Abstract
Background and Purpose:
Neurologic physical therapy (PT) can assist people with neurologic conditions and injuries to optimize their health and wellbeing by addressing barriers at the individual, relationship, community, and societal levels. The purpose of this special interest paper is to provide consensus-driven strategies to address barriers to implementing HPW-related neurologic PT practice.
Summary of Key Points:
Environmental scan, literature review, and expert input were used to determine barriers and develop strategies. Barriers include lack of time; low knowledge, self-efficacy and awareness; client complexity; lack of HPW resources; as well as concerns regarding payment and scope of practice. Four key strategies emerged: (1) develop and disseminate a consensus-based scope of practice for HPW in neurologic PT; (2) increase knowledge of resources related to HPW; (3) promote delivery models for HPW-related neurologic PT; and (4) encourage advocacy, community building and partnership along the continuum of care.
Recommendations for Clinical Practice:
Clinicians should practice to their full scope of HPW-related PT practice. This includes optimizing movement, including physical activity and fitness, as well as reinforcing the importance of healthy sleep, nutrition, stress, and smoking cessation. These activities address primary, secondary, and tertiary prevention. Clinicians are encouraged to report their experiences with HPW-focused delivery models and outcomes. Additional research is needed to understand the full impact of HPW on PT practice.
Health promotion and wellness (HPW) are critical to participation in valued activities and life roles.1, 2 Neurologic physical therapy (PT) is a healthcare delivery mechanism that is ideally placed to assist people with life-changing neurologic conditions and injuries to optimize their health and wellness despite their condition.3, 4 While there are various definitions, health promotion supports individuals, groups, or communities to enable the pursuit of and control over health improvements, prevention, and wellness.1, 5 Wellness incorporates all dimensions of individual and group existence, including optimal physical and emotional health, spirituality, social connectivity, psychological, and intellectual well-being.1, 5, 6 Furthermore, health is inclusive of quality of life and well-being, not merely the absence of disease.1, 5–7
Recent national and international efforts have called on PT to screen and address five core HPW components of healthy lifestyle behaviors: 1) physical activity, including lifestyle physical activity, structured exercise and sedentarism; 2) sleep; 3) stress; 4) nutrition; and 5) smoking.6, 8, 9 Physical activity is “any bodily movement produced by skeletal muscles that results in energy expenditure.”10 It can include basic activities of daily living or exercise, which is defined as “a subset of physical activity that is planned, structured, and repetitive” with an objective to improve or maintain physical fitness.10 Physical activity is the HPW component most often addressed by PT, and its benefits are well-documented.11, 12 However, the four other health behaviors also represent critical modifiable risk factors for the onset of non-communicable diseases (NCDs) such as heart disease and diabetes, which are important considerations in HPW neurologic PT practice.13 Although underexplored in PT literature and practice, these five health behaviors are modifiable risk factors that have been associated with the onset or worsening of neurologic conditions and injuries such as stroke,12, 14–22 spinal cord injury (SCI),23–29 traumatic brain injury (TBI), 30–34 multiple sclerosis (MS),35–38 and Parkinson disease (PD).39–44 PT screening and health promotion activities targeting all five of these health behaviors may reduce risk of NCD and improve the health, wellness, as well as disease-specific and functional outcomes, of clients with neurologic conditions and injuries. Table 1 provides examples of the interactions between modifiable risk factors related to health behaviors, NCDs, and neurologic conditions.
Table 1: Example relationships between neurologic conditions, noncommunicable diseases, and modifiable risk factors related to health behaviors that can be influenced by physical therapy.
Note: this is a non-exhaustive review of the topic.
| Condition | Prevalence of noncommunicable disease or modifiable risk factors related to health behaviors in neurologic condition or injury | Modifiable risk factors or health behavior associated with increased risk of developing neurologic condition or injury (incidence) | Modifiable risk factors or health behavior associated with worse outcomes when one has the neurologic condition |
|---|---|---|---|
| Stroke | • Stroke doubles the risk of having dementia21 • 50% prevalence of sleep disorders after stroke14 |
• Sleep impairment (insomnia) increases risk by 54%18 • High amounts of physical activity reduces risk by 20-25%12 • High cholesterol is associated with increased risk 19 |
• Sedentary lifestyle may aggravate post-stroke fatigue22 • Smoking increases risk of second stroke, MI, or death17, 20 |
| SCI | • 55-68% of population is overweight or obese23 • Increased risk of cardiovascular disease based on blood cholesterol values and hypertension25 • Poor sleep and sleep related breathing disorders are greater in SCI than the general population29 |
• Number of new SCI caused by falls is increasing, along with increased average age of new SCI24 | • Obesity may be associated with the development of upper extremity overuse injuries26 • Nutritional status influences pressure ulcer closure in 27 • Pain and anxiety increase risk of developing chronic health conditions 28 |
| PD | • One-third less active than older adults.42 • Sleep disorders, particularly REM behavior disorder, are common 43 |
• People who are less physically active have a greater incidence of developing PD41 | • More exercise is associated with slower decline in QOL and mobility40 • Poor nutritional status is associated with poorer functional gains during rehabilitation.44 |
| MS | • The prevalence of cardiovascular disease in patients over 60 years old is more than 40%.36 | • Smoking may be associated with a 50% increase in MS risk compared to non-smoking37 | • Relapse rates 2.6 times higher in MS patients with obesity, hypertension, and diabetes36 • Higher accrual of lesions in those with poor diets36 • Smoking contributes to an 80% increase in secondary-progressive MS risk37 |
| TBI | • Sports-related concussions increase risk of sleep distubance32 • Elderly individuals with a history of cancer may have worse outcomes of subsequent TBI31 |
• Complex relationships exist between TBI incidence/ prevalence with substance abuse, family violence, and social determinants of health33, 34 | • Chronic smoking impairs post-TBI recovery30 |
Since 2016, the Academy of Neurologic Physical Therapy (ANPT) has addressed HPW through several initiatives: the HPW Task Force, the IV Step Conference,3, 4 and the 2018 strategic plan, which identified the development of HPW resources as an action step “to advance practice, policy, research and education for those impacted by neurologic conditions.”45 Numerous additional sources have supported the importance of changing the current PT paradigm from a reactive system focused primarily on ‘sick care’ to more proactive health-focused care.6, 8, 9, 46
Although critically important, there are many unaddressed barriers to practicing HPW-related PT. The barriers are organized here through the social ecological model at the individual (client), relationship (clinician-client dyad), community (facilities, organizations), and societal (payment, social determinants of health) levels.47 Barriers related to clients include lack of interest or awareness that PTs provide HPW services, as well as condition complexity (i.e. comorbidities, cognition).6, 46, 48 At the level of the clinician-client dyad, barriers include lack of clinician time and added burden of addressing HPW,6, 46, 48 lack of physical therapist and referral source knowledge of the role of PT in HPW, and low clinician self-efficacy in specific HPW skills (i.e., motivational interviewing).6, 46 Community-level barriers include lack of accessible facilities and trained exercise professionals within local community networks,6, 49, 50 as well as fragmented HPW education resources across consumer and professional organizations.6, 46 Societal-level barriers include payment concerns due to the misperception that the scope of PT practice does not include HPW due to traditional foci on restoration of function.6, 46, 48 and the social determinants of health (SDOH).51 While the SDOH can contribute to barriers across all levels of the social ecological model, they are most notable at the societal level. The SDOH include the domains of economic stability; education access and quality; healthcare access and quality; neighborhood and built environment; and social and community context. These domains can become barriers to the success of physical therapy, as well as PA and HPW, and increase health disparities.51 The relative importance of these barriers may differ between clinicians, populations, and neurologic rehabilitation settings; thus, individually-tailored barriers assessments should be considered.52
Despite the importance of HPW, barriers have slowed implementation of HPW-focused care. The purpose of this special interest paper is to provide expert consensus-driven strategies to address the barriers to implementing HPW-related neurologic PT practice. These strategies sought to (1) develop and disseminate a consensus-based scope of practice for HPW practice in neurologic PT; (2) increase knowledge of resources related to HPW; (3) promote delivery models for HPW-related neurologic PT; as well as (4) encourage advocacy, community building and partnership along the continuum of care. Further, next steps are provided for clinicians and researchers to advance practice and address remaining knowledge gaps.
Methods
This paper represents the work of the ANPT HPW Task Force, which served under the Practice Committee beginning in 2016. The ANPT Board of Directors selected Task Force members after a call for applications sent to all ANPT members. The Task Force consisted of 7 individuals (clinicians, researchers, and educators), with an average 18±8 years of experience in the field and expertise across neurologic PT diagnoses, practice settings, classroom and clinical education, and HPW-related research areas (Table 2).
Table 2.
Characteristics of Health Promotion and Wellness Task Force Members (N=7)
| Credentials | N (%) |
|---|---|
| DPT | 3 (43%) |
| NCS | 4 (57%) |
| PhD | 5 (71%) |
| CEEAA | 2 (29%) |
|
| |
| Professional Area of Expertise | |
|
| |
| Research | 3 (43%) |
| Entry-Level DPT Teaching | 5 (71%) |
| Post-Professional Teaching | 3 (43%) |
| Residency Director/Mentor | 2 (29%) |
| Clinical Instructor | 1 (14%) |
| Expert Clinician | 4 (57%) |
|
| |
| Diagnostic Expertise | |
|
| |
| Stroke | 4 (57%) |
| Spinal Cord Injury | 1 (14%) |
| Brain Injury | 3 (43%) |
| Parkinson’s Disease | 1 (14%) |
| Multiple Sclerosis | 1 (14%) |
| Other Neurodegenerative | 1 (14%) |
|
| |
| HPW-Related Expertise | |
|
| |
| Research | 5 (71%) |
|
| |
| Entry-Level DPT Teaching | 6 (86%) |
|
| |
| Post-Professional Teaching | 5 (71%) |
|
| |
| Practice | 5 (71%) |
Abbreviations: CEEAA, certified exercise experts for aging adults; DPT, doctor of physical therapy; NCS, Board-Certified Clinical Specialist in Neurologic Physical Therapy; PhD, doctor of philosophy.
The HPW Task Force examined previously reported HPW priorities within general and neurologic PT practice, identified barriers, and executed an action plan. An environmental scan of existing literature and resources was conducted alongside consensus building with expert stakeholders. The environmental scan focused on investigating definitions of HPW, existing and needed resources related to HPW, the role of contemporary neurologic PT in HPW practice, barriers to HPW practice, and strategies to overcome these barriers. The environmental scan was conducted initially from 2016-2017, but remained iterative through 2020 as new information arose. Information gathered included international definitions,1, 5, 7 position statements from national and international PT organizations,3, 4, 8, 9, 53, 54 peer-reviewed literature on HPW practice and barriers, 2, 3, 6, 8, 9, 46, 48 and existing client-focused community resources available on the internet related to neurologic HPW.
