Abstract
Objective:
To assess the frequency and type of upper bonded retainer failure and to identify possible predisposing factors.
Materials and Methods:
The records of 466 consecutive patients with upper bonded retainers were analyzed retrospectively with respect to retainer failures and failure type as well as timing of failure, differences among operators, and the number of defects of the multibracket appliances (MB) prior to the retention period.
Results:
A total of 58.2% of all patients experienced retainer failures. The average failure odds were 1.26 failures per retainer. The odds were highest for 3-3 retainers (1.37) and lowest for the 1-1 retainer (0.54). The detachment and total loss rates were significantly influenced by operator experience—both rates were lower for experienced practitioners. Total retainer losses occurred more frequently in case of previous MB defects, while retainer fractures were seen more frequently when the retainer included the canines.
Conclusions:
Upper bonded retainer failures are a frequent problem during the retention period (58.2% of patients). Less operator experience correlated with higher failure rates. An increased number of total retainer losses must also be expected with a decreasing number of bonding sites and in cases involving previous MB defects.
Keywords: Orthodontic retainers, Upper bonded retainers, Failure rate, Detachment, Total loss, Fracture
INTRODUCTION
The upper incisor region has a high esthetic value, but it also exhibits a high relapse tendency after orthodontic treatment.1–3 At the same time, the patient's level of satisfaction with treatment is strongly related to the perceived stability of incisor position.4–6 Thus, retention is of special importance in this area.
It has been demonstrated7–10 that fixed retainers are a reliable form of retention for avoiding relapse and maintaining dental arch shape. Furthermore, they function regardless of patient cooperation, and they fulfill high esthetic expectations. Most studies available in the literature have clearly demonstrated that bonded retainers result in increased plaque accumulation but do not raise the risk for periodontal damage or enamel decalcification,8,9,11–15 while two other publications16,17 describe a higher risk for gingival recession.
Despite the aforementioned advantages, bonded retainers can only function reliably if they remain failure-free. However, to date there have been only two studies13,18 in the literature that provided numerical estimates of failure rates explicitly for upper bonded retainers (UBRs). The assessed failure rates varied considerably (3.1% vs 75.0%). Thus, despite the fact that UBRs are among the most frequent upper retention appliances currently used,7,19,20 there are no concise data on their failure frequency.
Possible predisposing factors for bonded retainer failure discussed in the literature9,10,13,21–27 are mainly the thickness and quality of the retainer wire, the type of composite used for bonding, the manner in which deficiencies are handled in terms of wetness or dryness of the bonding field, and occlusal trauma to the wire. Only four studies8,28–30 have considered operator experience as a possible cofactor for bonded retainer failure. In two studies,8,30 no influence of operator experience was observed for retainers in general; however, the sample size was too small to deduct an estimate of the effect size for UBRs. Johnsson et al.29 showed a significantly higher frequency of loosened or fractured retainers at a postgraduate clinic compared to a specialist clinic. Scheibe and Ruf28 clearly identified operator experience as a significant predisposing cofactor for lower bonded retainer failure. However, to date, no corresponding data exist for UBRs.
Therefore, the aim of the present study was to assess the absolute frequency of failures as well as the relative frequency of various failure types of UBRs during the retention phase. Additionally, we analyzed whether different retainer types, operator experience, or the number of defects during multibracket appliance (MB) treatment influenced the failure rate.
MATERIALS AND METHODS
The records of 2200 patients treated at the Department of Orthodontics, University of Giessen (Germany) were screened. The inclusion criteria were (1) active MB treatment completed between 1995 and 2006, (2) an active treatment and retention period that was normally completed according to German Social Insurance regulations (implying a written statement of completion by the orthodontist), and (3) insertion of a UBR. Four hundred sixty-six patients (286 males, 180 females) fulfilled all of the selection criteria. The average age of the patients at the time of first retainer bonding was 17.0 ± 6.0 years.
