Abstract
Hypertension treatment and control prevent more cardiovascular events than management of other modifiable risk factors. Although the age-adjusted proportion of US adults with controlled blood pressure (BP) defined as <140/90 mm Hg, improved from 31.8% in 1999–2000 to 48.5% in 2007–2008, it remained stable through 2013–2014 and declined to 43.7% in 2017–2018. To address the rapid decline in hypertension control, the National Heart, Lung, and Blood Institute and the Division for Heart Disease and Stroke Prevention of the Centers for Disease Control and Prevention convened a virtual workshop with multidisciplinary national experts. Also, the group sought to identify opportunities to reverse the adverse trend and further improve hypertension control. The workshop immediately preceded the Surgeon General’s Call to Action to Control Hypertension, which recognized a stagnation in progress with hypertension control. The presentations and discussions included potential reasons for the decline and challenges in hypertension control, possible “big ideas,” and multisector approaches that could reverse the current trend while addressing knowledge gaps and research priorities. The broad set of “big ideas” was comprised of various activities that may improve hypertension control, including: interventions to engage patients, promotion of self-measured BP monitoring with clinical support, supporting team-based care, implementing telehealth, enhancing community–clinical linkages, advancing precision population health, developing tailored public health messaging, simplifying hypertension treatment, using process and outcomes quality metrics to foster accountability and efficiency, improving access to high-quality health care, addressing social determinants of health, supporting cardiovascular public health and research, and lowering financial barriers to hypertension control.
Keywords: blood pressure, cardiovascular disease, hypertension, prevention, screening
Graphical Abstract
Graphical Abstract.
Hypertension is the predominant risk factor for cardiovascular disease (CVD) and kidney disease.1,2 Controlling blood pressure (BP) significantly reduces mortality and CVD risk among adults diagnosed with hypertension.3 In the United States, hypertension awareness, treatment, and control remain persistent challenges.4 Among adults with a hypertension diagnosis, control (<140/90 mm Hg) of this condition worsened from 53.8% in 2013–2014 to 43.7% in 2017–2018.5
The National Heart, Lung, and Blood Institute (NHLBI) and the Centers for Disease Control and Prevention (CDC) provide leadership in research and public health efforts to improve hypertension control. Building on the work of the Million Hearts initiative,6 CDC launched the National Hypertension Control Roundtable in 2020, a multisector group of public, private, and nonprofit organizations unified to improve national hypertension control, to reach the goal of at least 80% by 2025.7
On 5–6 October 2020, the NHLBI and CDC convened a workshop to discuss the decline in hypertension control and possible multilevel solutions, including research priorities and potential policies to address this public health problem. This manuscript summarizes the workshop and complements the Surgeon General’s Call to Action to Control Hypertension,26 published days after the workshop, which provides targeted strategies for multiple sectors to improve hypertension control in the United States.
THE DECLINE IN HYPERTENSION CONTROL AMONG US ADULTS
Data from the National Health and Nutrition Examination Survey (NHANES) indicate that hypertension control (<140/90 mm Hg) increased from 31.8% in 1999–2000 to 53.7% in 2009–2010, remained stable at 53.8% in 2013–2014, then fell to 43.7% in 2017–2018 (Figure 1).5 Using the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) BP guideline definition of hypertension control (<130/80 mm Hg), only 19% have controlled BP.5 The rapid fall in control was broad based and roughly comparable across age and race–ethnicity groups. In 2017–2018, younger (18–44 years), non-Hispanic (NH) Black adults, and adults without health insurance, a usual health care facility, or health care visits in the past year were less likely to have controlled BP.5 In 2003–2014, total medical care for adults with hypertension was nearly $2,000 more annually than adults without hypertension, equaling $131 billion in adjusted national expenditure.9 Furthermore, their inpatient costs were 2.5 times that of adults without hypertension. These data highlight opportunities for prompt and decisive action to avert the burdensome and costly personal, social, and economic complications of uncontrolled hypertension.
Figure 1.
Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018.5 Age-adjusted estimated proportion of adults with hypertension and controlled blood pressure. NHANES indicates National Health and Nutrition Examination Survey. Hypertension was defined as systolic blood pressure (SBP) level of 140 mm Hg or higher, diastolic blood pressure (DBP) level of 90 mm Hg or higher, and antihypertensive medication use. Controlled blood pressure was defined as SBP level lower than 140 mm Hg and DBP level lower than 90 mm Hg in panels (a) and (b) and SBP level lower than 130 mm Hg and DBP level lower than 80 mm Hg in panels (c) and (d). Treatment was defined by self-reported antihypertensive medication use. Among all adults with hypertension, blood pressure control from 1999–2000 through 2007–2008 yielded P < 0.001 for trend; from 2007–2008 through 2013–2014, P = 0.14 for trend; and from 2013–2014 through 2017–2018, P = 0.003 for trend. Among adults taking antihypertensive medication, blood pressure control from 1999–2000 through 2007–2008 yielded P < 0.001 for trend; from 2007–2008 through 2013–2014, P = 0.12 for trend; and from 2013–2014 through 2017–2018, P = 0.005 for trend. Age adjustment was performed using direct standardization with the standard being all adults across the entire period (1999–2018); the age categories used for standardization were 18–44 years (15.5%), 45–64 years (45.4%), 65–74 years (21.5%), and 75 years or older (17.7%). The line segments were generated using Joinpoint (National Cancer Institute). * Among all adults with hypertension. † Among adults who self-reported taking antihypertensive medication.
POTENTIAL REASONS FOR THE DECLINE IN HYPERTENSION CONTROL
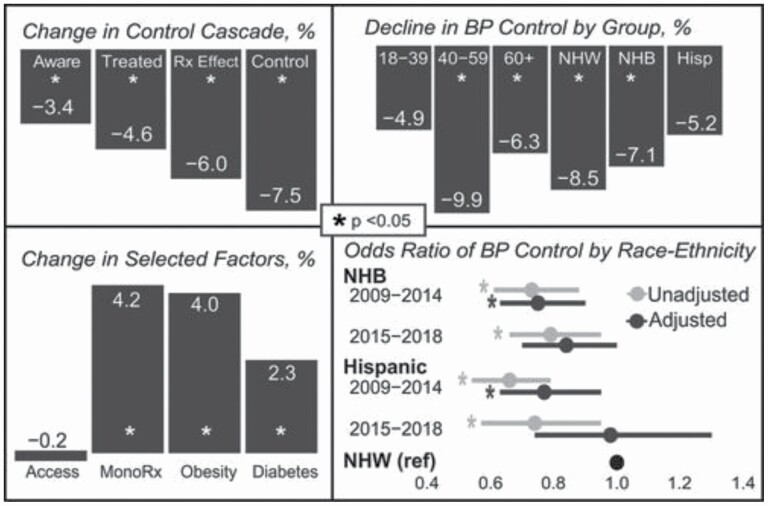
As illustrated in Figure 2, the decline in hypertension control was relatively comparable across age and race–ethnicity groups. Moreover, the decline in hypertension control reflected reductions in awareness and treatment of hypertension and treatment effectiveness or the proportion of treated adults controlled.8 However, access to care, defined as having health care insurance, a regular source of health care, and at least 1 health care visit in the past year, was unchanged in nearly every group. These recent data may suggest that health care quality for diagnosing, reflected in decreased awareness, and managing, reflected in lower rates of treatment and treatment effectiveness, may have fallen. In addition to a lower proportion of adults with hypertension taking antihypertensive medications, the proportion taking a single medication or monotherapy rose.8 The declining treatment and treatment intensity for hypertension was concurrent with a rise in diabetes and obesity, which require more and not less intensive treatment to achieve control.10 While disparities were not exacerbated in the recent fall in hypertension control during the 2015–2018 timeframe, neither did disparities significantly improve.8 The AHA has recently acknowledged structural racism as a root cause of health disparities in the United States that needs to be addressed.11 Although the factors that caused the decline in hypertension control are uncertain, potential contributing factors discussed at the workshop are presented below.
