Abstract
Objective
Children may be greatly affected by events that increase stress in individuals in general and are reported as the vulnerable groups during the coronavirus disease-19 (COVID-19) pandemic. But most of the studies in the literature investigating the mental effects of the pandemic on children were conducted with healthy children and limited study has evaluated the effect on children diagnosed with COVID-19. The aim of this study is to determine the anxiety level in paediatric patients diagnosed with COVID-19 and the affecting factors.
Methods
This descriptive study was conducted with 292 children aged 8–18 years who were diagnosed with COVID-19. Data were collected using the Descriptive Characteristics Questionnaire and the Screen for Child Anxiety Related Emotional Disorders (SCARED). Interviews were held by phone.
Results
Males were 51.4% of participants, the mean age was 16.04 ± 1.93. 84.1% of them had a chronic disease; the transmission source was family/relatives/friends for 41.1%. By social isolation, 49.3% were affected and 33.2% were affected by disease symptoms the most in this process. The most common symptoms were headache (61.6%), and asthenia (59.9%). Mean anxiety scale score was 25.5 ± 14.37. The effect of gender, number of symptoms and transmission source on anxiety score was significant (p < 0.05).
Conclusion
Paediatric patients diagnosed with COVID-19 were found to have high anxiety levels. It is recommended to re-evaluate the duration of children’s social participation and support the management of COVID-19 symptoms that affect their anxiety level.
Keywords: adolescent, anxiety, child, COVID-19, pandemic
INTRODUCTION
Coronavirus disease-19 (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. COVID-19 was first seen with unidentified pneumonia symptoms in Wuhan, China towards the end of 2019 and then became a pandemic by spreading all over the world. According to the World Health Organization (WHO) report dated 17 November 2021, there are 254 256 432 COVID-19 cases in the world and 5 112 461 people have died due to this infection [1]. COVID-19 showed a rapid spread in the entire world at the beginning of 2020 and in Turkey, the first case was reported on 13 March 2020. The current total number of cases is 8 388 542 according to data dated 18 November 2021 and 73 342 deaths were reported [2]. The first child COVID-19 case was confirmed on 20 January 2020 [3] and it was reported on 31 January 2020 that 20 children were infected in China [4]. According to the current Turkish report dated 8 November 2020, 0.76% of the cases are aged under five, 3.6% are between 5 and 14 aged, and 15.3% are aged between 15 and 24 [2].
Some literature data showed that COVID-19 is seen in children in all age groups starting from the neonatal period and in both gender. It is also reported that the prevalence in children is 2.4% and 90% of children are asymptomatic [5, 6]. In a systematic review in which 45 studies were examined, it was stated that the prevalence of infection in children ranged between 1% and 5% [7]. The course of COVID-19 is mild or moderate in children and the symptoms differ from adults. However, there is no enough scientific evidence regarding the use of drugs used in the treatment of COVID-19 in children. It was reported that some drugs used in the treatment of COVID-19 are not used in certain age groups among children [8]. The most common COVID-19 symptoms in children are fever and cough [9]. Although child cases have been reported all over the world, there are some unexplained situations regarding the effect of the infection on children [10].
Children and adolescents are highly vulnerable to the effect of constant stress sources since they are in sensitive developmental periods. Therefore, it is important to monitor and evaluate them mentally during and after the pandemic. A study examining the impacts of the pandemic on the mental health of children and adolescents reported that the pandemic has multidimensional impacts, pandemic stressors may trigger neuroinflammation and behavioural disorders and these stressors may lead to neuropsychiatric outcomes in adulthood. Also the study indicated that social isolation related to the pandemic may lead to neuroimmunoendocrine changes and measures are to be taken against mental health [11, 12]. After the COVID-19 pandemic, various psychological health problems such as anxiety and depression have emerged in societies and emotional disorders have increased [13–18].
Studies have been conducted related to the impacts of COVID-19 since it was declared a pandemic. But in the literature, most of the studies in the literature investigating the mental effects of the pandemic on children were conducted with healthy children and limited study has evaluated the effect on paediatric patients with COVID-19. For all this reasons, this study was designed to establish anxiety levels in paediatric patients aged 8–18 who were diagnosed with COVID-19 and the affecting factors, to determine the symptoms of the disease and to appoint change of anxiety levels according to some socio-demographic variables in children with COVID-19.
