Abstract
Background/Objectives:
The COVID-19 global outbreak allowed a natural experiment to observe how older adults changed social patterns and how it affected their emotional well-being. We studied the frequency and modes of social contact and their effects on older adults’ mood before and during the COVID-19 pandemic.
Design:
Phone-based surveys were administered weekly before and during the COVID-19 pandemic.
Setting:
Portland, Oregon; Detroit, Michigan.
Participants:
Older adults ≥ 75 years old (n=155, age=81.0±4.5, 72.3% women) in a randomized controlled trial, Internet-Based Conversational Engagement Clinical Trial (I-CONECT).
Measurements:
Low mood was self-reported as feeling downhearted or blue for three or more days in the past week. Social contact was self-reported by the amount of time spent in interactions, with whom (family; friends; others), and via which modes (in-person; phone/video-call; text/email/letter).
Results:
A total of 5,525 weeks of data was derived from 155 participants. Before the COVID-19 pandemic, average social interaction time spent in-person, on phone/video call, and via text/email/letter was 406, 141, and 68 minutes/week, respectively. During the COVID-19 pandemic, time spent in-person was reduced by 135 minutes/week, while time spent via phone/video-call and writing increased by 33 and 26 minutes/week, respectively. In-person family contact was associated with less low mood regardless of the pandemic (odds ratio=0.92, p<0.05). There was a COVID-19*text/email/letter with friends interaction (odds ratio=0.77, p=0.03), suggesting that during the COVID-19 pandemic, an increase of one hour of writing with friends per week was associated with a 23% decrease in the likelihood of experiencing low mood.
Conclusion:
The lost in-person time relating to COVID-19 restrictions tended to be partially compensated for with increased calls and writing time, although overall social interaction time decreased. During the COVID-19 pandemic, at least two types of social interactions (writing to friends, in-person family time) showed promise for mitigating low mood for older adults with limited social resources.
Keywords: stress, resilience, social isolation, virtual communication
Introduction
Meaningful social interactions have gained credibility to ward off the effects of stress on worsening immune function1, hypertension2, and cardiovascular health problems.3,4 Connecting with supportive social ties, including family members, friends, or healthcare providers5, is protective against depression via buffering the effects of stress and enhancing coping abilities.6 Conversely, limited social interactions may lead to maladaptation to stress (e.g., avoidance, withdrawal)7,8, depressive symptoms9, suicidal ideation10, slower recovery from illnesses11, cognitive decline and dementia12,13, and early death.14
Since the outbreak of the coronavirus disease 2019 (COVID-19), limiting social gathering and following stay-at-home orders have been critical to reducing exposure and spread of the virus. Although there is a common belief that older adults changed social patterns due to the outbreak of the COVID-19 pandemic to maintain psychological well-being, few studies had quantified the amount of change to test those hypotheses.7,15 Modes (in-person; phone/video-call; text/email/letter) of social interactions vary based on costs, availability, geographic restrictions, preferences, and previous experiences. Some older adults prefer in-person conversations, while others opt for video conferences, phone calls, texts, or emails.16 Less is known about whether older adults changed the modes to stay in touch with social ties after the COVID-19 pandemic and, if any, whether the change in social patterns was associated with low mood (blueness) over time.
This study examined the frequency and modes (in-person; phone/video call, text/email/letter) of social contact (family, friends, others) and their effects on mood using data collected before and during the COVID-19 pandemic in at-risk older adults (with limited social interactions prior to COVID-19). Since one of the recruitment states (Michigan) issued their first stay-at-home order on March 23, 2020, we treated data collected before March 23, 2020 as before the COVID-19 outbreak. The information gleaned from this study will inform our understanding of how increased socialization during the COVID-19 pandemic may help maintain emotional well-being for older adults with already limited social interactions before the COVID-19 pandemic.
