Abstract
Objective
To understand COVID-19 vaccine perspectives among healthcare workers serving diverse communities.
Methods
A dual English/Spanish survey was distributed to healthcare workers in the United States from 3/12/2021–4/22/2021 by the Migrant Clinicians Network, Society of Refugee Healthcare Providers, a Federally Qualified Healthcare Center, and social media advertisement to general primary care workers.
Results
517 responses were at least 50% complete and included in the analysis. Among these, 88% (457/517) indicated vaccine acceptance. Factors associated with acceptance included not reporting any vaccine concerns, identifying as male, ≥65 years of age, being a physician or advanced practice provider, and interacting directly with patients from refugee, immigrant, and migrant (RIM) communities. Participants identified educational information as most helpful for themselves when making a vaccine decision, but a healthcare provider’s recommendation as most helpful for their patients.
Conclusion
Healthcare workers, especially those serving RIM communities, are vaccine accepting. Tailoring vaccine-related information to healthcare workers may improve vaccine confidence for both themselves and patients who rely on them for information.
Keywords: COVID-19, Vaccine, Acceptance, Healthcare worker, Refugee, Immigrant
1. Introduction
Despite COVID-19 vaccines being available for over a year, the Kaiser Family Foundation reported only 77% of United States (US) adults have received at least one vaccine dose, as of January 2022 [1]. Reasons for this stalled uptake are multi-factorial but likely stem from attitudes and beliefs about COVID-19 vaccines and differential access to vaccines and healthcare [2]. Certain groups have been disproportionately impacted by the pandemic, such as some refugee, immigrant, and migrant (RIM) communities [3], [4], [5]. These communities may experience additional barriers (or opportunities) to vaccines and healthcare such as cultural beliefs and knowledge, insurance coverage, transportation access, ability to miss work (e.g. be fired for missing a single day), language barriers, and lack of trust (especially of government and public health organizations) [6], [7].
In many communities, healthcare workers are looked to as a trusted source of information about COVID-19 vaccines [8]. As trusted messengers, healthcare workers’ attitudes and beliefs have the potential to greatly influence the decisions of others, and their recommendations to patients can increase acceptance of COVID-19 vaccines [9]. Given their professional responsibilities, healthcare workers are also well-positioned to hear concerns voiced by patients and members of the communities they serve. This gives healthcare workers a unique perspective about the beliefs and attitudes, and factors in vaccine decisionmaking by their patients and communities. In addition, a healthcare worker’s own attitudes and beliefs may influence the information and the force of recommendation they provide to their patients.
Early in the pandemic when vaccines became widely available in the US, the limited publications assessing healthcare workers’ attitudes and beliefs demonstrated that a significant percentage of healthcare workers were hesitant about receiving the vaccine themselves [10], [11]. Additionally, there is little information about the relationship between a healthcare worker’s personal vaccine attitudes and beliefs and that of their patients. This information could hold important implications for clinical and public health measures seeking to increase vaccine acceptance.
The primary objective of this study was to understand the perspective toward COVID-19 vaccines of healthcare workers caring for diverse and at-risk communities. In addition, vaccine concerns that healthcare workers reported that their patients voiced, and the association of these voiced concerns with the attitudes and beliefs of their healthcare providers, was investigated. Finally, healthcare workers were queried regarding what health communication strategies would be most useful for them and their patients in making vaccine decisions.
2. Methods
2.1. Study population
Healthcare workers who care for patients from RIM communities were the primary population of interest. A healthcare worker was broadly defined as anyone involved in the provision of health services, including those who interface directly with patients and those who do not. This definition was thereby inclusive of a wide range of healthcare positions (community health worker, physician, medical assistant, etc.). To capture this population, partnerships with Migrant Clinicians Network (MCN), the Society of Refugee Healthcare Providers (SRHP), and a Federally Qualified Health Center (FQHC) in Florida were used for survey distribution. MCN and the SRHP are professional organizations for healthcare workers caring for immigrant and migrant workers and their families, and refugees, respectively [12], [13]. For comparison, the survey was also distributed to self-identified general primary care healthcare workers through social media. The activities were reviewed and determined not to constitute human subjects research by the University of Minnesota Institutional Review Board.
2.2. Survey content
A survey was developed to query COVID-19 vaccine perspectives of healthcare workers caring for RIM communities and to identify helpful messaging strategies (Supplementary Appendix A). The survey was written in English and a bilingual study author (AG) translated it into Spanish (Supplementary Appendix B). The survey was piloted by six healthcare workers and was refined based on feedback received from the pilot. Survey demographic questions inquired about gender, age, geographic location, professional role, self-identification as a member of a RIM community and, when applicable, characteristics of their patient population such as percentage RIM, nationalities, and if residing in a rural location. Survey questions inquired as to attitudes, beliefs, concerns, and vaccination intent of the participants (healthcare workers), and what information or tools might be useful in making vaccine decisions for themselves. Among participants who reported direct interaction with patients, questions were asked to assess the concerns being voiced by patients regarding vaccines and what messaging strategies may be helpful for their patients.
