Abstract
Objective:
To examine and compare the maxillofacial characteristics affecting chin deviation three-dimensionally in facial asymmetry patients with mandibular retrusion and mandibular prognathism.
Materials and Methods:
Maxillofacial computed tomography (CT) scan data were obtained from 48 orthognathic surgery patients (24 cases of mandibular retrusion and 24 cases of mandibular prognathism) with facial asymmetry. Although chin deviation was assessed on the basis of the ANS-to-menton line on frontal cephalograms, its contributing factors were evaluated on three-dimensional CT images. Maxillary height, ramus length, frontal ramal inclination, lateral ramal inclination, mandibular body length, and body height were defined on each side, and right-left differences were calculated and analyzed.
Results:
In an assessment of chin deviation, subjects in this study showed predominantly left side deviation regardless of the group, and the degree of menton deviation did not reveal significant differences between groups. In a comparison of right-left differences in contributing factors, all values were noted to be greater in the retrusion group, except for body height, which showed no difference between chin-deviated and contralateral sides. In particular, ramus length presented a statistically significant difference between the two groups.
Conclusion:
Based on the same degree of chin deviation in mandibular prognathism and retrusion in this study, results of right-left differences in contributing factors indicate that chin deviations are expressed easily in mandibular prognathism, whereas they occur only with significant right-left differences in relevant maxillofacial structures in individuals with mandibular retrusion.
Keywords: Chin deviation, Mandibular retrusion, Mandibular prognathism, Maxillofacial CT scan
INTRODUCTION
Facial asymmetry is a variation in the configuration of one side of the face from the other when viewed in relation to a projected midsagittal line or structures, sizes, and shapes not matching each other. According to previous studies,1–4 facial asymmetry is more prominent in the lower part of the face than in the cranial area. Severt and Proffit5 reported that 34% of patients who visited the University of North Carolina for orthodontic treatment had facial asymmetry, and 74% of those had chin deviation. Because chin deviation can cause functional and esthetic problems, investigation of maxillofacial characteristics affecting chin deviation is needed when an orthodontic treatment plan is established.
Frontal cephalograms and submentovertex radiographs have been used as popular diagnostic methods of facial asymmetry. However, the reliability of these two-dimensional cephalometric measurements for facial asymmetry evaluation is limited because some landmarks are difficult to identify because of overlap, and because images differ according to patients' head positioning. Using computed tomography (CT) imaging, clinicians can observe craniofacial structures from a range of viewing angles by changing the rotational axis, and they can remove the outer surfaces to observe the inner structures more precisely.6 However, conventional medical CT is not used widely in dentistry because of high radiation exposure, high cost, and metal artifacts around metal fillings and implants.7 Cone beam CT (CBCT) is used widely today because it provides easy access to the dental office through the use of computers, and it reduces costs and radiation dose.
CT analysis can be an excellent tool for identifying the major causes of chin deviation because of its accurate and quantitative measurement. Hwang et al.8 developed a new three-dimensional (3D) imaging analysis by which factors contributing to facial asymmetry could be measured accurately. Kwon et al.9 reported that the main cause of mandibular asymmetry is the mandibular skeletal factors themselves instead of a cranial base deformity. Baek et al.10 examined factors affecting chin point deviation in skeletal Class III malocclusion patients and concluded that facial asymmetries in skeletal Class III patients occur as the result of greater growth and mesial inclination of the ramus and greater maxillary vertical excess at the opposite site.
Literature reviews on facial asymmetry reveal that most studies have dealt with individuals with mandibular prognathism. Mandibular retrusion has attracted little interest, particularly regarding factors affecting chin deviation. The purpose of the present study was to examine the maxillofacial characteristics affecting chin deviation three-dimensionally in facial asymmetry patients and compare them between mandibular retrusion and mandibular prognathism.
