Abstract
In this cross-sectional population-based study, we used the baseline data of the Prospective Epidemiologic Research Studies in IrAN cohort study collected in Iran from 2014 to 2020. The main outcomes were the prevalence of hypertension and proportion of awareness, treatment, and control based on the 2017 ACC/AHA guideline compared to the seventh report of the Joint National Committee (JNC7). Of the total of 163,770 participants, aged 35–70 years, 55.2% were female. The sex-age standardized prevalence of hypertension was 22.3% (95% CI 20.6, 24.1) based on the JNC7 guideline and 36.5% (31.1, 41.8) based on the ACC/AHA guideline. A total of 24,312 participants [14.1% (10.1, 18.1)] were newly diagnosed based on the ACC/AHA guideline. Compared to adults diagnosed with hypertension based on the JNC7 guideline, the newly diagnosed participants were mainly young literate males who had low levels of risk factors and were free from conventional comorbidities of hypertension. About 30.7% (25.9, 35.4) of them (4.3% of the entire population) were eligible for pharmacologic intervention based on the ACC/AHA guideline. Implementation of the new guideline may impose additional burden on health systems. However, early detection and management of elevated blood pressure may reduce the ultimate burden of hypertension in Iran.
Subject terms: Cardiology, Diseases, Medical research, Epidemiology, Risk factors
Introduction
In 2017, the American College of Cardiology/American Heart Association (ACC/AHA) guideline was released1, in which lower thresholds (≥ 130/80 mmHg) were recommended for hypertension, and the upper end of prehypertension based on the seventh report of the Joint National Committee (JNC7)2,3 was reclassified as stage 1 hypertension. The rationale for this shift is the evidence showing that adults with blood pressure in this range have an approximately twofold increase in risk of cardiovascular diseases (CVDs) compared to adults with normal blood pressure4,5. Additionally, recent randomized clinical trials have demonstrated benefits from a systolic blood pressure (SBP) lower than 130 mm Hg6,7 including the Systolic Blood Pressure Intervention Trial (SPRINT) which demonstrated substantial reduction in CVD events by applying an intensive systolic blood pressure target < 120 mmHg8. In a very recent study, Whelton et al.9 reported that the stepwise rise in incident atherosclerotic CVDs and presence of coronary artery calcium begins at SBP levels as low as 90 mmHg. However, the implications of the new hypertension definitions are under debate. Using lower thresholds for definition of hypertension will lead to increase in estimated prevalence, which will impose additional burden on health systems especially in low-middle income countries with limited resources10–13. On the other hand, early diagnosis and treatment of high blood pressure among adults previously classified in the category of “pre-hypertension” may lead to reduced all-cause and CVD-specific mortality and morbidity5,13. Primordial prevention seems to be a necessity for maintaining optimal blood pressure levels even in adults free from traditional risk factors of CVD9.
Studies demonstrate that all-cause mortality and cardiovascular deaths attributable to high blood pressure doubled in Iran since 1990 and hypertension is the most important risk factor responsible for mortality in both sexes14,15. JNC7 is still the widely used guideline for definition and treatment of hypertension in Iran, specifically among general physicians in remote areas. However, recent guidelines are gradually becoming popular. It is of utmost importance to explore the impacts of stricter definitions for high blood pressure prevalence, treatment, and control to reduce the burden of CVD in a country with a high prevalence of hypertension as a middle-income nation. There is a slowly increasing trend towards using ACC/AHA guideline in Iran during the past couple of years. Therefore, exploring the potential impact of this guideline on definition, treatment, and control of hypertension in Iran is essential.
The main objective of the current study was to determine the impact of the two guidelines on estimated prevalence, awareness, treatment, and control of hypertension among a very large group of Iranians residing in various regions across the country.
Results
A total of 163,770 participants were recruited from 2014 to 2020, 115,979 (70.8%) participants lived in urban areas and 47,791 (29.2%) participants were rural dwellers. A total of 90,397 participants (55.2%) were female. The mean (SD) age of the participants was 49.4 (9.2) years and 35.5% of participants were in the 35–44 age category. A total of 33,675 participants (20.6%) had no schooling. Systolic and/or diastolic blood pressure was missing in 889 participants.
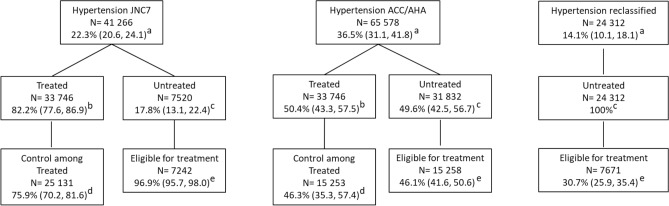
The sex-age standardized prevalence of hypertension was 22.3% (95% CI 20.6, 24.1) based on the JNC7 guideline and 36.5% (31.1, 41.8) based on the 2017 ACC/AHA guideline, which was 14.1% higher in absolute terms and 63.7% higher in relative terms (Fig. 1). The prevalence of hypertension based on the JNC7 guideline was significantly higher among females compared to males. In contrast, there was no difference in hypertension prevalence between sexes based on the ACC/AHA guideline. The prevalence of hypertension was greater with age regardless of guideline (Fig. 2).
Figure 1.