The UBRs were classified according to their location and number of bonding sites into canine-to-canine (3-3 UBR), lateral incisor–to–lateral incisor (2-2 UBR), and central incisor–to–central incisor (1-1 UBR) retainers and retainers comprising other teeth (other UBR).
All retainer failures, their type (detachment, total loss, fracture), and the time point of defect occurrence were consecutively extracted from the patient files. The retainer failures were defined as follows: (1) Total loss: all bonding sites of the retainer had become detached (in the statistical analysis, total losses were not additionally scored as detachments); (2) Detachment: one or more bonding sites had become detached, but the retainer was still in situ; and (3) Retainer fractures: the retainer wire had fractured at one or more sites.
For each apparent defect, the operator who had bonded the entire retainer or the detached bonding site was recorded. A distinction was made between experienced orthodontists and postgraduate students in order to analyze the influence of operator experience. To ensure a clear separation between the two groups, only dental practitioners who had completed postgraduate orthodontic training and who had thereafter worked exclusively in the field of orthodontics for at least 2 years at the time of retainer placement were classified as “experienced orthodontists.” As a consequence, five practitioners could be assigned to the “experienced orthodontists” group, while 32 postgraduate students were included in the study.
In addition, the number of defects during MB treatment (band/bracket failure, archwire loss or breakage, Herbst appliance loosening/breakage) was assessed as a possible predisposing cofactor for retainer failure. Patients without defects were compared to patients with one or more defects.
Statistical Analysis
Via Kaplan-Meier analysis, the survival rate of the retainers during the first year after placement was analyzed. The first failure within 365 days after retainer insertion was assessed as an event. Statistical significance was tested using the log rank test. In addition, statistical differences between retainer types and the relevance the possible predisposing factors (operator, number of defects during MB treatment) was calculated using the chi-square test. The following levels of significance were applied: P < .001 (***); P < .01 (**); P < .05 (*); and P ≥ .05 (ns, not significant).
RESULTS
One-Year Survival Rate
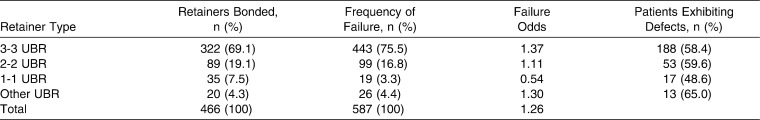
The Kaplan-Meier analysis (Figure 1) showed that 71.7% of the retainers survived the first year without any failures. It was noted that retainers bonded by orthodontists exhibited a significantly higher (P < .001) survival rate (83.9%) than did retainers bonded by postgraduate students (61.0%).
Figure 1.
One-year survival rate for upper bonded retainers (UBRs) according to the Kaplan-Meier analysis. The number of failure-free UBRs (survival rate) is plotted against time (days) for all UBRs (71.1% 5 solid line), UBRs bonded by experienced orthodontists (83.9% 5 dashed line), and postgraduate students (61.0% 5 dotted line).
Total Retention Period
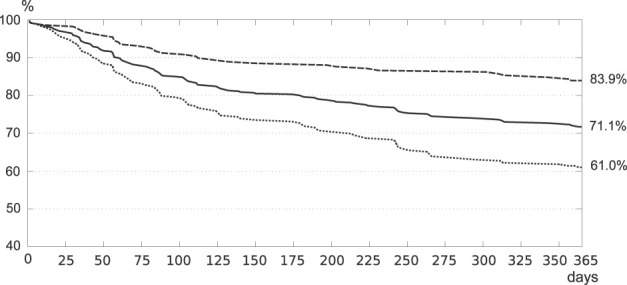
During the entire retention period (Table 1) of 30.0 ± 22.0 months, 58.2% of all patients exhibited one or more defects of their UBR. In total, 587 retainer failures occurred. These comprised 464 detachments, 67 total losses, and 56 retainer fractures. The average failure odds were 1.26 failures per retainer. The odds were highest for 3-3 retainers (1.37) and lowest for 1-1 retainer (0.54).