MATERIALS AND METHODS
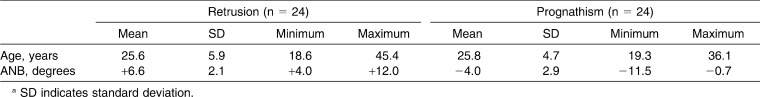
The sample consisted of 48 orthodontic patients (24 male, 24 female; mean age, 25.7 years; standard deviation [SD], 4.8 years) who had frontal cephalograms, lateral cephalograms, and multislice CT or CBCT images taken for a diagnosis of facial asymmetry at Chonnam National University Hospital, Gwangju, Korea, and Pusan National University Hospital, Pusan, Korea. Patients with chin deviation ranging from 2 to 10 degrees were selected.11 Chin deviation was assessed with the angle formed by crista galli (Cg)-anterior nasal spine (ANS) and ANS-menton lines on frontal cephalograms.12 Patients with a cleft lip and/or palate, plagiocephaly, hemifacial microsomia, and degenerative disease of the temporomandibular joint were excluded. Subjects were divided into two groups according to ANB degrees: prognathism group (12 men, 12 women; ANB<0 degrees; mean ANB, −4.0 ± 2.9 degrees; mean age, 25.8 ± 4.7 years) and retrusion group (12 men, 12 women; ANB>4 degrees; mean ANB, 6.6 ± 2.1 degrees; mean age, 25.6 ± 5.9 years). On the other hand, chin deviation was measured in linear distance, menton to Cg-ANS line, in addition to the angular measurement (Table 1).
Table 1.
Description of Sample Subjects Used in This Studya
Forty-one patients had their images scanned using a multislice CT scanner (Light Speed QX/I, GE Medical Systems, Milwaukee, Wis), whereas the remaining seven patients had their images scanned using a CBCT scanner (DCT Pro, Vatech, Su-Won, Korea). This study was approved by the Institutional Review Board for Medical Science at Chonnam National University Hospital, Gwangju, Korea.
Maxillofacial 3D images were created from CT scan DICOM data using V-Works 4.0 (CyberMed, Seoul, Korea). The Frankfort horizontal (FH) plane was constructed by connecting the right and left porion and the orbitale of one side; the midsagittal reference plane was constructed by connecting the opisthion (OP), the Cg, and the ANS. The mandibular plane was made by a plane connecting the right and left antegonion and menton. Right and left values of the six dimensions described here were measured according to Hwang et al.8 Measurements were as follows: (1) maxillary height, 6 to FH (Po-Or-Po), distance between the FH plane and the occlusal fossa of the maxillary first molar (mm); (2) ramus length, Cdsup-Goinf, distance between the highest point of the condyle and the lowest point of the gonion area (mm); (3) frontal ramal inclination, Cdlat-Golat to the midsagittal reference plane (Op-Cg-ANS), angle formed by the midsagittal reference plane and the external border of the ramus (degrees); (4) lateral ramal inclination, Cdpost-Gopost to FH (Po-Or-Po), angle formed by the FH plane and the posterior border of the ramus (degrees); (5) body length, Me-Gopost, distance between the menton and the most posterior point of the gonion area (mm); and (6) body height, 3 to mandibular plane (Ag-Me-Ag), distance from the mandibular canine cuspal tip perpendicular to the mandibular plane (mm). All measured values were recorded on a chart, and differences between right and left sides were calculated.
Statistical Analysis
Chi-square tests were used to test the significance of the difference in the chin deviation side between mandibular retrusion and prognathism groups, whereas Student's t-tests were used to test the significance of the difference in menton deviation between the two groups. To compare the values of each variable between chin-deviated and contralateral sides, paired t-tests were used in each group. Last, Student's t-tests were used to compare right and left differences between mandibular retrusion and prognathism groups. Statistical evaluations were performed at the 5% level of significance with Statistical Package for the Social Sciences (SPSS) software, version 16.0 (SPSS Inc, Chicago, Ill).