Number and weighted prevalence of hypertension, and proportion of treatment, control, and eligibility for pharmacologic intervention among adults classified as hypertensive based on both guidelines and the group of adults reclassified based on ACC/AHA guideline. aPrevalence of hypertensive participants among all study population. bProportion of hypertensive participants who are treated. cProportion of hypertensive participants who are untreated. dProportion of control among treated hypertensive participants. eProportion of untreated hypertensive participants eligible for pharmacologic intervention.
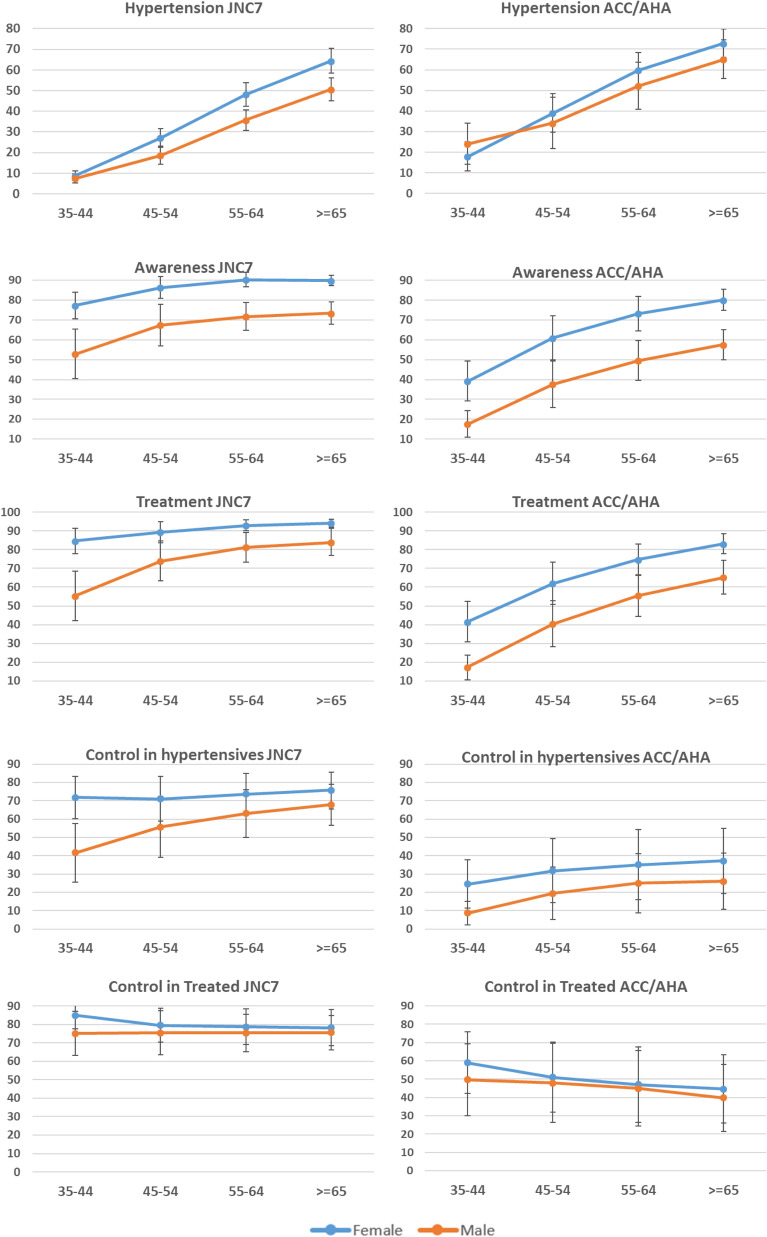
Figure 2.
Sex and age-specific prevalence of hypertension and proportion of awareness, treatment, and control based on the two guidelines.
A total of 24,312 (14.1% [10.1, 18.1]) participants who were classified in the category of “pre-hypertension” were reclassified into the hypertension category based on the ACC/AHA guideline (Fig. 1). Compared to adults traditionally diagnosed with hypertension based on the JNC7 report, the newly-diagnosed hypertensive adults based on the ACC/AHA guideline were more commonly male (62.1 vs. 42.9%), were younger than 55 years old (75.8 vs. 46.7%), were literate (74.5 vs. 57.4%), had normal BMI (23.2 vs. 15.5%), had high physical activity (39 vs. 29.5%), were free from diabetes (87.1, vs. 68.1%), were free from CKD (86.6 vs. 70.6%), had normal serum lipids (62.3 vs. 50.4%) and had low 10 year risk of ASCVD (90.1 vs. 72.5%) (Table 1). The shift from prehypertension based on JNC7 to stage 1 hypertension based on the ACC/AHA guideline was more prominent in males (Table 2).
Table 1.
