ABSTRACT
In the past 70 years, in order to strengthen disease prevention and improve people’s health, China had introduced a series of vaccine policies. However, compared with the permanent population, studies on the vaccination situation of the migrants were lacking. This study aimed to evaluate the vaccination rates of nine recommended vaccines (HepB, HepA, FIn, DTaP, JE, Rab, MPSV, HF, and TIG vaccine) among migrants and related determinants. We used nationwide data from the 2017 Migrant Population Dynamic Monitoring Survey (MDMS) to analyze the vaccination rates of migrants in terms of gender, age, marital status, household registration, education, health level, etc. The total vaccination rate of nine recommended vaccines was 64.8% (6488/10013). Education level and health level were positively correlated with vaccination rates, but age was negatively correlated with vaccination rates. Migrants from urban regions had a higher vaccination rate than those from rural regions. Among the nine recommended vaccines, HepB vaccination rate was the highest (59.08%), while HF vaccination rate was the lowest (4.08%). Combined with policies and demographic characteristics, the relationship between age, household registration, health level, education level and vaccination were studied. The findings suggested that more attention should be given to vaccination of migrants, and the monitoring of vaccination of such groups should be strengthened through information technology.
KEYWORDS: Migrants, vaccination rates, recommended vaccines, China
1. Introduction
Vaccination is considered to be an effective way to provide protection to public health.1,2 Since the founding of the People’s Republic of China, in order to promote the development and promotion of vaccines, the government has given much support to vaccine-related projects in various policies.3 Following the principle of “putting prevention first” since the 1950s, ways for the control of diseases have been carried out. Supplemental Table 1 showed some important vaccination policies in China from 1950 to 2021. Several essential policies were illustrated in the table. 1950 to 1965 was called the early stage of mass vaccination campaign period, in which smallpox vaccine was vigorously promoted. DT, JE, BCG, DTaP, IPV vaccination campaign were also carried out in this stage.4 Measures for the Implementation of Vaccination Work put forward more standardized requirements for vaccination. From 1966 to 1977, China entered the late stage of mass vaccination campaign stage, in which the variety and output of vaccines had been greatly improved. Further, barefoot doctors had laid a solid foundation for the realization of the vaccination service network in rural areas. The Notice on Strengthening Planned Immunization in 1978 announced the start of the immunization program period. Through this program, a number of infectious diseases harmful to the health had been brought under control. 2008 till now was called the age of the expanded national immunization program. In this period, the expanded programme of immunization (EPI) had been implemented in China, which was considered to be a national treasure that saved lives, prevented suffering, contributed to global health goals, and almost certainly lowered health care costs in the process. These policies have greatly reduced the incidence of diseases and improved the health of Chinese residents.5
According to the “China Migrants Development Report 2017,” there were 245 million migrants in 2016 in China, accounting for approximately 17.8% of the total population. Although the number of migrants was 1.71 million less than the previous year, the total number and its proportion in the total population were still very large.6 Therefore, we should pay great attention to this population. According to a previous study, compared with other permanent residents, immigrants had poorer health condition.7 There was a huge difference between the vaccination coverage rate of the migrants and the permanent population in China.8 Although Chinese government has established tons of policies to promote vaccination, the migrants’ vaccination situation was still worse than the entire population in China.
Many scholars have conducted researches on vaccination of migrants. They pointed out that the high incidence of some diseases was partly due to high population mobility and low vaccination rates among migrants.9 There was a low vaccine coverage in migrant populations along the Thailand-Myanmar Border.4 In Dalian, the coverage rate of the five vaccines (BCG, HepB, OPV, DTP and MV vaccine) for migrant children was significantly lower than that of local children.10 A delay was showed in the primary series vaccination especially among migrant children in Zhejiang province.11 In Guangdong, which is one of the provinces with the largest migrants, there was alarmingly low immunization coverage of migrant children.12 Even in Beijing, which was the capital of China, there was also a low age-appropriate immunization coverage of migrant children in densely populated areas.13 As to improve the vaccination rates, researchers suggested enhancing immunization informatization,5 giving greater support for vaccination of migrants and so on.14
We found that compared with the studies which focused on European countries,11 there was less research studying on the vaccination situation of the migrants in China. Moreover, the studies were mostly about the vaccination of migrant children, and lack of attention to the migrants who were or above 15 years old. Besides, the data used was concentrated in a certain region rather than national data, which lacked universality. In this study, we used 2017 MDMS survey data to analyze the vaccination situation of 10013 migrants nationwide and used logistic regression models to study the influencing factors of its vaccination situation. Likewise, we proposed relevant policy recommendations for increasing the vaccination rate of migrants.
2. Materials and methods
2.1. Data collection and study design
We used data from the 2017 MDMS Survey (Migrant Population Dynamic Monitoring Survey), a nationally representative demographic and health survey of migrant population conducted by National Health and Family Planning Commission of the People’s Republic of China (NHFPC). The target population of this study was Chinese internal migrants who were 15 years old or older in May 2017 and had spent more than one month at the destination cities.