MATERIAL AND METHODS
Design and population of the study
This descriptive and cross-sectional study was carried out between October 2020 and February 2021 in two big hospitals, which are located in the town where COVID-19 patients receive treatment in the province of Sanliurfa located in southeastern Turkey. Although the number of healthcare personnel working in the COVID-19 clinics of hospitals varied according to the course of the epidemic, at the time of the study, 10 nurses and 3 doctors were working in the service with a capacity of 16 beds. Since the number of paediatric patients in the study was lower than that of adult patients, no sample selection was made and all patients who were reached were included in the study. The sample of the study consisted of 292 paediatric patients aged 8–18 who were diagnosed with COVID-19.
Data collection tools
The data were collected using the Descriptive Characteristics Questionnaire and the Screen for Child Anxiety Related Emotional Disorders (SCARED). The Descriptive Characteristics Questionnaire consists of 27 questions and 2 sections. The first section includes questions for children and their parents (age, gender, parents’ educational status, number of siblings, etc.) and the second section consists of questions about the COVID-19 process (the duration of the child’s hospitalization, the belief that the COVID-19 process will end, the history of the child’s admission to intensive care, the history of a relative’s admission to intensive care or death due to COVID-19, level of knowledge about COVID-19, etc.).
In the study, the data were collected by phone calls since the children with COVID-19 were obliged to be isolated at the hospital/home. Phone calls were made within the week following the end of the quarantine period when the child and his family were available. Considering that the duration of discharge may affect the anxiety score, all children were interviewed at the same time period after discharge. Information on children isolated at home was obtained through retrospective examination of hospital records. Before starting to collect the data, children and their parents were informed about the study and their informed consent was obtained. All interviews were conducted by a paediatric nursing specialist who was among the authors of the study. Before the interview, the opinion of the child mental health specialist, who is among the authors of the study, was taken.
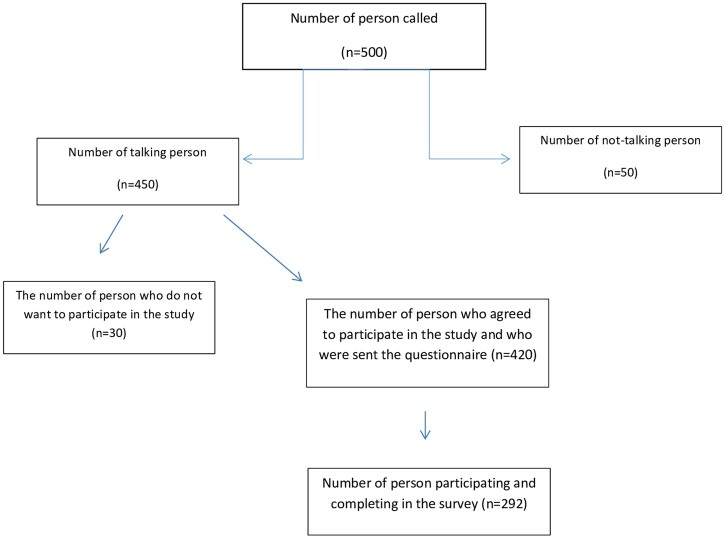
The questions in the data collection forms were prepared online and the link was sent to children’s and/or their parents’ phones. After receiving parents’ permission about their children’s involvement in the study, a link including the questionnaires was sent and the children were asked to answer the questions (Fig. 1).
Fig. 1.
Data collection process.
Screen for child anxiety related emotional disorders (SCARED)
The SCARED was developed by Birmaher et al. [19] to screen childhood anxiety disorders and its Turkish validity and reliability study was conducted by Karaceylan Cakmakci [20]. The SCARED comprises 41 items that are rated on a 3-point scale with responses: not true or hardly ever true (0 point), somewhat true or sometimes true (1 point) and very true or often true (2 point). The total anxiety score is the simple sum of all items and it is between 0 and 82 point. Birmaher et al. [19] reported the Cronbach alpha reliability coefficient as 0.74–0.93 for the general scale and subscales. In this study, the Cronbach alpha for the total scale score was 0.92.
