Abstract
Objective:
Suicide among Black youth is a significant public health concern, yet research investigating the epidemiology of suicide in this population is limited. This study examines current trends and precipitating circumstances of suicide by sex and age group in Black youth 5 to 17 years of age, using 2 national databases.
Method:
Data from the Web-based Injury Statistics Query and Reporting System (WISQARS) and the National Violent Death Reporting System (NVDRS) were used to investigate trends and precipitating circumstances of Black youth suicide from 2003 to 2017. We hypothesized suicide rates would increase over time for both sexes and all age groups (5–11, 12–14, and 15–17 years), and precipitating circumstances would differ by sex and age group. Trend analyses were conducted using Joinpoint regression software, version 4.8.0.01 (Surveillance Research Program, National Cancer Institute). Sex and age group comparisons of characteristics and precipitating circumstances were conducted using standard univariate statistical tests.
Results:
From 2003 to 2017, Black youth experienced a significant upward trend in suicide with the largest annual percentage change in the 15- to 17-year age group and among girls (4.9% and 6.6%, respectively). Mental health problems, relationship problems, interpersonal trauma and life stressors, and prior suicidal thoughts/behavior were the most common clinical characteristics and precipitating circumstances, with several varying by sex and age group.
Conclusion:
Increases in Black youth suicide calls for the prioritization of research aimed at identifying specific risk and protective factors as well as developmental mechanisms associated with Black youth suicidal behavior. To implement effective suicide prevention programming, understanding targets for intervention is necessary.
Keywords: Black youth suicide, NVDRS, age- and sex-specific trends
In the United States, suicide is the second leading cause of death in youths 5 to 17 years of age.1 In 2019, a total of 1,646 suicide deaths were reported, and more than 111,000 cases of self-harm behavior were seen in hospitals nationwide for this age group.1,2 Over the past decade, youth suicidal ideation and attempts have also increased substantially.3,4
Recent reports note the emergence of a racial disparity regarding youth suicide and suicidal behavior.4–7 In a national study combining suicide mortality data from 2001 to 2015, Black youths aged 5 to 12 years were approximately 2 times more likely to die by suicide than their White counterparts, a finding observed in boys and girls.6 A recent study using national Youth Risk Behavior Survey surveillance data revealed a significant increase in self-reported suicide attempts for Black youth between 2009 and 2019.4 Although racial disparities have been observed, the research investigating risk and protective factors and circumstances surrounding Black youth suicide is limited.8
Suicide risk in Black youth may differ from youth of other races and ethnicities. Risks for suicide among Black youth include experiences with racism and discrimination, racial disparities in mental health care utilization, poverty, trauma, violence, and exposure to the death among Black individuals in their neighborhoods and viewed through media outlets, which have all been found to have a disproportionate impact on Black youth.9–13 These factors faced by Black youth may cause the presentation of common risks linked to suicidal behavior (eg, depression) to present differently for Black youth compared to others.11,12,14 Understanding the risks for Black youth suicide and suicidal behavior is vital for the prevention of these behaviors. This is why the Congressional Black Caucus Emergency Taskforce on Black Youth Suicide9 and the National Institute of Mental Health (NIMH)8 have made it a priority for researchers to examine antecedents associated with suicide risk in Black youth.
The current study investigates trends and precipitating circumstances of suicide in Black youths aged 5 to 17 years, using national data from the Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System (WISQARS)1 and the National Violent Death Reporting System (NVDRS)15 from 2003 to 2017. We hypothesized that trends in Black youth suicide would increase during this timeframe, and that differences in characteristics and precipitating circumstances of suicide would be observed by sex and age group (5–11, 12–14, and 15–17 years). Identifying individual characteristics and precipitating circumstances associated with suicide in Black youth can inform targeted prevention strategies to reduce suicidal behavior in this traditionally understudied population of youth.
METHOD
Data from CDC-WISQARS1 and the NVDRS database15 were extracted by year for all Black youths 5 to 17 years of age who died by suicide from 2003 to 2017. We focused on the period from 2003 to 2017 because NVDRS data beyond 2017 are not yet publicly available. CDC-WISQARS is a national database that provides information on fatal injuries including the total number of deaths and rate per 100,000 for each cause of death.1 Data were obtained where the underlying cause of death code was listed as suicide (coded as X60-X84, Y87.0, and *U03 for the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10).
Characteristics and precipitating circumstances for suicide decedents were obtained from the NVDRS, a state-based surveillance system that collects data on suicide and violent deaths.15 NVDRS contains data from multiple sources including law enforcement agencies, coroner reports, medical examiners, crime laboratories, and death certificates. NVDRS currently exists in all 50 states; however, restricted use data on precipitating circumstances are available in only 35 states, Washington, DC, and Puerto Rico. Participating states included the following: Alaska, Arizona, California, Colorado, Connecticut, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Maine, Maryland, Massachusetts, Michigan, Minnesota, Nevada, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, Utah, Virginia, Washington, and Wisconsin.
Given developmental considerations of very young children, suicide is never coded as a cause of death for children ≤4 years1; therefore, the lower age limit in this study was 5 years. The upper age limit of 17 years was chosen to allow age group comparisons of elementary school–aged, early adolescent, and middle adolescent Black suicide decedents.
The total sample of Black youth suicide decedents from the NVDRS who met the inclusion criteria for age included 637 suicide deaths. For 38 of the cases, the underlying cause of death was not listed or was not coded as a suicide based on the ICD-10 (X60-X84, Y87.0, and U03). All 38 cases were reviewed by 3 of the authors (AHS, FV, and JAB) to ensure that the deaths were actual suicides. Of the 38 cases, 11 were deemed not suicide deaths. The final sample from NVDRS included 626 Black youths suicide decedents. This study was considered exempt according to review policies of the Institutional Review Board at the Abigail Wexner Research Institute at Nationwide Children’s Hospital.
A comparative sample of youth of other racial and ethnic backgrounds (eg, White, Asian, etc) was not included for this study, as the goal was to concentrate specifically on trends and precipitating circumstances in Black youth suicide decedents. Suicide literature investigating Black youth only is extremely limited, and the rates of suicide and suicidal behavior continue to rise in this population of youth.9,11–13 To prevent suicide and suicidal behavior in Black youth, setting the foundation of a comprehensive understanding of the current trends and risk factors associated with these behaviors that are specific to this population is essential.9,11–13 This study begins to address this issue.
Data Analysis
Trends in suicide rates by age group and sex were assessed using CDC-WISQARS data.1 Joinpoint regression, version 4.8.0.01 (Surveillance Research Program, National Cancer Institute), was used to test the significance of trends in suicide rates by age group and sex. The annual percent change (APC) was calculated and used to facilitate comparisons of trends by age group and sex.
Individual characteristics of suicide obtained from NVDRS included sex, age, ethnicity, suicide method, and injury location. Clinical characteristics included current mental health problem and/or treatment, mental health diagnosis, alcohol/drug-related circumstances, presence of alcohol or drugs at time of death, and physical health concerns. Precipitating circumstances of suicide included relationship problems (eg, family problem), history of abuse, interpersonal violence experiences (victim or perpetrator), school problems, death of a family member or friend, legal problems, and suicide-related circumstances (eg, disclosed intent to die by suicide).15 Categorical data were compared between age groups and sex using the χ2 statistic or Fisher’s exact test (FET), as indicated. Statistical significance was set at p < .05 (2-tailed). Statistical analyses were performed with SPSS, version 26.0.16
RESULTS
Suicide Trend Analyses Using CDC-WISQARS Data
From 2003 to 2017, a total of 1,810 suicide deaths occurred in Black youths (aged 5–11 years, n = 191; 12–14 years, n = 514; 15–17 years, n = 1,105; in all, 1,299 deaths for boys and 511 for girls), for an overall rate of 1.36 per 100,000. During this period, all age groups experienced a significant upward trend in suicide rates (Figure 1a–c). Black youth 15 to 17 years of age showed the largest significant increase (APC = 4.9%, 95% CI = 2.93–6.90, p < .001), followed by youth 5 to 11 years of age (APC = 3.9%, 95% CI = 1.42–6.68, p < .001) and youth 12 to 14 years of age (APC = 2.9%, 95% CI = 1.04–5.92, p < .006). For sex, both Black boys and girls experienced a significant upward trend in suicide rates, with the annual percent increase among Black girls (APC = 6.6, 95% CI = 4.12–9.10, p < .001) more than twice that of Black boys (APC = 2.8, 95% CI = 1.73–4.02, p < .001) (Figure 2).
