Abstract
Objective
To assess the utility of a 10-second tandem stance test in predicting gait impairment and the need for a mobility aid.
Design
Cross-sectional study.
Setting
Public hospital ambulatory and hospitalized care.
Participants
Participants were drawn from referrals to the physiotherapy service and patients identified by health care staff as needing mobility assessment. Eighty-seven people were referred to the study. Sixty-one individuals (N=61) consented to participate; mean age was 76±9.8 years and 61% were female. All participants were community dwelling.
Intervention
The 10-second tandem stance test and gait parameters were measured while walking with no walking aid, a walking stick, and a 4-wheeled walker were assessed.
Main Outcome Measures
Associations between the 10-second tandem stance test performance with prescribed walking aids (primary outcome variable), gait parameters (gait cycle time, cadence, stance phase, swing phase, double support, stride length, speed, peak angle velocity, maximal heel clearance), falls history, falls risk (Falls Risk for Older People in the Community [FROP-Com]), and walking aid use.
Results
Inability to maintain tandem stance for 10 seconds significantly increased the odds of requiring a prescribed walking aid (odds ratio [OR], 5.19; P=.01). Tandem stance test time was positively correlated with stride length, gait speed, peak angle velocity, and maximal heel clearance during the gait cycle. Correlation between tandem stance time and number of falls was weak but significant (ρ=−0.31, P=.01), and FROP-Com score for falls risk was negative and moderate for nonpreferred foot behind (ρ=−0.58, P<.01). The 10-second tandem stance with nonpreferred foot behind was associated with falling in previous 12 months (P=.04). Walking aid use history in subgroups with the individuals who cannot maintain the tandem stance with nonpreferred foot behind for 10 seconds was associated with falling in previous 12 months (OR, 55.00; 95% CI, 2.44-1238.46; P=.01).
Conclusions
The 10-second tandem stance test was associated with professionally prescribed walking aids, gait parameters with prescribed walking aids, falls, and walking aid use history, indicating the test may be useful to guide the prescription of walking aids.
Keywords: Accidental falls, Physical therapy specialty, Prescriptions, Rehabilitation, Self-help devices, Walking
List of abbreviations: FROP-Com, Falls Risk for Older People in the Community; MMSE, Mini-Mental State Examination; OR, odds ratio
The ability to walk is not only one of the most important and essential activities of daily living but it is also vital to older peoples’ independence and well-being.1 Many factors may impair walking, including physiological changes secondary to aging and acute or chronic diseases.2 Another consequence of walking impairment is increased risk of falling. Older people in particular are more prone to falling, with several gait parameters changes, such as decreased gait speed and worse performance on swing and double support phase, being independent predictors of falls in older people.3
The rate of falls in community-dwelling older people around the world is estimated to be between 30% and 40% each year.4 Fortunately, many falls are preventable.5 Falls risk may be reduced by the use of mobility aids by those with walking impairments.6 Other benefits include increased autonomy and enhanced confidence.7 However, Gell et al8 reported that there is evidence of incorrect mobility aid use in older people, and this can lead to increased risk of falls. Allen et al9 report that many people who may benefit from using mobility aids do not use them because of perceived stigma and social pressures.9 Regarding balance assessment, a range of validated and standardized tools can be used, each with their own limitations. A lesser known assessment is the tandem stance test. This involves a person assuming a standing posture with one foot in front of the other for a timed period, up to 60 seconds.10 This test can be used as a stand-alone test or in combination with other balance tests. According to Hile et al,11 the maximum holding time varies from 5-60 seconds in a given protocol, but 10 or 30 seconds are most typically reported in the literature.10,12, 13, 14, 15, 16
An association between gait speed and a tandem stance has previously been documented. Verghese et al3 demonstrated that slower gait speed was associated with an increased risk of falling. Individuals with a gait speed of 0.7 m/s or slower had 1.5 times greater risk of falls than participants with normal gait speed. Hile et al11 reported that people who were not able to assume tandem stance had a gait speed of 0.74 m/s, whereas people who were able to sustain tandem stance for 10 seconds or longer had a gait speed of 1.1 or higher. However, they found no statistical difference in gait speed between people who could hold the tandem stance position for less than 10 seconds, 10-29 seconds, and more than 30 seconds in people who are able to position their feet in tandem stance without support.11 This may indicate that the association between tandem stance test and gait speed may lie somewhere from not being able to perform tandem stance test to 10 seconds holding time of tandem stance. Hence, the 10-second tandem stance test may have utility as a quick clinical tool to predict gait impairment and hence the need for a mobility aid, gait reeducation, and fall prevention interventions. To date, an association between performance of the 10-second tandem stance test and prescription of walking aids has not been investigated.
