Abstract
Identifying persons who are least willing to receive a coronavirus disease 2019 (COVID-19) vaccine is critical for increasing uptake via targeted outreach. We conducted a survey of 23,819 Canadian Longitudinal Study on Aging participants from September 29 to December 29, 2020, to assess factors associated with COVID-19 vaccination willingness and reasons for willingness or lack thereof. Among adults aged 50–96 years, 84.1% (95% confidence interval (CI): 83.7, 84.6) were very or somewhat willing to receive a COVID-19 vaccine; 15.9% (95% CI: 15.4, 16.3) were uncertain or very or somewhat unwilling. Based on logistic regression, those who were younger, female, had lower education and income, were non-White, and lived in a rural area were less willing to receive a COVID-19 vaccine. After controlling for these factors, recent receipt of influenza vaccine (adjusted odds ratio = 14.3, 95% CI: 12.5, 16.2) or planning to receive influenza vaccine (adjusted odds ratio = 10.5, 95% CI: 9.5, 11.6), as compared with no receipt or planning, was most strongly associated with COVID-19 vaccination willingness. Willingness was also associated with believing one had never been infected with severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) and experiencing negative pandemic consequences. Safety concerns were most common among those unwilling. Our comprehensive assessment of COVID-19 vaccination willingness among older adults in Canada, a prioritized group for vaccination due to their risk of severe COVID-19 outcomes, provides a road map for conducting outreach to increase uptake, which is urgently needed.
Keywords: adults, Canada, Canadian Longitudinal Study on Aging, coronavirus disease 2019, COVID-19, SARS-CoV-2, vaccination, vaccines
Abbreviations
- aOR
adjusted odds ratio
- CI
confidence interval
- CLSA
Canadian Longitudinal Study on Aging
- COVID-19
coronavirus disease 2019
- SARS-Cov-2
severe acute respiratory syndrome coronavirus 2
Ensuring a high uptake of coronavirus disease 2019 (COVID-19) vaccination, especially among individuals at highest risk of severe outcomes, is the most critical challenge of the COVID-19 pandemic. More than 30 COVID-19 vaccines are authorized for use by regulatory authorities in more than 190 countries (1). Because ample evidence indicates that older adults are at increased risk for severe COVID-19 and that they experience high case fatality (2), many countries began vaccination campaigns by prioritizing older populations, typically after vaccinating health-care workers and other essential workers (3–5).
Globally, more than a year after the first COVID-19 vaccines were approved, more than 11 billion doses have been administered (6). Yet, this progress represents only the very beginning; COVID-19 vaccinations need to reach far more people to prevent and control the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). On the local scale, many communities rapidly implemented complex vaccination programs along with public health communication to promote vaccine uptake and increase trust and vaccine confidence, especially among communities for whom trust in the health-care system has been justifiably low. On the global scale, securing sufficient numbers of vaccine doses remains a significant challenge (7).
In 2019, the World Health Organization declared vaccine hesitancy a top threat to global health, despite vaccine availability (8). While billions of dollars and extensive efforts have been invested in COVID-19 vaccine development since early 2020 (7), significantly more research is needed to ensure that vaccination campaigns are successful and to identify persons who are least likely to get vaccinated, even in countries where vaccine confidence is generally high. Canada is one such country where uptake of routinely recommended adult vaccines is high relative to many other countries (9). For example, the Canadian Seasonal Influenza Vaccination Coverage Survey estimated that influenza vaccination coverage among adults aged 65 years or older in 2019–2020 was 70.3% (95% confidence interval (CI): 66.7, 73.8; n = 789), consistent with the previous 3 seasons (10). However, the introduction of COVID-19 vaccines in late 2020 presented many challenges beyond those facing routine vaccination, and additional evidence is needed to inform COVID-19 vaccination programs. Recent studies have assessed willingness to receive a COVID-19 vaccine across multiple countries, with acceptance rates varying widely (11). In Canada, the Canadian Community Health Survey found, during the last quarter of 2020, that 76.9% of respondents aged 12 years or older were somewhat or very willing to receive a COVID-19 vaccine (12). Now that COVID-19 vaccines are widely available in Canada, national estimates indicate that 88.7% of the eligible Canadian population aged 18 years or older is fully vaccinated with a primary series (as of January 22, 2022) (13).
We sought to utilize data from a large, existing longitudinal cohort study to go beyond previous surveys and comprehensively assess COVID-19 vaccination willingness in a generalizable sample of tens of thousands of older adults prior to the introduction of COVID-19 vaccines. We aimed to quantify COVID-19 vaccination willingness, to examine factors associated with lack of willingness, and to assess reasons for willingness and lack of willingness. Our primary goal was to generate critical empirical evidence to identify persons who would benefit most from targeted outreach to improve COVID-19 vaccine uptake and to inform resource allocation to enhance vaccination efforts. Given that COVID-19 vaccines have been available to older adults in Canada for more than a year (14), this research is very timely and is critical for understanding the epidemiology of COVID-19 vaccination willingness at present.
METHODS
Study setting: the Canadian Longitudinal Study on Aging
The Canadian Longitudinal Study on Aging (CLSA) is a nationally representative cohort study of 51,338 Canadian residents living in 10 provinces and aged 45–85 years at enrollment (2011–2015). Participants are followed every 3 years and complete biological, medical, psychological, social, lifestyle, and economic assessments. In total, 48,893 CLSA participants had completed follow-up 1 (95% retention) by mid-2018; the follow-up 2 visit was completed in 2021. CLSA methods are described in detail elsewhere (15–18).
Study design: the CLSA COVID-19 Questionnaire Study
We designed the CLSA COVID-19 Questionnaire Study to investigate the impact of the COVID-19 pandemic on the physical, mental, social, and economic well-being of Canadian adults (19–23). All 42,700 accessible CLSA participants were invited to participate in the COVID-19 Questionnaire Study (8,638 were not invited because they had died (n = 2,500), had withdrawn (n = 3,406), required a proxy (n = 318), or had no current contact information (or some other reason prevented contact) (n = 2,414)). The 34,498 participants with e-mail addresses were e-mailed and invited to participate online; the remaining 8,202 were contacted by telephone and invited to participate by phone. During recruitment, we found that 166 participants had died since the last contact and 23 required a proxy. Of the resulting 42,511 eligible CLSA participants invited to take part in the COVID-19 study, 28,559 (67.2%) consented. Participants did not receive compensation for participating.
The COVID-19 baseline survey was launched on April 15, 2020; participants were asked to complete multiple surveys throughout 2020. At the end of 2020, participants were asked to complete a COVID-19 exit survey. Survey questions and response options relevant to this analysis were designed on the basis of prior studies of COVID-19 vaccination willingness, prior studies of factors driving influenza vaccine uptake among older Canadians, and our expertise in conducting vaccination surveys. All core CLSA and COVID-19 questionnaires are available online (24). The core CLSA and the CLSA COVID-19 Questionnaire Study were approved by research ethics boards at all collaborating Canadian institutions.
We assessed the distribution of key demographic factors among all CLSA participants eligible for the COVID-19 Questionnaire Study, all participants who consented to take part in the COVID-19 Questionnaire Study, and all participants who completed the COVID-19 exit survey (see Web Table 1, available at https://doi.org/10.1093/aje/kwac029). The distributions of participants by age group, sex, and province were very similar between eligible CLSA participants and those who completed the CLSA COVID-19 exit survey, with slightly higher response among those aged 65–74 years (36.5% vs. 33.3%) and females (53.2% vs. 51.3%).