RESULTS
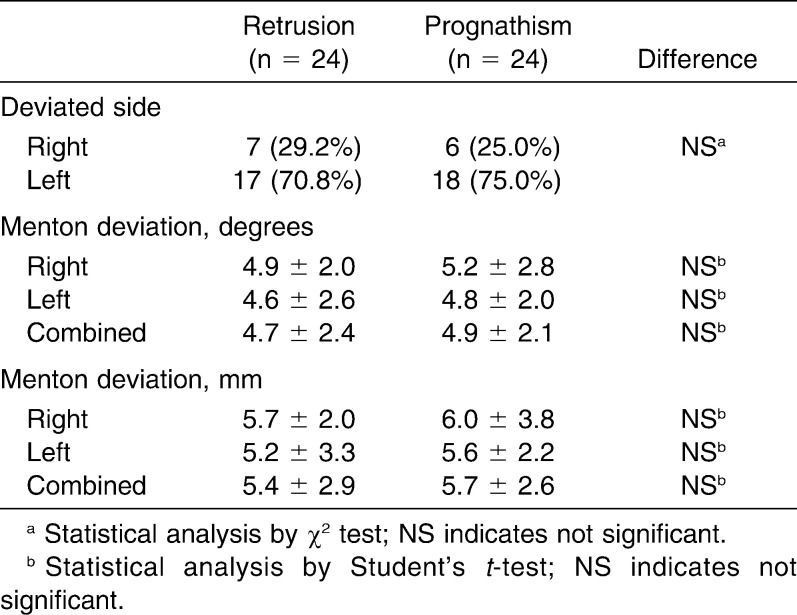
Frontal cephalometric analysis revealed left side chin deviations to be prominent regardless of the group: 70.8% for the mandibular retrusion group and 75.0% for the prognathism group. Comparison of menton deviation between the two groups also showed no significant differences in terms of angular and linear measurements (Table 2).
Table 2.
Data on Menton Deviation and Comparison of Mandibular Retrusion and Prognathism Groups
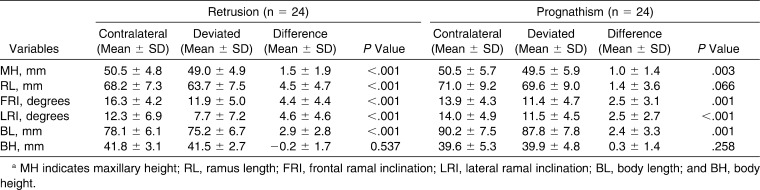
Evaluation of right-left differences in contributing factors showed that all measurements except for body height were higher in the contralateral side as expected, regardless of the group. In particular, all five measurements showed significant differences between chin-deviated and contralateral sides in the retrusion group. On the other hand, significant differences were noted in only four measurements in the prognathism group, and the levels of significance were low compared with the retrusion group. Comparison of the right-left difference between mandibular retrusion and prognathism groups revealed that all values were greater in the retrusion group, except for body height, which showed no difference between chin-deviated and contralateral sides. In particular, ramus length showed a statistically significant difference between the two groups (Table 3, Figure 1).
Table 3.
Data on Asymmetry Measurements and Comparison of Chin-Deviated and Contralateral Sides in Each Groupa
Figure 1.
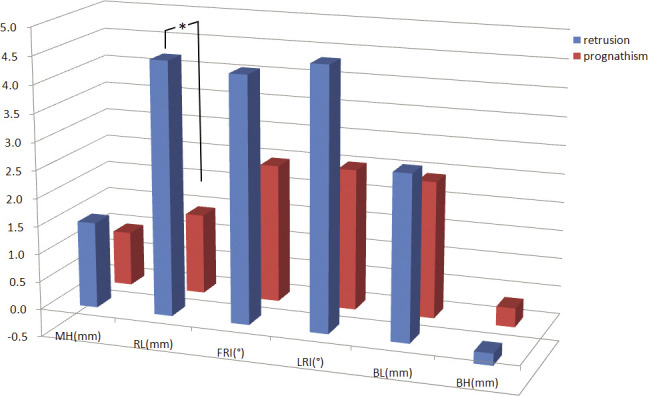
Comparison of the right-left difference between mandibular retrusion and prognathism groups. All values were greater in the retrusion group except for body height, which showed no difference between chin-deviated and contralateral sides. In particular, ramus length presented a statistically significant difference between the two groups. MH, maxillary height; RL, ramus length; FRI, frontal ramal inclination; LRI, lateral ramal inclination; BL, body length; BH, body height. *P < .05.
