Abstract
Objective:
To assess the mechanical stability of a newly revised orthodontic mini-implant design (N2) compared with a design introduced in Part 1 of the study (N1) and the most widely-used commercially-available design (CA). To evaluate the mean buccal bone thickness of maxillary and mandibular posterior teeth using cone-beam computed tomography (CBCT).
Materials and Methods:
From the CBCT scans of 20 patients, six tomographic cross-sections were generated for each tooth. Buccal bone thickness was measured from the most convex point on the bone to the root surface. CA (1.5 mm in diameter and 6 mm in length), N1, and N2 (shorter and narrower than N1) were inserted in simulated bone with cortical and trabecular bone layers. Mechanical stability was compared in vitro through torque and lateral displacement tests.
Results:
The bone thickness ranged from 2.26 to 3.88 mm. Maximum insertion torque was decreased significantly in N2 compared to N1. However, force levels for all displacement distances and torque ratio were the highest in N2, followed by N1 and CA (α = .05).
Conclusions:
Both torque and lateral displacement tests highlighted the enhanced stability of N2 compared with CA. Design revisions to N1 effectively mitigated N1's high insertion torque and thus potentially reduced microdamage to the surrounding bone. The N2 design is promising as evidenced by enhanced stability and high mechanical efficiency. Moreover, N2 is not limited to placement in interradicular spaces and has the capacity to be placed in the buccal bone superficial to the root surface with diminished risk of endangering nearby anatomic structures during placement and treatment.
Keywords: Mini-implants; TADs, Stability; Buccal bone thickness; Cortical bone; Micro-CT
INTRODUCTION
Orthodontic anchorage is defined as the resistance to unwanted tooth movement, and the control of anchorage is essential for successful orthodontic treatment outcomes. Mini-implants have grown in popularity as an important tool to facilitate maximum anchorage without the use of extra-oral appliances.1–4 As a result, patient compliance has become less crucial in treatment predictability. If placed properly, mini-implants can provide the patient with a more esthetic, convenient, and comfortable experience. Mini-implants have opened a new realm of orthodontics with treatment outcomes that were not previously possible with orthodontics alone.5
While the efficacy of mini-implants in orthodontics is no longer in question, prior studies have evaluated risk and stability factors with the goal of reducing the failure rates of orthodontic implants.6,7 Possible complications identified include root, nerve, blood vessel, and sinus damage during placement, implant fracture during removal, soft tissue inflammation, and infection.8 Different placement sites have been explored and interradicular sites are most commonly utilized.9 Ideal interradicular sites have been restricted to the buccal space mesial and distal to first molars10,11 because it is often challenging to find adequate interdental spacing.12 In addition, interradicularly placed mini-implants' proximity or contact with roots is possible during placement and tooth movements, and can contribute to implant loosening.7,13,14 Other non–tooth-bearing placement sites such as zygomatic buttress and retromolar pads often require additional surgical procedures2,15,16 and experience more frequent soft-tissue inflammation and clinical difficulty.17
In Part 1 of this study, a new mini-implant (N1) was introduced.18 N1 is significantly shorter than commercial designs to engage mostly in cortical bone as the quality and thickness of cortical bone is known to play a crucial role in its stability.19,20 Part 1 reported N1's improved stability compared with commercially-available designs and potential clinical strengths from short length to avoid biologic damages.18 However, it was concluded that N1's high insertion torque can introduce clinical difficulty and compromised stability from damage to surrounding bone,5,21 requiring further design improvements.
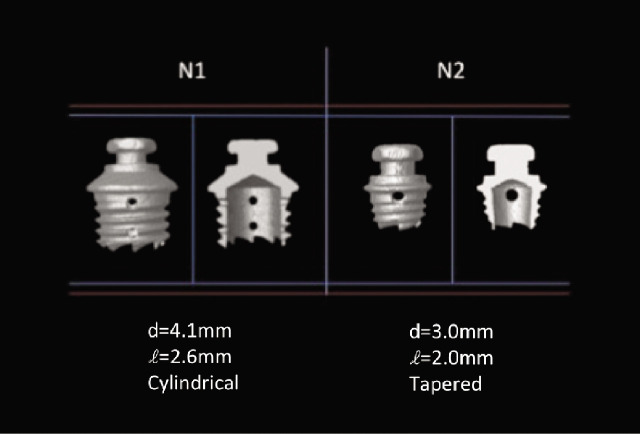
To maximize the possibility of utilizing mini-implants conveniently without the limitations of interradicular space and with decreased risk of root proximity, it would be beneficial to place the implant in the bone superficial to the root. A pilot study using cone-beam computed tomography (CBCT) was performed to evaluate the average buccal bone thickness of maxillary and mandibular posterior teeth where mini-implants are most frequently placed. This information was used to determine the appropriate length of the revised design (N2). Compared with N1, N2 has reduced length and diameter to decrease insertion torque, a tapered shape to enhance stability, and a tapered hollow interior to facilitate insertion with decreased friction (Figure 1).
