ABSTRACT
Scrub typhus, an acute febrile infectious disease prevalent in the “Tsutsugamushi Triangle”, is a mite-born rickettsial zoonosis, caused by Orientia tsutsugamushi. Although the clinical presentation is protean, it rarely causes abducens nerve palsy. We report a 14-year-old previously healthy Indian girl who presented with a recent onset right abducens nerve palsy and headache, but without fever and without the classic dermatological manifestation (“eschar”) of the disease. After exclusion of common infectious, autoimmune, and neoplastic causes, she was finally diagnosed with scrub typhus associated with an abducens nerve palsy, which responded to doxycycline therapy.
KEYWORDS: Abducens nerve palsy, Orientia tsutsugamushi, scrub typhus
Introduction
Amidst the ocular motor nerves, the sixth cranial nerve is deemed to be the most vulnerable to damage, because of its long intra-cranial and extra-axial course, extending from the ponto-medullary sulcus to the lateral rectus muscle in the orbit.1 The tortuous course, multiple points of fixation, and attachment to base of skull, keep it at risk of compression and damage.1
Scrub typhus is an acute febrile infectious disease prevalent in the “Tsutsugamushi Triangle”, which extends to the north to Siberia and the Kamchatka Peninsula, to the south to Australia, to the east to Japan and to the west to Afghanistan and India. It is a mite-born rickettsial zoonosis, caused by Orientia tsutsugamushi.2 Among the plethora of neurological manifestations associated with this disease, meningitis, encephalitis, cranial nerve paresis, transverse myelitis and polyneuropathy are the most documented.2 By contrast, abducens nerve palsy has rarely been reported.3–6
Scrub typhus is considered a rapidly emerging zoonotic disease.2 As its presentation is protean, it may be difficult for primary care physicians to suspect it in those patients presenting with apparently benign febrile illness, leading therefore to a delayed treatment. Primary care physicians should consider this disease in upcoming years while dealing with cases of fever of unknown origin, acute undifferentiated fever and, even, in cases with afebrile focal neurological deficits, especially in “Tsutsugamushi Triangle”.2 Testing is also simple and the tests are widely available. This is particularly important, as this infectious disease is well amenable to treatment with doxycycline and azithromycin, two commonly used, safe and affordable antibiotics that ensure cure.2
We herein report a 14-year-old previously healthy Indian girl who presented with a recent onset right abducens nerve palsy and headache, but without fever and without the classic dermatological manifestation (“eschar”) of the disease. After exclusion of common infectious, autoimmune, and paraneoplastic causes, she was finally diagnosed with scrub typhus associated with abducens nerve palsy, which responded to doxycycline therapy.
Informed consent statement
The patient’s guardian provided written informed consent to the publication of this case report.
Case report
A 14-year-old previously healthy Indian girl presented to the medical outpatient department with a 7 day history of headache and diplopia when looking to the right. There was no history of fever, nausea, vomiting, gait unsteadiness, loss of consciousness, weakness, autonomic disturbances or abnormal sensation. The diplopia had no waxing/waning or diurnal variation in pattern. The neuro-ophthalmological examination revealed a visual acuity of 6/6 in both eyes. Visual field testing was normal, as was the colour perception. The anterior poles, intraocular pressure and fundi were normal, and the optic nerves did not show disc oedema. Her pupils reacted briskly to light, without a relative afferent pupillary defect. There was no ptosis or proptosis. She showed restriction in abduction of the right eye with a 15-degree eso-deviation on Hirschberg corneal reflex test and she was 12-dioptre base out on a prism cover test. Diplopia was found in right lateral gaze, and in dextroelevation gaze. There was a contralateral synergistic overaction of the right and left medial recti. On cover testing, after covering the fixating eye (left eye), there was fixation of the right eye from the deviated position, which suggested a “manifest squint”. A forced duction test suggested a paralytic squint of the right eye. On a Hess chart, there was marked underaction of the right lateral rectus and slight overaction of the right and left medial recti. The neurological examination was unremarkable with intact cognition, cranial nerves (except the right sixth cranial nerve palsy) and normal motor, sensory, autonomic and cerebellar functions. Signs of trauma and meningeal irritation were absent. The rest of the systemic examination was unremarkable. From the history and clinical examination, it was clearly a case of isolated unilateral abducens nerve palsy with headache and the differential diagnoses, which were considered, are summarised in the Supplementary Table.
