Abstract
Background
Missed appointments diminish the continuity and quality of care.
Objective
To determine whether missing scheduled appointments is associated with characteristics of the populations in places where patients reside.
Design
Retrospective cross-sectional study using data extracted from electronic health records linked to population descriptors for each patient’s census tract of residence.
Patients
A total of 58,981 patients ≥18 years of age with 275,682 scheduled appointments during 2014–2015 at a multispecialty outpatient practice.
Main Measures
We used multinomial generalized linear mixed models to examine associations between the outcomes of scheduled appointments (arrived, canceled, or missed) and selected characteristics of the populations in patients’ census tracts of residence (racial/ethnic segregation based on population composition, levels of poverty, violent crime, and perceived safety and social capital), controlling for patients’ age, gender, type of insurance, and type of clinic service.
Key Results
Overall, 17.5% of appointments were missed. For appointments among patients residing in census tracts in the highest versus lowest quartile for each population metric, adjusted odds ratios (aORs) for missed appointments were 1.27 (CI 1.19, 1.35) for the rate of violent crime, 1.27 (CI 1.20, 1.34) for the proportion Hispanic, 1.19 (CI 1.12, 1.27) for the proportion living in poverty, 1.13 (CI 1.05, 1.20) for the proportion of the census tract population that was Black, and 1.06 (CI 1.01, 1.11 for perceived neighborhood safety.
Conclusions
Characteristics of the places where patients reside are associated with missing scheduled appointments, including high levels of racial/ethnic segregation, poverty, and violent crime and low levels of perceived neighborhood safety. As such, targeting efforts to improve access for patients living in such neighborhoods will be particularly important to address underlying social determinants of access to health care.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-021-06935-x.
KEY WORDS: missed appointment, social determinants, neighborhood characteristics
INTRODUCTION
Missed patient appointments decrease continuity of care, practice revenue, provider productivity, quality of care, and achievement of clinical performance targets.1–6 Missed appointments are also associated with increased use of emergency departments, increased health-care costs, decreased patient satisfaction, difficulties in arriving at optimal staffing levels, and worse clinical outcomes.2,7 A growing body of research aims to improve prediction of patient characteristics and clinic procedures associated with missing appointments, in order to inform interventions that might improve appointment keeping. In a systematic review of studies that examined the prediction of missed appointment rates in primary and specialty care settings, among 32 reports published between 2010 and 2020, the median of observed proportions of scheduled appointments that were missed was 18% and ranged from 6 to 45%.8 That same review identified nearly 40 features related to patient demographics, medical history, appointment details, and past appointment attendance that have been studied.8 Long intervals between the times that appointments are requested and scheduled and patients’ prior history of missing appointments are among the strongest predictors of missed appointments.9–11 Other predictors include young age, being uninsured or having public as opposed to private insurance, low socioeconomic status, long distances between places of residence and clinics, and being of Black/African American or Hispanic race/ethnicity.12–14
Among factors associated with missed appointments that have been catalogued in recent reviews, including predictive modeling studies, the characteristics of neighborhoods where patients reside have not been listed,8,9 despite growing attention to associations between neighborhood attributes and health. Residential segregation by race and ethnicity and related inequities in levels of poverty, perceived neighborhood safety, social cohesion, and violence are associated with heightened stress and risks for chronic diseases and mental health problems, including depression and related symptoms.15 Given these effects, we posit that by incorporating neighborhood characteristics into assessments of risks for missing appointments, we can add an additional element to the predictive modeling approach. This consideration parallels growing national attention to social determinants of health as part of efforts to improve the quality and outcomes of health care, including efforts to expand screening for such determinants and standardize their recording in electronic health records.16,17 Social determinants of health cluster in neighborhoods,15 and associations between neighborhood characteristics and health, have been observed for multiple conditions where outcomes depend heavily on patient adherence to health-care recommendations, such as diabetes and hypertension control18,19 and colorectal cancer screening.20 It follows that neighborhood characteristics might also affect adherence to appointment schedules.