Consensus building on the four strategies to address barriers to HPW practice included review, discussion and debate on the results of the environmental scan by HPW Task force members and consultation with other subject matter experts, including American Physical Therapy Association (APTA) leadership, ANPT leadership, and the APTA HPW Council. The APTA HPW Council is a networking and APTA-advising body who educate and advise health colleagues on the roles of PTs in health promotion, wellness, and prevention. The HPW Task Force synthesized this information, discussed and resolved any discrepancies through discussion at monthly meetings, a 2-day working meeting, and email communication. Ultimately a map of the four strategies to address the barriers identified was developed. Figure 1 illustrates this map depicting the relationship between the barriers and strategies, organized by the social ecological model.
Figure 1. Map Connecting Barriers to Strategies Promoting HPW in Neurologic Physical Therapy.
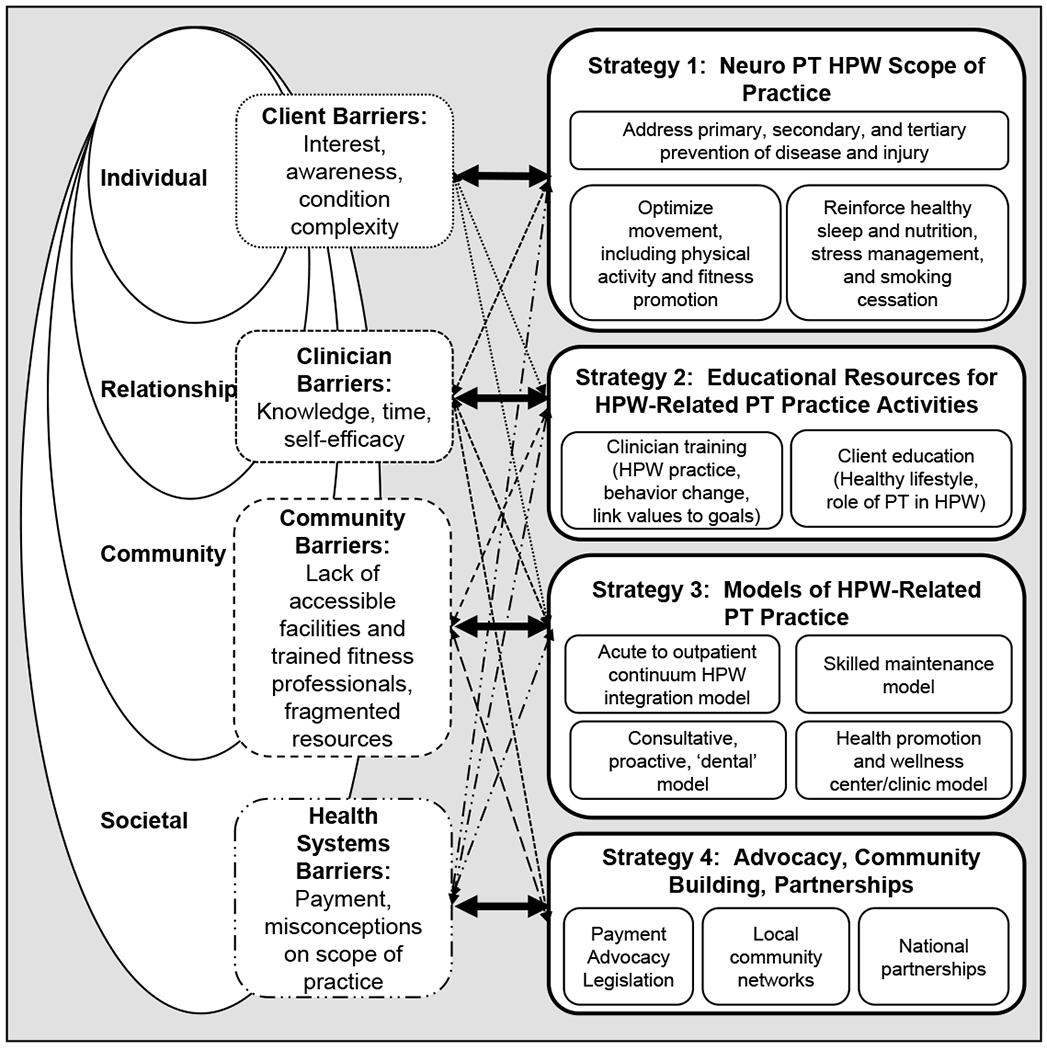
Barriers identified in the literature were organized using the social ecological model (Left). Strategies identified by the ANPT HPW Task Force are summarized (Right). Each strategy target barriers at a specific level of the social ecological model; however, each barrier is addressed by multiple strategies, and multiple strategies address each barrier (Center bidirectional arrows.
1. Develop and Disseminate a Consensus-Based Scope of Practice for HPW Practice in Neurologic PT
A clear consensus statement on HPW neurologic PT practice addresses barriers related to lack of public awareness regarding the role of PT in HPW, as well as a lack of knowledge or interest in HPW-related PT practice by neurologic physical therapists, referrers, and clients (Figure 1). A clear scope of practice also assists legislative advocacy and payment efforts. The scope of HPW-related neurologic PT includes addressing primary, secondary and tertiary prevention of disease and injuries by: (1) optimizing movement, including the promotion of physical activity and fitness and (2) reinforcing the importance of healthy sleep and nutrition, stress management, and smoking cessation. Resources supporting this scope were the APTA Guide to Physical Therapy Practice 3.0,5 the World Health Organization,7 the Ottawa Charter for Health Promotion,1 APTA House of Delegate (HOD) position statements,53, 54 articles outlining consensus work from the World Confederation for Physical Therapy,8, 9 and prior articles addressing HPW in neurologic PT practice.3, 4
Determining and disseminating expert consensus on HPW neurologic PT scope of practice helps to clarify controversial areas related to HPW in neurological PT practice, without attempting to extend practice. The first area of controversy is the role of PT in screening and addressing health behaviors beyond physical activity and fitness. The APTA HOD position statements are clear that nutrition, sleep, stress, and smoking are within PT scope of practice, as long as all local state licensing laws and regulations are followed and the clinician is acting within their own personal scope of practice based on training and expertise.
Another controversial area of HPW in neurologic PT is the understanding of the PT role in primary, secondary, and tertiary prevention. Traditional PT falls under the scope of tertiary prevention, or reducing the negative impact of ongoing illness or injury to improve function and quality of life.55 The role of neurologic PT in secondary prevention, or reducing the impact of disease and injury through screening and early intervention to prevent long-term problems has also been well-defined.3, 55 Secondary prevention is particularly important based on the role of physical activity in maintaining function, promoting quality of life, and decreasing risk of cardiovascular complications and NCDs in people with neurologic diseases. The role of PT in primary prevention, or the prevention of a disease or injury from occurring, is less prevalent, but growing.3, 6, 55 The most common examples of primary prevention in neurologic PT are the role of physical activity in cardiovascular and brain health, as well as community-based fall screenings for older adults, which could prevent traumatic spinal cord and brain injuries.
The APTA has been advancing the role of PT in primary prevention through position statements,53, 54 the Guide to PT Practice,5 the development of the Annual PT Visit and its associated training tools,56 and support of APTA HPW Council. Clinicians who work in community wellness settings, cash-based PT settings, or who consult on population-level initiatives are at the leading edge of primary prevention efforts. However, current advocacy work by the APTA for payment of PT services as part of wellness and prevention programs will advance primary prevention in more traditional healthcare settings.57 In addition to legislative advocacy, the APTA shares implementation plans for an Annual PT Visit across the lifespan, even in individuals with no known health conditions.56 Within traditional neurologic PT settings, clinicians can schedule an Annual PT Visit to address secondary and tertiary prevention within the context of their neurologic condition. During those annual visits, screening for health behaviors will also address primary prevention of NCDs. For example, screening for and addressing nutrition and smoking in an individual with MS may be associated with reduced signs of disease progression,36, 37 as well as primary prevention of NCDs such as obesity and lung disease. Although each payer is different, the initiation of direct access and reimbursable skilled maintenance therapy (see strategy 3) support neurologic physical therapists to address prevention in traditional healthcare settings. This article addresses ongoing barriers to HPW and prevention practice through the provision of implementation strategies and education. Physical therapists can then advocate to their healthcare administrators, referrers, and communities about their role in HPW and prevention.
2. Increase Knowledge of Resources related to HPW
Barriers related to low clinician knowledge, time, and self-efficacy are addressed by investigating and compiling existing clinician training and client education HPW resources (Figure 1) and addressing gaps in resources as identified. Compiling the existing resources also addresses barriers related to client knowledge and complexity, as well as the fragmented information available on community resources.
There is a growing number of high quality HPW education resources available for the general public and some for people with neurologic conditions. Reputable client-focused education resources include national and international professional organizations, consumer organizations, and government initiatives, as well as a variety of reputable disability advocacy and condition-specific organizations. The lack of awareness of these resources and spread of these resources across various organizations makes it difficult for practicing clinicians to find appropriate information quickly and may lead to duplicating work. Furthermore, many of the resources do not include the role of PT in HPW-related topics.
Existing educational resources that can facilitate HPW practice in neurologic PT are shared on the ANPT HPW webpage and summarized in Table 3. Increasing awareness of existing client-focused resources may reduce duplication of efforts by clinicians. Resources include education sheets, booklets, and videos developed by professional groups such as the APTA; the National Center on Health, Physical Activity and Disability (NCHPAD); and the Exercise is Medicine® (EIM) Campaign by the American College of Sports Medicine (ACSM). The ANPT HPW webpage includes up-to-date resources on each of the HPW topics, including examples from government initiatives and client-focused resources, such as nutrition materials provided by the U.S. Department of Agriculture, and healthy sleep information from the National Sleep Foundation. Using existing resources to support client education can benefit both clinicians and clients. They facilitate comprehensive rehabilitation and wellness programs and serve to link individuals to appropriate community organizations enhancing support and self-advocacy.