2.3. Survey administration
The survey was distributed in English and Spanish using Qualtrics software [14] between March 12 and April 14, 2021 in accordance with institutional policies for each group. No incentives were offered. Individual survey links were distributed using an organizational email list-serv for both MCN (n = 4588) and the SRHP (n = 357) with email reminders sent to those who had not completed the survey at seven and 12 days following the initial request. An anonymous survey link was disseminated through a single email among employees of an FQHC (n = 280). Finally, in order to sample participants from the national general primary care workforce who did not identify as primarily focused on RIM care, an anonymous survey link was shared using targeted advertisements in English and Spanish on Facebook, Instagram, and Messenger (Menlo Park, CA) over 14 days using the following parameters: location in the US; age between 24 and 64; education level of vocational certificate, associate degree, college graduate, master’s degree, professional degree, or doctorate degree; industry in “healthcare and medical services”; and interest of “primary care”, “primary care physician”, or “primary health care”.
2.4. Data analysis
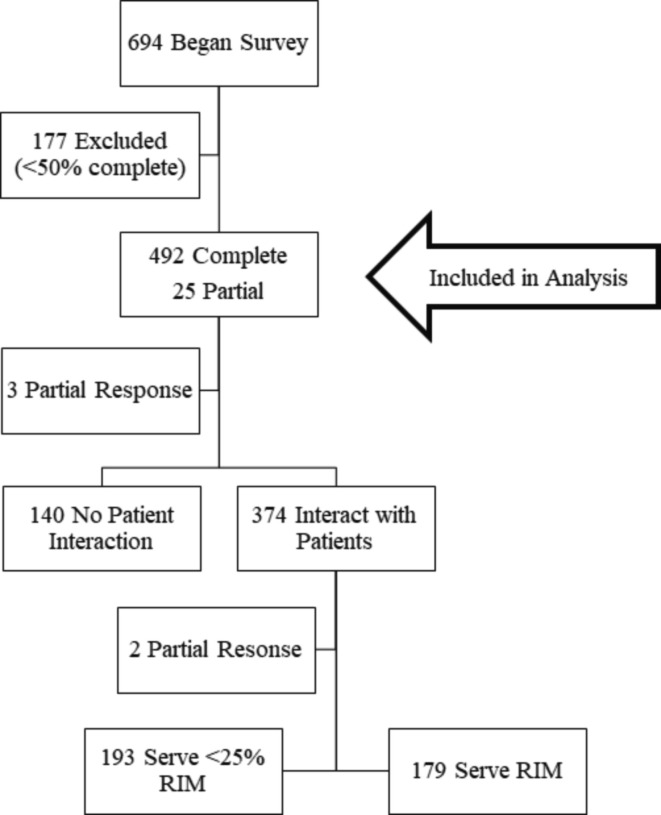
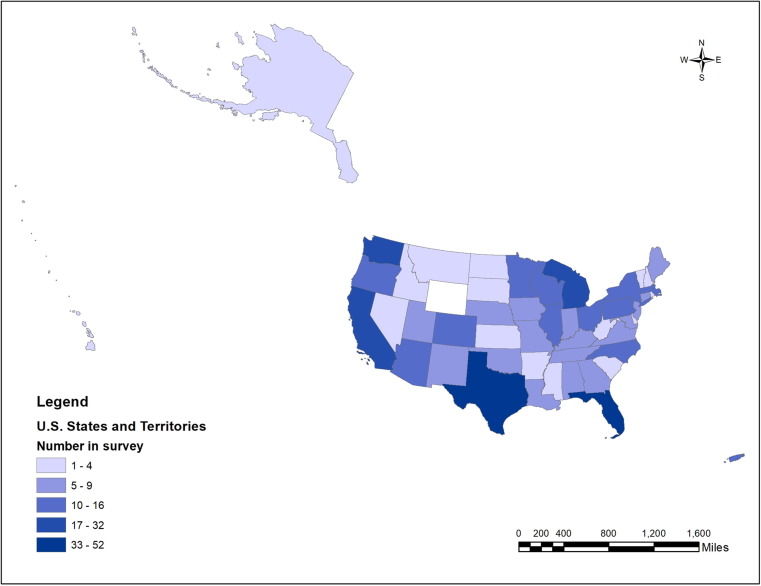
While 694 initiated the survey, 177 responses with less than 50% of questions complete were excluded to maximize sample size while minimizing bias toward responses that were mostly incomplete. The 517 remaining partial (n = 25) and complete (n = 492) responses were included in the analysis (Fig. 1 ). Survey participation was well-distributed throughout the US and territories (Supplemental Fig. 1). States were grouped into regions according to the US Census Bureau (West, Midwest, South, and Northeast) [15]. Healthcare worker positions were categorized into four groups as follows: physicians and advanced practice providers, nurses and ancillary staff members (including participants with professional degrees), medical assistants, and community health workers. Vaccine acceptance was defined as having received a vaccine dose or “definitely intending” to be vaccinated. Healthcare worker vaccine concern was defined as endorsing at least one doubt about vaccination.
