Abstract
Hypertension is an established risk factor for cardiovascular disease. Although controlling blood pressure reduces cardiovascular and stroke mortality and target organ damage, poor blood pressure control remains a clinical and public health challenge. Furthermore, racial and ethnic disparities in the outcomes of hypertension are well documented. In October of 2020, the U.S. Department of Health and Human Services published The Surgeon General’s Call to Action to Control Hypertension. The Call to Action emphasized, among other priorities, the need to eliminate disparities in the treatment and control of high blood pressure and to address social determinants as root causes of inequities in blood pressure control and treatment. In support of the goals set in the Call to Action, this review summarizes contemporary research on racial, ethnic, and socioeconomic disparities in hypertension and blood pressure control; describes interventions and policies that have improved blood pressure control in minoritized populations by addressing the social determinants of health; and proposes next steps for achieving equity in hypertension and blood pressure control.
Keywords: blood pressure, health disparity, health equity, hypertension, race, social determinants
Globally, hypertension is the leading risk factor for morbidity and mortality, with over 10 million deaths and 218 million disability-adjusted life years being attributable to high systolic blood pressure (SBP) in 2017 alone.1 In an analysis of electronic health record data from 1.25 million adults, total cardiovascular disease risk increased by 26% and 23% for every 20 mm Hg of SBP and 10 mm Hg of diastolic BP (DBP), respectively, and risk increased with increasing BP for individual cardiovascular diseases such as myocardial infarction, stroke, and heart failure.2
In October of 2020, the U.S. Department of Health and Human Services published The Surgeon General’s Call to Action to Control Hypertension.3 This report discussed the economic and health consequences of uncontrolled hypertension, set goals for improving rates of BP control; highlighted examples of successful interventions; and challenged Americans across different sectors to make BP control a priority. The impetus for the Call to Action was recent evidence of suboptimal BP control rates among US adults with hypertension, in whom the proportion with controlled BP declined from 53.8% in 2013–2014 to 43.7% in 2017–2018.4 During that same period, the proportion with controlled BP declined from 72.2% to 64.8% among US adults taking antihypertensive medication.4
In the United States, hypertension disproportionately affects minoritized racial and ethnic groups, particularly those that are socially and economically disadvantaged.5–8 Over time, cardiovascular risk factors and cardiovascular health outcomes have improved more slowly, or even worsened, among lower income and minoritized racial and ethnic populations compared with their higher income and White counterparts.9–11 The contributions of social and economic factors to health and wellbeing are well known.12 The ongoing Coronavirus Disease 2019 (COVID-19) pandemic has underscored the importance of these social factors on health outcomes such that Black, Indigenous People of Color (BIPOC), and communities of lower socioeconomic positions (SEPs) suffer higher risks of COVID-19 infection and mortality.13,14 Barriers such as living and working in environments that promote transmission of the virus have contributed to disparities in COVID-19.15,16 These social and economic factors along with lived environment are associated with disproportionately higher burden of chronic disease in BIPOC and are considered “root causes” of health inequalities.17,18
The Surgeon General’s Call to Action commits to eliminating differences in hypertension that are attributable to social conditions, with the ultimate goal of achieving health equity. In support of the Call to Action, this review article defines terms related to health equity, summarizes contemporary literature on disparities in hypertension and BP control with respect to race and ethnicity and the social determinants of health (SDoH); and discusses interventions that target the social determinants of BP control.
DEFINITION OF HEALTH EQUITY, HEALTH DISPARITIES, AND THE SDOH
Health equity has been defined as “the state in which everyone has the opportunity to attain full health potential and no one is disadvantaged from achieving this potential because of social position or any other socially defined circumstance.” 19 Linked with health equity is the term “health disparity,” which has been defined as “differences that exist among specific population groups in the United States in the attainment of full health potential.” 19 The SDoH is defined as “the conditions in which people live, learn, work, play, worship, and age.” 20 A useful framework for understanding the SDoH has been developed by the National Institute on Minority Health and Health Disparities (NIMHD).21 In this framework, the SDoH occur at multiple levels (e.g., individual or community) and across multiple domains (e.g., sociocultural environment or healthcare system). For example, at the individual level, a healthcare system determinant of health would be insurance coverage, while at the community level, a healthcare system determinant would be the availability of health services in a neighborhood.21
Though distinct concepts, health equity, health disparity, and the SDoH are interrelated. A 2017 report by the National Academies of Sciences, Engineering, and Medicine (NASEM) identified SDoH as fundamental causes of health disparities and inequities.19 Likewise, structural racism has been recognized by the American Heart Association as a fundamental driver of racial disparities and inequities in health overall and cardiovascular health in particular.22 In the following sections, we identify health disparities in hypertension and BP control experienced by race and ethnic groups and by different domains of the SDoH (SEP and neighborhood factors).