Weighted prevalence of hypertension based on the 2017 ACC/AHA and JNC7 hypertension guidelines across socio-demographic groups, and increase in prevalence defined based on the ACC/AHA guideline.
| JNC7 (N = 41,266) | ACC/AHA (N = 65,578) | Reclassified participants (N = 24,312) | Relative Difference in prevalence (%) | |
|---|---|---|---|---|
| Sex | ||||
| Male | 18.9 (16.9, 20.9) | 36.1 (29.6, 42.6) | 17.2 (12.4, 22.1) | 91 |
| Female | 25.9 (24.2, 27.7) | 36.8 (32.3, 41.4) | 10.9 (7.6, 14.1) | 42.1 |
| Age categories | ||||
| 35–44 | 8.0 (6.7, 9.2) | 21.9 (16.4, 27.5) | 14.0 (9.6, 18.4) | 173.8 |
| 45–54 | 22.9 (20.4, 25.4) | 38.1 (31.8, 44.3) | 15.2 (10.9, 19.4) | 66.4 |
| 55–64 | 41.9 (39.2, 44.6) | 55.9 (50.6, 61.1) | 14.0 (10.4, 17.6) | 33.4 |
| ≥ 65 | 57.9 (54.8, 60.9) | 68.4 (64.2, 72.6) | 10.5 (8.1, 13.0) | 18.1 |
| Residence | ||||
| Urban | 22.5 (20.5, 24.5) | 35.5 (29.0, 42.0) | 13.0 (8.2, 17.8) | 57.8 |
| Rural | 21.9 (18.2, 25.6) | 39.8 (33.5, 46.1) | 17.9 (15.1, 20.7) | 81.7 |
| Marital status | ||||
| Non-married | 31.5 (28.6, 34.4) | 43.2 (38.1, 48.2) | 11.7 (8.2, 15.1) | 37.1 |
| Married | 21.6 (19.8, 23.3) | 35.9 (30.5, 41.4) | 14.3 (10.3, 18.4) | 66.2 |
| Education | ||||
| Illiterate (no schooling) | 36.0 (32.2, 39.8) | 49.6 (44.2, 55.1) | 13.6 (10.1, 17.2) | 37.8 |
| ≤ 5 years (primary) | 21.4 (18.8, 24.1) | 35.8 (30.9, 40.7) | 14.4 (10.6, 18.2) | 67.3 |
| 6–8 years (middle) | 15.3 (13.1, 17.4) | 30.0 (23.6, 36.4) | 14.7 (10.0, 19.5) | 96.1 |
| 9–12 years (secondary) | 15.7 (13.7, 17.7) | 29.5 (23.7, 35.4) | 13.8 (9.7, 18.0) | 87.9 |
| > 12 years (university) | 15.5 (13.5, 17.5) | 29.8 (23.0, 36.5) | 14.3 (9.2, 19.3) | 92.3 |
| Wealth index | ||||
| Quintile 1 (poorest) | 27.8 (24.1, 31.6) | 42.8 (38.4, 47.1) | 14.9 (11.6, 18.3) | 54 |
| Quintile 2 | 24.5 (21.9, 27.0) | 39.2 (35.1, 43.2) | 14.7 (11.2, 18.2) | 60 |
| Quintile 3 | 22.5 (20.5, 24.4) | 36.4 (30.9, 41.8) | 13.9 (9.9, 17.9) | 61.8 |
| Quintile 4 | 19.5 (17.4, 21.7) | 33.3 (27.1, 39.6) | 13.8 (9.4, 18.2) | 70.8 |
| Quintile 5 (richest) | 19.5 (17.1, 21.9) | 33.0 (25.6, 40.4) | 13.5 (8.2, 18.8) | 69.2 |
| Body Mass Index (kg/m2) | ||||
| Underweight | 5.1 (4.1, 6.2) | 16.0 (11.3, 20.8) | 10.9 (6.5, 15.2) | 213.7 |
| Normal | 13.2 (11.4, 14.9) | 25.6 (20.8, 30.5) | 12.5 (9.0, 15.9) | 93.9 |
| Overweight | 21.8 (19.3, 24.4) | 36.4 (29.7, 43.1) | 14.5 (10.1, 18.9) | 67 |
| Obese | 31.9 (29.1, 34.8) | 47.1 (39.8, 54.4) | 15.2 (10.4, 19.9) | 47.6 |
| Physical activity | ||||
| Low activity | 27.8 (25.6, 29.9) | 42.2 (36.3, 48.1) | 14.5 (9.9, 19.0) | 51.8 |
| Medium activity | 22.8 (21.2, 24.4) | 36.0 (30.6, 41.4) | 13.2 (9.0, 17.3) | 57.9 |
| High activity | 17.6 (16.0, 19.2) | 32.2 (27.4, 37.0) | 14.6 (11.0, 18.2) | 83 |
| Waist to hip ratio | ||||
| Normal | 9.6 (8.3, 10.9) | 22.0 (18.2, 25.9) | 12.4 (9.3, 15.5) | 129.2 |
| High | 25.6 (22.8, 28.3) | 40.1 (33.0, 47.2) | 14.5 (9.9, 19.2) | 56.6 |
| Diabetes | ||||
| No | 18.0 (16.5, 19.4) | 32.4 (27.0, 37.8) | 14.4 (10.3, 18.6) | 80 |
| Yes | 47.7 (45.2, 50.2) | 59.8 (54.6, 65.0) | 12.1 (9.0, 15.2) | 25.4 |
| Dyslipidemia | ||||
| No | 17.5 (16.0, 19.0) | 31.2 (26.0, 36.5) | 13.7 (9.7, 17.7) | 78.3 |
| Yes | 31.0 (28.8, 33.2) | 45.8 (40.7, 51.0) | 14.8 (10.9, 18.8) | 47.7 |
| CVD history | ||||
| No | 18.7 (17.0, 20.5) | 33.5 (27.8, 39.1) | 14.7 (10.6, 18.9) | 79.1 |
| Yes | 62.6 (59.5, 65.5) | 69.8 (65.8, 73.9) | 7.2 (5.2, 9.2) | 11.5 |
| CKD | ||||
| No | 19.2 (17.2, 21.2) | 34.1 (28.0, 40.1) | 14.9 (10.6, 19.1) | 11.5 |
| Yes | 37.1 (33.3, 40.8) | 47.7 (42.5, 52.9) | 10.6 (8.0, 13.2) | 28.6 |
| High ASCVD risk | ||||
| No | 18.0 (16.6, 19.5)a | 32.1 (26.9, 37.4)b | 14.1 (9.9, 18.4)c | 78.3 |
| Yes | 61.6 (59.1, 64.2)a | 75.6 (71.6, 79.7)b | 14.0 (11.9, 16.1)c | 22.7 |
Table 2.