The MDMS conducted a probability proportional to size (PPS) sampling method which was a stratified, multi-stage and proportional scale sampling.15 According to the principle of randomness, sample points were drawn from the inflow areas where the migrants were relatively concentrated in 31 provinces (autonomous regions and municipalities) and the Xinjiang Production and Construction Corps, and sample surveys were carried out to obtain the results of the survey. It was representative of the whole country and all provinces. At the same time, eight representative cities (states and districts) were selected to conduct a special survey on the essential infectious diseases of the *migrants.16–19
In terms of sample size, on the basis of maintaining the representativeness, this survey had enhanced the representativeness of major cities and equalization key contact cities. The provincial sample size was divided into 7 categories, which contained 10000, 8000, 7000, 6000, 5000, 4000, and 2000 people respectively. The total sample size of the survey was about 170000, involving about 450000 family members of the migrants. The special survey involved 14000 registered population. To select the sample, the investigators experienced three stages. The first stage was select townships (towns and streets) according to the PPS method and the next stage was select villages (residents) in the selected townships (towns and sub-districts). And the last one was selecting individual survey subjects from the selected village (neighborhood) committees.
2.2. Measures
In this survey, the basic population situation, basic public health services, community management and services, resources, and environmental conditions and so on were provided by people in the village committee or neighborhood committee. The other parts were completed by on-site investigators (including investigation instructors and investigators). All investigators need to participate in investigation training classes and receive special training. In addition, investigators need to complete the compilation of a roster of individual survey subjects, clarify the scope of the survey area they were responsible for, and conducted on-site inspections of the selected areas. This survey was conducted via mobile phones or pads, and publicity work, contact with the interviewees and appointment time should be done before the survey. All personnel in the survey should ask questions one by one in the order of the questionnaire, and go through self-examination by the investigator and inspection by the person in charge. After the survey, personnel should be organized to conduct quality checks to ensure the accuracy and scientificity of the answers to the questionnaire.
The data from the survey included: personal and family basic information, migration and mobility experience, social security status, medical and health services, marriage and childbirth, etc. Factors affecting the prevalence of essential diseases were added to the 2017 MDMS survey. Vaccination information which was the mainly studied in this paper were also provided.
2.2.1. Vaccination rates of recommended vaccines
The primary outcome in the present study was whether a migrant was vaccinated (yes/no). In this study, data which answer were “unclear” were dropped. The respondents were asked to answer the questions about vaccination in details, including nine recommended vaccines (HepB, HepA, FIn, DTaP, JE, Rab, MPSV, HF, and TIG vaccine). The answers reflected the vaccination information of the migrant workers. The vaccination rate was calculated by dividing the number of people vaccinated by the total number of people and multiplying by 100%.
2.2.2. Demographic characteristics
We used six demographic characteristics as independent variables: gender (male or female); age (≦30, 31–40, 41–50, >50); marital status (single, married, divorced or widowed); region (rural or urban); education (middle school or below, high school, three-year technical college, university or above); health status (healthy, almost healthy, unhealthy but can take care of himself or herself, or unhealthy and cannot take care of himself or herself).
2.3. Statistical analysis
We used Stata version 14.0 to conduct the statistical analyses. Descriptive statistical analysis, including frequency and percentage, was used to summarize and report demographic variables and the vaccination information.
We also used logistic regression to test the associations between demographic characteristics (gender, age, marital status, region, education and health status) and vaccination rates. Results from logistic regressions were presented as odds ratio (OR) and 95% confidence intervals (CI). A p < .05 was considered as statistical significance in all analyses.
To examine the robust of the results, we conducted a sensitivity analysis by fitting different models to examine the robustness of the results. Model 1 was a univariate model which contained no adjustment. In model 2, we adjusted for birth year instead of age group to test the impact of birth year on vaccination (Table 4).
Table 4.
Sensitivity analysis on determinants of vaccination using logistic regression, N = 10013(Model 2)
| Variables | Vaccination |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| HepB | HepA | FIn | DTaP | JE | Rab | MPSV | HF | TIG | |