Table 3:
Sources of Educational Resources to Facilitate Physical Therapy Delivery of Health Promotion and Wellness Content to People with Neurologic Disorders
| Resource Source | Types of Resources Provided | Example Organizations |
|---|---|---|
| National and International Organizations | • Summary of State Policies • Clinician networking groups • Clinician education (fact sheets, presentations, tool boxes, knowledge synthesis) • National initiatives including ‘Exercise is Medicine’ • Consumer education |
• American Physical Therapy Association • World Confederation for Physical Therapy • American College of Sports Medicine • Preventive Cardiovascular Nurses Association • National Physical Activity Plan • World Health Organization • Center for Medicare Advocacy |
| Clinical Practice Guidelines Repositories | • Condition-specific guidelines may include information on physical activity • U.S. nutrition and physical activity guidelines |
• APTA Evidence-Based Practice Resources • National Institute for Health and Care Excellence (U.K.) • ParkinsonNet • U.S. Office of Disease Prevention and Health Promotion |
| Consumer Organizations | • Consumer education (websites, webinars, fact sheets, exercise programs) • Evidence-based health programs |
• National Multiple Sclerosis Society • Parkinson’s Foundation • American Stroke Association • United Spinal Association • Brain Injury Association • Evidence-based health programs at the Y (YMCA) • National Center on Health, Physical Activity and Disability by Centers for Disease Control and Prevention (NCHPAD) • National Sleep Foundation |
| Government Initiatives (United States) | • Consumer education (websites, fact sheets, videos) • Information for healthcare providers and exercise professionals • Virtual training programs • Activity tracking programs |
• National Institute on Aging • Move Your Way by Office of Disease Prevention and Health Promotion • Centers for Disease Control and Prevention Programs for Addressing Social Determinants of Health • MyPlate by U.S. Department of Agriculture |
Note: Please see the ANPT HPW Website for updated links to these resources60
While we encourage the use of existing reputable HPW education resources (Table 3), many of these resources target clients rather than physical therapists. They often do not clearly address the role of PT in HPW-related topics (e.g. when, where, and how to intervene). Several clinician training tools have been developed by and for physical therapists, which are now available online through ANPT. These tools can help address clinician barriers related to lack of knowledge and time by providing information about HPW screening and assessment tools, as well as behavior change strategies. These tools include: (1) the ANPT HPW webpage,58 (2) the ANPT Synapse Education Platform course, ‘Health Promotion and Wellness Strategies Applied in NeuroRehabilitation’ and (3) the ‘Bridging the Gap between PT and Lifelong Physical Activity and Exercise in People with Neurological Conditions Toolkit’.59 Any new resources developed should build upon existing resources, ensure accessibility, and address health literacy.
The ANPT HPW webpage (https://www.neuropt.org/practice-resources/health-promotion-and-wellness)60 was launched in 2019. It provides a platform for sharing reputable educational resources curated for physical therapists. Resources are organized as (1) clinician resources and tools, (2) client/patient resources and tools, (3) translation to practice setting tools, (4) foundational learning and key articles, and (5) links to information from the condition-specific ANPT Special Interest Groups on HPW topics. The HPW webpage is open to the public and updated regularly to share the most accurate and evidence-based information.
The ANPT Synapse Education Platform includes an online continuing education course titled ‘Health Promotion and Wellness Strategies Applied in NeuroRehabilitation.’ This course provides education on foundational HPW topics based on the US National Prevention Strategy (USNPS) health priorities as described by the APTA54 and international peer-reviewed literature in PT education.8 These concepts include the HPW domains of physical activity3, 4 (structured exercise, sedentarism, and lifestyle physical activity), nutrition,23, 36, 61 sleep health,14, 35, 62 stress management,15, 39, 63, 64 depression,35, 65–67 smoking cessation,16, 46, 68, 69 polypharmacy,70, 71 and violence prevention.72, 73 Additionally, the course provides clinical tools, including education on the role and scope of neurologic PT in HPW,8, 53, 54, 74, 75 as well as outcome measurement and screening tools for HPW and physical activity.76–79 The Synapse education course also includes information on health behavior change models and motivational interviewing-informed practice.50, 80–84
The ‘Bridging the Gap between PT and Lifelong Physical Activity and Exercise in People with Neurological Conditions’ document was developed originally by the ANPT Spinal Cord Injury Special Interest Group.85 With author permission, it was adapted for general neurologic PT audiences with additional resource material. This toolkit now provides detailed objectives and rationale for promoting lifelong physical activity, how to assist clients in connecting back to PT after an episode of care, and multiple appendices that serve as educational materials, worksheets, and references. The aim of this toolkit is to facilitate PT-client dialogue and shared decision-making around values, goals, barriers, and action planning to promote healthy physical activity and exercise habits for individuals living with a neurologic condition or injury.
Knowledge and dissemination of HPW principles and practice is also growing in entry-level DPT education, although more work is needed. Magnusson et al, provides core competencies for population health, prevention, health promotion and wellness in PT which can guide and enhance education of new clinicians and help programs address HPW-related CAPTE standards (7D11, 7D14. 7D19h, 7D20, 7D23, 7D34, 7D39, 7D40, 7D41).86 Rethorn et al.’s survey of DPT programs highlights the need for continued support of and resources for faculty to teach HPW.87
3. Promote Delivery Models for HPW-related Neurologic PT
The environmental scan and consensus building process led to identifying the importance of developing and disseminating delivery models for HPW-related PT practice to address barriers across all levels of the social ecological model. Sharing practical delivery models addresses barriers related to clinician time and knowledge; interest and awareness of clients and referrers; community exercise and education resources; as well as the understanding of the general public and third-party payers on how PT can address HPW (Figure 1). Four delivery models revealed in the environmental scan include: (1) acute to outpatient rehabilitation continuum model,49 (2) proactive consultative ‘dental’ model,88 (3) skilled maintenance model,89 and (4) health promotion and wellness center/clinic model.90, 91 Each model is defined, with delivery and documentation considerations in Table 4. Models may involve partnerships with evidence-based community programs, exercise professionals, caregivers (formal and informal), research studies, and community organizations.92, 93 All models should include screening for lifestyle health behaviors, including physical activity (e.g. structured exercise, sedentarism, and lifestyle physical activity), nutrition, smoking, sleep, and stress management. Clinicians should also consider how the SDOH can influence successful outcomes. Interventions should be delivered as appropriate per PT scope of practice, noting potential differences between practice settings, state regulations, and need for additional clinician training.
Table 4:
Physical Therapy Delivery Models Incorporating Health Promotion and Wellness
| Model* | Model 1 = Acute to Outpatient Continuum HPW Integration Model | Model 2 = Consultative, Proactive, ‘Dental’ Model | Model 3 = Skilled Maintenance Model | Model 4 = Health Promotion and Wellness Center/Clinic Model |
|---|---|---|---|---|
| Operational definition | • Introduce adapted lifestyle physical activity in acute rehab. • Foster independent community physical activity and enhance fitness in outpatient rehab. • Transition to semi-supervised or independent exercise through continuum of care.49 |
• Provide expertly tailored exercise prescription, monitoring, & progression. • Goals to restore, improve, or maintain function and to optimize movement. • Use proactively after diagnosis or for long-term monitoring in chronic disease.88 |
• Medicare coverage of SNF, HH, and OP services for skilled care to improve, maintain or prevent or slow further deterioration.89 • Functional gains not required. • Must be reasonable, necessary care that cannot be delivered by non-skilled personnel. |
• Exercise programs are completed with assist and progressed with PT monitoring or supervision as needed. • Part of a traditional rehab center, a stand-alone non-profit organization, or a community center. • Services provided by licensed or non-licensed professionals.90, 91 |
| Delivery considerations* | • Gradually fade visit frequency following restorative care to monitor transition to community exercise. • Consider transitioning to model 2-4, as needed. • Traditional payment model |
• Brief episode of care (~1-4 visits). • Follow-up episodes recommended every 3-12 months, depending on self-efficacy, independence, or risk of functional decline. • Traditional payment model |
• Bimonthly or monthly visits to monitor and modify optimizing movement programs.133 • Weekly visits if patient is at high risk for rapid change. • Medicare-specific model definition may not apply to all private insurers |
• Transition outpatient visits to community center outside healthcare delivery system. • Common barriers include accessibility and affordability. • Commonly cash or philanthropy-funded. |
| Documentation considerations** | • Document prior level of physical activity. • Create transition plans through continuum. • Document education and stage of change. |
• Document medical need for regular exercise and skilled exercise prescription. • Evaluate and document physical activity and exercise FITT-VP. |
• Justify skilled care clearly (i.e., medical need for exercise monitoring and adjustments due to complex and/or changing medical and functional needs). | • Vary depending on state practice act and individual center/clinic policies. • Evaluate and document physical activity and exercise FITT-VP. |
Common delivery considerations: All models should include screening for physical activity (structured exercise, sedentarism, and lifestyle physical activity, as well as nutrition, smoking, sleep, and stress management. Delivery should include HPW outcome measures, facilitating behavior change, and training caregiver and or extenders (e.g., PTA, non-licensed exercise professionals) as needed.
Common documentation considerations: All models should document physical activity and exercise assessments, as well as the need for skilled PT to assess, prescribe, monitor, and progress exercise in clients with neurologic conditions.
Abbreviations: FITT-VP, frequency intensity time type volume and progression; HH, home health; OP, outpatient; Rehab, rehabilitation; SNF, skilled nursing facility
Note: These delivery models may be modified with health policy changes over time.