Data source: CLSA COVID-19 Questionnaire Study exit survey
To assess COVID-19 vaccination willingness, we analyzed data collected during the COVID-19 Questionnaire Study exit survey, which was conducted between September 29 and December 29, 2020.
Self-reported likelihood of receiving a COVID-19 vaccine.
For our primary outcome, we assessed participants’ self-reported likelihood of receiving a COVID-19 vaccine. The participants were asked, “If a safe and effective COVID-19 vaccine were available to you, how likely would you be to choose to get the vaccine?”. Responses were categorized as “likely” if the respondent selected very or somewhat likely, and “unlikely” if they selected very or somewhat unlikely or uncertain. Participants who declared that they were likely to receive a COVID-19 vaccine were asked to select the primary reason that they would receive the vaccine from 6 options, including “other” (see Web Table 2). Participants who declared that they were unlikely to receive a COVID-19 vaccine were similarly asked to select their primary reason from 8 options, including “other.”
Sociodemographic factors.
We aimed to examine the relationship between willingness to receive a COVID-19 vaccine and the following: age group (50–54, 55–64, 65–74, or ≥75 years), sex at birth (male or female), race (White or other), highest educational level (less than secondary school graduation, secondary school graduation, some postsecondary education, or postsecondary degree/diploma), annual household income (in Canadian dollars; <$20,000, $20,000–$49,999, $50,000–$99,999, $100,000–$149,999, or ≥$150,000), province of residence (10 provinces), and urbanicity of residence (urban or rural location). Data on age, province, and urbanicity were collected via the COVID-19 exit survey. Data on sex, race, and highest educational level were collected during the CLSA baseline visit; the most recent income data were from CLSA follow-up 1. These variables were used under the assumption that they remained reasonably stable among older adults over this period. Similar to the demographic characteristics of the Canadian population aged 50 years or older, a small proportion of survey participants self-identified as a race other than White; thus, the race variable was dichotomized.
Uptake of influenza vaccine, belief about prior SARS-CoV-2 infection, and perception of the pandemic’s impact.
We also assessed whether factors beyond sociodemographic characteristics were associated with willingness to receive a COVID-19 vaccine. Specifically, we assessed the association between COVID-19 vaccination willingness and 1) self-reported influenza vaccine uptake (fall 2020), 2) belief that one was previously infected with SARS-CoV-2, and 3) perception of the impact of the COVID-19 pandemic on oneself and one’s household (Web Table 3). To assess influenza vaccination status in fall 2020, we asked participants to report whether they had received influenza vaccine between September 1, 2020, and the time of the survey, had not received influenza vaccine at the time of the survey but planned to, or did not plan to receive influenza vaccine. To assess participants’ belief in their prior SARS-CoV-2 infection status, we asked participants to report how likely they thought it was that they had been infected with the virus that causes COVID-19. Those who indicated that it was very or somewhat likely were categorized as “believing it was likely” they had been infected, those who selected “uncertain” remained in that category, and those who selected somewhat or very unlikely were categorized as “believing it was unlikely” they had been infected (Web Table 3). We chose to use these responses rather than actual SARS-CoV-2 test results because individuals’ perceived infection status was of primary interest, as it directly relates to an individual’s perception of their own risk; there were concerns that those who believed they had been infected already would fail to get vaccinated. To assess perceptions about the impact of the COVID-19 pandemic, we asked participants, “Taking everything about COVID-19 into account, how would you describe the consequences of COVID-19 on you and your household?”. Participants who selected very negative or negative were categorized as experiencing “negative consequences,” those who selected “no effect” remained in that category, and those who selected very positive or positive were categorized as experiencing “positive consequences” (Web Table 3). We hypothesized a priori that recent history of influenza vaccination, believing it was unlikely that one had been infected with SARS-CoV-2, and experiencing negative consequences due to the pandemic would be associated with a greater willingness to receive a COVID-19 vaccine.
Statistical analyses
Descriptive statistics (proportions and 95% CIs based on logit transformation) were used to characterize participants by 1) their likelihood of receiving a COVID-19 vaccine and 2) their primary reason for being likely or unlikely to receive a COVID-19 vaccine according to the sociodemographic characteristics described above. We used logistic regression and report adjusted odds ratios (aORs) and 95% CIs from assessment of the following associations. First, we assessed the association between demographic characteristics and self-reported likelihood of receiving a COVID-19 vaccine to determine which characteristics were most strongly associated with COVID-19 vaccination willingness. Next, we assessed the association between the 3 covariates about which we had hypothesized a priori and participants’ likelihood of receiving a COVID-19 vaccine: 1) influenza vaccination status (fall 2020), 2) belief about one’s prior infection with SARS-CoV-2, and 3) perception about the impact of the COVID-19 pandemic on oneself and one’s household. This model adjusted for all sociodemographic covariates (specified a priori). Participants with missing data about COVID-19 vaccination willingness were excluded from the analyses, as were participants with missing covariate data (they are included in the descriptive tables for completeness). Sampling weights for the CLSA COVID-19 Questionnaire Study have not been constructed; thus, the 95% CIs capture the precision of the estimates in the sample and reflect what they would be if the sample were a random sample of the Canadian population aged 50 years or older. Analyses were conducted using STATA, version 17.1 (StataCorp LLC, College Station, Texas).
RESULTS
Characteristics of participants
Of the 24,112 participants in the CLSA COVID-19 exit survey, 293 did not respond to the question about their likelihood of receiving a COVID-19 vaccine, and thus were excluded from the analysis. Among the 23,819 participants who reported their likelihood of receiving a COVID-19 vaccine, ages ranged from 50 years to 96 years (median, 68 years), 53.0% (n = 12,633) were female, and 96.1% (n = 22,887) were White. The largest proportions of participants had a postsecondary degree/diploma (78.3%; n = 18,658), reported annual income between Can$50,000 and Can$99,999 (35.6%; n = 8,474), resided in Ontario (23.2%; n = 5,526), and lived in an urban setting (81.7%; n = 19,467) (Table 1).
Table 1.