Weighted prevalence and absolute change in hypertension according to JNC7 and ACC/AHA guidelines.
| JNC 7% (95% CI) | ACC/AHA % (95% CI) | Absolute difference | |
|---|---|---|---|
| Males | |||
| Normal | 58.3 (50.9–65.4) | 58.3 (50.9–65.4) | 0 |
| Prehypertension or elevated blood pressure | 22.8 (17.6–29.1) | 5.6 (4.1–7.5) | − 17.2 |
| Stage 1 hypertension | 16.8 (15.4–18.3) | 27.1 (23.3–31.2) | 10.3 |
| Stage 2 hypertension | 2.1 (1.5–2.9) | 9.0 (6.7–12.0) | 6.9 |
| Females | |||
| Normal | 59.2 (54.0–64.2) | 59.2 (54.0–64.2) | 0 |
| Prehypertension or elevated blood pressure | 14.9 (11.3–19.3) | 4.0 (2.9–5.5) | − 10.9 |
| Stage 1 hypertension | 24.3 (22.9–25.6) | 28.7 (26.1–31.5) | 4.4 |
| Stage 2 hypertension | 1.7 (1.2–2.3) | 8.1 (6.2–10.6) | 6.4 |
| Both sexes | |||
| Normal | 58.8 (52.6–64.7) | 58.8 (52.6–64.7) | 0 |
| Prehypertension or elevated blood pressure | 18.9 (14.6–24.2) | 4.8 (3.5–6.5) | − 14.1 |
| Stage 1 hypertension | 20.5 (19.2–21.7) | 27.9 (24.8–31.1) | 7.4 |
| Stage 2 hypertension | 1.9 (1.3–2.6) | 8.6 (6.5–11.2) | 6.7 |
The proportion of awareness among hypertensive adults was 77.5% (73.3, 81.8) based on the JNC7 and 48.6% (41.9, 55.4) based on the ACC/AHA guideline. Among the reclassified participants, awareness was just 2.9% (1.5, 4.3). The reclassified participants aware of their elevated blood pressure compared to participants aware of their traditionally defined hypertension were mostly male (46.8 vs. 36.2%) and were less than 55 years old (64.9 vs. 42.9%), but the proportion of literacy was not different between the two groups. Awareness was higher among females and increased by age based on the ACC/AHA guideline (Fig. 2).
The proportion of treatment among hypertensive adults was 82.2% (77.6, 86.9) and 50.4% (43.3, 57.5) based on the JNC7 and the ACC/AHA guidelines respectively. None of the re-classified participants were treated (Fig. 1). Treatment also increased by age and was higher in females based on both guidelines (Fig. 2).
The proportion of control among hypertensive adults was 63.7% (55.7, 71.7) and 23.3% (14.6, 32.0) based on the JNC7 and the ACC/AHA guidelines respectively. Control among hypertensive adults was higher in females.
The proportion of control among treated was 75.9% (70.2, 81.6) and 46.3% (35.3, 57.4) based on JNC7 and ACC/AHA respectively (Fig. 1). Control among treated participants decreased along with increase in age based on the ACC/AHA guideline.
Finally, based on the JNC7 report, out of the untreated hypertensive adults, a total of 7242 participants (96.9% [95.7, 98.0]) were eligible for pharmacologic treatment and based on the ACC/AHA guideline, 15,258 participants (46.1% [41.6, 50.6]) were eligible. Out of the reclassified participants, 7671 participants (30.7% [25.9, 35.4]) were eligible for pharmacologic treatment (Fig. 1). In short, among the entire study population, 14.1% were newly diagnosed with hypertension based on the ACC/AHA guideline, while only 30.7% of these newly diagnosed adults (4.3% of the entire population) were eligible for pharmacologic treatment.
Discussion
In the current study, representing a large number of the Iranian population, a total of 6.5 million and 10.7 million Iranians aged 35–70 years, have hypertension based on the JNC7 and the ACC/AHA guidelines, respectively. Although there was some heterogeneity in prevalence across study centers, the application of the ACC/AHA guideline uniformly led to increase in relative prevalence (by 63.7%) and decrease in relative awareness (37.3%), treatment (38.7%), control among hypertensive adults (63.4%), and control among treated adults (39.5%). Yet, the increase in prevalence observed in our study was still lower than previous studies in Iran, which reported a more than a twofold higher prevalence based on the ACC/AHA guideline16–18. Less than twofold increases were also observed in other countries10,11,19,20.