| Gender (Female) | |||||||||
| Male | 1.05 (0.86–1.29) |
1.16 (0.92–1.47) |
1.08 (0.83–1.39) |
1.04 (0.75–1.44) |
0.90 (0.67–1.21) |
1.53** (1.12–2.08) |
1.11 (0.78–1.59) |
0.85 (0.49–1.07) |
1.85*** (1.38–2.50) |
| Birth year | 1.02*** (1.01–1.03) |
1.02** (1.00–1.03) |
1.02** (1.01–1.04) |
1.02 (1.00–1.03) |
1.01 (1.00–1.03) |
1.02 (1.00–1.03) |
1.01 (0.99–1.03) |
1.03 (1.00–1.07) |
1.01 (0.99–1.02) |
| Marital status (Single) | |||||||||
| Married/Having a relationship | 0.58*** (0.46–0.74) |
0.64** (0.49–0.83) |
0.62** (0.47–0.83) |
0.65* (0.45–0.93) |
0.71* (0.51–0.99) |
0.94 (0.66–1.34) |
0.72 (0.48–1.08) |
1.23 (0.62–2.44) |
0.84 (0.61–1.16) |
| Divorced/widowed | 0.75 (0.52–1.08) |
0.70 (0.47–1.06) |
0.62* (0.39–0.98) |
1.02 (0.60–1.74) |
0.87 (0.52–1.46) |
1.00 (0.59–1.72) |
1.12 (0.63–1.99) |
1.61 (0.61–4.20) |
0.92 (0.56–1.52) |
| Region(Rural) | |||||||||
| Urban | 0.95 (0.57–1.59) |
0.90 (0.48–1.69) |
1.26 (0.67–2.38) |
1.91 (0.94–3.89) |
1.54 (0.76–3.12) |
1.92* (1.01–3.64) |
0.78 (0.28–2.19) |
1.68 (0.50–5.65) |
1.33 (0.67–2.61) |
| Education(Middle school or below) | |||||||||
| High school | 1.23 (0.93–1.63) |
1.16 (0.84–1.62) |
1.55* (1.06–2.28) |
1.56 (0.95–2.57) |
1.00 (0.65–1.53) |
1.14 (0.73–1.79) |
1.32 (0.76–2.29) |
0.72 (0.31–1.68) |
0.91 (0.61–1.36) |
| Three-year technical college | 1.19 (0.90–1.57) |
1.16 (0.83–1.61) |
1.62* (1.11–2.35) |
1.75* (1.08–2.85) |
1.13 (0.74–1.71) |
1.30 (0.84–2.01) |
1.93* (1.15–3.24) |
0.96 (0.45–2.03) |
1.14 (0.77–1.68) |
| Bachelor degree or above | 1.76*** (1.28–2.43) |
1.24 (0.86–1.78) |
1.67* (1.11–2.52) |
1.79* (1.05–2.04) |
0.91 (0.56–1.47) |
1.48 (0.92–2.36) |
1.71 (0.96–3.06) |
0.72 (0.30–1.73) |
0.77 (0.48–1.23) |
| Health status(Healthy) | |||||||||
| Almost healthy | 0.90 (0.67–1.20) |
1.00 (0.71–1.41) |
1.18* (0.81–1.72) |
0.72 (0.42–1.24) |
0.56* (0.33–0.95) |
1.38 (0.91–2.10) |
0.84 (0.48–1.47) |
0.60 (0.21–1.71) |
0.86 (0.56–1.33) |
| Unhealthy, but can take care of himself/herself | 0.65 (0.30–1.37) |
0.75 (0.28–2.00) |
0.69 (0.20–2.36) |
0.38 (0.05–2.88) |
1.16 (0.39–3.42) |
- | 0.46 (0.06–3.49) |
- | 1.19 (0.44–3.20) |
| Unhealthy and cannot take care of himself/herself | - | - | - | - | - | - | - | - | - |
*p < .05, **p < .01, ***p < .001.
3. Results
3.1. Sample characteristics
The study sample contained 10013 migrants, including 4294 (42.88%) migrants under 31 years old, 3155 (31.51%) migrants between 31 and 40 years old, 1916 (19.14%) migrants between 41 and 50 years old and 648 (6.47%) migrants above 50 years old. Of the 10013 migrants with valid data, male and female respondents accounted for 50.14% and 49.86%. The majority respondents were married (including remarried or having a relationship) (75.28%) and most of the migrants were healthy when they were investigated (85.82%). More than 63% of migrants were from urban regions. Respondents who received middle school or below, high school, three-year technical college, university or above education took up for 21.41%, 27.08%, 29.44%, 22.06% respectively (Table 1).
Table 1.
Summary distribution of characteristics of migrants in China, N = 10013
| Variables | Level | N (%) | Vaccination N (%) |
|---|---|---|---|
| All | 10013(100%) | 6488 (64.8) | |
| Gender | Male | 5021(50.14) | 3254 (64.81) |
| Female | 4992(49.86) | 3234 (64.78) | |
| Age groups | ≤30 | 4294(42.88) | 2983 (69.47) |
| 31–40 | 3155(31.51) | 1986 (62.95) | |
| 41–50 | 1916(19.14) | 1183 (61.47) | |
| >50 | 648(6.47) | 336 (51.85) | |
| Marital status | Single | 2127(21.24) | 1613 (75.83) |
| Married/Having a relationship | 7538(75.28) | 4650 (61.69) | |
| Divorced/widowed | 348(3.48) | 225 (64.66) | |
| region | Rural | 3621(36.16) | 2139 (59.07) |
| Urban | 6392(63.84) | 4349 (68.04) | |
| Education | Middle school or below | 2144(21.41) | 1217 (56.76) |
| High school | 2712(27.08) | 1688 (62.24) | |
| Three-year technical college | 2948(29.44) | 1992 (67.57) | |
| University or above | 2209(22.06) | 1591 (72.02) | |
| Health status | Healthy | 8563(85.52) | 5573 (65.08) |
| Almost healthy | 1279(12.77) | 823 (64.35) | |
| Unhealthy, but can take care of himself/herself | 168(1.68) | 90 (53.57) | |
| Unhealthy and cannot take care of himself/herself | 3(0.03) | 2 (66.67) |
3.2. Vaccination rate of migrants
The proportion of migrants who reported had been vaccinated and had not been vaccinated was 64.8% (6488/10013) and 35.2% (3525/10013). In this study, people who did not know whether he/she had taken the vaccine were not calculated into the total sample (Table 1). The proportion of male and female migrants having taken vaccines was 64.81% (3254/5021) and 64.78% (3234/4992). The vaccination rate of people under 31 years old, single, urban region, bachelor’s degree or above were highest in each group, reporting 69.47% (2983/4294), 75.83% (1613/2127), 68.04% (4349/6392), 72.02% (1591/2209) respectively. In regard to the health status, the vaccination rate of people who were unhealthy and could not take care of himself or herself was 66.67%, which was the highest among this group. However, this health status group only had three respondents, therefore we chose the second highest group – healthy group as the group which reported the highest proportion 65.08% (5573/8563).
