Abstract
Background
In search of innovative approaches to the challenge of uncontrolled hypertension, we assessed the association between preference for immediate gratification (i.e., high discounting rate), low medication adherence, and uncontrolled blood pressure (BP) in adults with hypertension.
Methods
Using a probability discounting model and the Collier–Williams hypothetical discount rate framework, participants in this cross-sectional study reported their preference for a smaller amount of money available immediately (high discount rate; immediate gratification preference) vs. a larger amount available 1 year later (low discount rate; delayed gratification preference). Multivariable Poisson regression was used to test the association of high discounting rates with low antihypertensive medication adherence using the validated 4-item Krousel-Wood Medication Adherence Scale (K-Wood-MAS-4 score ≥1). Mediation of the association between high discounting rate and uncontrolled BP (systolic/diastolic BP ≥ 130/80 mm Hg) by low adherence was tested using the counterfactual approach.
Results
Among 235 participants (mean age 63.7 ± 6.7 years; 51.1% women; 41.9% Black), 50.6% had a high 1-year discount rate, 51.9% had low K-Wood-MAS-4 adherence, and 59.6% had uncontrolled BP. High discounting rates were associated with low adherence (adjusted prevalence ratio 1.58, 95% confidence interval (CI) 1.18, 2.12). Forty-three percent (95% CI 40.9%, 45.8%) of the total effect of high discount rate on uncontrolled BP was mediated by low adherence.
Conclusions
Adults with preference for immediate gratification had worse adherence; low adherence partially mediated the association of high discount rate with uncontrolled BP. These results support preference for immediate gratification as an innovative factor underlying low medication adherence and uncontrolled BP.
Keywords: 4-item Krousel-Wood Medication Adherence Scale (K-Wood-MAS-4), blood pressure, hypertension, immediate vs. delayed gratification, medication adherence, temporal discounting, time preferences
For most adults, hypertension is an asymptomatic disease. Taking medications daily to treat uncontrolled blood pressure (BP) (and reduce BP, decrease cardiovascular disease (CVD) risk,1 and prevent decline in quality of life)2 can be associated with medication side effects in some people (e.g., fatigue, sexual dysfunction, frequent urination),3 costs and inconvenience of taking medications, stigma associated with the diagnosis and the treatment,4 and subconscious concern that taking medications daily will increase stress and interfere with other priorities5; all of which can negatively impact quality of life. Understandably, patients may consciously or subconsciously weigh the immediate risk of taking BP medications (e.g., side effects) with delayed benefits (e.g., avoiding a future stroke) when deciding to take antihypertensive medications.6,7
Temporal discounting is the economists’ paradigm for measuring the degree to which people favor immediate over delayed outcomes during decision making, and therefore how they balance between sooner temptation and longer-term gratification.8,9 How people value rewards as a function of time (i.e., how they make intertemporal choice) has proven to be a good predictor of their overall well-being, actual life-time savings, and other outcomes.10–13 Prior research has examined the degree to which intertemporal choices that are present oriented (i.e., immediate gratification) can compromise current health care choices.14 Regarding hypertension, more present-oriented individuals (“high discounting” individuals—preference for immediate gratification) were less likely to check their BP regularly, to alter their diet to help control their hypertension, and to follow their physician’s advice15; however, associations with adherence and clinical outcomes were not assessed. Overall, there is a gap in knowledge as to whether time preference with hypothetical data corresponds to antihypertensive medication adherence and BP control and serves as a potential target for adherence interventions.
Consistent with the National Institutes of Health (NIH) Science of Behavior Change (SOBC) Initiative,16 intervention targets need to be measurable, malleable, and causally linked to behavior.16 Therefore, as a first step, we sought to expand on prior research and evaluate our hypotheses that time preference for immediate gratification (high discount rates) is associated with low medication adherence and uncontrolled BP in community dwelling Black and White women and men with established hypertension, using a temporal discounting paradigm. If the hypotheses are true, the results could lay the groundwork for future intervention studies to test whether tailoring patient–provider messages according to patient time preferences motivates adults with uncontrolled hypertension and low adherence to increase medication adherence behavior.
METHODS
Study design and sample
Community-dwelling adults, aged 55 years and above, were recruited into this cross-sectional study using community outreach to senior centers and senior living institutions, and research registries (Tulane University Clinical Translational Unit’s Volunteer Research Registry) (n = 94); and membership lists of Blue Cross Blue Shield of Louisiana, a statewide commercial insurer (n = 142). Eligibility criteria included a diagnosis of hypertension with current treatment with antihypertensive medication ascertained by self-report and no moderate to severe cognitive impairment (defined as fewer than 3 errors on the brief cognitive 6-item screener).17 Interviewer-administered questionnaires were used, and BP was measured by trained study staff. Only one person was excluded from the analysis due to incomplete self-reported adherence data, resulting in a sample size of n = 235. The study was approved by the Tulane University Institutional Review Board, verbal informed consent was obtained from all participants, and all procedures were conducted in accordance with institutional guidelines.