The results of our study showed that a total of 24,312 adults who were previously classified in the category of “pre-hypertension”, were shifted to stage 1 of hypertension based on the ACC/AHA 2017 guideline. These adults were mainly young and educated males, and many of them free from other metabolic risk factors and comorbidities of high blood pressure with a low 10-year risk of CVD events. These findings may mean that apparently healthy young low-risk male adults may be prone to developing high blood pressure later in life and they shall be detected and managed at early stages, particularly considering the fact that the risk of CVD mortality in males is higher than females, specifically in younger age groups5,21.
A similar study in Italy showed that the new blood pressure classification moved 37% of individuals from "pre-hypertension" to "stage 1" and 41% from "stage 1" to "stage 2" hypertension. These results were quite similar to the results of the current study and show that redistribution of hypertensive patients according to the ACC/AHA guideline may help to better identify uncontrolled hypertensive patients with high CVD risk profile22.
Implementation of the guideline necessitates that the public be informed and health care professionals use the updated guideline in practice. The result will be a higher number of adults diagnosed with hypertension, who should refer to health care professionals and be managed. There will thus be an apparent additional burden on health care systems. It is worth noting, however, that not all newly-diagnosed adults will require pharmacological treatment. Based on the new guideline, less than one third of the newly diagnosed adults, and mostly elderly groups, will require pharmacological treatment. Therefore, the guidance will not increase medication utilization among the majority, but will hopefully improve awareness and subsequent lifestyle modification before developing very high levels of blood pressure and its accompanying comorbidities later in their lives13. The Heart Outcomes Prevention Evaluation (HOPE)-3 trial demonstrated that treatment of adults with intermediate CVD risk has no benefit23. Meanwhile, there is recent evidence on cost-effectiveness of a low-cost community-based plan focused on non-pharmacologic but including pharmacologic intervention in three low-income countries (Bangladesh, India, and Sri Lanka)24. These results highlight the importance of an integrated non-pharmacological intervention among low and intermediate-risk adults, as recommended in the 2017 ACC/AHA guideline, specifically feasible in low and middle-income countries. Reclassification of adults to higher stages of hypertension compared to previous guidelines is predominantly aimed at improving non-pharmacological interventions and life-style changes. This is the main reason for abolishment of the definition of “pre-hypertension” in recent US guidelines.
The new definition by ACC/AHA was derived from observational studies and clinical trials, focused specifically on results of Systolic Blood Pressure Intervention Trial (SPRINT)8,25. There are, however, a number of other studies and trials that don’t support the new criteria and conclude that there is no additional benefit in implementing stricter definitions for hypertension26,27. Additionally, although not all newly-labeled hypertensive adults will require pharmacological treatment, there will be an increase in clinical encounters imposing burden of health system infrastructure. According to the AHA/ACC guideline, antihypertensive pharmacologic treatment is initiated for hypertensives with a blood pressure equal or higher than 140/90 mmHg, unless they are high risk28. This approach is similar to the ESC/ESH guidelines where for the overwhelming majority of hypertensives, treatment is initiated at this threshold and some consideration for pharmacological treatment can be given to adults with blood pressure 135–139/85–89 mmHg if they report CVD29–31. On the other hand, the American College of Physicians and the American Academy of Family Physician guideline was developed for adults 60 years and older and recommended pharmacological treatment to be initiated when SBP was 150 mmHg or higher, unless there was a prior history of stroke or transient ischemic attack, in which case pharmacologic treatment is initiated for blood pressures equal or higher than 140/90 mmHg32,33. In actuality, there are more similarities between the guidelines than differences34 with the primary difference focused on the definition of stage 1 hypertension. The debate will remain unresolved until longitudinal large-scale studies are conducted on cost-effectiveness and adverse events of different approaches and guidelines35–37.
Ultimately, it is worth mentioning that the apparent decrease in awareness, treatment, and control based on the ACC/AHA guideline is due to the fact that neither physicians and health care professionals are aware and use the new guideline in practice, nor the public are informed of the new criteria. Comparing awareness, treatment, and control between various guidelines will only be possible upon their implementation at large scale and for long time periods.
Educational campaigns provide excellent opportunities for improving the awareness of the public and the healthcare workers. World Hypertension Day, promoted by the International Society of Hypertension38, and the World Kidney Day39 are two exemplar educational campaigns that share this specific goal by providing free blood pressure measurements. In the meantime, using smart phones or tablets can be an excellent option for improving awareness in the general public during the campaigns40.
Our study has certain limitations. Despite the large scale of the study and the unique and standard protocol used in its design and implementation, there were variations in outcomes between centers. Therefore, we used study centers as the primary sampling units in our survey data analysis. The cross-sectional design of the study is another limitation that makes it impossible to explore and prove causal relationships. The next limitation is the exclusion of adults younger than 35 years from the study (based on the predetermined protocol of PERSIAN). The fourth limitation is that part of the data in this study was collected before the release of ACC/AHA guideline in 2017. Hereby, we actually aimed to explore what would be the impact if this guideline was applied. And the last limitation of this study is that the mean of first and second blood pressure measurement was used based on JNC7 instead of recording the highest based on the ACC/AHA guideline.
Conclusions
Overall, our results showed that implementation of the 2017 ACC/AHA guideline will lead to shifting a group of mainly young male adults to the category of stage 1 of hypertension. Future longitudinal studies are mandatory to explore whether the implementation of this strict guideline is cost-beneficial in various settings, especially in low and middle income countries with limited resources. The results of this study demonstrated the “clustering” of metabolic risk factors, which necessitates an integrated approach towards primordial prevention of these risk factors.