RACIAL AND ETHNIC DISPARITIES IN HYPERTENSION AND BLOOD PRESSURE CONTROL
Racial and ethnic differences in hypertension and blood pressure control
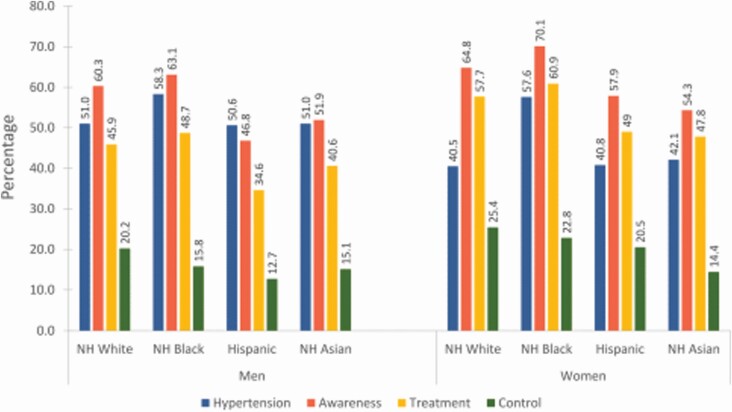
The prevalence of hypertension, hypertension awareness, hypertension treatment, and BP control by racial and ethnic group and sex is presented in Figure 1. Data for these estimates were obtained from the National Health and Nutrition Examination Surveys (NHANES) cycles 2015–2018. The prevalence of hypertension was higher and the prevalence of BP control was lower in non-Hispanic Black men and women compared with non-Hispanic White men and women.23 The prevalence of both hypertension awareness and treatment was higher when comparing non-Hispanic Black men and women to non-Hispanic White men and women.23 Furthermore, non-Hispanic Black adults also have a higher incidence of hypertension over the life course than do non-Hispanic White adults.24 The prevalence of hypertension was similar when comparing Hispanic men and women to non-Hispanic White men and women.23 Hypertension awareness, hypertension treatment, and BP control were less common in Hispanic men and women with hypertension than in non-Hispanic White men and women with hypertension.23 There is evidence that the risk for hypertension is higher in Hispanic adults compared with non-Hispanic White adults.25 The prevalence of hypertension was also similar when comparing non-Hispanic Asian men and women to non-Hispanic White men and women. Hypertension awareness, treatment, and control were all less common in non-Hispanic Asian men and women than in non-Hispanic White men and women.23
Figure 1.
Prevalence of hypertension, hypertension awareness, hypertension treatment, and blood pressure control among US adults ≥20 years of age by racial and ethnic group, 2015–2018.23 Abbreviation: NH, non-Hispanic. Hypertension was defined by a systolic blood pressure ≥130 mm Hg, or a diastolic blood pressure ≥80 mm Hg, or self-reported antihypertensive medication use, or being told on ≥2 occasions by a healthcare provider that one has hypertension. The prevalence of hypertension was calculated for US adults ≥20 years of age. Hypertension awareness was defined as ever being told by a healthcare provider that one has hypertension or high blood pressure. Hypertension treatment was defined by self-reported use of antihypertensive medication. Blood pressure control was defined by a systolic blood pressure <130 mm Hg and a diastolic blood pressure <80 mm Hg. The prevalence of hypertension awareness, hypertension treatment, and blood pressure control were calculated among US adults ≥20 years of age who had hypertension. All estimates were calculated using National Health and Nutrition Examination Survey data.
Factors driving race and ethnic disparities in hypertension and blood pressure control
The primary drivers of Black–White disparities in hypertension and BP control are more likely tied to behavioral and social factors and access to care than to biology.26 A study of Black participants in the Systolic Blood Pressure Reduction Intervention Trial (SPRINT) examined the association of West African genetic ancestry with BP trajectory over 3 years and found no evidence of a difference in BP trajectory across tertiles of West African genetic ancestry.27 Furthermore, in studies utilizing data from NHANES28 and the National Health Interview Survey (NHIS),29 the prevalence of hypertension was higher among US-born non-Hispanic Black adults compared with foreign-born non-Hispanic Black adults. Research examining ethnic differences in hypertension and cardiovascular health within non-Hispanic Black adults and the apparent health advantage among foreign-born Black persons such as African immigrants and Afro-Caribbeans is warranted.30
Differences in behavioral factors such as diet, weight, and medication adherence and SDoH such as education, income, and neighborhood resources contribute to Black–White disparities in hypertension.31–34 That the prevalence of hypertension awareness and treatment is higher in non-Hispanic Black vs. White adults23 suggests that disparities in BP control emerge once antihypertensive medications are initiated. Evidence is inconclusive as to whether treatment inertia occurs more-or-less in non-Hispanic Black compared with non-Hispanic White patients with hypertension.35–38 Differences in medication adherence between non-Hispanic Black and White adults have been more consistently identified, with non-Hispanic Black adults having lower antihypertensive medication adherence.39 Racial discrimination may also contribute to Black–White disparities in hypertension.40,41 In an analysis of data from participants in the Jackson Heart Study, a cohort of Black adults in the Jackson, MS metropolitan area, high and medium vs. low levels of self-reported lifetime discrimination were associated with a 34% and 49% increased risk of developing hypertension, respectively.40 Likewise, among Black participants in the Multi-Ethnic Study of Atherosclerosis (MESA), reporting any lifetime discrimination was associated with an increased risk of developing hypertension over follow-up.41
Hispanic adults in the United States have a higher burden of adverse SDoH than do non-Hispanic White adults. Hispanic adults have lower household incomes and are more likely to live in poverty than non-Hispanic White adults.42 Hispanic adults are also less likely to have health insurance and have lower healthcare utilization compared with non-Hispanic White adults.43 Despite being more likely to have adverse SDoH, the prevalence of hypertension is similar among Hispanic adults and non-Hispanic White adults.23 This apparent “paradox” may stem from healthier lifestyles and behaviors among recent Hispanic immigrants.44 Hypertension awareness, treatment, and control were lower in Hispanic adults compared with non-Hispanic White adults23 Lower access to and utilization of healthcare by Hispanic adults may explain these disparities.45,46 In an analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), Hispanic patients were less likely than non-Hispanic patients to have controlled hypertension at baseline. After the start of the trial, during which patients had similar access to healthcare, Hispanic adults were more likely to attain BP control.45 However, it is difficult to draw conclusions regarding the effects of SDoH on the burden of hypertension and BP control among Hispanic adults because of the paucity of disaggregated data on Hispanic adults of different ethnic origins. Studies comparing Hispanic ethnic groups suggest heterogeneity in the prevalence of hypertension and BP control.47 Research that investigates the SDoH and BP control within specific Hispanic ethnic groups is needed.