Figure 1.
N1 and N2 dimension comparisons.
The aim of this study was to assess the stability of the improved design (N2) compared with N1 and the most widely used commercially-available design (CA) using torque and lateral displacement tests.
MATERIALS AND METHODS
Buccal Bone Measurement: Pilot Study
Twenty subjects (mean age: 27.4 ± 7.4 years; range 18–43 years; 11 female and 9 male) with CBCT for initial orthodontic diagnostic records at the University of California, Los Angeles (UCLA) Section of Orthodontics were randomly selected for evaluation of buccal bone thickness for maxillary and mandibular premolars and molars. Exclusion criteria included patients with craniofacial and bone anomaly and teeth with excessive buccal or lingual root torque. According to the UCLA Office for Human Research Protection, this study was exempt from review by the institutional review board.
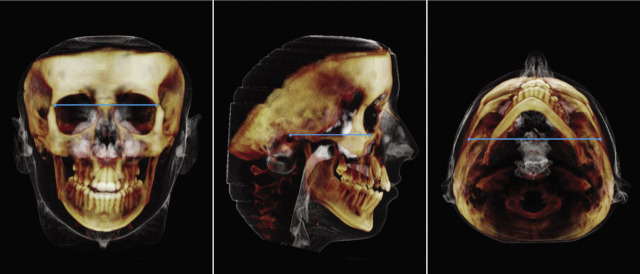
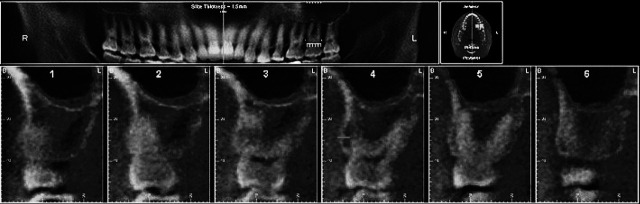
CBCT scans were captured using NewTom 3G (AFP Imaging, Elmsford, NY). Scans were performed using 12-inch field-of-view, 12-bit gray scale, and a 0.4-mm isotropic voxel. The scans were uploaded into Dolphin 3D software. Three-dimensional orientation of the skull was achieved in three views using a line drawn between Z points (Figure 2a), Frankfort horizontal plane (Figure 2b), and a line connecting the medial terminations of zygomaticotemporal sutures (Figure 2c). For each tooth, both right and left sides were measured and six tomographic cross-sections were resliced from mesial to distal. The distance between the most convex point of the buccal bone to the root surface was measured at the level of the furcation for molars and at the level where the root can be visualized in its entirety for premolars (Figure 3). The measurements were made by one operator separated by 2 weeks.
Figure 2.
Three-dimensional orientations. (a) Frontal view. (b) Right lateral view. (c) Submentovertex view.
Figure 3.
Measurement of buccal bone thickness using cross-sectional views of CBCT three-dimensional images.
Mechanical Testing
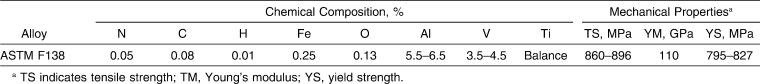
Ti-6Al-4V (ASTM F138) alloy mini-implants (Table 1) were divided into three groups: commercially-available (CA) design with 1.5 mm diameter and 6 mm length; the initial design (N1) with cylindrical shape, single-threading, shorter and wider dimensions; and the revised design (N2) with tapered shape, single-threading, and a decreased length and width from N1 (Figure 4).
Table 1.
Chemical Composition and Mechanical Properties of Micro-implants
Figure 4.