Key predictor: discounting
We assessed each participant’s underlying temporal discounting factor using a modified version of the Collier and Williams method9 and questions adapted from prior work.18 Each participant was provided a series of 10 questions that asked them to express a preference for $100 today (payoff now) compared to a higher amount in one year (payoff later); future amounts ranged from $105 to $212 (see Supplementary Table 1). Specific dollar amounts were chosen to span a typical range of discount rate as identified in prior work.
The discount rate associated with each choice was calculated as 12 × [e(ln(future payoff) − ln(now payoff))/12 − 1]. One-year discount rate was defined as the average between an implied lower bound (participant prefers payoff now) and the implied upper bound (participant prefers a payoff later). We identified the upper and lower bounds of their implied discount rates associated with the choice where they switched from preferring the payoff now to preferring the later 1-year payoff. For example, if the switch occurred between the choice of “$100 now/$120 in a year” and “$100 now/ $133 in a year,” we inferred that the individual’s discount rate was between 18.4% and 28.9%. Those who preferred the smallest 1-year payoff (i.e., when offered “$100 now/ $105 in a year,” chose “$105 in a year”) were assigned a discount rate between 0% and 4.9%, while those who did not switch to preferring the 1-year payoff even for the highest future payoff offered (i.e., when offered “$100 now/$212 in a year,” chose “$100 now”) were assigned a discount rate between 77.5% and 100%. High discount rate was defined as 1-year discount rate greater than the sample average.
Outcome measures: antihypertensive medication adherence and blood pressure
We assessed antihypertensive medication adherence using the validated open access self-report tool (the 4-item Krousel-Wood Medication Adherence Scale, or K-Wood-MAS-4). The K-Wood-MAS-4 was developed to predict pharmacy refill adherence in a sample of older women and men of Black and White race taking antihypertensive medications:19 using pharmacy refill in the prior year as the reference standard, the 4-item scale had moderate discrimination (C statistic of 0.704, 95% confidence interval (CI) 0.683-0.714); had sensitivity and specificity of 67.4% and 67.8%, respectively; and performed comparably to other published self-report adherence tools. Low K-Wood-MAS-4 adherence (score ≥ 1) is associated with uncontrolled BP (adjusted odds ratio (aOR) = 1.29, 95% CI 1.01, 1.65), incident CVD (adjusted hazard ratio = 2.29, 95% CI 1.61, 3.26),1 and decline in mental health related quality of life (aOR = 1.32; 95% CI 1.08,1.62).2 The tool is comprised of 4 items assessing different factors: forgetfulness, intentionally missing pills when one feels better, medication-taking self-efficacy, and physical health limitations (Supplementary Table 2). One point is assigned for each item response indicating suboptimal medication-taking, low self-efficacy, or physical health limitations. The K-Wood-MAS-4 score is calculated as the sum across items (range 0–4); low adherence is defined as K-Wood-MAS-4 score ≥ 1.
BP was measured by trained study staff using an oscillometric Omron Professional Intellisense Blood Pressure Monitor HEM-907XL. Uncontrolled BP was defined as systolic BP ≥ 130 mm Hg or diastolic BP ≥ 80 mm Hg based on the 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults.20
Covariates
Social Determinants of Health (SDOH), including demographic, clinical, and psychosocial covariates, were defined using published conceptual frameworks describing determinants of antihypertensive medication adherence.21–23 Demographic characteristics included age, sex (male vs. female), race (Black vs. White), marital status (married or cohabitating vs. other), and education (high school education or less vs. greater than high school education). Clinical characteristics included hypertension duration (<10 years vs. ≥10 years), body mass index (BMI; calculated as kg/m2),24 medication burden (<6 medications per day vs. ≥6 medications per day), emergency room (ER) visit or hospitalization in the last 2 years, and cardiometabolic comorbidities (self-reported diabetes, heart failure, myocardial infarction, stroke, or renal failure; dichotomized as 0 vs. ≥1). Depressive symptoms were assessed using the validated 8-item Patient Health Questionnaire depression scale (PHQ-8) and depressive symptoms were defined as PHQ-8 score ≥10.25 Psychosocial characteristics included trust in healthcare provider, beliefs about medications, and medication-taking self-efficacy. Trust in healthcare provider was assessed using the 11-item Trust in Physicians Scale (TPS),26 with “healthcare provider” substituted for “physician” across items. Low trust in healthcare provider was defined as a score in the lowest tertile of the distribution of scaled mean TPS scores. Beliefs about medications were assessed with the Beliefs about Medications Questionnaire (BMQ)-Specific:27 low necessity beliefs and high concerns beliefs about medications were defined as scores in the lowest and highest tertile of the distribution for the necessity and concerns subscales, respectively. Finally, low self-efficacy in managing hypertension was defined as a mean score <9 on a 5-item validated measure of self-efficacy to manage disease.28
Statistical analyses
Pearson’s chi-squared tests and Student’s t-tests were used to test for differences in participant characteristics by high vs. low 1-year discount rate. A separate multivariable Poisson regression model was used to estimate the prevalence ratio (PR) and 95% CI for the association of high 1-year discount rate with low K-Wood-MAS-4 adherence. The initial model was adjusted for demographic factors including age, sex, race, marital status, and education. Subsequent models were also adjusted for (1) hypertension duration, BMI, medication burden, cardiometabolic comorbidities, and depressive symptoms, and (2) trust in healthcare provider, beliefs about medications, and medication-taking self-efficacy.