Aggregated data examining the SDoH among Asian Americans suggests that they are under-represented among poor households and have a low rate of being uninsured.42,48 However, when subgroups are considered, there is great heterogeneity in SEP49 and hypertension50 among Asian Americans. Intrarace differences in SEP may contribute to the hypertension discrepancies between Asian ethnic groups.51–54 As with Hispanic adults, more recent Asian immigrants and those less assimilated into US culture have a lower prevalence of hypertension.55 Cultural perception of hypertension and medication side effects may partially explain the lower hypertension–BP control rate among Asian American vs. non-Hispanic White adults because antihypertensive medication adherence is less optimal in Asian adults.56,57 More studies are needed to identify social determinants of hypertension and BP control in Asian Americans of different ethnic groups.
RELATIONSHIP BETWEEN DOMAINS OF THE SDOH, HYPERTENSION, AND BLOOD PRESSURE CONTROL
Socioeconomic position
Socioeconomic position refers to the social and economic position of an individual or group within a society’s class structure.58 There are a number of markers of SEP, but the 2 commonly utilized in public health research are income and education. These markers are present at the level of the individual or family (e.g., annual family income) and at the level of communities (e.g., neighborhood poverty).58 Below we review contemporary evidence on the association of SEP, hypertension, and BP control.
Income may affect health by limiting access to health insurance, which, in turn, affects patients’ access to medical care.59,60 Low-income earning is also associated with poor health behaviors.61 Results from US studies that have examined the association of income with hypertension and BP control are mixed. Commodore-Mensah et al. found that, after multivariable adjustment for demographic characteristics, clinical risk factors, and SDoH, there was no association between family income–poverty ratio and BP control among adults in NHANES.6 However, NHANES participants with family income ≥400% federal poverty thresholds were more likely to have ideal BP levels as defined by the AHA Life’s Simple 7 criterion.62 This association was present after adjustment for demographic characteristics and SDoH. Community-level measures of economic resources have been associated with hypertension and BP control. In an analysis of data collected by Kaiser Permanente Northern California, Pantell et al. observed an association between residing in an area with concentrated neighborhood poverty and incident hypertension (hazard ratio: 1.26; 95% confidence interval [CI]: 1.00–1.59).63 Additionally, a study using ALLHAT data found lower odds of BP control (odds ratio: 0.48; 95% CI: 0.37–0.63) among participants who attended study sites that were located in counties with the lowest compared with highest quintile of county-level median income.5
Education may affect health through income, but also contributes to health through higher health-related knowledge and literacy.64 Prior research suggests an association between educational attainment and hypertension. US women with some college (prevalence ratio [PR]: 1.15; 95% CI: 1.06–1.25) or a high school level (PR: 1.17; 95% CI: 1.09–1.26) of education were more likely to have hypertension than women with a college degree.6 In addition, education was associated with incident hypertension among older adults (mean age of 61 years) in the Atherosclerosis Risk in Communities study (ARIC).65 The hazard ratios (95% CI) for hypertension comparing college and high school graduates to participants with less than high school education were 0.71 (0.59–0.86) and 0.82 (0.67–0.99), respectively.65 In the REasons for Geographic and Racial Differences in Stroke (REGARDS) study, education was associated with an increased risk for incident hypertension among Black and White men and women over a median of 9.4 years of follow-up.34 Contemporary studies of US populations have not observed associations between educational attainment and BP control among adults with hypertension.6
Neighborhood factors
The physical and social environments in which individuals’ reside may affect health directly in the case of environmental exposures or indirectly through promoting health behaviors.66 There is evidence that neighborhood characteristics are associated with incident hypertension and BP control. In the Dallas Heart Study, living in a neighborhood with a high vs. low level of neighborhood deprivation was associated with incident hypertension (odds ratio: 1.69; 95% CI: 1.02–2.82).67 Among participants in the University of Alabama at Birmingham Study of Aging, the odds of BP control comparing participants living in neighborhoods with the highest vs. lowest levels of disadvantage was 0.60 (95% CI: 0.40–0.60).68 Residential racial segregation has also been identified as a factor relevant to hypertension. An analysis of data from Black Coronary Artery Risk Development in Young Adults (CARDIA) study participants found that increasing levels of neighborhood segregation were associated with increases in SBP.69 Furthermore, over a period of 25 years, SBP was reduced in participants who moved from neighborhoods categorized as highly segregated to those categorized as medium and low segregation.69 Among Hispanic adults with hypertension, living in neighborhoods with higher concentrations of Hispanics and immigrants was associated with lower odds of taking antihypertensive medication and seeing a physician for hypertension in the past 12 months.70
INTERVENTIONS TARGETING THE SDOH OF HYPERTENSION
The SDoH are multilevel and occur across multiple domains.21 As such, there is no one intervention that could address every determinant. Many interventions that target different domains and levels will be required to achieve health equity. With varying success, contemporary interventions have sought to address the different social determinants of hypertension and BP control.