Demographic Characteristics of the 23,819 Participants Who Completed the CLSA COVID-19 Questionnaire Study Exit Survey Between September and December 2020 and Reported Their Likelihood of Receiving a COVID-19 Vaccine
| Total | Likely to Receive COVID-19 Vaccine | Unlikely to Receive COVID-19 Vaccine | ||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | No. | % | No. | % | 95% CI | No. | % | 95% CI |
| Total | 23,819 | 100.0 | 20,044 | 84.1 | 83.7, 84.6 | 3,775 | 15.9 | 15.4, 16.3 |
| Age group, years | ||||||||
| 50–54 | 1,096 | 4.6 | 902 | 82.3 | 79.9, 84.4 | 194 | 17.7 | 15.6, 20.1 |
| 55–64 | 7,219 | 30.3 | 5,887 | 81.5 | 80.6, 82.4 | 1,332 | 18.5 | 17.6, 19.4 |
| 65–74 | 8,707 | 36.6 | 7,491 | 86.0 | 85.3, 86.7 | 1,216 | 14.0 | 13.3, 14.7 |
| ≥75 | 6,797 | 28.5 | 5,764 | 84.8 | 83.9, 85.6 | 1,033 | 15.2 | 14.4, 16.1 |
| Sex at birth | ||||||||
| Male | 11,186 | 47.0 | 9,898 | 88.5 | 87.9, 89.1 | 1,288 | 11.5 | 10.9, 12.1 |
| Female | 12,633 | 53.0 | 10,146 | 80.3 | 79.6, 81.0 | 2,487 | 19.7 | 19.0, 20.4 |
| Highest educational level | ||||||||
| Less than secondary school graduation | 1,082 | 4.5 | 790 | 73.0 | 70.3, 75.6 | 292 | 27.0 | 24.4, 29.7 |
| Secondary school graduation | 2,329 | 9.8 | 1,808 | 77.6 | 75.9, 79.3 | 521 | 22.4 | 20.7, 24.1 |
| Some postsecondary education | 1,703 | 7.2 | 1,389 | 81.6 | 79.6, 83.4 | 314 | 18.4 | 16.7, 20.4 |
| Postsecondary degree/diploma | 18,658 | 78.3 | 16,025 | 85.9 | 85.4, 86.4 | 2,633 | 14.1 | 13.6, 14.6 |
| Not available | 47 | 0.2 | 32 | 68.1 | 53.6, 79.8 | 15 | 31.9 | 20.2, 46.4 |
| Annual household income, Can$ | ||||||||
| <20,000 | 832 | 3.5 | 566 | 68.0 | 64.8, 71.1 | 266 | 32.0 | 28.9, 35.2 |
| 20,000–49,999 | 4,779 | 20.1 | 3,740 | 78.3 | 77.1, 79.4 | 1,039 | 21.7 | 20.6, 22.9 |
| 50,000–99,999 | 8,474 | 35.6 | 7,243 | 85.5 | 84.7, 86.2 | 1,231 | 14.5 | 13.8, 15.3 |
| 100,000–149,999 | 4,555 | 19.1 | 3,997 | 87.7 | 86.8, 88.7 | 558 | 12.3 | 11.3, 13.2 |
| ≥150,000 | 3,731 | 15.7 | 3,385 | 90.7 | 89.8, 91.6 | 346 | 9.3 | 8.4, 10.2 |
| Not available | 1,448 | 6.1 | 1,113 | 76.9 | 74.6, 79.0 | 335 | 23.1 | 21.0, 25.4 |
| Race | ||||||||
| Non-White | 903 | 3.8 | 674 | 74.6 | 71.7, 77.4 | 229 | 25.4 | 22.6, 28.3 |
| White | 22,887 | 96.1 | 19,346 | 84.5 | 84.0, 85.0 | 3,541 | 15.5 | 15.0, 15.9 |
| Not available | 29 | 0.1 | 24 | 82.8 | 64.7, 92.6 | 5 | 17.2 | 5.4, 35.3 |
| Province of residence | ||||||||
| Newfoundland | 1,356 | 5.7 | 1,160 | 85.5 | 83.6, 87.3 | 196 | 14.5 | 12.7, 16.4 |
| Prince Edward Island | 383 | 1.6 | 319 | 83.3 | 79.2, 86.7 | 64 | 16.7 | 13.3, 20.8 |
| Nova Scotia | 2,135 | 9.0 | 1,885 | 88.3 | 86.9, 89.6 | 250 | 11.7 | 10.4, 13.1 |
| New Brunswick | 450 | 1.9 | 363 | 80.7 | 76.8, 84.1 | 87 | 19.3 | 15.9, 23.2 |
| Quebec | 4,282 | 18.0 | 3,425 | 80.0 | 78.8, 81.2 | 857 | 20.0 | 18.8, 21.2 |
| Ontario | 5,526 | 23.2 | 4,702 | 85.1 | 84.1, 86.0 | 824 | 14.9 | 14.0, 15.9 |
| Manitoba | 2,150 | 9.0 | 1,804 | 83.9 | 82.3, 85.4 | 346 | 16.1 | 14.6, 17.7 |
| Saskatchewan | 565 | 2.4 | 458 | 81.1 | 77.6, 84.2 | 107 | 18.9 | 15.8, 22.4 |
| Alberta | 2,382 | 10.0 | 1,960 | 82.3 | 80.7, 83.8 | 422 | 17.7 | 16.2, 19.3 |
| British Columbia | 4,590 | 19.3 | 3,968 | 86.4 | 85.4, 87.4 | 622 | 13.6 | 12.6, 14.6 |
| Urbanicity of residence | ||||||||
| Rural area | 4,228 | 17.8 | 3,340 | 79.0 | 77.7, 80.2 | 888 | 21.0 | 19.8, 22.3 |
| Urban area | 19,467 | 81.7 | 16,598 | 85.3 | 84.8, 85.8 | 2,869 | 14.7 | 14.2, 15.2 |
| Not available | 124 | 0.5 | 106 | 85.5 | 78.1, 90.7 | 18 | 14.5 | 9.3, 21.9 |
Abbreviations: CI, confidence interval; CLSA, Canadian Longitudinal Study on Aging; COVID-19, coronavirus disease 2019.
Self-reported likelihood of receiving a COVID-19 vaccine
The majority of participants (72.7%, 95% CI: 72.1, 73.3; n = 17,314) reported that they were very likely to receive a COVID-19 vaccine; 11.5% (95% CI: 11.1, 11.9; n = 2,730) were somewhat likely, 9.9% (95% CI: 9.5, 10.3; n = 2,352) were uncertain, 1.8% (95% CI: 1.6, 1.9; n = 420) were somewhat unlikely, and 4.2% (95% CI: 4.0, 4.5; n = 1,003) were very unlikely. Within every sociodemographic stratum, the majority indicated that they were very likely to receive a COVID-19 vaccine (Web Figures 1–3). Higher proportions of those who were very unlikely to receive a COVID-19 vaccine were in the 2 younger age groups (50–54 years (5.9%, 95% CI: 4.5, 7.3) and 55–64 years (5.6%, 95% CI: 5.1, 6.1)) as compared with the 2 older age groups (65–74 years (3.7%, 95% CI: 3.3, 4.1) and ≥75 years (3.1%, 95% CI: 2.7, 3.6)), were female (5.1%, 95% CI: 4.8, 5.5) as compared with male (3.2%, 95% CI: 2.8, 3.5), were non-White (7.6%, 95% CI: 5.9, 9.4) as compared with White (4.1%, 95% CI: 3.8, 4.3), had less education (7.0% (95% CI: 5.5, 8.5) with less than secondary school completion) as compared with more education (3.8% (95% CI: 3.5, 4.1) with a postsecondary degree/diploma), had lower income (9.6% (95% CI: 7.6, 11.6) with income <Can$20,000/year) as compared with higher income (2.4% (95% CI: 1.9, 2.9) with income ≥Can$150,000/year), and lived in a rural area (5.4%, 95% CI: 5.6, 7.1) as compared with an urban area (3.7%, 95% CI: 3.5, 4.0) (Web Figures 1–3). Overall, 84.1% (95% CI: 83.7, 84.6) of participants reported that they were very likely or somewhat likely to get a COVID-19 vaccine, while 15.9% (95% CI: 15.4, 16.3) were uncertain, very unlikely, or somewhat unlikely to get a COVID-19 vaccine (Table 1).
Primary reasons for being likely or unlikely to receive a COVID-19 vaccine
Among the 20,044 participants (84.2% of total) who were very/somewhat likely to receive a COVID-19 vaccine, 83 (0.4%) did not select a reason. Among those who gave responses (n = 19,961), most selected “I want to protect myself” (37.5%; n = 7,482), “I want to protect my family and loved ones” (25.7%; n = 5,124), or “I want to contribute to ending COVID-19 outbreaks” (24.0%; n = 4,796). (See all reasons, stratified by demographic factors, in Web Table 2.) Among the 3,775 participants (15.9% of total) who were uncertain or somewhat/very unlikely to receive a COVID-19 vaccine, 91 (2.4%) did not select a reason. Of the 3,684 with complete responses, the most common reason was “I am concerned about the safety of the vaccine” (64.2%; n = 2,365), followed by “I am concerned about how well the vaccine will protect” (18.4%; n = 677) and “other” (8.2%; n = 302). The distribution of reasons motivating persons who reported that they were unlikely to receive a COVID-19 vaccine is shown in Table 2 by demographic characteristics.