Routine blood tests were normal, except for raised erythrocyte sedimentation rate (56 mm/hr) and mild elevations of transaminases without hyperbilirubinaemia. Anti-nuclear antibody (ANA) screening using HEp-2 cells, ANA profile, antiphospholipid antibodies, anti-neutrophil cytoplasmic antibodies (cANCA and pANCA) were negative. Anti-acetylcholine receptor and anti-muscle-specific tyrosine kinase antibodies as well as anti-thyroid peroxidase and anti-thyroglobulin antibodies were also negative. Electrophysiological testing, including repetitive nerve stimulation and single fibre electromyography, was normal. Brain magnetic resonance imaging (MRI) with gadolinium revealed mild thickening and enhancement along the lateral walls of both cavernous sinuses (left more than right), basal cistern and posterior inter-hemispheric fissure, suggestive of meningitis (Figure 1). Cerebrospinal fluid (CSF) analysis revealed a mononuclear pleocytosis (20 cells/µl, all lymphocytes), normal glucose (45 mg/dL), and elevated protein content (102 mg/dL). Other CSF studies, including cytology examination, and cultures for relevant bacteria were negative, except for the presence of IgM antibodies against Orientia tsutsugamushi in both serum and CSF. Subsequently, a polymerase chain reaction confirmed the presence of Orientia tsutsugamushi in the CSF.
Figure 1.
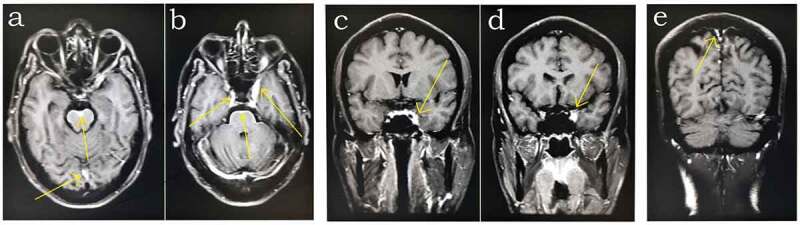
Gadolinium-enhanced T1-weighted magnetic resonance images. (a, b) Axial and (c, d, e) coronal imaging. Mild thickening and enhancement (arrows) can be seen along the lateral walls of the cavernous sinuses (left more than right) (b, c, d), basal cisterns (a, b) and posterior inter-hemispheric fissure (a, e), suggestive of meningitis.
She was put on oral doxycycline (100 mg twice per day for 14 days) and acetaminophen for the headaches. After 7 days, her headache had abated completely, but the right lateral rectus palsy took 6 weeks to recover fully. After 6 months’ follow-up, she did not have any recurrence of symptoms. Her neuro-ophthalmological and neurological examination remained normal.
Discussion
Age, history, clinical caveats and neuroimaging (preferably MRI) decide the differential diagnoses and work-up of patients with an abducens nerve palsy. In patients older than 50 years, it is generally due to ischaemic damage to the nerve, above all if there are other vascular risk factors (eg diabetes mellitis, arterial hypertension, dyslipidaemia, or tobacco use).7 In these cases, detailed work-up, including neuroimaging, should be considered when the palsy does not improve within 3 months.8 For younger patients, neuroimaging is mandatory.7 Our patient did not have any vascular risk factors neither had she a history of recurrent paresis. She was a teenager with neuroimaging suggestive of an infectious pathology, i.e. meningitis involving the walls of the cavernous sinus and basal cisterns.
Infection as the cause of abducens nerve palsy is well known.1 However, only four cases of scrub typhus associated with abducens nerve palsy have been reported (Table 1).3–6 Our case differs from the previous ones in some aspects. First, our patient neither reported nor was found to have a febrile episode associated with the illness. Although rare, afebrile cases of scrub typhus disease have been reported.9,10 Second, our patient did not have the pathognomonic “eschar” on her body, similar to the recently reported case by Ozair et al.6 Atypical manifestations of scrub typhus are on the rise in the tropics, which in turn increases the level of difficulty in diagnosing this multi-systemic infection.11 Last but not least, there was an apparent mismatch between the clinical findings (i.e., the right abducens nerve palsy) and the neuroimaging findings (contrast enhancement surrounding the cavernous sinus was more evident on the left side). The abducens nerve can be affected along its subarachnoid course, specifically as it ascends the clivus and turns 90 degrees anteriorly to enter Dorello’s canal.1 Indeed, lesions located elsewhere intracranially can secondarily affect the abducens nerve (an example of the poor localising value of a sixth nerve palsy).1 We think that the enhancement encircling the cavernous sinus was not the major contributing factor for the development of the nerve palsy in this case, rather that the nerve might have been subjected to infective (exudative) damage while traversing the subarachnoid space (headache, an extra-axial manifestation further supports this assumption).
Table 1.