In the Five Plus Nuts and Beans Randomized Trial, Black adults with hypertension and a SBP ≤160 mm Hg and a DBP ≤100 mm Hg who received care at a community-based health center were randomized to either receive personalized Dietary Approaches to Stop Hypertension (DASH) diet coaching, $30 a week to spend on preselected high-potassium foods, and free food delivery from a local supermarket to a local library in close proximity to the health center or to a control group that received printed materials on BP control and the DASH diet and $240 total to spend on food at the same supermarket as the intervention group.71 Notably, this intervention addressed multiple SDoH by providing participants with health education and nutritional coaching, reducing the financial burden to make healthier diet choices, and providing the healthier foods in a convenient location to participants. After 8 weeks of follow-up, the intervention group reported increased fruit and vegetable consumption and had an increase in urinary excretion of potassium; however, their BP change was not statistically significant. Though this study had null findings for BP change, the improvements to the intervention group’s diet were notable. Over the 8-week follow-up, the intervention group increased their fruit and vegetable consumption by 2.3 servings/day. Daily potassium consumption in the intervention group increased by nearly 1 g/day.71
The Los Angeles Barbershop Blood Pressure Study (LABBPS) randomized Black-owned barbershops to intervention and control arms. Black men ages 35–79 years who were regular patrons of the randomized shops participated in the study. Barbers at intervention shops were trained to measure BP and encourage participants to follow-up with a study pharmacist who were trained hypertension clinicians and measured participants’ BP, prescribed antihypertensive medications through a collaborative practice agreement, and encouraged lifestyle changes. Participants in the intervention group also received $25 at each pharmacist visit to cover the cost of prescribed generic drugs and transportation to the pharmacies to obtain their medications. Barbers at control shops provided participants with information on BP and encouraged follow-up with a healthcare provider. This intervention also targeted multiple SDoH. Among Black men, medical mistrust is a barrier to receiving routine healthcare, including blood pressure screening.72 Situating the LABBPS in barbershops not only made participation convenient for the men but may have also enhanced their trust in the care they were receiving as Black-owned barbershops are an important cultural institution for Black men.73 Additionally, the money provided for pharmacy visits reduced the cost barrier to medication taking and adherence.74 Results of this trial were impressive. The mean SBP in the intervention group and the control group fell by 27 and 9.3 mm Hg, respectively, after 6 months of follow-up.75 Results from follow-up studies suggest that reductions in SBP were sustained at 12 months76 and that the intervention was cost-effective.77
During the COVID-19 pandemic, community health workers (CHWs) were identified as critical agents in our nation’s public health infrastructure,78 but their efforts have long been shown to improve BP control and health behaviors in adults with hypertension.79–81 The services provided by CHWs are flexible,82 allowing them to address the diverse barriers to BP control among disadvantaged populations. Project AsPIRE (Asian American Partnership in Research and Empowerment) is one example of an effective intervention that utilized CHWs. This study randomized Filipino adults with hypertension to either attend 1 cardiovascular-related health education session led by Filipino CHWs and to receive a referral to primary care providers if needed (control group) or to attend 4 monthly cardiovascular-related health education sessions led by the CHWs (treatment group).81 The sessions were adapted to be culturally relevant to Filipino adults. The CHWs also met with treatment group participants in-person and by phone between sessions, helped them to set health goals, coordinated primary care visits and referrals, and provided social support. At the trial’s conclusion, treatment group participants had greater reductions in BP and higher odds of BP control than did control group participants.81
Interventions situated in places of faith have also proven effective at improving BP control and hypertension-related health behaviors.83,84 In the Racial and Ethnic Approaches to Community Health For Asian Americans Keep on Track (REACH FAR KOT) program, volunteers visited faith-based organizations, measured congregants’ BP, provided congregants with culturally adapted health counseling, and recommended patients see or referred patients to a primary care provider if they had high BP.84 Subsequent BP screenings at the faith-based organizations were conducted in intervals decided by each individual organization. After 6 months of follow-up, SBP was reduced by 3.9 mm Hg and DBP was reduced by 2.4 mm Hg among congregants with self-reported hypertension at baseline. Congregants with an SBP ≥160 mm Hg or a DBP ≥100 mm Hg at baseline had declines of 16.7 mm Hg for SBP and 8.3 mm Hg for DBP.84
Community-based interventions that target SDoH and link communities with healthcare services can improve health behaviors and BP. However, the broader social and policy environments in which individuals and communities are located may limit the population health impact of individual and community-level interventions, especially those targeting health behaviors.85 This is because individual behaviors and access to care are influenced by external factors such as the availability of resources needed to engage in health behaviors.86 Changes to health policy are also needed to close disparities in BP control. An example of a policy change for which there is evidence of benefits to BP control was the expansion of Medicaid under the Affordable Care Act (ACA). Angier et al. used electronic health record data to conduct a study that examined changes in BP control among newly insured, discontinuously insured, continuously uninsured, and continuously insured patients in the period before and the period after the ACA.87 Data came from 5 states that expanded Medicaid eligibility (California, Ohio, Oregon, Washington, and Wisconsin). This study found that BP control increased among all insurance groups but increased the most (8.6%) in patients who gained insurance after the Medicaid expansion. Moreover, when participants in the insurance groups were further stratified by level of social deprivation in the census tract of their residence, newly insured patients living in highly deprived areas had the greatest increase in BP control, with a 16% increase from the period before to after the Medicaid expansion.87 In a recent analysis evaluating the impact of Medicaid expansion on insurance rates and chronic disease outcomes in 946 federally qualified health centers, the federally qualified health centers in Medicaid expansion states observed a 9.24 percentage point (PP) decline in uninsurance rates and a comparative improvement in BP control (3.38-PP [95% CI: 0.80–5.96]) by year 5 among Black populations.88 Taken together, these studies suggest that Medicaid expansion was a viable approach to enhance healthcare access and improve BP control.
CONCLUSIONS AND FUTURE DIRECTIONS
Achieving health equity in hypertension and BP control is possible, but to do so will require commitment, innovation, and bold action. The scientific community and healthcare organizations have expressed their commitment to reducing health inequities, even acknowledging sociopolitical issues such as structural racism.22,89–91 The next step is to turn those commitments into action. Public health research in general and hypertension research in particular must consider the SDoH at levels including and above the individual. To date, structural and institutional determinants have largely been excluded from public health research.92 Research that disaggregates racial and ethnic groups and identifies specific disparities in health and specific solutions is needed. Technologies such as telehealth visits, home BP monitoring, and electronic health records should be leveraged on a wider scale to address the lack of routine access to care, with primary care investment playing a key role in achieving equity and BP management.93 Furthermore, widespread dissemination of community-based prevention programs like the Los Angeles Barbershop Blood Pressure program will require innovative healthcare financing and value-based payment model that prioritizes health equity.94
Lastly, and arguably most importantly, changes to policy will be required. The improvements to BP control among adults who gained health insurance under the ACA shows that policies that address healthcare access may reduce health disparities. Future policy strategies should target not only barriers to BP control but also risk factors for the development of hypertension. Payment reforms such as value-based care which rewards health systems for addressing disparities in BP control and reimburses interventions by CHWs and community pharmacists may advance health equity. Efforts such as population-wide reductions in sodium consumption, increases availability and affordability of heart-healthy foods, and the creation of accessible opportunities for engagement in physical activity should be prioritized.95,96 Future actions must not only target communities that experience disparities in hypertension and BP control but do so in a way that is conscious of how the SDoH contribute to disparities. These interventions and policies should be driven by the needs and desires of affected communities. The burden of overcoming historical and contemporary structural barriers should not be borne by the affected communities alone. Health equity in hypertension and BP control will only be achieved by all of us working together and disrupting age-old paradigms to focus on whole-person care.