To explore associations between high discount rates and low medication adherence by demographics, stratified analyses were performed by sex (male vs. female), race (Black vs. White), and age (<65 years vs. ≥65 years). Given the limited sample sizes for sub-groups, we limited the number of control variables included in the models to age, sex, race, marital status, and education (excluding the stratifying variable). Effect modification by age (<65 years vs. ≥65 years), sex, and race was tested by including a high discount rate-by-sex, high discount rate-by-race, or high discount rate-by-age interaction term in the demographics-adjusted model for the overall sample.
Finally, we tested mediation of the association between high discount rate and uncontrolled BP by low K-Wood-MAS-4 adherence using the counterfactual approach29; logistic regression was used for both outcome and mediator models. The natural direct effect, natural indirect effect, and marginal total effect were calculated using Stata’s paramed command and bias-corrected 95% CI were calculated using 500 iteration bootstraps. The percent mediated was calculated from model coefficients; the CI was estimated using a bootstrap resampling procedure with 500 iterations. All analyses were performed using Stata v14.1 (StataCorp, College Station, TX). The figure was created using R 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Participant characteristics
The overall sample of 235 participants was 51.1% female, 41.9% Black, with a mean age of 63.7 years (SD 6.7) (Table 1). Most participants were married (52.1%), had more than a high school education (81.3%), and had a diagnosis of hypertension for at least 10 years (66.2%). The mean BMI was 31.6 kg/m2 (SD 6.3). The average discount rate at 1 year was 0.49 (SD 0.30), with 50.6% classified as having a high 1-year discount rate (i.e., preference for immediate gratification). Low adherers accounted for 51.9% of the sample and 59.6% of participants had uncontrolled BP.
Table 1.
Participant characteristics (n = 235)
| Overall % (n) or Mean (SD) |
1-year discount rate | |||
|---|---|---|---|---|
| Low % (n) or Mean (SD) |
High % (n) or Mean (SD) |
P-value | ||
| Demographic and clinical characteristics | ||||
| Age, mean (SD) | 63.7 (6.7) | 63.8 (6.8) | 63.7 (6.7) | 0.960 |
| Female, % (n) | 51.1 (120) | 49.1 (57) | 52.9 (63) | 0.560 |
| Black race, % (n) | 41.9 (98) | 25.2 (29) | 58.0 (69) | <0.001 |
| Married, % (n) | 52.1 (122) | 61.7 (71) | 42.9 (51) | 0.004 |
| Greater than high school education, % (n) | 81.3 (191) | 87.1 (101) | 75.6 (90) | 0.025 |
| Hypertension diagnosed ≥10 years ago, % (n) | 66.2 (155) | 66.4 (77) | 66.1 (78) | 0.964 |
| Body mass index, mean (SD) | 31.6 (6.3) | 30.2 (5.1) | 33.0 (7.1) | <0.001 |
| ≥6 medications per day, % (n) | 49.4 (116) | 44.0 (51) | 54.6 (65) | 0.102 |
| ER visit or hospitalization, last 2 years, % (n) | 39.2 (92) | 34.5 (40) | 43.7 (52) | 0.148 |
| ≥1 cardiometabolic comorbidity, % (n) | 46.2 (108) | 33.0 (38) | 58.8 (70) | <0.001 |
| Depressive symptoms, % (n) | 10.4 (24) | 10.4 (12) | 10.4 (12) | 1.000 |
| Patient attitudes and beliefs | ||||
| Low trust in healthcare provider, % (n) | 41.7 (95) | 35.1 (40) | 48.3 (55) | 0.044 |
| Low necessity beliefs about medications, % (n) | 37.5 (88) | 39.7 (46) | 35.3 (42) | 0.490 |
| High concerns beliefs about medications, % (n) | 27.2 (64) | 23.3 (27) | 31.1 (37) | 0.178 |
| Low medication-taking self-efficacy, % (n) | 58.4 (135) | 57.0 (65) | 59.8 (70) | 0.665 |
| Medication adherence and blood pressure outcomes | ||||
| Low K-Wood-MAS-4 adherence, % (n) | 51.9 (122) | 38.8 (45) | 64.7 (77) | <0.001 |
| Uncontrolled blood pressure, % (n) | 59.6 (137) | 52.2 (60) | 67.0 (77) | 0.022 |
Abbreviations: ER, emergency room; K-Wood-MAS-4, 4-item Krousel-Wood Medication Adherence Scale; SD, standard deviation.