Statistical analysis
The independent variables of the study were children’s age, gender, number of symptoms, allergy status, and presence of a disease other than COVID-19, transmission source, and loss of relatives due to COVID-19. The dependent variable of the study was the mean total anxiety scale score. The data were analysed with SPSS v.23. Descriptive statistics were presented as number, percentage, mean and standard deviation. Homogeneity of the variables was examined using the Levene’s test. The effects of some variables on participants’ anxiety total scores were tested using the linear regression (enter step). The significance level was taken as p < 0.05.
Ethical aspects
Prior to the study, written permission was obtained from the Ministry of Health (2020-07-14T15_46_45), Harran University Ethics Committee (ethics committee approval dated 28 September 2020 and numbered 20.17.07), and the Provincial Directorate of Health. Before the study, the children and their parents were informed and their verbal and written consent was taken and patient data is anonymized.
RESULTS
The mean age of the children was 16.04 ± 1.93 (min: 9, max: 17). Of the children, 51.4% were male; 48.6% were female; 78.8% were in the 15–18 age range; 21.2% were aged 14 years and below. When the educational status of the mothers was examined, it was determined that 37% of the mothers and 27.7% of the fathers were primary school graduates. Of them, 52.7% had poor/inadequate income. Of the participants, 88.4% had received all of their vaccinations according to the age group; 2.1% had not received any vaccination; 82.9% stated that they had no allergy. The most common symptom was headache (61.6%), followed by asthenia (59.9%) and cough (50%). Table 1 shows the distribution of the answers given by children to the questions regarding the COVID-19 diagnosis.
Table 1.
Distribution of participants’ some descriptive characteristics regarding COVID-19
| Variables (n = 292) | n | % |
|---|---|---|
| Presence of a disease other than COVID-19 | ||
| Yes | 44 | 15.1 |
| No | 248 | 84.9 |
| Medication used regularly | ||
| Yes | 16 | 5.5 |
| No | 276 | 94.5 |
| COVID-19 transmission source | ||
| One of the family members | 67 | 22.9 |
| Close relatives | 35 | 12.0 |
| Friends | 18 | 6.2 |
| Unknown | 115 | 39.4 |
| Other (public transport, shopping mall, public places) | 57 | 19.5 |
| CT result | ||
| Negative | 16 | 5.5 |
| Positive | 35 | 12.0 |
| Not performed | 240 | 82.2 |
| The most common symptom | ||
| Headache | 180 | 61.6 |
| Asthenia | 175 | 59.9 |
| Cough | 146 | 50 |
| Loss of taste | 144 | 49.3 |
| Loss of smell | 140 | 47.9 |
| Joint pain | 131 | 44.9 |
| Hospitalization status | ||
| Yes | 19 | 6.5 |
| No | 272 | 93.2 |
| Following the hand washing rule during the COVID-19 process | ||
| Always | 201 | 68.8 |
| Often | 75 | 25.7 |
| Sometimes | 11 | 3.8 |
| Rarely | 5 | 1.7 |
| Following the mask wearing rule during the COVID-19 process | ||
| Always | 204 | 69.9 |
| Often | 62 | 21.2 |
| Sometimes | 19 | 6.5 |
| Rarely | 7 | 2.4 |
| Following the social distancing rule during the COVID-19 process | ||
| Always | 186 | 63.7 |
| Often | 70 | 24.0 |
| Sometimes | 27 | 9.2 |
| Rarely | 9 | 3.1 |
| Hospitalization in intensive care due to COVID-19 | ||
| No | 292 | 100.0 |
| Having a relative hospitalized in intensive care due to COVID-19 | ||
| Yes | 73 | 25.0 |
| No | 219 | 75.0 |
| Loss of a relative/contact due to COVID-19 | ||
| Yes | 40 | 13.7 |
| No | 248 | 84.9 |
| Degree of deceased person (n = 40) | ||
| First degree (mother, father, sister) | 1 | 2.5 |
| Second degree (grandmother, grandfather, aunt, uncle) | 15 | 37.5 |
| Third degree (first cousins, great-grandparents, aunt, uncle, etc.) | 3 | 7.5 |