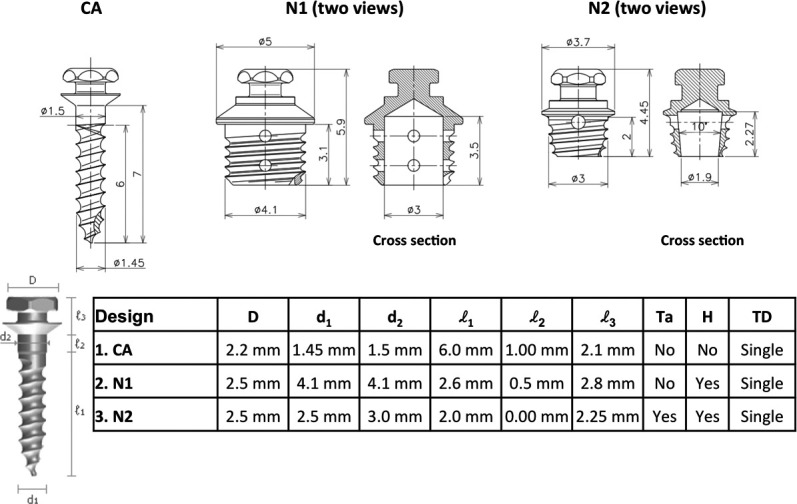
Characteristics of three mini-implant designs.
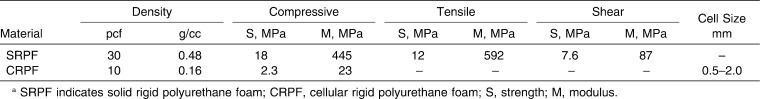
For each test, 20 mini-implants of each design were inserted by one technician into biosynthetic bone (Sawbones, Vashon, Wash) composed of two layers: 2 mm-thick 30 pcf cortical bone and 10 pcf trabecular bone (Table 2). A 1-mm thick acrylic sheet was used to simulate soft tissue thickness. All mini-implants were inserted perpendicular to the bone surface until their necks contacted the soft tissue simulation.20
Table 2.
Properties of Biosynthetic Material Simulating Cortical and Trabecular Bone
Torque Test
As in Part 1,18 each design of mini-implants (n = 20) was inserted and removed using a surgical engine and contra-angle handpiece (ElcomedSA200C, W&H, Burmoos, Austria). The unit was calibrated at each time, and rotation speed was set for 30 rpm. Maximum insertion torque (MIT) and maximum removal torque (MRT) were measured. Torque ratio (TR) of MRT to MIT was calculated: TR = MRT/MIT.
Lateral Displacement Test
Lateral displacement test was performed as described in Part 1.20 After a new set of mini-implants was inserted using a manual driver, mechanical testing was performed using the compression mode of Instron 5560 (Instron Corporation, Norwood, Mass). The software was programmed to record the perpendicular force as implants were displaced at 0.01 mm, 0.02 mm, and 0.03 mm, respectively, from their original position.
Statistical Method
Mean MIT, MRT, and force levels for each lateral displacement distance were compared across designs using one-way analysis of variance (ANOVA). Intraclass correlation was used to determine intrarater reliability. Statistical significance was defined as P < .05. Means and standard deviations were reported.
RESULTS
Buccal Bone Measurement: Pilot Study
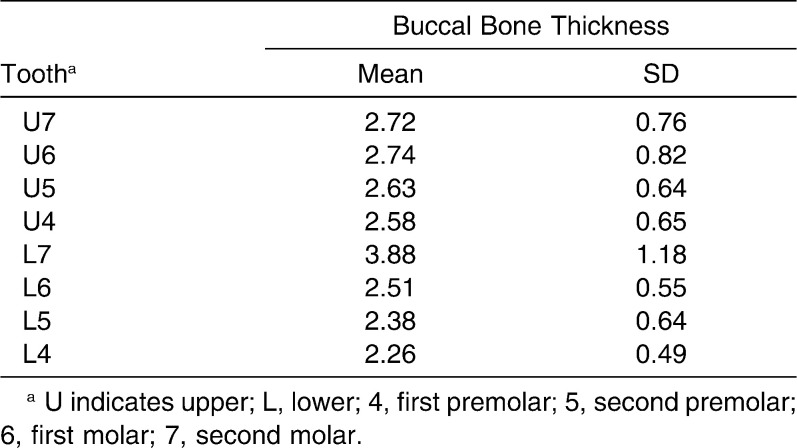
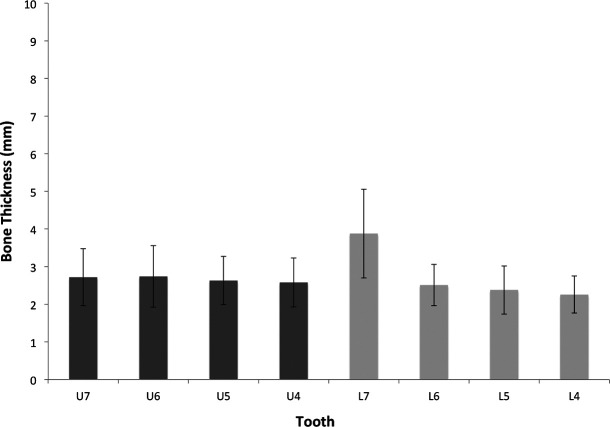
Intrarater reliability was high (r = 0.95), and the measurements proved to be reproducible. Mean values of buccal bone thickness are presented in Table 3 and Figure 5. The bone thickness ranged from 2.26 to 3.88 mm, and the thickest buccal bone was present in mandibular second molars and the least in the mandibular first premolars. The average buccal bone thickness of maxillary and mandibular posteriors was 2.71 mm.