Participants with high (immediate gratification) vs. low (delayed gratification) 1-year discount rate were more likely to be Black (58.0%, vs. 25.2%, P < 0.001), have 1 or more cardiometabolic comorbidities (58.8% vs. 33.0%, P < 0.001), and have low trust in healthcare providers (48.3% vs. 35.1%, P = 0.044). Those with high vs. low discount rates were also less likely to be married (42.9% vs. 61.7%, P = 0.004), and less likely to have more than a high school education (75.6% vs. 87.1%, P = 0.025). Mean BMI differed for those with high vs. low 1-year discount rate (33.0 kg/m2 (SD 7.1) vs. 30.2 kg/m2 (SD 5.1), P < 0.001). Participants with high vs. low 1-year discount rate were more likely to have low K-Wood-MAS-4 adherence (64.7% vs. 38.8%, P < 0.001) and uncontrolled BP (67.0% vs. 52.2%, P = 0.022).
Association of high discount rate with low medication adherence
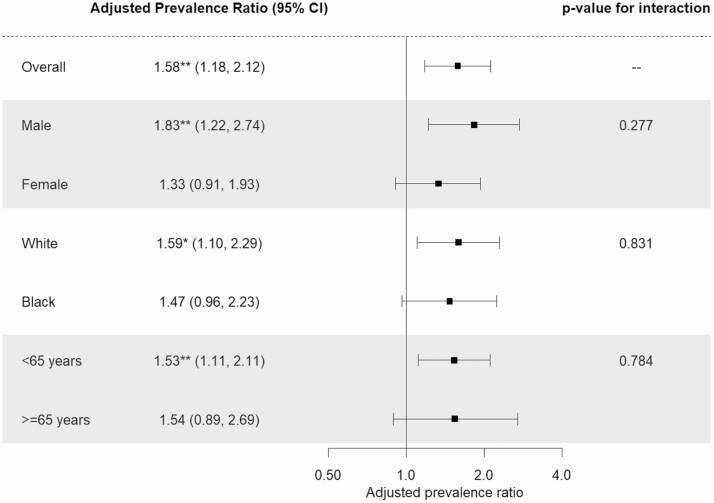
In the fully adjusted model predicting medication adherence, high 1-year discount rate was associated with low K-Wood-MAS-4 adherence (aPR = 1.58, 95% CI 1.18, 2.12, P = 0.002) (Table 2). In demographics-adjusted stratified models, the association between high 1-year discount rate and low K-Wood-MAS-4 adherence was stronger for males (aPR = 1.83, 95% CI 1.22, 2.74, P = 0.003) than females (aPR = 1.33, 95% CI 0.91, 1.93, P = 0.142), though this difference was not statistically significant (P-interaction = 0.277) (Figure 1). The association between high 1-year discount rate and low K-Wood-MAS-4 adherence was for White (aPR = 1.59, 95% CI 1.10, 2.29, P = 0.013) and Black (aPR = 1.47, 95% CI 0.96, 2.23, P = 0.073) participants (P-interaction = 0.831); and for <65 years old (aPR = 1.53, 95% CI 1.11, 2.11, P = 0.009) and ≥65 years old (aPR = 1.54, 95% CI 0.89, 2.69, P = 0.126) participants (P-interaction = 0.784).
Table 2.