Figure 2.
Hypertension control cascade and change in selected factors, NHANES 2009–2018.10 Abbreviation: NHANES, National Health and Nutrition Examination Survey.
SOCIAL DETERMINANTS OF HEALTH
Social determinants of health (SDoH), the conditions in which people are born, grow, work, live, and age, and the broader forces and systems which shape daily life,12 contribute to hypertension outcomes. Economic inequality continues to widen in the United States. The median net wealth increased by 33% among upper-income families between 2001 and 2016, while the median net worth of middle-income families and lower-income families declined by 20% and 45%, respectively.13 Widening wealth disparities are associated with poorer BP management, with adults with lower incomes having a higher likelihood of hypertension and a lower likelihood of achieving BP control.14 Evidence for this is found in a recent NHANES analysis; SDoH were associated with hypertension, stage 2 hypertension, and controlled BP.15 Hypertension prevalence was higher in NH Black and NH Asian adults than NH White adults. Lack of routine place for health care and being uninsured was associated with uncontrolled hypertension.15
One-third of the geographic variation in nonadherence to antihypertensive medications is associated with SDoH, such as poverty, food insecurity, weak social support systems, and unhealthy built environments16 that make self-care and self-management more challenging.14 Furthermore, recent data from NHANES have shown a higher prevalence of stage 2 hypertension in urban areas than rural areas.17 All 10 states with the highest prevalence of hypertension, which are located in the South, also have the highest rates of overweight and obesity.18 Notably, most of these states have not adopted Medicaid expansion,19 which improves access and affordability of care among low-income persons.20 Federally qualified health centers in Medicaid expansion states have experienced an improvement in hypertension and diabetes control compared with nonexpansion states, particularly among Black and Hispanic populations.21
THE OBESITY EPIDEMIC
Obesity, particularly visceral adiposity, is a significant risk factor for hypertension and contributes to uncontrolled BP.22 Obesity and diabetes are associated with uncontrolled treatment-resistant hypertension or the failure to control BP on 3 or more different antihypertensive medications.23 Recent NHANES data24 show worsening of the obesity epidemic in the United States. The prevalence of obesity among men increased from 27.5% in 1999–2000 to 43.0% in 2017–2018, and severe obesity doubled from 3.1% to 6.9% in the same period.24 Likewise, among women, the prevalence of obesity increased from 33.4% to 41.9%, and severe obesity increased from 6.2% to 11.5%.
HYPERTENSION GUIDELINE AND TREATMENT CONTROVERSIES
Hypertension care is complex. Multiple guidelines with different treatment thresholds, diagnostic criteria, and target goals introduce potential program, communication, and management complexity may have contributed to the decline in controlled BP.25 The 2017 AHA/ACC BP guideline27 and the report from members initially appointed to the Joint National Committee (JNC-8)28 have been the subject of debate and inconsistent implementation by some professional organizations and clinicians.29,30 For example, the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP) recommended that patients with hypertension who are 60 years and older should be treated to a systolic BP target of <150 mm Hg,31 aligning with the JNC-8 writing group recommendation, but conflicting with JNC-7 and the 2017 ACC/AHA BP guideline.27 It is unclear whether these inconsistencies contribute to reduced BP control. Of note, hypertension control to <140/<90 mm Hg declined more in adults 40–59 years than in those 60 years and older.8 This finding suggests that factors other than the JNC-8 report and ACP/AAFP recommendations for a higher systolic BP target may contribute to the broad-based decline in hypertension control.
LACK OF HYPERTENSION AWARENESS
While initiatives such as Million Hearts32 and Target: BP33 sought to improve hypertension awareness nationally, people living with hypertension are too often undiagnosed; they are “hiding in plain sight.” 34 Data from NHANES reported that hypertension awareness increased from 69.9% in 1999 to 84.7% in 2013–2014, it declined to 77% in 2017–2018.5 This suggests that almost 23% of adults with hypertension are not aware of it and are therefore not being treated.5 Increasing overall awareness is needed, alongside tailored interventions to increase awareness among subgroups. For example, young adults (18–44 years old) may be prioritized, as awareness among this age group (62.0%) is lower than estimates among older age groups (45–64 years, 79.3%; 65–74 years, 85.4%; ≥75 years, 82.1%).5,35
CLINICIAN-LEVEL CHALLENGES
Interrelated clinician-level challenges may contribute to the decline in hypertension control. Primary care clinicians (henceforth, clinicians) are at the frontline for diagnosing and treating hypertension. However, clinical or therapeutic inertia, the failure to initiate or intensify therapy during visits, contributes to suboptimal hypertension control.36 Clinicians are not optimally titrating or otherwise managing patient-specific combination therapy for hypertension due to uncertainty about the patient’s true BP, concerns about side effects, optimism that control will be eventually achieved, time constraints, patient nonadherence, and competing patient demands.37 The number of adults who could gain control of their hypertension and prevent avoidable CVD through such systematic care is substantial: 57.8 million adults through initiation or intensification of treatment and 50.5 million through lifestyle modification.38
Increasing burnout among clinicians and clinician teams also contributes to clinical inertia.39,40 Leading causes of burnout include long hours on computerized work, bureaucratic tasks, loss of autonomy, and payer requirements. The high burden of chronic disease and lack of integrated guidelines for efficiently managing multiple chronic conditions also imposes a major load on clinicians. Estimates indicate that primary care clinicians would need nearly 22 hours daily to implement evidence-based guidelines.41 Ten hours are required to implement guidelines for the 10 most common chronic conditions, including hypertension. Clinicians are responsible for high performance on other quality metrics in addition to hypertension control.42 Furthermore, clinicians burdened with excessive workloads and insufficient resources are more likely to burnout, and expanding expectations to address SDoH and lifestyle issues, without training, resources, and system improvements, may worsen rather than aid the situation.43
Available tools to prevent and mitigate uncontrolled hypertension (e.g., Million Hearts Hypertension Control Change Package, 2nd edition44) can be further implemented to expand impact. Also, team-based care, which is recommended in BP and CVD prevention guidelines, is not consistently implemented in primary care.45 These facts highlight potential opportunities to integrate guidelines and redesign elements of chronic condition management to improve efficiency and effectiveness.
“BIG IDEAS” TO IMPROVE HYPERTENSION CONTROL IN THE UNITED STATES
The following “big ideas” summarize potential solutions to reversing the worsening trend in hypertension control. Best practices and promising options that may be used to overcome barriers to hypertension control across diverse communities are also summarized in Table 1. Some options may depend upon new partnerships inside and outside the traditional clinical environment, and new partners may need to be engaged to maximize impact.