Funding
“Drs. Commodore-Mensah and Ogedegbe report funding from the American Heart Association Health Equity Research Network (HERN) Project: Prevention of Hypertension (Grant Numbers: 882415 and 878088, respectively). Dr. Ogedegbe also reports funding from the National Heart, Lung, and Blood Institute (NHLBI) Grant 5UG3HL151310-02. The views expressed in this work are those of the authors and do not necessarily represent the official position of the funding organizations.
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392:1923–1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, White IR, Caulfield MJ, Deanfield JE, Smeeth L, Williams B, Hingorani A, Hemingway H. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014; 383:1899–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Control Hypertension. US Department of Health and Human Services, Office of the Surgeon General: Washington, DC, 2020. [Google Scholar]
- 4. Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA 2020; 324:1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shahu A, Herrin J, Dhruva SS, Desai NR, Davis BR, Krumholz HM, Spatz ES. Disparities in socioeconomic context and association with blood pressure control and cardiovascular outcomes in ALLHAT. J Am Heart Assoc 2019; 8:e012277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Commodore-Mensah Y, Turkson-Ocran RA, Foti K, Cooper LA, Himmelfarb CD. Associations between social determinants and hypertension, stage 2 hypertension, and controlled blood pressure among men and women in the United States. Am J Hypertens 2021; 34:707–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pinheiro LC, Reshetnyak E, Sterling MR, Levitan EB, Safford MM, Goyal P. Multiple vulnerabilities to health disparities and incident heart failure hospitalization in the REGARDS study. Circ Cardiovasc Qual Outcomes 2020; 13:e006438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reshetnyak E, Ntamatungiro M, Pinheiro LC, Howard VJ, Carson AP, Martin KD, Safford MM. Impact of multiple social determinants of health on incident stroke. Stroke 2020; 51:2445–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beckman AL, Herrin J, Nasir K, Desai NR, Spatz ES. Trends in cardiovascular health of US adults by income, 2005–2014. JAMA Cardiol 2017; 2:814–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nadruz W Jr, Claggett B, Henglin M, Shah AM, Skali H, Rosamond WD, Folsom AR, Solomon SD, Cheng S. Widening racial differences in risks for coronary heart disease. Circulation 2018; 137:1195–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abdalla SM, Yu S, Galea S. Trends in cardiovascular disease prevalence by income level in the United States. JAMA Netw Open 2020; 3:e2018150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health 2011; 32:381–398. [DOI] [PubMed] [Google Scholar]
- 13. Clouston SAP, Natale G, Link BG. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: a examination of the emergence of social inequalities. Soc Sci Med 2021; 268:113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open 2021; 4:e2036462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ahmad K, Erqou S, Shah N, Nazir U, Morrison AR, Choudhary G, Wu WC. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS One 2020; 15:e0241327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rogers TN, Rogers CR, VanSant-Webb E, Gu LY, Yan B, Qeadan F. Racial disparities in COVID-19 mortality among essential workers in the United States. World Med Health Policy 2020; 12:311–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995:80–94. [PubMed] [Google Scholar]
- 18. Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol 2015; 41:311–330. [Google Scholar]
- 19. National Academies of Sciences Engineering and Medicine. Communities in Action: Pathways to Health Equity. The National Academies Press: Washington, DC, 2017. [PubMed] [Google Scholar]
- 20. Office of Disease Prevention and Health Promotion. Social Determinants of Health. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. [Google Scholar]
- 21. Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The National Institute on Minority Health and Health Disparities Research Framework. Am J Public Health 2019; 109:S16–S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, Sanchez E, Sharrief AZ, Sims M, Williams O; American Heart Association . Call to Action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation 2020; 142:e454–e468. [DOI] [PubMed] [Google Scholar]
- 23. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation 2021; 143:e254–e743. [DOI] [PubMed] [Google Scholar]
- 24. Thomas SJ, Booth JN III, Dai C, Li X, Allen N, Calhoun D, Carson AP, Gidding S, Lewis CE, Shikany JM, Shimbo D, Sidney S, Muntner P. Cumulative incidence of hypertension by 55 years of age in blacks and whites: the CARDIA study. J Am Heart Assoc 2018; 7:e007988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: the Multi-Ethnic Study of Atherosclerosis. Hypertension 2011; 57:1101–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mensah GA. Black-white disparities: more than just race. J Am Heart Assoc 2019; 8:e014272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rao S, Segar MW, Bress AP, Arora P, Vongpatanasin W, Agusala V, Essien UR, Correa A, Morris AA, de Lemos JA, Pandey A. Association of genetic West African ancestry, blood pressure response to therapy, and cardiovascular risk among self-reported black individuals in the Systolic Blood Pressure Reduction Intervention Trial (SPRINT). JAMA Cardiol 2021; 6:388–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brown AGM, Houser RF, Mattei J, Mozaffarian D, Lichtenstein AH, Folta SC. Hypertension among US-born and foreign-born non-Hispanic Blacks: National Health and Nutrition Examination Survey 2003–2014 data. J Hypertens 2017; 35:2380–2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Turkson-Ocran