Table 5 summarizes examples of how each delivery model can be applied, with a focus on physical activity. The models are applicable across various neurologic conditions and injuries where documented evidence for the benefits of healthy lifestyle behaviors exists, including SCI,94, 95 TBI,96, 97 stroke,90, 98–100 MS,101–104 and PD.105–107 With each delivery model, clinicians should measure and track physical activity outcomes appropriate to the setting. Measures may include aerobic fitness, accelerometer or pedometer-measured step counts (or wheelchair push counts),108, 109 brief patient-reported outcome measures such as the Physical Activity Vital Sign,110, 111 the Godin Leisure Time Exercise Questionnaire,79 or the longer International Physical Activity Questionnaire to assess sedentary time.112, 113 Physical therapists should also facilitate healthy behavior change9, 46, 50, 114, 115 using the readiness to change questionnaire116 and exercise self-efficacy scales.114, 115 If a client cannot be independent with their exercise maintenance and progression despite behavior change strategies, clinicians should train and utilize caregivers and or extenders (e.g., physical therapist assistants or non-licensed exercise professionals as appropriate). In addition to physical activity, Table 5 includes screening tools and education regarding nutrition,117 smoking,8, 118 sleep,119, 120 and stress management.56, 121, 122 Screening and education should ensure client health literacy123 and advocacy for connection to environmental and personal supports in the community and healthcare system.56
Table 5:
Application Examples of Health Promotion and Wellness Delivery Models
| Model | Model 1 = Acute to Outpatient Continuum HPW Integration Model | Model 2 = Consultative, Proactive, ‘Dental’ Model | Model 3 = Skilled Maintenance Model | Model 4 = Health Promotion and Wellness Center/Clinic |
|---|---|---|---|---|
| Client Examples (non-exhaustive) | Individual with new injury (e.g. stroke, TBI, SCI) or illness in acute inpatient rehabilitation | Individual newly diagnosed with neuro-degenerative condition (e.g. PD, MS) or individual with chronic condition (stroke) | Individual with significant impairment or chronic condition at high risk of functional decline (e.g. ALS, advanced PD, MS) | Individual with subacute injury or illness requiring significant community support (e.g. subacute SCI, stroke) |
| Physical Activity and Exercise Promotion within PT Delivery Model | Educate on the importance of lifestyle physical activity. Facilitate peer mentor visit describing active lifestyle. In OP PT, introduce to progressive walking programs and adaptive exercise equipment. Fade frequency of visits while investigating community-based physical activity resources. Transition to model 4. | Baseline evaluation of walking, balance, physical activity, and exercise participation. 3 additional visits every 2-4 weeks to increase duration and intensity of structured exercise program in community gym with trainer. Condition-specific exercise programs. Re-check in 6 months. | OP or HH PT 1-2/week. Transitioned to 1-2x/month during periods of stability, to provide skilled care to monitor for changes in functional status. Problem-solve, modify, and progress exercise, recommend equipment. Family/client education and training. | Refer to a specialized medical fitness center for post-rehabilitation exercise. Center is staffed by PT, OT, and exercise physiologists who provide a fitness evaluation, and design and assist as needed in an individualized exercise plan. Center is accessible and has condition-specific equipment (e.g. standing frame, body weight support, FES cycle, and wheelchair treadmill. |
| Cost of Physical Activity Plan of Care within PT Delivery Model | Insurance co-pays, followed by model 4 costs. | Insurance copays, community exercise expenses (gym, trainers, PD-specific exercise class). | Insurance co-pay | Monthly gym membership (Medicare Silver Sneakers coverage), cash-pay for additional services with scholarships available (personal training/exercise therapy). |
| Example of physical activity measures | • Prior activity level with PA measure | • Physical Activity Vital Sign110, 111 • Godin Leisure Time Exercise Questionnaire79 • Exercise Self-Efficacy114, 115 • Accelerometry-based measure108, 109 |
• International Physical Activity Questionnaire-Long form112, 113 • Accelerometry-based measures108, 109 |
• Physical Activity Vital Sign110, 111 • Godin Leisure Time Exercise Questionnaire79 • Exercise Self-Efficacy Scale114, 115 • Accelerometry-based measures108, 109 |
|
Example Additional HPW Measures and/or Screening Questions
* Can be Used in Any Model** |
Nutrition • How many fruits and vegetables do you eat per day? • Starting the Conversation Tool117 • Readiness to Change116 Sleep • How many hours of sleep do you regularly get? Do you feel well rested when you wake up? • Pittsburgh quality sleep index119 • Stop-Bang Questionnaire for Sleep Apnea120 Stress • How is your stress level? • Perceived stress scale-14121 • Brief-COPE122 Smoking • Do you smoke? (non-smoker, current smoker, stopped smoking in the past 6 months)? • Readiness to Change116 |
|||
|
Additional HPW Education Component Examples Can be Used in Any Model** See table 3 for educational resource materials. |
Nutrition • Recommend well-balanced diet and dietician consult. • Educate on how diet impacts energy and activity. Sleep • Educate on sleep hygiene. • Educate on reducing sedentarism and increasing lifestyle PA. • Recommend peer and caregiver support groups. Caregiver respite services if needed. Stress • Educate on stress management, possibly including meditation and mindfulness. • Recommend counseling or peer support groups Smoking • Use MI-informed communication strategies • Use the 5A’s and 5R’s model for smoking cessation education and support.8, 118 • Educate on importance of smoking cessation • Recommend peer support groups |
|||
The additional HPW measures, screening questions, and education should be applied across all the delivery models as needed for their clients. Education should begin with assessment or screening questions, dialogue to understand readiness to change, and should proceed using principles of shared decision-making.
Abbreviations: ALS, amyotrophic lateral sclerosis; CVA, cerebrovascular accident; FES, functional electrical Stimulation; HH, home health; OP, outpatient; OT, occupational therapy; PD, Parkinson’s disease; PT, physical therapy; SCI, spinal cord injury; y/o, years old
One healthy lifestyle behavior is presented in each model in Table 5, but these examples can be applied across all models due to similarities in screening and educational approaches. The following example highlights the similarities and differences for one HPW area, nutrition, in two delivery models. In an acute care setting, the physical therapist may ask informal screening questions regarding nutrition, and refer to an inpatient registered dietician for full assessment and intervention. The informal screen may be completed by asking ‘How many servings of fruit and vegetables do you typically eat per day?’ to gauge overall healthy eating habits; ‘Have you had any changes in your diet since entering the hospital?’ to assess changes and current intake; and ‘How much water have you drunk today?’ to determine hydration and potential impact on PT.6, 56 The physical therapist then provides education on the importance of nutrition to PT, physical activity, function, and overall well-being, and requests a referral to a dietician as appropriate.6 In contrast, in an outpatient proactive consultative dental model, nutrition may be assessed formally through a screening tool such as the ‘Starting the Conversation’ Tool or using similar informal screening questions as in acute care.117 Depending on the results of the nutrition screening, the physical therapist may further explore readiness to change nutritional habits and provide general healthy eating resources from the U.S. Department of Agriculture consumer-facing nutrition website. The physical therapist can also request a referral to a registered dietician for further assessment and intervention if needed. Current payment limitations on dietary services in outpatient settings highlights the importance of screening for HPW topics and providing appropriate referrals during acute rehabilitation when the service is more accessible. Screening resources, including interview questions, standardized tools, and frameworks, for assessing lifestyle health behaviors and readiness to change are available through several resources including the newly updated Annual PT Visit available through the APTA.6, 8, 46, 56
One common feature across all four delivery models is the need to approach PT with a strong foundation in behavior change techniques. Incorporating behavior change strategies into physical therapy requires knowledge of theories and models, as well as the ability to apply that knowledge in practice. Knowledge of the behavior change theories have been well summarized by Bezner and colleagues (2017).50 They have also been summarized in the ANPT HPW Synapse Education series. Theories addressed include the transtheoretical model,124 which includes aspects of readiness to change125 and self-efficacy.126 It is recommended that readers interested in health behavior change consider both self-study using seminal texts, such as that by Glanz and colleagues (2015) and continuing education courses.127
4. Encourage Advocacy, Community Building and Partnership along the Continuum of Care
The final strategy to improve delivery of HPW-related neurologic PT practice is through advocacy, community building and establishing partnerships along the continuum of care. This strategy addresses barriers related to payment, public interest and awareness on the importance of HPW and accessibility, as well as time and efficiency of the clinician related to ease of community referrals (Figure 1). Physical therapists are advancing the role of HPW in legislative efforts and partnerships with outside organizations. Additionally, physical therapists may help drive change to address SDOH through advocacy and population health initiatives. These relationships at the national and local level may be through governmental organizations, nonprofit organizations, or community wellness centers.
At the national level, the APTA has partnerships with ACSM’s Exercise is Medicine® campaign and the Academy of Geriatric Physical Therapy’s (AGPT) has a collaboration with National Council on Aging (NCOA). Additionally, the APTA is a partner of the Physical Activity Plan Alliance committed to implementing the National Physical Activity Plan. Other national PT groups addressing the need for advocacy include the APTA’s HPW Council, the ANPT Advocacy and Consumer Affairs Committee, the ANPT Membership and Public Relations Committee, and the HPW Special Interest Group of the Academy of Geriatric Physical Therapy. Because important HPW partnerships can span neurologic and non-neurologic populations, APTA’s HPW Council is an ideal avenue to facilitate communication of national and international efforts between groups.
One example highlighting the importance of cross-group communication is the recently developed population health, prevention, health promotion and wellness competencies for entry-level DPT practice.86 The APTA”s HPW Council sponsored this document and communicate it to PT educators across specialty areas.86
At the local levels, clinicians may need to advocate with clinic administration and payers to set up processes to integrate HPW delivery models. For example, they should consider appropriate referrals, electronic documentation, and communication between providers. Further, they can enhance engagement and ease transitions to lifelong physical activity and exercise by connecting clients with local adaptive exercise trainers and evidence-based programs in their communities. There are at least 10 professional organizations that train exercise professionals to work with people with disabilities and medical conditions. Examples of these organizations include ACSM, American Council on Exercise, and NCHPAD. It is also important for clinicians to be aware of evidence-based exercise programs in their local communities. As part of the AGPT/NCOA partnership, tools were developed to help therapists understand and connect clients to evidence-based programs such as a Matter of Balance (Moving for Better Balance), Enhance Fitness, and NeuroFit.128–130 Standardized implementation and training procedures ensure consistent delivery to maximize outcomes. Therapists are encouraged to follow the joint work of AGPT/NCOA to disseminate these evidence-based programs.131
Next Steps to Advance HPW Practice and Address Knowledge Gaps
To advance HPW-related neurologic PT practice, clinicians should practice to the full scope of PT practice within the various HPW delivery models presented, while being aware of state and local policies and personal expertise that could influence their care. They should use existing resources and develop partnerships with wellness organizations in their community. Additionally, the ANPT may consider national partnership development with consumer advocacy organizations to promote the role of PT in physical activity promotion. Clinicians are encouraged to document outcomes and share experiences through local and national education programs, case study manuscripts, communication with peers via the ANPT neuro listserv, and legislative advocacy through APTA’s Legislative Action Center. Measuring outcomes and sharing knowledge are essential components of evidence-based practice. Barriers to HPW practice have been well-documented,6, 46, 48 and thus sharing successful practical examples of implementation strategies and outcomes could enhance delivery world-wide.
Additional research is needed to address knowledge gaps related to HPW neurologic PT practice. The first recommendation for researchers is to develop, refine, and synthesize knowledge related to clinically-feasible, valid patient-reported and accelerometer-based measures of physical activity.78, 79, 108, 109 These measures will have improved utility with a better understanding of their psychometric properties across populations. Publishing knowledge translation tools to facilitate real-world implementation of these measures could enhance the likelihood of success. Second, researchers studying traditional restorative PT interventions are encouraged to consider the impact of nutrition, sleep, smoking cessation, stress management, lifestyle physical activity and, sedentarism, as potentially impactful covariates in the study design. Knowledge translation research should examine the impact of PT-led HPW interventions on client-specific barriers, including readiness to change and self-efficacy. Additionally, research is needed to explore the role of the SDOH on PT outcomes, particularly environmental factors such as safe places for physical activity and healthy food.132 Large-scale clinical trials on the role of neurologic PT in improving physical activity and other lifestyle behaviors should measure outcomes related to the development of NCDs, hospitalization rates, quality of life, and participation. Finally, PT health services researchers may want to partner with payers to conduct demonstration projects related to PT for HPW.