We divided the migrant population into 7 groups based on the birth year of: 1936–1946, 1947–1956, 1957–1966, 1967–1976, 1977–1986, 1987–1996, 1997–2006. The nine vaccination rates of HepB, HepA, FIn, DTaP, JE, Rab, MPSV, HF, and TIG were related to the birth year of the migrants to draw Figure 1. In addition, we also corresponded to Figure 1 the vaccination stage from 1950 to the present. In Table 1, we discussed key policies and the vaccines of different stages since 1950 (including the early stage of mass vaccination campaigns, the late stage of mass vaccination campaigns, the early stage of the immunization program, the late stage of the immunization program, the age of the expanded national immunization program) in detail. Compared with women, men were more likely to take HepA (25.71%), Rab (12.87%), TIG (15.61%) vaccine and less likely to take other 6 vaccines. In terms of age, young people had a higher vaccination rate than others. Interestingly, migrants who had not getting married or divorced or widowed had higher vaccination rates than those who were married or having a relationship. People whose regions were urban reported higher vaccination rates than others. Although the migrants who were unhealthy and could not take care of himself or herself reported the highest vaccination rates, due to the small sample in this group, we treated healthy people as those with the highest vaccination rates (Table 2).
Figure 1.
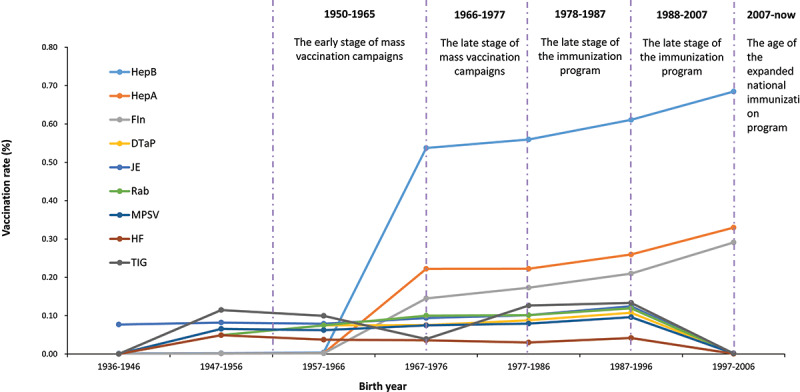
Vaccination rates of migrants by birth year and vaccination policies.
Table 2.
Numbers and proportion of different vaccination types of migrants, N = 10013
| Variables | Vaccination rate (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| HepB | HepA | FIn | DTaP | JE | Rab | MPSV | HF | TIG | |
| All | 5916(59.08) | 2535(25.32) | 2023(20.20) | 1059(10.58) | 1237(12.35) | 1138(11.37) | 943(9.42) | 409(4.08) | 1299 (12.97) |
| Gender | |||||||||
| Male | 2937(58.49) | 1291(25.71) | 997(19.86) | 502(10.00) | 608(12.11) | 646(12.87) | 455(9.06) | 198(3.94) | 784(15.61) |
| Female | 2979(59.68) | 1244(24.92) | 1026(20.55) | 557(11.16) | 629(12.60) | 492(9.86) | 488(9.78) | 211(4.23) | 515(10.32) |
| Age | |||||||||
| ≤30 | 2752(64.09) | 1246(29.02) | 1038(24.17) | 552(12.86) | 653(15.21) | 551(12.83) | 477(11.11) | 205(4.77) | 582(13.55) |
| 31–40 | 1825(57.84) | 732(23.20) | 576(18.26) | 301(9.54) | 345(10.94) | 349(11.06) | 274(8.68) | 118(3.74) | 413(13.09) |
| 41–50 | 1049(54.75) | 418(21.82) | 323(16.86) | 163(8.51) | 183(9.55) | 185(7.78) | 149(7.78) | 58(3.03) | 236(12.32) |
| >50 | 290(44.75) | 139(21.45) | 86(13.27) | 43(6.64) | 56(8.64) | 53(6.64) | 43(6.64) | 28(4.32) | 68(10.49) |
| Marital status | |||||||||
| Single | 1490(70.05) | 724(34.04) | 595(27.97) | 333(15.66) | 387(18.19) | 306(14.39) | 275(12.93) | 121(5.69) | 304(14.29) |
| Married/Having a relationship | 4216(55.93) | 1697(22.51) | 1345(17.84) | 680(9.02) | 799(10.60) | 790(10.48) | 629(8.34) | 265(3.52) | 945(12.54) |
| Divorced/widowed | 210(60.34) | 114(32.76) | 83(23.85) | 46(13.22) | 51(14.66) | 42(12.07) | 39(11.21) | 23(6.61) | 50(14.37) |
| Region | |||||||||
| Rural | 1936(53.47) | 770(21.26) | 666(18.39) | 366(10.11) | 436(12.04) | 404(11.16) | 306(8.45) | 143(3.95) | 475(13.12) |
| Urban | 3980(62.27) | 1765(27.61) | 1357(21.23) | 693(10.84) | 801(12.53) | 734(11.48) | 637(9.97) | 266(4.16) | 824(12.89) |
| Education | |||||||||
| Middle school or below | 1069(49.86) | 473(22.06) | 357(16.65) | 169(7.88) | 235(10.96) | 188(8.77) | 156(7.28) | 72(3.36) | 264(12.31) |
| High school | 1522(56.12) | 674(24.85) | 560(20.65) | 289(10.66) | 314(11.58) | 304(11.21) | 241(8.89) | 106(3.91) | 342(12.61) |
| Three-year technical college | 1818(61.67) | 769(26.09) | 624(21.17) | 329(11.16) | 377(12.79) | 361(12.25) | 302(10.24) | 127(4.31) | 399(13.53) |