RN, Nmezi NA, Botchway MO, Szanton SL, Golden SH, Cooper LA, Commodore-Mensah Y. Comparison of cardiovascular disease risk factors among African immigrants and African Americans: an analysis of the 2010 to 2016 National Health Interview Surveys. J Am Heart Assoc 2020; 9:e013220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Commodore-Mensah Y, Himmelfarb CD, Agyemang C, Sumner AE. Cardiometabolic health in African immigrants to the United States: a call to re-examine research on African-descent populations. Ethn Dis 2015; 25:373–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Non AL, Gravlee CC, Mulligan CJ. Education, genetic ancestry, and blood pressure in African Americans and whites. Am J Public Health 2012; 102:1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mujahid MS, Diez Roux AV, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence (the Multi-Ethnic Study of Atherosclerosis). Am J Hypertens 2011; 24:187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Feldman JM, Waterman PD, Coull BA, Krieger N. Spatial social polarisation: using the index of concentration at the extremes jointly for income and race/ethnicity to analyse risk of hypertension. J Epidemiol Community Health 2015; 69:1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Howard G, Cushman M, Moy CS, Oparil S, Muntner P, Lackland DT, Manly JJ, Flaherty ML, Judd SE, Wadley VG, Long DL, Howard VJ. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA 2018; 320:1338–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Umscheid CA, Gross R, Weiner MG, Hollenbeak CS, Tang SS, Turner BJ. Racial disparities in hypertension control, but not treatment intensification. Am J Hypertens 2010; 23:54–61. [DOI] [PubMed] [Google Scholar]
- 36. Manze M, Rose AJ, Orner MB, Berlowitz DR, Kressin NR. Understanding racial disparities in treatment intensification for hypertension management. J Gen Intern Med 2010; 25:819–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Blair IV, Steiner JF, Hanratty R, Price DW, Fairclough DL, Daugherty SL, Bronsert M, Magid DJ, Havranek EP. An investigation of associations between clinicians’ ethnic or racial bias and hypertension treatment, medication adherence and blood pressure control. J Gen Intern Med 2014; 29:987–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fontil V, Pacca L, Bellows B, Khoong E, McCulloch C, Pletcher M, Bibbins-Domingo K. Abstract 17207: impact of racial differences in treatment intensification and missed visits on disparities in BP control. Circulation 2020; 142:A17207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ferdinand KC, Yadav K, Nasser SA, Clayton-Jeter HD, Lewin J, Cryer DR, Senatore FF. Disparities in hypertension and cardiovascular disease in blacks: the critical role of medication adherence. J Clin Hypertens (Greenwich) 2017; 19:1015–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Forde AT, Sims M, Muntner P, Lewis T, Onwuka A, Moore K, Diez Roux AV. Discrimination and hypertension risk among African Americans in the Jackson Heart Study. Hypertension 2020; 76:715–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Forde AT, Lewis TT, Kershaw KN, Bellamy SL, Diez Roux AV. Perceived discrimination and hypertension risk among participants in the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc 2021; 10:e019541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Creamer J. Inequalities Persist Despite Decline in Poverty for All Major Race and Hispanic Origin Groups. United States Census Bureau: Washington, DC, 2020. https://www.census.gov/library/stories/2020/09/poverty-rates-for-blacks-and-hispanics-reached-historic-lows-in-2019.html. [Google Scholar]
- 43. Health and Health Care for Hispanics in the United States. Kaiser Family Foundation, 2019. https://www.kff.org/infographic/health-and-health-care-for-hispanics-in-the-united-states/. [Google Scholar]
- 44. Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, Davis D, Escamilla-Cejudo JA. Hispanic health in the USA: a scoping review of the literature. Public Health Rev 2016; 37:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Margolis KL, Piller LB, Ford CE, Henriquez MA, Cushman WC, Einhorn PT, Colon PJ Sr, Vidt DG, Christian R, Wong ND, Wright JT Jr, Goff DC Jr; Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial Collaborative Research Group . Blood pressure control in hispanics in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Hypertension 2007; 50:854–861. [DOI] [PubMed] [Google Scholar]
- 46. Bacon E, Riosmena F, Rogers RG. Does the Hispanic health advantage extend to better management of hypertension? The role of socioeconomic status, sociobehavioral factors, and health care access. Biodemography Soc Biol 2017; 63:262–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sorlie PD, Allison MA, Avilés-Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, Lavange LM, Raij L, Schneiderman N, Wassertheil-Smoller S, Talavera GA. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens 2014; 27:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Keisler-Starkey K, Bunch LN.. Health Insurance Coverage in the United States: 2019. US Government Publishing Office: Washington, DC, 2020. [Google Scholar]
- 49. Asante-Muhammad D, Sim S.. Racial Wealth Snapshot: Asian Americans and the Racial Wealth Divide. National Community Reinvestment Coalition, 2020. https://ncrc.org/racial-wealth-snapshot-asian-americans-and-the-racial-wealth-divide/. [Google Scholar]