Associations between high 1-year discount rate and low medication adherence (n = 235)
| Low K-Wood-MAS-4 adherence (score ≥ 1) | ||||
|---|---|---|---|---|
| Unadjusted PR (95% CI) |
Model 1 PR (95% CI) |
Model 2 PR (95% CI) |
Model 3 PR (95% CI) |
|
| High 1-year discount rate | 1.67*** (1.28, 2.17) |
1.56** (1.18, 2.06) |
1.63*** (1.22, 2.16) |
1.58** (1.18, 2.12) |
| Age | 0.98 (0.96, 1.00) |
0.98 (0.96, 1.00) |
0.98 (0.96, 1.00) |
|
| Female | 0.93 (0.73, 1.19) |
0.88 (0.68, 1.14) |
0.93 (0.72, 1.21) |
|
| Black race | 1.29 (0.99, 1.69) |
1.39* (1.06, 1.82) |
1.36* (1.03, 1.79) |
|
| Married | 1.02 (0.80, 1.30) |
0.99 (0.77, 1.27) |
1.00 (0.78, 1.28) |
|
| Greater than high school education | 1.28 (0.93, 1.75) |
1.40* (1.02, 1.92) |
1.29 (0.95, 1.76) |
|
| Hypertension diagnosed ≥10 years ago | 1.03 (0.78, 1.36) |
0.99 (0.75, 1.31) |
||
| Body mass index | 0.99 (0.97, 1.01) |
0.99 (0.97, 1.01) |
||
| ≥6 medications per day | 1.01 (0.77, 1.33) |
0.96 (0.74, 1.26) |
||
| ≥1 cardiometabolic comorbidity | 0.88 (0.66, 1.17) |
0.94 (0.71, 1.25) |
||
| Depressive symptoms | 1.61** (1.21, 2.14) |
1.45* (1.05, 2.01) |
||
| Low trust in healthcare provider | 1.05 (0.82, 1.34) |
|||
| High concerns beliefs about medications | 1.12 (0.86, 1.45) |
|||
| Low medication-taking self-efficacy | 1.17 (0.89, 1.55) |
Model 1 adjusted for age, sex, race, marital status, and education. Model 2 adjusted for covariates in Model 1 plus hypertension duration, body mass index, medication burden, cardiometabolic comorbidities, and depressive symptoms. Model 3 adjusted for covariates in Model 2 plus trust in healthcare provider, beliefs about medications, and medication-taking self-efficacy. Abbreviations: CI, confidence interval; K-Wood-MAS-4, 4-item Krousel-Wood Medication Adherence Scale; PR, prevalence ratio.
*P < 0.05, **P < 0.01, ***P < 0.001.
Figure 1.
Associations between high 1-year discount rate and low adherence assessed by the 4-item Krousel-Wood Medication Adherence Scale, overall and by sex, race, and age. Models adjusted for age (<65 years vs. ≥65 years), sex, race, marital status, education (minus the stratifying variable). P-value for interaction come from separate fully adjusted models for overall sample. *P < 0.05, **P < 0.01.
Mediation analysis
Using the counterfactual approach to mediation analysis, 43% (95% CI 40.9%, 45.8%) of the total effect of high 1-year discount rate on uncontrolled BP was mediated by low K-Wood-MAS-4 adherence (natural direct effect: aOR = 1.44, 95% CI 0.65, 2.98; natural indirect effect: aOR = 1.32, 95% CI 1.05, 1.70; Table 3).
Table 3.
Mediation of association between high 1-year discount rate and uncontrolled blood pressure by low adherence
| Natural direct effect, aOR (95% CI) | 1.44 (0.65, 2.98) |
| Natural indirect effect, aOR (95% CI) | 1.32 (1.05, 1.70) |
| Marginal total effect, aOR (95% CI) | 1.90 (0.80, 3.97) |
| % of total effect mediated (95% CI) | 43.1% (40.9%, 45.8%) |
Bias-corrected confidence intervals reported for 3 effect estimates. Outcome and mediator models adjusted for age, sex, race, marital status, education, hypertension duration, body mass index, medication burden, cardiometabolic comorbidities, depressive symptoms, trust in healthcare provider, beliefs about medications, and medication-taking self-efficacy. Abbreviations: aOR, adjusted odds ratio; CI, confidence interval.
DISCUSSION
While there are multiple established factors influencing antihypertensive medication adherence behavior,21,22 to our knowledge, the associations between time preference for immediate gratification and low medication adherence (using an open access validated self-report adherence tool) and uncontrolled BP have been understudied. Our recent research has revealed the relatively low proportion of variance in both objective (6.4% for PDC) and subjective (14.8% for K-Wood-MAS-4) adherence explained by traditional risk factors in a sample of older adults; these results provide insight into why current adherence interventions focused on traditional risk factors have not resulted in more than modest improvements in adherence behavior.23 Persistent low adherence rates coupled with the low explanatory power of traditional barriers suggest other factors may be at play, including people’s time preferences. This suggests a gap in our current understanding of how patients weigh risks and benefits of taking BP medications and the need to examine this problem in novel ways.
Compared with adults with low discount rate (preference for delayed gratification) adults with high discount rate (preference for immediate gratification) had low medication adherence. Thus, those who favored the lesser vs. the greater reward when it was available immediately reported, on average, worse adherence. The data also support an indirect effect of high discounting rate on BP control via medication adherence. Our results suggest an alternate approach to understanding medication adherence in adults with hypertension and add to the current knowledge about the associations between time preferences and adherence to antihypertensive medications and BP control. Chapman et al.30 reported that responses to a monetary time preference scenario were not significantly correlated with any adherence measure (i.e., self-report, pill count, or BP) in a sample of 195 older adults with hypertension (mean age 79.2 years, 65.9% women, race not reported). More recently, Sansbury et al.31 reported the first cross-sectional evidence that future time perspective (preference for delayed gratification) and age showed direct effects on increased medication adherence (178 adults—mean age 62.9; 61.2% women; 30.3% Black—with hypertension and diabetes). Of note, the Chapman study included older participants than the Sansbury study. The inconsistent findings may be explained by prior work on how increasing age influences a shorter perceived residual lifespan that shifts people’s focus from prolonging life in the future to enjoying the present.32 This highlights the need for tailoring interventions according to subjective residual lifespan which could be influenced by age and the severity of illness.33 Our study, which includes a sample of adults (mean age 63.7 years), extends the existing knowledge by supporting the potential role for preference for immediate gratification as a key factor underlying low medication adherence, which is itself associated with uncontrolled BP, and for use of behavioral economic models in understanding patients’ health decision making and behaviors. These data align with the expanded conceptual framework that incorporates time preference as an emerging determinant of medication taking behavior.23
Similar to our findings, other studies assessing the effect of time preferences in heart failure,33 diabetes,31,34 and multiple sclerosis35 reported significant associations between time preferences and real-world health behaviors, suggesting a role for time preferences underlying medication adherence behaviors across chronic diseases.