| Bachelor degree or above | 1507(68.22) | 619(28.02) | 482(21.82) | 272(12.31) | 311(14.08) | 285(12.90) | 244(11.05) | 104(4.71) | 294(13.31) |
| Health status | |||||||||
| Healthy | 5106(59.63) | 2164(25.27) | 1743(20.36) | 915(10.69) | 1078(12.59) | 954(11.14) | 815(9.52) | 359(4.19) | 1087(12.69) |
| Almost healthy | 732(57.23) | 336(26.27) | 251(19.62) | 134(10.48) | 146(11.42) | 176(13.76) | 120(9.38) | 49(3.83) | 195(15.25) |
| Unhealthy, but can take care of himself/herself | 76(45.24) | 33(19.64) | 27(16.07) | 8(4.76) | 12(7.14) | 7(4.17) | 7(4.17) | 0(0.00) | 16(9.52) |
| Unhealthy and cannot take care of himself/herself | 2(66.67) | 2(66.67) | 2(66.67) | 2(66.67) | 1(33.33) | 1(33.33) | 1(33.33) | 1(33.33) | 1(33.33) |
3.3. Factors related to vaccination for migrants
In the multivariate logistic regression model (Table 3), gender, age, marital status, region, education, health status were associated with the vaccination of each vaccine. This model showed that male migrants had significantly higher odds of being vaccinated with HepA (OR: 0.10; 95%CI: −0.05–0.11), Rab (OR: 0.36; 95%CI: 0.23–0.49) and TIG (OR: 0.51; 95%CI: 0.39–0.63) vaccine. Compared with migrants whose age were or younger than 30, migrants age 50 or above were most likely to have been vaccinated. In this group, except for the HF vaccination, other vaccines all showed significantly higher odds. Migrants who were married or having a relationship reported significantly lower odds than those who were single in all vaccines except for TIG vaccine. Migrants from urban region reported significantly higher odds than others in HepB (OR: 0.25; 95%CI: 0.17–0.34), HepA (OR: 0.32; 95%CI: 0.22–0.42) and FIn (OR: 0.15; 95%CI: 0.15–0.46) vaccine. Migrants with higher education level had higher odds than those whose education level was middle school or below. Migrants with three-year technical college (OR: 0.25; 95%CI: 0.13–0.38) and bachelor’s degree or above (OR: 0.52, 95%CI: 0.56–0.66) showed significantly higher odds in HepB vaccine. In DTaP, Rab, MPSV vaccine, people with higher education level all showed varying degrees of higher odds. Almost healthy migrants had significantly higher odds of being vaccinated with Rab (OR: 0.35, 95%CI: −0.17–0.53) while migrants who were unhealthy but could take care of himself or herself showed lower odds (OR: −0.82; 95%CI: −1.59–0.06). Migrants who were unhealthy but could take care of himself or herself also reported significantly lower odds in HepB (OR: −0.33; 95%CI: −0.65–0.01), DTaP (OR: −0.66, 95%CI: −1.38–0.07), MPSV (OR: −0.71, 95%CI: −1.48–0.06). According to the sensitivity analysis, the results were robust in different models.
Table 3.
Determinants of vaccination using logistic regression, N = 10013
| Variables | Vaccination |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| HepB | HepA | FIn | DTaP | JE | Rab | MPSV | HF | TIG | |
| Gender (Female) | |||||||||
| Male | 0.03 (−0.05–0.11) |
0.10** (0.01–0.19) |
0.02 (−0.08–0.12) |
−0.06 (−0.19–0.07) |
0.01 (−0.11–0.14) |
0.36*** (0.23–0.49) |
−0.02 (−0.16–0.11) |
−0.03 (−0.23–0.18) |
0.51*** (0.39–0.63) |
| Age (≤30) | |||||||||
| 31–40 | −0.07 (−0.18–0.04) |
−0.17** (−0.29–0.04) |
−0.21** (−0.34–0.08) |
−0.12 (−0.29–0.05) |
−0.19** (−0.35–0.03) |
−0.09 (−0.25–0.08) |
−0.12 (−0.30–0.06) |
−0.08 (−0.35–0.19) |
−0.10 (−0.21–0.10) |
| 41–50 | −0.08 (−0.21–0.05) |
−0.25** (−0.39–0.09) |
−0.30*** (−0.46–0.14) |
−0.17 (−0.29–0.05) |
−0.32** (−0.52–0.11) |
−0.18* (−0.39–0.02) |
−0.17 (−0.40–0.05) |
−0.22 (−0.56–0.13) |
−0.13 (−0.33–0.05) |
| >50 | −0.42*** (−0.61–0.23) |
−0.29** (−0.51–0.06) |
−0.59*** (−0.85–0.33) |
−0.41** (−0.77–0.05) |
−0.43** (−0.75–0.11) |
−0.35** (−0.68–0.02) |
−0.30* (0.66–0.06) |
0.21 (−0.25–0.68) |
−0.35** (−0.65–0.06) |
| Marital status (Single) | |||||||||
| Married/Having a relationship | −0.46*** (−0.58–0.35) |
−0.43*** (−0.56–0.31) |
−0.40*** (−0.53–0.27) |
−0.49*** (−0.66–0.32) |
−0.47*** (−0.63–0.31) |