Table 1.
Best practices and promising options for overcoming barriers to hypertension control
| 1. Create a patient registry to reach high-risk and undiagnosed patients (e.g., elevated blood pressure readings without diagnosis). |
| 2. Improve trust and provide support via community engagement based on shared decision-making and understanding of community needs and challenges, including SDoH. |
| 3. Identify method(s) for SMBP monitoring, including digital home monitoring for rapid feedback and action. Promote data sharing between patient and clinical team by facilitating rapid, appropriate treatment response, as needed timely exchange of readings and clinical advice. |
| 4. Develop or tailor existing toolkits to provide health care teams with resources to provide lifestyle counseling, address social needs and health literacy, and customize communications with patients. |
| 5. Coordinate community and health care services to build trust and effective deployment of community health care worker assets within a team. |
| 6. Drive adoption of treatment protocols with specific goal ranges and parameters for medication intensification and timely follow-up, referral pathways for patients who do not achieve hypertension control, and healthy lifestyle recommendations. |
| 7. Coordinate treatment of comorbidities such as obesity, hyperlipidemia, and diabetes that may often underlie resistance to pharmacotherapy. |
Abbreviations: SDoH, social determinants of health; SMBP, self-measured blood pressure.
PATIENT-CENTERED HYPERTENSION CARE
A patient-centered approach to care considers a patient’s perspective, psychosocial context, values, and goals.46 Designing hypertension care around the patient and adopting the patient-centered medical home approach has been shown to improve BP control, self-efficacy, and medication adherence.47,48 Flexible care models and delivery mechanisms (i.e., mobile health units, telehealth, pharmacist extenders) may be needed to meet the needs of diverse patients. Furthermore, well-functioning patient-centered medical homes are associated with higher rates of hypertension control than other primary care settings.49
Motivating and engaging patients in self-management are crucial to hypertension control, which requires an informed and activated patient.50 Patient activation interventions, such as those that include engagement and self-management education to enhance problem-solving skills and self-efficacy, can improve hypertension control compared with education alone.51
Shared decision-making, an approach where clinicians and patients make decisions together using the best available evidence and in alignment with patients’ preferences and values, may promote health equity and improve clinical outcomes.8,52 Shared decision-making related to hypertension management is particularly challenging due to the diverse treatment regimens available and lifestyle changes recommended.27 Barriers to consistent engagement in hypertension management are persistent and many times cannot be overcome without support outside of the clinical environment.8 For example, some patients sometimes must choose between paying for food or medications, while others may weigh the benefits of walking outside vs. risks to their safety in a high-crime neighborhood. Almost 4 million Americans forgo medical care due to transportation barriers every year.53
SIMPLIFY HYPERTENSION TREATMENT
Hypertension control can be achieved. Examples of effective initiatives include large insurance-based managed care (e.g., Kaiser Permanente54), national CDC-based initiatives (e.g., Million Hearts), community-based partnerships (e.g., Barbershop Study,55 community pharmacist engagement), Medicaid-directed programs, the Ochsner Hypertension Digital Medicine Program,56 and replications of the Kaiser model in federally qualified health systems.57 Additionally, Target:BP, an AHA—American Medical Association (AMA) collaborative based on the MAP (Measure accurately, Act rapidly, Partner with patients/families/communities) Quality Improvement (QI) framework,58 provides guidance on simplifying hypertension treatment.
These programs include practice facilitation, supporting tools and resources, evidence-based strategies and action steps, performance metrics, peer-to-peer learning, and may be adapted to suit diverse clinical settings. To maximize effectiveness, hypertension treatment protocols should be implemented to ensure that patients receive recommended treatment, reduce nonclinical variations, reinforce the benefits of control, the importance of medications, and healthy lifestyle practices.27
Single-pill combinations (SPCs) of antihypertensive medications should be considered in treatment simplification because it improves hypertension control and cardiovascular outcomes.27,59 Numerous studies and reports document that patients who initiate therapy on 2- and 3-drug SPCs of antihypertensive therapy are more likely to take their medications, achieve lower BP values, have higher rates of hypertension control, and experience lower rates of CVD and death.60,61 Thus, 1 simple strategy for reducing therapeutic inertia is to begin antihypertensive therapy with a SPC.60,61 Further progress on optimization of initial SPCs may require a multilateral effort that includes education of clinicians, patients, further guideline recommendations, i.e., more aligned with the current European guideline,62 ready availability of affordable, effective, and well-tolerated SPCs may facilitate uptake of this treatment course.
SUPPORT SELF-MEASURED BP MONITORING WITH CLINICAL SUPPORT
A recent AHA/AMA Policy Statement63 emphasizes the clinical and cost-effectiveness of self-measured blood pressure (SMBP) monitoring. Other scientific statements, guidelines, and meta-analyses have stressed the value of SMBP monitoring,27,64–66 and the CDC established SMBP monitoring with clinical support as a best practice.67 The wider use of SMBP monitoring with clinical support may help reverse the worsening trend in hypertension control and link clinical care and communities. SMBP monitoring engages patients in their care and can improve hypertension control when accompanied by patient education, support by community health workers, case management, or pharmacy support.67 SMBP readings have been shown to be more prognostic of stroke, CVD, and other target organ damage than office-based readings.63,68 Evidence on SMBP monitoring comes predominantly from studies with research personnel interacting with patients. Research has focused on relative risks of hypertension phenotypes (white coat hypertension and masked hypertension) and less on adherence to hypertension treatment.66 While there are extensive outcome studies correlating SMBP monitoring with clinical outcomes in White and Asian populations, there are fewer on Black and Hispanic adults.67
Wider use of SMBP monitoring may occur because of inclusion in quality measures. The clinical quality measures (e.g., Healthcare Effectiveness Data and Information Set [HEDIS] Controlling High BP and Centers for Medicare and Medicaid Services [CMS] Controlling High BP) recently began including patient-generated BP readings, but health information technology solutions that can seamlessly import BP readings into electronic health records are still needed.69 Readings from SMBP, when fully integrated into electronic health records, can inform timely shared decision-making and reduce patient burden associated with recording and transmitting BP data.70 Wide effective use of this approach may be enhanced by validated and affordable devices, insurance coverage of devices, and internet access for patients.63
Federal guidance71,72 allows for high deductible health plans to cover SMBP devices and antihypertensive medications on a predeductible basis. Recently, Medicare expanded reimbursement for the instruction of proper SMBP measurement techniques and the collection of data connected to clinical decision-making and use of SMBP devices via the use of Current Procedural Terminology (CPT) codes, which provides a sustainable funding stream for clinical systems.63 However, uptake of CPT codes for SMBP has been slow,73 and health system-based billing and coding software changes may be needed to accompany the policy intervention.