DISCUSSION
Frontal cephalograms or facial photographs might be useful for evaluating the presence and level of asymmetry, but 3D imaging is essential for examining causes and contributing factors of facial asymmetry. In this study, CT images were used to identify the contributing factors in chin deviation. As a scanner, multislice CT or CBCT was used. Multislice CT offers improved contrast and spatial resolution in all three dimensions compared with conventional CT.13–16 Recently developed CBCT provides a maxillofacial 3D image with low cost and less radiation.16 It is reported that CBCT also ensures high-dimensional accuracy in facial structure measurements.17–19 Mischkowski et al.20 reported that helical CT is by approximately 0.06 mm and 0.55 mL more accurate in average length and volume measurements than CBCT, but the difference is so imperceptible that there is no problem when CBCT is used clinically. Misch et al.21 and Pinsky et al.22 reported no significant difference in the value of actual measurements with a CBCT scan by measuring length and volume of artificially made skeletal defects in the mandible. In this study, it was more difficult to eliminate all tissue from each condylar head using the program's sculpt function when CBCT images were used compared with multislice CT images, but this did not affect measurements. Kim et al.23 evaluated the reproducibility of measurements representing asymmetry of the mandible, and intraexaminer reproducibility of the measurements was found to be high when correlation coefficients were higher than 0.9. Ludlow et al.17 concluded that the experience of the operator has a positive effect on measurement accuracy and reproducibility. In this study, landmark identification and the six measurements listed previously were carried out three times by an experienced examiner. The mean value of three measurements was used.
In assessment of chin deviation, subjects showed predominantly left side deviation regardless of the group. Patients' chins deviated to the left side in 70.8% of the retrusion group and 75% of the prognathism group. This is similar to the findings of Severt and Proffit,5 who stated that 85% of patients showing dentofacial deformity including jaw deviation had chin deviation to the left. Heraguchi et al.24 also documented left side deviation of the menton from the midline in 60% to 80% of patients with a skeletal Class III malocclusion who exhibited facial asymmetry.
A menton deviation is used as a quantitative evaluation standard for the degree of asymmetry in the diagnosis of facial asymmetry and is the primary determining factor in perceived facial asymmetry. The degree of menton deviation was similar in the mandibular retrusion and prognathism groups. Forty-eight patients with chin deviation ranging from 2 to 10 degrees were selected. Patients with severe menton deviation greater than 10 degrees were excluded to compare asymmetry patients without a pathologic condition. The results of no significant differences in menton deviation between retrusion and prognathism groups in this study indicate that mandibular retrusion patients have a similar amount of chin deviation compared with mandibular prognathism individuals, but appearance is not perceived well in mandibular retrusion patients.
In evaluation of right-left differences in terms of contributing factors, all measurements except for body height showed larger values on the contralateral side in both groups as expected. Hwang et al.8 suggested that the chin is deviated to the shorter side of the ramus length and/or mandibular body length, the smaller side of the maxillary height, and the smaller side of the ramal inclinations from a frontal or lateral view. All statements regarding geometry in the formation of asymmetry were identical to results obtained in the present study, indicating that chin deviation can develop from right and left differences in many relevant maxillofacial structures, including ramus inclinations and maxillary height, as well as ramus and mandibular body length. Baek et al.10 reported that the asymmetry group had shorter ramus height on the chin-deviated side and greater inclination of the ramus on the opposite side. Although skeletal Class III patients alone were used as subjects in their study. The present study showed that those characteristics are apparent regardless of mandibular retrusion or prognathism.