Table 1.
Absolute (n) and Relative (%) Frequency of the 466 Upper Bonded Retainers (UBRs) Analyzed, Their Failure Rates, and the Prevalence of Patients Exhibiting Retainer Defects Are Given Separately for 3-3 UBRs (Cuspid to Cuspid), 2-2 UBRs (Lateral Incisor to Lateral Incisor), 1-1 UBRs (Central Incisor to Central Incisor), and Other UBRs (Retainers Comprising Other Teeth)
In 11.6% of the patients, the retainer was completely lost once or several times (one loss, 9.7%; several losses, 1.9%); in other words, all bonding sites became detached at the “same” time. Total losses were more frequent in 1-1 UBRs (37.1%; P < .01) than in the other retainer types (20.2%, 2-2 UBRs; 15.0%, other UBRs; 10.2%, 3-3 UBRs) (Figure 2) and occurred more frequently (22.5% vs 5.1%; P < .001) when the retainer had been bonded by postgraduate students rather than by orthodontists. Patients with one or more appliance defects during previous MB treatment lost their retainer more often (13.8%; P < .05) than did patients without defects during their MB phase (6.8%).
Figure 2.
Frequency (%) of failures (total loss, detachment, and fracture) of different types of upper bonded retainers.
A detachment of one or more bonding sites occurred in 37.9% of the patients; 18.9% of all bonding sites were affected. Even though only 5.7% of the bonding sites of 1-1 UBRs detached, compared to 17.5% of the bonding sites in other UBRs, 19.0% in 3-3 UBRs, and 21.3% in 2-2 UBRs, the group differences did not reach statistical significance (Figure 2). Detachment of bonding sites was significantly less frequent (10.7% vs 26.2%; P < .01) in retainers bonded by orthodontists compared to those bonded by postgraduate students. For three clinicians who worked in the department for a long period both during their postgraduate and orthodontic periods, a clear learning curve could be seen (Figure 3). No relationship between the number of appliance defects during the MB phase and the frequency of detachments was noted.
Figure 3.
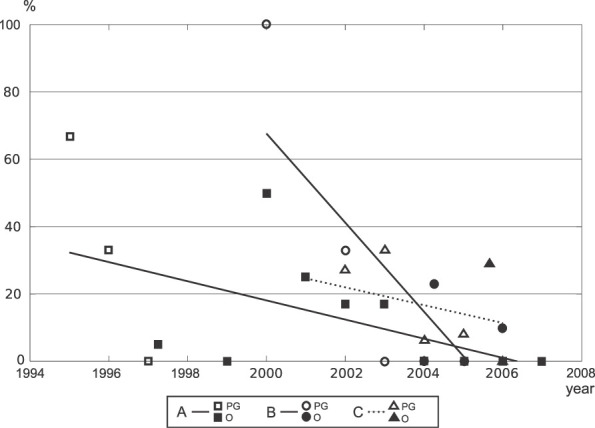
Development of the failure rates of three practitioners (A, B, and C) during their postgraduate student (PG) and orthodontist (O) periods. Please note the decrease in failure rate for all practitioners over time and thus with increasing experience.
A fracture of the UBR wire was seen in 10.5% of the patients (9.7%, one fracture; 0.8%, multiple fractures). Even though only 5.6–5.7% of the 2-2 and 1-1 UBRs fractured, compared to 13.4% of the 3-3 UBRs and 30.0% of the other UBRs (Figure 2), the group differences did not reach statistical significance. No relationship between operator experiences or the number of appliance defects during the MB phase and the frequency of fractures was seen.
In looking at the relationship among the occurrence of the first defect of a retainer, the type of defect, and the time the retainer had been in place (Figure 4), it was noticed that the probability of a detachment occurring clearly decreased with time, while the fracture probability increased.