IMPLEMENT TELEHEALTH FOR HYPERTENSION MANAGEMENT
Telehealth has been increasingly adopted since the COVID-19 pandemic and presents a unique opportunity to improve hypertension control. A recent International Expert Position Paper noted that “telemedicine in hypertension management should include remote monitoring and transmission of vital signs (notably BP) and medication adherence plus education on lifestyle and risk factors, with video consultation as an option.” 74
The position paper describes studies that find telehealth also facilitates team-based care and shifts hypertension care from the traditional “brick-and-mortar” BP care approach.74 Telehealth for hypertension control may benefit patients, clinicians, and health care systems, but the impact on hypertension control and racial–ethnic disparities needs additional study.74 Telehealth reduces patient-level barriers to hypertension control such as transportation challenges, childcare, and taking time off work for appointments74; this reduction in barriers suggests that telehealth may be cost-saving for patients.
INCENTIVIZE TEAM-BASED CARE
Team-based care, a health system intervention to enhance patient care by having 2 or more health care professionals work together, is another best practice.45,75 In a prior meta-analysis, team-based care with medication titration by physicians and clinicians other than physicians resulted in pooled mean systolic BP reductions of 5.7 and 6.6 mm Hg, respectively.76 Team-based care with treatment protocols has a robust empirical foundation and can advance hypertension control.76,77
These studies suggest that most patients can be successfully managed with team-based care. Expanding team-based care may require addressing professional “turf” issues, which often involve debates regarding who can and who should provide health care services independently.78
Team-based care involving pharmacists is an effective strategy to improve hypertension control.79,80 Trials involving pharmacists result in mean systolic BP reductions of 6.1 mm Hg.81 Prior researchers have suggested that wider use of pharmacists may be enhanced if they could independently prescribe antihypertensive therapy, without collaborative practice agreements, with reimbursement at levels that covers the costs of their services.82,83
Team-based care involving nurses improves hypertension outcomes.83 Nurse-led team-based care results in a mean SBP reduction of 5.84 mm Hg.83 Nurses measure BP, provide patient education, conduct community-based screenings, and implement community-based hypertension control programs84,85 and nurse practitioners diagnose and manage hypertension. In the United Kingdom, nurse prescribers who are registered nurses undergo specific training, which allows them to prescribe medications from a specified list without physician supervision.86 Findings from global studies suggest that expanding the role of the nurse in team-based care to include nurse-prescribing or titrating of hypertension medications may be a promising way to improve hypertension control85,87 and presents an opportunity for future study.
Community health workers are frontline health workers who are essential allies in improving hypertension control and advancing health equity.88,89 Because community health workers often come from the communities they serve, they are more likely to be culturally sensitive and adept at overcoming socioeconomic and other barriers to hypertension control.90 In the United States, community health workers are effective team members in managing hypertension and other chronic conditions and serve as a link between the community and clinic.91
Since payers often determine reimbursement models, efforts engaging them in more effectively supporting team-based care is worthwhile.92 Payers may also support value-based care to reimburse health care teams based on the quality of hypertension care rather than the current fee-for-service model.93
ENHANCE COMMUNITY–CLINICAL LINKAGES
Strong linkages and synergies between the clinic and community can improve the management of chronic conditions.94 The continuum of community–clinical linkage ranges from networking (e.g., information exchange between the community and clinic) to merging (e.g., both entities operate as 1 entity and roles and culture are blended).94
When staffing and funding permit, local public health departments can help link community members with local primary care practices. One recent example, the Accountable Health Communities initiative established by CMS, funds bridge organizations to build linkages between clinicians and community organizations to support robust screening, referral, and navigation services for patients with unmet health and social needs.95 Early results of the Accountable Health Communities initiative suggest a need for enhanced navigation, patient tracking, and community resources—roles that state and local health departments may provide.
An assessment of projected costs and integrated data systems needs may be used to inform future decisions regarding community–clinic linkages infrastructure. Since financial resources vary by community, some may not have sufficient resources to support these linkages. Since the workshop, the Office of Minority Health and Health Resources and Services Administration (HRSA) have announced the National Hypertension Control Initiative—a cooperative agreement with AHA focusing on hypertension control improvement using MAP, SMBP monitoring, and community–clinic linkages in HRSA health centers serving approximately 9 million patients.96
USE PERFORMANCE AND QUALITY METRICS TO ENHANCE ACCOUNTABILITY
The 2019 AHA/ACC Clinical Performance and Quality Measures for Adults with High Blood Pressure inform the assessment of adherence to hypertension guidelines in clinical practice.42 Effective data systems may need to include electronic health records with QI feedback and community information. Data systems aligned with hypertension control incentives may be more helpful. Treatment standardization can be achieved by providing rapidly disseminated QI metrics that demonstrate clinician performance compared with team-based performance.97 There is an opportunity to design simpler and more constructive QI metrics that may further accountability and align with incentives. QI metrics may also be measured at the community level and can be reported publicly. Enhanced electronic health record standards for meaningful use, which incorporate actionable decision-making to identify people with uncontrolled hypertension and an integrated approach to support data collection for patient care, population, QI, and research, should be helpful.97 Stratifying performance measures and QI metrics by SDoH may uncover health and health care disparities, data which may be used to advance efforts to address these issues.
ENHANCE ACCESS TO HIGH-QUALITY HEALTH CARE AND EXPLORE NEW HEALTH CARE DELIVERY OPTIONS
Healthy People 2030, the nation’s health and well-being objectives for the coming decade, prioritizes improved access to high-quality health care and control of hypertension as central factors in promoting the nation’s health.98 The lack of access to high-quality health care may be driven by limited insurance coverage. Muntner et al.5 observed that controlled BP was more likely among the insured (43.2%–53.4%) (than the uninsured (24.2%). Having health insurance does not equate to uniform coverage, benefits, or access, and people who are “underinsured” may face similar barriers as those without insurance. High-quality hypertension management may consider removing barriers to achieving control and may be supported by focused insurance coverage of essential elements.99
While broad-scale interventions to improve hypertension control have been documented,44 the approach to coverage of these activities may be fragmented or limited in reimbursement. Patient barriers to optimal hypertension management include lack of coverage of validated BP devices, copayments for antihypertensive medications, or transportation challenges, all of which might be addressed through expanded insurance coverage, value-based payments, or use of mail-order pharmacies.26,100 The CMS have recognized the benefit of value-based insurance design in addressing SDOH, and recently provided a roadmap for states in further exploring these models. In addition, the CMS Innovation Center has plans to fund value-based insurance design models throughout the United States aiming to evaluate their effectiveness in reducing expenditures, improving quality of care and enhancing the coordination and efficiency of health care delivery.101 Prior research assessing the benefit of implementing key components of value-based insurance design have noted differences in outcomes by race/ethnic group, potentially highlighting the value of these interventions in promoting health equity.102
DEVELOP TAILORED PUBLIC HEALTH MESSAGING ON IMPORTANCE OF HYPERTENSION CONTROL
Effective messaging, led by the National High Blood Pressure Education Program (NHBPEP), contributed to the public health successes of the 1960s and 1970s.103 The current trend in hypertension control may warrant additional programs. Public health messaging may be adapted to reach all demographics of the US population. As the United States continues to diversify,104 public health messaging may be tailored to diverse populations.