Fig. 1.
Participant response.
Nationality information relating to both the participant and patient populations were categorized according to the World Bank Regional Units (Africa, East Asia and Pacific, Europe and Central Asia, Latin America and Caribbean, Middle East and North Africa, and South Asia) [16]. When response distribution allowed, further granularity was attained. The World Bank Europe and Central Asia regional unit was subdivided into Eastern Europe plus Russia and an Other European region. The Latin America and Caribbean region was subdivided into Mexican, Caribbean, and Other Latin American regions. When Hispanic or Latinx ethnicity rather than nationality was provided by the participant (n = 112), responses were categorized as “Other Latin American”. When “African” was provided rather than nationality, responses were categorized in the Africa region (n = 5), but responses containing “Asian” were not grouped with another region (n = 9) because of the inability to disaggregate by World Bank region.
R statistical software version 4.1.1 was used for all analyses [17]. Univariate analyses were performed to identify factors associated with vaccine acceptance and association between healthcare worker and patient vaccine concerns. Logistic regression was performed to characterize an association with vaccine acceptance related to healthcare worker serving RIM communities and professional role. Maps were created using ArcGIS version 10.6 (ESRI, Redlands, CA) [18].
3. Results
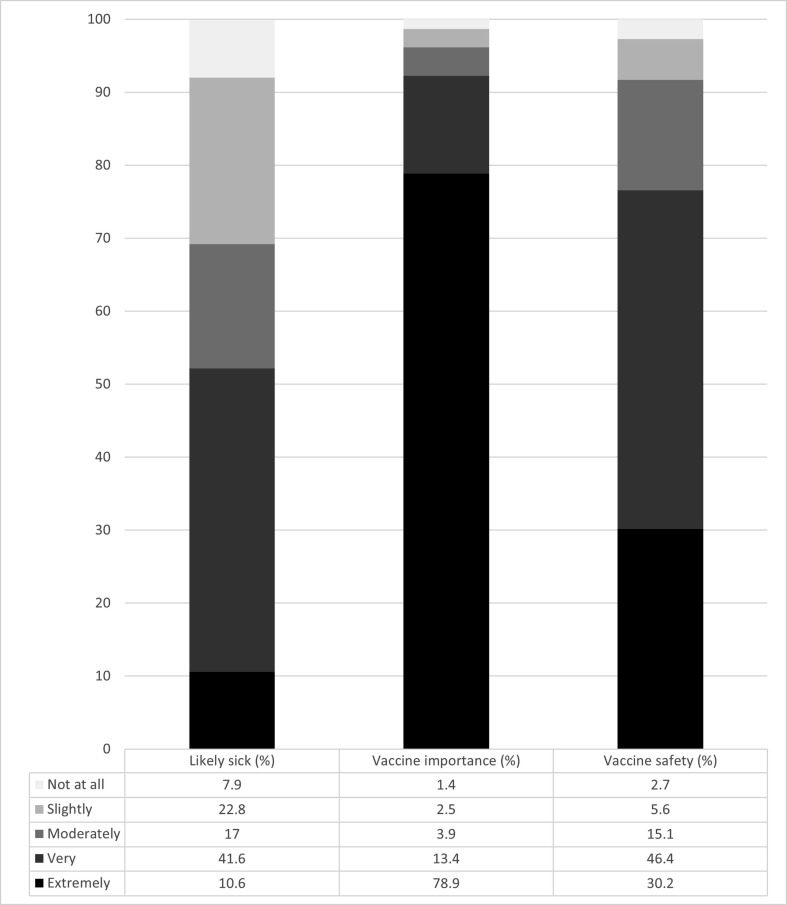
Of the 517 survey responses included in analysis, 204 were recruited by MCN (response rate = 4.5%), 72 by SRHP (response rate = 20.2%), 33 by the FQHC (response rate 11.8%), and 208 by social media advertisements. The majority of participants identified as female (431, 83.4%), were younger than age 65 (466, 90.1%), were either a physician or advanced practice provider (242, 46.8%), and directly interacted with patients (374, 72.3%). Half (270, 52.2%) of participants felt they were somewhat or extremely likely to become ill from COVID-19 and most perceived the vaccine as very or extremely important in prevention (477, 92.3%), and very or extremely safe (396, 76.6%) (Supplemental Fig. 2).