METHODS
We extracted patient-level data from the practice management system for a multispecialty adult practice at the Drexel University College of Medicine for 97,152 patients with scheduled appointments at internal medicine and related specialty clinics from January 1, 2014, through December 31, 2015. For each patient, we extracted data on self-reported race/ethnicity (non-Hispanic White, non-Hispanic Black/African American, non-Hispanic Asian [subsequently referred to as White, Black, or Asian, respectively, for brevity], Hispanic, other/unknown); age as of January 1, 2014; gender (male, female, in transition, unspecified); type of health insurance (private, Medicare, Medicare Advantage, Medicaid, Medicaid mental health coverage [administered separately from general Medicaid coverage in Pennsylvania], uninsured/self-insured/unspecified); and address of residence. For each scheduled appointment, we extracted data on the clinic service for which the appointment was made, including cardiology, family medicine, internal medicine, dermatology, endocrinology, hematology/oncology, infectious diseases, nephrology, neurology, pulmonary, radiation oncology, rheumatology, gastroenterology/hepatology, sleep medicine, sports medicine, travel medicine, or unspecified. We classified appointment outcomes into four categories: patient arrived for the scheduled appointment (arrived), patient canceled the appointment prior to the scheduled date (canceled), clinic staff canceled the appointment (staff- canceled), or patient did not arrive for a scheduled appointment or canceled on the scheduled date (missed).
We used ArcGIS 10.5 (Esri) with the Business Analyst 2016 Composite Address Locator to automatically geocode patient addresses.21 Among 69,054 patients with Philadelphia addresses, addresses were geocoded and census tracts of residence were assigned for 68,156 (98.7%), among whom > 90% of addresses were geocoded automatically and the remainder geocoded manually. Compared to those for whom the address was geocoded, patients whose addresses were not geocoded were less likely to be White (20.2% vs. 29.7%, p < 0.001), more likely to be covered by Medicaid or be uninsured (37.3% vs. 30.1%, p < 0.0001), but did not differ significantly by gender. Records available to us did not include information on housing status. It is possible that some patients with insecure housing provided a temporary address that was geocoded and that others were among those without a geocoded address.
Because of our interest in whether patients arrived, canceled, or missed their appointments, we excluded those whose appointments were canceled by clinic staff. Given our interest in adult internal medicine and related services, we excluded appointments among those < 18 years of age. Because of the small number of patients whose gender was recorded as “in transition” or unspecified, we excluded those whose gender was not listed as male or female. To focus on adult patients with typical patterns of periodic or episodic health-care use, we excluded those with > 20 scheduled appointments during the study period, such as patients receiving weekly treatments for extended periods. This cut-point was based on the bi-modal distribution of numbers of scheduled appointments per patient. The 4480 patients excluded for this reason represented 7.1% of patients prior to this exclusion step and had 35.4 scheduled appointments per patient, compared to 4.9 scheduled appointments per patient among remaining patients. Lastly, we excluded 3 scheduled appointments for which the practice management system did not specify the specialty for the scheduled visit. The effect of each of these exclusions on the number of study patients and scheduled appointments is summarized in Table 1. This resulted in a final study population of 58,981 patients with 275,682 scheduled appointments. The median number of scheduled appointments per patient was 3 (interquartile range [IQR], 1–6), and patients with one, 2–5, and 6–20 scheduled appointments accounted for 28.0%, 42.5%, and 29.5% total appointments, respectively.
Table 1.
Numbers of Excluded Patients and Scheduled Appointments
| Excluded | Remaining | |||
|---|---|---|---|---|
| Number of patients | Number of scheduled appointments | Number of patients | Number of scheduled appointments | |
| Philadelphia residents | 69,054 | 474,157 | ||
| Exclusion criteria | ||||
| Unable to geocode place of residence | 898 | 5279 | 68,156 | 468,878 |
| Visits canceled by clinic staff | 673 | 8744 | 67,483 | 460,134 |
| Age < 18 years | 4019 | 11,429 | 63,464 | 448,705 |
| Gender not specified as male or female | 3 | 126 | 63,461 | 448,579 |
| Clinic specialty type not specified | 0 | 3 | 63,461 | 448,576 |
| Patients with > 20 visits during study period | 4480 | 158,724 | 58,981 | 289,852 |
For each patient, we obtained data that described the population living in their census tract of residence using multiple sources collated by the Drexel University Urban Health Collaborative.22 This included the percentages who were Black or Hispanic, measures that correlate strongly with racial/ethnic segregation in Philadelphia and that we considered as a proxy for racial/ethnic segregation. For example, compared to a segregation index that takes into account the racial/ethnic distribution of the population in a census tract and its surrounding tracts (i.e., a census tract with a high proportion of Black residents that is surrounded by census tracts with a high proportion of Black residents would have a high segregation index),23 the Pearson correlation coefficient between the Black segregation index and percentage of the population in the tract that is Black is 0.95; the corresponding correlation for the Hispanic segregation index and Hispanic population proportion is 0.94. Other census tract measures were the percentage living below the federally defined poverty threshold, based on 5-year estimates for 2011–2015 from the American Community Survey;24 and rates of violent crime (homicides, rapes, aggravated assaults, robberies, other assaults) per 10,000 population, as recorded by the Philadelphia Police Department for 2014–2015.25,26 Because perceived neighborhood safety and objectively measured crime rates are generally not correlated,27,28 we considered the percentage of census tract residents who perceived their neighborhoods as safe, derived from the 2012 Southeastern Pennsylvania Household Health Survey as previously described.21,29,30 Perceived neighborhood safety was based on responses to 2 questions: (1) “In the past month, did you not go someplace during the day because you felt you would not be safe?” and (2) “Is there a park or other outdoor space in your neighborhood that you’re comfortable visiting during the day?” Those who responded “no” to the first question and “yes” to the second were classified as perceiving that their neighborhoods were safe; those who responded “yes” to the first question or “no” to the second were classified as not perceiving that their neighborhood was safe. Lastly, we included a measure of perceived social capital (range = 0 to 3), similarly derived from the same survey, based the average of responses to 3 questions scored using a zero (never) to 3 (always) scale: (1) “How likely are people in your neighborhood willing to help their neighbors?” (2) “Most people in my neighborhood can be trusted.” (3) “I feel that I belong and am a part of my neighborhood.” In preliminary analyses, we considered composite measures of social vulnerability but opted to focus on specific rather than summary measures.