Methods
Research design
This is a secondary data analysis of 155 participants from a randomized controlled trial, the Internet-Based Conversational Engagement Clinical Trial (I-CONECT, ClinicalTrials.gov: NCT02871921).17 The I-CONECT study examines whether enhancing social interaction via video-chat can improve cognitive function. This study is an extension of the previous pilot trial 18,19 where efficacy was shown. The experimental group participates in 30-minute video chats with trained conversational staff (4 times/week for the first 6 months, 2 times/week for additional 6 months) and weekly check-in telephone calls. The control group receives only weekly check-in calls. Participants were recruited from Detroit, Michigan, and Portland, Oregon. The project is explained in detail elsewhere.17 Briefly, in the I-CONECT study, inclusion criteria were age 75 or older, normal cognition or mild cognitive impairment (MCI) assessed by trial neuropsychologists and neurologists, and self-reported limited social interactions as defined by at least one of the following: 1) score ≤ 12 on the 6-item Lubben Social Network Scale (LSNS-6)20, 2) engagement in sustained conversations (30 minutes or longer) fewer than twice per week, per subject self-report, 3) answered “often” to at least one question on the 3-item UCLA Loneliness Scale21. Exclusion criteria included 1) having dementia, 2) severe depressive symptoms operationally defined as a 15-item Geriatric Depression Scale (GDS-15)22 score > 7, 3) current alcohol or substance abuse, 4) unstable medical conditions, 5) active systemic cancer within 5 years of the screening visit, or 6) surgery that required full sedation with intubation within 6 months of screening. Study approval was obtained from the Institutional Review Board at the Oregon Health & Science University (IRB 10005560) using a single IRB process. All the participants provided written informed consent and were included in the analysis (experimental and control groups). For the results presented in this manuscript, we included participants whose data were available as of August 2021.17
Weekly health questionnaire
All participants regardless of treatment group assignment received weekly check-in phone calls from research staff and answered survey questions addressing items listed below before and during the COVID-19 pandemic.
Low mood.
Low mood (“Blueness”) was identified via a self-report question: “Have you felt downhearted or blue for 3 or more days in the past week? (Yes/No)”
Social contact.
Social contact was self-reported by participants and included the amount of time spent in the previous week, with whom (family; friends; others), and via which modes (in-person; phone/video call; text/email/letter). The definition of family members included those to whom the participant is related to by birth, marriage, or adoption. The definition of friends included those whom the participant knows and has a bond of mutual affection, and those who live in the neighborhood. Others include anyone else, such as volunteers, healthcare providers, business people, or other hired help.
Participants were asked: 1) “Did you spend time with any family members (or friends/ others) in-person this week?” 2) “Did you spend time talking with any family members (or friends) on the phone or by video chat this week?” and “Did you spend time communicating with any family members (or friends) in writing, such as email, text, or letter writing this week?” If yes, there was a follow-up question about the time spent on each social contact “In total, how long did you meet with family (or friends; or others), counted in minutes or hours?” Response scores ranged from 0–7, with higher score indicating more time spent with the person. Response scores were converted into minutes for further analysis (60, 120, 180, 240, 300, and 360 minutes for response scores 1–2, 3, 4, 5, 6, and 7, respectively). Since participants received weekly calls from research staff and participated in video chats (if in the experimental group), only the time spent in-person was included as interactions with “others”.
Analytical approach
We compared the time spent with whom (family; friends; others) and via which modes (in-person; phone/video call (henceforth categorized as “call”); text/email/letter (henceforth categorized as “writing”)) before and during COVID-19 and their associations with low mood using a generalized estimating equations (GEE) logit model. In the GEE model, multiple weekly observations from each individual are included, while within-individual correlations are considered in estimating standard errors. The time before and during the COVID-19 pandemic (March 23, 2020) was indicated by a dummy variable (0/1). We included all the variables in one GEE model to identify which types of social interactions were beneficial to mood: seven types of social contact (in-person family, in-person friends, in-person others, call family, call friends, writing family, writing friends) and their interaction terms with the COVID-19 pandemic dummy variable. SAS procedure PROC GEE was used for the analysis.23
Participant characteristics (age, sex, race, years of education, marital status, depressive symptoms), living situation (alone, with a spouse or partner, with a relative, friend or roommate, with others), and treatment assignments (blinded as A vs. B) were included as covariates. Depressive symptoms were measured by the Geriatric Depression Scale-15 (GDS-15).24 The GDS-15 has 15 items; each item was scored as YES (1) or NO (0). A higher total score indicates more depressive symptoms.