Clinical perspective
With current research findings linking time preferences, temporal discounting and medication adherence decision making and behavior change,31,36 time preference for immediate gratification may serve as modifiable factor underlying poor medication adherence. According to Brown and Segal,7 temporal orientation is something learned, which implies it can be unlearned and thus is modifiable. Because the benefits of treating hypertension are primarily focused on the future, there is a need for interventions and monitoring strategies that assist people focused on immediate gratification to make the connections between taking daily medications now and avoiding future adverse consequences.
When health care providers and professionals encounter patients who are low adherers and have high discount rate (preference for immediate gratification), healthcare recommendations can be tailored to emphasize the immediate benefits from taking medications as prescribed to control hypertension and to build a therapeutic alliance that capitalizes on new intrinsic motivation for medication adherence.31 Furthermore, insurers and employers may employ immediate incentives for improvements in medication adherence—such as lottery payouts to enrollees who regularly fill antihypertensive medications and maintain BP control. If proven effective, successful interventions could empower patients to improve health behaviors and outcomes and reduce the high burden of hypertension and its sequalae.
Limitations and strengths
Limitations
This was a cross-sectional study with a sample of adults (mean age 63.7 years, 52.1% married, 81.3% with greater than high school education, 51.1% women, and 41.9% Black) from one region of the United States and generalizability is limited; causal inferences cannot be made. The study was not powered to fully explore subgroup differences; however, the information is helpful in describing patterns by age, race, and sex for the association between time preferences and adherence behavior, in planning future studies and in conducting systematic reviews and meta-analyses. Future work in larger, more diverse samples would allow for additional insight. An indirect, self-report adherence measure was used and cannot verify actual medication taking; however, low K-Wood-MAS-4 adherence is associated with pharmacy refill, uncontrolled BP, incident CVD events, and decline in mental quality of life.1,2 While we included education level as a surrogate for socioeconomic status (SES), we were unable to fully explore the confounding effect of SES on the association between high discounting rate and low antihypertensive medication adherence. Although there is a potential limitation of social desirability bias in participant responses to the discounting questions, it is unlikely to be a significant factor in this analysis given the pattern of participant responses yielding a low number with very low discount rates and the prior research validating the method. Finally, while analyses adjusted for many key SDOH influencing antihypertensive medication adherence,21,37–40 future work should also consider other factors such as medication regimen complexity,23,31 perception of susceptibility to complications,31 implicit attitudes toward medications,23,41 and socioeconomic status.
Strengths
This study contributes to existing evidence regarding an understudied link between time preferences in medication-taking decisions and medication adherence behavior and clinical outcomes in a sample of community-dwelling older adults (51.1% women) with treated hypertension, and an objective measure of BP control assessed by trained study staff. Our study included a high proportion of Blacks (41.9%), a population with reported high rates of low adherence to antihypertensive medications and uncontrolled BP and bearing a significant burden of hypertension and its sequelae. Our findings are consistent with Brown and Segal7 who reported that Blacks as compared to Whites were more present-oriented (immediate gratification) regarding their daily experiences with managing hypertension. Given the opportunities to improve health and medical care provided to racially and ethnically diverse populations and address the adverse impact of comorbid hypertension on the disproportionate burden of COVID-19 in vulnerable groups,42 there is an urgent need to identify and address novel mechanisms underlying poor adherence behavior across racial groups. These findings suggest time preference as a potential target for adherence research among minority populations aimed at improving medication-taking behavior.
Preference for immediate gratification was directly associated with worse medication adherence and indirectly associated with uncontrolled BP in adults with established hypertension. These results signal the potential for time preferences as a novel target for improving medication-taking behavior and blood pressure control.