Table 2.
Distribution of Self-Reported Reasons for Being Very or Somewhat Unlikely to Receive a COVID-19 Vaccine Among 3,684 Individuals Who Participated in the CLSA COVID-19 Questionnaire Study Exit Survey, September–December 2020a
| Primary Reason for Being Unlikely to Receive COVID-19 Vaccine | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I Am Not Concerned About Getting COVID-19 Myself | I Am Not Concerned That My Family or Loved Ones Are at Risk for Getting COVID-19 | I Am Not Concerned About COVID-19 in General | I Am Concerned About the Safety of the Vaccine | I Am Concerned About How Well the Vaccine Will Protect | I Am Concerned About the Cost of the Vaccine | I Do Not Like Needles | Other | ||||||||||
| Characteristic | Total No. of Respondents | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| Total | 3,684 | 3.1 | 2.6, 3.7 | 0.6 | 0.4, 0.9 | 4.2 | 3.6, 4.9 | 64.2 | 62.6, 65.7 | 18.4 | 17.2, 19.7 | 0.3 | 0.1, 0.5 | 1.0 | 0.7, 1.4 | 8.2 | 7.4, 9.1 |
| Age group, years | |||||||||||||||||
| 50–54 | 188 | 4.3 | 2.1, 8.3 | 0.5 | 0.1, 3.7 | 8.0 | 4.9, 12.8 | 63.3 | 56.2, 69.9 | 14.9 | 10.5, 20.7 | 0.0 | NE | 0.0 | NE | 9.0 | 5.7, 14.1 |
| 55–64 | 1,304 | 2.6 | 1.9, 3.6 | 0.5 | 0.3, 1.1 | 5.8 | 4.6, 7.2 | 64.4 | 61.8, 67.0 | 18.6 | 16.6, 20.8 | 0.3 | 0.1, 0.8 | 0.6 | 0.3, 1.2 | 7.1 | 5.9, 8.7 |
| 65–74 | 1,194 | 2.7 | 1.9, 3.8 | 0.4 | 0.2, 1.0 | 3.6 | 2.7, 4.8 | 65.7 | 62.9, 68.3 | 19.7 | 17.5, 22.0 | 0.3 | 0.1, 0.8 | 0.8 | 0.4, 1.4 | 7.0 | 5.6, 8.5 |
| ≥75 | 998 | 4.1 | 3.0, 5.5 | 1.0 | 0.5, 1.9 | 2.3 | 1.5, 3.4 | 62.3 | 59.3, 65.3 | 17.1 | 14.9, 19.6 | 0.3 | 0.1, 0.9 | 1.9 | 1.2, 3.0 | 10.9 | 9.1, 13.0 |
| Sex at birth | |||||||||||||||||
| Male | 1,256 | 5.5 | 4.4, 6.9 | 0.5 | 0.2, 1.1 | 7.3 | 6.0, 8.9 | 59.0 | 56.3, 61.7 | 20.2 | 18.1, 22.5 | 0.2 | 0.0, 0.6 | 1.0 | 0.5, 1.7 | 6.4 | 5.1, 7.9 |
| Female | 2,428 | 1.9 | 1.4, 2.5 | 0.7 | 0.4, 1.1 | 2.6 | 2.1, 3.4 | 66.9 | 65.0, 68.7 | 17.4 | 16.0, 19.0 | 0.3 | 0.2, 0.7 | 1.0 | 0.7, 1.5 | 9.1 | 8.1, 10.4 |
| Educational level | |||||||||||||||||
| Less than secondary school graduation | 279 | 5.0 | 3.0, 8.3 | 0.4 | 0.1, 2.5 | 4.7 | 2.7, 7.9 | 58.8 | 52.9, 64.4 | 16.1 | 12.3, 20.9 | 0.7 | 0.2, 2.8 | 2.5 | 1.2, 5.2 | 11.8 | 8.5, 16.2 |
| Secondary school graduation | 506 | 3.8 | 2.4, 5.8 | 0.6 | 0.2, 1.8 | 4.5 | 3.0, 6.7 | 61.3 | 56.9, 65.4 | 20.6 | 17.3, 24.3 | 0.2 | 0.0, 1.4 | 1.6 | 0.8, 3.1 | 7.5 | 5.5, 10.2 |
| Some postsecondary education | 308 | 2.6 | 1.3, 5.1 | 0.0 | NE | 2.6 | 1.3, 5.1 | 72.4 | 67.1, 77.1 | 11.4 | 8.3, 15.4 | 0.3 | 0.0, 2.3 | 0.6 | 0.2, 2.6 | 10.1 | 7.2, 14.0 |
| Postsecondary degree/diploma | 2,577 | 2.9 | 2.3, 3.6 | 0.7 | 0.5, 1.2 | 4.3 | 3.6, 5.2 | 64.3 | 62.5, 66.2 | 19.1 | 17.6, 20.6 | 0.2 | 0.1, 0.5 | 0.7 | 0.5, 1.2 | 7.7 | 6.8, 8.8 |
| Not available | 14 | 0.0 | NE | 0.0 | NE | 7.1 | 1.0, 37.1 | 71.4 | 43.9, 88.9 | 14.3 | 3.6, 42.7 | 0.0 | NE | 0.0 | NE | 7.1 | 1.0, 37.1 |
| Annual household income, Can$ | |||||||||||||||||
| <20,000 | 256 | 5.5 | 3.3, 9.0 | 0.0 | NE | 3.5 | 1.8, 6.6 | 58.2 | 52.1, 64.1 | 18.0 | 13.7, 23.2 | 0.8 | 0.2, 3.1 | 1.6 | 0.6, 4.1 | 12.5 | 9.0, 17.1 |
| 20,000–49,999 | 1,010 | 2.7 | 1.8, 3.9 | 0.6 | 0.3, 1.3 | 4.3 | 3.2, 5.7 | 60.3 | 57.2, 63.3 | 20.5 | 18.1, 23.1 | 0.2 | 0.0, 0.8 | 1.6 | 1.0, 2.6 | 9.9 | 8.2, 11.9 |
| 50,000–99,999 | 1,201 | 3.1 | 2.2, 4.2 | 0.7 | 0.4, 1.4 | 4.1 | 3.1, 5.4 | 65.4 | 62.6, 68.0 | 19.3 | 17.2, 21.6 | 0.2 | 0.0, 0.7 | 0.8 | 0.4, 1.5 | 6.4 | 5.2, 7.9 |
