Introduction
Palmoplantar keratodermas (PPK) are a diverse group of dermatologic conditions characterized by the thickening of palms and soles because of excessive keratinization.1 PPKs are classified as either hereditary or acquired depending on their onset. Hereditary PPKs are associated with genetic mutations, whereas acquired PPKs have numerous causes, including malignancy, medications, infection, inflammatory dermatoses, and systemic disease. PPK has also been reported in association with malnutrition2; however, the pathophysiology and prevalence of this etiology remains unclear. Herein, we report a case of acquired PPK in a patient with severe malnutrition and multiple vitamin deficiencies that resolved after change in dietary intake and vitamin supplementation. Our findings suggest that consideration of nutritional status early on in the workup for acquired PPK may be beneficial for both timely diagnosis and treatment.
Case report
A 41-year–old man with a history of undifferentiated connective tissue disease, irritable bowel syndrome, and Gilbert disease presented with multisystem complaints, including blurry vision, right knee pain, and a red rash on his legs. Concomitantly, he was undergoing a workup for a yearlong, unintentional weight loss and abdominal discomfort with more recent onset of PPK and gingival bleeding. He reported a 2-year history of debilitating poor appetite, constipation, and abdominal discomfort after ingestion of specific foods (eg, fruit and meat), which led to a highly selective diet primarily composed of grains, potatoes, nuts, and cheese. He had no prior personal or family history of PPK. He denied any history of repeated trauma to his hands but notably worked as a cabinet maker.
Physical examination was notable for cachexia, edema, and ecchymosis on the right knee, perifollicular petechial rash with associated corkscrew hairs on the arms and legs (Fig 1, A and B), splinter hemorrhages in the nails, scattered gingival hemorrhages (Fig 1, C), focal and punctate hyperkeratotic plaques on the palms (Fig 1, D), and mild hyperkeratotic plaques on the soles.
Fig 1.
Multiple mucocutaneous manifestations of malnutrition. The patient presented with (A) perifollicular petechial rash with ecchymoses, (B) corkscrew hairs, (C) gingival hemorrhages, and (D) palmar keratoderma.
Skin biopsy of the right thigh revealed a sparse perivascular and adnexal lymphocytic infiltrate (Fig 2, A) and mild follicular distortion with perifollicular hemorrhage (Fig 2, B). Laboratory studies were notable for undetectable vitamin C; folate, 3.9 ng/mL (normal range, 5.9-24.8 ng/mL); vitamin A, 0.22 mg/L (normal range, 0.3-1.2 mg/L); alpha tocopherol, 5.5 mg/L (normal range, 5.5-18 mg/L); 25-OH vitamin D, 6 ng/mL (normal range, 25-80 ng/mL); vitamin B6, 29 nmol/L (normal range, 20-125 nmol/L); thiamine 44 nmol/L (normal range, 70-180 nmol/L); thyroid-stimulating hormone, 7.99 uIU/mL (normal range, 0.45-5.33 uIU/mL); free T3, 0.81 ng/dL (normal range, 0.61-1.3 ng/dL); hemoglobin, 9.9 g/dL (normal range, 13.5-17.5 g/dL); and albumin, 3.1 g/dL (normal range, 3.5-5.1 g/dL). Additional workup, including levels of arsenic, zinc, vitamin B3, vitamin B12, and copper as well as autoimmune and infectious etiologies (including Whipple disease), was unremarkable. Arthrocentesis of his right knee revealed hemarthrosis. Esophagogastroduodenoscopy, colonoscopy, and magnetic resonance enterography did not reveal significant abnormalities. Ophthalmologic examination revealed bilateral superficial punctate keratosis of the eyes, blepharitis, and meibomian gland dysfunction. The patient was started on intravenous folate (1 mg daily) and intramuscular vitamin C (1000 mg daily) and then placed on daily oral folic acid 5 mg, ascorbic acid 1000 mg, and adult multivitamin with instructions to increase his caloric intake and diversify his diet.
