Abstract
Objective:
To evaluate the success rate of Bollard miniplate anchorage for bone anchored maxillary protraction (BAMP).
Materials and Methods:
Twenty-five consecutive patients (mean age, 12.0 ± 1.2 years; range, 8.7–14.8 years) with maxillary hypoplasia without congenital or acquired deformation were included in this study. A total of 100 Bollard modified miniplates were placed by the same surgeon. Ninety-nine miniplates were inserted under general anesthesia, and one was placed under local anesthesia because of initially soft bone conditions. Loading of the miniplates with 150 g elastics was initiated at 17.5 ± 6.9 days (range, 11–38 days) after surgery. Mean follow-up was provided at 20.8 ± 11.1 months (range, 6.5–46.2 months).
Results:
The overall success rate of miniplate anchorage in terms of stability was 97%. During orthodontic loading, five miniplates showed signs of mobility. After interruption of loading over 2 months, two miniplates became stable again. However, a total of three miniplates needed to be removed and were successfully replaced under local anesthesia after a mean healing period of 3 months.
Conclusion:
Skeletal anchorage by means of Bollard modified miniplates is effective for BAMP. Success depends on proper presurgical patient counseling, minimal invasive surgery, good postsurgical instructions, and orthodontic follow-up.
Keywords: Miniplate anchorage, Bone anchored maxillary protraction, Success rate
INTRODUCTION
Correction of maxillary hypoplasia during growth by orthopedic maxillary protraction was pioneered by Delaire in the 1970s.1,2 The main disadvantages of Delaire face mask therapy are noncompliance due to discomfort, dentoalveolar compensation, and clockwise rotation of the mandible.3–6 To reduce these side effects, modified methods of maxillary protraction were developed consisting of (1) maxillary distraction by a rigid external distractor7–12; (2) maxillary distraction with a face mask after Le Fort I corticotomy in cleft patients13–15; and (3) face mask combined with skeletal anchorage in the upper jaw.16–18 The first two modified methods of maxillary protraction involved Le Fort I corticotomy or osteotomy; the two latter protocols still involved the use of a face mask.
Over several years, bone anchored maxillary protraction (BAMP) without corticotomy or osteotomy with the use of class III elastics between miniplate skeletal anchorage in the upper and lower jaw was introduced.19,20 With this approach, an extraoral face mask is no longer needed and intermaxillary traction can be applied 24 hours a day. Preliminary studies based on conventional two-dimensional (2D) cephalometric analysis21,22 and three-dimensional (3D) virtual treatment outcome analysis23 showed already very promising results. However, the stability and success rate of miniplate anchorage for BAMP had not been investigated yet. Hence, the aim of this prospective study was to evaluate the success rate of Bollard miniplate anchorage for BAMP in growing children.
MATERIALS AND METHODS
This prospective study was approved by the Institutional Review Board of the AZ St-Jan Hospital. A total of 25 consecutive patients were included. All patients were referred for BAMP by four different orthodontists (L.G.: n = 4; T.B.: n = 1; V.G.: n = 1; and H.D.C.: n = 19), and all presented with maxillary hypoplasia and Angle Class III malocclusion. No patients had clefts, syndromes, or traumatic history. The mean age of patients at the time of surgery was 12.0 ± 1.2 years (range, 8.7–14.8 years). Seven male (mean age, 12.0 ± 1.2 years; range, 10.7–14.8 years) and 18 female patients (mean age, 12.2 ± 1.3 years; range, 8.7–13.7 years) were included.