3.1. Vaccine acceptance
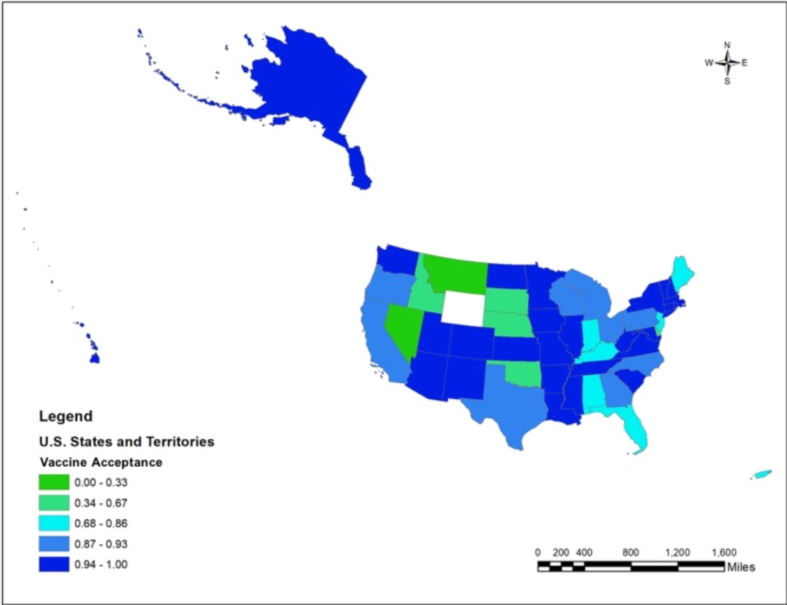
Among all participants, 457 (88.4%) were considered vaccine accepting (received or definitely intending to receive the vaccine when available to them), with 426 (82.4%) having received at least a single dose. Of the remaining unvaccinated participants, three (0.6%) would “probably” get the vaccine, 12 (2.3%) were “unsure”, 33 (6.4%) “did not intend to be vaccinated”, and 12 (2.3%) “preferred not to answer”. Vaccine acceptance was seen throughout the US (Fig. 2 ). Participants who did not endorse any vaccine concern were more likely to be vaccine accepting (OR 22.97, 95% CI: 8.10–65.12). Additional factors associated with vaccine acceptance included identifying as male, being 65 years of age or older, being a physician or an advanced practice provider, affiliation with the SRHP, and having direct patient interaction with RIM community members (p < 0.5 for all) (Table 1 ). After adjustment for being a physician or an advanced practice provider, healthcare workers who provide care for RIM patients were more likely to be vaccine accepting (OR 9.02, 95% CI: 1.14–71.17).
Fig. 2.
Vaccine acceptance by participant location.
Table 1.
Participant characteristics by vaccine acceptance.*
|
Yes (n = 457) % (n) |
No (n = 48) % (n) |
p-value | |
|---|---|---|---|
| Vaccine Concern | <0.001 | ||
| None | 98.7 (309) | 1.3 (4) | |
| ≥1 | 77.1 (148) | 22.9 (44) | |
| Gender | <0.01 | ||
| Female | 90.6 (384) | 9.4 (40) | |
| Male | 93.3 (70) | 6.7 (5) | |
| Non-binary/other/prefer not to answer | 50.0 (3) | 50.0 (3) | |
| Age | 0.04 | ||
| <25 | 66.7 (2) | 33.3 (1) | |
| 25–39 | 87.9 (124) | 12.1 (17) | |
| 40–64 | 90.4 (281) | 9.7 (30) | |
| 65+ | 100.0 (50) | 0.0 (0) | |
| Role/education | <0.001 | ||
| Physician/Advanced Practice Provider | 94.4 (234) | 5.6 (14) | |
| Nurse/Ancillary Staff | 89.5 (94) | 10.5 (11) | |
| Medical Assistant | 72.4 (21) | 27.6 (8) | |
| Community Health Worker | 85.3 (58) | 14.7 (10) | |
| Distribution Group | <0.001 | ||
| Society of Refugee Healthcare Providers | 100.0 (72) | 0.0 (0) | |
| Migrant Clinicians Network | 92.3 (180) | 7.7 (15) | |
| Federally Qualified Health Center | 78.1 (25) | 21.9 (7) | |
| Social Media | 87.4 (180) | 12.6 (26) | |
| Geographic Location | 0.50 | ||
| West | 91.8 (101) | 8.2 (9) | |
| Midwest | 90.7 (97) | 9.4 (10) | |
| South | 88.6 (163) | 11.4 (21) | |
| Northeast | 95.8 (68) | 4.2 (3) | |
| US Territory | 86.7 (13) | 13.3 (2) | |
| Identify as a member of a Refugee, Immigrant, or Migrant (RIM) Community | 0.90 | ||
| Yes | 90.9 (70) | 9.1 (7) | |
| No | 91.1 (380) | 8.9 (37) | |
| Direct Interaction with Patients | 0.60 | ||
| Yes | 91.1 (336) | 8.9 (33) | |
| No | 89.6 (120) | 10.4 (14) | |
| Patients from RIM Community | <0.001 | ||
| Yes | 95.5 (169) | 4.5 (8) | |
| No | 87.4 (166) | 12.6 (24) | |
| Patients Reside in Rural Area | 0.07 | ||
| Yes | 86.8 (92) | 13.2 (14) | |
| No | 92.8 (244) | 7.2 (19) |
does not include 12 participants who preferred not to answer the question regarding vaccine acceptance.
