ABSTRACT
Vaccination for the novel coronavirus disease 2019 (COVID-19) provides an effective approach for the general improvement of social safety and individual health. However, given that the current COVID-19 vaccine can only work for a period of time, the continuous vaccination of the vaccine will be particularly important. Using the Health Action Process Approach (HAPA) Model, Expectation Confirmation Model (ECM) and vaccine hesitancy (VH) theory, this research evaluates the continuous vaccination for COVID-19. This research selected Chinese survey platform to recruit respondents and conducted online surveys. A total of 768 Chinese individuals who were vaccinated participated in the survey, and 561 responses were effective after screening. Six valuable and novel findings are identified through this research. First, perceived efficacy has a positive significant impact on vaccination intention, but the positive effects of outcome expectancy and risk perception on vaccination intention are not significant. Second, social positive cues play a significant role in promoting vaccination intention. Third, VH has a negative significant influence on vaccination intention. Fourth, vaccination behavior produces a positive significant effect on perceived usefulness and satisfaction, respectively. Fifth, perceived usefulness exerted a positive significant impact on satisfaction and continuous vaccination, respectively. Sixth, satisfaction has no positive significant influence on continuous vaccination. Our theoretical model, which is the main contribution of this research, indicates that individual continuous vaccination is a process from motivation to intention, and from intention to behavior, and then from behavior to continuous vaccination.
KEYWORDS: Novel coronavirus disease 2019 (COVID-19), continuous vaccination, vaccination intention, vaccine hesitancy (VH), structural equation modeling (SEM)
Introduction
At the end of 2019, the novel coronavirus disease 2019 (COVID-19) broke out in the form of a pandemic, and the rapid onset of this disease has brought with it considerable challenges for many or all countries in the world (including challenges in political, economic, social, and security sectors).1 Nowadays, more and more countries are developing COVID-19 vaccines to prevent the epidemic.2 For example, the United States of America started vaccinations on December 15, 2020. As of October 16, 2021, 65% of Americans are completely vaccinated.3 By the end of 2020, the 27 countries of the European Union had begun vaccinations. As of October 16, 2021, the vaccination rates in Spain and Portugal have exceeded 80%.3 China began implementing COVID-19 vaccinations at the end of 2020, so that by October 16, 2021, the proportion of Chinese completely vaccinated has reached 76%.3 Currently, governments around the world still believe that the COVID-19 vaccine will prove an effective means of preventing the epidemic.
Although various countries are actively carrying out COVID-19 vaccinations, it is undeniable that the COVID-19 vaccines developed at this stage usually have an expiration date.4 In other words, COVID-19 vaccines will expire after a period of time and will no longer protect the public who have been vaccinated. At this time, if countries around the world still cannot identify a better approach to preventing the virus, people will have to vaccinate again in order to protect themselves. More importantly, it is reported that COVID-19 can mutate under certain circumstances.5 In this case, individuals also need to be vaccinated against this ever-changing virus. Therefore, continuous vaccination will become an inevitable task. In order to do this well, governments around the world have to consider the following critical question:
RQ: what factors will affect the continuous vaccination of COVID-19 vaccine?
Until the current day, studies on COVID-19 vaccination have mainly focused on the intention,6 hesitancy,7 acceptance,8 and other issues. There exist few empirical studies that analyze continuous vaccination, however, continuous vaccination may still be one of the most effective governmental measures for monitoring and controlling macro-level population health problems in the future. It has a positive effect on national security, personal health, and personal travel safety. Due to the shortcomings of existing studies, it is necessary to analyze the continuous vaccination for COVID-19 using empirical data. By way of this research, policy makers and government officials can not only learn of the public’s continuous vaccination process, but also determine which factors most significantly affect continuous vaccination. The insights of this research enrich the fields of emergency management, clinical medicine, and public health. Furthermore, this research has valuable practical implications for governments and decision-making departments to optimize the public’s continuous vaccination and innovate the safety system of vaccination.
In this study, we explore the key factors of citizens’ continuous vaccination and analyze the process and effect of these factors on continuous vaccination. In the case of COVID-19, we consider the public’s continuous vaccination to be a three-stage response process as follows: motivation, -intention, and -behavior. In other words, this process goes from psychological perception to behavioral intention and then from behavioral intention to actual behavior. To explore this response process, we constructs a theoretical model to analyze the entire impact process of continuous vaccination based on the Health Action Process Approach (HAPA) Model, the Expectation Confirmation Model (ECM) and the vaccine hesitancy (VH) theory. Then, we empirically evaluate the direct and indirect effects of factors at every stage of the continuous vaccination process. As a theoretical contribution of this research, the theoretical model can be used to evaluate continuous vaccination for COVID-19. It can not only reflect the response process of the public’s continuous vaccination, but also prove which factors can produce a significant effect on the public’s continuous vaccination.
Theoretical background and research hypotheses
HAPA model
The HAPA model divides human health behavior into three stages: pre-intention stage, intention stage, and action stage.9 Specifically, the pre-intention stage means that the individuals are aware of the danger of not taking a certain health behavior and firmly believe that they have the ability to take this behavior, so as to form the behavior intention.9 The intention stage reflects the individuals belief that they can deal with various obstacles when taking some behavior then promote them to make a behavior plan and try to do so.9 The action stage indicates actions produced by the individuals under the regulation of self-efficacy, as well as the withdrawal, maintenance, and recovery of this action.9 In the present study, we used the components and variables from the HAPA model and designed a theoretical model that has three stages in sequence: motivation, intention, and behavior. In the motivation stage, we evaluate individuals’ perceptions of the harms of unhealthy behaviors related to COVID-19 and assess whether they are capable of taking on healthy behaviors.10 This stage includes three variables: risk perception, perceived self-efficacy, and outcome expectancy. The intention stage is to measure the subjective intention of the individual to adopt the COVID-19 vaccine,11 including the vaccination intention, social positive cues, and VH. The third stage of the model is the behavior stage, which is used to reflect the actual behavior of individual vaccination.11 This stage holds four variables: vaccination behavior, perceived usefulness, satisfaction, and continuous vaccination.