| Fourth degree or no kinship | 21 | 52.5 |
| Believing that the COVID-19 pandemic will end | ||
| Yes | 149 | 51.0 |
| No | 143 | 49.0 |
| Having sufficient knowledge about COVID-19 | ||
| Yes | 205 | 70.2 |
| No | 26 | 8.9 |
| Indecisive | 61 | 20.9 |
| The most affecting situation during the COVID-19 diagnosis processa | ||
| Social isolation, staying home | 144 | 49.3 |
| Disease symptoms | 97 | 33.2 |
| Getting behind with school and education life | 53 | 18.2 |
| Fear of death or death of relatives | 32 | 11.0 |
| Fear of not being able to overcome the disease | 27 | 9.2 |
| Fear of infecting others | 26 | 8.9 |
| Increased economic troubles | 7 | 2.4 |
In this study, the children’s mean anxiety scale score was 25.5 ± 14.37 (min 0–max 69). The subscale mean scores of the scale were determined as 5.87 ± 4.84 for panic/somatic (0–25), 6.79 ± 4.7 (0–18) for general anxiety, 4.96 ± 3.08 (0–14) for separation anxiety, 6.15 ± 3.68 (0–14) for social phobia, and 1.8 ± 1.7 (0–8) for school phobia.
Table 2 examines the effect of gender, number of symptoms, age, allergy, presence of a comorbid disease, transmission source and loss of a relative due to COVID-19 variables on the anxiety scores of children diagnosed with COVID-19. The effect of gender (p < 0.001), number of symptoms (p = 0.001) and transmission source (p < 0.001) values on the anxiety score was significant. The mean anxiety score was 29.54 for girls and 21.71 for boys. The effect of age (two groups; 9–14 and 15–18), allergy (two groups; yes and no), presence of a comorbid disease (two groups; yes and no) and loss of a relative due to COVID-19 (two groups; yes and no) on the anxiety score was not statistically significant (p > 0.05).
Table 2.
Examination of the effects of some variables on participants’ anxiety levels
| Unstandardized coefficients |
Standardized coefficients | t | p value | ||
|---|---|---|---|---|---|
| Source | B | Standard error | |||
| Gender | −6.104 | 1.594 | −0.213 | −3.828 | <0.001* |
| Number of symptoms | 3.859 | 1.118 | 0.189 | 3.453 | 0.001* |
| Age | 1.400 | 1.950 | 0.040 | 0.718 | 0.473 |
| Allergy | 3.749 | 2.093 | 0.099 | 1.791 | 0.074 |
| Presence of a disease | 3.778 | 2.188 | 0.094 | 1.726 | 0.085 |
| Transmission source | −3.582 | 0.902 | −0.224 | −3.970 | <0.001* |
| Loss of a relative due to COVID-19 | 0.676 | 2.273 | 0.016 | 0.297 | 0.766 |
Linear regression model. *p<0.05 were represented in bold.
R 2 = 0.183 (Adjusted R Squared = 0.163).
The effect of the number of symptoms experienced by children due to the diagnosis of COVID-19 on the anxiety score was important. The score was 22.42 in children with 0–5 symptoms, 27.63 in children with 6–10 symptoms, and 30.89 in children with 11 symptoms or above. According to the number of symptoms, the group with the highest anxiety score consisted of children with 11 symptoms and above and the group with the lowest score consisted of children with 0–5 symptoms (Table 3).
Table 3.
Descriptive statistics for anxiety scores according to gender and number of symptoms
| Girl | Boy | Total | |
|---|---|---|---|
| 0–5 symptoms | 26.44 ± 1.77 | 19.89 ± 1.44 | 22.42 ± 1.15 |
| 6–10 symptoms | 31.47 ± 1.65 | 21.21 ± 1.84 | 27.63 ± 1.32 |
| 11 symptoms and above | 31.65 ± 4.16 | 30.29 ± 3.26 | 30.89 ± 2.55 |
| Total | 29.54 ± 1.18 | 21.71 ± 1.11 | 25.52 ± 0.84 |
A score difference of 3.182 was found between the mean scores of those with 0–5 symptoms and those with 6–10 symptoms. A score difference of 7.806 was found between the mean scores of those with 0–5 symptoms and those with 11 symptoms. There was a difference of 4.624 between the mean scores of those with 6–10 symptoms and those with 11 symptoms (Table 3).