With the exception of Table 2, which describes the characteristics of study patients and the census tracts where they resided, our unit of analysis was scheduled appointments. For each scheduled appointment, we considered information about the type of clinic where the appointment was scheduled; the patient’s individual characteristics (age, gender, race/ethnicity, type of health insurance), subsequently labeled as “personal characteristics;” and characteristics of the population in the census tract where the patient resided (levels of racial/ethnic segregation as reflected by racial/ethnic composition, poverty, violent crime, perceived neighborhood safety, perceived neighborhood social capital), subsequently referred to as “census tract characteristics.”
Table 2.
Characteristics of Study Patients and the Census Tracts Where They Resided
| Number of patients | 58,981 |
|---|---|
| Personal characteristics | |
| Female (percentage) | 58.7 |
| Years of age, mean (SD) | 43.6 (17.9) |
| Race/ethnicity (percentage) | |
| Asian | 6.2 |
| Black | 42.6 |
| Hispanic | 7.9 |
| White | 30.7 |
| Other/unknown | 12.6 |
| Insurance (percentage) | |
| Commercial | 48.1 |
| Medicaid | 28.0 |
| Medicare | 9.9 |
| Medicare Advantage | 8.5 |
| Medicaid mental health | 3.4 |
| Uninsured/self-insured/unspecified | 2.0 |
| Number of census tracts | 379 |
| Characteristics of populations in patients’ census tracts of residence:* | |
| Percentage non-Hispanic White, median (IQR) | 25.5 (5.3, 64.0) |
| Percentage Hispanic, median (IQR) | 5.3 (2.7, 10.9) |
| Percentage Black, median (IQR) | 32.5 (9.6, 80.9) |
| Percentage non-Hispanic Asian, median (IQR) | 3.8 (1.0, 9.4) |
| Percentage living below federal poverty level, median (IQR) | 29.0 (15.4, 40.9) |
| Violent crimes per 10,000 population, median (IQR) | 235.6 (135.4, 397.8) |
| Social capital index,† median (IQR) | 1.8 (1.7, 1.9) |
| Percentage who perceived their neighborhood as safe, median (IQR) | 90.6 (82.7, 94.3) |
*Median and interquartile (q1, q3) range (IQR) for census tracts
†0 = lowest social capital, 3 = highest social capital
We first examined univariate associations between appointment outcomes and patient characteristics and census tract characteristics, using chi-square tests. We then constructed a series of multinomial generalized linear mixed (GLM) models to estimate adjusted odds ratios for associations between appointment outcomes and various combinations of patient and census tract characteristics. We attempted to conduct multi-level models by including separate random effects for both patient and census tract, but due to computational limitations, we were unable to successfully run these models. Because the within-person correlation of visits was higher than the between-person correlation within census tract, we chose to include a random effect for patient nested within census tract to best account for the correlation in the final model. In sensitivity analyses, the fixed effects for the neighborhood attributes were similar for models with only a census-tract-level random effect (assuming independence within person) and our final models with the random effect of patient nested in census tract. In our final model, for each scheduled visit we included the patient’s gender (male, female); age group (18–25, 26–50, 51–64, 65–74, 75+); race/ethnicity (White, Black, Asian, Hispanic, other/unknown); clinic type where the appointment was scheduled; and insurance status (private, Medicare, Medicare Advantage, Medicaid, Medicaid mental health, uninsured/self-insured/unspecified), and the census tract characteristics. Census tracts were categorized by quartiles for violent crime rates per 10,000 population; the percentages of the census tract populations that were Black, Hispanic, living in poverty, and perceived their neighborhood as safe; and the average social capital index. Because census tract characteristics had low to moderate correlation with one another (range of correlation coefficients, 0.36–0.53), we included all in the same model. In addition, we examined each census tract characteristic individually in a separate model as a sensitivity test. Additional sensitivity testing included a model that removed the exclusion for patients with > 20 scheduled appointments during the study period.