| 100,000–149,999 | 548 | 3.1 | 1.9, 4.9 | 0.4 | 0.1, 1.4 | 4.7 | 3.2, 6.9 | 66.8 | 62.7, 70.6 | 16.2 | 13.4, 19.6 | 0.2 | 0.0, 1.3 | 0.4 | 0.1, 1.4 | 8.2 | 6.2, 10.8 |
| ≥150,000 | 341 | 1.8 | 0.8, 3.9 | 0.9 | 0.3, 2.7 | 4.4 | 2.7, 7.2 | 71.6 | 66.5, 76.1 | 15.8 | 12.3, 20.1 | 0.0 | NE | 0.3 | 0.0, 2.1 | 5.3 | 3.3, 8.2 |
| Not available | 328 | 4.3 | 2.5, 7.1 | 0.9 | 0.3, 2.8 | 4.3 | 2.5, 7.1 | 64.6 | 59.3, 69.9 | 14.9 | 11.5, 19.2 | 0.9 | 0.3, 2.8 | 0.9 | 0.3, 2.8 | 9.1 | 6.5, 12.8 |
| Race | |||||||||||||||||
| Non-White | 223 | 3.6 | 1.8, 7.0 | 0.0 | NE | 5.4 | 3.1, 9.2 | 65.9 | 59.5, 71.8 | 15.7 | 11.5, 21.1 | 0.9 | 0.2, 3.5 | 2.2 | 0.9, 5.3 | 6.3 | 3.8, 10.8 |
| White | 3,456 | 3.1 | 2.6, 3.7 | 0.7 | 0.4, 1.0 | 4.1 | 3.5, 4.9 | 64.1 | 62.4, 65.6 | 18.6 | 17.3, 19.9 | 0.2 | 0.1, 0.5 | 0.9 | 0.6, 1.3 | 8.3 | 7.5, 9.3 |
| Not available | 5 | 0.0 | NE | 0.0 | NE | 20.0 | 2.7, 69.1 | 80.0 | 30.9, 97.3 | 0.0 | NE | 0.0 | NE | 0.0 | NE | 0.0 | 0.0 |
| Province of residence | |||||||||||||||||
| Newfoundland | 194 | 4.7 | 2.4, 8.7 | 1.0 | 0.3, 4.0 | 4.1 | 2.1, 8.1 | 62.7 | 55.7, 69.2 | 16.1 | 11.5, 21.9 | 0.0 | NE | 2.1 | 0.8, 5.4 | 9.3 | 6.0, 14.3 |
| Prince Edward Island | 64 | 4.7 | 1.5, 13.6 | 0.0 | NE | 4.7 | 1.5, 13.6 | 64.1 | 51.7, 74.8 | 17.2 | 9.8, 28.4 | 0.0 | NE | 1.6 | 0.2, 10.3 | 7.8 | 3.3, 17.4 |
| Nova Scotia | 243 | 2.1 | 0.9, 4.8 | 0.4 | 0.1, 2.9 | 4.9 | 2.8, 8.5 | 62.1 | 55.9, 68.0 | 21.0 | 16.3, 26.6 | 0.4 | 0.1, 2.9 | 0.4 | 0.1, 2.9 | 8.6 | 5.7, 12.9 |
| New Brunswick | 86 | 4.7 | 1.8, 11.7 | 0.0 | NE | 2.3 | 0.6, 8.8 | 72.1 | 61.7, 80.5 | 11.6 | 5.6, 20.3 | 0.0 | NE | 1.2 | 0.2, 7.8 | 8.1 | 3.9, 16.1 |
| Quebec | 831 | 2.2 | 1.4, 3.4 | 1.0 | 0.5, 1.9 | 6.3 | 4.8, 8.1 | 53.4 | 50.0, 56.8 | 27.8 | 24.9, 30.9 | 0.2 | 0.1, 1.0 | 0.8 | 0.4, 1.8 | 8.3 | 6.6, 10.4 |
| Ontario | 808 | 3.6 | 2.5, 5.1 | 0.5 | 0.2, 1.3 | 1.9 | 1.1, 3.1 | 69.8 | 66.5, 72.9 | 15.7 | 13.4, 18.4 | 0.2 | 0.1, 1.0 | 1.2 | 0.7, 2.3 | 7.1 | 5.5, 9.0 |
| Manitoba | 338 | 3.0 | 1.6, 5.4 | 0.3 | 0.0, 2.1 | 3.3 | 1.8, 5.8 | 70.1 | 65.0, 74.8 | 13.6 | 10.3, 17.7 | 0.0 | NE | 1.5 | 0.6, 3.5 | 8.3 | 5.8, 11.7 |
| Saskatchewan | 105 | 2.9 | 0.9, 8.5 | 1.9 | 0.5, 7.3 | 8.6 | 4.5, 15.7 | 64.8 | 55.2, 73.3 | 11.4 | 6.6, 19.1 | 0.0 | NE | 1.0 | 0.1, 6.5 | 9.5 | 5.2, 16.8 |
| Alberta | 414 | 3.1 | 1.8, 5.3 | 0.2 | 0.0, 1.7 | 4.8 | 3.1, 7.4 | 69.6 | 65.0, 73.8 | 14.3 | 11.2, 18.0 | 0.5 | 0.1, 1.9 | 0.7 | 0.2, 2.2 | 6.8 | 4.7, 9.6 |
| British Columbia | 602 | 3.5 | 2.3, 5.3 | 0.7 | 0.2, 1.8 | 4.0 | 2.7, 5.9 | 64.6 | 60.7, 68.3 | 16.4 | 13.7, 19.6 | 0.5 | 0.2, 1.5 | 0.5 | 0.2, 1.5 | 9.8 | 7.7, 12.4 |
| Urbanicity of residence | |||||||||||||||||
| Rural area | 871 | 3.1 | 2.1,4.5 | 0.8 | 0.4, 1.7 | 4.9 | 3.7, 6.6 | 60.4 | 57.1, 63.6 | 20.4 | 17.9, 23.2 | 0.2 | 0.1, 0.9 | 1.3 | 0.7, 2.3 | 8.8 | 7.1, 10.9 |
| Urban area | 2,795 | 3.1 | 2.5, 3.8 | 0.6 | 0.4, 0.9 | 4.0 | 3.4, 4.8 | 65.5 | 63.7, 67.2 | 17.7 | 16.4, 19.2 | 0.3 | 0.1, 0.5 | 0.9 | 0.6, 1.3 | 7.9 | 7.0, 9.0 |
| Not available | 18 | 5.6 | 0.8, 30.7 | 0.0 | NE | 0.0 | NE | 50.0 | 28.4, 71.6 | 16.7 | 5.5, 40.9 | 5.6 | 0.8, 30.7 | 5.6 | 0.8, 30.7 | 16.7 | 5.5, 40.9 |
Abbreviations: CI, confidence interval; CLSA, Canadian Longitudinal Study on Aging; COVID-19, coronavirus disease 2019; NE, not estimable.
a Study participants who reported that they were uncertain, were somewhat unlikely, or were very unlikely to receive a COVID-19 vaccine selected their primary reason from a list of 7 options or selected “other.”