Sex, living situation, and marital status may affect the relationship between COVID-19 and time spent in various social interaction types. Therefore, we conducted sensitivity analyses on significant COVID-19*social type terms through three-way interaction (COVID-19*friend writing*sex; COVID-19*friend writing*living situation; COVID-19*friend writing*marital status).
Results
One hundred fifty-five participants (age = 81.0 ± 4.5, 72.3% women) were included in the analysis (Table 1). A total of 5,525 weeks of survey data were analyzed (3,047 and 2,478 weeks before and during the COVID-19 pandemic, respectively). On average, 35.6 (SD = 11.6) weeks of data were collected per participant.
Table 1.
Participant baseline characteristics (n = 155)
| Characteristics | Mean±SD; n(%) |
|---|---|
| Age | 80.99 ± 4.51 |
| Female | 112 (72.3) |
| African American | 27 (17.4) |
| Years of education | 15.19 ± 2.24 |
| Marital status | |
| Married | 34 (21.9) |
| Widowed | 62 (40.0) |
| Divorced | 51 (32.9) |
| Other | 8 (5.2) |
| Living situation | |
| Live alone | 99 (63.9) |
| With a spouse/ partner | 33 (21.3) |
| With a relative, friend, roommate | 14 (9.0) |
| Other | 9 (5.8) |
| Depression, GDS-15 | 2.30 ± 1.76 |
GDS-15 (Geriatric Depression Scale-15)
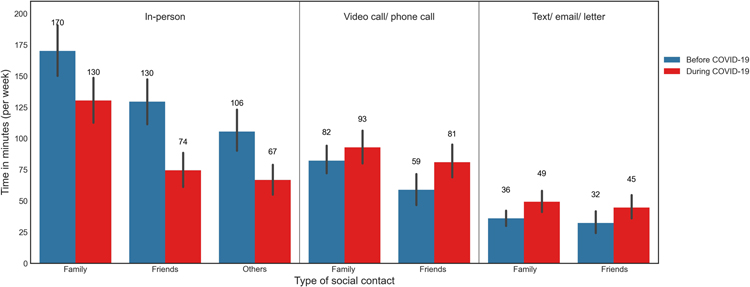
Before the COVID-19 pandemic, the weekly average time spent in-person, on calls, and via writing were 406, 141, and 68 minutes, respectively. On average, there was a 76-minute reduction in total social contact per week during the COVID-19 pandemic. During the COVID-19 pandemic, the time spent in-person had reduced by 135 minutes per week, while the time spent via call and writing increased by 33 and 26 minutes per week, respectively (Figure 1).
Figure 1.
Time spent on modes and types of social contact (per week) before and during the COVID-19 pandemic
Before COVID-19, the weekly average time spent in-person with family, friends, and others were 288, 221, and 106 minutes, respectively. During the COVID-19 pandemic, the time spent with family, friends, and others had reduced by 16, 21, 39 minutes per week, respectively (Figure 1).
The GEE model revealed that more in-person family contact was associated with less low mood regardless of the pandemic (odds ratio=0.92, p<0.05), suggesting that an increase of 1 hour of in-person family time per week was associated with a 8% decrease in the likelihood of experiencing sustained low mood (three or more days per week) (Table 2).
Table 2.