Limitations
While this paper identifies and compiles important strategies to address barriers to HPW practice, limitations should be considered. The suggested strategies primarily target clinicians. The resources provided may not address problems experienced by clients in underserved communities or specific geographic areas. Additionally, limited information is included on how to change processes and policies at the level of the health systems or payers. Future work in these areas could ease the burden placed on clients, as well as the burdens on physical therapists delivering primary prevention or addressing population health. Finally, methodologic limitations include lack of a systematic review and lack of a formal Delphi process. Rather, environmental scan, narrative review, expert opinion, and informal expert consensus were used. Future work should develop systematic reviews and clinical practice guidelines as more evidence becomes available.
Conclusion
Shifting from a reactive care model to a proactive model of PT that includes HPW will take individual and collective efforts. Implementing the strategies identified here clarifies the role of PT to all stakeholders and addresses previously reported barriers to HPW practice. Physical therapists can help people be well despite living with a neurologic condition or injury. Individuals living with neurologic conditions need experienced and knowledgeable clinicians to optimize movement, health, and wellbeing.
Supplementary Material
Acknowledgements
We thank the ANPT Evidence Based Documents Committee and Board of Directors, the APTA HPW Council, ANPT HPW Taskforce consultants (Jennifer Gansen, Rupal Patel, Catherine Siengsukon), ANPT HPW Committee, and Hadiya Green Guerrero, PT, DPT a Senior Practice Specialist at the APTA for their feedback and support in initial consensus building on health and wellness priorities in neurologic PT practice and/or external review of the manuscript. Additionally, we thank Ella Nettnin, BS for assistance with figure and manuscript formatting.
Sources of Funding:
This work was supported in part by the Academy of Neurologic Physical Therapy, National Institutes of Health’s National Institute on Aging (P30AG059988), Department of Defense (PD190069), Agency for Healthcare Research and Quality (F32HS025077), and Foundation for Physical Therapy (NIFTI2016). SAB and SF receive funding from the National Institutes of Health. ECHB, SF, KJH, KM have no additional sources of funding to report. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders. However, Members of the Academy of Neurologic Physical Therapy Board of Directors and Evidence-Based Documents Committee provided feedback on drafts of this manuscript.
Potential Conflicts of Interest:
All authors received honoraria and travel support related to this work from the Academy of Neurologic Physical Therapy as members of the Health Promotion and Wellness Task Force. Additionally, AR is a member of the World Health Organization Development Group for a Package of Rehabilitation Interventions for Traumatic Brain Injury. MRR received additional concurrent funding from the National Institute of Disability, Independent Living, and Rehabilitation Research; Academy of Neurologic Physical Therapy; Parkinson’s Foundation; and Davis Phinney Foundation. SAB has a patent pending (18KU028M-02). ECHB, SF, KJH, KM have no additional potential conflicts of interest to report.
Footnotes
- ANPT Synapse Center Online continuing education course “Health Promotion & Wellness Strategies Applied to Neurorehabilitation.”
- Two-day preconference course at the Combined Sections Meeting of the American Physical Therapy Association. January 2019 titled “Health Promotion and Wellness Strategies Applied to Neurorehabilitation.”
- Related resources are shared on the ANPT HPW webpage (https://www.neuropt.org/practice-resources/health-promotion-and-wellness)
Contributor Information
Miriam R Rafferty, Shirley Ryan AbilityLab; Northwestern University Feinberg School of Medicine Departments of Physical Medicine and Rehabilitation and Psychiatry and Behavioral Science.
Elissa C Held Bradford, Saint Louis University, Department of Physical Therapy and Athletic Training.
Stacy Fritz, University of South Carolina, Arnold School of Public Health, Department of Exercise Science, Physical Therapy Program.
Karen J Hutchinson, College of Health and Rehabilitation Sciences: Sargent College, Boston University, Boston, MA.
Kimberly Miczak, MossRehabilitation Hospital.
Arielle Resnick, Kessler Institute for Rehabilitation.
Sandra A Billinger, University of Kansas Medical Center, Department of Physical Therapy and Rehabilitation Science, Department of Neurology, Department of Physical Medicine and Rehabilitation.
References:
- 1.World Health Organization. The Ottawa Charter for Health Promotion. World Health Organization. Accessed April 30, 2016, https://www.who.int/healthpromotion/conferences/previous/ottawa/en/ [Google Scholar]
- 2.Adams T, Bezner J, Steinhardt M. The Conceptualization and Measurement of Perceived Wellness: Integrating Balance across and within Dimensions. Am J Health Promot. Jan-Feb 1997;11(3):208–18. doi: 10.4278/0890-1171-11.3.208 [DOI] [PubMed] [Google Scholar]
- 3.Quinn L, Morgan D. From Disease to Health: Physical Therapy Health Promotion Practices for Secondary Prevention in Adult and Pediatric Neurologic Populations. J Neurol Phys Ther. Jul 2017;41 Suppl 3:S46–s54. doi: 10.1097/npt.0000000000000166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kimberley TJ, Novak I, Boyd L, Fowler E, Larsen D. Stepping up to Rethink the Future of Rehabilitation: Iv Step Considerations and Inspirations. J Neurol Phys Ther. Jul 2017;41 Suppl 3(Suppl 3):S63–s72. doi: 10.1097/npt.0000000000000182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Physical Therapy Association. Guide to Physical Therapy Practice 3.0. American Physical Therapy Association 2014. Updated Nov 27, 2016. Accessed April 30, 2016. http://guidetoptpractice.apta.org/ [Google Scholar]
- 6.Bezner JR. Promoting Health and Wellness: Implications for Physical Therapist Practice. Phys Ther. Oct 2015;95(10):1433–44. doi: 10.2522/ptj.20140271 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Constitution. World Health Organization. Accessed Feb 2, 2021. https://www.who.int/about/who-we-are/constitution
- 8.Dean E, Greig A, Murphy S, et al. Raising the Priority of Lifestyle-Related Noncommunicable Diseases in Physical Therapy Curricula. Phys Ther Jul 2016;96(7):940–8. doi: 10.2522/ptj.20150141 [DOI] [PubMed] [Google Scholar]
- 9.Dean E, Skinner M, Myezwa H, et al. Health Competency Standards in Physical Therapist Practice. Phys Ther. Sep 1 2019;99(9):1242–1254. doi: 10.1093/ptj/pzz087 [DOI] [PubMed] [Google Scholar]
- 10.Caspersen CJ, Powell KE, Christenson GM. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public health reports (Washington, DC : 1974). Mar-Apr 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- 11.Ellis T, Motl RW. Physical Activity Behavior Change in Persons with Neurologic Disorders: Overview and Examples from Parkinson Disease and Multiple Sclerosis. J Neurol Phys Ther. Jun 2013;37(2):85–90. doi: 10.1097/NPT.0b013e31829157c0 [DOI] [PubMed] [Google Scholar]
- 12.Gallanagh S, Quinn TJ, Alexander J, Walters MR. Physical Activity in the Prevention and Treatment of Stroke. ISRN Neurol. 2011;2011:953818–953818. doi: 10.5402/2011/953818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Noncommunicable Diseases. World Health Organization. Updated April 13, 2021. Accessed June 6, 2021. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases [Google Scholar]
- 14.Khot SP, Morgenstern LB. Sleep and Stroke. Stroke. 2019;50(6):1612–1617. doi:doi: 10.1161/STROKEAHA.118.023553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawrence M, Booth J, Mercer S, Crawford E. A Systematic Review of the Benefits of Mindfulness-Based Interventions Following Transient Ischemic Attack and Stroke. International journal of stroke : official journal of the International Stroke Society. Aug 2013;8(6):465–74. doi: 10.1111/ijs.12135 [DOI] [PubMed] [Google Scholar]
- 16.Brunner Frandsen N, Sørensen M, Hyldahl TK, Henriksen RM, Bak S. Smoking Cessation Intervention after Ischemic Stroke or Transient Ischemic Attack. A Randomized Controlled Pilot Trial. Nicotine Tob Res. Apr 2012;14(4):443–7. doi: 10.1093/ntr/ntr233 [DOI] [PubMed] [Google Scholar]
- 17.Chen J, Li S, Zheng K, et al. Impact of Smoking Status on Stroke Recurrence. J Am Heart Assoc. Apr 16 2019;8(8):e011696. doi: 10.1161/jaha.118.011696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu MP, Lin HJ, Weng SF, Ho CH, Wang JJ, Hsu YW. Insomnia Subtypes and the Subsequent Risks of Stroke: Report from a Nationally Representative Cohort. Stroke. May 2014;45(5):1349–54. doi: 10.1161/strokeaha.113.003675 [DOI] [PubMed] [Google Scholar]
- 19.Yu Q, Wu Y, Jin Q, Chen Y, Lin Q, Liu X. Development and Internal Validation of a Multivariable Prediction Model for 6-Year Risk of Stroke: A Cohort Study in Middle-Aged and Elderly Chinese Population. BMJ open. Jul 7 2021;11(7):e048734. doi: 10.1136/bmjopen-2021-048734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epstein KA, Viscoli CM, Spence JD, et al. Smoking Cessation and Outcome after Ischemic Stroke or Tia. Neurology. Oct 17 2017;89(16):1723–1729. doi: 10.1212/wnl.0000000000004524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leys D, Hénon H, Mackowiak-Cordoliani M-A, Pasquier F. Poststroke Dementia. The Lancet Neurology. 2005/November/01/ 2005;4(11):752–759. doi: 10.1016/S1474-4422(05)70221-0 [DOI] [PubMed] [Google Scholar]