Methods
Study design
The current study used data from the Prospective Epidemiologic Research Studies in IrAN (PERSIAN) cohort with a population-based cross-sectional design in the baseline recruitment phase. Detailed methods of PERSIAN are published elsewhere41,42 In short, a total of 163,770 participants aged 35–70 years were recruited in 18 cohort centers located in 16 provinces in Iran between 2014 and 2020. Participants were recruited through cluster random sampling. The sample was selected to include all ethnic groups in Iran residing in regions with various climates. The exclusion criteria were unwillingness to participate in the study, living in the designated area for less than 9 months, and physical and psychosocial disability impeding the enrollment process. Data collected during the entire 6-year period has been aggregated in the current analysis.
In the first step, trained personnel visited households to invite eligible individuals (based on inclusion criteria) to participate in the study. If individuals agreed to participate, they were requested to refer to their local cohort center in overnight fasting state and to bring the medications they use. Upon arrival, written informed consent form was signed by all participants. They underwent biospecimen collection (blood, urine, hairs, and nails) as well as anthropometric measurements, following protocols established by the US National Institutes of Health43. A structured questionnaire including 482 items was filled out during a face-to-face interview. Demographic characteristics, socioeconomic status, lifestyle, past medical history and family history, and medication history were queried. PERSIAN was approved by the ethics committees of the Digestive Disease Research Institute in Tehran University of Medical Sciences and Health Services, and the Medical Sciences Universities supervising each cohort in local study centers. All methods were carried out in accordance with relevant guidelines and regulations. Participants in PERSIAN will be followed for up to 15 years.
Definitions of outcomes
The main outcomes in this study were prevalence, awareness, treatment, and control of hypertension, and eligibility for treatment based on both JNC72,3 and the 2017 ACC/AHA guidelines1. Treatment was defined as self-reported intake or the antihypertensive medications that the participant brought with himself/herself to the study center. Awareness was defined as self-reported history of being diagnosed with hypertension by a physician or a health care professional.
Protocols for blood pressure measurement were developed and validated in the pilot phase of the study. Personnel were meticulously trained by the core team of the PERSIAN to use Riester Exacta 1350 sphygmomanometers across all study centers. Sphygmomanometers were calibrated annually. Trained personnel measured blood pressure in sitting position after 10 min of rest, twice from the right arm and twice from the left arm, with one-minute interval between each of the two consecutive measurements. Personnel were specifically trained to round the measured blood pressure to the nearest 2 mmHg. The average of the second measurements from right and left arms were calculated and considered as the level of blood pressure. Multiple cuff sizes were available for use to best fit the participant’s arm. Trained supervisors at study centers monitored the process of blood pressure measurement and controlled the quality of measurement and data entry. Supervisors used a checklist for monitoring and evaluation of the blood pressure measurement conducted by each of the personnel. Personnel were retrained in case supervisors observed mistakes.
Definitions of determinants
Demographic characteristics included sex, age, area of residence (rural, urban), and marital status (married versus non-married). Socio-economic status was defined based on education and wealth index. Education was defined in 5 levels: no schooling (< 1 year of primary school), primary school (1–5 years), middle school (6–8 years), high school (9–12 years), and university (> 12 years). Wealth index was calculated using multiple correspondence analysis (MCA) on household assets and divided into 5 quintiles. For physical activity, metabolic equivalents of tasks (METs) were calculated and divided into tertiles. Body mass index (BMI) was calculated and divided into four groups: underweight (< 18.5 kg/m2), normal (≥ 18.5 and < 25 kg/m2), overweight (≥ 25 and < 30 kg/m2), and obese (≥ 30 kg/m2). A high waist to hip ratio (WHR) was defined as a ratio ≥ 0.9 in males or ≥ 0.85 in females. Diabetes was defined as self-reported usage of relevant medications or fasting blood sugar (FBS) ≥ 126 mg/dL. Dyslipidemia was defined as low density cholesterol (mg/dL) ≥ 160 and/or total cholesterol (mg/dl) ≥ 240 and/or high density cholesterol (mg/dL) < 40 and/or reporting a history of using lipid lowering medications. Chronic kidney disease (CKD) was defined as glomerular filtration rate (GFR) < 60 ml/min. The 10-year risk of atherosclerosis CVD (ASCVD) based on the ACC/AHA guideline was calculated for all participants44.
Statistical analyses
We calculated the sex and age standardized prevalence of hypertension, the proportion of awareness, treatment, and control among hypertensive patients, the proportion of control among treated patients, and the proportion of untreated adults who were eligible for pharmacologic intervention based on both guidelines. Given the cluster sampling, we used a complex survey design to obtain summary measures. We used sampling weights defined as the inverse probability of being selected in the survey based on data of the national census in 2016. For all estimates, 95% confidence intervals were reported. Data were analyzed using Stata software (version 14.1) (Stata Corp, College Station, TX, USA).
Ethics approval
PERSIAN was approved by the ethics committees of the Digestive Disease Research Institute in Tehran University of Medical Sciences and Health Services, and the Medical Sciences Universities supervising each cohort in local study centers.
Acknowledgements
The authors would like to thank all people who participated in the PERSIAN cohort study, and all staff members for collaborating in data collection.