The mean score was 31.42 in the group who reported transmission from family and friends, 29.63 in the group who thought they were infected in public places and 22.99 in the group who did not know the transmission source. The highest anxiety score was obtained in the group who reported transmission from family and friends (Table 4).
Table 4.
Descriptive statistics of some variables of the participants
| Variables | Mean ± S.D. | |
|---|---|---|
| Age | 9–14 years | 26.05 ± 1.81 |
| 15–18 years | 25.38 ± 0.95 | |
| Allergy | Yes | 29.44 ± 2.15 |
| No | 24.71 ± 0.91 | |
| Presence of a disease | Yes | 29.84 ± 2.06 |
| No | 24.75 ± 0.91 | |
| Transmission source | Family, friends | 29.17 ± 1.26 |
| Public places | 27.26 ± 1.93 | |
| Unknown | 20.85 ± 1.28 | |
| Loss of a relative due to COVID-19 | Yes | 24.78 ± 2.29 |
| No | 25.65 ± 0.91 |
DISCUSSION
Adolescence is the transition period from childhood to adulthood. During this period, significant changes are seen in biological, psychological, social and other areas [21, 22]. In the COVID-19 process, the focus has been more on older people, and the psychosocial and emotional states of adolescents have been given less attention. However, it is stated that in this process, the physical and mental health, peer relationships, and future plans of the adolescents are affected in an unpredictable way [23]. Paediatric patients are exposed to much negative information from the media or from the conversations of adults nearby during the coronavirus pandemic. Furthermore, they experience changes in their daily routines and socialization processes with their peers are interrupted due to quarantines. Besides many effects, it is stated that the COVID-19 pandemic can cause many psychological effects in paediatric patients such as anxiety, fear and concerns [24, 25]. For instance, in the COVID-19 epidemic, measures such as physical distance, quarantine and staying away from the school environment negatively affect the development of adolescents. Many children are anxious due to isolation and fear and worry about losing their relatives or their own health due to the virus. In addition, there is an increase in anxiety about adolescents’ failure and failure to plan for the future [21].
In this study, 78.8% of the children are between the ages of 15–18. In the study, the mean anxiety scale score of the participants was 25.5 ± 14.76; 50% of them scored 25, the cut-off score of the scale, or above and their anxiety levels were high. It is thought that the high anxiety scores in the study are due to the fact that the majority of the sample consists of adolescents between the ages of 15–18 and this age group is more inclined experiencing these anxiety than others. In a study conducted with high school students in China during the outbreak, the prevalence of anxiety symptoms was 37.4% [17]. In another study conducted with 7143 university students, the prevalence of anxiety was 24.9% [26]. The anxiety rate was reported to be 33.06% in a group aged between 8 and 17 in Turkey [27]. The anxiety rate was reported higher in a group aged between 17 and 19 in Italy [23]. The rate of anxiety in children and adolescents during the pandemic is higher compared to the pre-pandemic period [17, 28]. The results of our study, which is the only study conducted on the anxiety level of paediatric patients diagnosed with COVID-19, show that the rate of anxiety during diagnosis is higher.
When anxiety scores were evaluated according to gender, similar to our study, girls were reported to have higher anxiety scores [17, 23, 29]. In a study, on the other hand, no difference was found between gender in terms of anxiety scores [26]. In our study, there was no significant difference when the effect of the age variable on the anxiety score was examined. In the literature, when children and adolescents were compared, some data showed that the anxiety scores increased as age increased [17, 29]. In our study, no significant change was observed in the anxiety levels of the individuals in the presence of another comorbid disease. However, some studies showed that the anxiety level increases in the presence of a chronic disease during the COVID-19 process [30, 31].