Supplementary Material
ACKNOWLEDGMENTS
This work was funded by a U54 GM104940 pilot award (Krousel-Wood -PI) from the Louisiana Clinical and Translational Science (LA CaTS) Center and the National Institutes of Health (NIH)/National Institute of General Medical Sciences (NIGMS). The authors receive NIH funding from R01 HL133790 (Krousel-Wood—Multi-PI; Peacock—Study Manager), K12 HD043451 (Krousel-Wood—PI; Peacock and Craig—Data Analysts), R01 HL130500 (Krousel-Wood—Site PI and Co-Investigator), UL1 TR001417 (Krousel-Wood—TL1 Co-Director), P20 GM109036 (Krousel-Wood—Co-Investigator), and 1R01DA047365-01A1 (Bradford). Study conclusions are those of the authors and do not necessarily represent the official position of LA CaTS, NIH, or NIGMS. We extend our thanks to our students and colleagues, including Kayla Hudson, Taylor Johnson, James Marsh, Alexandra McNally, and Julia Silver, as well as our study participants, without whom this work would not have been possible. The data underlying this article will be shared on reasonable request to the corresponding author.
DISCLOSURE
The authors declared no conflict of interest. This work, in part, was presented as a poster at the 2020 virtual Academy Health Annual Meeting.
REFERENCES
- 1. Krousel-Wood M, Peacock E, Joyce C, Li S, Frohlich E, Re R, Mills K, Chen J, Stefanescu A, Whelton P, Tajeu G, Kronish I, Muntner P. A hybrid 4-item Krousel-Wood Medication Adherence Scale predicts cardiovascular events in older hypertensive adults. J Hypertens 2019; 37:851–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Peacock E, Joyce C, Craig LS, Lenane Z, Holt EW, Muntner P, Krousel-Wood M. Low medication adherence is associated with decline in health-related quality of life: results of a longitudinal analysis among older women and men with hypertension. J Hypertens 2021; 39:153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Grégoire JP, Moisan J, Guibert R, Ciampi A, Milot A, Côté I, Gaudet M. Tolerability of antihypertensive drugs in a community-based setting. Clin Ther 2001; 23:715–726. [DOI] [PubMed] [Google Scholar]
- 4. Johnson HM, Warner RC, LaMantia JN, Bowers BJ. “I have to live like I’m old.” Young adults’ perspectives on managing hypertension: a multi-center qualitative study. BMC Fam Pract 2016; 17:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Krousel-Wood M, Kegan R, Whelton PK, Lahey LL. Immunity-to-change: are hidden motives underlying patient nonadherence to chronic disease medications? Am J Med Sci 2014; 348:121–128. [DOI] [PubMed] [Google Scholar]
- 6. Christensen-Szalanski JJ, Northcraft GB. Patient compliance behavior: the effects of time on patients’ values of treatment regimens. Soc Sci Med 1985; 21:263–273. [DOI] [PubMed] [Google Scholar]
- 7. Brown CM, Segal R. Ethnic differences in temporal orientation and its implications for hypertension management. J Health Soc Behav 1996; 37:350–361. [PubMed] [Google Scholar]
- 8. Ainslie G. Specious reward: a behavioral theory of impulsiveness and impulse control. Psychol Bull 1975; 82:463–496. [DOI] [PubMed] [Google Scholar]
- 9. Coller M, Williams MB. Eliciting individual discount rates. Exper Econ 1999;2:107–127. [Google Scholar]
- 10. Bradford D, Courtemanche C, Heutel G, McAlvanah P, Ruhm C. Time preferences and consumer behavior. J Risk Uncertainty 2017;55:119–145. [Google Scholar]
- 11. Luhmann CC. Temporal decision-making: insights from cognitive neuroscience. Front Behav Neurosci 2009; 3:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sellitto M, Ciaramelli E, di Pellegrino G. The neurobiology of intertemporal choice: insight from imaging and lesion studies. Rev Neurosci 2011; 22:565–574. [DOI] [PubMed] [Google Scholar]
- 13. Shamosh NA, Gray JR. Delay discounting and intelligence: a meta-analysis. Intell 2008;36:289–305. [Google Scholar]
- 14. Bradford WD. The association between individual time preferences and health maintenance habits. Med Decis Making 2010;30:99–112. [DOI] [PubMed] [Google Scholar]
- 15. Axon RN, Bradford WD, Egan BM. The role of individual time preferences in health behaviors among hypertensive adults: a pilot study. J Am Soc Hypertens 2009; 3:35–41. [DOI] [PubMed] [Google Scholar]
- 16. Nielsen L, Riddle M, King JW, Aklin WM, Chen W, Clark D, Collier E, Czajkowski S, Esposito L, Ferrer R, Green P, Hunter C, Kehl K, King R, Onken L, Simmons JM, Stoeckel L, Stoney C, Tully L, Weber W; NIH Science of Behavior Change Implementation Team . The NIH Science of Behavior Change Program: transforming the science through a focus on mechanisms of change. Behav Res Ther 2018; 101:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002; 40:771–781. [DOI] [PubMed] [Google Scholar]
- 18. Bradford WD, Dolan P, Galizzi MM. Looking ahead: Subjective time perception and individual discounting. J Risk Uncertainty 2019;58:43–69. [Google Scholar]