ECM
The ECM was originally designed to understand consumers’ purchase behaviors.12 According to this model, whether consumers buy the same product again depends on the consumers’ satisfaction with the purchased product, and this satisfaction is the difference between the expected benefit of the product before the purchase and the actual benefit after the purchase.13 In this study, we believe that the ECM can be used to explain the continuous vaccination of the COVID-19 vaccine. The main reason is that the process of individual formation of continuous vaccination is similar to the process in ECM. Specifically, after an individual is vaccinated for the first time, an initial expectation of the COVID-19 vaccine and vaccination will be formed. Secondly, after a period of experience and evaluation, the individual will develop various feelings about the COVID-19 vaccine and vaccination. Finally, an individual with positive feelings will have the vaccination behavior again, while others with negative feelings will stop subsequent vaccinations.
VH theory
VH refers to a delay in acceptance or refusal of vaccination despite availability of vaccination services.14 In 2019, the World Health Organization (WHO) listed VH as one of the top 10 threats to global health.15 VH is a complex phenomenon and varies with place, time, and vaccines. According to the VH theory, VH can affect the individual’s acceptance of vaccination, which directly leads to the reduction of vaccination coverage and population immunity.16 It could hinder the complete implementation of the immunization program and increase the risk of preventable disease outbreaks and epidemics.17 Since the COVID-19 vaccine was developed as recently as 2020, some questions about its side effects, efficacy, and rigorousness are still being raised by the public, which will lead to VH. Based on Quinn’s research (2019),18 we use three second-order factors of complacency, convenience, and confidence to measure VH.
Impacts of motivation stage on intention stage
According to the HAPA model, for health behavior, the individual expects to maximize its positive outcomes and minimize its negative outcomes.19 Currently, many studies have shown that positive outcome is expected to predict behavior intention.20 In the context of COVID-19, vaccination intention is an effective health protection behavior intention. In this sense, the positive outcome of this behavior is obvious. Therefore, we propose the following hypothesis:
H1: Outcome expectancy has a positive significant impact on vaccination intention.
According to the research of Bhattacherjee and Shrivastava (2018),21 when individuals implement a certain behavior, they often fail to implement or terminate the implementation due to perceived risks. When individuals subjectively believe that the risk and cost of this behavior are high, their willingness to implement it will be greatly reduced.22 Currently, the side effects, efficacy, rigorousness, and other issues of the COVID-19 vaccine have not eliminated individuals’ doubts about its risks. Therefore, we propose the following hypothesi:s
H2: Risk perception has a negative significant impact on vaccination intention.
In addition, several recent studies have indicated that an individual’s perceived self-efficacy can positively influence behavior intention.23 In the context of COVID-19, vaccination is an effective way to protect health. Therefore, individuals’ perceived self-efficacy on the positive outcome of this behavior can stimulate their vaccination intention. Therefore, we propose the following hypothesis:
H3: Perceived self-efficacy has a positive significant impact on vaccination intention.
Impacts of intention stage on behavior stage
Previous studies have demonstrated that social positive cues have a significant positive impact on an individual’s behavioral intentions.24,25 In the context of COVID-19, the doctor’s recommendations and vaccination reports are social positive cues to vaccine adoption. In accordance with the findings of existing research, we argue that social positive cues can motivate the public to vaccinate and to promote behavioral intention conducive to vaccination. Therefore, we propose the following hypothesis:
H4: Social positive cues play a significant role in promoting vaccination intention.
VH theory believes that VH is a comprehensive manifestation of individual gender, age, culture, religious beliefs, and other factors.26 At present, studies have shown that VH has a negative significant effect on behavior intention.18,27 In the context of COVID-19, Sallam et al.26 indicated that VH was related to the COVID-19 vaccination. The similar finding was also confirmed by the research of Kwok et al.6 Therefore, based on the above argument, we propose the following hypothesis:
H5: VH has a negative significant impact on vaccination intention.
The HAPA model proves that intention has a positive significant impact on behavior.9 The positive impact of intention on behavior can be supported by other classic theories and models, such as the Theory of Planned Behavior.28 In terms of vaccination, we also believe that vaccination intention can positively affect vaccination behavior. Therefore, we propose the following hypothesis:
H6: Vaccination intention has a positive significant impact on vaccination behavior.
Impacts in the behavior stage
In the ECM, confirmation can have a direct impact on perceived usefulness and satisfaction.12 Moreover, many previous studies have also verified that confirmation can positively affect perceived usefulness and satisfaction.29,30 The actual behavior can achieve the comparison of individual expectations and experiences, and it is a process by which individual expectations are confirmed in the actual process.31 We believe that this argument can also be applied to COVID-19. Therefore, we propose the following hypotheses:
H7: Vaccination behavior has a positive significant impact on perceived usefulness.
H8: Vaccination behavior has a positive significant impact on satisfaction.
Bhattacherjee et al.32 believed that perceived usefulness was regarded as a degree of utilitarianism to improve work performance, which was a long-term belief that combined expectations. According to this point of view, perceived usefulness is the decisive factor influencing individual emotions and subsequent behaviors. At present, most studies have demonstrated that perceived usefulness has a direct impact on individual satisfaction and continuous behaviors.33,34 Therefore, we propose the following hypotheses:
H9: Perceived usefulness has a positive significant impact on satisfaction.
H10: Perceived usefulness has a positive significant impact on continuous vaccination.
The ECM believes that satisfaction is an important variable for predicting continued use intentions and behaviors.12 Many scholars, working in various fields, have proven that satisfaction has a positive effect on continued use intentions and behaviors.29,35 The more satisfied the public is with vaccination, the more they tend to continue vaccination. Therefore, we propose the following hypothesis:
H11: Satisfaction has a positive significant impact on continuous vaccination.
In view of the above hypotheses, we construct the theoretical model of this study in Figure 1.
Figure 1.