Factors associated with self-reported likelihood of receiving a COVID-19 vaccine
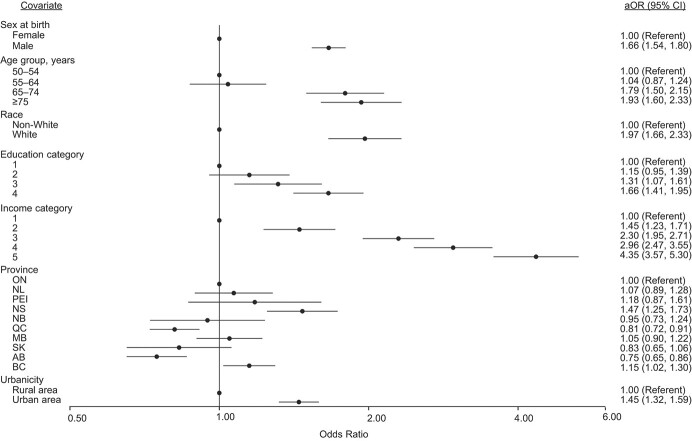
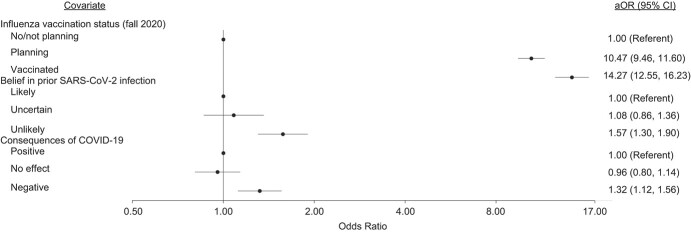
Individuals aged 65 years or older (versus younger), males (versus females), those who selected White race (versus any other race), those with a higher educational level (versus lower), those with higher income (versus lower), and those living in urban areas (versus rural areas) were significantly more likely to report willingness to receive a COVID-19 vaccine (see Figure 1 for aORs and 95% CIs). Regarding the association between self-reported influenza vaccination status during fall 2020 and likelihood of receiving a COVID-19 vaccine, we found that 30.2% (n = 7,192) of participants had received influenza vaccine early in the 2020 season, 51.2% (n = 12,201) planned to receive it, and 17.7% (n = 4,221) did not plan to receive it (Web Table 4). After accounting for all demographic factors, those who had received influenza vaccine (aOR = 14.3, 95% CI: 12.5, 16.2) and those planning to receive an influenza vaccine (aOR = 10.5, 95% CI: 9.5, 11.6) were significantly more likely to be willing to receive a COVID-19 vaccine than those who did not receive or plan to receive influenza vaccine (Figure 2).
Figure 1.
Association between sociodemographic characteristics and being likely to receive a coronavirus disease 2019 (COVID-19) vaccine among 22,183 participants responding to the CLSA COVID-19 Questionnaire Study exit survey, September–December 2020. Adjusted odds ratios (aORs), shown as dots, and 95% confidence intervals (CIs), shown as bars, were drawn from a logistic regression model based on participants who had complete data and are plotted on the logarithmic scale. Education refers to highest attained educational level, categorized as follows: less than secondary school graduation (category 1); secondary school graduation, no postsecondary education (category 2); some postsecondary education (category 3); and postsecondary degree/diploma (category 4). Income refers to annual household income in Canadian dollars, categorized as follows: <$20,000 (category 1); $20,000–$49,999 (category 2); $50,000–$99,999 (category 3); $100,000–$149,000 (category 4); and ≥$150,000 (category 5). AB, Alberta; BC, British Columbia; CLSA, Canadian Longitudinal Study on Aging; MB, Manitoba; NB, New Brunswick; NL, Newfoundland; NS, Nova Scotia; ON, Ontario; PEI, Prince Edward Island; QC, Quebec; SK, Saskatchewan.
Figure 2.
Association between prior influenza vaccination and coronavirus disease 2019 (COVID-19)-pandemic–specific factors and being likely to receive a COVID-19 vaccine among 20,990 participants in the CLSA COVID-19 Questionnaire Study exit survey, September–December 2020. Associations are shown for 3 covariates of interest: self-reported influenza vaccination status during the 2020–2021 influenza season, belief in having been infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) previously, and impact of the COVID-19 pandemic on the participant and their household. Adjusted odds ratios (aORs), shown as dots, and 95% confidence intervals (CIs), shown as bars, were drawn from a logistic regression model based on participants who had complete data and are plotted on a logarithmic scale. We estimated aORs from a model that adjusted for age, sex, race, education, income, province, and urbanicity of residence, as described in the Methods section of the text. CLSA, Canadian Longitudinal Study on Aging.
With regard to participants’ beliefs about their SARS-CoV-2 infection history, 4.5% (n = 1,063) of respondents believed it was likely they had been infected with the virus that causes COVID-19, 87.4% (n = 20,487) believed it was unlikely, and 8.1% (n = 1,893) were uncertain (Web Table 4). After accounting for all demographic factors, those who believed they were unlikely to have been infected were significantly more likely (aOR = 1.6, 95% CI: 1.3, 1.9) to be willing to receive a COVID-19 vaccine than those who believed they had already been infected (Figure 2).
Finally, with respect to the impact of the COVID-19 pandemic, we found that 61.0% (n = 14,529) of participants reported overall negative consequences, 6.4% (n = 1,534) reported positive consequences, and 29.1% (n = 6,941) indicated there had been no effect (Web Table 4). After accounting for all demographic factors, those who reported a negative overall impact were significantly more likely (aOR = 1.3, 95% CI: 1.1, 1.6) to be willing to receive a COVID-19 vaccine than those who believed the consequences had been positive overall (Figure 2). The unadjusted odds ratios for each association described are given in Web Tables 5 and 6.
DISCUSSION
Health Canada first authorized a COVID-19 vaccine for use in Canada in December 2020, and throughout 2021, COVID-19 vaccines were widely available. We conducted a rigorous and in-depth assessment of self-reported willingness to receive a COVID-19 vaccine using a large, established cohort to determine which groups are least likely to be vaccinated and thus would benefit most from outreach and resource allocation to improve uptake. While we found that 84.1% of Canadian adults aged 50 years or older reported that they were likely to receive a COVID-19 vaccine, willingness varied in important ways. Notably, we found that adults who were 50–64 years of age, female, non-White, less educated, lower-income, and living in rural areas were significantly less likely to be willing to be vaccinated. While much attention has been devoted to vaccination uptake by sociodemographic group in Canada and elsewhere, the differences between subgroups that we found were relatively small. After controlling for these demographic characteristics, receipt of influenza vaccine in fall 2020 (aOR = 14.3, 95% CI: 12.5, 16.2) or plans to receive influenza vaccine (aOR = 10.5, 95% CI: 9.5, 11.6) were both most strongly associated with COVID-19 vaccination willingness. In our investigation of reasons that underlie willingness or lack of willingness to be vaccinated, which took place prior to any COVID-19 vaccine approval, we found that the safety of COVID-19 vaccines was the primary concern identified by a majority of uncertain or unwilling participants, followed by concerns about vaccine effectiveness. In addition, those who believed that they had already been infected with SARS-CoV-2 were less willing to receive a COVID-19 vaccine, suggesting perhaps that they believe they are already protected or that they may be unaware that COVID-19 vaccination is recommended regardless of prior infection. Finally, we found that those who categorized the impact of the COVID-19 pandemic on themselves and their households as positive overall were also less likely to be willing to be vaccinated.
Our assessment of COVID-19 vaccination willingness prior to vaccine introduction aligns very closely with current uptake of COVID-19 vaccination in Canada by age group as of January 22, 2022, given that 88.8% of adults aged 50–59 years (versus 80.8% who were very/somewhat likely and 10.6% who were uncertain in our study; total 91.4%), 92.8% of those aged 60–69 years (versus 84.4% very/somewhat likely and 9.4% uncertain in our study; total 93.8%), 95.5% of those aged 70–79 years (versus 86.6% very/somewhat likely and 9.0% uncertain in our study; total 95.6%), and 96.6% of those aged ≥80 years (versus 83.1% very/somewhat likely and 11.6% uncertain in our study; total 94.7%) have been fully vaccinated with a COVID-19 vaccine primary series (13). The fact that our results are quite similar to current vaccination uptake, which has largely plateaued, suggests that persons who said they were very or somewhat likely to get vaccinated in late 2020 probably got vaccinated when they became eligible. In addition, current uptake rates suggest that the majority of persons who were uncertain also got vaccinated.
