weight reduction, but there was a decrease in localized adipose tissue (identified in the measurements of plicometry, perimetry, and ultrasonography).11
The observed results may be justified by the use of combination therapy, UCV+RF, suggesting that the combination of the two modalities favors different physiological responses similarly, and which is believed to amplify the effect of one therapy on the other.7–11
The UCV produces a significant reduction in adipocyte size, causing a reduction in subcutaneous fat. The cavitation induces adipocyte destabilisation, causing the rupture of these cells and allowing the extravasation of triglycerides and lipids into the extracellular space.10 The results of adipose tissue biopsies in the study by Bani et al11 indicated that the mean size of the subcutaneous adipocytes was significantly reduced compared to the placebo-treated areas.11After cell rupture, the content consists mainly of triglycerides that are dispersed in the interstitial space and transported through the lymphatic system to the liver. These triglycerides are slowly metabolized into fatty acids that can enter directly into muscle cells or adjacent adipocytes as an energy source, and glycerol that are used as energy fuel by muscles (glycogen).12,13
It is observed that the reduction of adiposity and modelling of the adjacent connective tissue promotes ameasures reduction effect. However, disorganisation of the collagen fibers can be noticed, which coincide with reports of skin flaccidity after adipocyte volume loss. To minimize these responses, the combination of UCV associated with radiofrequency may potentiate these results, since RF favors a reorganization of connective tissue. RF acts on the immediate contraction of collagen fibers, activation of fibroblasts and remodelling of connective tissue, as well as promoting an increase in metabolism and decrease of fat.14–16
The UCV promoted a measure reduction effect; however, the group that received the association with RF presented a greater reduction of the adipose layer. The measurement reduction and the adipose layer verification on ultrasonography may have occurred due to the increment generated by RF in the adiposity zone. Another possible explanation is its ability to reach higher temperatures and to obtain not only effect on skin flaccidity with comfort but also the effects on adipose tissue through higher and more comfortable temperatures for the patient.8,17,18
The combined therapy named ‘ultrafrequency’ promotes the reduction of adiposity through the cavitation mechanism generated by mechanical waves and by the thermal effect. The thermal effect is associated with the action of the radiofrequency, which can promote a lipolytic response; but in the ultrafrequency, the association with a response generated in the connective tissue is observed, modulating the collagen and thus reducing tissue flaccidity.8
The results presented in this study, such as the reported loose clothing, skin texture improvement and skin firmness, corroborate with the additional effects the radiofrequency would promote on the UCV treatment, collaborating with analyses of flaccidity decrease in different clinical radiofrequency use situations. Regarding the treatment result satisfaction, the volunteers submitted to the application of ultracavitation associated with radiofrequency indicated high satisfaction percentage. In addition, this group responded with the highest satisfaction degrees: “excellent", "very good treatment" and "good treatment". This shows an important relationship between positive results that were obtained through the collected data.
Limitations. This study had limitations because it did not perform immunohistochemical analysis of adipose tissue after the application of UCV+RF. It is also observed the absence of a follow-up analysis, to verify the permanence of the results.
CONCLUSION
Tt may be concluded that the simultaneous use of ultracavitation and the radiofrequency promoted greater reduction of the localized adiposity and cutaneous flaccidity, with plicometry, perimetry, and ultrasonography measurement reductions in comparison with the control groups and with the isolated use of UCV.
ACKNOWLEDGMENTS
The authors declare their appreciation to the in integrated clinics and the dermatofunctional physiotherapeutic ambulatory of the University UNI-RN, where the treatment was carried out.