Figure 4.
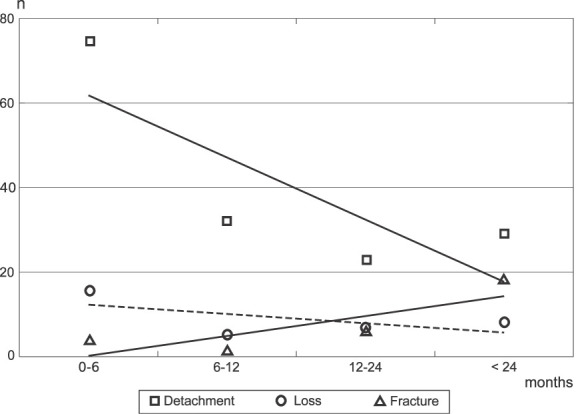
Relationship among the occurrence of the first defect of a retainer, the type of failure, and the time during which the retainer in place.
DISCUSSION
To the best of our knowledge, there are only four studies1,8,13,18 in the literature that examined failure rates of UBRs. The respective numbers of patients examined were 22, 45, 120, and 135, thus making the present study the largest conducted to date.
While the retrospective nature of the present study has its advantages in terms of group size, it does have certain disadvantages. Owing to the large number of practitioners involved over the years, the patients' records exhibited significant interindividual variation in terms of the quality of documentation. Thus, failures during active treatment (cofactor) as well as the retainer failures during retention may have been inconsistently or incompletely documented, thus implying the risk of underestimation of the actual retainer failure rates. However, as there is no flat-rate payment in the German health insurance system, it may be assumed that the documentation should have been acceptable. In addition, the type of composite or the technical procedure for retainer bonding were only rarely documented and, thus, could not be evaluated. Nevertheless, there was no difference in the basic department composite regimen between orthodontists and postgraduates.
Despite the small number of publications available in the literature, the comparison of the present findings with those of previous publications proved to be difficult. In two8,18 of the four studies, UBRs were included, but a separate analysis for upper and lower bonded retainers was not performed for every failure type, nor was the survival rate included. Furthermore, two of the studies1,8 did not differentiate between the various types of failures and instead referred to “failures” or “bonding failures” in general terms. Therefore, it was unclear whether different types of failure did in fact not occur or whether they were simply not included in the analysis. Finally, to our knowledge, total loss of a UBR has not been examined specifically in any prior study.
Over the entire observation period, 11.6% of patients exhibited at least one total retainer loss. This type of failure is most unfavorable for both patients and practitioners, as in many cases a new retainer has to be fabricated, resulting in both clearly increased costs and extended chair time compared to single bonding site detachments.
Differentiating the total losses by retainer type revealed that the 1-1 UBRs exhibited the highest total loss rate (37.1%). This seems understandable, because in 1-1 UBRs only two bonding sites must detach for a total loss to occur, while all other retainers are held in place by more bonding sites. The loss rates for 2-2 UBRs (20.2%) and 3-3 UBRs (10.2%) indicate that each additional two bonding sites decrease the loss rate by roughly a factor of two. On the other hand, postgraduate bonding increases the loss rate by a fourfold measure compared to orthodontist bonding (22.5% vs 5.1%).
Patients exhibiting failures during MB treatment showed a significantly (P < .05) higher loss rate than did patients without MB failures. This might be due to a consistent difference regarding the level of patient compliance during both active treatment and retention. Furthermore, patient-specific anomalies, such as differences in enamel structure caused by fluorosis or eating or soft drink consumption habits, may have contributed to this outcome.31–33 No comparable data are available in literature.
Throughout the retention period, 18.9% of all bonding sites detached. This rate is in concordance with those of previous studies13,18 with a clearly differentiated analysis of detachments, which reported detachment rates of 16.4% and 18.6%, respectively. The present detachment rate was influenced significantly by operator experience (10.7% vs 26.6%).