Table 3.
Average Buccal Bone Thickness (mean mm ± SD) for Maxillary and Mandibular Posterior Teeth
Figure 5.
The mean buccal bone thickness (mm) for posterior teeth.
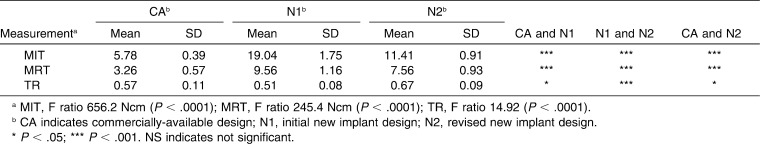
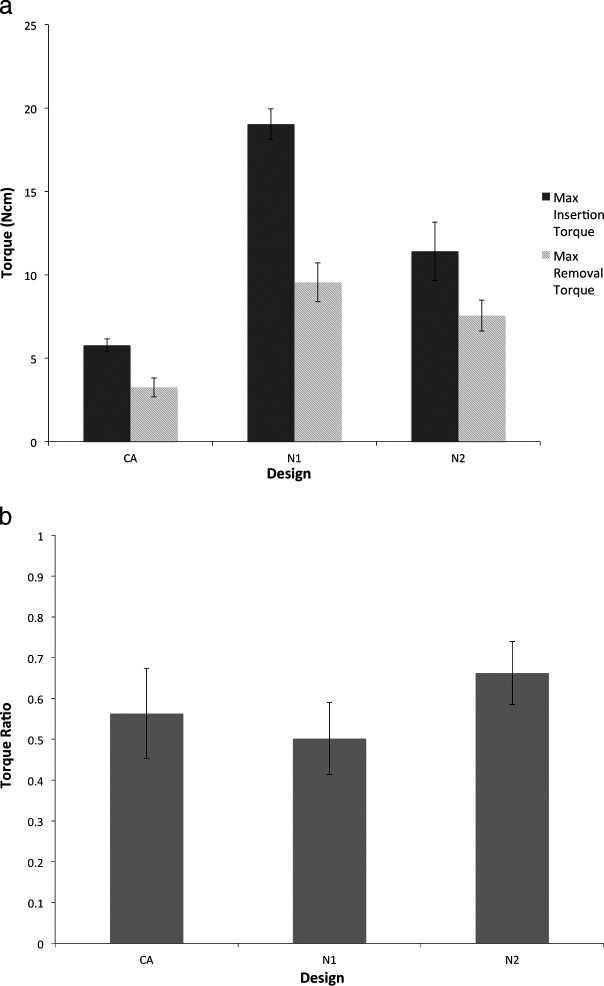
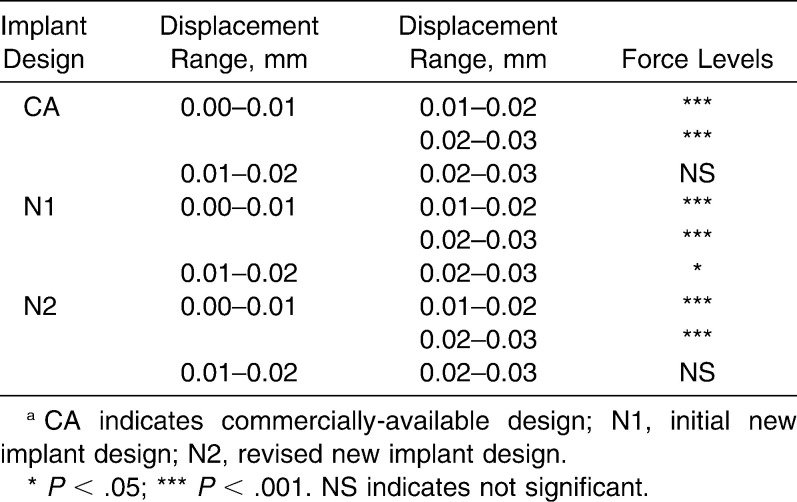
Torque Test
Both mean MIT and MRT were highest in N1, followed by N2 and CA (Table 4, Figure 6a). MRT was lower than MIT in all groups. The means of both MIT and MRT in all groups were statistically different at P < .0001 (Table 4). N2 showed higher MIT and MRT than the CA mini-implants. N2 with decreased length and diameter resulted in reductions in both MIT and MRT compared to N1. Torque ratio of N2 was the highest followed by N1 and CA (Figure 6b), and the means of TR in all groups were statistically different at P < .05 (Table 4). TR of N2 was high because MIT was decreased significantly from N1 by 7.63 Ncm, but MRT was decreased relatively less by 2.0 Ncm.