- 22.Duncan F, Kutlubaev MA, Dennis MS, Greig C, Mead GE. Fatigue after Stroke: A Systematic Review of Associations with Impaired Physical Fitness. International Journal of Stroke. 2012;7(2):157–162. doi: 10.1111/j.1747-4949.2011.00741.x [DOI] [PubMed] [Google Scholar]
- 23.Bigford G, Nash MS. Nutritional Health Considerations for Persons with Spinal Cord Injury. Top Spinal Cord Inj Rehabil. Summer 2017;23(3):188–206. doi: 10.1310/sci2303-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Y, He Y, DeVivo MJ. Changing Demographics and Injury Profile of New Traumatic Spinal Cord Injuries in the United States, 1972-2014. Arch Phys Med Rehabil. Oct 2016;97(10):1610–9. doi: 10.1016/j.apmr.2016.03.017 [DOI] [PubMed] [Google Scholar]
- 25.Nash MS, Mendez AJ. A Guideline-Driven Assessment of Need for Cardiovascular Disease Risk Intervention in Persons with Chronic Paraplegia. Arch Phys Med Rehabil. Jun 2007;88(6):751–7. doi: 10.1016/j.apmr.2007.02.031 [DOI] [PubMed] [Google Scholar]
- 26.Vives Alvarado JR, Felix ER, Gater DR Jr. Upper Extremity Overuse Injuries and Obesity after Spinal Cord Injury. Top Spinal Cord Inj Rehabil. 2021;27(1):68–74. doi: 10.46292/sci20-00061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kenneweg KA, Welch MC, Welch PJ. A 9-Year Retrospective Evaluation of 102 Pressure Ulcer Reconstructions. J Wound Care. Sep 1 2020;29(Sup9a):S48–s56. doi: 10.12968/jowc.2020.29.Sup9a.S48 [DOI] [PubMed] [Google Scholar]
- 28.Cao Y, DiPiro N, Krause JS. Association of Secondary Health Conditions with Future Chronic Health Conditions among Persons with Traumatic Spinal Cord Injury. Top Spinal Cord Inj Rehabil. 2020;26(4):283–289. doi: 10.46292/sci20-00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giannoccaro MP, Moghadam KK, Pizza F, et al. Sleep Disorders in Patients with Spinal Cord Injury. Sleep Med Rev. Dec 2013;17(6):399–409. doi: 10.1016/j.smrv.2012.12.005 [DOI] [PubMed] [Google Scholar]
- 30.Sivandzade F, Alqahtani F, Cucullo L. Traumatic Brain Injury and Blood-Brain Barrier (Bbb): Underlying Pathophysiological Mechanisms and the Influence of Cigarette Smoking as a Premorbid Condition. Int J Mol Sci. Apr 14 2020;21(8)doi: 10.3390/ijms21082721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seno S, Tomura S, Ono K, Tanaka Y, Ikeuchi H, Saitoh D. Poor Prognostic Factors in Elderly Patients Aged 75 Years Old or Older with Mild Traumatic Brain Injury. J Clin Neurosci. Sep 2019;67:124–128. doi: 10.1016/j.jocn.2019.06.007 [DOI] [PubMed] [Google Scholar]
- 32.Stevens DJ, Alghwiri A, Appleton SL, et al. Should We Lose Sleep over Sleep Disturbances after Sports-Related Concussion? A Scoping Review of the Literature. The Journal of head trauma rehabilitation. Jun 15 2021;doi: 10.1097/htr.0000000000000701 [DOI] [PubMed] [Google Scholar]
- 33.Wilson T, Wisborg T, Vindenes V, Jamt RG, Furuhaugen H, Bogstrand ST. Psychoactive Substances Have Major Impact on Injuries in Rural Arctic Norway - a Prospective Observational Study. Acta Anaesthesiol Scand. Jul 2021;65(6):824–833. doi: 10.1111/aas.13807 [DOI] [PubMed] [Google Scholar]
- 34.Ayton D, Pritchard E, Tsindos T. Acquired Brain Injury in the Context of Family Violence: A Systematic Scoping Review of Incidence, Prevalence, and Contributing Factors. Trauma, violence & abuse. Jan 2021;22(1):3–17. doi: 10.1177/1524838018821951 [DOI] [PubMed] [Google Scholar]
- 35.Sadeghi Bahmani D, Razazian N, Farnia V, Alikhani M, Tatari F, Brand S. Compared to an Active Control Condition, in Persons with Multiple Sclerosis Two Different Types of Exercise Training Improved Sleep and Depression, but Not Fatigue, Paresthesia, and Intolerance of Uncertainty. Mult Scler Relat Disord. Nov 2019;36:101356. doi: 10.1016/j.msard.2019.07.032 [DOI] [PubMed] [Google Scholar]
- 36.Jakimovski D, Weinstock-Guttman B, Gandhi S, et al. Dietary and Lifestyle Factors in Multiple Sclerosis Progression: Results from a 5-Year Longitudinal Mri Study. J Neurol. Apr 2019;266(4):866–875. doi: 10.1007/s00415-019-09208-0 [DOI] [PubMed] [Google Scholar]
- 37.Degelman ML, Herman KM. Smoking and Multiple Sclerosis: A Systematic Review and Meta-Analysis Using the Bradford Hill Criteria for Causation. Mult Scler Relat Disord. Oct 2017;17:207–216. doi: 10.1016/j.msard.2017.07.020 [DOI] [PubMed] [Google Scholar]
- 38.Tanasescu R, Constantinescu CS, Tench CR, Manouchehrinia A. Smoking Cessation and the Reduction of Disability Progression in Multiple Sclerosis: A Cohort Study. Nicotine Tob Res. Apr 2 2018;20(5):589–595. doi: 10.1093/ntr/ntx084 [DOI] [PubMed] [Google Scholar]
- 39.Advocat J, Enticott J, Vandenberg B, Hassed C, Hester J, Russell G. The Effects of a Mindfulness-Based Lifestyle Program for Adults with Parkinson’s Disease: A Mixed Methods, Wait List Controlled Randomised Control Study. BMC Neurol. Sep 8 2016;16:166. doi: 10.1186/s12883-016-0685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rafferty MR, Schmidt PN, Luo ST, et al. Regular Exercise, Quality of Life, and Mobility in Parkinson’s Disease: A Longitudinal Analysis of National Parkinson Foundation Quality Improvement Initiative Data. Journal of Parkinson’s Disease 2017;7(1):193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Belvisi D, Pellicciari R, Fabbrini G, Tinazzi M, Berardelli A, Defazio G. Modifiable Risk and Protective Factors in Disease Development, Progression and Clinical Subtypes of Parkinson’s Disease: What Do Prospective Studies Suggest? Neurobiol Dis. Feb 2020;134:104671. doi: 10.1016/j.nbd.2019.104671 [DOI] [PubMed] [Google Scholar]
- 42.van Nimwegen M, Speelman AD, Hofman-van Rossum EJ, et al. Physical Inactivity in Parkinson’s Disease. J Neurol. Dec 2011;258(12):2214–21. doi: 10.1007/s00415-011-6097-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gagnon JF, Bédard MA, Fantini ML, et al. Rem Sleep Behavior Disorder and Rem Sleep without Atonia in Parkinson’s Disease. Neurology. Aug 27 2002;59(4):585–9. doi: 10.1212/wnl.59.4.585 [DOI] [PubMed] [Google Scholar]
- 44.Nagano T, Kakuma T, Umezu Y, Yanagawa T. Nutritional Status and Activities of Daily Living in Patients with Parkinson’s Disease. PLoS One. 2021;16(2):e0246329. doi: 10.1371/journal.pone.0246329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Academy of Neurologic Physical Therapy. Strategic Plan 2018-2022. Academy of Neurologic Physical Therapy. Accessed January 20, 2021. https://www.neuropt.org/about-us/strategic-plan-2018-2020 [Google Scholar]
- 46.Lein DH Jr., Clark D, Graham C, Perez P, Morris D. A Model to Integrate Health Promotion and Wellness in Physical Therapist Practice: Development and Validationpromoting Health and Wellness: Implications for Physical Therapist Practice. Phys Ther. Dec 1 2017;97(12):1169–1181. doi: 10.1093/ptj/pzx090 [DOI] [PubMed] [Google Scholar]
- 47.Principles of Community Engagement. (Centers for Disease Control and Prevention and the Agency for Toxic Substances and Disease Registry) 21–23 (2011).
- 48.Lowe A, Littlewood C, McLean S. Understanding Physical Activity Promotion in Physiotherapy Practice: A Qualitative Study. Musculoskelet Sci Pract. Jun 2018;35:1–7. doi: 10.1016/j.msksp.2018.01.009 [DOI] [PubMed] [Google Scholar]
- 49.Rimmer JH, Henley KY. Building the Crossroad between Inpatient/Outpatient Rehabilitation and Lifelong Community-Based Fitness for People with Neurologic Disability. J Neurol Phys Ther. Jun 2013;37(2):72–7. doi: 10.1097/NPT.0b013e318291bbf6 [DOI] [PubMed] [Google Scholar]
- 50.Bezner JR, Lloyd LK, Crixell SH, Burke TJ. The Health Care Provider’s Role in Supporting Positive Health Behavior Change: Developing an Effective and Supportive Communication Approach. Medical Research Archives. 2017;5(9) [Google Scholar]
- 51.Office of Disease Prevention and Health Promotion. Social Determinants of Health. U.S. Department of Health and Human Services. Accessed February 26, 2021. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health [Google Scholar]
- 52.Graham ID, Logan J, Harrison MB, et al. Lost in Knowledge Translation: Time for a Map? J Contin Educ Health Prof Winter 2006;26(1):13–24. doi: 10.1002/chp.47 [DOI] [PubMed] [Google Scholar]
- 53.American Physical Therapy Association. Physical Therapists’ Role in Prevention, Wellness, Fitness, Health Promotion, and Management of Disease and Disability Hod P06-19-27-12 [Amended: Hod P06-16-06-05; Initial: Hod P06-15-23-15] American Physical Therapy Association House of Delegates. Updated Sept 20, 2019. Accessed Feb 2, 2021. https://www.apta.org/apta-and-you/leadership-and-governance/policies/association-role-advocacy [Google Scholar]
- 54.American Physical Therapy Association. Health Priorities for Populations and Individuals Hod P06-19-41-15 [Initial Hod P06-15-20-11]. American Physical Therapy Association House of Delegates. Updated Sept 20, 2019. Accessed Feb 2, 2021. https://www.apta.org/apta-and-you/leadership-and-governance/policies/health-priorities-populations-individuals [Google Scholar]
- 55.Institute for Work & Health. Primary, Secondary and Tertiary Prevention. Institute for Work & Health. Accessed January 20, 2021. https://www.iwh.on.ca/what-researchers-mean-by/primary-secondary-and-tertiary-prevention [Google Scholar]
- 56.American Physical Therapy Association. Annual Physical Therapy Visit. American Physical Therapy Association. Accessed Feb 2, 2021. https://www.apta.org/patient-care/interventions/annual-checkup [Google Scholar]
- 57.American Physical Therapy Association. 2021-2022 Public Policy Priorities. Accessed June 7, 2021. https://www.apta.org/siteassets/advocacy/apta-public-policy-priorities.pdf
- 58.Academy of Neurologic Physical Therapy. Parkinson’s Disease Evaluation Database to Guide Effectiveness (Pd-Edge). Updated 2014. Accessed October 27, 2017, http://www.neuropt.org/professional-resources/neurology-section-outcome-measures-recommendations/parkinson-disease