SAS (v9.4) was used for statistical analyses. All statistical tests are 2-tailed, and odds ratio estimates are shown with 95% confidence intervals. We considered statistical tests to be statistically significant when p values were < 0.05, and we considered odds ratios with CIs that did not include 1.0 to be different from 1.0.
The study was reviewed and approved by the Drexel University Institutional Review Board.
RESULTS
Among the 58,981 Philadelphia residents included in the study population (Table 2), 59% were female, the mean age was 44 years, 43% were Black, and 31% were White. Private insurance was the most common form of health insurance (48%), followed by Medicaid (28%). Members of the study population resided in 379 Philadelphia census tracts, including 376 tracts with 10 or more study residents. Among populations in the census tracts where patients resided, the median percentage of residents who were Black was 32% (interquartile range [IQR], 10–81%), Hispanic 5% (IQR, 3–11%), and living below the federal poverty level 29% (IQR, 15–41%) (Table 2). The median social capital index was 1.8 (IQR, 1.7–1.9), and the median percentage who perceived their neighborhood as safe was 91% (IQR, 83–94%) (Table 2).
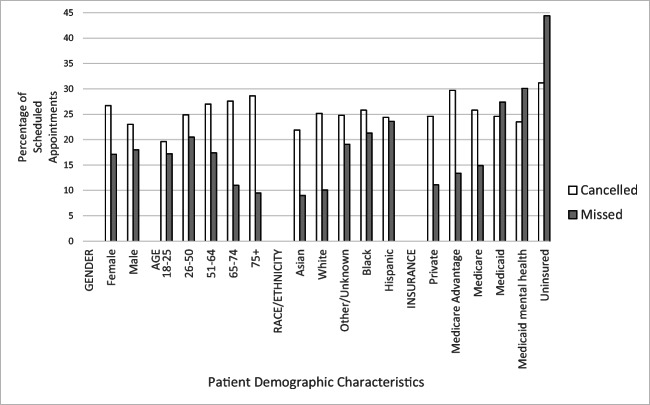
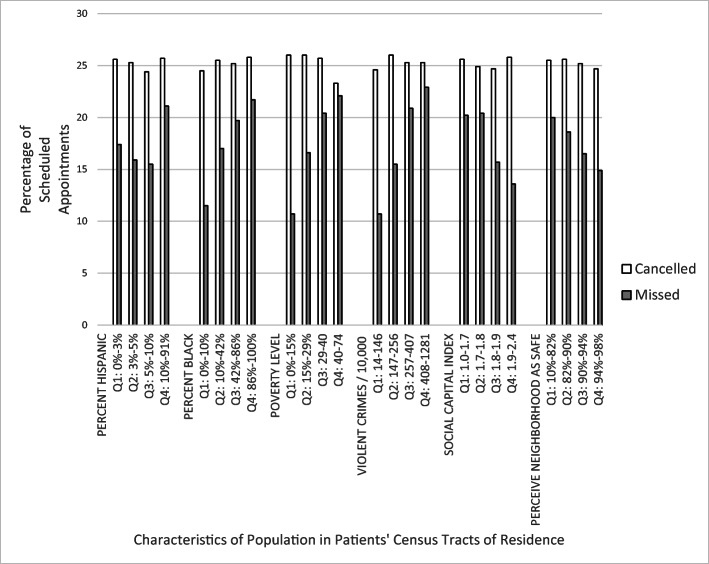
Overall, 17.5% of 275,682 scheduled appointments resulted in a missed appointment, 25.3% in cancelation, and 57.3% in an arrival. In unadjusted univariate comparisons, cancelation rates generally varied less by patient and census tract characteristics than missed appointment rates, Figures 1 and 2, with the exception that cancelation rates increased with increasing age across all age groups while missed appointment rates declined with increasing age among those > 25 years of age (Fig. 1). Missed appointment rates were higher among Black and Hispanic patients and those with other/unknown race/ethnicity than among White or Asian patients and among those insured by Medicaid or uninsured than those covered by private insurance or Medicare (Fig. 1). In examining missed appointment rates by census tract characteristics, missed appointment rates were highest among patients residing in census tracts with the highest proportions of Hispanic and Black residents, the highest proportions of residents living in poverty, the highest rates of violent crime, the lowest levels of perceived social capital, and the lowest proportions of residents who perceived their neighborhoods as safe (Fig. 2).