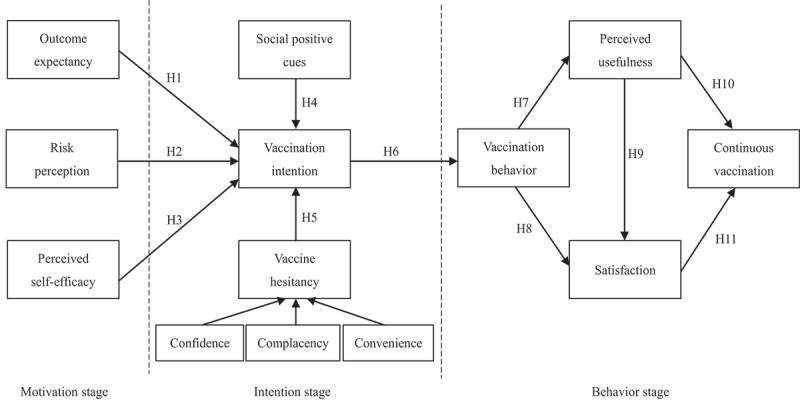
Research model.
Legend: In the case of COVID-19, public responses proceed as follows: motivation, -intention, and -behavior. This process goes from psychological perception to behavioral intention and then from behavioral intention to actual behavior.
Methodology
We selected as subject citizens of China who have been vaccinated; this was due to three reasons. First, China has been studying the COVID-19 vaccine since March 2020. In June 2020, the country started its first clinical trial of the COVID-19 vaccine. In addition, China officially joined the COVID-19 Vaccine Global Access in October 2020 and began administering COVID-19 vaccinations at the end of 2020.3 In this sense, China was one of the world’s leading countries in the development of the COVID-19 vaccine; therefore, we expected to obtain high-quality data from this country. Second, as of July 7, 2021, the number of COVID-19 vaccinations in China has exceeded 1.32 billion doses,3 making data collection in this country optimal for obtaining sufficient and effective samples. Third, the Chinese government adopted the principle of voluntary rather than compulsory vaccination during the process of COVID-19 vaccinations. Each Chinese citizen can choose whether or not to vaccinate according to his or her preferences; in this respect, the policy environment of China meets the basic requirements for continuous vaccination as outlined in this research.
Measures
In this study, we designed 32 measurement items to measure the 12 variables in the theoretical model. The scale was designed as a 7-point Likert scale. In the Likert scale, the respondents needed to express their opinions on items related to all variables. For all the response options, “1” represented strongly disagreement, “2” was somewhat disagreement, “3” indicated disagreement, “4” meant neutral, “5” indicated agreement, “6” was somewhat agreement and “7” denoted strongly agreement. All variables and their items are shown in Table 1. The content of each item was designed with reference to prior valid measures. We refined the survey contents of the scale to obtain high-quality data. Throughout the investigation, all items were conducted in Chinese.
Table 1.
Specific measurement items of the scale
| Variables | Items | References | |
|---|---|---|---|
| Outcome expectancy (OE) | OE1: If I get vaccinated, I will feel healthier. | 36 | |
| OE2: If I get vaccinated, I will feel better mentally. | |||
| OE3: If I get vaccinated, I will have fewer health problems. | |||
| Risk perception (RP) | RP1: I am concerned about the vaccine efficacy. | 37 | |
| RP2: I am concerned about the vaccine side effects. | |||
| RP3: I am concerned about the vaccine rigor of testing. | |||
| RP4: I am concerned that I may be allergic to the vaccine. | |||
| Perceived self-efficacy (PS) | PS1: I am certain that I can get vaccinated, even if I have to mobilize myself. | 9 | |
| PS2: I am certain that I can get vaccinated, even if it is difficult. | |||
| Social positive cues (SPC) | SPC1: I will get vaccinated when the doctor recommends it. | 37 | |
| SPC2: I will get vaccinated when vaccination becomes popular. | |||
| SPC3: I will get vaccinated when I know enough about vaccine. | |||
| Vaccine hesitancy (VH) | Confidence (CF) | CF1: I think the vaccine is not safe. | 18 |
| CF2: I think the vaccine is not effective. | |||
| Complacency (CP) | CP1: I think the vaccine is not important. | ||
| CP2: I think the vaccine is not necessary. | |||
| Convenience (CV) | CV1: I think the vaccine is not convenient. | ||
| CV2: I think the vaccine is not free. | |||
| Vaccination intention (VI) | VI1: I intend to get all doses of the vaccine during the vaccination period. | 38 | |
| VI2: I will try to get all doses of the vaccine during the vaccination period. | |||
| VI3: I plan to get all doses of the vaccine during the vaccination period. | |||
| Vaccination behavior (VB) | VB1: I often get vaccinated during the vaccination period. | 39 | |
| VB2: I get all doses of the vaccine during the vaccination period. | |||
| Satisfactory (SAT) | SAT1: Overall, I am satisfied with the vaccine. | 40 | |
| SAT2: The vaccine I am currently getting meets my expectations. | |||
| SAT3: I am very pleased with my experience with getting vaccinated. | |||
| Continuous vaccination (CVN) | CVN1: I am likely to continue to get vaccinated in the future. | 40 | |
| CVN2: I intend to consistently get vaccinated in the future. | |||
| CVN3: I intend to continue getting vaccinated rather than discontinue the vaccine. | |||
| Perceived usefulness (PU) | PU1: I think that vaccine is useful for my life. | 40 | |
| PU2: Getting vaccinated improves my health. | |||
| PU3: Getting vaccinated helps me conveniently perform many tasks. | |||
Data collection
A pilot survey was deployed to evaluate whether the scale was suitable for studying continuous vaccination. 30 individuals participated in this pilot survey. The survey results showed that the items were easy to understand and highly related to the survey topics. However, we found that there was a large proportion of missing values in some personal attributes of the respondents, such as income, workplace, and nature of workplace. Therefore, due to the effects of missing values, we used only “gender,” “age,” “education” and “province” as survey variables and did not set income and other variables in our investigation of personal attribute information.