Generalized estimating equations model with the outcome being low mood (based on 5,525 weeks of survey data)
| Parameter | Estimate | SE | Odds ratio [95% CI] | p-value | |
|---|---|---|---|---|---|
| Intercept | 4.68 | 4.10 | 0.25 | ||
| COVID-19 event (yes/no) | −0.29 | 0.29 | 0.75 [0.43–1.32] | 0.32 | |
| Family | In-person time | −0.08 | 0.04 | 0.92 [0.86–0.99] | 0.046* |
| In-person time*COVID-19 | 0.05 | 0.05 | 1.05 [0.95–1.15] | 0.35 | |
| Video/call time | 0.02 | 0.05 | 1.02 [0.92–1.13] | 0.74 | |
| Video/call time*COVID-19 | 0.01 | 0.08 | 1.01 [0.86–1.19] | 0.90 | |
| Writing time | 0.12 | 0.08 | 1.13 [0.97–1.32] | 0.13 | |
| Writing time*COVID-19 | −0.06 | 0.12 | 0.94 [0.74–1.19] | 0.60 | |
| Friend | In-person time | −0.05 | 0.03 | 0.95 [0.89–1.02] | 0.18 |
| In-person time*COVID-19 | −0.02 | 0.07 | 0.98 [0.86–1.12] | 0.80 | |
| Video/call time | 0.04 | 0.08 | 1.04 [0.89–1.20] | 0.63 | |
| Video/call time*COVID-19 | 0.07 | 0.09 | 1.07 [0.91–1.28] | 0.40 | |
| Writing time | 0.02 | 0.07 | 1.02 [0.89–1.16] | 0.79 | |
| Writing time*COVID-19 | −0.26 | 0.12 | 0.77 [0.61–0.97] | 0.03* | |
| Others | In-person time | −0.004 | 0.04 | 1.00 [0.92–1.07] | 0.93 |
| In-person*COVID | 0.01 | 0.06 | 1.01 [0.90–1.13] | 0.84 | |
| Demographics | Age | −0.13 | 0.04 | 0.88 [0.81–0.95] | <0.01* |
| Gender, female | 0.90 | 0.54 | 2.46 [0.85–7.12] | 0.10 | |
| Race, White | 0.43 | 0.34 | 1.54 [0.79–2.98] | 0.21 | |
| Education, years | 0.06 | 0.08 | 1.06 [0.90–1.25] | 0.47 | |
| Depression severity | 0.25 | 0.09 | 1.28 [1.08–1.52] | <0.01* | |
| Marital status, married | 0.02 | 0.66 | 1.02 [0.28–3.69] | 0.98 | |
| Living situation, alone | 0.16 | 0.49 | 1.17 [0.45–3.06] | 0.75 | |
| Treatment group (blinded as A vs. B) | 0.09 | 0.29 | 1.09 [0.62–1.95] | 0.76 |
Note:
p<0.05; All the variables were included in one GEE model.
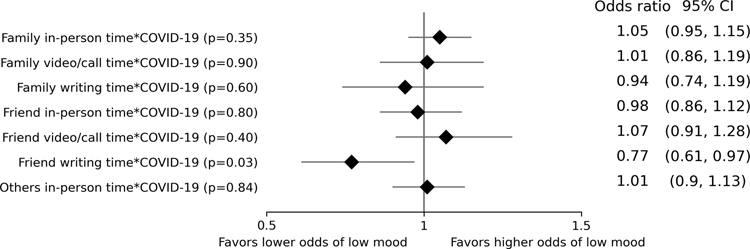
There was a COVID-19*writing time with friends interaction (odds ratio=0.77, p=0.03), suggesting that during the COVID-19 pandemic, an increase of 1 hour of writing with friends per week was associated with a 23% decrease in the likelihood of experiencing sustained low mood (three or more days per week) (Table 2; Figure 2). Sensitivity results showed that there were no sex, living situation, or marital status effects on the relationship between writing to friends and mood during the COVID-19 pandemic (p=0.73; p=0.98; p=0.78).
Figure 2.
Forest plot showing the odds ratio of social interaction time and COVID-19 interaction effect on incident low mood
Discussion
Using longitudinal data collected before and during the COVID-19 pandemic, we provide evidence to support a common belief that older adults had changed social patterns (frequency, modes) due to COVID-19 restrictions. We further examined how changes in social interactions may affect low mood in a group of at-risk older adults (with limited social interactions before COVID-19). Our data showed that the lost in-person time due to COVID-19 restrictions tended to be partially compensated for with increased calls and writing time, although the overall social interaction time decreased. During the COVID-19 pandemic, at least two types of social interactions (writing to friends, in-person family time) showed promise for mitigating low mood. The current study shows that, during a disease outbreak that may cause mental adversity, maintaining social ties with a bond of mutual affection (family and friends) is essential to increase emotional resilience.