3.2. Association between healthcare worker concerns and reporting of patient concerns
Among the 374 healthcare workers who self-identified as directly interacting with patients, 138 (36.9%) expressed at least one vaccine concern. The most frequently expressed concern was “unknown vaccine effects” (96, 25.7%) followed by “how new the vaccine is” (75, 19.0%), “known side effects” (71, 18.0%), fast “speed of development” (71, 18.0%), and the “government’s role in development” (56, 15.0%). Some expressed that being vaccinated is “something people I trust don’t think I should do” (46, 12.3%). Among those concerned about known side effects, they were most worried about anaphylaxis and allergic reactions (57, 81%), followed by fever and chills (20, 15%), headache (3, 2%), and tiredness (2, 2%) with none being most worried about arm pain and swelling. Healthcare workers with at least one vaccine concern were more likely to report that their patients also had concerns such as the newness of the vaccine, how it was made, how it works, and what it contains. However, they were not more likely than healthcare workers without any vaccine concerns to report patients expressing concerns over safety or side effects (Table 2 ).
Table 2.
Association between healthcare worker vaccine concern and reporting a patient vaccine concern.*
|
Healthcare worker concern (n = 138) % (n) |
Healthcare worker without concern (n = 236) % (n) |
p-value | |
|---|---|---|---|
| Patient concern | |||
| Newness of the vaccine | 0.004 | ||
| Rarely | 12.1 (16) | 15.9 (36) | |
| Sometimes | 37.1 (49) | 51.1 (116) | |
| Most of the time | 50.8 (67) | 33.0 (75) | |
| How the vaccine was made | 0.02 | ||
| Rarely | 29.6 (39) | 40.5 (92) | |
| Sometimes | 41.7 (55) | 41.9 (95) | |
| Most of the time | 28.8 (38) | 17.6 (40) | |
| How the vaccine works | 0.007 | ||
| Rarely | 24.2 (32) | 35.7 (81) | |
| Sometimes | 48.5 (64) | 49.3 (112) | |
| Most of the time | 27.3 (36) | 15.0 (34) | |
| What the vaccine contains | 0.009 | ||
| Rarely | 30.3 (40) | 37.0 (84) | |
| Sometimes | 40.2 (53) | 47.1 (107) | |
| Most of the time | 29.6 (39) | 15.9 (36) | |
| How safe the vaccine is | 0.08 | ||
| Rarely | 10.6 (14) | 7.9 (18) | |
| Sometimes | 22.7 (30) | 33.9 (77) | |
| Most of the time | 66.7 (88) | 58.2 (132) | |
| Side effects of the vaccines | 0.13 | ||
| Rarely | 9.9 (13) | 9.7 (22) | |
| Sometimes | 31.8 (42) | 42.3 (96) | |
| Most of the time | 58.3 (77) | 48.0 (109) | |
| Healthcare worker vaccine acceptance | <0.001 | ||
| Yes | 76.1 (102) | 99.6 (234) | |
| No | 23.9 (32) | 0.4 (1) |
Includes the 374 respondents who reported directly interacting with patients.
3.3. Geographic variance of beliefs
There was no statistically significant variation in vaccine acceptance among healthcare workers by geographic location within the US (p = 0.5). Among healthcare workers who reported directly interacting with patients, there was no association with vaccine acceptance between those whose patients were from a rural location and those whose patients were not (p = 0.07). Healthcare workers who reported directly interacting with RIM communities were well-distributed throughout the US, as was the world geographic regional distribution of RIM communities served by survey participants (Supplemental Fig. 3). Healthcare workers who interacted with RIM and non-RIM communities alike most frequently reported patients voicing concerns about “how safe the vaccine is” and there was no substantial variation in this patient-expressed vaccine concern by world geographic regional distribution of RIM communities.
3.4. Preferred messaging strategies
Healthcare workers ranked educational information as most helpful for them and their colleagues in making vaccine decisions (201, 39.1%), followed by a recommendation from their healthcare provider (190, 37.0%), and encouragement from a trusted source (123, 23.9%). Of the types of educational information that healthcare workers identified as helpful for themselves and their colleauges, handouts were the most preferred method (71, 35.3%) and vaccine FAQs the most requested topic (80, 39.8%). For patients making a vaccine decision, healthcare workers who directly interacted with patients reported that a “recommendation from their healthcare provider during a one-on-one encounter” was most helpful (n = 172, 49%), followed by encouragement from a trusted source (n = 98, 28%), and educational information (n = 80, 23%).