Given the feasibility and practical operability of formal investigation, we posted our questionnaires on the Sojump website (http://www.sojump.com/), a specialized online survey system in China similar to Qualtrics.com or SurveyMonkey.com in the United States. An advertisement for the survey was posted for one week on public forums. During the investigation, we used an open invitation as our recruiting method. The scale randomly popped up on the Sojump website. We selected registered members of Sojump as our target population. The website currently has over 60 million registered members who are located in various provinces across China. When invited to participate in the survey, members were provided with three options, “participate now,” “maybe next time,” or “do not ask again.” There was no loss of benefit in case a member chose not to participate. Participation in the survey was totally voluntary, and anonymity was ensured by configuring the survey application to disregard any respondent’s identifying information. To improve the quality of our data, we paid U.S. $ 0.8 for each respondent to participate. To protect respondents’ privacy, “gender” and “province” were set as the nominal variables, while “age” and “education” were set as ordinal variables. The entire investigation period lasted one month (from May 10, 2021, to June 9, 2021). In total, 768 members participated in the study. We applied the following screening item: Have you been vaccinated? Respondents who had not been vaccinated were not used as research samples. In addition, when screening the questionnaires, we deleted some samples of responses that were obviously unreasonable. Moreover, samples with a large number of missing values were excluded. The effective sample included 561 individuals after the data screening. Table 2 provides more detailed descriptive statistics.
Table 2.
Descriptive statistics of the respondents’ characteristics
| Demographics | Category | Frequency | Percentage |
|---|---|---|---|
| Gender | Male | 269 | 48.0 |
| Female | 292 | 52.0 | |
| Age | ≤20 | 56 | 10.0 |
| 21–30 | 198 | 35.3 | |
| 31–40 | 176 | 31.4 | |
| 41–50 | 107 | 19.0 | |
| ≥50 | 24 | 4.3 | |
| Education | High school or below | 32 | 5.7 |
| Junior college | 88 | 15.7 | |
| University | 284 | 50.6 | |
| Master’s degree or higher | 157 | 28.0 | |
| Province | Shandong | 78 | 13.9 |
| Henan | 70 | 12.5 | |
| Chongqing | 61 | 10.9 | |
| Hunan | 60 | 10.7 | |
| Sichuan | 57 | 10.2 | |
| Heilongjiang | 55 | 9.8 | |
| Guangdong | 43 | 7.6 | |
| Jiangsu | 34 | 6.0 | |
| Others | 103 | 18.4 |
According to Westland,41 when the number (N) of respondents is more than 5 times the estimated parameter (p) of a model (i.e., N:p > 5:1), the stability of the correlation matrix and the reliability of the analysis results can be guaranteed. Our conceptual model estimates 80 parameters and the number of effective samples is greater than 400. Thus, the sample sizes are acceptable for hypothesis tests. In addition, we consulted the 2020 China Statistical Yearbook,42 and then conducted a χ2 test to examine the similarities between the distributions of national population attributes and the distributions of respondents’ characteristics. The results for gender (χ2(1) = 2.33, p = .13), age (χ2(4) = 6.75, p = .15), education (χ2(3) = 4.06, p = .26) and province (χ2(8) = 15.43, p = .05) show no significant differences in the distributions of demographics. Therefore, the sample in this study is representative to a certain extent.
Results
Reliability and validity test
Before hypothesis testing, the reliability and validity of the scale were tested. Using SPSS 17.0 and Lisrel 8.7 software, we conducted an exploratory factor analysis. In a series of analysis results, the KMO value was 0.89, which suggests that the 561 effective sample data in this study were suitable for factor analysis.43 Furthermore, this analysis extracted 12 factors that explained 88.66% of total variance, which indicates that these factors represent most of the information of the 32 items.44 In addition, the factor loadings of all 32 items were not less than 0.7, which demonstrates that these items can be analyzed for reliability and validity.45 Table 3 shows the specific factor loading of each item.
Table 3.
Statistical results of factor loadings, reliability test and convergent validity test
| Factors | Items | Loadings | AVE | CR | Cronbach α | |
|---|---|---|---|---|---|---|
| OE | OE1 | 0.80 | 0.68 | 0.87 | 0.91 | |
| OE2 | 0.83 | |||||
| OE3 | 0.85 | |||||
| RP | RP1 | 0.88 | 0.80 | 0.94 | 0.93 | |
| RP2 | 0.92 | |||||
| RP3 | 0.92 | |||||
| RP4 | 0.86 | |||||
| PS | PS1 | 0.77 | 0.59 | 0.74 | 0.89 | |
| PS2 | 0.77 | |||||
| SPC | SPC1 | 0.71 | 0.52 | 0.76 | 0.94 | |
| SPC2 | 0.72 | |||||
| SPC3 | 0.73 | |||||
| CF | CF1 | 0.78 | 0.62 | 0.76 | 0.95 | |
| CF2 | 0.79 | |||||
| VH | CP | CP1 | 0.81 | 0.63 | 0.77 | 0.95 |
| CP2 | 0.78 | |||||
| CV | CV1 | 0.78 | 0.55 | 0.71 | 0.84 | |
| CV2 | 0.70 | |||||
| VI | VI1 | 0.73 | 0.55 | 0.79 | 0.97 | |
| VI2 | 0.75 | |||||
| VI3 | 0.75 | |||||
| VB | VB1 | 0.88 | 0.76 | 0.86 | 0.98 | |
| VB2 | 0.86 | |||||
| SAT | SAT1 | 0.76 | 0.53 | 0.77 | 0.95 | |
| SAT2 | 0.73 | |||||
| SAT3 | 0.70 | |||||
| CVN | CVN1 | 0.81 | 0.70 | 0.88 | 0.96 | |
| CVN2 | 0.87 | |||||
| CVN3 | 0.83 | |||||
| PU | PU1 | 0.75 | 0.55 | 0.78 | 0.94 | |
| PU2 | 0.73 | |||||
| PU3 | 0.74 | |||||
OE = outcome expectancy; RP = risk perception; PS = perceived self-efficacy; SPC = social positive cues; VH = vaccine hesitancy; CF = confidence; CP = complacency; CV = convenience; VI = vaccination intention; VB = vaccination behavior; SAT = satisfactory; CVN = continuous vaccination; PU = perceived usefulness.