- 59.Academy of Neurologic Physical Therapy Spinal Cord Injury Special Interest Group and Health Promotion and Wellness Task Force/Committee. Bridging the Gap between Physical Therapy and Lifelong Physical Activity and Exercise in People with Neurologic Conditions: A Toolkit for Physical Therapists and Physical Therapist Assistants. Academy of Neurologic Physical Therapy. Updated 2021. Accessed June 7, 2021. https://neuropt.org/docs/default-source/health-promotion-and-wellness-committee-docs/bridging-the-gap-neuro-pt-physical-activity-toolkit_full-version-2020_.pdf?sfvrsn=b0265f43_2 [Google Scholar]
- 60.Academy of Neurologic Physical Therapy. Health Promotion and Wellness Resources. Academy of Neurologic Physical Therapy. Accessed May 30, 2020. http://neuropt.org/practice-resources/health-promotion-and-wellness [Google Scholar]
- 61.Morris DM, Kitchin EM, Clark DE. Strategies for Optimizing Nutrition and Weight Reduction in Physical Therapy Practice: The Evidence. Physiother Theory Pract. Jul 2009;25(5-6):408–23. doi: 10.1080/09593980902835369 [DOI] [PubMed] [Google Scholar]
- 62.Siengsukon CF, Al-dughmi M, Stevens S. Sleep Health Promotion: Practical Information for Physical Therapists. Physical therapy. 2017;97(8):826–836. [DOI] [PubMed] [Google Scholar]
- 63.Marshall RS, Laures-Gore J, Love K. Brief Mindfulness Meditation Group Training in Aphasia: Exploring Attention, Language and Psychophysiological Outcomes. International journal of language & communication disorders. Jan 2018;53(1):40–54. doi: 10.1111/1460-6984.12325 [DOI] [PubMed] [Google Scholar]
- 64.Ghielen I, Rutten S, Boeschoten RE, et al. The Effects of Cognitive Behavioral and Mindfulness-Based Therapies on Psychological Distress in Patients with Multiple Sclerosis, Parkinson’s Disease and Huntington’s Disease: Two Meta-Analyses. J Psychosom Res. Jul 2019;122:43–51. doi: 10.1016/j.jpsychores.2019.05.001 [DOI] [PubMed] [Google Scholar]
- 65.Herring MP, Fleming KM, Hayes SP, Motl RW, Coote SB. Moderators of Exercise Effects on Depressive Symptoms in Multiple Sclerosis: A Meta-Regression. American journal of preventive medicine. Oct 2017;53(4):508–518. doi: 10.1016/j.amepre.2017.04.011 [DOI] [PubMed] [Google Scholar]
- 66.Wu PL, Lee M, Huang TT. Effectiveness of Physical Activity on Patients with Depression and Parkinson’s Disease: A Systematic Review. PLoS One. 2017;12(7):e0181515. doi: 10.1371/journal.pone.0181515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mulroy SJ, Hatchett PE, Eberly VJ, et al. Objective and Self-Reported Physical Activity Measures and Their Association with Depression and Satisfaction with Life in Persons with Spinal Cord Injury. Arch Phys Med Rehabil. Oct 2016;97(10):1714–20. doi: 10.1016/j.apmr.2016.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bodner ME, Dean E. Advice as a Smoking Cessation Strategy: A Systematic Review and Implications for Physical Therapists. Physiother Theory Pract. Jul 2009;25(5-6):369–407. doi: 10.1080/09593980903011887 [DOI] [PubMed] [Google Scholar]
- 69.Haasova M, Warren FC, Ussher M, et al. The Acute Effects of Physical Activity on Cigarette Cravings: Systematic Review and Meta-Analysis with Individual Participant Data. Addiction. Jan 2013;108(1):26–37. doi: 10.1111/j.1360-0443.2012.04034.x [DOI] [PubMed] [Google Scholar]
- 70.Cosano G, Giangreco M, Ussai S, et al. Polypharmacy and the Use of Medications in Inpatients with Acquired Brain Injury During Post-Acute Rehabilitation: A Cross-Sectional Study. Brain injury. 2016;30(3):353–362. [DOI] [PubMed] [Google Scholar]
- 71.Kitzman P, Cecil D, Kolpek JH. The Risks of Polypharmacy Following Spinal Cord Injury. The journal of spinal cord medicine. 2017;40(2):147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hughes K, Bellis MA, Jones L, et al. Prevalence and Risk of Violence against Adults with Disabilities: A Systematic Review and Meta-Analysis of Observational Studies. Lancet. Apr 28 2012;379(9826):1621–9. doi: 10.1016/s0140-6736(11)61851-5 [DOI] [PubMed] [Google Scholar]
- 73.Lund EM. Community-Based Services and Interventions for Adults with Disabilities Who Have Experienced Interpersonal Violence: A Review of the Literature. Trauma, violence & abuse. Oct 2011;12(4):171–82. doi: 10.1177/1524838011416377 [DOI] [PubMed] [Google Scholar]
- 74.Copay AG, Subach BR, Glassman SD, Polly DW, Schuler TC. Understanding the Minimum Clinically Important Difference: A Review of Concepts and Methods. Spine J. 2007 Sep-Oct 2007;7(5):541–6. doi: 10.1016/j.spinee.2007.01.008 [DOI] [PubMed] [Google Scholar]
- 75.de Almeida AA, Gomes da Silva S, Fernandes J, et al. Differential Effects of Exercise Intensities in Hippocampal Bdnf, Inflammatory Cytokines and Cell Proliferation in Rats During the Postnatal Brain Development. Neurosci Lett. Oct 2013;553:1–6. doi: 10.1016/j.neulet.2013.08.015 [DOI] [PubMed] [Google Scholar]
- 76.Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of Standardized Outcome Measures in Physical Therapist Practice: Perceptions and Applications. Physical therapy. 2009;89(2):125–135. [DOI] [PubMed] [Google Scholar]
- 77.Yeomans SG, Yeomans SG. The Clinical Application of Outcomes Assessment. Appleton & Lange; Stamford, CT; 2000. [Google Scholar]
- 78.Golightly YM, Allen KD, Ambrose KR, et al. Physical Activity as a Vital Sign: A Systematic Review. Prev Chronic Dis. Nov 30 2017;14:E123. doi: 10.5888/pcd14.170030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Godin G, Shephard RJ. A Simple Method to Assess Exercise Behavior in the Community. Can J Appl Sport Sci. Sep 1985;10(3):141–6. [PubMed] [Google Scholar]
- 80.Dierckx K, Deveugele M, Roosen P, Devisch I. Implementation of Shared Decision Making in Physical Therapy: Observed Level of Involvement and Patient Preference. Phys Ther. Oct 2013;93(10):1321–30. doi: 10.2522/ptj.20120286 [DOI] [PubMed] [Google Scholar]
- 81.Elwyn G, Lloyd A, Joseph-Williams N, et al. Option Grids: Shared Decision Making Made Easier. Patient Educ Couns. Feb 2013;90(2):207–12. doi: 10.1016/j.pec.2012.06.036 [DOI] [PubMed] [Google Scholar]
- 82.Scheel-Sailer A, Post MW, Michel F, Weidmann-Hugle T, Baumann Holzle R. Patients’ Views on Their Decision Making During Inpatient Rehabilitation after Newly Acquired Spinal Cord Injury-a Qualitative Interview-Based Study. Health expectations : an international journal of public participation in health care and health policy. Oct 2017;20(5):1133–1142. doi: 10.1111/hex.12559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zizzo N, Bell E, Lafontaine AL, Racine E. Examining Chronic Care Patient Preferences for Involvement in Health-Care Decision Making: The Case of Parkinson’s Disease Patients in a Patient-Centred Clinic. Health expectations : an international journal of public participation in health care and health policy. Aug 2017;20(4):655–664. doi: 10.1111/hex.12497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Held Bradford E, Finlayson M, White Gorman A, Wagner J. Maximizing Gait and Balance: Behaviors and Decision-Making Processes of Persons with Multiple Sclerosis and Physical Therapists. Disability and Rehabilitation. 2017:1–12. doi: 10.1080/09638288.2017.1283448 [DOI] [PubMed] [Google Scholar]
- 85.Joyce M, Larson C, Tappan R. Bridging the Gap between Physical Therapy and Long-Term Physical Activity and Training in People with Spinal Cord Injury (Sci): Recommendations from the Sci Special Interest Group. Academy of Neurologic Physical Therapy Spinal Cord Special Interest Group. Accessed May 30, 2020. http://neuropt.org/docs/default-source/sci-sig/white-paper/healthwellnesssci_final.pdf?sfvrsn=4 [Google Scholar]
- 86.Magnusson DM, Rethorn ZD, Bradford EH, et al. Population Health, Prevention, Health Promotion, and Wellness Competencies in Physical Therapist Professional Education: Results of a Modified Delphi Study. Phys Ther. Apr 13 2020;doi: 10.1093/ptj/pzaa056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rethorn ZD, Maxwell JL, Bezner JR, et al. What Are Dpt Program Practices and Attitudes Related to Population Health, Prevention, Health Promotion, and Wellness? Results of a National Survey. Phys Ther. Jan 4 2021;101(1)doi: 10.1093/ptj/pzaa178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rafferty MR, MacDonald J, Byskosh A, et al. Using Implementation Frameworks to Provide Proactive Physical Therapy for People with Parkinson Disease: Case Report. Phys Ther. Dec 16 2019;99(12):1644–1655. doi: 10.1093/ptj/pzz129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Center for Medicare Advocacy. The Jimmo Implementation Council. Accessed May 24, 2016. http://www.medicareadvocacy.org/jimmo-implementation-council/
- 90.Rose DK, Schafer J, Conroy C. Extending the Continuum of Care Poststroke: Creating a Partnership to Provide a Community-Based Wellness Program. J Neurol Phys Ther. Jun 2013;37(2):78–84. doi: 10.1097/NPT.0b013e3182941c37 [DOI] [PubMed] [Google Scholar]
- 91.Rimmer JH. Getting Beyond the Plateau: Bridging the Gap between Rehabilition and Community-Based Exercise. Physical Medicine and Rehabilitation. 2012;4:857–861. [DOI] [PubMed] [Google Scholar]
- 92.Richardson J, Tang A, Guyatt G, et al. Fit for Function: Study Protocol for a Randomized Controlled Trial. Trials. Jan 15 2018;19(1):39. doi: 10.1186/s13063-017-2416-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ploughman M, Shears J, Harris C, et al. Effectiveness of a Novel Community Exercise Transition Program for People with Moderate to Severe Neurological Disabilities. NeuroRehabilitation. 2014;35(1):105–12. doi: 10.3233/nre-141090 [DOI] [PubMed] [Google Scholar]
- 94.Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, et al. Evidence-Based Scientific Exercise Guidelines for Adults with Spinal Cord Injury: An Update and a New Guideline. Spinal cord. 2018/April/01 2018;56(4):308–321. doi: 10.1038/s41393-017-0017-3 [DOI] [PubMed] [Google Scholar]