Table 4.
Maximum Insertion Torque (MIT, Mean Ncm ± SD), Maximum Removal Torque (MRT, Mean Ncm ± SD), and Torque Ratio (TR, MRT/MIT) (Mean ± SD) of Each Design
Figure 6.
(a) The means of maximum insertion and removal torque. (b) The means for torque ratio (MRT/MIT).
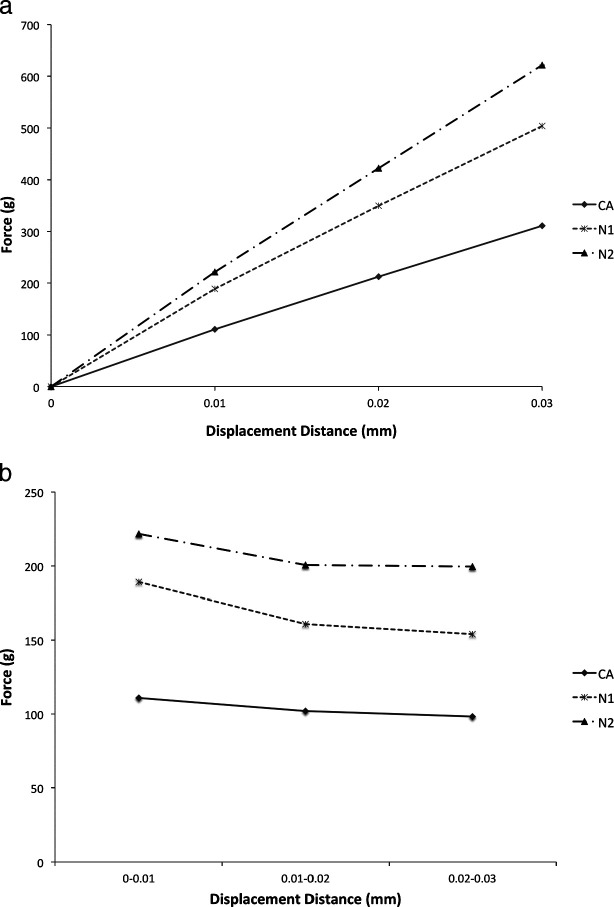
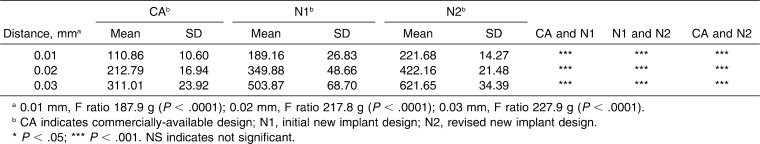
Lateral Displacement Test
Unlike the torque tests, mean force required for all three distances was greatest in N2, followed by N1 and CA (Figure 7a, Table 5). The means in all groups were significantly different at P < .0001 (Table 5).
Figure 7.
(a) Lateral displacement test summary. (b) Force required for subsequent 0.01 mm displacement.
Table 5.
Force Levels (Mean g ± SD) at 0.01-, 0.02-, 0.03-mm Lateral Displacement of Each Design
Figure 7b shows the force levels for the differences of each displacement distance by design. Across designs, the means of increment force levels were different at P < .05. For all designs, the initial displacement of 0.01 mm required the highest force compared with subsequent displacements. N1 experienced statistically significant reduction in force required for all three subsequent increments, but N2 and CA force levels for second and third 0.01-mm displacement increments were not statistically different (Table 6).
Table 6.