REFERENCES
- Friedmann DP. A review of the aesthetic treatment of abdominal subcutaneous adipose tissue: background, implications, and therapeutic options. Dermatologic Surgery. 2015;41(1):18–34. doi: 10.1097/DSS.0000000000000209. [DOI] [PubMed] [Google Scholar]
- Costa RB, Garcez VF, Limana MD. Terapia combinada (ultrassom e eletroterapia) na redução da adiposidade abdominal: relato de casos. ConScientiae Saúde. 2017;15(4):665–670. [Google Scholar]
- Meyer PF, Davi Costa E, Silva J, Santos de Vasconcelos L, de Morais Carreiro E, Valentim da Silva RM. Cryolipolysis: seleção de pacientes e considerações especiais. 2018;11:499–503. doi: 10.2147/CCID.S146258. 16 de outubro. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer PF, Carvalho MGF, Andrade LL, Lopes RNS, Delgado AM, Araujo HG et al. Efeitos da ultracavitação no tecido adiposo de coelhos. Fisioter Bras. 2012;13:106–111. [Google Scholar]
- Avantaggiato A, Bertuzzi G, Addonisio T, Iannucci G, Vitiello U, Carinci F. Radiofrequency treatments: what can we expect?. Journal of biological regulators and homeostatic agents. 2016;30(1):217–22. 2. [PubMed] [Google Scholar]
- Gentile RD, Kinney BM, Sadick NS. Radiofrequency Technology in Face and Neck Rejuvenation. Facial Plast Surg Clin North Am. 2018;26(2):123–134. doi: 10.1016/j.fsc.2017.12.003. May. [DOI] [PubMed] [Google Scholar]
- Coleman KM, Pozner J. Combination therapy for rejuvenation of the outer thigh and buttock: a review and our experience. Dermatologic Surgery. 2016;42:S124–S30. doi: 10.1097/DSS.0000000000000752. [DOI] [PubMed] [Google Scholar]
- Barnes D. Porto Alegre: Essência do Saber Ed.; 2019. Ultrafrequência. pp. p. 119–23. [Google Scholar]
- Narins RS, Brandt F, Leyden J, Lorenc ZP, Rubin M, Smith S. A randomized, double-blind, multicenter comparison of the efficacy and tolerability of restylane versus zyplast for the correction of nasolabial folds. Dermatol Surg. 2003;29(6):588–95. doi: 10.1046/j.1524-4725.2003.29150.x. Jun. [DOI] [PubMed] [Google Scholar]
- Segot-Chicq E, Compan-Zaouati D, Wolkenstein P, Consoli S, Rodary C, Delvigne V, Guillou V, Poli F. Development and validation of a questionnaire to evaluate how a cosmetic product for oily skin is able to improve well-being in women. J Eur Acad Dermatol Venereol. 2007;21(9):1181–6. doi: 10.1111/j.1468-3083.2007.02193.x. Oct. [DOI] [PubMed] [Google Scholar]
- Bertolini SMG, Coelho KC, Fries LMV, Sorti GS, Zorzi YR. Análise dos Efeitos da Lipólise em Mulheres com Adiposidade Abdominal: Revisão Sistemática. Rev. Científica JOPEF. 2015. 19 1. [Google Scholar]
- Bani D, Li AQ, Freschi G, Russo GL. Histological and Ultrastructural Effects of Ultrasound-induced Cavitation on Human Skin Adipose Tissue. Plastic and Reconstr Surg – Global Open. 2013;1(6):41. doi: 10.1097/GOX.0b013e3182a7f222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva RMV, Meyer PF, Santos BR, Felix JLO, Ronzio OA. Efectos del ultrasonido de alta potencia en la adiposidad localizada. Fisioterapia (Madrid. Ed. impressa). 2014;36(1):1–5. [Google Scholar]
- Ding T, Zhang S, Fu Q, Xu Z, Wan M. Ultrasound line-by-line scanning method of spatial-temporal active cavitation mapping for high-intensity focused ultrasound. Ultrasonics. 2014;54(1):147–55. doi: 10.1016/j.ultras.2013.04.011. [DOI] [PubMed] [Google Scholar]
- Shek SY, Yeung CK, Chan JC, Chan HH. The efficacy of a combination non-thermal focused ultrasound and radiofrequency device for noninvasive body contouring in Asians. Lasers Surg Med. 2016;48(2):203–7. doi: 10.1002/lsm.22406. [DOI] [PubMed] [Google Scholar]
- Alvarez N, Ortiz G, Vicente V, Alcaraz M, Sanchez-Pedreño P. The effects of radiofrequency on skin: experimental study. Lasers Surg Med. 2008;40(2):76–82. doi: 10.1002/lsm.20594. Feb. [DOI] [PubMed] [Google Scholar]
- De Carvalho G. F, da Silva R. M. V, de Mesquita Filho J. J, Meyer P. F, Ronzio O. A, de Oliveira Medeiros J., Nóbrega M. M. Avaliação dos efeitos da radiofrequência no tecido conjuntivo. Revista brasileira de medicina. 2011;68:10–25. [Google Scholar]
- Manuskiatti W, C, Wachirakaphan C N, Lektrakul, NH S, Varothai S. TriPollar – Aparelho de radiofrequência para Redução do Volume Abdominal e Tratamento da Celulite: Estudo Piloto. 2009. JEADV.
- Sadick N, Rothaus KO. Aesthetic Applications of Radiofrequency Devices. Clin Plast Surg. 2016;43(3):557–65. doi: 10.1016/j.cps.2016.03.014. Jul. [DOI] [PubMed] [Google Scholar]