- 95.Garshick E, Mulroy S, Graves DE, Greenwald K, Horton JA, Morse LR. Active Lifestyle Is Associated with Reduced Dyspnea and Greater Life Satisfaction in Spinal Cord Injury. Arch Phys Med Rehabil. Oct 2016;97(10):1721–7. doi: 10.1016/j.apmr.2016.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wise EK, Hoffman JM, Powell JM, Bombardier CH, Bell KR. Benefits of Exercise Maintenance after Traumatic Brain Injury. Arch Phys Med Rehabil. Aug 2012;93(8):1319–23. doi: 10.1016/j.apmr.2012.05.009 [DOI] [PubMed] [Google Scholar]
- 97.Hassett L, Moseley AM, Harmer AR. Fitness Training for Cardiorespiratory Conditioning after Traumatic Brain Injury. Cochrane Database Syst Rev Dec 29 2017;12:Cd006123. doi: 10.1002/14651858.CD006123.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Billinger SA, Arena R, Bernhardt J, et al. Physical Activity and Exercise Recommendations for Stroke Survivors: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke. Aug 2014;45(8):2532–53. doi: 10.1161/STR.0000000000000022 [DOI] [PubMed] [Google Scholar]
- 99.Ezeugwu VE, Manns PJ. Sleep Duration, Sedentary Behavior, Physical Activity, and Quality of Life after Inpatient Stroke Rehabilitation. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. Sep 2017;26(9):2004–2012. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.009 [DOI] [PubMed] [Google Scholar]
- 100.Crozier J, Roig M, Eng JJ, et al. High-Intensity Interval Training after Stroke: An Opportunity to Promote Functional Recovery, Cardiovascular Health, and Neuroplasticity. Neurorehabil Neural Repair. Jun 2018;32(6-7):543–556. doi: 10.1177/1545968318766663 [DOI] [PubMed] [Google Scholar]
- 101.Venasse M, Edwards T, Pilutti LA. Exploring Wellness Interventions in Progressive Multiple Sclerosis: An Evidence-Based Review. Current treatment options in neurology. Apr 10 2018;20(5):13. doi: 10.1007/s11940-018-0497-2 [DOI] [PubMed] [Google Scholar]
- 102.Moss BP, Rensel MR, Hersh CM. Wellness and the Role of Comorbidities in Multiple Sclerosis. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics. Oct 2017;14(4):999–1017. doi: 10.1007/s13311-017-0563-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Edwards T, Pilutti LA. The Effect of Exercise Training in Adults with Multiple Sclerosis with Severe Mobility Disability: A Systematic Review and Future Research Directions. Mult Scler Relat Disord. Aug 2017;16:31–39. doi: 10.1016/j.msard.2017.06.003 [DOI] [PubMed] [Google Scholar]
- 104.Latimer-Cheung AE, Martin Ginis KA, Hicks AL, et al. Development of Evidence-Informed Physical Activity Guidelines for Adults with Multiple Sclerosis. Arch Phys Med Rehabil. Sep 2013;94(9):1829–1836.e7. doi: 10.1016/j.apmr.2013.05.015 [DOI] [PubMed] [Google Scholar]
- 105.Rabin ML, Stevens-Haas C, Havrilla E, et al. Complementary Therapies for Parkinson’s Disease: What’s Promoted, Rationale, Potential Risks and Benefits. Movement disorders clinical practice. Sep 2015;2(3):205–212. doi: 10.1002/mdc3.12170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Speelman AD, van Nimwegen M, Bloem BR, Munneke M. Evaluation of Implementation of the Parkfit Program: A Multifaceted Intervention Aimed to Promote Physical Activity in Patients with Parkinson’s Disease. Physiotherapy. Jun 2014;100(2):134–41. doi: 10.1016/j.physio.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 107.Schenkman M, Moore CG, Kohrt WM, et al. Effect of High-Intensity Treadmill Exercise on Motor Symptoms in Patients with De Novo Parkinson Disease: A Phase 2 Randomized Clinical Trial. JAMA Neurol. Feb 1 2018;75(2):219–226. doi: 10.1001/jamaneurol.2017.3517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Joseph C, Stromback B, Hagstromer M, Conradsson D. Accelerometry: A Feasible Method to Monitor Physical Activity During Sub-Acute Rehabilitation of Persons with Stroke. Journal of rehabilitation medicine. May 8 2018;50(5):429–434. doi: 10.2340/16501977-2326 [DOI] [PubMed] [Google Scholar]
- 109.Wendel N, Macpherson CE, Webber K, et al. Accuracy of Activity Trackers in Parkinson Disease: Should We Prescribe Them? Phys Ther. Aug 1 2018;98(8):705–714. doi: 10.1093/ptj/pzy054 [DOI] [PubMed] [Google Scholar]
- 110.Ball TJ, Joy EA, Gren LH, Cunningham R, Shaw JM. Predictive Validity of an Adult Physical Activity “Vital Sign” Recorded in Electronic Health Records. J Phys Act Health. Oct 7 2015;doi: 10.1123/jpah.2015-0210 [DOI] [PubMed] [Google Scholar]
- 111.Ball TJ, Joy EA, Gren LH, Shaw JM. Concurrent Validity of a Self-Reported Physical Activity “Vital Sign” Questionnaire with Adult Primary Care Patients. Prev Chronic Dis. 2016;13:E16. doi: 10.5888/pcd13.150228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chastin SF, Culhane B, Dall PM. Comparison of Self-Reported Measure of Sitting Time (Ipaq) with Objective Measurement (Activpal). Physiol Meas. Nov 2014;35(11):2319–28. doi: 10.1088/0967-3334/35/11/2319 [DOI] [PubMed] [Google Scholar]
- 113.Craig CL, Marshall AL, Sjöström M, et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med Sci Sports Exerc. Aug 2003;35(8):1381–95. doi: 10.1249/01.Mss.0000078924.61453.Fb [DOI] [PubMed] [Google Scholar]
- 114.Resnick B, Jenkins LS. Testing the Reliability and Validity of the Self-Efficacy for Exercise Scale. Nursing research. May-Jun 2000;49(3):154–9. doi: 10.1097/00006199-200005000-00007 [DOI] [PubMed] [Google Scholar]
- 115.Kroll T, Kehn M, Ho P-S, Groah S. The Sci Exercise Self-Efficacy Scale (Eses): Development and Psychometric Properties. International Journal of Behavioral Nutrition and Physical Activity. 2007/August/30 2007;4(1):34. doi: 10.1186/1479-5868-4-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Heather N, Rollnick S, Bell AJA. Predictive Validity of the Readiness to Change Questionnaire. 1993;88(12):1667–1677. [DOI] [PubMed] [Google Scholar]
- 117.Paxton AE, Strycker LA, Toobert DJ, Ammerman AS, Glasgow RE. Starting the Conversation Performance of a Brief Dietary Assessment and Intervention Tool for Health Professionals. American journal of preventive medicine. Jan 2011;40(1):67–71. doi: 10.1016/j.amepre.2010.10.009 [DOI] [PubMed] [Google Scholar]
- 118.World Health Organization. Toolkit for Delivering the 5a’s and 5r’s Brief Tobacco Interventions in Primary Care. World Health Organization. Accessed Feb 2, 2021. https://www.who.int/tobacco/publications/smoking_cessation/9789241506953/en/ [Google Scholar]
- 119.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. May 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 120.Chung F, Yegneswaran B, Liao P, et al. Stop Questionnaire: A Tool to Screen Patients for Obstructive Sleep Apnea. Anesthesiology. May 2008;108(5):812–21. doi: 10.1097/ALN.0b013e31816d83e4 [DOI] [PubMed] [Google Scholar]
- 121.Cohen S, Kamarck T, Mermelstein R. A Global Measure of Perceived Stress. Journal of Health and Social Behavior. 1983;24(4):385–396. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 122.Carver CS. You Want to Measure Coping but Your Protocol’s Too Long: Consider the Brief Cope. International journal of behavioral medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- 123.Chew LD, Griffin JM, Partin MR, et al. Validation of Screening Questions for Limited Health Literacy in a Large Va Outpatient Population. Journal of general internal medicine. 2008;23(5):561–566. doi: 10.1007/s11606-008-0520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Marshall SJ, Biddle SJ. The Transtheoretical Model of Behavior Change: A Meta-Analysis of Applications to Physical Activity and Exercise. Ann Behav Med. Fall 2001;23(4):229–46. [DOI] [PubMed] [Google Scholar]
- 125.Prochaska JO, DiClemente CC. Stages and Processes of Self-Change of Smoking: Toward an Integrative Model of Change. J Consult Clin Psychol. Jun 1983;51(3):390–5. [DOI] [PubMed] [Google Scholar]
- 126.Bandura A Health Promotion by Social Cognitive Means. Health Educ Behav. Apr 2004;31(2):143–64. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 127.Glanz K, Rimer BK, Viswanath K. Health Behavior: Theory, Research, and Practice. 5th Edition ed. Jossey-Bass; 2015. [Google Scholar]
- 128.Saccone D Ymca’s Moving for Better Balance: Concepts of Collaboration. presented at: International Council on Active Aging Annual Meeting 2016; [Google Scholar]
- 129.Wallace JI, Buchner DM, Grothaus L, et al. Implementation and Effectiveness of a Community-Based Health Promotion Program for Older Adults. The Journals of Gerontology: Series A. 1998;53A(4):M301–M306. doi: 10.1093/gerona/53A.4.M301 [DOI] [PubMed] [Google Scholar]
- 130.Basia B, Anne S-C, Elizabeth AP, Barbara W, Susan JS, James PL. The Effects of a Community-Based Exercise Program on Function and Health in Older Adults: The Enhancefitness Program. Journal of Applied Gerontology. 2006/August/01 2006;25(4):291–306. doi: 10.1177/0733464806290934 [DOI] [Google Scholar]
- 131.APTA Geriatrics. Partnerships - National Council on Aging. Academy of Geriatric Physical Therapy. Accessed May 30, 2020. https://geriatricspt.org/consumers/partnerships%20-%20National%20Council%20on%20Aging.cfm
- 132.Rethorn ZD, Cook C, Reneker JC. Social Determinants of Health: If You Aren’t Measuring Them, You Aren’t Seeing the Big Picture. J Orthop Sports Phys Ther. Dec 2019;49(12):872–874. doi: 10.2519/jospt.2019.0613 [DOI] [PubMed] [Google Scholar]
- 133.Sebelski CA, Hoogenboom BJ, Hayes AM, Held Bradford E, Wainwright SF, Huhn K. The Intersection of Movement and Clinical Reasoning: Embodying “Body as a Teacher” to Advance the Profession and Practice. Physical Therapy. 2019;100(2):201–204. doi: 10.1093/ptj/pzz137 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