FIGURE 1.
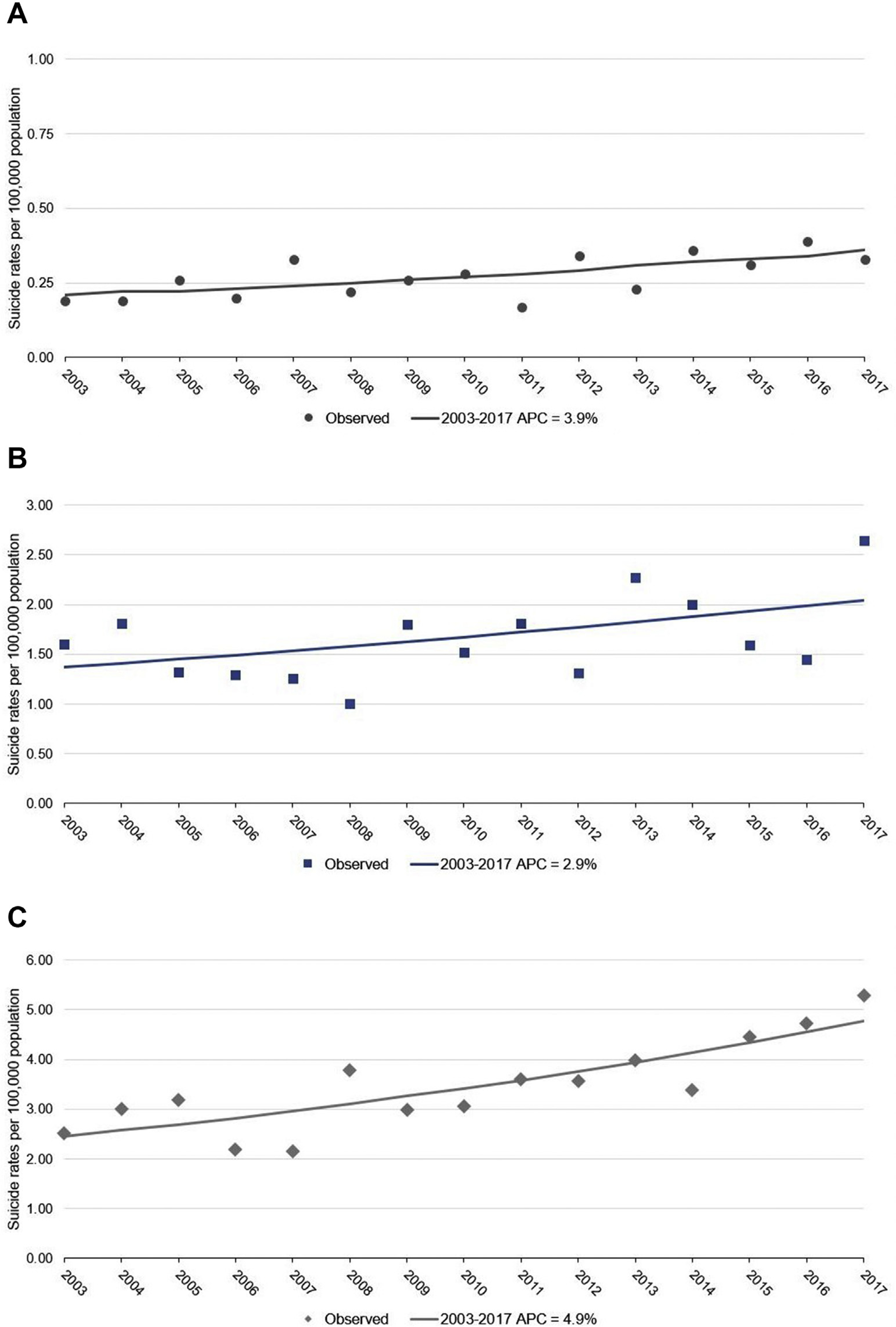
Suicide Trends Among Black Youth Aged 5–17 Years in the United States from CDC-WISQARS (2003–2017)
Note: (A) Ages 5–11 years. (B) Ages 12–14 years. (C) Ages 5–17 years. aAPC = annual percent change. CDC-WISQARS = Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System.
FIGURE 2.
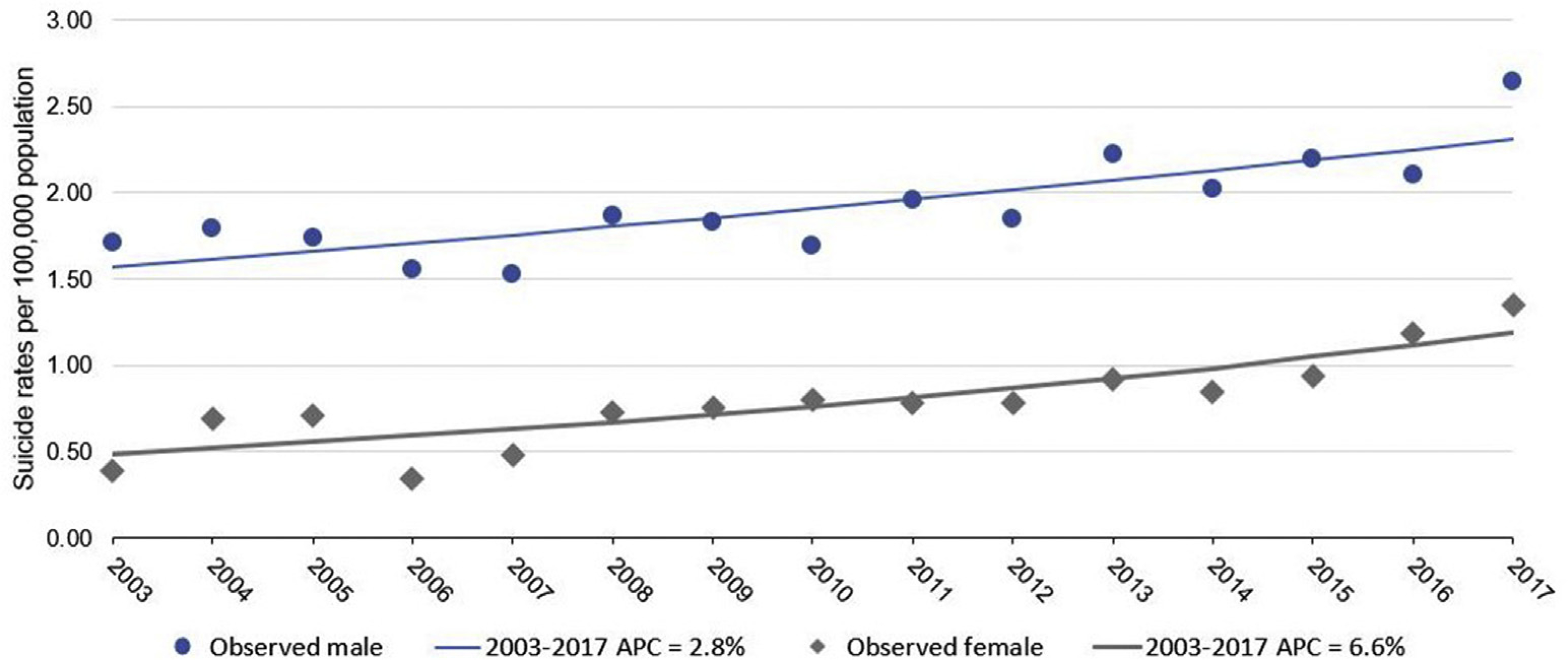
Suicide Trends by Sex Among Black Youth Aged 5 to 17 Years in the United States, from CDC-WISQARS (2003–2017)
Note: aAPC = annual percent change. CDC-WISQARS = Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System
NVDRS Analyses by Age Group
Overall, Black youth suicide decedents were mostly boys (71.4%), non-Hispanic (96.5%), and between 15 and 17 years of age (58.9%). In addition, the decedents were more likely to have died by hanging/strangulation/suffocation (62.1%) and to have done so in their own residence (78.9%) (Table 1).
TABLE 1.