- 50. Koirala B, Turkson-Ocran RA, Baptiste D, Koirala B, Francis L, Davidson P, Himmelfarb CD, Commodore-Mensah Y. Heterogeneity of cardiovascular disease risk factors among Asian immigrants: insights from the 2010 to 2018 National Health Interview Survey. J Am Heart Assoc 2021; 10:e020408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cook WK, Tseng W, Tam C, John I, Lui C. Ethnic-group socioeconomic status as an indicator of community-level disadvantage: a study of overweight/obesity in Asian American adolescents. Soc Sci Med 2017; 184:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Feldman JM, Conderino S, Islam NS, Thorpe LE. Subgroup variation and neighborhood social gradients—an analysis of hypertension and diabetes among Asian patients (New York City, 2014–2017). J Racial Ethn Health Disparities 2021; 8:256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Jose P, Zhao B, Chung S, Fortmann S, Palaniappan L. PS1-46: variation in hypertension prevalence among Asian American subgroups: results from PACS (Pan Asian Cohort Study). Clin Med Res 2013; 11:136. [Google Scholar]
- 54. Ursua R, Aguilar D, Wyatt L, Tandon SD, Escondo K, Rey M, Trinh-Shevrin C. Awareness, treatment and control of hypertension among Filipino immigrants. J Gen Intern Med 2014; 29:455–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Divney AA, Echeverria SE, Thorpe LE, Trinh-Shevrin C, Islam NS. Hypertension prevalence jointly influenced by acculturation and gender in US immigrant groups. Am J Hypertens 2019; 32:104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liu Q, Quan H, Chen G, Qian H, Khan N. Antihypertensive medication adherence and mortality according to ethnicity: a cohort study. Can J Cardiol 2014; 30:925–931. [DOI] [PubMed] [Google Scholar]
- 57. Chen M-L, Hu J. Health disparities in Chinese Americans with hypertension: a review. Int J Nurs Sci 2014; 1:318–322. [Google Scholar]
- 58. Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health 1997; 18:341–378. [DOI] [PubMed] [Google Scholar]
- 59. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q 2009; 87:443–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Gunja MK, Collins SR.. Who Are the Remaining Uninsured, and Why Do They Lack Coverage? Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018. Publisher Commonwealth Fund, 2019. https://www.commonwealthfund.org/publications/issue-briefs/2019/aug/who-are-remaining-uninsured-and-why-do-they-lack-coverage?redirect_source=/publications/2019/aug/who-are-remaining-uninsured-and-why-do-they-lack-coverage. [Google Scholar]
- 61. Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol 2010; 36:349–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Egan BM, Li J, Sutherland SE, Jones DW, Ferdinand KC, Hong Y, Sanchez E. Sociodemographic determinants of Life’s Simple 7: implications for achieving cardiovascular health and health equity goals. Ethn Dis 2020; 30:637–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Pantell MS, Prather AA, Downing JM, Gordon NP, Adler NE. Association of social and behavioral risk factors with earlier onset of adult hypertension and diabetes. JAMA Netw Open 2019; 2:e193933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. JAMA 2005; 294:2879–2888. [DOI] [PubMed] [Google Scholar]
- 65. McDoom MM, Palta P, Vart P, Juraschek SP, Kucharska-Newton A, Diez Roux AV, Coresh J. Late life socioeconomic status and hypertension in an aging cohort: the atherosclerosis risk in communities study. J Hypertens 2018; 36:1382–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci 2010; 1186:125–145. [DOI] [PubMed] [Google Scholar]
- 67. Claudel SE, Adu-Brimpong J, Banks A, Ayers C, Albert MA, Das SR, de Lemos JA, Leonard T, Neeland IJ, Rivers JP, Powell-Wiley TM. Association between neighborhood-level socioeconomic deprivation and incident hypertension: a longitudinal analysis of data from the Dallas heart study. Am Heart J 2018; 204:109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Buys DR, Howard VJ, McClure LA, Buys KC, Sawyer P, Allman RM, Levitan EB. Association between neighborhood disadvantage and hypertension prevalence, awareness, treatment, and control in older adults: results from the University of Alabama at Birmingham Study of Aging. Am J Public Health 2015; 105:1181–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kershaw KN, Robinson WR, Gordon-Larsen P, Hicken MT, Goff DC Jr, Carnethon MR, Kiefe CI, Sidney S, Diez Roux AV. Association of changes in neighborhood-level racial residential segregation with changes in blood pressure among black adults: the CARDIA study. JAMA Intern Med 2017; 177:996–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Viruell-Fuentes EA, Ponce NA, Alegría M. Neighborhood context and hypertension outcomes among Latinos in Chicago. J Immigr Minor Health 2012; 14:959–967. [DOI] [PubMed] [Google Scholar]
- 71. Miller ER III, Cooper LA, Carson KA, Wang NY, Appel LJ, Gayles D, Charleston J, White K, You N, Weng Y, Martin-Daniels M, Bates-Hopkins B, Robb I, Franz WK, Brown EL, Halbert JP, Albert MC, Dalcin AT, Yeh HC. A dietary intervention in urban African Americans: results of the “Five Plus Nuts and Beans” randomized trial. Am J Prev Med 2016; 50:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Powell W, Richmond J, Mohottige D, Yen I, Joslyn A, Corbie-Smith G. Medical mistrust, racism, and delays in preventive health screening among African-American men. Behav Med 2019; 45:102–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, Knowles P, Storm JS, Adhikari E, Bibbins-Domingo K, Coxson PG, Pletcher MJ, Hannan P, Haley RW. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med 2011; 171:342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Fang J, Chang T, Wang G, Loustalot F. Association between cost-related medication nonadherence and hypertension management among US adults. Am J Hypertens 2020; 33:879–886. [DOI] [PubMed] [Google Scholar]