4. Discussion
Our results indicated a higher degree of healthcare worker vaccine acceptance than previously reported during the study period, with 88% of participants having received at least one vaccine dose or intending to be vaccinated as of April 2021, prior to employer vaccine mandates. This was encouraging when compared to earlier reports of healthcare worker vaccination intent ranging from 36% in fall of 2020 [10] to 50–60% in winter of 2020 [11], [19]. Interestingly, our finding that 82% of healthcare workers self-reported receiving at least one vaccine dose was higher than other reports suggesting that 52–76% of healthcare workers [20], [21], [22], [23] and 64% of all US adults had been vaccinated by spring of 2021 [24]. Related to their educational and work experiences, healthcare workers likely have a general understanding of vaccines’ role in community and individual disease prevention and thus may be more vaccine acceptant than the general population. Healthcare workers may also be motivated to receive the vaccine as an example for others, given that they are frequently viewed as respected and trusted authorities [8], which was further supported by our findings that healthcare workers identified their vaccine recommendation as helpful for patients.
We found that among those who interact directly with patients from RIM communities, acceptance rose to 96%, as compared to 87% among those who directly interact with <25% RIM community members (p < 0.001). While an association between higher education and vaccine acceptance has been established [10], [11], [20], it is notable that healthcare workers serving more predominantly RIM populations were more vaccine accepting in this evaluation, and compared with other literature assessing vaccine acceptance among healthcare workers. The reason for this higher acceptance is unknown but may be that those who provide healthcare for RIM communities feel a greater sense of social responsibility, tend to work in settings that emphasize disease prevention, or have a deeper appreciation for morbidity and mortality that infectious diseases cause worldwide.
Variation in COVID-19 vaccine uptake by state has been closely followed [25] and, although a prior study reported healthcare worker vaccine acceptance being highest in the South [10], we did not find differences in acceptance by geographic region. Similarly, while COVID-19 acceptance in the general population has been lower in rural areas [26], [27], and among rural healthcare workers in other publications [10], [22], we did not identify a statistically significant difference in vaccine acceptance among healthcare workers serving rural communities. The lack of difference in vaccine acceptance by geographic region suggests that healthcare workers in our sample may not have been as influenced by regional factors.
The balance between having vaccine concerns and accepting vaccination is complex. While our findings demonstrated that healthcare workers with any vaccine concern had a twenty times higher odds of not intending to be vaccinated, 32% of vaccine accepting participants endorsed at least one concern, suggesting that concern alone is insufficient to dissuade some people from vaccination. Instead, this suggests a complex and multi-factorial risk and benefit consideration when deciding whether to be vaccinated. As indicated by our findings, many healthcare workers thought they were likely to become ill (“get sick”) from COVID-19 (perhaps related to increased exposure in healthcare settings) and that a vaccine was important to prevent disease spread, which may contribute to a vaccine decision where the perceived benefits of vaccination overcome some concerns. Our finding of similar vaccine acceptance, regardless of involvement directly with patient care, may also suggest that risk perception among healthcare workers was related more to a general understanding of disease than a specific fear of acquiring COVID-19 at the patient interface.
The relationship between healthcare worker vaccine concern and perceived patient concerns was unexpected and, to our knowledge, not previously identified during the COVID-19 pandemic. While this association was not indicative of concordance between patient and healthcare worker views, especially given that healthcare providers may over-estimate patient concerns [28], this association raises important questions about the impact of healthcare worker vaccine perspectives on communication and interpretation of patient concerns. For example, an important question is if healthcare workers who have reservations themselves may be projecting concerns on, or to, patients, and if these concerns influence the strength of the recommendation they provide to their patients. Alternatively, if healthcare workers with reservations are more attuned toward vaccine concerns in others, leading to a greater awareness of patient concerns, they may have greater opportunity to address concerns and positively influence vaccine decision-making. These questions raise many interesting avenues for further study that incorporates patient perceptions, healthcare worker and patient interactions, and vaccine uptake to further ellucidate this relationship.
A benefit of this methodology was that we were able to assess perspectives toward COVID-19 vaccines while simultaneously gathering information about preferred vaccine-related communications that organizations could act on in real-time during a public health crisis. Because of this methodology we found that healthcare workers most preferred educational information to help them make a decision about COVID-19 vaccination. This may suggest that, when making a decision, healthcare workers rely on their own decision-making capability and acceptance of recommendations from expert authorities. This is consistent with a prior study where healthcare workers most frequently identified themselves as the sole contributor to making a decision, and also reported that medical literature and experts influence their decision [11].
An additional benefit of our methodology is that, following survey completion, we were able to provide descriptive results back to the distribution partners, allowing them to use the findings in development of vaccination strategies at their organizations. Furthermore, by distributing the survey among healthcare workers, we were able to identify not only their own vaccine perspectives, but also topics of concern for patients with potential to refine material to meet concerns by nationality and geographic location. While we did not find significant variation in patient-voiced concerns by the predominant nationalities served by healthcare workers, identifying patterns of patients’ vaccine-related concerns using healthcare workers’ experiences could be helpful in the future to tailor communication materials for communities who already experience barriers to effective vaccine communications related to cultural, language, and health literacy differences.