Characteristics and Precipitating Circumstances of Black Youth Suicide Decedents Aged 5–17 Years in the United States, From the National Violent Data Reporting System (NVDRS) (2003–2017)
|
Age 5–11 y (n = 75)
|
Age 12–14 y (n = 182)
|
Age 15–17 y (n = 369)
|
Statistic | df | p | ||||
| Characteristic | n | % | n | % | n | % | |||
| Sex (% girls) | 14a | 18.7 | 68b | 37.4 | 97a | 26.3 | χ2 = 11.44 | 2 | .003 |
| Ethnicity | FET | .792 | |||||||
| Non-Hispanic | 73 | 97.3 | 176 | 96.7 | 355 | 96.2 | |||
| Hispanic | 1 | 1.3 | 4 | 2.2 | 11 | 3.0 | |||
| Unknown | 1 | 1.3 | 1 | 0.5 | 2 | 0.5 | |||
| Suicide Method | χ2 = 76.08 | 4 | <.001 | ||||||
| Hanging, strangulation, or suffocation | 69 | 92.0 | 141 | 77.5 | 179 | 48.5 | |||
| Firearm | 4 | 5.3 | 33 | 18.1 | 157 | 42.5 | |||
| Poisoning and other methodsa | 2 | 2.7 | 8 | 4.4 | 33 | 8.9 | |||
| Injury occurred at decedent’s residence (% Yes) | 71a | 94.7 | 161a | 88.5 | 262b | 71.0 | χ2 = 39.75 | 3 | <.001 |
| Precipitating Circumstances b | |||||||||
| Relationship problems | |||||||||
| Boyfriend/girlfriend problem | 1a | 1.4 | 10a | 6.5 | 65b | 19.9 | FET | <.001 | |
| Boyfriend/girlfriend problem was a crisis | 1a | 1.4 | 3a | 1.9 | 26b | 8.0 | FET | .007 | |
| Family problem | 26a | 37.7 | 56a | 36.4 | 73b | 22.3 | χ2 = 13.71 | 2 | .001 |
| Family problem was a crisis | 10a | 14.5 | 27a | 17.5 | 26a,b | 8.0 | χ2 = 10.19 | 2 | .006 |
| Friend problem | 15 | 21.7 | 33 | 21.4 | 55 | 16.8 | χ2 = 1.93 | 2 | .381 |
| Friend problem was a crisis | 0 | 0.0 | 2 | 1.3 | 6 | 1.8 | FET | .778 | |
| Precipitating Circumstances b |
Age 5–11 y (n = 75)
|
Age 12–14 y (n = 182)
|
Age 15–17 y (n = 369)
|
||||||
| n | % | n | % | n | % | Statistic | df | p | |
| Interpersonal Trauma and Life Stressors | |||||||||
| Decedent had a history of abuse | 4 | 5.8 | 3 | 1.9 | 8 | 2.4 | FET | .257 | |
| Suicide directly precipitated by abuse | 0 | 0.0 | 3 | 1.9 | 1 | 0.3 | FET | .147 | |
| Perpetrator of interpersonal violence | 2 | 2.9 | 4 | 2.6 | 15 | 4.6 | FET | .655 | |
| Victim of interpersonal violence | 0 | 0.0 | 3 | 1.9 | 2 | 0.6 | FET | .247 | |
| Involved in physical fight immediately before death | 1 | 1.4 | 1 | 0.6 | 3 | 0.9 | FET | .844 | |
| An argument or conflict led to the decedent’s death | 13 | 18.8 | 42 | 27.3 | 59 | 18.0 | χ2 = 5.60 | 2 | .061 |
| Timing of the argument that led to death | |||||||||
| Injury occurred during argument | 0 | 0.0 | 0 | 0.0 | 7 | 2.1 | FET | .116 | |
| Injury occurred within 24 h of argument | 10a | 14.5 | 31a | 20.1 | 33a,b | 10.1 | χ2 = 9.13 | 2 | .010 |
| Injury occurred between 24 h and 2 wk | 0 | 0.0 | 1 | 0.6 | 5 | 1.5 | FET | .593 | |
| Physical health problem | 2 | 2.9 | 2 | 1.3 | 11 | 3.4 | FET | .474 | |
| School problem | 23a | 33.3 | 57a | 37.0 | 70b | 21.4 | χ2 = 14.32 | 2 | .001 |
| School problem was a crisis | 6a | 8.7 | 13a | 8.4 | 12a,b | 3.7 | χ2 = 5.87 | 2 | .053 |
| Death of friend or family member | 5 | 7.2 | 9 | 5.8 | 19 | 5.8 | χ2 = 0.22 | 2 | .897 |
| Crime and Criminal Activity | |||||||||
| Recent criminal legal problem | 0a | 0.0 | 6a | 3.9 | 32b | 9.8 | FET | .002 | |
| Other legal problem | 0 | 0.0 | 2 | 1.3 | 8 | 2.4 | FET | .471 | |
| Suicide-Related Circumstances | |||||||||
| History of suicidal thoughts or plans | 12 | 17.4 | 24 | 15.6 | 52 | 15.9 | χ2 = 0.12 | 2 | .941 |
| History of suicide attempt | 10 | 14.5 | 27 | 17.5 | 56 | 17.1 | χ2 = 0.34 | 2 | .844 |
| Suicide intent disclosed within past month | 19 | 27.5 | 24 | 15.6 | 72 | 22.0 | χ2 = 4.72 | 2 | .095 |
| Suicide note | 8a | 11.6 | 33a | 21.4 | 83b,a | 25.4 | χ2 = 6.36 | 2 | .042 |
| Recent suicide of friend or family member | 1 | 1.4 | 3 | 1.9 | 6 | 1.8 | FET | .967 | |
Note: FET = Fisher’s exact test.
Other suicide methods include fall, transportation-related, drowning, cut/pierce, fire/burn, overdose, and unspecified methods.
Precipitating circumstances were known in 550 youths: 5–11 y (n = 69); 12–14 y (n = 154); 15–17 y (n = 327).
Within the 12- to 14-year-old group, the proportion of Black girls was higher (37.4%) compared to the 5- to 11-year-old (18.7%) and 15- to 17-year-old (26.3%) groups (χ2 = 11.44, df = 2, p = .003). For suicide method, the highest proportion of hanging/strangulation/suffocation was observed in the 5- to 11-year-old (92%) and 12- to 14-year-old (77.5%) groups, and the highest proportion of firearm suicides was present in the 15- to 17-year-old group (42.5%; χ2 = 76.08, df = 4, p < .001). Regarding location of death, 5- to 11-year-old (94.7%) and 12- to 14-year-old (88.5%) Black suicide decedents had a higher proportion of suicides occur in their residence compared to the older age group (71.0%; χ2 = 39.75, df = 3, p < .001).
Regarding precipitating circumstances, 550 (87.9%) Black youths (aged 5–11 years, n = 69; 12–14 years, n = 154; and 15–17 years, n = 327) had circumstances marked in NVDRS as known and were included in the data analysis. For age group analyses (Tables 1 and 2), differences were found for relationship problems, timing of arguments prior to death, school problems, crime/criminal activity, leaving a suicide note, mental health diagnoses, and substance use concerns.
TABLE 2.