Figure 1.
Appointment outcomes (canceled or missed) by patient demographic characteristics for 275,682 scheduled appointments among 58,981 patients.
Figure 2.
Appointment outcomes (canceled or missed) by characteristics of populations in patients’ census tracts of residence for 275,682 scheduled appointments among 58,981 patients.
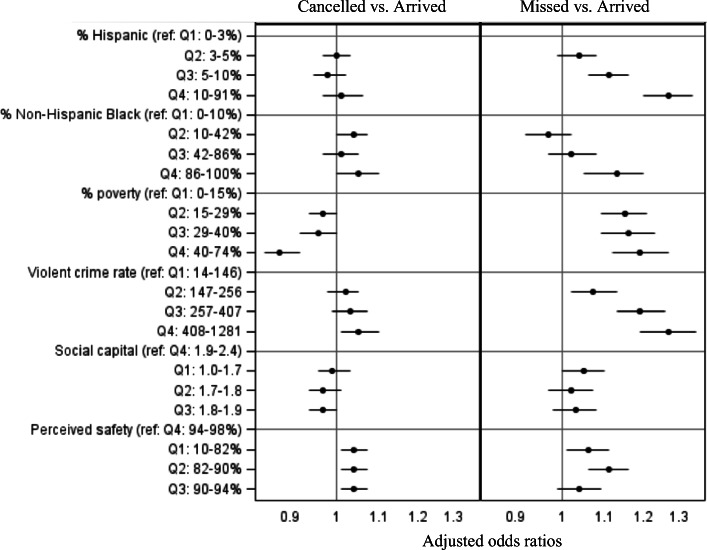
In the final GLM model, which examined clinic type and personal and census tract characteristics simultaneously, patterns of associations between appointment outcomes and patient characteristics generally paralleled those observed in the unadjusted univariate analysis, with the exception that patients 18–25 years of age had the highest odds of missing appointments relative to those 26–50 years of age (aOR = 1.06, 95% CI = 1.01, 1.11) (Supplement Table 1). Appointments among those living in census tracts in the second to fourth quartiles for successively higher levels of violent crime and poverty had successively higher odds of being missed relative to appointments for those living in the lowest quartile census tracts for these indices (Fig. 3 and Supplement Table 1). For appointments among those living in census tracts with different proportions of Black residents, the aOR was significantly > 1.0 only for those living in tracts in the highest versus lowest quartile (Fig. 3 and Supplement Table 1). Appointments among those living in census tracts in the 3rd and 4th highest quartiles for percentages of Hispanic residents had the higher odds for resulting in a missed appointment than those among patients living in tracts in the lowest quartile for percentage of Hispanic residents (Fig. 3 and Supplement Table 1). Adjusted ORs for missed and canceled appointments for all variables in the final model, including clinic type, are available in Supplement Table 1.
Figure 3.
Adjusted odds ratios for attributes of the populations in census tracts where patients with study appointments resided, by quartile, for missed and canceled appointments relative to kept (arrived) appointments.
Final model associations between missed appointments and poverty level, violent crime rates, and perceived neighborhood safety were attenuated relative to associations observed in sensitivity testing that examined each census tract characteristic individually in separate models (Supplement Table 2). The association between missed appointments and perceived neighborhood social capital was statistically significant in the single-variable model (Supplement Table 2) but not for all levels of perceived neighborhood safety in the full model (Fig. 3 and Supplement Table 1). In the single-variable model, the association with the percentage of the census tract population that was Black was statistically significant for the 2nd–4th quartiles relative to the lowest-level quartile (lowest percentage Black), but was attenuated in the full model such that only the highest quartile (highest percent Black) showed a statistically significant difference from the lowest quartile (Supplement Table 2). A model that removed the exclusion for patients with > 20 visits during the study period did not yield substantially different conclusions (Supplement Table 3).
DISCUSSION
Among scheduled appointments for patients receiving care at clinics affiliated with an urban, university health-care system, living in census tracts with higher levels of racial/ethnic segregation, poverty, and violent crime and lower levels of perceived neighborhood safety was associated with missing appointments.