The composite reliability (CR) values and Cronbach α values were used to evaluate the reliability of the scale. Detailed analysis results are shown in Table 3. Based on this table, it can be seen that CR values and Cronbach α values of all factors exceeded 0.7, which indicates that the scale had high reliability.46
In the validity test, we intended to test the convergent validity and discriminant validity of the scale respectively. The average variance extracted (AVE) was used to analyze the convergent validity. The analysis results were also shown in Table 3 We can see that all AVE values were greater than 0.5, which demonstrates that this scale had satisfactory convergent validity.47 In addition, the confirmatory factor analysis (CFA) was used to test the discriminant validity of the scale. After the CFA, we discovered that the square roots of AVE values were greater that these coefficients, which indicates that the discriminant validity of the scale meets the requirements for analysis.48
Hypothesis tests
Using Lisrel 8.7 software, structural equation modeling was used to test our hypotheses. The analysis results of this model are shown in Table 4. We learned that all the fit indices results were acceptable, which demonstrates that our hypothesis tests that are used in this model were reasonable and effective.48
Table 4.
Evaluation results of the research model
| Fitting indices | Absolutely indices |
Parsimony indices |
Incremental indices |
||||||
|---|---|---|---|---|---|---|---|---|---|
| χ2/df | GFI | AGFI | RMSEA | PNFI | PGFI | CFI | NFI | IFI | |
| Values of fitting indices | 2.76 | 0.90 | 0.82 | 0.07 | 0.87 | 0.72 | 0.98 | 0.98 | 0.98 |
| Evaluation criteria values48 | <3 | >0.9 | >0.8 | <0.08 | >0.5 | >0.5 | >0.9 | >0.9 | >0.9 |
χ2 = Chi-square; df = degree of freedom; GFI = Goodness-of-Fit Index; AGFI = Adjusted Goodness-of-Fit Index; RMSEA = Root Mean Square Error of Approximation; PNFI = Parsimony Normed Fit Index; PGFI = Parsimony Goodness of Fit Index; CFI = Comparative Fit Index; NFI = Normed Fit Index; IFI = Incremental Fit Index.
Figure 2 shows the model’s normalized path coefficients. In the motivation stage, we learned that perceived self-efficacy had a positive significant influence on vaccination intention (β = 0.1, p < .05), but this effect did not appear in the relationship between outcome expectancy and vaccination intention (β = 0.04, p > .05) and between risk perception and vaccination intention (β = 0.03, p > .05). Therefore, H3 may be accepted, but H1 and H2 were not. In the intention stage, we found that social positive cues (β = 0.13, p < .01) and VH (β = −0.67, p < .001) exerted a positive and negative significant impact on vaccination intention, respectively, which supports H4 and H5. Moreover, vaccination intention positively affected vaccination behavior significantly (β = 0.75, p < .001), so H6 was supported. In the behavior stage, we noted that vaccination behavior had a significantly positive impact on perceived usefulness (β = 0.62, p < .001) and satisfaction (β = 0.26, p < .001), respectively. Thus, H7 and H8 were supported. In addition, perceived usefulness produced a positive significant influence on satisfaction (β = 0.73, p < .001) and continuous vaccination (β = 0.88, p < .001), respectively. Thus, H9 and H10 were supported. However, the positive effect of satisfaction on continuous vaccination was not significant (β = −0.06, p > .05), so H11 was not supported.
Figure 2.
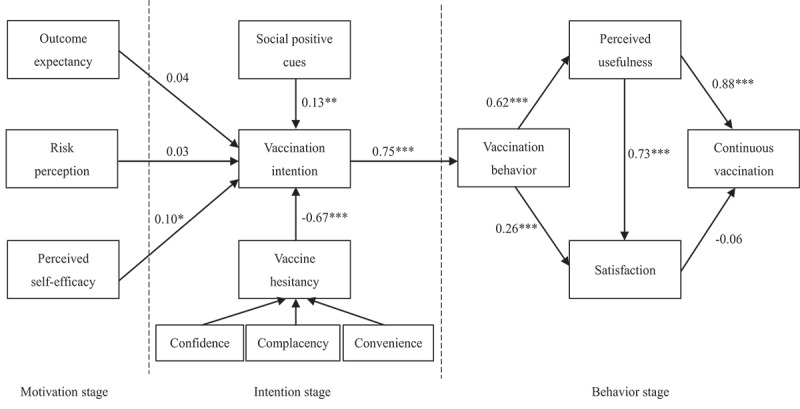
Hypothesis testing results.
Legends: It illustrates the direct and indirect effects of individual continuous vaccination for COVID-19.
Discussion
By combining the HAPA model, ECM, and VH theory, we produced a theoretical model that explores the impact process of continuous vaccination in COVID-19 and obtained six valuable findings. First, perceived self-efficacy has a positive significant impact on vaccination intention, but the effects of outcome expectancy and risk perception on vaccination intention are not significant. This finding is not completely consistent with the views in the HAPA model, in which the three variables – that is, outcome expectancy, risk perception, and perceived self-efficacy – are all pre-factors of behavioral intention.9 In the context of COVID-19, when individuals expect a positive outcome of vaccination, they will be more likely to take on these behaviors. The empirical results prove that individual will exert perceived self-efficacy by evaluating the positive outcome of behavior. However, in the context of COVID-19, the roles of outcome expectancy and risk perception have not been demonstrated. We believe that one possible reason for this result is that this study is an empirical analysis carried out in China; at present, China is one of the few countries where the global epidemic is well controlled, so in this region, the public’s concern about COVID-19 is not as serious as when the virus first broke out. Conversely, the public does not feel safe about the newly developed COVID-19 vaccine. In other words, vaccination may not be the safest health behavior in the minds of the Chinese public. Therefore, in the context of COVID-19, only the effect of perceived self-efficacy on behavioral intention has been proven.