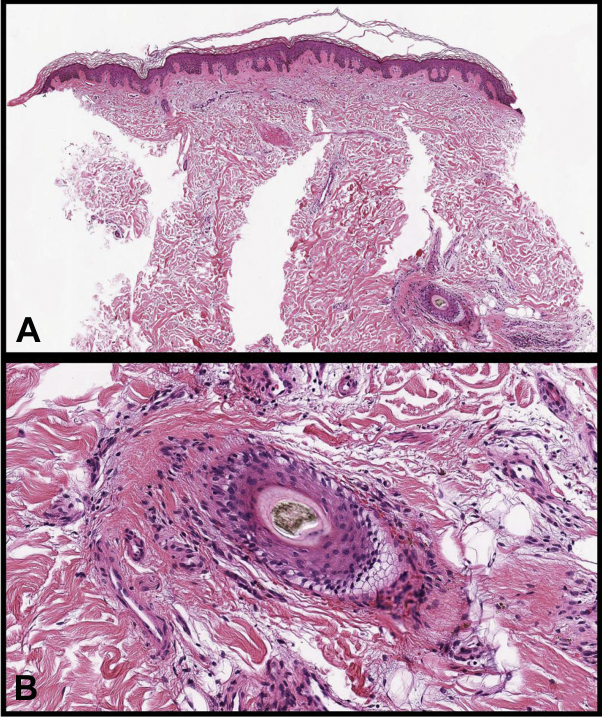
Fig 2.
Histopathology of perifollicular petechial rash. A, A punch biopsy specimen taken from the right leg demonstrated a sparse perivascular and adnexal lymphocytic infiltrate. B, Mild follicular distortion with perifollicular hemorrhage. (Original magnification: A, ×50; B, ×200.)
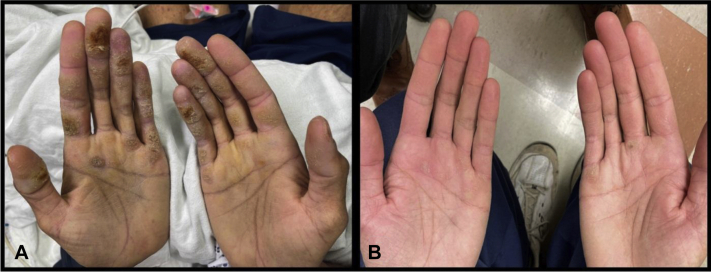
After 4 weeks of vitamin supplementation and improved diet, the patient’s weight increased by 20 pounds and his keratoderma resolved (Fig 3, A and B). Repeated laboratory tests revealed concentrations of vitamin C, 14 umol/L (normal range, 23-114 umol/L); folate, 5.3 ng/mL (normal range, 5.9-24.8 ng/mL); vitamin A, 0.34 mg/L (normal range, 0.3-1.2 mg/L); and vitamin B1, 76 nmol/L (normal range, 70-180 nmol/L).
Fig 3.
Clinical response to improved diet and vitamin supplementation. A, Palmar aspect of the patient’s hands on the day of admission. B, Palmar aspect of the patient’s hand 4 weeks after starting vitamin supplementation.
Discussion
Our patient’s clinical, laboratory, and histopathologic findings are consistent with malnutrition-induced scurvy and PPK. No underlying malabsorptive process or alcohol abuse disorder was identified, and his severe malnutrition has been attributed to avoidant/restrictive food intake disorder and/or intestinal dysmotility. Numerous causes of acquired PPK have been described, including chemicals, drugs, malnutrition, hypothyroidism, myxedema, inflammatory skin diseases, and infections.1,2 Given our patient’s extensive weight loss, there was significant concern for an undiagnosed malignancy. A thorough workup, including pan computed tomography scan, flow cytometry, endoscopy, and magnetic resonance enterography, was unrevealing. Instead, the most striking clinical and laboratory findings were related to severe malnutrition, including deficiency of vitamin A, thiamine, folate, vitamin C, and vitamin D. Our patient exhibited many of the classic mucocutaneous findings of scurvy, including perifollicular hemorrhages, corkscrew hairs, ecchymoses, splinter hemorrhages, and gingival hemorrhages, as well as extracutaneous manifestations, including hemarthrosis, anemia, and vasomotor instability (ie, transient low blood pressure).3 His dry eye syndrome may also be due to severe malnutrition, because both hypovitaminosis A and D are known causes of dry eye syndrome.4,5 Although other etiologies of his PPK were considered, including previously described causes of thyroid dysfunction1 and Whipple disease,6 resolution of his PPK after improvement in his overall nutritional status and vitamin repletion is most supportive of a nutritional etiology.