Our first finding was that, although participants temporarily substituted face-to-face contact with calls and writing instead during the COVID-19 pandemic, there was still an approximately 76-minute reduction in total social contact per week. In our sample, 64% of volunteers lived alone – compared to approximately 28% of all noninstitutionalized older adults lived alone in the United States in 2018.25 This unique sample offered the opportunity to study the social pattern changes in a group of at-risk older adults before and during the COVID-19 pandemic. Notably, even a small amount of lost social interaction time can be stressful, leading to further negative consequences if the situation is not managed and intervened.7,26 The Conservation of Resources theory posits that resource loss (in our case, lost social interaction time) is stressful, and individuals must invest resources to offset further resource loss.27 Otherwise, individuals may be vulnerable to an ongoing loss called “an action of loss spirals.” For example, studies found that under stress, at-risk individuals were more likely to alienate support due to emotional turbulences, putting them in a socially isolated situation.9 In a socially isolated situation, individuals may not be able to access limited resources outside their social circle28, therefore possibly creating a vicious cycle.
Our second finding was that, during the COVID-19 pandemic, at least two social activities (in-person family interaction, writing with friends) showed promise for maintaining mood in older adults with limited social interactions. This finding is in line with previous population-based observational studies. Increased in-person family time but not telephone or written time predicted decreased depression in older adults.29 A higher frequency of connecting with friends was found to be associated with a lower likelihood of depression in older adults but not younger adults.30,31 Our finding builds on these studies by examining modes of communication within social ties during a disease outbreak. Many possibilities may explain the effect of writing (text/email/letter) with friends on mood. First, qualitative studies have found that older adults prefer letter writing because it affords a personal touch with varying degrees of format (content, tone, paper style) to cultivate strong ties and reconnect with weak ties.16 Alternatively, vulnerable populations like socially isolated older adults tend to be excluded from technology-based communication services which require video capabilities (e.g., lack mobile devices and faster network connectivity). The lack of experience in using the technology may be a hurdle for vulnerable older adults as well.32 These possibilities may explain why we did not see an effect of trial group (video chat experimental group vs. control group) on mood that previous longitudinal studies have shown.15,33
We recognize this study had certain limitations. Psychological well-being was indicated by one question asked weekly over time, i.e., low mood. This dichotomous mood item has been used in previous studies34,35 and showed its sensitivity to detect mood changes before and during the COVID-19 pandemic.35 Yet we cannot describe the severity or symptoms of depression from a single question. The amount of social interaction was self-reported. However, unlike traditional survey approaches where assessment occurs infrequently (e.g., annually), we collected data weekly asking about activities in the previous week, which reduced the recall bias. A previous daily diary-based study showed that older adults spent approximately 245–294 minutes per week connecting with family.36 In the current study, older adults with limited social interactions reported on average 288 minutes of family contact per week before the COVID-19 pandemic. The similarity in total family contact time among older adults between these two methodologies provides support that weekly surveys have sufficient resolution to measure social contact frequency as daily diaries, for which the latter is often impractical over the long term. Future studies may use commercial software to quantify social media time and video/ phone calls objectively.37 Additionally, we did not attempt to describe the strength and quality of social ties, which might affect their emotional states. Further, more research on the type of conversations and individual personality traits would increase our understanding of the emotional and structural needs of older adults with limited social interactions (e.g., relieving stress, catching up on news, reassuring of worth, needing instrumental help).19 Finally, the participants included in this study were free from severe depressive symptoms (using operational criteria using the GDS-15) and dementia. Therefore, the generalizability of our study findings is limited.
Lack of social interactions is a modifiable risk factor for various adverse health outcomes. The COVID-19 pandemic global outbreak allowed a natural experiment to observe how older adults modified their social patterns and how COVID-19 restrictions affected their emotional well-being. The evidence collected from this study can be used in many ways. When designing interventions that aim to reduce health adversity by increasing types and frequencies of social interactions, the “dosage” of social types can be referenced from this study.38 Following those who could and could not compensate for their lost interaction time during the COVID-19 pandemic is warranted to identify the impact of this pandemic on longitudinal outcomes.
Key Points:
There was approximately a 76-minute reduction in total social contact per week due to the COVID-19 pandemic in older adults with limited social interactions.
Amid the COVID-19 pandemic, increased time in two social activities (writing to friends, in-person family interaction) showed promise for mitigating low mood.
Why does this matter?
The evidence collected from this study can be referenced in future disease outbreaks to provide effective social interactions for socially isolated older adults.
Acknowledgment
We would like to thank participants in the I-CONECT study.
Funding:
This work was supported by the National Institutes of Health (AG051628, AG056102, P30AG066518).
Footnotes
Conflict of interest: HHD serves as a consultant for Biogen. Other authors have no conflicts.