Clinical Characteristics and Precipitating Circumstances of Black Youth Suicide Decedents Aged 5–17 Years in the United States, from the National Violent Data Reporting System (NVDRS) (2003–2017)
|
Age 5–11 y (n = 75)
|
Age 12–14 y (n = 182)
|
Age 15–17 y (n = 369)
|
Statistic | df | p | ||||
| Clinical characteristic a | n | % | n | % | n | % | |||
| Mental health characteristic | |||||||||
| Current mental health problem | 22 | 31.9 | 55 | 35.7 | 113 | 34.6 | χ2 = 0.31 | 2 | .309 |
| Current mental health treatment | 17 | 24.6 | 42 | 27.3 | 76 | 23.2 | χ2 = 0.92 | 2 | .632 |
| History of mental health treatment | 19 | 27.5 | 49 | 31.8 | 103 | 31.5 | χ2 = 0.47 | 2 | .790 |
| Current depressed mood | 12 | 17.4 | 32 | 20.8 | 87 | 26.6 | χ2 = 3.76 | 2 | .153 |
| Mental health diagnosisb | |||||||||
| Depression/dysthymia | 5a | 22.7 | 27 | 49.1b | 76c | 67.3 | χ2 = 16.78 | 2 | <.001 |
| Bipolar disorder | 1 | 4.5 | 8 | 14.5 | 15 | 13.3 | FET | .535 | |
| Schizophrenia | 1 | 4.5 | 0 | 0.0 | 5 | 4.4 | FET | .283 | |
| Anxiety disorder | 1 | 4.5 | 3 | 5.5 | 12 | 10.6 | FET | .546 | |
| PTSD | 0 | 0.0 | 1 | 1.8 | 1 | 0.9 | FET | .751 | |
| ADD/ADHD | 16a | 72.7 | 20 | 36.4b | 20c | 17.7 | χ2 = 28.59 | 2 | <.001 |
| Other mental disorder | 8 | 36.4 | 17 | 30.9 | 25 | 22.1 | χ2 = 2.77 | 2 | .251 |
| Alcohol/drug-related precipitating circumstances | |||||||||
| Alcohol problem | 0 | 0.0 | 0 | 0.0 | 3 | 0.9 | FET | .702 | |
| Other substance problem | 1a | 1.4 | 2a | 1.3 | 22a,b | 6.7 | FET | .013 | |
|
Age 5–11 y (n = 75)
|
Age 12–14 y (n = 182)
|
Age 15–17 y (n = 369)
|
|||||||
| Clinical characteristic a | n | % | n | % | n | % | Statistic | df | p |
| Presence of alcohol or drugs at time of death | |||||||||
| Alcohol | |||||||||
| Number tested | 44 | 63.8 | 93 | 60.4 | 196 | 59.9 | χ2 = 0.90 | 4 | .925 |
| Present (among those tested) | 1 | 2.3 | 2 | 2.2 | 11 | 5.6 | FET | .722 | |
| Amphetamine | |||||||||
| Number tested | 22 | 31.9 | 64 | 41.6 | 125 | 38.2 | χ2 = 3.53 | 4 | .474 |
| Present (among those tested) | 2 | 9.1 | 0 | 0.0 | 5 | 4.0 | FET | .215 | |
| Opioids | |||||||||
| Number tested | 27 | 39.1 | 64 | 41.6 | 130 | 39.8 | χ2 = 1.24 | 4 | .872 |
| Present (among those tested) | 0 | 0.0 | 2 | 3.1 | 8 | 6.2 | FET | .789 | |
| Marijuana | |||||||||
| Number tested | 18 | 26.1 | 46 | 29.9 | 96 | 29.4 | χ2 = 1.42 | 4 | .841 |
| Present (among those tested) | 1a | 5.6 | 2a | 4.3 | 28b | 29.2 | FET | .004 | |
| Benzodiazepines | |||||||||
| Number tested | 11 | 15.9 | 27 | 17.5 | 58 | 17.7 | χ2 = 2.29 | 4 | .682 |
| Present (among those tested) | 0 | 0.0 | 1 | 3.7 | 3 | 5.2 | FET | .878 | |
| Antidepressants | |||||||||
| Number tested | 18 | 26.1 | 49 | 31.8 | 76 | 23.2 | χ2 = 5.98 | 4 | .201 |
| Present (among those tested) | 2 | 11.1 | 7 | 14.3 | 12 | 15.8 | FET | .446 | |
Note: ADD/ADHD, attention-deficit disorder/attention-deficit/hyperactivity disorder; FET = Fisher exact test; PTSD = posttraumatic stress disorder.
Clinical characteristics were known in 550 youths: 5–11 y (n = 69); 12–14 y (n = 154); 15–17 y (n = 327).
Present in those with a current mental health problem.
Boyfriend/girlfriend problems/crises and recent criminal/legal problems were more prevalent in the 15- to 17-year-old Black suicide decedents compared to younger suicide decedents (aged 5–11 and 12–14 years). Family problems/crises and school problems were more common in the younger age groups (5–11 and 12–14 years) compared to the older (aged 15–17 years) suicide decedents. Younger Black youth who died by suicide were less likely to leave a suicide note compared with older Black decedents (15–17 years). No group differences emerged for friendship problems/crises (Table 1).
Approximately 35% of Black suicide decedents were identified as having a current mental health problem prior to death (Table 2); however, there were no age group differences in rates of current mental health problems, current/past mental health treatment, and current depressed mood. Among Black youth decedents with a current mental health problem, two significant findings were present. First a diagnosis of depression/dysthymia was most common in the 15- to 17-year-old Black decedents (67.3%) compared with the 12- to 14-year-old (49.1%) and 5- to 11-year-old decedents (22.7%; χ2 = 16.78, df = 2, p < .001). Second, a diagnosis of attention-deficit disorder/attention-deficit hyperactive disorder (ADD/ADHD) was most common in the 5- to 11-year-old Black decedents (72.7%) compared with 12- to 14-year-old (36.4%) and 15- to 17-year-old (17.7%) decedents (χ2 = 28.59, df = 2, p < .001).
Rates of alcohol or substance use problems were generally low among Black suicide decedents; however, significant differences were found between age groups for rates of substance use problems unrelated to alcohol. Rates were highest in the oldest age group (6.7%) compared with the 2 younger age groups (1.4% for age 5–11 years; 1.3% for age 12–14 years; FET, p = .013). Consistent with this finding, 29.2% of 15- to 17-year-old Black youths decedents tested positive for marijuana (n = 160) compared to the younger age groups (5.6% for age 5–11 years; 4.3% for age 12–14 years; FET, p = .004).
NVDRS Analyses by Sex
Overall (Table 3), both Black female and male suicide decedents died by hanging/strangulation/suffocation, followed by firearms. The proportion of suicides by hanging/strangulation/suffocation was higher for Black girls compared to boys (74.3% and 57.3%, respectively); for firearm suicides, the proportion was higher for Black boys compared to girls (37.4% and 15.1%, respectively; χ2 = 31.55, df = 2, p < .001). No sex differences were found for age, ethnicity, or injury location (decedent’s residence vs not).
TABLE 3.
Characteristics and Precipitating Circumstances of Black Youth Suicide Decedents Aged 5–17 Years By Sex in the United States, From the National Violent Data Reporting System (NVDRS) (2003–2017)
| Boys (n = 447) |
Girls (n = 179) |
Statistic | df | p | |||
|---|---|---|---|---|---|---|---|
| Characteristics | n | % | n | % | |||
| Age (Mean/SD) | 14.6 | 2.3 | 14.5 | 2.0 | t = 0.74 | 624 | .461 |
| Ethnicity | FET | .754 | |||||
| Non-Hispanic | 433 | 96.9 | 171 | 95.5 | |||
| Hispanic | 10 | 2.2 | 6 | 3.4 | |||
| Unknown | 4 | 0.9 | 2 | 1.1 | |||
| Suicide method | χ2 = 31.55 | 2 | <.001 | ||||
| Hanging, strangulation, or suffocation | 256 | 57.3 | 133 | 74.3 | |||
| Firearm | 167 | 37.4 | 27 | 15.1 | |||
| Poisoning and other methodsa | 24 | 5.4 | 19 | 10.6 | |||
| Injury occurred at decedent’s residence (% yes) | 344 | 77.0 | 150 | 83.8 | χ2 = 5.45 | 1 | .065 |
| Precipitating circumstances b | |||||||
| Relationship problems | |||||||
| Boyfriend/girlfriend problem | 49 | 12.6 | 27 | 16.9 | χ2 = 1.77 | 1 | .183 |
| Boyfriend/girlfriend problem was a crisis | 16 | 4.1 | 14 | 8.8 | χ2 = 4.75 | 1 | .029 |
| Family problem | 105 | 26.9 | 50 | 31.3 | χ2 = 1.05 | 1 | .306 |
| Family problem was a crisis | 39 | 10.0 | 24 | 15.0 | χ2 = 2.80 | 1 | .094 |
| Friend problem | 73 | 18.7 | 30 | 18.8 | χ2 = 0.00 | 1 | .993 |
| Friend problem was a crisis | 5 | 1.3 | 3 | 1.9 | FET | .598 | |
| Interpersonal trauma and life stressors | |||||||
| Decedent had a history of abuse | 9 | 2.3 | 6 | 3.8 | χ2 = 0.89 | 1 | .346 |
| Suicide directly precipitated by abuse | 3 | 0.8 | 1 | 0.6 | FET | .857 | |
| Perpetrator of interpersonal violence | 18 | 4.6 | 3 | 1.9 | FET | .148 | |
| Victim of interpersonal violence | 2 | 0.5 | 3 | 1.9 | FET | .150 | |
| Involved in physical fight immediately before death | 5 | 1.3 | 0 | 0.0 | FET | .328 | |
| An argument or conflict led to the decedent’s death | 73 | 18.7 | 41 | 25.6 | χ2 = 3.29 | 1 | .070 |
| Timing of the argument that led to death | |||||||
| Injury occurred during argument | 5 | 1.3 | 2 | 1.3 | FET | >.999 | |
| Injury occurred within 24 hrs of argument | 43 | 11.0 | 31 | 19.4 | χ2 = 6.79 | 1 | .009 |
| Injury occurred between 24 hrs and 2 wk | 6 | 1.5 | 0 | 0.0 | FET | .188 | |
| Physical health problem | 7 | 1.8 | 8 | 5.0 | χ2 = 4.39 | 1 | .036 |
| School problem | 110 | 28.2 | 40 | 25.0 | χ2 = 0.59 | 1 | .443 |
| School problem was a crisis | 26 | 6.7 | 5 | 3.1 | χ2 = 2.68 | 1 | .102 |
| Death of friend or family member | 26 | 6.7 | 7 | 4.4 | χ2 = 1.06 | 1 | .304 |
| Crime and criminal activity | |||||||
| Recent criminal legal problem | 34 | 8.7 | 4 | 2.5 | FET | .009 | |
| Other legal problem | 9 | 2.3 | 1 | 0.6 | FET | .295 | |
| Suicide-related circumstances | |||||||
| History of suicidal thoughts or plans | 53 | 13.6 | 35 | 21.9 | χ2 = 5.80 | 1 | .016 |
| History of suicide attempt | 44 | 11.3 | 49 | 30.6 | χ2 = 30.21 | 1 | <.001 |
| Suicide intent disclosed within past month | 81 | 20.8 | 34 | 21.3 | χ2 = 0.02 | 1 | .900 |
| Suicide note | 64 | 16.4 | 60 | 37.5 | χ2 = 28.90 | 1 | <.001 |
| Recent suicide of friend or family member | 6 | 1.5 | 4 | 2.5 | FET | .487 | |
Note: FET = Fisher’s exact test.