Malnutrition remains a recognized but poorly understood cause of acquired PPK. Several acquired vitamin deficiencies, including vitamin A, zinc, and thiamine deficiencies, are associated with an array of mucocutaneous manifestations. Vitamin A deficiency causes xerosis and leads to scaling and fissuring as well as follicular hyperkeratosis or phrynoderma.7,8 Zinc deficiency causes multifocal eczematous eruption characteristically localizing to the distal extremities, anogenital areas, and periorificial areas.8 Thiamine deficiency, or beriberi, is associated with waxy, edematous skin, and in 1 report, thiamine supplementation was associated with improvement in malnutrition-associated PPK.2,8 This report by Lee et al2 describes skin disorders, including cutaneous pigmentation, PPK, and nail changes, observed in the inmates at the Lake Xingkai State Farm concentration camp in Northeast China. Thousands of inmates who worked long hours with their hands developed protein energy malnutrition, vitamin deficiencies, and dry, calloused, fissured palms and soles. Similar to our patient, the palmar lesions were most severe over the finger tips. Interestingly, Lee et al2 reported that the hand lesions improved with empiric thiamine injections (50 mg once or twice), suggesting that thiamine deficiency in combination with mechanical trauma may induce a form of PPK. Our patient had a low serum thiamine level and worked as a cabinet maker, which may further support this theory. In the context of severe malnutrition and multiple vitamin deficiencies, it is difficult to identify a single culprit for our patient’s PPK despite these known dermatologic associations.
Because acquired PPKs are associated with a wide range of underlying etiologies, workup and treatment can be challenging for patients and practitioners. Our case demonstrates that malnutrition is an important and potentially underappreciated etiology of acquired PPK. This is exemplified by the resolution of our patient’s PPK solely with nutritional supplementation in the absence of keratolytics. If review of symptoms is notable for signs of weight loss, anorexia, or gastrointestinal symptoms, obtaining a detailed nutritional history is a key first step toward identifying risk factors for malnutrition. Prompt nutrition consultation and workup including serum vitamin concentrations should then be considered. Although traditional conservative treatment options for PPK, including topical keratolytics, retinoids, and topical steroids, may be beneficial,1 correction of the underlying vitamin deficiencies and poor nutritional state should be a primary focus of the treatment plan.
Conflicts of interest
None disclosed.
Acknowledgments
The authors thank the patient for his willingness to share his case. We thank Eric Palecek, MD for providing clinical images.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Patel S., Zirwas M., English J.C., III Acquired palmoplantar keratoderma. Am J Clin Dermatol. 2007;8(1):1–11. doi: 10.2165/00128071-200708010-00001. [DOI] [PubMed] [Google Scholar]
- 2.Lee B.Y., Hogan D.J., Ursine S., Yanamandra K., Bocchini J.A. Personal observation of skin disorders in malnutrition. Clin Dermatol. 2006;24(3):222–227. doi: 10.1016/j.clindermatol.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Kern M., Gardner J.M. Mucocutaneous manifestations of scurvy. N Engl J Med. 2020;382(20):e56. doi: 10.1056/NEJMicm1911315. [DOI] [PubMed] [Google Scholar]
- 4.Sommer A, West KP. Vitamin A Deficiency: Health, Survival and Vision. Oxford University Press; 1995:99-147.
- 5.Kurtul B.E., Özer P.A., Aydinli M.S. The association of vitamin D deficiency with tear break-up time and Schirmer testing in non-Sjögren dry eye. Eye (Lond) 2015;29(8):1081–1084. doi: 10.1038/eye.2015.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juárez Y., España S., Fernández-Díaz M.L., Lueiro M. Scurvy and acquired ichthyosis associated to Whipple’s disease. Article in Spanish. Actas Dermosifiliogr. 2006;97(9):587–590. doi: 10.1016/s0001-7310(06)73472-x. [DOI] [PubMed] [Google Scholar]
- 7.Nosewicz J., Spaccarelli N., Roberts K.M., et al. The epidemiology, impact, and diagnosis of micronutrient nutritional dermatoses part 1: zinc, selenium, copper, vitamin A, and vitamin C. J Am Acad Dermatol. 2022;86(2):267–278. doi: 10.1016/j.jaad.2021.07.079. [DOI] [PubMed] [Google Scholar]
- 8.Lee L.W., Yan A.C. Skin manifestations of nutritional deficiency disease in children: modern day contexts. Int J Dermatol. 2012;51(12):1407–1418. doi: 10.1111/j.1365-4632.2012.05646.x. [DOI] [PubMed] [Google Scholar]