Second, social positive cues play a significant role in promoting vaccination intention. This finding is similar to the evidence obtained from existing studies.24,25 When an individual perceives a threat and realizes that a beneficial action can be taken in order to mitigate this threat, the action will occur as cues trigger this action. In other words, cues to action can stimulate individuals to take protective measures or behaviors. In an environment where vaccination is questioned by the public at this stage, reliable knowledge, suggestions, and information are important guidelines for determining the intention of public behavior. The results of our analysis show that social positive cues are important elements that affect the public’s behavioral intentions. However, combining the third finding, based on the values of path coefficient, we conclude that compared with VH, social positive cues have a relatively limited effect on behavioral intention. This also shows that the public still holds, to a certain extent, a variety of concerns about vaccination.
Third, VH has a negative significant influence on vaccination intention. This finding is consistent with existing studies and illustrates a dilemma for COVID-19 vaccine at this stage.18,27,49–51 China was one of the first countries in the world to develop the COVID-19 vaccines and has recently exported them. However, VH is a global trend, with approximately 90% of countries across the globe reporting this situation.16 Moreover, due to fewer clinical trials, side effects, effectiveness, and other reasons, the COVID-19 vaccines still have not been fully recognized in the public mind. In this sense, VH has also produced a non-negligible influence on vaccination intention. Although China implements a free vaccination policy for the public, the value of path coefficient shows that the negative impact of VH on vaccination intention is still great.
Fourth, vaccination behavior produces a positive significant effect on perceived usefulness and satisfaction, respectively. This finding is completely consistent with the views in ECM.12 In the context of COVID-19, the public compares their own experience of vaccination with their own expectations after vaccination behavior. If their expectations are confirmed, they will feel that the vaccination is useful and be satisfied with vaccination. According to the first and third findings of this study, we can conclude that the public’s recognition of the COVID-19 vaccine is not high. However, the empirical analysis results show that when the public is vaccinated, they find that their own expectations can be confirmed. So far, there have been no cases of adverse reactions due to vaccination in China. Moreover, the vaccinated public has a reliable health code, which allows them to more freely and safely enter some public places. The public can not only perceive the usefulness of the vaccine, but also feel satisfied with the vaccination process and experience. This indicates to some extent that the COVID-19 vaccine is not so bad at this stage.
Fifth, perceived usefulness exerted a positive significant impact on satisfaction and continuous vaccination, respectively. This finding can be used as a supplement to previous research findings.33,34 If individuals feel that they can obtain a valuable experience in the actual behavior process, and believe that this behavior is useful to them, they will have a positive attitude toward the experience. At this time, their satisfaction and dependence on the experience will increase, and their willingness and tendency to continue using it will also be enhanced. The empirical results show that the COVID-19 vaccine is similar to other vaccines. Its usefulness can not only enhance public’s satisfaction, but also prompt them to be vaccinated again. Moreover, based on the values of path coefficient, we can see that the positive impact of perceived usefulness is prominent. This explains that the perceived usefulness of the COVID-19 is an important factor affecting public emotions and subsequent behaviors.
Sixth, satisfaction has no positive significant influence on continuous vaccination. This finding is different from previous research,29,35 and it indicates the particularity of the COVID-19 vaccine. From the perspective of rational people, individuals are more willing to continue to use products or services that are useful to them and that satisfy them. However, this evidence cannot be proved in the context of COVID-19. We speculate that the main reason for this finding is that vaccination is a comprehensive behavior that is affected by various factors such as gender, age, race, culture, and education.52 Satisfaction may influence several of these factors, but these impacts are not enough to contribute to continuous vaccination. We did not examine the impact of VH on continuous vaccination in the behavior stage, but based on the factor loadings of the VH variable in the intention stage, we find that the public’s VH mainly focuses on confidence and complacency. Based on the items of confidence and complacency in this study, we can understand that confidence indicates that the public is not sure about the COVID-19 vaccine, while complacency means that the public believes that the COVID-19 vaccine is not very important and necessary. In other words, when it comes to COVID-19 vaccine, the public remains skeptical and does not regard vaccination as necessary to protect health. Therefore, perhaps due to the potential impact of VH, satisfaction does not have a significant effect on continuous vaccination.
Conclusions
Vaccination for the COVID-19 provides an effective approach for the general improvement of social safety and individual health. To date, few studies have analyzed the continuous vaccination for COVID-19 vaccine and its impact process. Using the HAPA Model, ECM and VH theory, this research evaluates the continuous vaccination for COVID-19. We summarize our study’s practical contributions. First, governments of various countries need to strengthen all types of vaccination publicity. In this regard, it is best for relevant departments to publicize the benefits of the health behavior of vaccination through typical case interviews and experimental reports, so as to enhance the public’s perceived self-efficacy of vaccination. At the same time, doctors’ recommendations and popularization of vaccination knowledge can also be used to stimulate the public to vaccinate. In addition, it is necessary to minimize the public’s VH. An effective approach would be to ask groups that have been vaccinated to highlight the safety and necessity of vaccination in order to help increase public confidence and reduce complacency for vaccination. The above practices will have a positive impact on the public’s vaccination. Second, government and related policy-making institutions should take full advantage of the perceived usefulness of vaccination; in this regard, medical research departments need to strengthen clinical exploration of vaccination and constantly strive to improve the effect of vaccination, so that the public can experience the usefulness of vaccines in protecting physical and mental health. In addition, government should also ensure convenience and provide benefits to the vaccinated public. For instance, in terms of travel, shopping, and medical services, relevant departments can provide certain priorities and discounts for vaccinated groups so that they can really feel the usefulness of vaccination. The above measures will prompt the vaccinated population to get vaccinated again in the future.
A major limitation of this study is that we conducted data collection in China. Currently, the Chinese government has implemented a voluntary vaccination policy for COVID-19 vaccine. Therefore, the findings of this study may not be applicable to those countries that implement a compulsory vaccination policy. In addition, we find that VH has a negative significant impact on vaccination intention for the first time. So, does this variable have a similar effect on continuous vaccination? Researchers can explore this issue in the future.
Funding Statement
This work was supported by the Key Supported Discipline of Guizhou Provence [2020-2022]; MOE (Ministry of Education in China) Project of Humanities and Social Sciences [21YJC630161].