Our findings are consistent with those of prior studies that have correlated residence in racially, and to a lesser extent ethnically, segregated neighborhoods with worse physical and mental health outcomes.31–37 Racial and ethnic residential segregation in the USA reflects the cumulative effects of decades of federal, state, and local policies and law enforcement practices that explicitly or implicitly sought to exclude Black Americans from opportunities in home ownership, which reflected overtly racist positions and institutionalized racism, and which adversely affected opportunities for employment and wealth accumulation.38 The consequences include adverse health effects arising from interacting effects of poverty, violence, and stress.15 Exactly how neighborhood attributes such as segregation, crime, poverty, and perceived safety act to affect whether patients will attend scheduled appointments cannot be assessed from our study. Tung et al. draw upon social deprivation theory to posit that the social environment including racial segregation, demographics, and features of the built environment interact to constrain “health-enabling resources.”39 In all likelihood, census tract population characteristics associated with missed appointments present or reflect stressors that can disrupt patients’ daily routines and interfere with, distract from, or complicate appointment keeping. This is consistent with prior observations that living in racially segregated neighborhoods in Philadelphia is associated with not being up to date with recommended colorectal cancer screening, which requires special scheduling and preparation, and with poor control of diabetes and hypertension, which requires sustained attention to self-management.20,21
Our findings suggest that interventions aimed at reducing missed appointments that focus on outreach to individual patients might overlook a broader context of neighborhood factors that affect appointment keeping, indicating the need for a more community-oriented approach to reducing missed appointments. Interventions have included texting reminders, shorter lead times for appointments, offering incentives, offering free ride share services, and substituting telemedicine visits for in person visits. 40–42 with varying levels of success. Additional consideration of the circumstances in neighborhoods where residents have higher levels of missed appointments might allow for more effective promotion of these approaches at community levels. For example, the engagement of community health workers, who are often members of the neighborhoods they serve and can reach patients where they live, is an effective approach in improving adherence to cancer screening recommendations, cardiovascular disease and diabetes prevention, and diabetes self-management 43 and might play an important role in improving appointment keeping more broadly. Additional alternative approaches might include the use of telemedicine visits,44 mobile health clinics, or allowing walk-in appointments for those who have missed scheduled appointments to mitigate the higher rates of missed appointments in some neighborhoods.
Our study has multiple limitations. It was conducted at a single multispecialty institution in Philadelphia, a city with high levels of poverty relative to other comparably sized or larger cities, and our experience might not be applicable elsewhere. We have a robust registry of neighborhood characteristics 26 that may not be available in other settings. There was a substantial proportion of patients whose race/ethnicity was classified as unknown/other, which might have occurred because patients did not identify as members of a single race or ethnic group or opted not to provide this information or because clinic staff did not record this information at the point of care. Resulting misclassification of race/ethnicity might have affected observed associations between race/ethnicity and appointment outcomes but is unlikely to have affected observed associations with neighborhood characteristics. Since this study was conducted, the large hospital that formerly provided inpatient care services for the population served by our clinics and where many of the clinicians employed by our clinics also provided inpatient care closed.45 Downstream consequences included the closure or relocation of multiple outpatient services represented in our study, obviating opportunities for follow-up studies or missed appointment prevention interventions at our study site.
In conclusion, characteristics of the populations in census tracts where patients reside were associated with missing scheduled clinic appointments, after taking into account personal characteristics that are also associated with missing appointments. This likely reflects an unmeasured mix of factors that interferes with appointment keeping. To date, efforts to reduce missed appointments have been targeted to individual patients with personal characteristics associated with higher levels of not keeping appointments. Our findings suggest that community-level interventions geared to the situations of patients living in neighborhoods with high levels of missed appointments might augment current intervention strategies.