−0.27** (−0.44–0.10) |
−0.35*** (−0.53–0.17) |
−0.47** (−0.59–0.35) |
−0.11 (−0.28–0.05) |
| Divorced/widowed | −0.18 (−0.43–0.07) |
0.12 (−0.14–0.38) |
0.05 (−0.24–0.33) |
0.03 (−0.32–0.39) |
0.01 (−0.33–0.35) |
0.00 (−0.18–0.10) |
0.07 (−0.32–0.45) |
−0.18 (−0.43–0.07) |
−.12 (−0.23–0.46) |
| Region(Rural) | |||||||||
| Urban | 0.25*** (0.17–0.34) |
0.32*** (0.22–0.42) |
0.15** (0.04–0.26) |
−0.01 (−0.15–0.13) |
0.17 (−0.12–0.15) |
−0.05 (−0.18–0.09) |
0.12 (−0.04–0.26) |
0.26 (0.17–0.34) |
−0.04 (−0.17–0.09) |
| Education(Middle school or below) | |||||||||
| High school | 0.10* (−0.02–0.22) |
0.00 (−0.14–0.15) |
0.12 (−0.04–0.27) |
0.22** (0.01–0.43) |
−0.08 (−0.26–0.11) |
0.22* (0.02–0.42) |
0.10 (−0.12–0.32) |
0.10 (−0.02–0.22) |
0.00 (−0.17–0.19) |
| Three-year technical college | 0.25*** (0.13–0.38) |
−0.01 (−0.16–0.13) |
0.06 (−0.10–0.21) |
0.20* (−0.01–0.41) |
−0.05 (−0.24–0.14) |
0.30** (0.10–0.51) |
0.19* (−0.03–0.41) |
0.25 (0.13–0.38) |
0.10 (−0.09–0.28) |
| Bachelor degree or above | 0.52*** (0.38–0.66) |
0.06 (−0.10–0.22) |
0.07 (−0.10–0.24) |
0.31** (0.08–0.54) |
0.05 (−0.15–0.26) |
0.37** (0.15–0.58) |
0.26** (0.02–0.50) |
0.52 (0.38–0.66) |
0.08 (−0.12–0.28) |
| Health status(Healthy) | |||||||||
| Almost healthy | 0.01 (−0.12–0.13) |
0.12* (−0.02–0.26) |
0.07 (−0.08–0.22) |
0.09 (−0.10–0.29) |
0.00 (−0.19–0.19) |
0.35*** (−0.17–0.53) |
0.07 (−0.14–0.28) |
0.00 (−0.11–0.13) |
0.28** (0.11–0.45) |
| Unhealthy, but can take care of himself/herself | −0.33** (−0.65–0.01) |
−0.26 (−0.66–0.13) |
−0.10 (−0.53–0.33) |
−0.66* (−1.38–0.07) |
−0.50 (−1.10–0.11) |
−0.82** (−1.59–0.06) |
−0.71** (−1.48–0.06) |
−0.33 (−0.65–0.01) |
−0.21 (−0.74–0.32) |
| Unhealthy and cannot take care of himself/herself | −.31 (−2.15–2.76) |
1.52 (−0.91–3.95) |
2.03 (−0.43–4.49) |
2.93** (0.46–5.39) |
1.12 (−1.32–3.56) |
1.35 (−1.08–3.78) |
1.57 (−0.86–4.00) |
0.31* (−2.15–2.76) |
1.10 (−1.32–3.51) |
*p < .05, **p < .01, ***p < .001.
4. Discussion
Our study estimated the number and proportion of migrants who had taken HepB, HepA, FIn, DTaP, JE, Rab, MPSV, HF and TIG vaccine in China. From the results, the vaccination rate of the migrants in this survey was lower than the vaccination rate of the entire population at the same stage, lower than the national immunization program’s target which was 85% and some scholars had conducted study in this field. For instance, Liu et al. analyzed the vaccination rate of resident children and floating children in Beijing, and found that the vaccination rate of the floating population was 15% lower than that of the permanent population in terms of BCG, HepB, OPV, DPT, and MV vaccine.20 At the same time, according to existing research, the vaccination rate of the entire population of migrants was close to or lower than that of floating children during the same period or before,21 which was associated with different immunization policies at different periods. Most migrants (64.8%) had been vaccinated and HepB vaccine was been vaccinated most (59.08%), far below the 85% vaccination rate requirement of the target population immunization program. Migrants been vaccinated with other vaccines were less than the HepB vaccination, and the HF vaccine was been vaccinated least (4.08%).
Demographic characteristics would influence the vaccination rate of migrants. In general, there was almost no difference between male (64.81%) and female (64.78%) vaccination rates. The vaccination rate would decrease with age (from 69.47% to 51.85%). The vaccination rate of migrants who were not single (61.69%) was lower than that of single (75.83%) or divorced/widowed (64.66%) people. The vaccination rate of migrants from urban region (68.04%) was slightly higher than others (59.07%). The higher level of education, the higher possibility of vaccination. At the same time, health status and vaccination rates were also positively correlated.