Other suicide methods include fall, transportation-related, drowning, cut/pierce, fire/burn, overdose, and unspecified methods.
Precipitating circumstances were known in 550 youths: boys (n = 390); girls (n = 160).
Regarding precipitating circumstances, 390 Black male decedents and 160 female decedents had circumstances marked in NVDRS as known and were included in the data analysis. Sex differences were found for boyfriend/girlfriend crises, timing of arguments prior to death, physical health problems, crime/criminal activity, suicide-related circumstances (eg, prior suicide attempts), and mental health characteristics/diagnoses (Tables 3 and 4).
TABLE 4.
Clinical Characteristics of Black Youth Suicide Decedents Aged 5–17 Years by Sex in the United States, From the National Violent Data Reporting System (NVDRS) (2003–2017)
| Boys (n = 447) |
Girls (n = 179) |
||||||
|---|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | Statistic | df | p |
| Mental health characteristica | |||||||
| Current mental health problem | 123 | 31.5 | 67 | 41.9 | χ2 = 5.36 | 1 | .021 |
| Current mental health treatment | 86 | 22.1 | 49 | 30.6 | χ2 = 4.50 | 1 | .034 |
| History of mental health treatment | 107 | 27.4 | 64 | 40.0 | χ2 = 8.36 | 1 | .004 |
| Current depressed mood | 86 | 22.1 | 45 | 28.1 | χ2 = 2.31 | 1 | .129 |
| Mental health diagnosisb | |||||||
| Depression/dysthymia | 60 | 48.8 | 48 | 71.6 | χ2 = 15.36 | 1 | <.001 |
| Bipolar disorder | 14 | 11.4 | 10 | 14.9 | χ2 = 1.92 | 1 | .165 |
| Schizophrenia | 4 | 3.3 | 2 | 3.0 | FET | .818 | |
| Anxiety disorder | 7 | 5.7 | 9 | 13.4 | χ2 = 5.89 | 1 | .015 |
| PTSD | 1 | 0.8 | 1 | 1.5 | FET | .498 | |
| ADD/ADHD | 51 | 41.5 | 5 | 7.5 | χ2 = 12.29 | 1 | <.001 |
| Other mental disorder | 33 | 26.8 | 17 | 25.4 | χ2 = 0.64 | 1 | .423 |
| Alcohol/drug-related precipitating circumstances | |||||||
| Alcohol problem | 3 | 0.8 | 0 | 0.0 | FET | .560 | |
| Other substance problem | 21 | 5.4 | 4 | 2.5 | FET | .178 | |
| Presence of alcohol or drugs at time of death | |||||||
| Alcohol | |||||||
| Number tested | 238 | 61.0 | 95 | 59.4 | χ2 = 0.51 | 2 | .775 |
| Present (among those tested) | 10 | 4.2 | 4 | 4.2 | FET | .809 | |
| Amphetamine | |||||||
| Number tested | 151 | 38.7 | 60 | 37.5 | χ2 = 0.51 | 2 | .975 |
| Present (among those tested) | 7 | 4.6 | 0 | 0.0 | FET | .405 | |
| Opioids | |||||||
| Number tested | 158 | 40.5 | 63 | 39.4 | χ2 = 0.17 | 2 | .917 |
| Present (among those tested) | 6 | 3.8 | 4 | 6.3 | FET | .823 | |
| Marijuana | |||||||
| Number tested | 114 | 29.2 | 46 | 28.8 | χ2 = 0.29 | 2 | .866 |
| Present (among those tested) | 27 | 23.7 | 4 | 8.7 | FET | .165 | |
| Benzodiazepines | |||||||
| Number tested | 61 | 15.6 | 35 | 21.9 | χ2 = 2.23 | 2 | .328 |
| Present (among those tested) | 3 | 4.9 | 1 | 2.9 | FET | .780 | |
| Antidepressants | |||||||
| Number tested | 98 | 25.1 | 45 | 28.1 | χ2 = 2.26 | 2 | .323 |
| Present (among those tested) | 13 | 13.3 | 8 | 17.8 | χ2 = 1.76 | 3 | .623 |
Note: ADD/ADHD = attention deficit disorder/attention deficit hyperactivity disorder; FET = Fisher’s exact test; PTSD = posttraumatic stress disorder.
Precipitating circumstances were known in 550 youths: boys (n = 390); girls (n = 160).
Based on current mental health problem.
Black female decedents were more likely to experience a boyfriend/girlfriend crisis prior to suicide compared to male decedents (8.8% vs 4.1%; χ2 = 4.75, df = 1, p < .029), but no group differences in other relationship problems emerged. The timing of the suicide death for Black girls was more likely to occur within 24 hours of an argument compared to Black boys (19.4% vs 11.0%; χ2 = 6.79, df = 1, p = .009). Black female decedents were more likely to have a physical health problem compared to male decedents (5.0% vs 1.8%; χ2 = 4.39, df = 1, p = .036), whereas male decedents were more likely to experience a recent criminal/legal problem compared to female decedents (8.7% vs 2.5%; χ2 = 6.82, df = 1, p = .009). Finally, for suicide-related circumstances, Black female decedents were more likely to have a history of suicidal thoughts/plans (21.9% vs 13.6%; χ2 = 5.80, df = 1, p = .016), suicide attempts (30.6% vs 11.3%; χ2 = 30.21, df = 1, p < .001), and to leave a suicide note (37.5% vs 16.4%; χ2 = 28.90, df = 1, p < .001) compared to male decedents.
Compared to Black male decedents, Black female decedents were more likely to have a current mental health problem (41.9% vs 31.5%, χ2 = 5.36, df = 1, p = .021), receive current mental health treatment (30.6% vs 22.1%; χ2 = 4.50, df = 1, p = .034), and to have a history of mental health treatment (40.0% vs 27.4%; χ2 = 8.36, df = 1, p < .004) prior to death (Table 4). When comparing Black female and male suicide decedents on current mental health problems, depression/dysthymia (71.6% vs 48.8%; χ2 = 15.36, df = 1, p < .001) and anxiety (13.4% vs 5.7%; χ2 = 5.89, df = 1, p = .015) were more common in girls, whereas ADD/ADHD was more common in boys (41.5% vs 7.5%; χ2 = 12.29, df = 1, p < .001). No sex differences were observed in rates of alcohol/substance problems or in the presence of alcohol/drugs at time of death.