Additional mass social media strategies to improve behaviors contributing to hypertension control may be warranted. Celebrities could be engaged in motivating the public to be screened (“Katie Couric effect”), increasing public awareness of the connection between uncontrolled hypertension and CVD.105
RESEARCH OPPORTUNITIES
The workshop developed a list of research opportunities based on review of the possible causes of the decline in hypertension control and further study of the big ideas discussed at the workshop (Table 2). Some research opportunities have a growing evidence base, while others are more limited, each may require substantial commitment and investment to assess its importance in improving hypertension control.
Table 2.
Research gaps and opportunities
| Effective multisector approaches to improve hypertension control. |
| How to achieve team-based approaches with clinicians other than physicians, particularly on adjusting medications. |
| Effectiveness of self-measured blood pressure monitoring in diverse populations, diverse clinical settings, and relationship to cardiovascular disease outcomes in diverse populations. |
| Role of community health workers in community–clinical linkages to improve hypertension control. |
| Effectiveness of community-primary care linkages to mitigate social determinants of health that prevent patients from achieving hypertension control. |
| Incentive models and identify drivers of implementation among diverse populations. |
| Effective strategies for small independent practices to achieve superior control. |
| Interventions (i.e., toolkits, change packages, etc.) that are scalable and sustainable and part of quality care in diverse settings. |
| Mechanisms of feedback at the point of care that help clinicians engage patients in informed, shared decision-making regarding blood pressure control. |
| Alignment of incentives and drivers to improve access to high-quality care and reduce inequities and variation in outcomes. |
| Payment and benefit designs which are the most effective in achieving better hypertension control. |
| Strategies to overcome behavioral change challenges of lifestyle change at individual, community, and societal levels. |
| Effective messaging around blood pressure control and health for clinicians and patients and the general public. |
| How social determinants of health cause hypertension and reduce the effectiveness of hypertension control. |
| Integrated guidelines and other strategies that improve health care efficiency and improve hypertension control. |
| How telehealth may improve hypertension control by reducing health disparities and enhance team-based care. |
OPPORTUNITIES FOR ACTION
The US Surgeon General’s Call to Action to Control Hypertension has brought the importance of controlling hypertension to the forefront of the public health agenda.26 The day prior to the release of the Call to Action, workshop participants discussed the potential benefits of making hypertension control a community-level and national vital sign. To foster guideline-based care improvements in hypertension control, leaders from different sectors, including federal and state governments, major integrated health systems, payers, the medical device industry, pharmaceutical industry, and other sectors, can consider partnering to provide relevant expertise.106
Uncontrolled hypertension leads to largely preventable death and unnecessary suffering.2,107 Now is an opportune time to eliminate disparities in hypertension control.26 Disparities in SDoH between racial and ethnic minority groups may constitute an injustice, and the workshop participants support the efforts of the CDC, NIH, and nonfederal partners to address these issues.11,108–110 Consequently, national strategies to reduce the health and economic burden of uncontrolled hypertension may necessitate examining the adverse impact of structural racism and promoting health equity. Improving hypertension control would have a significant population health impact in a short period.26 We need all hands on deck to steer the nation back on track to improving hypertension control to the national goal of at least 80% by 2025.7
DISCLOSURE
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute (NHLBI), the National Institutes of Health, or the Centers for Disease Control and Prevention.
Conflicts of Interest
The authors declare no conflicts of interest. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute (NHLBI), the National Institutes of Health, or the Centers for Disease Control and Prevention.
REFERENCES
- 1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 2. Clark D III, Colantonio LD, Min YI, Hall ME, Zhao H, Mentz RJ, Shimbo D, Ogedegbe G, Howard G, Levitan EB, Jones DW, Correa A, Muntner P. Population-attributable risk for cardiovascular disease associated with hypertension in black adults. JAMA Cardiol 2019; 4:1194–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387:957–967. [DOI] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention (CDC). Hypertension Cascade: Hypertension Prevalence, Treatment and Control Estimates Among US Adults Aged 18 Years and Older Applying the Criteria from the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2013–2016. Atlanta, GA: US Department of Health and Human Services, 2019. [Google Scholar]
- 5. Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA 2020; 324:1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Frieden TR, Berwick DM. The “Million Hearts” initiative—preventing heart attacks and strokes. N Engl J Med 2011; 365:e27. [DOI] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention (CDC). National Hypertension Control Roundtable. https://www.cdc.gov/dhdsp/programs/hypertension-roundtable.htm. Accessed 20 May 2020.
- 8. Egan BM, Li J, Sutherland SE, Rakotz MK, Wozniak GD. Hypertension control in the United States 2009 to 2018: factors underlying falling control rates during 2015 to 2018 across age- and race-ethnicity groups. Hypertension 2021; 78:578–587. [DOI] [PubMed] [Google Scholar]
- 9. Kirkland EB, Heincelman M, Bishu KG, Schumann SO, Schreiner A, Axon RN, Mauldin PD, Moran WP. Trends in healthcare expenditures among US adults with hypertension: national estimates, 2003–2014. J Am Heart Assoc 2018; 7:e008731. https://pubmed.ncbi.nlm.nih.gov/29848493/ (doi: 10.1161/JAHA.118.008731). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. NCD Risk Factor Collaboration (NCD-RisC)—Americas Working Group. Trends in cardiometabolic risk factors in the Americas between 1980 and 2014: a pooled analysis of population-based surveys. Lancet Glob Health 2020; 8: e123–e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, Sanchez E, Sharrief AZ, Sims M, Williams O; American Heart Association . Call to Action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation 2020; 142:e454–e468. [DOI] [PubMed] [Google Scholar]
- 12. Marmot M, Friel S, Bell R, Houweling TA, Taylor S; Commission on Social Determinants of Health . Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008; 372:1661–1669. [DOI] [PubMed] [Google Scholar]
- 13. Horowitz JM, Igielnik R, Kochhar R.. Most Americans Say There Is Too Much Economic Inequality in the U.S., but Fewer Than Half Call It a Top Priority. Washington, DC: Pew Research Center, 2020. [Google Scholar]
- 14. Anstey DE, Christian J, Shimbo D. Income inequality and hypertension control. J Am Heart Assoc 2019; 8:e013636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Commodore-Mensah Y, Turkson-Ocran RA, Foti K, Cooper LA, Himmelfarb CD. Associations between social determinants and hypertension, stage 2 hypertension, and controlled blood pressure among men and women in the United States. Am J Hypertens 2021; 34:707–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Donneyong MM, Chang TJ, Jackson JW, Langston MA, Juarez PD, Sealy-Jefferson S, Lu B, Im W, Valdez RB, Way BM, Colen C, Fischer MA, Salsberry P, Bridges JFP, Hood DB. Structural and social determinants of health factors associated with county-level variation in non-adherence to antihypertensive medication treatment. Int J Environ Res Public Health 2020; 17:6684. (doi: 10.3390/ijerph17186684). https://www.mdpi.com/1660-4601/17/18/6684?type=check_update&version=1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ostchega Y, Hughes JP, Zhang G, Nwankwo T, Graber J, Nguyen DT. Differences in hypertension prevalence and hypertension control by urbanization among adults in the United States, 2013–2018. Am J Hypertens 2021. https://academic.oup.com/ajh/advance-article/doi/10.1093/ajh/hpab067/6257011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Trust for America’s Health. The State of Obesity: Better Policies for a Healthier America 2020. https://www.tfah.org/wp-content/uploads/2020/09/TFAHObesityReport_20.pdf. Accessed 29 December 2020.