Supplementary Information
(DOCX 39 kb)
Acknowledgements
The authors thank the three anonymous peer reviewers of their original submission for their thoughtful criticisms and suggestions.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alaeddini A, Yang K, Reddy C, Yu S. A probabilistic model for predicting the probability of no-show in hospital appointments. Health Care Manag Sci. 2011;14:146–57. doi: 10.1007/s10729-011-9148-9. [DOI] [PubMed] [Google Scholar]
- 2.Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015;18:131–6. doi: 10.1089/pop.2014.0047. [DOI] [PubMed] [Google Scholar]
- 3.Guzek LM, Gentry SD, Golomb MR. The Estimated Cost of “No-Shows” in an Academic Pediatric Neurology Clinic. Pediatric Neurology. 2015;52:198–201. doi: 10.1016/j.pediatrneurol.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 4.Moore CG, Wilson-Witherspoon P, Probst JC. Time and Money: Effects of No-Shows at a Family Practice Residency Clinic. Fam Med. 2001;33:522–7. [PubMed] [Google Scholar]
- 5.Nguyen DL, Dejesus RS, Wieland ML. Missed appointments in resident continuity clinic: patient characteristics and health care outcomes. J Graduate Med Education. 2011;3:350–5. doi: 10.4300/JGME-D-10-00199.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hwang AS, Atlas SJ, Cronin P, Ashburner JM, Shah SJ, He W, Hong CS. Appointment “no-shows” are an independent predictor of subsequent quality of care and resource utilization outcomes. J General Int Med. 2015;30:1426–33. doi: 10.1007/s11606-015-3252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2016;16:13. doi: 10.1186/s12913-015-1243-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carreras-García D, Delgado-Gómez D, Llorente-Fernández F, Arribas-Gil A. Patient no-show prediction: A systematic literature review. Entropy. 2020;22:675. doi: 10.3390/e22060675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dantas LF, Fleck JL, Cyrino Oliviera FL, Hamacher S. No-shows in appointment scheduling - a systematic literature review. Health Policy. 2018;122:412–21. doi: 10.1016/j.healthpol.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Norris JB, Kumar C, Chand S, Moskowitz H, Shade SA, Willis DR. An empirical investigation into factors affecting patient cancellations and no-shows at outpatient clinics. Decis Support Syst. 2014;57:428–43. doi: 10.1016/j.dss.2012.10.048. [DOI] [Google Scholar]
- 11.Partin MR, Gravely A, Gellad ZF, et al. Factors associated with missed and cancelled colonoscopy appointments at veterans health administration facilities. Clin Gastroenterol Hepatol. 2016;142:259–67. doi: 10.1016/j.cgh.2015.07.051. [DOI] [PubMed] [Google Scholar]
- 12.Rosenbaum JI, Mieloszyk RJ, Hall CS, Hippe DS, Gunn ML, Bhargava P. Understanding Why Patients No-Show: Observations of 2.9 Million Outpatient Imaging Visits Over 16 Years. J Am College Radiology. 2018;15:944–50. doi: 10.1016/j.jacr.2018.03.053. [DOI] [PubMed] [Google Scholar]
- 13.Glover M, Daye D, Khalilzadeh O, Pianykh O, Rosenthal DI, Brink JA, Flores EJ. Socioeconomic and demographic predictors of missed opportunities to provide advanced imaging services. J Am College Radiology. 2017;14:1403–11. doi: 10.1016/j.jacr.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 14.Majeroni BA, Cowan T, Osborne J, Graham RP. Missed appointments and Medicaid managed care. Arch Fam Med. 1996;5:507–11. doi: 10.1001/archfami.5.9.507. [DOI] [PubMed] [Google Scholar]
- 15.Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 16.National Association of Community Health Centers. Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE). Available at: http://www.nachc.org/research-and-data/prapare/. Accessed December 30, 2020.
- 17.Institute for Alternative Futures. Community Health Centers Leveraging the Social Determinants of Health. Available at: https://kresge.org/sites/default/files/IAF-CHCsLeveragingSDH.pdf. Accessed December 30, 2020.
- 18.Liu L, Núñez AE. Multilevel and urban health modeling of risk factors for diabetes mellitus: a new insight to public health and preventive medicine. Adv Prev Med 2014: 246049. [DOI] [PMC free article] [PubMed]
- 19.Lê-Scherban F, Ballester L, Castro JC, Cohen S, Melly S, Moore KM, Buehler J. Neighborhood characteristics associated with diabetes and hypertension control among an urban African American population: A study of geo-linked electronic health records. Prev Med Repts. 2019;15:100953. doi: 10.1016/j.pmedr.2019.100953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buehler JW, Castro JC, Cohen S, Zhao Y, Melly S, Moore K. Personal and neighborhood attributes associated with cervical and colorectal cancer screening in an urban African American Population. Prev Chronic Dis. 2019;16:190030. doi: 10.5888/pcd16.190030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ESRI. ArcGIS for Desktop: Creating a composite address locator (ArcMap 10.5). Available at: http://desktop.arcgis.com/en/arcmap/10.5/manage-data/geocoding/creating-a-composite-address-locator.htm. Accessed December 30, 2020.
- 22.Urban Health Collaborative, Drexel University. Data Repository. Available at: https://drexel.edu/uhc/resources/data/. Accessed April 29, 2021.
- 23.ESRI. How Hot Spot Analysis (Getis-Ord Gi*) works. Available at: https://pro.arcgis.com/en/pro-app/latest/tool-reference/spatial-statistics/h-how-hot-spot-analysis-getis-ord-gi-spatial-stati.htm. Accessed December 30, 2020.
- 24.United States Census Bureau. American Community Survey. Available at: https://www.census.gov/programs-surveys/acs/. Accessed December 30, 2020.