Cross Comparison of Force Required for 0.01-mm Increment Within Each Designa Tested by Fisher LSD Test
DISCUSSION
Interradicular spaces are generally the site of choice for mini-implant placement for their ease of access, simplicity of procedure, and less traumatic placement.9,22 However, the availability of sufficient interradicular spacing can be limited given the recommended minimum clearance of 2 mm between the implant and tooth surface.4 Thus, placement in interdental spaces restricts the choice of placement sites, biomechanics of orthodontic treatment, and size of mini-implants as the spaces are not always adequate to accommodate mini-implants with varying dimensions.23 It is therefore recommended that for placement in interradicular spaces, implants should be smaller than 1.5 mm in diameter and 6 mm in length.21,24 The commercial design used in this study has these dimensions and showed significantly compromised stability compared with the new designs (N1 and N2). In addition, mini-implants in interradicular spaces can damage or encroach upon roots and periodontal ligament during placement and orthodontic treatment and eventually lead to implant loosening.25,26 The new implants are designed to avoid root and other biologic damage and to allow placement in the bone superficial to the root surface in addition to interradicular bone.
According to the pilot CBCT study, the minimum average buccal bone thickness of 2.3 mm was discovered, and the length was shortened from 2.6 mm (N1) to 2 mm (N2) to be embedded exclusively in the bone superficial to tooth surfaces. Design revisions of shortened length, decreased diameter, and tapered interior successfully reduced excessive insertion torque of N1. The tapered and hollow interior of N2 likely diminished bone friction experienced during placement of N1 and thus further decreased insertion torque. An insertion torque range of 3.28 to 14.65 Ncm without implant breakage and bone fracture was identified,27 and N2's mean MIT was within this physiologic limit, while N1's mean MIT exceeded this range. Insertion torque needs to be balanced as high insertion torque was found to cause tensile and compressive stress to both cortical and cancellous bone tissue, and excessive stress could cause irreversible damage to the bone.28 On the other hand, very low tensile stress during placement can be insufficient to properly stimulate bone repair.28
N1 showed greater MIT and MRT than N2 consistent with previously reported positive correlation between diameter and torque values.18,29 In contrast, N2 required the greatest force to displace all three distances of 0.01, 0.02, and 0.03 mm in the lateral displacement test. This discrepancy in stability hierarchy may contribute to the microcracks introduced during the placement of N1 with high MIT. The study by Lee and Baek29 highlighted the increase in microdamage, such as the number of cracks, crack length, and crack radius, with the greater diameter but not with the added tapering of mini-implants. Similarly, N1's large diameter led to compromised mechanical stability by generating microdamage to the surrounding bone, while N2's tapering enhanced stability without the increase in microdamage. In addition, TR indicates mechanical efficiency of easy placement but relatively more difficult removal.30 Compared with N1, N2 experienced a considerable reduction in MIT (by 40%) as desired but not as much reduction in MRT (by 20%). Therefore, TR of N2 was significantly higher than N1 and CA. In mini-implant assisted orthodontics, high torque ratio of N2 design can be a more valuable mechanical property than individual torque values.
The lateral displacement test measures the force applied in transverse direction consistent with how mini-implants are utilized during orthodontic treatment.18 The lateral displacement test may be a more accurate method of assessing mechanical stability than torque testing as it better corresponds to clinical orthodontics. Clinicians experience that initial micro-movement or mobility is crucial to the success of mini-implants. Critical threshold of 50 µm to 150 µm micro-movement exists for dental implants according to Holst et al.,26 but these values cannot be applied to orthodontic implants because of differences in size and force level. Thus, in this study, the force for the smallest distances within the range of Instron 5560 equipment's sensitivity for accurate measurements was used. Pilot studies showed that 0.01 mm and additional increments of 0.01 to 0.03 mm demonstrated an evident pattern. Unlike N1, N2 did not show statistically reduced force level for 0.02- to 0.03-mm increments compared with 0.01- to 0.02-mm increments. Thus, N2's capacity to withstand as much force for subsequent displacements can be indicative of superior stability.