The strong association between vaccination rates and age, marital status, region, education, health status were consistent with previous research.12,13,15 From the perspective of age, the negative correlation between age and vaccination was likely to be related to policies. According to the time when this survey took place, people under 30 were born after 1987. At this time, the planned immunization program had been carried out for nearly 10 years and had achieved certain results. And since China launched the national basic public health service project in 2009, vaccination had become an important part of the project, and it had received more support and guidance. The project establishes health files for residents, which could detect the health status of the entire population in time, and the management of migrants was becoming more standardized. At the same time, with the continuous development of China, people’s awareness of disease prevention had improved, and people were becoming more aware of the importance of vaccination. Those over the age of 50, were born before 1967, which was the early stage of planned immunization, and the vaccination work had not been standardized and perfected yet.
In terms of household registration, the vaccination rate of migrants from urban regions was generally higher than that from rural region. There was a certain relationship between the management of health service personnel and better medical and health conditions in urban areas. From the perspective of education level, the higher the educated group’s vaccination rate was higher, which was closely related to the important part of health education in school education. The more educated migrants had the higher the level of understanding of vaccines which had beneficial effects on human health, and thus made better decisions on vaccination. However, there was also the possibility that the parents of the more educated group had relatively higher education and economic levels, so they would be vaccinated during their childhood. Because this survey didn’t contain parents’ education level, economic status and other variables, it could not control the influence of parents’ factors. From the perspective of health level, the vaccination situation of healthy migrants was better than that of people who were almost healthy or unhealthy but able to take care of themselves. However, because vaccination might also have an impact on health, the causal relationship could not be evaluated by the model of this article.
It was gratifying that the General Office of the National Health and Family Planning Commission issued the “Equalization of Basic Public Health and Family Planning Services for Migrants” in 2017, requiring that the vaccination rate of the migrants be included in the basic public health and family planning services for the migrant’s equalization work evaluation index system. In the future, more attention should be given to the vaccination of migrants and the government is supposed to give this group more policy support through basic public health services, information technology, etc.
Our study has certain limitations. Firstly, because this data was second handed, much basic information could only be obtained based on the questions in the original survey. There were several factors related to the vaccination rates (such as occupation, household income, knowledge about vaccines and the willingness of others to vaccinate) which were not available just from this survey. Secondly, because the study was conducted out in 2017, the data might not represent the current practice patterns. For example, during the five years, the population had changed and some policies about migrants also altered, which would influence the vaccination situation. Thirdly, there might be a reverse causal relationship between the factors involved in this article and the vaccination rates. For example, the vaccination situation may affect the health of the migrants, yet we did not analyze this during the research process.
5. Conclusion
We studied the vaccination situation of the migrants and related influencing factors, including gender, age, marital status, region, education and health status. Because of the universality and enforcement of vaccination, more attention should be given to the vaccination situation of the migrants. We think that in the process of formulating policies, the government should give more consideration and more policy support to the special circumstances of the migrants. At the same time, the publicity and education of vaccination should be strengthened to enhance the vaccination awareness of the migrants.
Supplementary Material
Funding Statement
This work was funded by the National Natural Science Foundation of China [grant number 72042002, 71934002, 72122001, 72061160491]; The National Science and Technology Key Projects on Prevention and Treatment of Major infectious disease of China [grant number 2020ZX10001002]; The National Key Research and Development Project of China [grant numbers 2020YFC0846300, 2019YFC1710301].
Author contributions
Conceptualization, J.W. J.Z., Y.B., and J.L.; methodology, J.W. and J.L.; software, Y.B.; validation, J.W. J.Z., Y.B., X.W., Y.C. and J.L.; formal analysis, Y.B.; data curation, Y.B. and J.L.; writing—original draft preparation, J.W., J.Z. Y.B. and J.L.; writing—review and editing, J.W. J.Z., Y.B., X.W., Y.C., and J.L.; visualization, Y.B.; supervision, Y.B. J.L.; funding acquisition, J.W. and J.L. All authors have read and agreed to the final version of the manuscript.
Data availability statement
Data are available from the corresponding author by request https://www.ncmi.cn/phda/dataDetails.do?id=CSTR:A0006.11.A000T.201906.000225.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2021.1981088.