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Dhama K, Sharun K, Tiwari R, Dadar M, Malik YS, Singh KP, Chaicumpa W.. COVID-19, an emerging coronavirus infection: advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum Vaccin Immunother. 2020;16(6):1232–38. doi: 10.1080/21645515.2020.1735227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ledford H, Cyranoski D, Van Noorden R.. The UK has approved a COVID vaccine-here’s what scientists now want to know. Nature. 2020;588:205–06. doi: 10.1038/d41586-020-03441-8. [DOI] [PubMed] [Google Scholar]
- 3.MedSci . Bulletin of global COVID-19 and vaccination on October 18, 2021. Published 2021. [accessed 2021 Oct 30]. https://www.medsci.cn/article/show_article.do?id=79a3218e95fd.
- 4.Chinadaily . COVID-19 vaccine: answers to frequently asked questions. Published 2021. [accessed 2021 Oct 30]. http://www.chinadaily.com.cn/m/shanghai/jiading/2021-01/12/content_37542334.htm.
- 5.Dinleyici EC, Borrow R, Safadi MAP, van Damme P, Munoz FM. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum Vaccin Immunother. 2021;17(2):400–07. doi: 10.1080/21645515.2020.1804776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwok KO, Li KK, Wei WI, Tang A, Wong SYS, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021;114:103854. doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Commun Health. 2021;46(2):270–77. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8(3):482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA). Rehabil Psychol. 2011;56(3):161–70. doi: 10.1037/a0024509. [DOI] [PubMed] [Google Scholar]
- 10.Wu T, Qu S, Fang Y, Ip M, Wang Z. Behavioral intention to perform risk compensation behaviors after receiving HPV vaccination among men who have sex with men in China. Hum Vaccin Immunother. 2019;15(7–8):1737–44. doi: 10.1080/21645515.2019.1622975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamilton K, Smith SR, Keech JJ, Moyers SA, Hagger MS. Application of the health action process approach to social distancing behavior during covid-19. Appl Psychol-Health Well Being. 2020;12(4):1244–69. doi: 10.1111/aphw.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhattacherjee A. Understanding information systems continuance: an expectation-confirmation model. MIS Quart. 2001;25(3):351–70. doi: 10.2307/3250921. [DOI] [Google Scholar]
- 13.Zhang H, Lu Y, Gupta S, Gao P. Understanding group-buying websites continuance: an extension of expectation confirmation model. Internet Res. 2015;25(5):767–93. doi: 10.1108/IntR-05-2014-0127. [DOI] [Google Scholar]
- 14.Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34):4165–75. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 15.The Daily Star . Ten threats to global health in 2019. Published 2019. [accessed 2021 July 30]. https://www.thedailystar.net/health/news/ten-threats-global-health-2019-1693402.
- 16.Hotez P. America and Europe’s new normal: the return of vaccine-preventable diseases. Pediatr Res. 2019;85:912–14. doi: 10.1038/s41390-019-0354-3. [DOI] [PubMed] [Google Scholar]
- 17.Piot P, Larson HJ, O’Brien KL, N’kengasong J, Ng E, Sow S, Kampmann B. Immunization: vital progress, unfinished agenda. Nature. 2019;575(7781):119–29. doi: 10.1038/s41586-019-1656-7. [DOI] [PubMed] [Google Scholar]
- 18.Quinn SC, Jamison AM, An J, Hancock GR, Freimuth VS. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: results of a national survey of White and African American adults. Vaccine. 2019;37(9):1168–73. doi: 10.1016/j.vaccine.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 19.Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. 2008;57(1):1–29. doi: 10.1111/j.1464-0597.2007.00325.x. [DOI] [Google Scholar]
- 20.Schwarzer R, Hamilton K. Changing behavior using the health action process approach. New York (NY): Cambridge University Press; 2020. [Google Scholar]
- 21.Bhattacherjee A, Shrivastava U. The effects of ICT use and ICT Laws on corruption: a general deterrence theory perspective. Gov Inform Q. 2018;35(4):703–12. doi: 10.1016/j.giq.2018.07.006. [DOI] [Google Scholar]
- 22.Joveini H, Rohban A, Eftekhar Ardebili H, Dehdari T, Maheri M, Hashemian M. The effects of an education program on hookah smoking cessation in university students: an application of the Health Action Process Approach (HAPA). J Subst Use. 2020;25(1):62–69. doi: 10.1080/14659891.2019.1664655. [DOI] [Google Scholar]
- 23.Buglar ME, White KM, Robinson NG. The role of self-efficacy in dental patients’ brushing and flossing: testing an extended Health Belief Model. Patient Educ Couns. 2010;78(2):269–72. doi: 10.1016/j.pec.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 24.Rezaei R, Mianaji S. Using the health belief model to understand farmers’ intentions to engage in the on-farm food safety practices in Iran. J Agr Sci Tech-Iran. 2019;21(3):561–74. https://jast.modares.ac.ir/article-23-15517-en.html. [Google Scholar]
- 25.Koloseni DN, Lee CY, Gan ML. Understanding information security behaviours of Tanzanian government employees: a health belief model perspective. Int J Technol Hum Interact. 2019;15(1):15–32. doi: 10.4018/IJTHI.2019010102. [DOI] [Google Scholar]
- 26.Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, Yaseen A, Ababneh NA, Bakri FG, Mahafzah A. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiao X, Wong RM. Vaccine hesitancy and perceived behavioral control: a meta-analysis. Vaccine. 2020;38(33):5131–38. doi: 10.1016/j.vaccine.2020.04.076. [DOI] [PubMed] [Google Scholar]
- 28.Ajzen I. The theory of planned behavior. Organ Behav Hum Dec. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 29.Veeramootoo N, Nunkoo R, Dwivedi YK. What determines success of an e-government service? Validation of an integrative model of e-filing continuance usage. Gov Inform Q. 2018;35(2):161–74. doi: 10.1016/j.giq.2018.03.004. [DOI] [Google Scholar]