- 19. Kaiser Family Foundation. Status of State Medicaid Expansion Decision: Interactive Map. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/. Accessed 4 August 2021.
- 20. Baumgartner J, Collins S, Radley D, Hayes S. How the Affordable Care Act (ACA) has narrowed racial and ethnic disparities in insurance coverage and access to health care, 2013–18. Health Serv Res 2020; 55:56–57. [Google Scholar]
- 21. Cole MB, Kim J, Levengood TW, Trivedi AN. Association of Medicaid expansion with 5-year changes in hypertension and diabetes outcomes at federally qualified health centers. JAMA Health Forum 2021; 2:e212375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Garrison RJ, Kannel WB, Stokes J III, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med 1987; 16:235–251. [DOI] [PubMed] [Google Scholar]
- 23. Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, Egan BM, Flack JM, Gidding SS, Judd E, Lackland DT, Laffer CL, Newton-Cheh C, Smith SM, Taler SJ, Textor SC, Turan TN, White WB; American Heart Association Professional/Public Education and Publications Committee of the Council on Hypertension; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Genomic and Precision Medicine; Council on Peripheral Vascular Disease; Council on Quality of Care and Outcomes Research; and Stroke Council . Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension 2018; 72:e53–e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, Hales CM. Trends in obesity prevalence by race and Hispanic origin—1999–2000 to 2017–2018. JAMA 2020; 324:1208–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ewen S, Mahfoud F, Böhm M. Blood pressure targets in the elderly: many guidelines, much confusion. Eur Heart J 2019; 40:2029–2031. [DOI] [PubMed] [Google Scholar]
- 26. U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Control Hypertension. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2020. [Google Scholar]
- 27. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018; 71:e127–e248. [DOI] [PubMed] [Google Scholar]
- 28. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520. [DOI] [PubMed] [Google Scholar]
- 29. Steichen O. The burden of conflicting guidelines. J Hypertens 2020; 38:1945–1947. [DOI] [PubMed] [Google Scholar]
- 30. Wright JT Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med 2014; 160:499–503. [DOI] [PubMed] [Google Scholar]
- 31. Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA, Fitterman N, Barry MJ, Horwitch CA, Iorio A, McLean RM; Clinical Guidelines Committee of the American College of Physicians and the Commission on Health of the Public and Science of the American Academy of Family Physicians . Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med 2017; 166:430–437. [DOI] [PubMed] [Google Scholar]
- 32. Ritchey MD, Loustalot F, Wall HK, Steiner CA, Gillespie C, George MG, Wright JS. Million Hearts: description of the national surveillance and modeling methodology used to monitor the number of cardiovascular events prevented during 2012–2016. J Am Heart Assoc 2017; 6:e006021. (doi: 10.1161/JAHA.117.006021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Target: BP. Target: BP Fact Sheet. http://www.heart.org/idc/groups/heart-public/@wcm/@mwa/documents/downloadable/ucm_482030.pdf. Accessed 13 September 2021.
- 34. Wall HK, Hannan JA, Wright JS. Patients with undiagnosed hypertension: hiding in plain sight. JAMA 2014; 312:1973–1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Foti K, Wang D, Appel LJ, Selvin E. Hypertension awareness, treatment, and control in US adults: trends in the hypertension control cascade by population subgroup (National Health and Nutrition Examination Survey, 1999–2016). Am J Epidemiol 2019; 188:2165–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fine LJ, Cutler JA. Hypertension and the treating physician: understanding and reducing therapeutic inertia. Hypertension 2006; 47:319–320. [DOI] [PubMed] [Google Scholar]
- 37. Berlowitz DR. Clinical inertia and the 2017 ACA/AHA guideline. J Clin Hypertens (Greenwich) 2018; 20:1392–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ritchey MD, Gillespie C, Wozniak G, Shay CM, Thompson-Paul AM, Loustalot F, Hong Y. Potential need for expanded pharmacologic treatment and lifestyle modification services under the 2017 ACC/AHA Hypertension Guideline. J Clin Hypertens (Greenwich) 2018; 20:1377–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Agency for Healthcare Research and Quality. Physician Burnout. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html#:~:text=Conclusion,shortages%20in%20primary%20care%20physicians. Accessed 30 December 2020.
- 40. Goldberg DG, Soylu TG, Grady VM, Kitsantas P, Grady JD, Nichols LM. Indicators of workplace burnout among physicians, advanced practice clinicians, and staff in small to medium-sized primary care practices. J Am Board Fam Med 2020; 33:378–385. [DOI] [PubMed] [Google Scholar]
- 41. Yarnall KS, Østbye T, Krause KM, Pollak KI, Gradison M, Michener JL. Family physicians as team leaders: “time” to share the care. Prev Chronic Dis 2009; 6:A59. [PMC free article] [PubMed] [Google Scholar]
- 42. Casey DE Jr, Thomas RJ, Bhalla V, Commodore-Mensah Y, Heidenreich PA, Kolte D, Muntner P, Smith SC Jr, Spertus JA, Windle JR, Wozniak GD, Ziaeian B. 2019 AHA/ACC clinical performance and quality measures for adults with high blood pressure: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes 2019; 12:e000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. National Academies of Sciences, Engineering, and Medicine. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: National Academies Press (US); 2019. [PubMed] [Google Scholar]
- 44. Centers for Disease Control and Prevention. Hypertension Control Change Package, 2nd edn. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2 2020. [Google Scholar]
- 45. Community Preventive Services Task Force. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med 2014; 47:100–102. [DOI] [PubMed] [Google Scholar]
- 46. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001. [PubMed]
- 47. Pourat N, Chen X, Lee C, Zhou W, Daniel M, Hoang H, Sripipatana A. Assessing the impact of patient-centered medical home principles on hypertension outcomes among patients of HRSA-Funded Health Centers. Am J Hypertens 2019; 32:418–425. [DOI] [PubMed] [Google Scholar]
- 48. Choudhry NK, Kronish IM, Vongpatanasin W, Ferdinand KC, Pavlik VN, Egan BM, Schoenthaler A, Houston Miller N, Hyman DJ; American Heart Association Council on Hypertension; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology . Medication adherence and blood pressure control: a scientific statement from the American Heart Association. Hypertension 2021; 79:e1–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. DeVries A, Li CH, Sridhar G, Hummel JR, Breidbart S, Barron JJ. Impact of medical homes on quality, healthcare utilization, and costs. Am J Manag Care 2012; 18:534–544. [PubMed] [Google Scholar]
- 50. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002; 288:1775–1779. [DOI] [PubMed] [Google Scholar]
- 51. Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health 2014; 104:e25–e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Langford AT, Williams SK, Applegate M, Ogedegbe O, Braithwaite RS. Partnerships to improve shared decision making for patients with hypertension—health equity implications. Ethn Dis 2019; 29:97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Health Research & Educational Trust. Social Determinants of Health Series: Transportation and the Role of Hospitals. https://www.aha.org/ahahret-guides/2017-11-15-social-determinants-health-series-transportation-and-role-hospitals. Accessed 3 August 2021.