As the US has now extended COVID-19 vaccine availability to children, healthcare workers remain essential in vaccination efforts. As such, they must be supported with updated vaccine information so that they are well-equipped when recommending vaccines to their patients. In other public health responses, such as addressing vaccine acceptance on a larger scale (e.g., childhood measles or annual influenza vaccines), it may be helpful to similarly leverage healthcare workers’ role within communities to understand the best methods for addressing vaccine concerns. Additionally, elucidating the relationship between healthcare worker and patient vaccines may provide helpful insight about vaccine decision-making. In the case of a future infectious disease threat requiring an urgent response, similar surveys of healthcare workers can quickly gather essential information for designing public health interventions.
This study has many important limitations. Generalizability of the findings is limited by cross-sectional data that represents only a snapshot of time during the pandemic, methodology that included a relatively novel use of social media as a comparison group, and low response rates. Likewise, generalizability to all healthcare workers is limited since we focused on healthcare workers in primary care settings and who provide care for RIM communities, likely excluding the perspectives of healthcare workers in specialist or sub-specialist settings, or who primarily work in hospitals or care facilities. An additional limitation is that, due to response distribution, we were unable to do a multivariate analysis that included survey group in addition to education in describing our finding that healthcare workers who directly interact with patients from RIM communities were more vaccine accepting. For this reason it is unclear whether the association of vaccine acceptance with healthcare workers who serve RIM communities was driven primarily by one study group as the Society of Refugee Healthcare Providers had 100% vaccine acceptance.
Our findings highlight the importance of engaging healthcare workers during pandemic vaccination campaigns. Despite expressing vaccine concerns, healthcare workers, especially those serving RIM communities, were very accepting of COVID-19 vaccines and played an essential role in helping patients make vaccine decisions. Our findings also emphasize the importance of prioritizing different methods of messaging for different audiences as healthcare workers preferred handouts related to frequently asked questions about vaccines for their own decision-making yet indicated their patients may prefer a recommendation from their healthcare provider. In public health efforts, similar methods of conducting surveys can provide real-time, actionable information related not only to vaccine perspectives, but ideal methods of communication, leading to more efficient responses.
Funding
This work was supported by the United States Centers for Disease Control and Prevention and the International Organization for Migration through an award to the National Resource Center for Refugees, Immigrants, and Migrants [CK000495-03-00/ES1874]. CT receives support from the National Institute of Allergy and Infectious Diseases [T32 AI055433]. This work is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: William Stauffer reports a relationship with Wolters Kluwer UpToDate that includes: speaking and lecture fees. William Stauffer reports a relationship with Emergent BioSolutions Inc that includes: speaking and lecture fees.
Acknowledgements
The authors would like to thank the Community Leadership Board at the National Resource Center for Refugees, Immigrants, and Migrants, and Dr. Michelle Weinberg with the Division of Global Migration and Quarantine at the Centers for Disease Control and Prevention, for guidance in determining the overarching objectives of this project. Additionally, the authors thank James Sutton with the Society of Refugee Healthcare Providers; Giovanni Lopez-Quezada with the Migrant Clinicians Network; Colette Heid with Treasure Coast Community Health; and Syreeta Wilkins with the National Resource Center for Refugees, Immigrants, and Migrants for their assistance with survey distribution.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.03.011.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Supplementary figure 1.
Geographic distribution of participants.
Supplementary figure 2.
Perceptions about likelihood of COVID-19 illness, and vaccine importance and safety (n=517).
Supplementary figure 3.
Distribution of refugee, immigrant, and migrant populations served by healthcare workers.
References:
- 1.Kaiser Family Foundation. KFF COVID-19 Vaccine Monitor Dashboard. KFF 2021. https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/ [accessed February 9, 2022].
- 2.Fisk R.J. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Global Health J. 2021;5:51–55. doi: 10.1016/j.glohj.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Đoàn L.N., Chong S.K., Misra S., Kwon S.C., Yi S.S. Immigrant Communities and COVID-19: Strengthening the Public Health Response. Am J Public Health. 2021;111:S224–S231. doi: 10.2105/AJPH.2021.306433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang M., Gurung A., Anglewicz P., Yun K. COVID-19 and Immigrant Essential Workers: Bhutanese and Burmese Refugees in the United States. Public Health Rep. 2021;136:117–123. doi: 10.1177/0033354920971720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reid A., Ronda-Perez E., Schenker M.B. Migrant workers, essential work, and COVID-19. Am J Ind Med. 2021;64:73–77. doi: 10.1002/ajim.23209. [DOI] [PubMed] [Google Scholar]
- 6.Wilson L., Rubens-Augustson T., Murphy M., Jardine C., Crowcroft N., Hui C., et al. Barriers to immunization among newcomers: A systematic review. Vaccine. 2018;36(8):1055–1062. doi: 10.1016/j.vaccine.2018.01.025. [DOI] [PubMed] [Google Scholar]
- 7.Thomas C.M., Osterholm M.T., Stauffer W.M. Critical considerations for COVID-19 vaccination of refugees, immigrants, and migrants. Am J Trop Med Hygiene. 2021;104:433–435. doi: 10.4269/ajtmh.20-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher K.A., Nguyen N., Crawford S., Fouayzi H., Singh S., Mazor K.M. Preferences for COVID-19 vaccination information and location: Associations with vaccine hesitancy, race and ethnicity. Vaccine. 2021;39:6591–6594. doi: 10.1016/j.vaccine.2021.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen K.H., Yankey D., Lu P.-J., Kriss J.L., Brewer N.T., Razzaghi H., et al. Report of Health Care Provider Recommendation for COVID-19 Vaccination Among Adults, by Recipient COVID-19 Vaccination Status and Attitudes — United States, April–September 2021. MMWR Morb Mortal Wkly Rep. 2021;70(50):1723–1730. doi: 10.15585/mmwr.mm7050a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shekhar R., Sheikh A.B., Upadhyay S., Singh M., Kottewar S., Mir H., et al. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines. 2021;9(2):119. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaw J., Stewart T., Anderson K.B., Hanley S., Thomas S.J., Salmon D.A., et al. Assessment of U.S. health care personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Migrant Clinicians Network. Who We Are. Migrant Clinicians Network 2021. https://www.migrantclinician.org/about/our-story [accessed November 21, 2021].