Significant research conducted both prior to and during the COVID-19 pandemic has demonstrated that reasons for vaccine hesitancy are complex and multidimensional and that multiple factors may simultaneously promote or prevent vaccination (25). In our study, we aimed to characterize demographic and pandemic-related factors that are associated with a lack of willingness to receive a COVID-19 vaccine to provide an empirical basis for determining who may benefit most from dedicated efforts to increase willingness. It is clear that tailored public health outreach will be needed, though identifying interventions that could effectively increase uptake was beyond the scope of our study. However, by evaluating COVID-19 vaccination willingness among older Canadian adults in a setting where vaccine uptake is generally high, we identified those who were least likely to be willing to receive a COVID-19 vaccine, which provides insight into the epidemiology of vaccine willingness. Our finding that recent influenza vaccination was a key predictor of COVID-19 vaccination willingness is important and suggests that public health practitioners should consider complementary reasons why individuals fail to receive recommended influenza vaccine and have failed to receive COVID-19 vaccine despite availability. Multiple approaches have previously been used to address influenza vaccine hesitancy, including promotion of the community-wide benefits of vaccination (26, 27), which may prove valuable when developing novel approaches to improve COVID-19 vaccine uptake. Determining how to address a lack of vaccine willingness most effectively and how to combat misinformation was beyond the scope of this study; future research could build upon our results, which identified persons who would benefit most from interventions, and evaluate tailored interventions directly.
To our knowledge, this study is the largest COVID-19 vaccination willingness survey of older Canadian adults conducted to date, and it draws inference from an established national cohort rather than a convenience sample. We went beyond previous studies by recruiting a more broadly representative group of older adults, persons aged 50–96 years. For example, we did not limit the sample to those who had Internet access; 20% of eligible participants were contacted and invited to participate via phone. For these reasons, our study adds to previously published work concerning COVID-19 vaccination willingness. For example, in June 2020, Statistics Canada surveyed 4,000 Canadians aged 15 years or older (28). Like our study, that study identified safety concerns as the main reason for lack of willingness to get vaccinated; however, other important factors such as influenza vaccination or participants’ experience with respect to the COVID-19 pandemic were not investigated, and results were not stratified by other demographic characteristics. An online survey conducted in June 2020 in 19 countries, including Canada, with around 700 participants per country, found that 71.5% of respondents aged 18 years or older were very/somewhat likely to get vaccinated, though country-specific data were not presented and reasons behind self-reported likelihood of vaccination were not investigated (11). Comparability between studies of vaccination willingness is a challenge because of major differences in terms of design, setting, age groups, and other factors (29–31).
The primary limitations of our study are that we did not have information about participants’ vaccination decision once they became eligible for vaccination and that we could not investigate every possible reason for lack of COVID-19 vaccination willingness. As we noted above, vaccination rates in January 2022 were very similar to the proportions of persons we identified in 2020 who were very/somewhat likely to receive a COVID-19 vaccine, plus a proportion who were uncertain at that time. In addition, only 302 participants who were unwilling to receive a COVID-19 vaccine selected “other” as their primary reason, suggesting our survey presented reasons that resonated with the majority of participants in the last quarter of 2020 when these data were collected. Finally, these results may not be generalizable to other contexts, including those contexts where trust in vaccines is generally low, where vaccination has been highly politicized, or where lack of COVID-19 vaccine availability and access are primary barriers to uptake. Future studies could examine the role of other factors, such as perception of risk or having a chronic condition, and their association with COVID-19 vaccination willingness.
Studies examining COVID-19 vaccination willingness continue to be of utmost urgency. Where vaccination campaigns are in early stages, lessons learned from vaccination willingness studies can inform initial efforts before local data are available. In localities where vaccination campaigns have been ongoing and uptake has plateaued, as in Canada, significant investment is needed to conduct outreach to those most likely to continue to refuse vaccination without intervention. We provide a road map for these efforts by identifying persons who may benefit most from additional outreach, support, and resources to increase their willingness to be vaccinated. High COVID-19 vaccine uptake is the most powerful tool available for prevention and control of SARS-CoV-2, and public health officials, health professionals, and community leaders should pursue evidence-based approaches to increase vaccination willingness.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Biostatistics, and Occupational Health, Faculty of Medicine and Health Sciences, McGill University, Montreal, Quebec, Canada (Nicole E. Basta, Giorgia Sulis, Christina Wolfson); Department of Health Research Methods, Evidence and Impact, Faculty of Health Sciences, McMaster University, Hamilton, Ontario, Canada (Nazmul Sohel, Lauren E. Griffith, Parminder Raina); Department of Medicine, Faculty of Medicine and Health Sciences, McGill University, Montreal, Quebec, Canada (Christina Wolfson); CLSA Data Curation Centre, Research Institute of the McGill University Health Centre, Montreal, Quebec, Canada (Christina Wolfson, Geva Maimon); Labarge Centre for Mobility in Aging, McMaster University, Hamilton, Ontario, Canada (Lauren E. Griffith, Parminder Raina); McMaster Institute for Research on Aging, McMaster University, Hamilton, Ontario, Canada (Lauren E. Griffith, Parminder Raina); Department of Community Health and Epidemiology, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada (Susan Kirkland); Division of Geriatric Medicine, Department of Medicine, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada (Susan Kirkland); Department of Medicine, Faculty of Medicine, University of Calgary, Calgary, Alberta, Canada (Jacqueline M. McMillan); Department of Statistics and Actuarial Science, Faculty of Mathematics, University of Waterloo, Waterloo, Ontario, Canada (Mary Thompson); and Department of Psychiatry and Behavioral Neurosciences, Faculty of Health Sciences, McMaster University, Hamilton, Ontario, Canada (Parminder Raina).
The Canadian Longitudinal Study on Aging (CLSA) is led by Drs. Parminder Raina, Christina Wolfson, and Susan Kirkland.
Funding for the CLSA COVID-19 Questionnaire Study was provided by the Juravinski Research Institute, the Faculty of Health Sciences of McMaster University, the Provost Fund of McMaster University, the McMaster Institute for Research on Aging, the Public Health Agency of Canada, and the Nova Scotia COVID-19 Health Research Coalition. Funding for the CLSA is provided by the government of Canada through the Canadian Institutes of Health Research (grant LSA 94473) and the Canada Foundation for Innovation. N.E.B. holds a Tier 2 Canada Research Chair in Infectious Disease Prevention. L.E.G. is supported by the McLaughlin Foundation Professorship in Population and Public Health. P.R. holds the Raymond and Margaret Labarge Chair in Optimal Aging and Knowledge Application for Optimal Aging, is the Director of the McMaster Institute for Research on Aging and the Labarge Centre for Mobility in Aging, and holds a Tier 1 Canada Research Chair in Geroscience.
This research was conducted using the CLSA COVID-19 Questionnaire Study data, version 1; the CLSA baseline data, versions 3.7 (tracking cohort) and 5.2 (comprehensive cohort); and the CLSA follow-up 1 data, versions 2.2 (tracking cohort) and 3.0 (comprehensive cohort), accessed via the CLSA Consortium (CLSA Consortium no. 21CON001; P.R., Principal Investigator). Data are available from the CLSA investigators (www.clsa-elcv.ca) for researchers who meet the criteria for access to deidentified CLSA data. Custom software code that supports the results of this study can be made available upon request from the corresponding author.