- 54. Jaffe MG, Young JD. The Kaiser Permanente Northern California Story: improving hypertension control from 44% to 90% in 13 years (2000 to 2013). J Clin Hypertens (Greenwich) 2016; 18:260–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Victor RG, Lynch K, Li N, Blyler C, Muhammad E, Handler J, Brettler J, Rashid M, Hsu B, Foxx-Drew D, Moy N, Reid AE, Elashoff RM. A cluster-randomized trial of blood-pressure reduction in black barbershops. N Engl J Med 2018; 378:1291–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Milani RV, Lavie CJ, Ventura HO. New aspects in the management of hypertension in the digital era. Curr Opin Cardiol 2021; 36:398–404. [DOI] [PubMed] [Google Scholar]
- 57. Centers for Disease Control and Prevention (CDC). Hypertension Management Program (HMP) Toolkit. https://www.cdc.gov/dhdsp/pubs/toolkits/hmp-toolkit/index.htm. Accessed 1 August 2021.
- 58. Egan BM, Sutherland SE, Rakotz M, Yang J, Hanlin RB, Davis RA, Wozniak G. Improving hypertension control in primary care with the measure accurately, act rapidly, and partner with patients protocol. Hypertension 2018; 72:1320–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Tsioufis K, Kreutz R, Sykara G, van Vugt J, Hassan T. Impact of single-pill combination therapy on adherence, blood pressure control, and clinical outcomes: a rapid evidence assessment of recent literature. J Hypertens 2020; 38:1016–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rea F, Corrao G, Merlino L, Mancia G. Initial antihypertensive treatment strategies and therapeutic inertia. Hypertension 2018; 72:846–853. [DOI] [PubMed] [Google Scholar]
- 61. Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SA, Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension 2009; 53:646–653. [DOI] [PubMed] [Google Scholar]
- 62. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; Authors/Task Force Members . 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018; 36:1953–2041. [DOI] [PubMed] [Google Scholar]
- 63. Shimbo D, Artinian NT, Basile JN, Krakoff LR, Margolis KL, Rakotz MK, Wozniak G; American Heart Association and the American Medical Association . Self-measured blood pressure monitoring at home: a joint policy statement from the American Heart Association and American Medical Association. Circulation 2020; 142:e42–e63. [DOI] [PubMed] [Google Scholar]
- 64. Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D; American Heart Association; American Society of Hypertension; Preventive Cardiovascular Nurses Association . Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Cardiovasc Nurs 2008; 23:299–323. [DOI] [PubMed] [Google Scholar]
- 65. Muntner P, Einhorn PT, Cushman WC, Whelton PK, Bello NA, Drawz PE, Green BB, Jones DW, Juraschek SP, Margolis KL, Miller ER III, Navar AM, Ostchega Y, Rakotz MK, Rosner B, Schwartz JE, Shimbo D, Stergiou GS, Townsend RR, Williamson JD, Wright JT Jr, Appel LJ; 2017 National Heart, Lung, and Blood Institute Working Group . Blood pressure assessment in adults in clinical practice and clinic-based research: JACC Scientific Expert Panel. J Am Coll Cardiol 2019; 73:317–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Community Preventive Services Task Force (CPSTF). Cardiovascular Disease Prevention and Control: Self-measured Blood Pressure Monitoring Interventions for Improved Blood Pressure Control. https://www.thecommunityguide.org/sites/default/files/assets/CVD-Self-Measured-Blood-Pressure_4.pdf. Accessed 23 July 2019.
- 67. Centers for Disease Control and Prevention (CDC). Self-measured Blood Pressure Monitoring with Clinical Support. https://www.cdc.gov/dhdsp/pubs/docs/Best_Practice_Guide_SMBP_508.pdf. Accessed 20 August 2020.
- 68. Schwartz JE, Muntner P, Kronish IM, Burg MM, Pickering TG, Bigger JT, Shimbo D. Reliability of office, home, and ambulatory blood pressure measurements and correlation with left ventricular mass. J Am Coll Cardiol 2020; 76:2911–2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Cohen DJ, Dorr DA, Knierim K, DuBard CA, Hemler JR, Hall JD, Marino M, Solberg LI, McConnell KJ, Nichols LM, Nease DE Jr, Edwards ST, Wu WY, Pham-Singer H, Kho AN, Phillips RL Jr, Rasmussen LV, Duffy FD, Balasubramanian BA. Primary care practices’ abilities and challenges in using electronic health record data for quality improvement. Health Aff (Millwood) 2018; 37:635–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. McManus RJ, Mant J, Haque MS, Bray EP, Bryan S, Greenfield SM, Jones MI, Jowett S, Little P, Penaloza C, Schwartz C, Shackleford H, Shovelton C, Varghese J, Williams B, Hobbs FD, Gooding T, Morrey I, Fisher C, Buckley D. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA 2014; 312:799–808. [DOI] [PubMed] [Google Scholar]
- 71. Center for Value-Based Insurance. Expanding Flexibility in HSA-Eligible High Deductible Health Plans. https://vbidcenter.org/initiatives/hsa-high-deductible-health-plans-2/. Accessed 5 July 2021.
- 72. Internal Revenue Service Notice 2019-45. Additional Preventive Care Benefits Permitted to be Provided by a High Deductible Health Plan Under § 223. https://www.irs.gov/pub/irs-drop/n-19-45.pdf. Accessed 16 October 2021.
- 73. Wall HK, Wright JS, Jackson SL, Daussat L, Ramkissoon N, Schieb LJ, Stolp H, Tong X, Loustalot F. How do we jump-start self-measured blood pressure monitoring in the U.S.? Addressing barriers beyond the published literature. Am J Hypertens 2022; 35:244–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Omboni S, McManus RJ, Bosworth HB, Chappell LC, Green BB, Kario K, Logan AG, Magid DJ, Mckinstry B, Margolis KL, Parati G, Wakefield BJ. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an international expert position paper. Hypertension 2020; 76:1368–1383. [DOI] [PubMed] [Google Scholar]
- 75. Centers for Disease Control and Prevention (CDC). Promoting Team-Based Care to Improve High Blood Pressure Control. https://www.cdc.gov/dhdsp/pubs/guides/best-practices/team-based-care.htm. Accessed 16 April 2021.
- 76. Mills KT, Obst KM, Shen W, Molina S, Zhang HJ, He H, Cooper LA, He J. Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients: a systematic review and meta-analysis. Ann Intern Med 2018; 168:110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. World Health Organization(WHO). HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care: Evidence-Based Treatment Protocols. Geneva: World Health Organization; 2018. [Google Scholar]
- 78. Kliff S. Obamaare is ramping up a turf war. Washington Post 2013. https://www.washingtonpost.com/news/wonk/wp/2013/02/27/how-obamacare-is-ramping-up-a-health-care-turf-war/ [Google Scholar]
- 79. Proia KK, Thota AB, Njie GJ, Finnie RK, Hopkins DP, Mukhtar Q, Pronk NP, Zeigler D, Kottke TE, Rask KJ, Lackland DT, Brooks JF, Braun LT, Cooksey T; Community Preventive Services Task Force . Team-based care and improved blood pressure control: a community guide systematic review. Am J Prev Med 2014; 47:86–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Carter BL, Bosworth HB, Green BB. The hypertension team: the role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens (Greenwich) 2012; 14:51–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Cheema E, Sutcliffe P, Singer DR. The impact of interventions by pharmacists in community pharmacies on control of hypertension: a systematic review and meta-analysis of randomized controlled trials. Br J Clin Pharmacol 2014; 78:1238–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. National Council for Prescription Drug Programs. Billing Guidance for Pharmacists’ Professional and Patient Care Services. https://www.ncpdp.org/NCPDP/media/pdf/WhitePaper/Billing-Guidance-for-Pharmacists-Professional-and-Patient-Care-Services-White-Paper.pdf?ext=.pdf. 2021.