In the study, the most common symptoms were determined as headache, asthenia and cough (61.6%, 59.9% and 50%), respectively. In the literature, there are different results regarding the symptoms but fever and cough generally appear as the predominant clinical characteristics. However, the data on the prevalence of cough and other upper respiratory tract symptoms support our study [32–34].
As in many studies, the most common transmission source was one of the family members who shared the same house with the child. Many studies reported that the most important transmission source was, similarly, one of the family members, especially the parents [32, 35]. These results showed that children were less effective in transmission and were less likely to be infected by someone outside the home. The fact that the studies were conducted after the schools were closed may have affected the results. Further studies on the subject and interventions should be conducted in this process to prevent the negative effects of social isolation and being away from school and friends on children and adolescents [25].
The rate of those who were asymptomatic was 10.1% and similar results were reached when the literature was examined. In the literature, the rate of those who were asymptomatic ranges between 4% and 23% [32, 36]. When the effect of the number of symptoms on the total scale score was examined, it was found that the increase in the number of symptoms affected the anxiety scale score and that the anxiety score increased as the number of symptoms increased (Tables 2 and 3; p < 0.05). Although the rate of children and adolescents who were asymptomatic was high, the participants stated that the disease symptoms (33.1%) were the most affecting factor during the process after social isolation, being away from friends and relatives when they were asked ‘What affected you the most in this process?’ These results revealed that the symptomatic group was psychologically most affected by COVID 19 symptoms and that both physicians and nurses should focus more on symptom management in this group.
Since the children and young individuals are in isolation during the COVID-19 process, they suddenly lost many activities that form their daily routines such as school, non-class activities, social interactions, and physical activity, which allow them to be together with their peers and social circles. These can be the important factors that increase their anxiety considering that anxiety disorders occur in the absence of interpersonal communication [37]. Anxiety symptoms are the most common clinical diagnoses in children and adolescents and are considered a risk factor for other psychiatric disorders in adulthood. Facing disruptions in the increasingly complex social environment during the pandemic and deteriorations in various living areas can worsen anxiety and increase social costs for families [29]. For this reason, more attention should be paid to the mental health of children and adolescents and necessary measures should be taken in this process.
This study has some limitations, also. The study was actualized only with COVID-19 paediatric patients. In the study to be done in future, to better evaluate effects of COVID 19 on anxiety levels in children, it will be better to add a control group, trying to match with the patient group as much as possible. On the other hand, in the literature, it is seen that there is not enough data about anxiety levels and reasons of children with COVID-19 and this study presents important information on this subject. In this way, it is thought that the results of the study will guide health services provided for children diagnosed with COVID-19.
In this study, it was determined that paediatric patients diagnosed with COVID-19 had high anxiety levels. Although the prevalence of COVID-19 is lower in children than in adults, symptoms caused by COVID-19, compulsory isolation, etc. affect the mental state of children. Therefore, it is recommended to re-evaluate the duration of social involvement for children and make appropriate interventions on the management of COVID-19 symptoms, which is an issue that affects the anxiety level and is neglected by health professionals and parents.
REFERENCES
- 1. WHO. Coronavirus Disease (COVID-19). https://covid19.who.int (18 November 2021, date last accessed).
- 2. COVID-19 Türkiye Web Portalı. Türkiye’de Durum. 2021. https://covid19.tubitak.gov.tr/turkiyede-durum (18 November 2021, date last accessed).
- 3. Chan J, Yuan S, Kok K-H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020;395:514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen Z-M, Fu J-F, Shu Q, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr 2020;16:240–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. She J, Liu L, Liu W.. COVID-19 epidemic: disease characteristics in children. J Med Virol 2020;92:747–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics 2020;145:20200702. [DOI] [PubMed] [Google Scholar]
- 7. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr 2020;109:1088–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bialek S, Gierke R, Hughes M, et al. ; CDC COVID-19 Response Team. Coronavirus disease 2019 in children-United States, February 12–April 2, 2020. MMWR Morb Mortal Wkly Rep 2020;69:422–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. CDC. COVID-19 in Children and Teens. 2021. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/children/symptoms.html (3 February 2021, date last accessed).