Ten and a half percent of the patients exhibited wire fractures at various positions along the retainer. The numbers of fractures increased with time and when canines had been bonded. A similar rate was found by Lumsden et al.18 Dahl and Zachrisson13 offered similar results in their study involving the contact of the lower canine with the wire. Because this contact—unlike the incisors—is point-shaped, the probability for a fracture is increased.
While the incidence of total losses and detachments had a peak during the first 6 months of retention, fractures peaked after 24 months. These results are in line with those of the literature.8,18,30 The early bonding failure peak may be explained by either bonding error or the increased tooth mobility short term after MB appliance debonding. The late retainer fracture peak seems to be due to bite deepening, resulting in canine trauma to the wire and fatigue fracture.
The present study clearly demonstrates that reduced operator experience is a predisposing factor for retainer failure. Previously, only Lumsden et al.18 and Segner and Heinrici8 had analyzed this relationship, but only Lumsden et al.18 conducted a Kaplan-Meier analysis exclusively for UBRs (1-year survival rate = 57%). Thus, in comparison, the present 1-year survival rate was higher both for orthodontists (83.9%) and for postgraduate students (61.0%). This is noteworthy, because in the examination by Lumsden et al.18 all retainers were placed by the same operator, whose experience in orthodontics is, however, not stated. In contrast, Segner and Heinrici8 did not find any association between operator experience and failure rates. Basically, it seems logical that postgraduate students have less routine and thus more failures. In addition, in a university setting such as the one in which the present study was performed, the postgraduate student will additionally have the disadvantage of being assisted by less experienced nurses. Therefore, the present findings for postgraduate failure rates might be a little higher than would be expected under private office conditions.
At first glance, the survival rate of UBRs, with an overall average of 71.1%, seems a satisfactory result. However, in looking at the decreased survival rate of postgraduate students (61%), it quickly becomes clear that UBRs are prone to defects more often than we would have expected. This becomes even clearer when we consider that almost 60% of the patients experienced one or more defects during the retention period and that the failure odds were 1.26 per bonded retainer. Giving the clinically well-known problem that the most frequent UBR failure type—the detachment—frequently goes unnoticed by the patient, and given the fact that detachments peak during the first 6 months after MB debonding, frequent retention controls might be advisable during that period.
CONCLUSIONS
Upper bonded retainers exhibited frequent failures (odds 1 = 1.26 failures per retainer).
Detachments were the most frequent failure.
One or more defects during active MB treatment were associated with significantly higher detachment and total loss rates.
The detachment and total loss rates were significantly influenced by operator experience—both rates were lower for experienced practitioners.
REFERENCES