Abbreviations
- ACC
American College of Cardiology
- AHA
American Heart Association
- ASCVD
Atherosclerotic cardiovascular disease
- BMI
Body mass index
- CI
Confidence interval
- CKD
Chronic kidney disease
- CVD
Cardiovascular disease
- DBP
Diastolic blood pressure
- FBS
Fasting blood sugar
- HDL
High-density lipoprotein
- JNC7
Seventh report of the Joint National Committee
- LDL
Low-density lipoprotein
- MCA
Multiple correspondence analysis
- MET
Metabolic equivalent of task
- PERSIAN
Prospective epidemiologic research studies in IrAN
- SBP
Systolic blood pressure
- WHR
Waist-to-hip ratio
Author contributions
All authors either contributed to the conception or design of the work, or contributed to acquisition, analysis, or interpretation of data. S.G.S., F.N., H.P., and M.P. drafted the manuscript. F.N., F.K., A.E., and R.M. critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Funding
This study used the data obtained from the PERSIAN (Prospective Epidemiological Research Studies in IrAN) Cohort study in Iran. This work was supported by Tehran University of Medical Sciences and Health Services through Grant no. 700/534.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Sadaf G. Sepanlou and Farid Najafi.
References
- 1.Whelton PK, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A Report of the American College of Cardiology/American Heart association task force on clinical practice guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/hyp.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.James PA, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 4.Bundy JD, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: A systematic review and network meta-analysis. JAMA Cardiol. 2017;2:775–781. doi: 10.1001/jamacardio.2017.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carey RM, Whelton PK. Prevention, detection, evaluation, and management of high blood pressure in adults: Synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann. Intern. Med. 2018;168:351–358. doi: 10.7326/m17-3203. [DOI] [PubMed] [Google Scholar]
- 6.Bangalore S, Rimoldi SF, Messerli FH. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 2016;374:2293. doi: 10.1056/NEJMc1602668. [DOI] [PubMed] [Google Scholar]
- 7.Xie X, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: Updated systematic review and meta-analysis. Lancet. 2016;387:435–443. doi: 10.1016/s0140-6736(15)00805-3. [DOI] [PubMed] [Google Scholar]
- 8.Wright JT, Jr, et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whelton SP, et al. Association of normal systolic blood pressure level with cardiovascular disease in the absence of risk factors. JAMA Cardiol. 2020;5:1011–1018. doi: 10.1001/jamacardio.2020.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abariga SA, Khachan H, Al Kibria GM. Prevalence and determinants of hypertension in india based on the 2017 ACC/AHA guideline: Evidence from the India national family health survey. Am. J. Hypertens. 2020;33:252–260. doi: 10.1093/ajh/hpz181. [DOI] [PubMed] [Google Scholar]
- 11.Barszczyk A, et al. Potential impact of the 2017 high blood pressure guideline beyond the United States: A case study of the People's Republic of China. Am. J. Hypertens. 2020 doi: 10.1093/ajh/hpaa094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khera RI, of,, et al. ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ. 2017;362(k2357):2018. doi: 10.1136/bmj.k2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muntner P, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137:109–118. doi: 10.1161/circulationaha.117.032582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stanaway JD. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/s0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Worldwide trends in blood pressure from to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 1975;389(37–55):2017. doi: 10.1016/s0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asgari S, Khaloo P, Khalili D, Azizi F, Hadaegh F. Status of Hypertension in Tehran: Potential impact of the ACC/AHA 2017 and JNC7 Guidelines, 2012–2015. Sci. Rep. 2019;9:6382. doi: 10.1038/s41598-019-42809-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahdavi M, et al. Insight into blood pressure targets for universal coverage of hypertension services in Iran: The 2017 ACC/AHA versus JNC 8 hypertension guidelines. BMC Public Health. 2020;20:347. doi: 10.1186/s12889-020-8450-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mirzaei M, Mirzaei M, Mirzaei M, Bagheri B. Changes in the prevalence of measures associated with hypertension among Iranian adults according to classification by ACC/AHA guideline 2017. BMC Cardiovasc. Disord. 2020;20:372. doi: 10.1186/s12872-020-01657-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garies S, et al. Prevalence of Hypertension, Treatment, And Blood Pressure Targets in Canada Associated With the 2017 American College of Cardiology and American Heart Association Blood Pressure Guidelines. JAMA Netw. Open. 2019;2:e190406. doi: 10.1001/jamanetworkopen.2019.0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li D, et al. Increased risk of hypertension in young adults in Southwest China: Impact of the 2017 ACC/AHA high blood pressure guideline. Curr. Hypertens. Rep. 2019;21:21. doi: 10.1007/s11906-019-0926-y. [DOI] [PubMed] [Google Scholar]
- 21.Bots SH, Peters SAE, Woodward M. Sex differences in coronary heart disease and stroke mortality: A global assessment of the effect of ageing between 1980 and 2010. BMJ Glob. Health. 2017;2:e000298. doi: 10.1136/bmjgh-2017-000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tocci G, et al. Reclassification of hypertensive outpatients according to new US guidelines on high blood pressure. Am. J. Hypertens. 2019;32:77–87. doi: 10.1093/ajh/hpy139. [DOI] [PubMed] [Google Scholar]