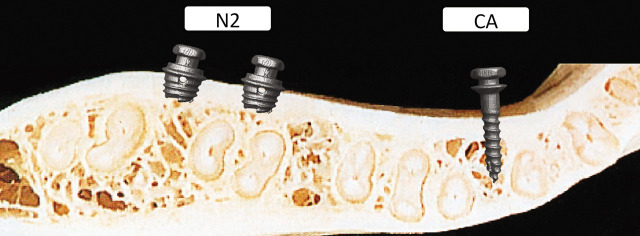
Therefore, N2 has the evident potential to be a superior design maintaining the advantages of N1 reported in Part 1: improved stability with maximum surface area engaged in cortical bone. As Cope recommended for mini-implant's future,31 N2's capacity to withstand force greater than 500 g with minimal displacement makes mini-implants for orthopedic movements a reality. N2's shorter length can further minimize risks to nearby anatomic structures such as root structures, sinus, and neurovascular bundles. For carefully selected cases, N2 can also be placed in the bone superficial to root surfaces and can continue to allow the same convenience to the clinician and patients as implants placed at interradicular sites. This superficial placement permits mini-implants to perform more efficient en-masse retraction and to be inserted without the limitation of interradicular space (Figure 8). When placing N2 in the buccal bone superficial to the root, dental expansion and molar angulation alterations need to be monitored, and the use of an appliance such as a transpalatal arch to maintain transverse dimension should be considered. Lastly, clinical trials and in vivo studies examining bone remodeling and cellular responses with N2 are required to confirm the findings of this mechanical study.
Figure 8.
Potential placement sites for N2 and CA mini-implant designs.
CONCLUSIONS
Our pilot study on buccal bone thickness of posterior teeth using CBCT showed minimum mean thickness to be 2.3 mm, and the new design (N2) was shortened to 2 mm accordingly.
Both torque and lateral displacement tests highlighted the enhanced stability of N2 compared with the most widely used commercial design (CA), which has recommended dimensions to be inserted in interradicular spaces.
N2's modified dimensions effectively mitigated insertion torque of N1, while generally maintaining comparable removal torque, resulting in high torque ratio and mechanical efficiency. N2 had superior stability to N1 in lateral displacement tests, possibly because of microdamage generated to the surrounding bone by N1's large diameter.
N2 design is very promising because it showed enhanced stability with adequate insertion torque. It has the capacity to be placed in the buccal bone superficial to the root surface and is not limited to placement in interradicular spaces, thus minimizing the risk of endangering nearby anatomic structures during placement and orthodontic treatment.
REFERENCES
- 1.Kyung S. H, Lee J. Y, Shin J. W, Hong C, Dietz V, Gianelly A. A. Distalization of the entire maxillary arch in an adult. Am J Orthod Dentofacial Orthop. 2009;135:S123–S132. doi: 10.1016/j.ajodo.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 2.Chung K. R, Kim S. H, Choo H, Kook Y. A, Cope J. B. Distalization of the mandibular dentition with mini-implants to correct a Class III malocclusion with a midline deviation. Am J Orthod Dentofacial Orthop. 2010;137:135–146. doi: 10.1016/j.ajodo.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 3.Park H. S, Kwon T. K, Sung J. H. Nonextraction treatment with microscrew implants. Angle Orthod. 2004;74:539–549. doi: 10.1043/0003-3219(2004)074<0539:NTWMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Liou E. J, Pai B. C, Lin J. C. Do miniscrews remain stationary under orthodontic forces? Am J Orthod Dentofacial Orthop. 2004;126:830–835. doi: 10.1016/j.ajodo.2003.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Young K. A, Melrose C. A, Harrison J. E. Skeletal anchorage systems in orthodontics: absolute anchorage. A dream or reality? J Orthod. 2007;34:101–110. doi: 10.1179/146531207225022005. [DOI] [PubMed] [Google Scholar]
- 6.Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 7.Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung H. M, Takano-Yamamoto T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2007;131:S68–S73. doi: 10.1016/j.ajodo.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 8.Reynders R, Ronchi L, Bipat S. Mini-implants in orthodontics: a systematic review of the literature. Am J Orthod Dentofacial Orthop. 2009;135:564.e1–e19. doi: 10.1016/j.ajodo.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 9.Chaimanee P, Suzuki B, Suzuki E. Y. “Safe Zones” for miniscrew implant placement in different dentoskeletal patterns. Angle Orthod. 2011 Jan 24 doi: 10.2319/061710-111.1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carano A, Velo S, Leone P, Siciliani G. Clinical applications of the Miniscrew Anchorage System. J Clin Orthod. 2005;39:9–24. [PubMed] [Google Scholar]