Clinical profile of previously reported patients with abducens nerve palsy associated with scrub typhus disease
| Authors | Age (years)/Sex | Presenting symptoms | Eschar | Non-neurological symptoms | Neurological manifestations | CSF findings | Brain MRI | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Lee et al.3 | 24/F | Fever, chills, myalgia, rashes and oliguria | Yes | Fever, chills and myalgia | Diplopia, nystagmus and left esotropia | White cells: 32/mm3; protein: 51 mg/dl; glucose: 69 mg/dl; detection of Orientia tsutsugamushi DNA | Normal | Doxycycline | Complete recovery after four months |
| Bhardwaj et al.4 | 23/F | High grade fever and myalgia | Yes | Fever, myalgia and eschar on the lower back | Disorientation, diplopia with right esotropia, right lateral rectus weakness | White cells: 15/mm3 (mononuclear pleocytosis); protein: 40 mg/dl; glucose: 60 mg/dl; PCR for Orientia tsutsugamushi positive |
Normal | Doxycycline | Completely resolved |
| Ete et al.5 | 22/F | High grade continuous fever, altered sensorium, headache, and confused speech | Yes | Fever and jaundice | Headache, altered sensorium and bilateral sixth nerve palsy | White cells: 3/mm3(predominantly lymphocytes); protein: 117 mg/dl; glucose: 54 mg/dl | Not reported | Doxycycline and azithromycin | Recovery started from day 3, but complete recovery was not reported |
| Ozair et al.6 | 27/F | History of fever, followed by altered sensorium, jaundice, and diplopia | No | Fever and jaundice | Right sixth nerve palsy and Glasgow Coma Scale of 14 | White cells: 10/mm3 (80% lymphocytes); protein:137 mg/dl; glucose: 53 mg/dl | Patchy leptomeningeal enhancement | Doxycycline | Gradual recovery of lateral rectus palsy without any deficits |
CSF = cerebrospinal fluid; DNA = deoxyribonucleic acid; MRI = magnetic resonance imaging; PCR = polymerase chain reaction.
There are at least three pathogenetic mechanisms for the development of abducens nerve palsy in scrub typhus3;−6 First, by vasculitic/perivasculitic infarction of the vasa-nervorum of the sixth cranial nerve. Second, by intermittent temporary/persistent compression with exudates percolating through the subarachnoid space around the nerve resulting in focal demyelination/ischaemia. Finally, by stretching the points of fixation and areas of attachment to the base of the skull. Of note is that in none of the five cases (including the present one) of scrub typhus associated with abducens nerve palsy, was gadolinium enhancement of the nerve observed.
To conclude, this report arguably describes the first case of afebrile scrub typhus with abducens nerve palsy without an “eschar”, which improved with doxycycline without sequelae. Clinicians should include scrub typhus in the list of differential diagnoses of any sudden onset focal neurological deficit with clinical, laboratory or imaging evidence of infection in an endemic area. Delay in diagnosis may lead to multi-organ-dysfunction-syndrome and death in this otherwise curable disease.
Supplementary Material
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/01658107.2021.1909073.
Author contributions
All authors contributed significantly to the creation of this manuscript; each fulfilled criteria as established by the ICMJE.
Declaration of interest statement
The authors declare that they have no conflict of interest.
References
- 1.Azarmina M, Azarmina H.. The six syndromes of the sixth cranial nerve. J Ophthalmic Vis Res. 2013;8:160–171. [PMC free article] [PubMed] [Google Scholar]
- 2.Rana A, Mahajan SK, Sharma A, Sharma S, Verma BS, Sharma A.. Neurological manifestations of scrub typhus in adults. Trop Doct. 2017;47:22–25. doi: 10.1177/0049475516636543. [DOI] [PubMed] [Google Scholar]
- 3.Lee YH, Yun YJ, Jeong SH. Isolated abducens nerve palsy in a patient with scrub typhus. J Aapos. 2010;14:460–461. doi: 10.1016/j.jaapos.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Bhardwaj B, Panda P, Revannasiddaiah S, Bhardwaj H. Abducens nerve palsy in a patient with scrub typhus: a case report. Trop Biomed. 2013;30:706–709. [PubMed] [Google Scholar]
- 5.Ete T, Mishra J, Barman B, Mondal S, Sivam RK. Scrub typhus presenting with bilateral lateral rectus palsy in A female. J Clin Diagn Res. 2016;10:Od16–17. doi: 10.7860/JCDR/2016/18177.7617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozair A, Kumar V, Himanshu D, Bhat V. A rare etiology behind isolated lateral rectus palsy: scrub typhus. J Family Med Prim Care. 2020;9:2538–2540. doi: 10.4103/jfmpc.jfmpc_287_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richards BW, Jones FR Jr., Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992;113:489–496. doi: 10.1016/S0002-9394(14)74718-X. [DOI] [PubMed] [Google Scholar]
- 8.Nair AG, Ambika S, Noronha VO, Gandhi RA. The diagnostic yield of neuroimaging in sixth nerve palsy–Sankara Nethralaya Abducens Palsy Study (SNAPS): report 1. Indian J Ophthalmol. 2014;62:1008–1012. doi: 10.4103/0301-4738.146000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ichimura K, Uchida Y, Arai K, et al. Afebrile scrub typhus (Tsutsugamushi disease) with acute respiratory distress syndrome. Internal Medicine. 2002;41:667–670. doi: 10.2169/internalmedicine.41.667. [DOI] [PubMed] [Google Scholar]
- 10.Kodiatte AA, Kaur, S, Loomba, V. Scrub typhus presenting without fever. International Journal of Advances in Medicine. 2018;5:1308–1310. doi: 10.18203/2349-3933.ijam20183914. [DOI]
- 11.Guleria VS, Sharda C, Sood AK, Kumar V. Scrub typhus: atypical presentation in subhimalayan region. Med J Armed Forces India. 2018;74:180–182. doi: 10.1016/j.mjafi.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