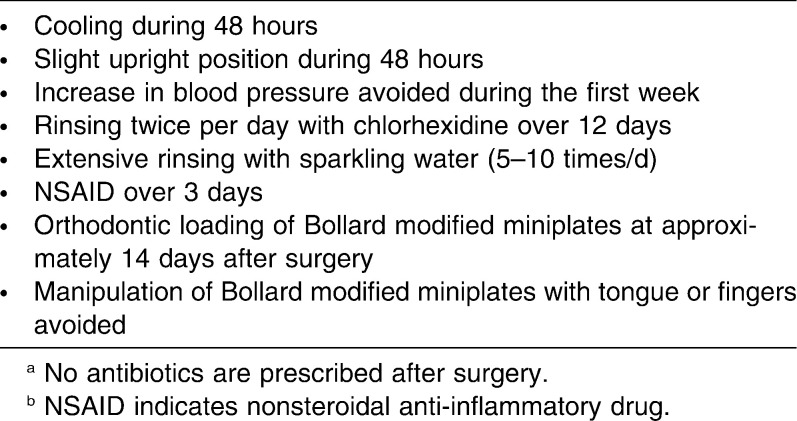
Presurgical patient counseling and surgery under general anesthesia were provided in a one-day clinic visit to all patients by the same surgeon. Although insertion of four plates can be done under local anesthesia, young patients feel more comfortable with a procedure done under sedation or under a short general anesthesia. In all patients, the same miniplate anchorage system (Bollard Modified Miniplate, Tita-Link, Brussels, Belgium) was placed in a standardized way after a minimal invasive flap was raised, as previously described.24 In the upper jaw, “Upper Bollards with hooks” were placed at the right and left infrazygomatic crest, while in the lower jaw, “Lower Bollards with hooks” were placed on both sides between the lower canine and the lateral incisor (Figure 1). In all patients, the Bollard miniplates were fixed with monocortical (5–7 mm length; 2.3 mm diameter) Titamed Bollard Miniplate Screws (Titamed, Wervik, Belgium). Upper miniplates were fixed by three screws, and two screws were used in the mandible (Figure 2). In the first six patients, self-tapping screws were used, and in the following 19 patients, self-drilling screws were applied. A single dose of IV antibiotics (amoxicillin and clavulanic acid) was given during surgery, but no corticosteroids were administered. Postsurgical instructions were given to all patients by the same surgeon and by the referring orthodontist. Patients were instructed not to manipulate the miniplates with tongue or fingers. Loading of Bollard modified miniplates with 150 g elastics was initiated by the referring orthodontist 17.5 ± 6.9 days (range, 11–38 months) after surgery and was maintained for a period of 12 months. Mean follow-up was 20.8 ± 11.1 months (range, 6.5–46.2 months).
Figure 1.
Placement of Bollard modified miniplates for bone anchored maxillary protraction (BAMP). In this particular case, a square wire was placed in the 0.018 × 0.025-inch tube of the lower left Bollard to slightly modify the vector of intermaxillary traction to avoid irritation of gingival soft tissues in the left lower jaw.
Figure 2.
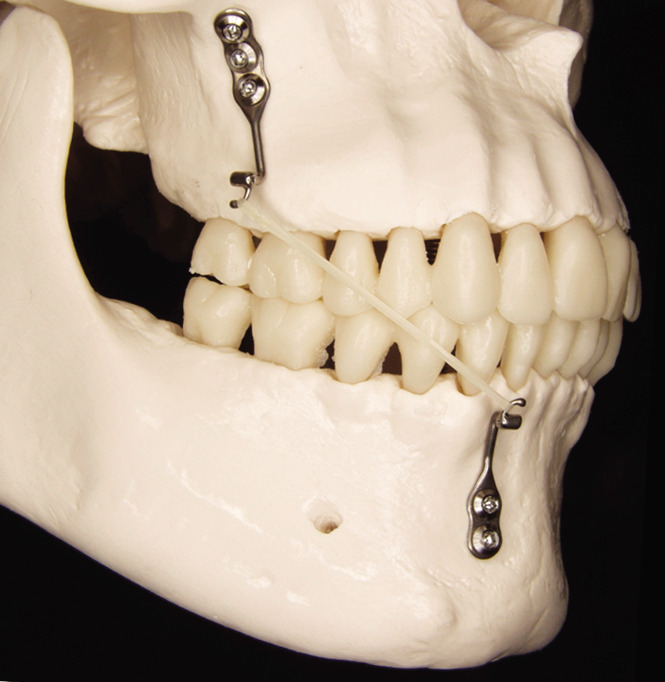
The upper miniplate is fixed by three monocortical screws at the infrazygomatic crest, and the lower miniplate with two screws between the lateral incisor and the canine.
RESULTS
In 25 consecutive patients, 99 Bollard modified miniplates could be placed with excellent primary stability under general anesthesia. In one 12-year-old male patient, fixation of the upper miniplate at the right infrazygomatic crest with good primary stability was not feasible because bone conditions were soft. After a bone healing period of 12 weeks, the upper miniplate could be successfully fixed under local anesthesia. In the lower jaw, miniplates could be placed in all patients between the lateral incisor and the canine.