- 30.Oghuma AP, Libaque-Saenz CF, Wong SF, Chang Y. An expectation-confirmation model of continuance intention to use mobile instant messaging. Telemat Inform. 2016;33(1):34–47. doi: 10.1016/j.tele.2015.05.006. [DOI] [Google Scholar]
- 31.Lee MC. Explaining and predicting users’ continuance intention toward e-learning: an extension of the expectation-confirmation model. Comput Educ. 2010;54(2):506–16. doi: 10.1016/j.compedu.2009.09.002. [DOI] [Google Scholar]
- 32.Bhattacherjee A, Perols J, Sanford C. Information technology continuance: a theoretic extension and empirical test. J Comput Inform Syst. 2008;49(1):17–26. doi: 10.1080/08874417.2008.11645302. [DOI] [Google Scholar]
- 33.Sarkar S, Khare A. Influence of expectation confirmation, network externalities, and flow on use of mobile shopping apps. Int J Hum-Comput Int. 2019;35(16):1449–60. doi: 10.1080/10447318.2018.1540383. [DOI] [Google Scholar]
- 34.Al-Emran M, Arpaci I, Salloum SA. An empirical examination of continuous intention to use m-learning: an integrated model. Educ Inf Technol. 2020;25(4):2899–918. doi: 10.1007/s10639-019-10094-2. [DOI] [Google Scholar]
- 35.Liao C, Chen JL, Yen DC. Theory of planning behavior (TPB) and customer satisfaction in the continued use of e-service: an integrated model. Comput Hum Behav. 2007;23(6):2804–22. doi: 10.1016/j.chb.2006.05.006. [DOI] [Google Scholar]
- 36.Schwarzer R, Renner B. Social-cognitive predictors of health behavior: action self-efficacy and coping self-efficacy. Health Psychol. 2000;19(5):487–95. doi: 10.1037/0278-6133.19.5.487. [DOI] [PubMed] [Google Scholar]
- 37.Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Health. 2021;9:34. doi: 10.3389/fpubh.2021.632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Catalano HP, Knowlden AP, Birch DA, Leeper JD, Paschal AM, Usdan SL. Using the theory of planned behavior to predict HPV vaccination intentions of college men. J Am Coll Health. 2017;65(3):197–207. doi: 10.1080/07448481.2016.1269771. [DOI] [PubMed] [Google Scholar]
- 39.Homer PM, Kahle LR. A structural equation test of the value-attitude-behavior hierarchy. J Pers Soc Psychol. 1988;54(4):638–46. doi: 10.1037/0022-3514.54.4.638. [DOI] [Google Scholar]
- 40.Park E. User acceptance of smart wearable devices: an expectation-confirmation model approach. Telemat Inform. 2020;47:101318. doi: 10.1016/j.tele.2019.101318. [DOI] [Google Scholar]
- 41.Westland JC. Lower bounds on sample size in structural equation modeling. Electron Commer Res Appl. 2010;9(6):476–87. doi: 10.1016/j.elerap.2010.07.003. [DOI] [Google Scholar]
- 42.National Bureau of Statistics of China . 2020 China statistical yearbook. Published 2021. [accessed 2021 Nov 6]. http://www.stats.gov.cn/tjsj/ndsj/2020/indexeh.htm.
- 43.Li L, Li J. Factors affecting young Chinese women’s intentions to uptake human papillomavirus vaccination: an extension of the theory of planned behavior model. Hum Vaccin Immunother. 2020;16(12):3123–30. doi: 10.1080/21645515.2020.1779518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou M, Qu S, Zhao L, Campy KS, Wang S. Parental perceptions of human papillomavirus vaccination in central China: the moderating role of socioeconomic factors. Hum Vaccin Immunother. 2019;15(7–8):1688–96. doi: 10.1080/21645515.2018.1547605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao M, Liu H, Qu S, He L, Campy KS. Factors associated with parental acceptance of influenza vaccination for their children: the evidence from four cities of China. Hum Vaccin Immunother. 2021;17(2):457–64. doi: 10.1080/21645515.2020.1771988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fan CW, Chen IH, Ko NY, Yen CF, Lin CY, Griffiths MD, Pakpour AH. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. Hum Vaccin Immunother. 2021;17(10):1–8. doi: 10.1080/21645515.2021.1933687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou M, Zhao L, Kong N, Campy KS, Wang S, Qu S. Predicting behavioral intentions to children vaccination among Chinese parents: an extended TPB model. Hum Vaccin Immunother. 2018;14(11):2748–54. doi: 10.1080/21645515.2018.1496765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jongen VW, van der Loeff MFS, Boyd A, Petrignani M, Prins M, van der Wal M, Nielen A, de Melker H, Paulussen TGWM, Alberts CJ. Human papillomavirus vaccination uptake: a longitudinal study showing ethnic differences in the influence of the intention-to-vaccinate among parent-daughter dyads. Hum Vaccin Immunother. 2021;17(4):990–99. doi: 10.1080/21645515.2020.1808411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chaudhary FA, Ahmad B, Khalid MD, Fazal A, Javaid MM, Butt DQ. Factors influencing COVID-19 vaccine hesitancy and acceptance among the Pakistani population. Hum Vaccin Immunother. 2021;17(10):3365–70. doi: 10.1080/21645515.2021.1944743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cooper S, van Rooyen H, Wiysonge CS. COVID-19 vaccine hesitancy in South Africa: how can we maximize uptake of COVID-19 vaccines? Expert Rev Vaccines. 2021;20(8):921–33. doi: 10.1080/14760584.2021.1949291. [DOI] [PubMed] [Google Scholar]
- 51.Hossain E, Rana J, Islam S, Khan A, Chakrobortty S, Ema NS, Bekun FV. COVID-19 vaccine-taking hesitancy among Bangladeshi people: knowledge, perceptions and attitude perspective. Hum Vaccin Immunother. 2021:1–10. doi: 10.1080/21645515.2021.1944743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ward J, Raude J. Understanding influenza vaccination behaviors: a comprehensive sociocultural framework. Expert Rev Vaccines. 2014;13(1):17–29. doi: 10.1586/14760584.2014.863156. [DOI] [PubMed] [Google Scholar]