DISCUSSION
This is the first study, to our knowledge, to examine trends and precipitating circumstances of suicide in Black youth only by age group and sex combining national data from both the CDC-WISQARS1 and NVDRS.15 From 2003 to 2017, the rate of suicide in Black youth increased every year for both boys and girls across all age groups. These results support recent findings suggesting that the rate of suicide and suicidal behaviors in Black youth has increased over time.3–7 Black youths in the 15- to 17-year-old group experienced the largest percentage change (annual increase of 4.9%), followed by youths in the 5- to 11-year-old group (annual increase of 3.9%) (Figure 1a–c). Regarding trends by sex, Black girls had the largest APC (6.6%). The increase across all age groups and both sexes indicates that suicide is an all-encompassing problem for Black youth. Further investigation to determine what factors underlie these increases is necessary to provide avenues for interventions needed to mitigate the likelihood of these behaviors.
When examining precipitating circumstances using the NVDRS,15 findings suggest that suicide prevention efforts and clinical care for Black youth should differ depending upon the youth’s sex and developmental stage. For example, in our study, Black child suicide decedents (aged 5–11 years) who were diagnosed with a mental health concern were more likely to be diagnosed with ADD/ADHD (73%) compared to the other age groups. These findings are consistent with our previous report5 and together suggest that suicide prevention strategies for 5- to 11-year-old youth, in general, should involve families of youth diagnosed with ADHD. Educating caregivers of children with ADHD on the signs of suicidal behavior and conducting youth screenings at primary care/psychiatry appointments for ADHD may decrease suicidal behaviors in this at-risk population. Although Black youth are typically underdiagnosed with ADHD compared to their White counterparts, a recent study suggests that this may be changing.17 The study found that Black youths aged 2 to 17 years had a higher prevalence of ADHD diagnosis and received more mental health treatment for ADHD compared to White youth.17 Educating caregivers of youth with ADHD and screening youth at appointments for ADHD management may provide an opportunity for timely intervention if children are in crisis.
Black youths in the 12- to 14-year-old group included more female decedents than any other age group. Overall, Black girls experienced the highest annual increase in suicide rates, regardless of age. This is consistent with previous research that found that the gap between female and male suicides is closing.18 Our data suggest that 75% of Black female decedents in the 12- to 14-year-old group died by hanging/strangulation/suffocation, which implies that Black girls in this age group may be using more lethal suicide means, and that interventions for Black families should include education on the restriction of lethal means. Moreover, Black girls were more likely to experience a boyfriend/girlfriend crisis prior to death and died by suicide within 24 hours of an argument compared to Black boys. Considering these findings, interventions for Black girls may also need to focus on conflict resolution skills and coping mechanisms for interpersonal challenges. One such program specific for Black girls is Sisters of Nia.19,20
Sisters of Nia is an Afrocentric school-based intervention for early adolescent Black girls that focuses on enhancing ethnic identity, encouraging an androgynous gender role, and strengthening positive relationships.19 20 It is not specific to suicide prevention; however, it could be adapted to incorporate lessons within the original sessions (eg, “healing the hurt”). This intervention has shown increases in ethnic identity, which is a protective factor associated with higher academic achievement, self-esteem, prosocial behaviors, and decreases in violence use and relational aggression.19,20 Adaptation of this intervention could be extremely beneficial for this high-risk group of Black girls. Furthermore, the adapted intervention could be constructed for implementation in community settings that Black youth frequent (eg, community centers, faith-based organizations, and after-school programs) to ensure that Black girls are not singled out in the school setting. Finally, there is a version specific for Black boys called Brothers of Ujima,21 which discusses and teaches the same concepts as Sisters of Nia.
For the 15- to 17-year-old group, Black youths were more likely to die by firearms, to have a recent criminal/legal problem, to have boyfriend/girlfriend problems/crises, to test positive for marijuana at time of death, to have a substance use concern unrelated to alcohol and, if diagnosed with a mental health concern, to be more likely to be diagnosed with depression/dysthymia. These results have been found in previous research when comparing early adolescents to young children5; however, depression is less likely to be diagnosed in Black adolescents compared to other youth of different racial and ethnic backgrounds.14,22 Further investigation is needed concerning the presentation of depression in Black youth, along with potential clinician biases in diagnosing depression in Black youth.23
The association between suicidal behaviors and substance use in youth and young adults has been found in previous studies,24–26 but not specifically among Black youth. Our study may be the first to document this association. Incorporating education on the association between substance use and suicidal behaviors on a universal level for youth and their families seeking mental health services for substance use disorders may prevent both behaviors from occurring. Also, interventions that increase ethnic identity in Black youth have been associated with decreased substance use engagement.12,19 Incorporating interventions for suicidal behavior prevention that increases ethnic identity might be extremely beneficial for Black youth.
Concerning criminal/legal problems, it is necessary to determine what universal suicide prevention efforts are being conducted with this at-risk group of youth. Enhanced evidence-based interventions and suicide prevention training for juvenile justice professionals on the unique risks for suicide in justice-involved youth may be warranted.27 The presentation of mental health symptoms in Black youth such as depression, substance abuse, or externalizing behaviors are more likely to lead to disciplinary action and juvenile justice involvement, instead of requisite mental health treatment.28–30 Helping Black youth and their families access mental health services instead of involving the criminal justice system may be an opportunity to prevent suicide death.
Our findings suggest that suicide prevention efforts for Black youth will depend on developmental age and sex. In terms of addressing relationship problems in the younger age group (5–14 years), Sisters of Nia19,20 for Black girls and Brothers of Ujima21 for boys could be extremely beneficial. For Black adolescents (aged 15–17 years), the Adapted–Coping with Stress Course (A-CWS)31 could be valuable. The A-CWS intervention, based on the Adolescent Coping with Stress Course (CWS),32 is a school-based, 15-group session intervention for Black adolescents.33 Group sessions teach Black youth how to do the following: (1) to identify feelings when experiencing stress; (2) to reduce negative thoughts; (3) to acknowledge stressors in their lives; (4) to develop coping mechanisms to deal with stressful experiences; and (5) to plan for stressful times in the near future (eg, final examination week at school). Preliminary findings suggest that the A-CWS is effective in reducing suicidal behavior in Black adolescents,31 and testing this intervention on a larger scale would be advantageous.
Schools have been touted as promising settings for universal suicide prevention; however, Black youth may feel uncomfortable disclosing suicidal ideation and behaviors in these settings.34 For this study, school problems were indicated as a precipitating circumstance in younger Black youths (aged 5–14 years), and research demonstrates a longstanding racial disparity in school disciplinary action, with suspension, expulsion, and detention more prevalent in Black youth compared to their White counterparts for the same behaviors.30,35 Thus, Black youth may choose not to disclose suicidal ideation and behaviors in the school setting nor to engage at any level to address psychiatric concerns because of fear of disciplinary action.
Implementing suicide prevention for Black youth in community settings (eg, community centers, Boys and Girls Clubs, after-school programs, faith-based organizations) is recommended by the Congressional Black Caucus Taskforce report and in several recent publications concerning Black youth suicide prevention.9,11–13 Community settings may be deemed as safe spaces for Black youth. Black youth may feel that staff are culturally competent, have experienced the same stressors as they have (eg, racism), and may believe that the staff can assess and understand problems that they are experiencing and can intervene appropriately if necessary. Training community organization leaders and youth workers/volunteers on the warning signs associated with suicide/suicidal behavior and how to intervene when Black youth are experiencing these signs could be a low-cost and highly effective method of suicide prevention for Black youth; yet, to our knowledge, this is an untapped area for intervention.