No infections occurred. Four patients, however, complained about irritation of the mucosa of the cheeks or lower lip at the first visit after surgery. This was easily solved by covering the fixation unit of the miniplate with a small piece of soft wax, until edema of the soft tissues completely disappeared. The overall success rate in terms of stability of Bollard miniplate anchorage was 97%. During orthodontic loading, five miniplates in five different patients showed signs of mobility with small discomfort. In these cases, loading was interrupted for 2 months. After this period, two miniplates became stable again, and three miniplates needed to be removed and replaced under local anesthesia 3 months later. In two patients, fracture of a hook of the miniplate occurred and was solved by insertion of a custom-made hook of a square wire in the 0.018 × 0.025-inch tube of the fixation unit.
DISCUSSION
Failure and success rates of miniscrews have been well investigated in the literature.25–29 Miniplates have been shown to be well accepted as skeletal anchorage by both patients and providers and have turned out to be a safe and effective adjunct for complex orthodontic treatment.24 However, the success rate of miniplates for skeletal anchorage in orthodontics30–33 has not been investigated so thoroughly as that of miniscrews, and research has been limited to adolescent and adult patients. Compared with miniscrews and microscrews, miniplates showed greater stability.31 However, only the effect of continuous loading on miniplate stability has been investigated. The forces generated by intermaxillary elastics are discontinuous in time, magnitude, and direction because of movements of the mandible during speech, chewing, and swallowing.
To our knowledge, up to now no report has been published on the failure rate of miniplates used for maxillary protraction by intermaxillary elastics in young growing patients. BAMP is the most critical procedure regarding stability and patient morbidity in the use of miniplate anchorage in orthodontics. Initial mechanical retention of osteosynthesis screws is mainly influenced by the thickness and density of the external cortical bone and is reduced in growing children compared with adult patients. In a prospective study on 200 miniplates, most failures occurred in the youngest patients.24 However, the mean age of patients in this study was 24 years, and different miniplate designs and loading protocols were used.
Results of this prospective study showed a high overall success rate of 97%. All failures occurred in the upper jaw in contrast to reported higher failure rates of miniscrews in the lower jaw.29,34–36 The latter data, however, were derived from clinical studies in older patients. Only a few studies37–39 have documented the success rates of miniscrews in early teenagers. Also, in a retrospective study on the stability of 68 miniplates, all failures were observed in the mandible.30 However, the patients were adults, the plates in the lower jaw were inserted between the first and second molars, and the design of the plates complicated oral hygiene. All failures in our study occurred in the youngest patients. The authors therefore propose not to place miniplates for skeletal anchorage in orthodontics before the age of 11 years, because of increased risk of poor bone quality. No significant differences were observed in the stability of plates fixed by self-taping or self-drilling screws. Therefore the authors recommend self-drilling screws, which are easier to use.
The high success rate in this study may be related to several factors: (1) presurgical counseling of the patient, (2) minimal invasive surgery with decreased patient morbidity and adequate postsurgical instructions (Table 1), and (3) good orthodontic follow-up. Presurgical counseling is extremely important to prepare both young patients and their parents. Special attention should be paid to the importance of avoiding repetitive manipulation of the miniplates by tongue or fingers after surgery. Minimal invasive surgery consisting of small incisions, tunnel preparation, and gentle handling of the soft tissues is of major importance. Application of Elocom cream (mometasone furoate 1 mg) to the lips, additional local anesthesia (xylocaine 1% adrenaline) for vasoconstriction, and topical application of Exacyl (tranexamic acid) proved useful in decreasing postsurgical swelling and patient morbidity. Extensive rinsing with NaCl during surgery is important to avoid infection; application of wax to the miniplates at the end of surgery proved very helpful in decreasing soft tissue irritation.
Table 1.
Postsurgical Instructions to the Patienta,b
Last but not least, good orthodontic follow-up consisting of oral hygiene instructions and evaluation of miniplate anchorage (ie, local gingival status, mobility, hygiene, elastic force) is essential for treatment outcome.
CONCLUSIONS
Miniplate anchorage with Bollard modified miniplates is highly effective for bone anchored maxillary protraction (BAMP).
Success depends on proper presurgical patient counseling, minimal invasive surgery, good postsurgical instructions, and orthodontic follow-up.
Acknowledgments
The authors thank the orthodontists T. Bataille, V. Geerinckx, L. Govaert, and H. De Clerck for their cooperation.