- 75. Victor RG, Lynch K, Li N, Blyler C, Muhammad E, Handler J, Brettler J, Rashid M, Hsu B, Foxx-Drew D, Moy N, Reid AE, Elashoff RM. A cluster-randomized trial of blood-pressure reduction in black barbershops. N Engl J Med 2018; 378:1291–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Victor RG, Blyler CA, Li N, Lynch K, Moy NB, Rashid M, Chang LC, Handler J, Brettler J, Rader F, Elashoff RM. Sustainability of blood pressure reduction in black barbershops. Circulation 2019; 139:10–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Bryant KB, Moran AE, Kazi DS, Zhang Y, Penko J, Ruiz-Negrón N, Coxson P, Blyler CA, Lynch K, Cohen LP, Tajeu GS, Fontil V, Moy NB, Ebinger JE, Rader F, Bibbins-Domingo K, Bellows BK. Cost-effectiveness of hypertension treatment by pharmacists in black barbershops. Circulation 2021; 143:2384–2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ibe CA, Hickman D, Cooper LA. To advance health equity during COVID-19 and beyond, elevate and support community health workers. JAMA Health Forum 2021; 2: e212724. [DOI] [PubMed] [Google Scholar]
- 79. Brownstein JN, Chowdhury FM, Norris SL, Horsley T, Jack L Jr, Zhang X, Satterfield D. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med 2007; 32:435–447. [DOI] [PubMed] [Google Scholar]
- 80. Cooper LA, Roter DL, Carson KA, Bone LR, Larson SM, Miller ER III, Barr MS, Levine DM. A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. J Gen Intern Med 2011; 26:1297–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ursua RA, Aguilar DE, Wyatt LC, Trinh-Shevrin C, Gamboa L, Valdellon P, Perrella EG, Dimaporo MZ, Nur PQ, Tandon SD, Islam NS. A community health worker intervention to improve blood pressure among Filipino Americans with hypertension: a randomized controlled trial. Prev Med Rep 2018; 11:42–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Allen CG, Brownstein JN, Satsangi A, Escoffery C. Community health workers as allies in hypertension self-management and medication adherence in the United States, 2014. Prev Chronic Dis 2016; 13:E179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Schoenthaler AM, Lancaster KJ, Chaplin W, Butler M, Forsyth J, Ogedegbe G. Cluster randomized clinical trial of FAITH (Faith-Based Approaches in the Treatment of Hypertension) in blacks. Circ Cardiovasc Qual Outcomes 2018; 11:e004691. [DOI] [PubMed] [Google Scholar]
- 84. Yi SS, Wyatt LC, Patel S, Choy C, Dhar R, Zanowiak JM, Chuhan H, Taher MD, Garcia M, Kavathe R, Kim S, Kwon SC, Islam NS. A faith-based intervention to reduce blood pressure in underserved metropolitan New York immigrant communities. Prev Chronic Dis 2019; 16:E106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Brown AF, Ma GX, Miranda J, Eng E, Castille D, Brockie T, Jones P, Airhihenbuwa CO, Farhat T, Zhu L, Trinh-Shevrin C. Structural interventions to reduce and eliminate health disparities. Am J Public Health 2019; 109:S72–S78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Coulon SM, Wilson DK, Egan BM. Associations among environmental supports, physical activity, and blood pressure in African-American adults in the PATH trial. Soc Sci Med 2013; 87:108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Angier H, Green B, Fankhauser K, Marino M, Huguet N, Larson A, DeVoe J. Role of health insurance and neighborhood-level social deprivation on hypertension control following the Affordable Care Act health insurance opportunities. Soc Sci Med 2020; 265:113439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Cole MB, Kim J-H, Levengood TW, Trivedi AN. Association of Medicaid expansion with 5-year changes in hypertension and diabetes outcomes at federally qualified health centers. JAMA Health Forum 2021; 2:e212375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Angell SY, McConnell MV, Anderson CAM, Bibbins-Domingo K, Boyle DS, Capewell S, Ezzati M, de Ferranti S, Gaskin DJ, Goetzel RZ, Huffman MD, Jones M, Khan YM, Kim S, Kumanyika SK, McCray AT, Merritt RK, Milstein B, Mozaffarian D, Norris T, Roth GA, Sacco RL, Saucedo JF, Shay CM, Siedzik D, Saha S, Warner JJ. The American Heart Association 2030 Impact Goal: a presidential advisory from the American Heart Association. Circulation 2020; 141:e120–e138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Benjamin IJ, Valentine CM, Oetgen WJ, Sheehan KA, Brindis RG, Roach WH, Harrington RA, Levine GN, Redberg RF, Broccolo BM, Hernandez AF, Douglas PS, Piña IL, Benjamin EJ, Coylewright MJ, Saucedo JF, Ferdinand KC, Hayes SN, Poppas A, Furie KL, Mehta LS, Erwin JP, Mieres JH, Murphy DJ, Weissman G, West CP, Lawrence WE, Masoudi FA, Jones CP, Matlock DD, Miller JE, Spertus JA, Todman L, Biga C, Chazal RA, Creager MA, Fry ET, Mack MJ, Yancy CW, Anderson RE. 2020 American Heart Association and American College of Cardiology Consensus Conference on professionalism and ethics: a consensus conference report. J Am Coll Cardiol 2021; 77:3079–3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Itchhaporia D. Paving the way for health equity in cardiology: why does it matter? J Am Coll Cardiol 2021; 77:2613–2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Hardeman RR, Murphy KA, Karbeah J, Kozhimannil KB. Naming institutionalized racism in the public health literature: a systematic literature review. Public Health Rep 2018; 133:240–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Fiscella K, Tobin JN, Ogedegbe G. Aligning payment and policies with health care value and equity: blood pressure as a National Vital Sign. JAMA Health Forum 2021; 2:e212965. [DOI] [PubMed] [Google Scholar]
- 94. Kazi DS, Ogedegbe O, Bibbins-Domingo K. Addressing the last-mile problem in blood pressure control—scaling up community-based interventions. JAMA Health Forum 2021; 2:e212022. [DOI] [PubMed] [Google Scholar]
- 95. He FJ, Brinsden HC, MacGregor GA. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens 2014; 28:345–352. [DOI] [PubMed] [Google Scholar]
- 96. Park HK, Lee Y, Kang BW, Kwon KI, Kim JW, Kwon OS, Cobb LK, Campbell NRC, Blakeman DE, Kim CI. Progress on sodium reduction in South Korea. BMJ Glob Health 2020; 5:e002028. [DOI] [PMC free article] [PubMed] [Google Scholar]