- 25.Philadelphia Police Department. Crime Maps and Stats. Available at: https://www.phillypolice.com/crime-maps-stats/. Accessed December 30, 2020.
- 26.OpenDataPhilly. Public Safety. Available at: https://www.opendataphilly.org/group/public-safety-group. Accessed December 30, 2020.
- 27.Forsyth A, Wall M, Choo T, Larson N, Van Riper D, Neumark-Sztainer D. Perceived and Police-Reported Neighborhood Crime: Linkages to Adolescent Activity Behaviors and Weight Status. J Adolesc Health. 2015;57(2):222–8. doi: 10.1016/j.jadohealth.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kerr Z, Evenson KR, Moore K, Block R, Diez Roux AV. Changes in walking associated with perceived neighborhood safety and police-recorded crime: The multi-ethnic study of atherosclerosis. Prev Med. 2015;73:88–93. doi: 10.1016/j.ypmed.2015.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Public Health Management Corporation. PHMC’s Community Health Data Base Southeastern Pennsylvania Household Health Survey Data Sources. Available at: http://chdb.phmc.org/householdsurvey.html. Accessed December 30, 2020.
- 30.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165:858–67. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 31.Schulz A, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Educat Behav. 2004;31:55–71. doi: 10.1177/1090198104265598. [DOI] [PubMed] [Google Scholar]
- 32.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 33.Polednak AP. Poverty, residential segregation, and black/white mortality rates in urban areas. J Health Care Poor Underserved. 1993;4:363–73. doi: 10.1353/hpu.2010.0094. [DOI] [PubMed] [Google Scholar]
- 34.Collins CA, Williams DR. Segregation and mortality: the deadly effects of racism? Sociological Forum. 1999;14:495–523. doi: 10.1023/A:1021403820451. [DOI] [Google Scholar]
- 35.Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Soc Sci Med. 1998;47:469–76. doi: 10.1016/S0277-9536(98)00128-2. [DOI] [PubMed] [Google Scholar]
- 36.Pruitt SL, Lee SJC, Tiro JA, Xuan L, Ruiz JM, Inrig S. Residential racial segregation and mortality among black, white, and hispanic urban breast cancer patients in Texas, 1995-2009. Cancer. 2015;121:1845–55. doi: 10.1002/cncr.29282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hayanga AJ, Zeliadt SB, Backhus LM. Residential segregation and lung cancer mortality in the United States. JAMA Surg. 2013;148:37–42. doi: 10.1001/jamasurgery.2013.408. [DOI] [PubMed] [Google Scholar]
- 38.Rothstein R. The Color of Law: A Forgotten History of How Our Government Segregated American. First Edition. New York: Liveright Publishing; 2017. [Google Scholar]
- 39.Tung EL, Cagney KA, Peek ME, Chin MH. Spatial context and health inequity: Reconfiguring race, place, and poverty. J Urban Health. 2017;94(6):757–763. doi: 10.1007/s11524-017-0210-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu C, Harvey HB, Jaworsky C, Shore MT, Guerrier CE, Pianykh O. Text message reminders reduce rutpatient radiology no-shows but do not improve arrival punctuality. J Am College Radiology. 2017;14:1049–54. doi: 10.1016/j.jacr.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 41.Chaiyachati KH, Hubbard RA, Yeager A, Mugo B, Lopez S, Asch E, Shi C, Shea JA, Rosin R, Grande D. Association of rideshare-based transportation services and missed primary care appointments: a clinical trial . JAMA Intern Med 2018;178:383-89 [Correction. JAMA Intern Med 2018;178:731-32]. [DOI] [PubMed]
- 42.Horvath M, Levy J, L'Engle P, Carlson B, Ahmad A, Ferranti J. Impact of health portal enrollment with email reminders on adherence to clinic appointments: a pilot study. J Medical Internet Res. 2011;13:e41. doi: 10.2196/jmir.1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.The Community Guide. Community Health Workers. Available at: https://www.thecommunityguide.org/content/community-health-workers. Accessed April 23, 2021.
- 44.Franciosi EB, Tan AJ, Kassamali B, Leonard N, Zhou G, Krueger S, Rashighi M, LaChance A. The Impact of Telehealth Implementation on Underserved Populations and No-Show Rates by Medical Specialty During the COVID-19 Pandemic. Telemed J E Health. 2021 Apr 7. doi: 10.1089/tmj.2020.0525. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 45.Rosenbaum L. Losing Hahnemann — Real-life lessons in “value-based” medicine. N Engl J Med. 2019;381:1193–95. doi: 10.1056/NEJMp1911307. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 39 kb)