- 23.Lonn EM, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N. Engl. J. Med. 2016;374:2009–2020. doi: 10.1056/NEJMoa1600175. [DOI] [PubMed] [Google Scholar]
- 24.Jafar TH, et al. A community-based intervention for managing hypertension in Rural South Asia. N. Engl. J. Med. 2020;382:717–726. doi: 10.1056/NEJMoa1911965. [DOI] [PubMed] [Google Scholar]
- 25.Vaduganathan M, et al. Baseline blood pressure, the 2017 ACC/AHA high blood pressure guidelines, and long-term cardiovascular risk in SPRINT. Am. J. Med. 2018;131:956–960. doi: 10.1016/j.amjmed.2017.12.049. [DOI] [PubMed] [Google Scholar]
- 26.Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: A systematic review and meta-analysis. JAMA Intern. Med. 2018;178:28–36. doi: 10.1001/jamainternmed.2017.6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ihm SH, Bakris G, Sakuma I, Sohn IS, Koh KK. Controversies in the 2017 ACC/AHA hypertension guidelines: Who can be eligible for treatments under the new guidelines? An asian perspective. Circ J. 2019;83:504–510. doi: 10.1253/circj.CJ-18-1293. [DOI] [PubMed] [Google Scholar]
- 28.German CA, et al. Implications of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline in a modern primary prevention multi-ethnic prospective cohort (multi-ethnic study of atherosclerosis) Am. J. Cardiol. 2019;123:1076–1082. doi: 10.1016/j.amjcard.2018.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bakris G, Ali W, Parati G. ACC/AHA versus ESC/ESH on hypertension guidelines: JACC guideline comparison. J. Am. Coll. Cardiol. 2019;73:3018–3026. doi: 10.1016/j.jacc.2019.03.507. [DOI] [PubMed] [Google Scholar]
- 30.Gijón-Conde T, et al. Impact of the European and American guidelines on hypertension prevalence, treatment, and cardiometabolic goals. J. Hypertens. 2019;37:1393–1400. doi: 10.1097/hjh.0000000000002065. [DOI] [PubMed] [Google Scholar]
- 31.Williams B, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 32.Jaeger BC, et al. Cardiovascular disease and mortality in adults aged ≥60 years according to recommendations by the American College of Cardiology/American Heart Association and American College of Physicians/American Academy of Family Physicians. Hypertension. 2019;73:327–334. doi: 10.1161/hypertensionaha.118.12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qaseem A, et al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: A clinical practice guideline from the American college of physicians and the American academy of family physicians. Ann. Intern. Med. 2017;166:430–437. doi: 10.7326/m16-1785. [DOI] [PubMed] [Google Scholar]
- 34.Whelton PK, Williams B. The 2018 European Society of Cardiology/European Society of Hypertension and 2017 American College of Cardiology/American Heart association blood pressure guidelines: More similar than different. JAMA. 2018;320:1749–1750. doi: 10.1001/jama.2018.16755. [DOI] [PubMed] [Google Scholar]
- 35.Bress AP, et al. Potential cardiovascular disease events prevented with adoption of the 2017 American College Of Cardiology/American Heart Association Blood Pressure Guideline. Circulation. 2019;139:24–36. doi: 10.1161/circulationaha.118.035640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cho SMJ, Lee H, Kim HC. Differences in prevalence of hypertension subtypes according to the 2018 Korean Society of Hypertension and 2017 American College of Cardiology/American Heart Association guidelines: The Korean National Health and Nutrition Examination Survey, 2007–2017 (KNHANES IV-VII) Clin. Hypertension. 2019;25:26. doi: 10.1186/s40885-019-0129-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bell KJL, Doust J, Glasziou P. Incremental benefits and harms of the 2017 American College of Cardiology/American Heart Association High blood pressure guideline. JAMA Intern. Med. 2018;178:755–757. doi: 10.1001/jamainternmed.2018.0310. [DOI] [PubMed] [Google Scholar]
- 38.Volpe M, Tocci G, Borghi C, Parati G. New opportunities for monitoring blood pressure control and awareness in the population: insights from 12-Year editions of the world hypertension day. High Blood Pressure Cardiovas Prevent Official J Italian Soc Hypertension. 2016;23:333–335. doi: 10.1007/s40292-016-0172-1. [DOI] [PubMed] [Google Scholar]
- 39.Bakris GL, Ritz E. The message for World Kidney Day 2009: hypertension and kidney disease: a marriage that should be prevented. J. Clin. Hypertension. 2009;11:144–147. doi: 10.1111/j.1751-7176.2009.00092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ni Z, et al. Chinese physicians' perspectives on the 2017 American College of Cardiology/American Heart Association hypertension guideline: A mobile app-based survey. High Blood Pressure Cardiovas Prevent Official J Italian Soc Hypertension. 2019;26:247–257. doi: 10.1007/s40292-019-00321-9. [DOI] [PubMed] [Google Scholar]
- 41.Poustchi H, et al. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): Rationale, objectives, and design. Am. J. Epidemiol. 2018;187:647–655. doi: 10.1093/aje/kwx314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eghtesad S, et al. The PERSIAN cohort: providing the evidence needed for healthcare reform. Arch. Iran. Med. 2017;20:691–695. [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES). Anthropometry ProceduresManual. Atlanta, GA; 2007. https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf. Accessed October 23, 2020.
- 44.Goff DC, Jr, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014;63:2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.