Sponsor’s Role: The sponsor had no role in the design, methods, data collection, analysis, or preparation of the article.
References
- 1.Shields GS, Spahr CM, Slavich GM. Psychosocial interventions and immune system function: A systematic review and meta-analysis of randomized clinical trials. JAMA psychiatry. 2020;77(10):1031–1043. doi: 10.1001/jamapsychiatry.2020.0431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sneed RS, Cohen S. Negative social interactions and incident hypertension among older adults. Heal Psychol. 2014;33(6):554. doi: 10.1037/hea0000057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lepore SJ, Allen KA, Evans GW. Social support lowers cardiovascular reactivity to an acute stressor. Psychosom Med. 1993;55(6):518–524. doi: 10.1097/00006842-199311000-00007 [DOI] [PubMed] [Google Scholar]
- 4.Uchino BN, Holt-Lunstad J, Uno D, Flinders JB. Heterogeneity in the social networks of young and older adults: Prediction of mental health and cardiovascular reactivity during acute stress. J Behav Med. 2001;24(4):361–382. doi: 10.1023/a:1010634902498 [DOI] [PubMed] [Google Scholar]
- 5.Razai MS, Oakeshott P, Kankam H, Galea S, Stokes-Lampard H. Mitigating the psychological effects of social isolation during the covid-19 pandemic. bmj. 2020;369:1–5. doi: 10.1136/bmj.m1904 [DOI] [PubMed] [Google Scholar]
- 6.McInnis OA, McQuaid RJ, Matheson K, Anisman H. The moderating role of an oxytocin receptor gene polymorphism in the relation between unsupportive social interactions and coping profiles: Implications for depression. Front Psychol. 2015;6:1133. doi: 10.3389/fpsyg.2015.01133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kotwal AA, Holt-Lunstad J, Newmark RL, et al. Social isolation and loneliness among San Francisco bay area older adults during the COVID-19 shelter-in-place orders. J Am Geriatr Soc. 2021;69(1):20–29. doi: 10.1111/jgs.16865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robb CE, de Jager CA, Ahmadi-Abhari S, et al. Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: A survey of older adults in London, UK. Front Psychiatry. 2020;11:1–12. doi: 10.3389/fpsyt.2020.591120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santini ZI, Jose PE, Cornwell EY, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Heal. 2020;5(1):e62–e70. doi: 10.1016/S2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- 10.Wand APF, Zhong B-L, Chiu HFK, Draper B, De Leo D. COVID-19: The implications for suicide in older adults. Int psychogeriatrics. 2020;32(10):1225–1230. doi: 10.1017/S1041610220000770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaw JG, Farid M, Noel-Miller C, et al. Social isolation and medicare spending: Among older adults, objective isolation increases expenditures while loneliness does not. J Aging Health. 2017;29(7):1119–1143. doi: 10.1177/0898264317703559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–446. doi: 10.1016/S0140-6736(20)30367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans IEM, Martyr A, Collins R, Brayne C, Clare L. Social isolation and cognitive function in later life: A systematic review and meta-analysis. J Alzheimer’s Dis. 2019;70(s1):S119–S144. doi: 10.3233/JAD-180501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237. doi: 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- 15.Hajek A, König H-H. Social isolation and loneliness of older adults in times of the CoViD-19 pandemic: Can use of online social media sites and video chats assist in mitigating social isolation and loneliness? Gerontology. 2021;67(1):121–124. doi: 10.1159/000512793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hope A, Schwaba T, Piper AM. Understanding digital and material social communications for older adults. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems.; 2014:3903–3912. doi: 10.1145/2556288.2557133 [DOI] [Google Scholar]