- 1.Naraghi S, Andren A, Kjellberg H, Mohlin B. O. Relapse tendency after orthodontic correction of upper front teeth retained with a bonded retainer. Angle Orthod. 2006;76:570–576. doi: 10.1043/0003-3219(2006)076[0570:RTAOCO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Helm S, Kreiborg S, Solow B. Psychosocial impact of malocclusion: a 15-year follow-up study in 30-year-old Danes. Am J Orthod. 1985;87:110–118. doi: 10.1016/0002-9416(85)90020-x. [DOI] [PubMed] [Google Scholar]
- 3.Van der Linden F. Theoretical and practical aspects of crowding in the human dentition. J Am Dent Assoc. 1974;89:139–153. doi: 10.14219/jada.archive.1974.0308. [DOI] [PubMed] [Google Scholar]
- 4.Mollov N. D, Lindauer S. J, Best A. M, Shroff B, Tufekci E. Patient attitudes toward retention and perceptions of treatment success. Angle Orthod. 2010;80:468–473. doi: 10.2319/102109-594.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Espeland L. V, Stenvik A. Perception of personal dental appearance in young adults: relationship between occlusion, awareness, and satisfaction. Am J Orthod Dentofacial Orthop. 1991;100:234–241. doi: 10.1016/0889-5406(91)70060-A. [DOI] [PubMed] [Google Scholar]
- 6.Shaw W. C. Factors influencing the desire for orthodontic treatment. Eur J Orthod. 1981;3:151–162. doi: 10.1093/ejo/3.3.151. [DOI] [PubMed] [Google Scholar]
- 7.Cerny R. The reliabilty of bonded lingual retainers. Aust Orthod. 2007;23:24–29. [PubMed] [Google Scholar]
- 8.Segner D, Heinrici B. Bonded retainers—clinical reliability. J Orofac Orthop. 2000;61:352–358. doi: 10.1007/pl00001905. [DOI] [PubMed] [Google Scholar]
- 9.Årtun J, Spadafora A. T, Shapiro P. A. A 3-year follow-up study of various types of orthodontic canine-to-canine retainers. Eur J Orthod. 1997;19:501–509. doi: 10.1093/ejo/19.5.501. [DOI] [PubMed] [Google Scholar]
- 10.Bearn D. R, McCabe J. F, Gordon P. H, Aird J. C. Bonded orthodontic retainers: the wire-composite interface. Am J Orthod Dentofacial Orthop. 1997;111:67–74. doi: 10.1016/s0889-5406(97)70304-4. [DOI] [PubMed] [Google Scholar]
- 11.Booth F. A, Edelman J. M, Proffit W. R. Twenty-year follow-up of patients with permanently bonded mandibular canine-to-canine retainers. Am J Orthod Dentofacial Orthop. 2008;133:70–76. doi: 10.1016/j.ajodo.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 12.Butler J, Dowling P. Orthodontic bonded retainers. J Ir Dent Assoc. 2005;51:29–32. [PubMed] [Google Scholar]
- 13.Dahl E. H, Zachrisson B. U. Long-term experience with direct-bonded lingual retainers. J Clin Orthod. 1991;25:619–630. [PubMed] [Google Scholar]
- 14.Årtun J. Caries and periodontal reactions associated with long-term use of different types of bonded lingual retainers. Am J Orthod. 1984;86:112–118. doi: 10.1016/0002-9416(84)90302-6. [DOI] [PubMed] [Google Scholar]
- 15.Zachrisson B. U. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod. 1977;71:440–448. doi: 10.1016/0002-9416(77)90247-0. [DOI] [PubMed] [Google Scholar]
- 16.Tacken M. P, Cosyn J, De Wilde P, Aerts J, Govaerts E, Vannet B. V. Glass fibre reinforced versus multistranded bonded orthodontic retainers: a 2 year prospective multi-centre study. Eur J Orthod. 2010;32:117–123. doi: 10.1093/ejo/cjp100. [DOI] [PubMed] [Google Scholar]
- 17.Levin L, Samorodnitzky-Naveh G. R, Machtei E. E. The association of orthodontic treatment and fixed retainers with gingival health. J Periodontol. 2008;79:2087–2092. doi: 10.1902/jop.2008.080128. [DOI] [PubMed] [Google Scholar]
- 18.Lumsden K. W, Saidler G, McColl J. H. Breakage incidence with direct-bonded lingual retainers. Br J Orthod. 1999;26:191–194. doi: 10.1093/ortho/26.3.191. [DOI] [PubMed] [Google Scholar]