REFERENCES
- 1.Delaire J. Manufacture of the “orthopedic mask.”. Rev Stomatol Chir Maxillofac. 1971;72:579–582. [PubMed] [Google Scholar]
- 2.Delaire J. Treatment of Class III with dentofacial orthopedic mask. Acta Odontol Venez. 1979;17:168–200. [PubMed] [Google Scholar]
- 3.Baik H. S. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 4.Kapust A. J, Sinclair P. M, Turley P. K. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113:204–212. doi: 10.1016/s0889-5406(98)70141-6. [DOI] [PubMed] [Google Scholar]
- 5.Takada K, Petdachai S, Sakuda M. Changes in dentofacial morphology in skeletal Class III children treated by a modified maxillary protraction headgear and a chin cup: a longitudinal cephalometric appraisal. Eur J Orthod. 1993;15:211–221. doi: 10.1093/ejo/15.3.211. [DOI] [PubMed] [Google Scholar]
- 6.Baccetti T, McGill J. S, Franchi L, McNamara J. A, Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 7.Polley J. W, Figueroa A. A. Rigid external distraction: its application in cleft maxillary deformities. Plast Reconstr Surg. 1998;102:1360–1372; discussion 1373–1374. [PubMed] [Google Scholar]
- 8.Figueroa A. A, Polley J. W. Management of severe cleft maxillary deficiency with distraction osteogenesis: procedure and results. Am J Orthod Dentofacial Orthop. 1999;115:1–12. doi: 10.1016/S0889-5406(99)70310-0. [DOI] [PubMed] [Google Scholar]
- 9.Figueroa A. A, Polley J. W, Ko E. W. Maxillary distraction for the management of cleft maxillary hypoplasia with a rigid external distraction system. Semin Orthod. 1999;5:46–51. doi: 10.1016/s1073-8746(99)80042-5. [DOI] [PubMed] [Google Scholar]
- 10.Swennen G, Dujardin T, Goris A, De Mey A, Malevez C. Maxillary distraction osteogenesis: a method with skeletal anchorage. J Craniofac Surg. 2000;11:120–127. doi: 10.1097/00001665-200011020-00009. [DOI] [PubMed] [Google Scholar]
- 11.Swennen G, Figueroa A. A, Schierle H, Polley J. W, Malevez C. Maxillary distraction osteogenesis: a two-dimensional mathematical model. J Craniofac Surg. 2000;11:312–317. doi: 10.1097/00001665-200011040-00006. [DOI] [PubMed] [Google Scholar]
- 12.Hierl T, Hemprich A. A novel modular retention system for midfacial distraction osteogenesis. Br J Oral Maxillofac Surg. 2000;38:623–626. doi: 10.1054/bjom.2000.0469. [DOI] [PubMed] [Google Scholar]
- 13.Molina F, Ortiz Monasterio F, de la Paz Aguilar M, Barrera J. Maxillary distraction: aesthetic and functional benefits in cleft lip-palate and prognathic patients during mixed dentition. Plast Reconstr Surg. 1998;101:951–963. doi: 10.1097/00006534-199804040-00010. [DOI] [PubMed] [Google Scholar]
- 14.Swennen G, Colle F, De May A, Malevez C. Maxillary distraction in cleft lip palate patients: a review of six cases. J Craniofac Surg. 1999;10:117–122. doi: 10.1097/00001665-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Rachmiel A, Aizenbud D, Ardekian L, Peled M, Laufer D. Surgically-assisted orthopedic protraction of the maxilla in cleft lip and palate patients. Int J Oral Maxillofac Surg. 1999;28:9–14. [PubMed] [Google Scholar]
- 16.Singer S. L, Henry P. J, Rosenberg I. Osseointegrated implants as an adjunct to facemask therapy: a case report. Angle Orthod. 2000;70:253–262. doi: 10.1043/0003-3219(2000)070<0253:OIAAAT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Enacar A, Giray B, Pehlivanoglu M, Iplikcioglu H. Facemask therapy with rigid anchorage in a patient with maxillary hypoplasia and severe oligodontia. Am J Orthod Dentofacial Orthop. 2003;123:571–577. doi: 10.1067/mod.2003.S0889540603000520. [DOI] [PubMed] [Google Scholar]
- 18.Kircelli B. H, Pektas Z. O. Midfacial protraction with skeletally anchored face mask therapy: a novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440–449. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 19.De Clerck H. J, Geerinckx V, Silicano S. The zygoma anchorage system. J Clin Orthod. 2002;36:455–459. [PubMed] [Google Scholar]