- 17.Yu K, Wild K, Potempa K, et al. The Internet-based conversational engagement clinical trial (I-CONECT) in socially isolated adults 75+ years old: Randomized controlled trial protocol and COVID-19 related study modifications. Front Digit Heal. 2021;3:1–14. doi: 10.3389/fdgth.2021.714813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dodge HH, Zhu J, Mattek NC, et al. Web-enabled conversational interactions as a method to improve cognitive functions: Results of a 6-week randomized controlled trial. Alzheimer’s Dement Transl Res Clin Interv. 2015;1(1):1–12. doi: 10.1016/j.trci.2015.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cerino ES, Hooker K, Goodrich E, Dodge HH. Personality moderates intervention effects on cognitive function: A 6-week conversation-based intervention. Gerontologist. 2020;60(5):958–967. doi: 10.1093/geront/gnz063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lubben J, Blozik E, Gillmann G, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46(4):503–513. doi: 10.1093/geront/46.4.503 [DOI] [PubMed] [Google Scholar]
- 21.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin Gerontol J Aging Ment Heal. 1986;5(1–2):165–173. doi: 10.1300/J018v05n01_09 [DOI] [Google Scholar]
- 23.SAS Institute Inc. SAS software version 9.4, Cary, NC, USA. [Google Scholar]
- 24.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- 25.Administration for Community Living. 2019 Profile of Older Americans. Washington, DC; 2019. [Google Scholar]
- 26.Cacioppo JT, Hawkley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46(3):S39–S52. doi: 10.1353/pbm.2003.0063 [DOI] [PubMed] [Google Scholar]
- 27.Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Appl Psychol. 2001;50(3):337–421. doi: 10.1111/1464-0597.00062 [DOI] [Google Scholar]
- 28.Harasemiw O, Newall N, Shooshtari S, Mackenzie C, Menec V. From social integration to social isolation: The relationship between social network types and perceived availability of social support in a national sample of older Canadians. Res Aging. 2018;40(8):715–739. doi: 10.1177/0164027517734587 [DOI] [PubMed] [Google Scholar]
- 29.Teo AR, Choi H, Andrea SB, et al. Does mode of contact with different types of social relationships predict depression in older adults? Evidence from a nationally representative survey. J Am Geriatr Soc. 2015;63(10):2014–2022. doi: 10.1111/jgs.13667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Werner-Seidler A, Afzali MH, Chapman C, Sunderland M, Slade T. The relationship between social support networks and depression in the 2007 National Survey of Mental Health and Well-being. Soc Psychiatry Psychiatr Epidemiol. 2017;52(12):1463–1473. doi: 10.1007/s00127-017-1440-7 [DOI] [PubMed] [Google Scholar]
- 31.Fiori KL, Antonucci TC, Cortina KS. Social network typologies and mental health among older adults. Journals Gerontol Ser B Psychol Sci Soc Sci. 2006;61(1):P25–P32. doi: 10.1093/geronb/61.1.P25 [DOI] [PubMed] [Google Scholar]
- 32.Seifert A, Cotten SR, Xie B. A double burden of exclusion? Digital and social exclusion of older adults in times of COVID-19. Journals Gerontol Ser B. 2020;76(3):e99–e103. doi: 10.1093/geronb/gbaa098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teo AR, Markwardt S, Hinton L. Using Skype to beat the blues: Longitudinal data from a national representative sample. Am J Geriatr Psychiatry. 2019;27(3):254–262. doi: 10.1016/j.jagp.2018.10.014 [DOI] [PubMed] [Google Scholar]
- 34.Thielke SM, Mattek NC, Hayes TL, et al. Associations between observed in-home behaviors and self-reported low mood in community-dwelling older adults. J Am Geriatr Soc. 2014;62(4):685–689. doi: 10.1111/jgs.12744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leese MI, Bernstein JPK, Dorociak KE, et al. Older Adults’ daily activity and mood changes detected during the COVID-19 pandemic using remote unobtrusive monitoring technologies. Innov Aging. 2021;5(4):1–9. doi: 10.1093/geroni/igab032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cornwell B Age trends in daily social contact patterns. Res Aging. 2011;33(5):598–631. doi:/ 10.1177/0164027511409442 [DOI] [Google Scholar]
- 37.Kaye J, Mattek N, Dodge HH, et al. Unobtrusive measurement of daily computer use to detect mild cognitive impairment. Alzheimer’s Dement. 2014;10(1):10–17. doi: 10.1016/j.jalz.2013.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anstey KJ, Peters R, Zheng L, et al. Future directions for dementia risk reduction and prevention research: An international research network on dementia prevention consensus. J Alzheimer’s Dis. 2020;(Preprint):1–10. doi: 10.3233/JAD-200674 [DOI] [PMC free article] [PubMed] [Google Scholar]