- 83. Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med 2009; 169:1748–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Spruill TM, Williams O, Teresi JA, Lehrer S, Pezzin L, Waddy SP, Lazar RM, Williams SK, Jean-Louis G, Ravenell J, Penesetti S, Favate A, Flores J, Henry KA, Kleiman A, Levine SR, Sinert R, Smith TY, Stern M, Valsamis H, Ogedegbe G. Comparative effectiveness of home blood pressure telemonitoring (HBPTM) plus nurse case management versus HBPTM alone among Black and Hispanic stroke survivors: study protocol for a randomized controlled trial. Trials 2015; 16:97. doi: 10.1186/s13063-015-0605-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Himmelfarb CR, Commodore-Mensah Y, Hill MN. Expanding the role of nurses to improve hypertension care and control globally. Ann Glob Health 2016; 82:243–253. [DOI] [PubMed] [Google Scholar]
- 86. Mejzner N, Clark CE, Smith LF, Campbell JL. Trends in the diagnosis and management of hypertension: repeated primary care survey in South West England. Br J Gen Pract 2017; 67:e306–e313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Courtenay M. Nurse prescribing and community practitioners. J Fam Health Care 2010; 20:78–80. [PubMed] [Google Scholar]
- 88. Centers for Disease Control and Prevention (CDC). Addressing Chronic Disease Through Community Health Workers: A Policy and Systems-Level Approach. Atlanta, GA, CDC Division for Heart Disease and Stroke Prevention. 2015. [Google Scholar]
- 89. Ibe CA, Hickman D, Cooper LA. To advance health equity during COVID-19 and beyond, elevate and support community health workers. JAMA Health Forum 2021; 2:e212724. [DOI] [PubMed] [Google Scholar]
- 90. World Health Organization(WHO). Community Health Workers: What Do We Know About Them?https://www.who.int/hrh/documents/community_health_workers.pdf. Accessed 6 December 2018.
- 91. Allen CG, Brownstein JN, Satsangi A, Escoffery C. Community health workers as allies in hypertension self-management and medication adherence in the United States, 2014. Prev Chronic Dis 2016; 13:E179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Dehmer SP, Baker-Goering MM, Maciosek MV, Hong Y, Kottke TE, Margolis KL, Will JC, Flottemesch TJ, LaFrance AB, Martinson BC, Thomas AJ, Roy K. Modeled health and economic impact of team-based care for hypertension. Am J Prev Med 2016; 50:S34–S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. McClellan MB, Bleser WK, Joynt Maddox KE. Advancing value-based cardiovascular care: the American Heart Association value in healthcare initiative. Circ Cardiovasc Qual Outcomes 2020; 13:e006610. [DOI] [PubMed] [Google Scholar]
- 94. Centers for Disease Control and Prevention. Community-Clinical Linkages for the Prevention and Control of Chronic Diseases: A Practitioner’s Guide. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2016. [Google Scholar]
- 95. Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities—addressing social needs through Medicare and Medicaid. N Engl J Med 2016; 374:8–11. [DOI] [PubMed] [Google Scholar]
- 96. Health Resources and Services Administration. FY 2021 Supplemental Funding for Hypertension (NCHI-HC). https://bphc.hrsa.gov/program-opportunities/national-hypertension-control-initiative. Accessed 4 August 2021.
- 97. Lu Y, Huang C, Mahajan S, Schulz WL, Nasir K, Spatz ES, Krumholz HM. Leveraging the electronic health records for population health: a case study of patients with markedly elevated blood pressure. J Am Heart Assoc 2020; 9:e015033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Office of Disease Prevention and Health Promotion. Healthy People 2030: Health Care. https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-care. Accessed 5 July 2021.
- 99. Frieden TR, Varghese CV, Kishore SP, Campbell NRC, Moran AE, Padwal R, Jaffe MG. Scaling up effective treatment of hypertension—a pathfinder for universal health coverage. J Clin Hypertens (Greenwich) 2019; 21:1442–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Chang TE, Ritchey MD, Park S, Chang A, Odom EC, Durthaler J, Jackson SL, Loustalot F. National rates of nonadherence to antihypertensive medications among insured adults with hypertension, 2015. Hypertension 2019; 74:1324–1332. [DOI] [PubMed] [Google Scholar]
- 101. Choudhry NK, Bykov K, Shrank WH, Toscano M, Rawlins WS, Reisman L, Brennan TA, Franklin JM. Eliminating medication copayments reduces disparities in cardiovascular care. Health Aff (Millwood) 2014; 33:863–870. [DOI] [PubMed] [Google Scholar]
- 102. Centers for Medicare and Medicaid Services. Medicare Advantage Value-Based Insurance Design Model. https://innovation.cms.gov/innovation-models/vbid. Accessed 4 July 2021.
- 103. Jones DW, Hall JE. The National High Blood Pressure Education Program: thirty years and counting. Hypertension 2002; 39:941–942. [DOI] [PubMed] [Google Scholar]
- 104. Commodore-Mensah Y, Selvin E, Aboagye J, Turkson-Ocran RA, Li X, Himmelfarb CD, Ahima RS, Cooper LA. Hypertension, overweight/obesity, and diabetes among immigrants in the United States: an analysis of the 2010–2016 National Health Interview Survey. BMC Public Health 2018; 18:773-018-5683-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Ahuja R, Ayala C, Tong X, Wall HK, Fang J. Public awareness of health-related risks from uncontrolled hypertension. Prev Chronic Dis 2018; 15:E40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Casey DE Jr, Daniel DM, Bhatt J, Carey RM, Commodore-Mensah Y, Holmes A, Smith AP, Wozniak G, Wright JT Jr. Controlling high blood pressure: an evidence-based blueprint for change. Am J Med Qual 2021. https://journals.lww.com/ajmqonline/Abstract/9000/Controlling_High_Blood_Pressure__An_Evidence_Based.99979.aspx [DOI] [PubMed] [Google Scholar]
- 107. Zhou D, Xi B, Zhao M, Wang L, Veeranki SP. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III Linked Mortality Study. Sci Rep 2018; 8:9418. 10.1038/s41598-018-27377-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. American Public Health Association. Racism is a Public Health Crisis. https://www.apha.org/topics-and-issues/health-equity/racism-and-health/racism-declarations. Accessed 17 October 2021.
- 109. Centers for Disease Control and Prevention (CDC). Racism and Health. https://www.cdc.gov/healthequity/racism-disparities/index.html. Accessed 17 October 2021.
- 110. National Institutes of Health. Ending Structural Racism. https://www.nih.gov/ending-structural-racism. Accessed 17 October 2021.