Finally, mental health characteristics were another precipitating circumstance where sex differences were present. Approximately one-third of the Black youths, 31.5% of boys and 41.9% of girls, had an identified mental health concern. This raises the question as to whether a mental health concern and/or suicide risk were missed prior to death. Literature suggests that Black youth are more likely to be misdiagnosed and less likely to be identified with internalizing disorders compared to White youth.14,36 Accurately identifying mental health symptoms in Black youth is a problem for providers and families, which presents a barrier to mental health treatment for this group.37–39
For mental health treatment, Black boys who died by suicide were less likely to have current mental health treatment or a history of mental health treatment compared to girls who died by suicide. Extant research finds that Black youth, particularly boys, are more vulnerable to stigma related to mental illness and treatment,40 with their help seeking compromised by masculine norms and gender-based notions of help-seeking behaviors.41,42 Black boys may prefer to resolve their psychiatric concerns among their families, instead of receiving formal treatment, which suggests the importance of network-based interventions and strategies to incorporate the family in the treatment process.40 Therefore, strategies to connect Black boys to mental health treatment must lead with mitigating masculinity notions that prohibit formal help-seeking behaviors.
Church-based mental health programming for Black families may hold promise for alleviating barriers to treatment for Black youth,43,44 as well as incorporating mental health resources in workforce development programs.45 In studies of mental health treatment engagement, perceptual barriers (eg, stigma, perceived relevance of treatment) vs actual barriers (eg, transportation, childcare) are powerful predictors of engagement.46,47 Addressing these perceptual barriers up front may increase treatment use.
Finally, for suicide prevention to be effective for Black youth, not only is it important to acknowledge the differences present by age and sex, but we must also see Black youth suicide prevention through a different lens and must address the systemic racism and trauma experienced by Black youth on a regular basis.11–13 Racism is associated with poor mental health outcomes,10 and to ignore the influence of racism on Black youth suicide/suicidal behavior could potentially exacerbate the current circumstances. A recent article suggests that incorporating principles of justice, equity, diversity, and inclusion (JEDI lens) is a necessity when interpreting risk factors associated with Black youth suicide/suicidal behavior and when assessing, diagnosing, and treating mental health concerns in Black youth.11 When formulating Black youth suicide prevention efforts, the use of the JEDI lens11 is highly relevant and, if incorporated, could be effective in reducing suicide and suicidal behavior in Black youth.
This study is not without limitations. Currently, the NVDRS is in all 50 states; however, the restricted database consisted of only 35 states, Washington, DC, and Puerto Rico. The analyses performed did not include factors such as sexual orientation and gender identity, which limits the generalizability of our findings to all Black youth. Precipitating circumstances were also unknown in 11% of the sample, which also limits the generalizability of the findings. For the data analyses, no corrections were made for the multiple comparisons between sex and age groups, and we did not include a comparison group of youth of other racial and ethnic backgrounds for the analyses. Data concerning experiences with racial discrimination, stereotypes, and racism were not included, although all have been associated with poor mental health outcomes and all are found to have a disproportionate impact on Black youth.9–13,33,48,49 Finally, we limited our study to the quantitative elements of the NVDRS.
Black youth suicide is increasing, yet research addressing risk and protective factors associated with this increase and the testing of suicide prevention programs in this community is lacking.9,13 To our knowledge, this is the first study to examine trends and precipitating circumstances of suicide among Black youth only by age and sex. This study’s findings suggest that precipitating circumstances differed by developmental stage and sex; for suicide prevention efforts to be effective for Black youth, age and sex must be considered along with specific risk factors associated with Black youth suicide and suicidal behavior.
Acknowledgments
Dr. Sheftall received grant support for the conduct of this research from the National Institute of Mental Health (NIMH; R21MH116206) and the American Foundation for Suicide Prevention (AFSP; YIG-1-152-19). NIMH and AFSP were not involved in the study design, collection/analysis/interpretation of the data, or manuscript preparation. Dr. Lindsey receives grant funding from NIMH (R34MH119390) which supported his effort during the writing of this manuscript.
Footnotes
Disclosure: Dr. Bridge has received research grant support from NIMH, the Patient-Centered Outcomes Research Institute, and the Centers for Disease Control and Prevention. He has served as a member of the Scientific Advisory Board of Clarigent Health. Drs. Sheftall, Ruch, Boyd, Lindsey and Ms. Vakil have reported no biomedical financial interests or potential conflicts of interest.
This article is part of a special series devoted to addressing bias, bigotry, racism, and mental health disparities through research, practice, and policy. The series is edited by Assistant Editor Eraka Bath, MD, Deputy Editor Wanjikũ F.M. Njoroge, Associate Editor Robert R. Althoff, MD, PhD, and Editor-in-Chief Douglas K. Novins, MD.
Contributor Information
Arielle H. Sheftall, Center for Suicide Prevention and Research, Abigail Wexner Research Institute at Nationwide Children’s Hospital, Columbus, Ohio; The Ohio State University College of Medicine, Columbus.
Fatima Vakil, Center for Suicide Prevention and Research, Abigail Wexner Research Institute at Nationwide Children’s Hospital, Columbus, Ohio.
Donna A. Ruch, Center for Suicide Prevention and Research, Abigail Wexner Research Institute at Nationwide Children’s Hospital, Columbus, Ohio.
Rhonda C. Boyd, Children’s Hospital of Philadelphia, Pennsylvania; Perelman School of Medicine, University of Pennsylvania, Philadelphia.
Michael A. Lindsey, Silver School of Social Work, New York University, New York; McSilver Institute for Poverty Policy and Research, New York.
Jeffrey A. Bridge, Center for Suicide Prevention and Research, Abigail Wexner Research Institute at Nationwide Children’s Hospital, Columbus, Ohio; The Ohio State University College of Medicine, Columbus.
REFERENCES
- 1.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS)[online]: Fatal injury data, leading causes of death reports 1981– 2019. Accessed January 1, 2021; https://www.cdc.gov/injury/wisqars/fatal.html.
- 2.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS)[online]: Nonfatal injury reports 2000–2019. Accessed February 1, 2021; https://webappa.cdc.gov/sasweb/ncipc/nfirates.html.
- 3.Ertl A, Crosby AE, Blair JM. Youth suicide: an opportunity for prevention. J Am Acad Child Adolesc Psychiatry. 2020;59:1019–1021. 10.1016/j.jaac.2020.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ivey-Stephenson AZ, Demissie Z, Crosby AE, et al. Suicidal ideation and behaviors among high school students–Youth Risk Behavior Survey, United States, 2019. MMWR Suppl. 2020;69:47–55. 10.15585/mmwr.su6901a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheftall AH, Asti L, Horowitz LM, et al. Suicide in elementary school-aged children and early adolescents. Pediatrics. 2016;138. 10.1542/peds.2016-0436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bridge JA, Horowitz LM, Fontanella CA, et al. Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatr. 2018;172:697–699. 10.1001/jamapediatrics.2018.0399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindsey M, Sheftall A, Xiao YY, Joe S. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics. 2019;144. 10.1542/peds.2019-1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayer L, Colpe L, Pearson J, Rooney M, Murphy E. Advancing research in child suicide: a call to action. J Am Acad Child Adolesc Psychiatry. 2020;59:1028–1035. 10.1016/j.jaac.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 9.Suicide Prevention Resource Center. Ring the alarm: The crisis of black youth suicide in America. 2019. Accessed September 30, 2021. https://www.sprc.org/news/ring-alarm-crisis-black-youth-suicide-america
- 10.Pachter LM, Coll CG. Racism and child health: a review of the literature and future directions. J Dev Behav Pediatr. 2009;30:255–263. 10.1097/DBP.0b013e3181a7ed5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bath E, Njoroge WFM. Coloring outside the lines: making Black and Brown lives matter in the prevention of youth suicide [Comment]. Journal of the American Academy of Child and Adolescent Psychiatry. 2021;60:17–21. 10.1016/j.jaac.2020.09.013. [DOI] [PubMed] [Google Scholar]
- 12.Meza JI, Bath E. One size does not fit all: making suicide prevention and interventions equitable for our increasingly diverse communities. J Am Acad Child Adolesc Psychiatry. 2021;60:209–212. 10.1016/j.jaac.2020.09.019. [DOI] [PubMed] [Google Scholar]
- 13.Sheftall AH, Miller AB. Setting a ground zero research agenda for preventing Black youth suicide. JAMA Pediatr. 2021;175:890–892. 10.1001/jamapediatrics.2021.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen L, Huang LN, Arganza GF, Liao Q. The influence of race and ethnicity on psychiatric diagnoses and clinical characteristics of children and adolescents in children’s services. Cult Divers Ethn Minor Psychol. 2007;13:18–25. 10.1037/1099-9809.13.1.18. [DOI] [PubMed] [Google Scholar]
- 15.National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. National Violent Death Reporting System (NVDRS). Accessed August 5, 2015; https://www.cdc.gov/violenceprevention/datasources/nvdrs/.