- 11.Monnerat C, Restle L, Mucha J. N. Tomographic mapping of mandibular interradicular spaces for placement of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2009;135:428.e1–e9. doi: 10.1016/j.ajodo.2008.12.003. ; discussion 428–429. [DOI] [PubMed] [Google Scholar]
- 12.Chen Y, Kyung H. M, Zhao W. T, Yu W. J. Critical factors for the success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofacial Orthop. 2009;135:284–291. doi: 10.1016/j.ajodo.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 13.Motoyoshi M, Ueno S, Okazaki K, Shimizu N. Bone stress for a mini-implant close to the roots of adjacent teeth—3D finite element analysis. Int J Oral Maxillofac Surg. 2009;38:363–368. doi: 10.1016/j.ijom.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 14.Lee Y. K, Kim J. W, Baek S. H, Kim T. W, Chang Y. I. Root and bone response to the proximity of a mini-implant under orthodontic loading. Angle Orthod. 2010;80:452–458. doi: 10.2319/070209-369.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sugawara J, Daimaruya T, Umemori M, Nagasaka H, Takahashi I, Kawamura H, Mitani H. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 2004;125:130–138. doi: 10.1016/j.ajodo.2003.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Costa A, Raffaini M, Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998;13:201–209. [PubMed] [Google Scholar]
- 17.Park H. S, Lee S. K, Kwon O. W. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod. 2005;75:602–609. doi: 10.1043/0003-3219(2005)75[602:GDMOTU]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Hong C, Lee H, Webster R, Kwak J, Wu B. M, Moon W. Stability comparison between commercially available mini-implants and a novel design. Angle Orthod. 2001 Feb 9 doi: 10.2319/092410-556.1. [Epub ahead of print] Preprint. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baumgaertel S, Hans M. G. Buccal cortical bone thickness for mini-implant placement. Am J Orthod Dentofacial Orthop. 2009;136:230–235. doi: 10.1016/j.ajodo.2007.10.045. [DOI] [PubMed] [Google Scholar]
- 20.Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery—clinical, prospective, biomechanical, and imaging study. Bone. 2005;37:776–780. doi: 10.1016/j.bone.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 21.Jolley T, Chung C. Peak torque values at fracture of orthodontic miniscrews. J Clin Orthod. 2007;41:326–328. [PubMed] [Google Scholar]
- 22.Yamada K, Kuroda S, Deguchi T, Takano-Yamamoto T, Yamashiro T. Distal movement of maxillary molars using miniscrew anchorage in the buccal interradicular region. Angle Orthod. 2009;79:78–84. doi: 10.2319/020408-68.1. [DOI] [PubMed] [Google Scholar]
- 23.Fayed M. M, Pazera P, Katsaros C. Optimal sites for orthodontic mini-implant placement assessed by cone beam computed tomography. Angle Orthod. 2010;80:939–951. doi: 10.2319/121009-709.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park J, Cho H. J. Three-dimensional evaluation of interradicular spaces and cortical bone thickness for the placement and initial stability of microimplants in adults. Am J Orthod Dentofacial Orthop. 2009;136:314.e1–e12. doi: 10.1016/j.ajodo.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 25.Chen Y. H, Chang H. H, Chen Y. J, Lee D, Chiang H. H, Yao C. C. Root contact during insertion of miniscrews for orthodontic anchorage increases the failure rate: an animal study. Clin Oral Implants Res. 2008;19:99–106. doi: 10.1111/j.1600-0501.2007.01418.x. [DOI] [PubMed] [Google Scholar]
- 26.Holst A. I, Karl M, Karolczak M, Goellner M, Holst S. Quantitative assessment of orthodontic mini-implant displacement: the effect of initial force application. Quintessence Int. 2010;41:59–66. [PubMed] [Google Scholar]
- 27.Chen Y, Kyung H. M, Gao L, Yu W. J, Bae E. J, Kim S. M. Mechanical properties of self-drilling orthodontic micro-implants with different diameters. Angle Orthod. 2010;80:821–827. doi: 10.2319/103009-607.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sotto-Maior B. S, Rocha E. P, Almeida E. O, Freitas-Júnior A. C, Anchieta R. B, Cury A. A. Influence of high insertion torque on implant placement: an anisotropic bone stress analysis. Braz Dent J. 2010;21:508–514. doi: 10.1590/s0103-64402010000600005. [DOI] [PubMed] [Google Scholar]
- 29.Lee N. K, Baek S. H. Effects of the diameter and shape of orthodontic mini-implants on microdamage to the cortical bone. Am J Orthod Dentofacial Orthop. 2010;138:8.e1–e8. doi: 10.1016/j.ajodo.2010.02.019. ; discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 30. Kim YK, Kim YJ, Yun PY, Kim JW. Effects of the taper shape, dual-thread, and length on the mechanical properties of mini-implants. Angle Orthod. 2009;79:908–914. [DOI] [PubMed]
- 31.Cope J. B. Temporary anchorage devices in orthodontics: a paradigm shift. Semin Orthod. 2005;8:3–9. [Google Scholar]