- 13.Society of Refugee Healthcare Providers. Welcome to the Society of Refugee Healthcare Providers 2021. https://refugeesociety.org/ [accessed July 6, 2021].
- 14.Qualtrics. Qualtrics. Provo, UT, USA: Qualtrics; 2005.
- 15.US Census Bureau. 2010 Census Regions and Divisions of the United States. The United States Census Bureau 2018. https://www.census.gov/geographies/reference-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html [accessed August 26, 2021].
- 16.World Bank Group. World Bank Units. World Bank 2021. https://www.worldbank.org/en/about/unit [accessed June 28, 2021].
- 17.R Core Team. R . R Foundation for Statistical Computing; Vienna, Austria: 2021. A language and environment for statistical computing. [Google Scholar]
- 18.Esri. ArcGIS. Redlands, CA: Esri Inc.; 2018.
- 19.Smith H.L., Prescher M.J., Sittig K.R., Veach L.A. Severe acute respiratory coronavirus virus 2 (SARS-CoV-2) vaccine acceptance in employees in an integrated health system in the Midwest. ASHE. 2021;1 doi: 10.1017/ash.2021.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirzinger A, Kearney A, Hamel L, Brodie M. KFF/The Washington Post Frontline Health Care Workers Survey - Vaccine Intentions. KFF 2021. https://www.kff.org/report-section/kff-washington-post-frontline-health-care-workers-survey-vaccine-intentions/ [accessed March 22, 2021].
- 21.Lee J.T., Althomsons S.P., Wu H., Budnitz D.S., Kalayil E.J., Lindley M.C., et al. Disparities in COVID-19 Vaccination Coverage Among Health Care Personnel Working in Long-Term Care Facilities, by Job Category, National Healthcare Safety Network — United States, March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(30):1036–1039. doi: 10.15585/mmwr.mm7030a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reses H.E., Jones E.S., Richardson D.B., Cate K.M., Walker D.W., Shapiro C.N. COVID-19 vaccination coverage among hospital-based healthcare personnel reported through the Department of Health and Human Services Unified Hospital Data Surveillance System, United States, January 20, 2021-September 15, 2021. Am J Infect Control. 2021;49:1554–1557. doi: 10.1016/j.ajic.2021.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Green-McKenzie J., Shofer F.S., Momplaisir F., Kuter B.J., Kruse G., Bilal U., et al. Factors Associated With COVID-19 Vaccine Receipt by Health Care Personnel at a Major Academic Hospital During the First Months of Vaccine Availability. JAMA Network Open. 2021;4(12):e2136582. doi: 10.1001/jamanetworkopen.2021.36582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamel L, Lopes L, Sparks G, Stokes M, Brodie M. KFF COVID-19 Vaccine Monitor: April 2021. KFF 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-april-2021/ [accessed February 8, 2022].
- 25.The New York Times. See How Vaccinations Are Going in Your County and State. The New York Times 2021. https://www.nytimes.com/interactive/2020/us/covid-19-vaccine-doses.html [accessed October 27, 2021].
- 26.Kirzinger A, Sparks G, Brodie M. KFF COVID-19 Vaccine Monitor- Rural America. KFF 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-rural-america/ [Accessed October 27, 2021].
- 27.Murthy B.P., Sterrett N., Weller D., Zell E., Reynolds L., Toblin R.L., et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties — United States, December 14, 2020–April 10, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(20):759–764. doi: 10.15585/mmwr.mm7020e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Healy C.M., Montesinos D.P., Middleman A.B. Parent and provider perspectives on immunization: are providers overestimating parental concerns? Vaccine. 2014;32:579–584. doi: 10.1016/j.vaccine.2013.11.076. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.