- 16.IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp.; 2012. [Google Scholar]
- 17.Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. J Clin Child Adolesc Psychol. 2018;47:199–212. 10.1080/15374416.2017.1417860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in suicide among youth aged 10 to 19 years in the United States, 1975 to 2016. JAMA Netw Open. 2019;2:e193886. 10.1001/jamanetworkopen.2019.3886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belgrave FZ, Reed MC, Plybon LE, Butler DS, Allison KW, Davis T. An evaluation of Sisters of Nia: a cultural program for African American girls. J Black Psychol. 2004;30: 329–343. 10.1177/0095798404266063. [DOI] [Google Scholar]
- 20.Aston C, Graves SL, McGoey K, Lovelace T, Townsend T. Promoting sisterhood: the impact of a culturally focused program to address verbally aggressive behaviors in Black girls. Psychol Sch. 2018;55:50–62. 10.1002/pits.22089. [DOI] [Google Scholar]
- 21.Belgrave FZ, Allison KW, Wilson J, Tademy R. Brothers of Ujima: A Cultural Enrichment Program to Empower Adolescent African-American Males. Champaign, IL: Research Press; 2011. [Google Scholar]
- 22.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138. 10.1542/peds.2016-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ofonedu ME, Percy WH, Harris-Britt A, Belcher HME. Depression in inner city African American youth: a phenomenological study. J Child Family Stud. 2013;22:96–106. 10.1007/s10826-012-9583-3. [DOI] [Google Scholar]
- 24.Swahn M, Bossarte R, Choquet M, Hassler C, Falissard B, Chau N. Early substance use initiation and suicide ideation and attempts among students in France and the United States. Int J Public Health. 2012;57:95–105. 10.1007/s00038-011-0255-7. [DOI] [PubMed] [Google Scholar]
- 25.Brent DA. Risk factors for adolescent suicide and suicidal behavior: mental and substance abuse disorders, family environmental factors, and life stress. Suicide Life Threat Behav. 1995;25(Suppl):52–63. [PubMed] [Google Scholar]
- 26.Rowan A Adolescent substance abuse and suicide. Depress Anxiety. 2001;14:186–191. 10.1002/da.1065. [DOI] [PubMed] [Google Scholar]
- 27.Ruch DA, Sheftall AH, Schlagbaum P, Fontanella CA, Campo JV, Bridge JA. Characteristics and precipitating circumstances of suicide among incarcerated youth. J Am Acad Child Adolesc Psychiatry. 2019;58:514–524. 10.1016/j.jaac.2018.07.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramey DM. The social structure of criminalized and medicalized school discipline. Sociol Educ. 2015;88:181–201. 10.1177/0038040715587114. [DOI] [Google Scholar]
- 29.Barnes JC, Motz RT. Reducing racial inequalities in adulthood arrest by reducing inequalities in school discipline: evidence from the school-to-prison pipeline. Dev Psychol. 2018;54:2328–2340. 10.1037/dev0000613. [DOI] [PubMed] [Google Scholar]
- 30.Paschall KW, Gershoff ET, Kuhfeld M. A two decade examination of historical race/ethnicity disparities in academic achievement by poverty status. J Youth Adolesc. 2018; 47:1164–1177. 10.1007/s10964-017-0800-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson WL, Case MH, Whipple CR, et al. Culturally grounded stress reduction and suicide prevention for African American adolescents. Practice Innovations. 2016;1: 117–128. 10.1037/pri0000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clarke GN, Lewinsohn PM. Instructor’s Manual for the Adolescent Coping With Stress Course. Portland: OR: Oregon Health Sciences University; 1995. [Google Scholar]
- 33.Robinson WL, Whipple CR, Jason LA, Flack CE. African American adolescent suicidal ideation and behavior: the role of racism and prevention. J Community Psychol. 2021; 49:1282–1295. 10.1002/jcop.22543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marraccini ME, Griffin D, O’Neill C, et al. School risk and protective factors of suicide: a cultural model of suicide risk and protective factors in schools. Sch Psychol Rev. 2021; 1–24. 10.1080/2372966X.2020.1871305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xiao Y, Romanelli M, Velez-Grau C, Lindsey MA. Unpacking racial/ethnic differences in the associations between neighborhood disadvantage and academic achievement: mediation of future orientation and moderation of parental support. J Youth Adolesc. 2021; 50:103–125. 10.1007/s10964-020-01319-6. [DOI] [PubMed] [Google Scholar]
- 36.Mizock L, Hrkins D. Diagnostic bias and conduct disorder: improving culturally sensitive diagnosis. Child Youth Serv. 2011;32:243–253. 10.1080/0145935X.2011.605315. [DOI] [Google Scholar]
- 37.Planey AM, Smith SM, Moore S, Walker TD. Barriers and facilitators to mental health help-seeking among African American youth and their families: a systematic review study. Child Youth Serv Rev. 2019;101:190–200. 10.1016/j.childyouth.2019.04.001. [DOI] [Google Scholar]
- 38.Fante-Coleman T, Jackson-Best F. Barriers and facilitators to accessing mental healthcare in Canada for Black youth: a scoping review. Adolesc Res Rev. 5:115–136. 10.1007/s40894-020-00133-2 [DOI] [Google Scholar]
- 39.Breland-Noble AM. Mental healthcare disparities affect treatment of black adolescents. Psychiatr Ann. 2004;34:534–538. 10.3928/0048-5713-20040701-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lindsey MA, Joe S, Nebbitt V. Family matters: the role of mental health stigma and social support on depressive symptoms and subsequent help seeking among African American boys. J Black Psychol. 2010;36:458–482. 10.1177/0095798409355796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scott LD, Munson MR, McMillen JC, Snowden LR. Predisposition to seek mental health care among Black males transitioning from foster care. Child Youth Serv Rev. 2007;29:870–882. 10.1016/j.childyouth.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lindsey MA, Brown DR, Cunningham M. Boys do(n’t) cry: Addressing the unmet mental health needs of African American boys. Am J Orthopsychiatry. 2017;87:377–383. 10.1037/ort0000198. [DOI] [PubMed] [Google Scholar]
- 43.Hankerson SH, Weissman MM. Church-based health programs for mental disorders among African Americans: a review. Psychiatr Serv. 2012;63:243–249. 10.1176/appi.ps.201100216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Molock SD, Matlin S, Barksdale C, Puri R, Lyles J. Developing suicide prevention programs for African American youth in African American churches. Suicide Life-Threat Behav. 2008;38:323–333. 10.1521/suli.2008.38.3.323. [DOI] [PubMed] [Google Scholar]
- 45.Tandon SD, Dariotis JK, Tucker MG, Sonenstein FL. Coping, stress, and social support associations with internalizing and externalizing behavior among urban adolescents and young adults: revelations from a cluster analysis. J Adolesc Health. 2013;52:627–633. 10.1016/j.jadohealth.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 46.Lindsey MA, Brandt NE, Becker KD, et al. Identifying the common elements of treatment engagement interventions in children’s mental health services. Clin Child Fam Psychol Rev. 2014;17:283–298. 10.1007/s10567-013-0163-x. [DOI] [PubMed] [Google Scholar]
- 47.Becker KD, Lee BR, Daleiden EL, Lindsey M, Brandt NE, Chorpita BF. The common elements of engagement in children’s mental health services: which elements for which outcomes? J Clin Child Adolesc Psychol. 2015;44:30–43. 10.1080/15374416.2013.814543. [DOI] [PubMed] [Google Scholar]
- 48.Austin JL, Jeffries EF, Winston W 3rd, Brady SS. Race-related stressors and resources for resilience: associations with emotional health, conduct problems, and academic investment among African American early adolescents. J Am Acad Child Adolesc Psychiatry. 2021. 10.1016/j.jaac.2021.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brownlow BN, Sosoo EE, Long RN, Hoggard LS, Burford TI, Hill LK. Sex differences in the impact of racial discrimination on mental health among Black Americans. Curr Psychiatry Rep. 2019;21:112. 10.1007/s11920-019-1098-9. [DOI] [PubMed] [Google Scholar]