Comparison of right and left differences between mandibular retrusion and prognathism groups revealed all values to be higher in the retrusion group, except for body height, which showed no difference between chin-deviated and contralateral sides. In particular, ramus length showed a statistically significant difference between the two groups. The right and left difference in ramus length in the retrusion group was 4.5 mm, whereas it was only 1.4 mm in the prognathism group. Sezgin et al.25 reported that the Angle Class II division 1 groups had a more asymmetric condyle than the other malocclusion groups, including Class III, in their study, which examined the effects of different occlusion types on mandibular asymmetry in young individuals using panoramic radiography. Given that there were no significant differences in menton deviation between mandibular retrusion and prognathism groups, the results of right-left differences in contributing factors indicate that chin deviation is expressed easily in mandibular prognathism, whereas it occurs only with significant right-left differences in relevant maxillofacial structures in mandibular retrusion. These results suggest that regarding chin deviation, more attention should be paid when a treatment plan is established in mandibular prognathism patients.
Larger differences between chin-deviated and contralateral sides in the mandibular retrusion group indicate that chin deviation is affected evenly by contributing factors. Conversely, chin deviation is likely to be developed irregularly in mandibular prognathism individuals. In other words, a certain factor affects chin deviation predominantly, whereas other factors do not contribute to the asymmetry of an individual in mandibular prognathism. These findings suggest that more detailed study on the formation of asymmetry is needed on an individual basis in patients with mandibular prognathism.
On the other hand, the fact that frontal ramal inclination on the contralateral side was greater than on the chin-deviated side, particularly in the retrusion group, should be considered when surgical correction of mandibular retrusion patients with mandibular asymmetry is planned. Right and left differences in frontal ramal inclination might be perceived easily by patients other than lateral ramal inclination, which cannot be observed on the frontal view. Although most patients are satisfied with correcting the chin deviation through orthognathic surgery, some patients complain of asymmetric facial contours even after successful correction of the chin deviation. It should be noted that right-left differences in ramal inclination on the frontal view are not corrected by the regular mandibular surgical procedure. Additional procedures, such as augmentation or ostectomy, should be considered, particularly in the diagnosis and surgical treatment planning of mandibular retrusion patients who show distinct right-left differences in ramal inclination, in addition to ramal length.
CONCLUSION
Based on the same degree of chin deviation in mandibular prognathism and retrusion, chin deviation is expressed easily in mandibular prognathism, whereas it occurs only with significant right-left differences in relevant maxillofacial structures in individuals with mandibular retrusion.
REFERENCES
- 1.Vig P. S, Hewitt A. B. Asymmetry of the human facial skeleton. Angle Orthod. 1975;45:125–129. doi: 10.1043/0003-3219(1975)045<0125:AOTHFS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Shah S. M, Joshi M. R. An assessment of asymmetry in the Normal Craniofacial complex. Angle Orthod. 1978;48:141–148. doi: 10.1043/0003-3219(1978)048<0141:AAOAIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Grayson B. H, McCarthy J. G, Bookstein F. Analysis of craniofacial asymmetry by multiplane cephalometry. Am J Orthod. 1983;84:217–224. doi: 10.1016/0002-9416(83)90129-x. [DOI] [PubMed] [Google Scholar]
- 4.Peck S, Peck L, Kataja M. Skeletal asymmetry in esthetically pleasing faces. Angle Orthod. 1990;61:43–48. doi: 10.1043/0003-3219(1991)061<0043:SAIEPF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Severt T. R, Proffit W. R. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int J Adult Orthodon Orthognath Surg. 1997;12:171–176. [PubMed] [Google Scholar]
- 6.Kawamata A, Ariji Y, Langlais R. P. Three-dimensional computed tomography imaging in dentistry. Dent Clin North Am. 2000;44:395–410. [PubMed] [Google Scholar]