- 19. Krousel-Wood M, Joyce C, Holt EW, Levitan EB, Dornelles A, Webber LS, Muntner P. Development and evaluation of a self-report tool to predict low pharmacy refill adherence in elderly patients with uncontrolled hypertension. Pharmacotherapy 2013; 33:798–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018; 138:e484–e594. [DOI] [PubMed] [Google Scholar]
- 21. Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol 2004; 19:357–362. [DOI] [PubMed] [Google Scholar]
- 22. Krousel-Wood M, Joyce C, Holt E, Muntner P, Webber LS, Morisky DE, Frohlich ED, Re RN. Predictors of decline in medication adherence: results from the cohort study of medication adherence among older adults. Hypertension 2011; 58:804–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Krousel-Wood M, Craig LS, Peacock E, Zlotnick E, O’Connell S, Bradford D, Shi L, Petty R. Medication adherence: expanding the conceptual framework. Am J Hypertens 2021; 34:895–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weir CB, Jan A.. BMI Classification Percentile and Cut off Points. StatPearls Publishing LLC,Treasure Island, FL, 2019. [PubMed] [Google Scholar]
- 25. Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009; 114:163–173. [DOI] [PubMed] [Google Scholar]
- 26. Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med Care 1999; 37:510–517. [DOI] [PubMed] [Google Scholar]
- 27. Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 1999; 47:555–567. [DOI] [PubMed] [Google Scholar]
- 28. Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health 2012; 37:15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods 2013; 18:137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chapman GB, Brewer NT, Coups EJ, Brownlee S, Leventhal H, Leventhal EA. Value for the future and preventive health behavior. J Exp Psychol Appl 2001; 7:235–250. [PubMed] [Google Scholar]
- 31. Sansbury B, Dasgupta A, Guthrie L, Ward M. Time perspective and medication adherence among individuals with hypertension or diabetes mellitus. Patient Educ Couns 2014; 95:104–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Charles ST, Carstensen LL. Social and emotional aging. Annu Rev Psychol 2010; 61:383–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chew HSJ, Sim KLD, Choi KC, Chair SY. Relationship between self-care adherence, time perspective, readiness to change and executive function in patients with heart failure. J Behav Med 2020; 43:1–11. [DOI] [PubMed] [Google Scholar]
- 34. Reach G, Boubaya M, Brami Y, Lévy V. Disruption in time projection and non-adherence to long-term therapies. Patient Prefer Adherence 2018; 12:2363–2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bruce JM, Bruce AS, Lynch S, Thelen J, Lim SL, Smith J, Catley D, Reed DD, Jarmolowicz DP. Probability discounting of treatment decisions in multiple sclerosis: associations with disease knowledge, neuropsychiatric status, and adherence. Psychopharmacology (Berl) 2018; 235:3303–3313. [DOI] [PubMed] [Google Scholar]
- 36. Zhao X, Villagran MM, Kreps GL, McHorney C. Gain versus loss framing in adherence-promoting communication targeting patients with chronic diseases: the moderating effect of individual time perspective. Health Commun 2012; 27:75–85. [DOI] [PubMed] [Google Scholar]
- 37. Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res 2013; 11:54–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Williams LG, Peacock E, Joyce C, Bazzano LA, Sarpong D, Whelton PK, Holt EW, Re R, Frohlich E, He J, Muntner P, Krousel-Wood M. Risk Factors for low pharmacy refill adherence among older hypertensive men and women by race. Am J Med Sci 2018; 356:464–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tajeu GS, Kent ST, Kronish IM, Huang L, Krousel-Wood M, Bress AP, Shimbo D, Muntner P. Trends in Antihypertensive medication discontinuation and low adherence among Medicare Beneficiaries initiating treatment from 2007 to 2012. Hypertension 2016; 68:565–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bailey JE, Hajjar M, Shoib B, Tang J, Ray MM, Wan JY. Risk factors associated with antihypertensive medication nonadherence in a statewide Medicaid population. Am J Med Sci 2014; 348:410–415. [DOI] [PubMed] [Google Scholar]
- 41. Craig LS, Peacock E, Mohundro BL, Silver JH, Marsh J, Johnson TC, Kelly PA, Bazzano LA, Cunningham M, Petty RE, Krousel-Wood M. Implicit and explicit attitudes toward antihypertensive medications explain variation in pharmacy refill and self-reported adherence beyond traditional risk factors: potential novel mechanism underlying adherence. J Am Heart Assoc 2021; 10:e018986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ferdinand K, Batieste T, Fleurestil M. Contemporary and future concepts on hypertension in African Americans: COVID-19 and beyond. J Natl Med Assoc 2020; 112:315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.