- 19.Renkema A. M, Sips E. T, Bronkhorst E, Kuijipers-Jagtman A. M. A survey on orthodontic retention procedures in The Netherlands. Eur J Orthod. 2009;31:432–437. doi: 10.1093/ejo/cjn131. [DOI] [PubMed] [Google Scholar]
- 20.Singh P, Grammati S, Kirschen R. Orthodontic retention patterns in the United Kingdom. J Orthod. 2009;36:115–121. doi: 10.1179/14653120723040. [DOI] [PubMed] [Google Scholar]
- 21.Aldrees A. M, Al-Mutairi T. K, Hakami Z. W, Al-Malki M. M. Bonded orthodontic retainers: a comparison of initial bond strength of different wire-and-composite combinations. J Orofac Orthop. 2010;71:290–299. doi: 10.1007/s00056-010-9947-5. [DOI] [PubMed] [Google Scholar]
- 22.Cooke M. E, Sherriff M. Debonding force and deformation of two multi-stranded lingual retainer wires bonded to incisor enamel: an in vitro study. Eur J Orthod. 2010;32:741–746. doi: 10.1093/ejo/cjq017. [DOI] [PubMed] [Google Scholar]
- 23.Yagci A, Uysal T, Ertas H, Amasyali M. Mikroleakage between composite/wire and composite/enamel interfaces of flexible spiral wire retainers: direct versus indirect application methods. Orthod Craniofac Res. 2010;13:118–124. doi: 10.1111/j.1601-6343.2010.01486.x. [DOI] [PubMed] [Google Scholar]
- 24.Sari Z, Uysal T, Başçiftçi F. A, Inan O. Occlusal contact changes with removable and bonded retainers in a 1-year retention period. Angle Orthod. 2009;79:867–872. doi: 10.2319/101608-536.1. [DOI] [PubMed] [Google Scholar]
- 25.Uysal T, Ulker M, Baysal A, Usumez S. Different lingual retainer composites and the microleakage between enamel-composite and wire-composite interfaces. Angle Orthod. 2008;78:941–946. doi: 10.2319/072707-350.1. [DOI] [PubMed] [Google Scholar]
- 26.Störmann I, Ehmer U. A prospective randomized study of different retainer types. J Orofac Orthop. 2002;63:42–50. doi: 10.1007/s00056-002-0040-6. [DOI] [PubMed] [Google Scholar]
- 27.Radlanski R. J, Zain N. D. Stability of the bonded lingual wire retainer—a study of the initial bond strength. J Orofac Orthop. 2004;65:321–335. doi: 10.1007/s00056-004-0401-4. [DOI] [PubMed] [Google Scholar]
- 28.Scheibe K, Ruf S. Lower bonded retainers: survival and failure rates particularly considering operator experience. J Orofac Orthop. 2010;71:300–307. doi: 10.1007/s00056-010-1015-7. [DOI] [PubMed] [Google Scholar]
- 29.Johnsson A. C, Tofelt L. N, Kjellberg H. Subjective evaluation of orthodontic treatment and potential side effects of bonded lingual retainers. Swed Dent J. 2007;31:35–44. [PubMed] [Google Scholar]
- 30.Lie Sam Foek D. J, Ozcan M, Verkerke G. J, Sandham A, Dijkstra P. U. Survival of flexible, braided, bonded stainless steel lingual retainers: a historic cohort study. Eur J Orthod. 2008;30:199–204. doi: 10.1093/ejo/cjm117. [DOI] [PubMed] [Google Scholar]
- 31.Shida K, Kitasako Y, Burrow M, Tagami J. Micro-shear bond strengths and etching efficacy of a two-step self-etching adhesive system to fluorosed and non-fluorosed enamel. Eur J Oral Sci. 2009;117:182–186. doi: 10.1111/j.1600-0722.2009.00609.x. [DOI] [PubMed] [Google Scholar]
- 32.Oncag G, Tuncer A. V, Tosun Y. S. Acidic soft drinks effects on the shear bond strength of orthodontic brackets and a scanning electron microscopy evaluation of the enamel. Angle Orthod. 2005;75:247–253. doi: 10.1043/0003-3219(2005)075<0243:ASDEOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 33.Ulusoy C, Müjdeci A, Gökay O. The effect of herbal teas on the shear bond strength of orthodontic brackets. Eur J Orthod. 2009;31:385–389. doi: 10.1093/ejo/cjn129. [DOI] [PubMed] [Google Scholar]