References
- 1.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P.. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150–59. PMID: 24598724. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 2.Crowcroft NS, Stein C, Duclos P, Birmingham M.. How best to estimate the global burden of pertussis? Lancet Infect Dis. 2003;3(7):413–18. PMID: 12837346. doi: 10.1016/s1473-3099(03)00669-8. [DOI] [PubMed] [Google Scholar]
- 3.Nan W, Ling T, Wuqi Q. Review of vaccine-related policies in the 60 years since the founding of the People’s Republic of China. J Med Res. 2010;39(8):21–23. doi: 10.3969/j.1673-548X.2010.08.006. [DOI] [Google Scholar]
- 4.Kaji A, Parker DM, Chu CS, Thayatkawin W, Suelaor J, Charatrueangrongkun R, Salathibuppha K, Nosten FH, McGready R. Immunization coverage in migrant school children along the Thailand-Myanmar border. J Immigr Minor Health. 2016;18(5):1038–45. PMID: 26483180. doi: 10.1007/s10903-015-0294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hao L, Glasser JW, Su Q, Ma C, Feng Z, Yin Z, Goodson JL, Wen N, Fan C, Yang H, et al. Evaluating vaccination policies to accelerate measles elimination in China: a meta-population modelling study. Int J Epidemiol. 2019;48(4):1385. PMID: 31056644. doi: 10.1093/ije/dyz103. [DOI] [PubMed] [Google Scholar]
- 6.National Health and Family Planning Commission of the People’s Republic of China . China Migrants Development Report. China Population Press; 2016. [Google Scholar]
- 7.Wang W, Chen R, Ma Y, Sun X, Qin X, Hu Z. The impact of social organizations on HIV/AIDS prevention knowledge among migrants in Hefei, China. Global Health. 2018;14(1):41. PMID: 29695304. doi: 10.1186/s12992-018-0359-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, Remais JV. Urbanisation and health in China. Lancet. 2012;379(9818):843–52. PMID: 22386037. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hu X, Xiao S, Chen B, Sa Z. Gaps in the 2010 measles SIA coverage among migrant children in Beijing: evidence from a parental survey. Vaccine. 2012;30(39):5721–25. PMID: 22819988. doi: 10.1016/j.vaccine.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Xiuyan J, Wen W, Yinan H, Mei Z, Qian L, Wenbin L, Ying P, Shiwei M, Bin W. Study on the immunization situation of 5 vaccines to the children living in migrant population gathering area in Dalian city. Chin J Vaccines Immunization. 2008;14(6):546–48. doi: 10.3969/j.1006-916X.2008.06.017. [DOI] [Google Scholar]
- 11.Hargreaves S, Nellums LB, Ramsay M, Saliba V, Majeed A, Mounier-Jack S, Friedland JS. Who is responsible for the vaccination of migrants in Europe? Lancet. 2018;391(10132):1752–54. PMID: 29739550. doi: 10.1016/S0140-6736(18)30846-8. [DOI] [PubMed] [Google Scholar]
- 12.Han K, Zheng H, Huang Z, Qiu Q, Zeng H, Chen B, Xu J. Vaccination coverage and its determinants among migrant children in Guangdong, China. BMC Public Health. 2014;14:203. PMID: 24568184. doi: 10.1186/1471-2458-14-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun M, Ma R, Zeng Y, Luo F, Zhang J, Hou W. Immunization status and risk factors of migrant children in densely populated areas of Beijing, China. Vaccine. 2010;28(5):1264–74. PMID: 19941996. doi: 10.1016/j.vaccine.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 14.Chen J. Internal migration and health: re-examining the healthy migrant phenomenon in China. Soc Sci Med. 2011;72(8):1294–301. PMID: 21435765. doi: 10.1016/j.socscimed.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Zhu Z, Guo M, Petrovsky DV, Dong T, Hu Y, Wu B. Age and regional disparity in HIV education among migrants in China: migrants population dynamic monitoring survey, 2014-2015. Int J Equity Health. 2019;18(1):104. PMID: 31269954. doi: 10.1186/s12939-019-0999-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) . Progress in hepatitis B prevention through universal infant vaccination–China, 1997-2006. MMWR Morb Mortal Wkly Rep. 2007;56(18):441–45. PMID: 17495790. [PubMed] [Google Scholar]
- 17.Wang Q, Yue N, Zheng M, Wang D, Duan C, Yu X, Zhang X, Bao C, Jin H. Influenza vaccination coverage of population and the factors influencing influenza vaccination in mainland China: a meta-analysis. Vaccine. 2018;36(48):7262–69. PMID: 30340886. doi: 10.1016/j.vaccine.2018.10.045. [DOI] [PubMed] [Google Scholar]
- 18.Sonder GJ, Bovée LP, Baayen TD, Coutinho RA, van den Hoek JA. Effectiveness of a hepatitis A vaccination program for migrant children in Amsterdam, The Netherlands (1992-2004). Vaccine. 2006;24(23):4962–68. PMID: 16675076. doi: 10.1016/j.vaccine.2006.03.075. [DOI] [PubMed] [Google Scholar]
- 19.Etana B, Deressa W. Factors associated with complete immunization coverage in children aged 12-23 months in Ambo Woreda, Central Ethiopia. BMC Public Health. 2012;12:566. PMID: 22839418. doi: 10.1186/1471-2458-12-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meiping S, Dawei L, Aihua L, Donglei L, Chenyang F, Liang M, Li L, Xuechun Z. Investigation of immunization coverage rate of children living in floating population area and the affecting factors. Chin J Vaccines Immunization. 2002;8(2):91–94. doi: 10.3969/j.1006-916X.2002.02.011. [DOI] [Google Scholar]
- 21.Dawei L, Meiping S, Weixiang L, Chenyang F, Li L, Donglei L, Yang Z, Lingyun W, Xuechun Z. Comparative study on immunization coverage rates of nine vaccines between local and floating children. Chin J Vaccines Immunization. 2007;13(2):165–69. doi: 10.3969/j.1006-916X.2007.02.017. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available from the corresponding author by request https://www.ncmi.cn/phda/dataDetails.do?id=CSTR:A0006.11.A000T.201906.000225.