- 10. Tezer H, Bedir DT.. Novel coronavirus disease (COVID-19) in children. Turk J Med Sci 2020;50:592–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shigemura J, Ursano RJ, Morganstein JC, et al. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci 2020;74:281–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. de Figueiredo CS, Sandre PC, Portugal LCL, et al. COVID-19 pandemic impact on children and adolescents' mental health: biological, environmental, and social factors. Prog Neuropsychopharmacol Biol Psychiatry 2021;106:110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Van Der Velden PG, Contino C, Das M, et al. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. J Affect Disord 2020;277:540–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li Y, Duan W, Chen Z.. Latent profiles of the comorbidity of the symptoms for posttraumatic stress disorder and generalized anxiety disorder among children and adolescents who are susceptible to COVID-19. Child Youth Serv Rev 2020;116:105235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vindegaard N, Benros ME.. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 2020;89:531–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Panda PK, Gupta J, Chowdhury SR, et al. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J Trop Pediatr 2021;67:fmaa122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhou S-J, Zhang L-G, Wang L-L, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry 2020;29:749–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang Y, Zhao N.. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020;288:112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Birmaher B, Khetarpal S, Brent D, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 1997;36:545–53. [DOI] [PubMed] [Google Scholar]
- 20. Karaceylan Çakmakçı F. Çocuklarda anksiyete bozukluklarını tarama ölçeği geçerlik ve güvenirlik çalışması. Spesiality thesis [dissertation]. Kocaeli University, Kocaeli, 2004.
- 21. WHO. Coronavirus disease (COVID-19): adolescents and youth. 2020. https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-adolescents-and-youth (31 May 2020, date last accessed).
- 22. Fox SE, Levitt P, Nelson IIC.. How the timing and quality of early experiences influence the development of brain architecture. Child Dev 2010;81:28–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Smirni P, Lavanco G, Smirni D.. Anxiety in older adolescents at the time of COVID-19. JCM 2020;9:3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Danese A, Smith P, Chitsabesan P, et al. Child and adolescent mental health amidst emergencies and disasters. Br J Psychiatry 2020;216:159–62. [DOI] [PubMed] [Google Scholar]
- 25. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395:912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020;287:112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Şahin B, Hoşoğlu E, Önal B.. Anxiety symptoms in healthcare workers and their children during the COVID-19 pandemic in Turkey. Nam Kem Med J 2020;8:321–30. [Google Scholar]
- 28. Bitsko RH, Holbrook JR, Ghandour RM, et al. Epidemiology and impact of health care provider–diagnosed anxiety and depression among US children. J Dev Behav Pediatr 2018;39:395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord 2020;275:112–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Abawi O, Welling MS, van den Eynde E, et al. COVID-19 related anxiety in children and adolescents with severe obesity: a mixed-methods study. Clin Obes 2020;10:e12412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Senkalfa BP, Sismanlar Eyuboglu T, Aslan AT, et al. Effect of the COVID-19 pandemic on anxiety among children with cystic fibrosis and their mothers. Pediatr Pulmonol 2020;55:2128–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Götzinger F, Santiago-García B, Noguera-Julián A, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Heal 2020;4:653–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Parri N, Lenge M, Buonsenso D; Coronavirus Infection in Pediatric Emergency Departments (CONFIDENCE) Research Group. Children with COVID-19 in pediatric emergency departments in Italy. N Engl J Med 2020;383:187–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Macias-Parra M, Fortes-Gutierrez S, Aguilar-Gomez N, et al. Clinical and epidemiological characteristics of paediatric patients diagnosed with COVID-19 in a tertiary hospital in Mexico City. J Trop Pediatr 2021;67:fmab025. [DOI] [PubMed] [Google Scholar]
- 35. Ding Y, Yan H, Guo W.. Clinical characteristics of children with COVID-19: a meta-analysis. Front Pediatr 2020;8:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rabinowicz S, Leshem E, Pessach IM.. COVID-19 in the pediatric population-review and current evidence. Curr Infect Dis Rep 2020;22:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry Investig 2020;17:175–6. [DOI] [PMC free article] [PubMed] [Google Scholar]