- 20.De Clerck H. J, Cornelis M. A, Cevidanes L. H, Heymann G. C, Tulloch C. J. Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg. 2009;67:2123–2129. doi: 10.1016/j.joms.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cevidanes L, Baccetti T, Franchi L, McNamara J. A, Jr, De Clerck H. Comparison of two protocols for maxillary protraction: bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010;80:799–806. doi: 10.2319/111709-651.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Clerck H, Cevidanes L, Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop. 2010;138:577–581. doi: 10.1016/j.ajodo.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heymann G. C, Cevidanes L, Cornelis M, De Clerck H. J, Tulloch J. F. Three-dimensional analysis of maxillary protraction with intermaxillary elastics to miniplates. Am J Orthod Dentofacial Orthop. 2010;137:274–284. doi: 10.1016/j.ajodo.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cornelis M. A, Scheffler N. R, Mahy P, Siciliano S, De Clerck H. J, Tulloch J. F. Modified miniplates for temporary skeletal anchorage in orthodontics: placement and removal surgeries. J Oral Maxillofac Surg. 2008;66:1439–1445. doi: 10.1016/j.joms.2008.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen Y. J, Chang H. H, Lin H. Y, Lai E. H, Hung H. C, Yao C. C. Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Implants Res. 2008;19:1188–1196. doi: 10.1111/j.1600-0501.2008.01571.x. [DOI] [PubMed] [Google Scholar]
- 26.Schätzle M, Männchen R, Zwahlen M, Lang N. P. Survival and failure rates of orthodontic temporary anchorage devices: a systematic review. Clin Oral Implants Res. 2009;20:1351–1359. doi: 10.1111/j.1600-0501.2009.01754.x. Epub 2009 Sep 30. Review. [DOI] [PubMed] [Google Scholar]
- 27.Viwattanatipa N, Thanakitcharu S, Uttraravichien A, Pitiphat W. Survival analyses of surgical miniscrews as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2009;136:29–36. doi: 10.1016/j.ajodo.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 28.Chen Y, Kyung H. M, Zhao W. T, Yu W. J. Critical factors for the success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofacial Orthop. 2009;135:284–291. doi: 10.1016/j.ajodo.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 29.Crismani A. G, Bertl M. H, Celar A. G, Bantleon H. P, Burstone C. J. Miniscrews in orthodontic treatment: review and analysis of published clinical trials. Am J Orthod Dentofacial Orthop. 2010;137:108–113. doi: 10.1016/j.ajodo.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 30.Choi B. H, Zhu S. J, Kim Y. H. A clinical evaluation of titanium miniplates as anchors for orthodontic treatment. Am J Orthod Dentofacial Orthop. 2005;128:382–384. doi: 10.1016/j.ajodo.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y. J, Chang H. H, Huang C. Y, Hung H. C, Lai E. H, Yao C. C. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007;18:768–775. doi: 10.1111/j.1600-0501.2007.01405.x. Epub 2007 Sep 14. [DOI] [PubMed] [Google Scholar]
- 32.Chen C. H, Hsieh C. H, Tseng Y. C, Huang I. Y, Shen Y. S, Chen C. M. The use of miniplate osteosynthesis for skeletal anchorage. Plast Reconstr Surg. 2007;120 doi: 10.1097/01.prs.0000264110.54862.95. [DOI] [PubMed] [Google Scholar]
- 33.Eroğlu T, Kaya B, Cetinşahin A, Arman A, Uçkan S. Success of zygomatic plate-screw anchorage system. J Oral Maxillofac Surg. 2010;68:602–605. doi: 10.1016/j.joms.2009.04.132. [DOI] [PubMed] [Google Scholar]
- 34.Park H. S. Clinical study on success rate of microscrew implants for orthodontic anchorage. Korean J Orthod. 2003;33:151–156. [Google Scholar]
- 35.Chen C. H, Chang C. S, Hsieh C. H, et al. The use of microimplants in orthodontic anchorage. J Oral Maxillofacial Surg. 2006;64:1209–1213. doi: 10.1016/j.joms.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 36.Miyawaki S, Koyama I, Inoue M. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 37.Park H. S, Jeong S. H, Kwon O. W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 38.Gelgor I. E, Buyukyilmaz T, Karaman A. I, Dolanmaz D, Kalayci A. Intraosseous screw-supported upper molar distalization. Angle Orthod. 2004;74:838–850. doi: 10.1043/0003-3219(2004)074<0838:ISUMD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 39.Herman R. J, Currier G. F, Miyake A. Mini-implant anchorage for maxillary canine retraction: a pilot study. Am J Orthod Dentofacial Orthop. 2006;130:228–235. doi: 10.1016/j.ajodo.2006.02.029. [DOI] [PubMed] [Google Scholar]