- 7.Bergersen E. O. Enlargement and distortion in cephalometric radiography: compensation tables for linear measurements. Angle Orthod. 1980;50:230–244. doi: 10.1043/0003-3219(1980)050<0230:EADICR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Hwang H. S, Hwang C. H, Lee K. H, Kang B. C. Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry. Am J Orthod Dentofacial Orthop. 2006;130:779–785. doi: 10.1016/j.ajodo.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 9.Kwon T. G, Park H. S, Ryoo H. M, Lee S. H. A comparison of craniofacial morphology in patients with and without facial asymmetry: a three-dimensional analysis with computed tomography. Int J Oral Maxillofac Surg. 2006;35:43–48. doi: 10.1016/j.ijom.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Baek S. H, Cho I. S, Chang Y. I, Kim M. J. Skeletodental factors affecting chin point deviation in female patients with Class III malocclusion and facial asymmetry: a three-dimensional analysis using computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:628–639. doi: 10.1016/j.tripleo.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Kusayama M, Motohashi N, Kuroda T. Relationship between transverse dental anomalies and skeletal asymmetry. Am J Orthod Dentofacial Orthop. 2003;123:329–337. doi: 10.1067/mod.2003.41. [DOI] [PubMed] [Google Scholar]
- 12.Grummons D. C, Kappeyne M. A. A frontal asymmetry analysis. J Clin Orthod. 1987;21:448–465. [PubMed] [Google Scholar]
- 13.Vannier M. W, Marsh J. L, Warren J. O. Three dimensional CT reconstruction images for craniofacial surgical planning and evaluation. Radiology. 1984;150:179–184. doi: 10.1148/radiology.150.1.6689758. [DOI] [PubMed] [Google Scholar]
- 14.Kalender W. A, Seisser W, Klotz E, Vock P. Spiral volumetric CT with single-breath-hold technique, continuous transport, and continuous scanner rotation. Radiology. 1990;176:181–183. doi: 10.1148/radiology.176.1.2353088. [DOI] [PubMed] [Google Scholar]
- 15.Kalender W. A, Polacin A, Süss C. A comparison of conventional and spiral CT: an experimental study on the detection of spherical lesions. J Comput Assist Tomogr. 1994;18:167–176. doi: 10.1097/00004728-199403000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Swennen G. R, Schutyser F. Three-dimensional cephalometry: spiral multi-slice vs cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2006;130:410–416. doi: 10.1016/j.ajodo.2005.11.035. [DOI] [PubMed] [Google Scholar]
- 17.Ludlow J. B, Laster W. S, See M, Bailey L. J, Hershey G. Accuracy of measurements of mandibular anatomy in cone-beam computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:534–542. doi: 10.1016/j.tripleo.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Periago D. R, Scarfe W. C, Moshiri M, Scheetz J. P, Silveira A. M, Farman A. G. Linear accuracy and reliability of cone beam CT derived 3-dimensional images constructed using an orthodontic volumetric rendering program. Angle Orthod. 2008;78:387–395. doi: 10.2319/122106-52.1. [DOI] [PubMed] [Google Scholar]
- 19.Honey O. B, Scarfe W. C, Hilgers M. J, Klueber K, Silveira A. M, Haskell B. S, Farman A. G. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop. 2007;132:429–438. doi: 10.1016/j.ajodo.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 20.Mischkowski R. A, Pulsfort R, Ritter L, Neugebauer J, Brochhagen H. G, Keeve E. Geometric accuracy of a newly developed cone-beam device for maxillofacial imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:551–559. doi: 10.1016/j.tripleo.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 21.Misch K. A, Yi E. S, Sarment D. P. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–1266. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 22.Pinsky H. M, Dyda S, Pinsky R. W, Misch K. A, Sarment D. P. Accuracy of three-dimensional measurements using cone-beam CT. Dentomaxillofac Radiol. 2006;35:410–416. doi: 10.1259/dmfr/20987648. [DOI] [PubMed] [Google Scholar]
- 23.Kim G. W, Kim J. H, Lee K. H, Hwang H. S. Reproducibility of asymmetry measurements of mandible in three-dimensional CT imaging. Korean J Orthod. 2008;38:314–327. [Google Scholar]
- 24.Haraguchi S, Iguchi Y, Takada K. Asymmetry of the face in orthodontic patients. Angle Orthod. 2008;78:421–426. doi: 10.2319/022107-85.1. [DOI] [PubMed] [Google Scholar]
- 25.Sezgin O. S, Celenk P, Arici S. Mandibular asymmetry in different occlusion patterns. Angle Orthod. 2007;77:803–807. doi: 10.2319/092506-392. [DOI] [PubMed] [Google Scholar]