We thank the CLSA Research Team: Drs. Andrew Costa, Laura Anderson, and Cynthia Balion (McMaster University, Hamilton, Ontario, Canada); Asada Yukiko (Dalhousie University, Halifax, Nova Scotia, Canada); Benoît Cossette and Melanie Levasseur (University of Sherbrooke, Sherbrooke, Quebec, Canada); Scott Hofer and Theone Paterson (University of Victoria, Victoria, British Columbia, Canada); David Hogan (University of Calgary, Calgary, Alberta, Canada); Teresa Liu-Ambrose (University of British Columbia, Vancouver, British Columbia, Canada); Verena Menec and Philip St. John (University of Manitoba, Winnipeg, Manitoba, Canada); Gerald Mugford and Zhiwei Gao (Memorial University of Newfoundland, St. Johns, Newfoundland, Canada); Vanessa Taler and Patrick Davidson (University of Ottawa, Ottawa, Ontario, Canada); and Andrew Wister and Theodore Cosco (Simon Fraser University, Burnaby, British Columbia, Canada).
The views expressed in this article are those of the authors and do not reflect those of the funding agencies.
Conflict of interest: none declared.
REFERENCES
- 1. Basta NE, Moodie EEM, McGill University COVID19 Vaccine Tracker Team . COVID19 Vaccine Tracker. Approved vaccines. https://covid19.trackvaccines.org/vaccines/approved/. Accessed October 1, 2021.
- 2. Levin AT, Hanage WP, Owusu-Boaitey N, et al. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020;35(12):1123–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Castro MC, Singer B. Prioritizing COVID-19 vaccination by age. Proc Natl Acad Sci U S A. 2021;118(15):e2103700118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Goldstein JR, Cassidy T, Wachter KW. Vaccinating the oldest against COVID-19 saves both the most lives and most years of life. Proc Natl Acad Sci U S A. 2021;118(11):e2026322118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ritchie H, Ortiz-Ospina E, Beltekian D, et al. Our World in Data. COVID-19: vaccination policy. https://ourworldindata.org/covid-vaccination-policy. Accessed October 1, 2021.
- 6. Ritchie H, Ortiz-Ospina E, Beltekian D, et al. Our World in Data. Coronavirus (COVID-19) vaccinations. https://ourworldindata.org/covid-vaccinations. Accessed October 1, 2021.
- 7. Wouters OJ, Shadlen KC, Salcher-Konrad M, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397(10278):1023–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization . Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. Published 2019. Accessed October 1, 2021.
- 9. Organisation for Economic Co-operation and Development . Influenza vaccination rates. https://data.oecd.org/healthcare/influenza-vaccination-rates.htm. Accessed October 1, 2021.
- 10. Public Health Agency of Canada . Seasonal Influenza Vaccination Coverage in Canada, 2019–2020. Ottawa, ON, Canada: Public Health Agency of Canada; 2020. [Google Scholar]
- 11. Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Statistics Canada . COVID-19 vaccine willingness among Canadian population groups. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2021001/article/00011-eng.htm. Published March 26, 2021. Modified August 20, 2021. Accessed October 1, 2021.
- 13. National Advisory Committee on Immunization, Public Health Agency of Canada . COVID-19 vaccination in Canada. https://health-infobase.canada.ca/covid-19/vaccination-coverage/. Updated January 22, 2022. Accessed January 28, 2022.
- 14. National Advisory Committee on Immunization, Public Health Agency of Canada . Guidance on the prioritization of key populations for COVID-19 immunization. https://open.canada.ca/data/en/dataset/2a2ac352-84aa-4b7b-9e14-43d9c8c28b15. Published February 12, 2021. Modified February 12, 2021. Accessed October 1, 2021.
- 15. Raina P, Wolfson C, Kirkland S, et al. Cohort profile: the Canadian Longitudinal Study on Aging (CLSA). Int J Epidemiol. 2019;48(6):1752–3j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kirkland SA, Griffith LE, Menec V, et al. Mining a unique Canadian resource: the Canadian Longitudinal Study on Aging. Can J Aging. 2015;34(3):366–377. [DOI] [PubMed] [Google Scholar]
- 17. Sakib MN, Shooshtari S, St John P, et al. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: an analysis of Canadian Longitudinal Study on Aging data. BMC Public Health. 2019;19(1):243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tuokko H, Griffith LE, Simard M, et al. Cognitive measures in the Canadian Longitudinal Study on Aging. Clin Neuropsychol. 2017;31(1):233–250. [DOI] [PubMed] [Google Scholar]
- 19. Canadian Longitudinal Study on Aging . COVID-19 Questionnaire (Baseline). (Version 1.2, April 15, 2020). Hamilton, ON, Canada: CLSA National Coordinating Centre; 2020. https://www.clsa-elcv.ca/doc/4263. Accessed October 1, 2021. [Google Scholar]
- 20. Canadian Longitudinal Study on Aging . COVID-19 Questionnaire (Weekly). (Version 1.4, May 8, 2020). Hamilton, ON, Canada: CLSA National Coordinating Centre; 2020. https://www.clsa-elcv.ca/doc/4265. Accessed October 1, 2021. [Google Scholar]
- 21. Canadian Longitudinal Study on Aging . COVID-19 Questionnaire (Biweekly—Telephone). (Version 1.4, May 8, 2020). Hamilton, ON, Canada: CLSA National Coordinating Centre; 2020. https://www.clsa-elcv.ca/doc/4267. Accessed October 1, 2021. [Google Scholar]
- 22. Canadian Longitudinal Study on Aging . COVID-19 Questionnaire (Monthly—Web and Telephone). (Version 1.5, June 5, 2020). Hamilton, ON, Canada: CLSA National Coordinating Centre; 2020. https://www.clsa-elcv.ca/doc/4269. Accessed October 1, 2021. [Google Scholar]
- 23. Canadian Longitudinal Study on Aging . COVID-19 Questionnaire (Exit). (Version 1.1, September 23, 2020). Hamilton, ON, Canada: CLSA National Coordinating Centre; 2020. https://www.clsa-elcv.ca/doc/4271. Accessed October 1, 2021. [Google Scholar]
- 24. Canadian Longitudinal Study on Aging . Data collection. https://www.clsa-elcv.ca/researchers/data-collection. Accessed October 1, 2021.
- 25. Dubé E, Bettinger JA, Fisher WA, et al. Vaccine acceptance, hesitancy and refusal in Canada: challenges and potential approaches. Can Commun Dis Rep. 2016;42(12):246–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Malosh R, Ohmit SE, Petrie JG, et al. Factors associated with influenza vaccine receipt in community dwelling adults and their children. Vaccine. 2014;32(16):1841–1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Logan J, Nederhoff D, Koch B, et al. ‘What have you HEARD about the HERD?’ Does education about local influenza vaccination coverage and herd immunity affect willingness to vaccinate? Vaccine. 2018;36(28):4118–4125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Frank K, Arim R. Canadians’ Willingness to Get a COVID-19 Vaccine: Group Differences and Reasons for Vaccine Hesitancy. (Catalogue no. 45-28-0001). Ottawa, ON, Canada: Statistics Canada; 2020. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00073-eng.htm. Accessed October 1, 2021. [Google Scholar]
- 29. Malani PN, Solway E, Kullgren JT. Older adults’ perspectives on a COVID-19 vaccine. JAMA Health Forum. 2020;1(12):e201539. [DOI] [PubMed] [Google Scholar]
- 30. Kelly BJ, Southwell BG, McCormack LA, et al. Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infect Dis. 2021;21(1):338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nikolovski J, Koldijk M, Weverling GJ, et al. Factors indicating intention to vaccinate with a COVID-19 vaccine among older U.S. adults. PloS One. 2021;16(5):e0251963. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.