This study aimed to evaluate the utility of the 10-second tandem stance test in determining the need for mobility aid use for balance impairment and fall prevention. Specifically, associations were explored between the 10-second tandem stance test and prescribed walking aids, gait parameters, fall history, falls risk, and history of walking aid use.
Methods
This study used a cross-sectional design. Ethics approval was granted by the Hunter New England Local Health District Human Ethics Research Committee.
Study participants
Participants were drawn from referrals to the physiotherapy service and any patients identified by health care staff as needing mobility assessment at Armidale Rural Referral Hospital in Australia from March 2019 to December 2019. All participants provided written informed consent. Eligibility for inclusion was an ability to walk 10 m with or without a walking aid and with or without assistance. Exclusion criteria included acute severe neurologic conditions, recent orthopedic surgery or fracture, and cognition impairment determined by a Mini-Mental State Examination (MMSE) score <24.17
Study procedure
Demographic information including age, sex, foot dominance, and MMSE scores were collected at the commencement of the data collection session.
Prior to commencing physical testing, participants were randomized to either first perform the 10-second tandem stance test or to undergo gait analysis. The 10-second tandem stance test was administered following the method described by Guralnik et al.10 Participants were provided with a demonstration and instructions by the researcher. Participants stood holding on to a railing while placing one foot in front of the other. The foot to be positioned behind or front was self-selected by participants and recorded. The researcher stood behind and to the left of participants, outside of their vision, ready to provide support if needed. Timing started as contact with the railing was released and continued for 10 seconds or until participants contacted external support or moved out of tandem stance. No practice was allowed. The test was performed twice. Next, participants were asked to change the foot order, and the test was repeated twice in that position. It was important to test with alternate legs in the front position because in tandem stance there is weight bearing asymmetry between the legs, whereby the front leg is primarily responsible for postural mechanisms to control anteroposterior sway.18 Mobility status information was obtained by recording the walking aid(s) they had been prescribed by a health professional, the walking aid(s) they regularly used, and the walking aid they used at the time of their latest fall.
Gait parameters were measured using the PhysiGait Lab gait analysis system.a The parameters collected were gait cycle time, cadence, stance ratio, swing ratio, stride length, double support ratio, gait speed, maximal angular velocity during swing, and maximal heel clearance. Validity of this instrument against an optical motion capture system (Vicon, Oxford Metrics) in young and elderly populations has previously been established.19,20 Reliability of gait parameters has been demonstrated with intraclass correlation coefficients ranging from 0.91-0.96.19,20 Participants walked a 20-m straight walking course 3 times, first with no aid, then with a walking stick,and finally with a 4-wheeled walker. Participants were instructed to walk at their comfortable pace as described by Guralnik et al.10
Retrospective falls were measured by asking the participant to recall the number of falls they had experienced in the preceding 12 months.11 The World Health Organization definition was used to classify a fall, defining a fall as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.”4(p4)
Falls risk was assessed using the Falls Risk for Older People in the Community (FROP-Com) questionnaire, which was developed to examine multifactorial falls risk, reporting intraclass correlation coefficients of 0.93 and 0.81 for intrarater reliability and interrater reliability, respectively.21 The sum yields an overall falls risk score, ranging from 0-60. A higher score indicates greater risk.
Data analysis and sample size calculation
Data detailing demographic characteristics of participants, MMSE scores, walking aid prescribed, falls risk, and falls history were summarized descriptively. The 10-second tandem stance results were summarized as median and interquartile range (IQR) for all participants and stratified according to prescribed walking aid. Three participants did not have walking aid prescription assessment by their data collection. They were excluded from a part of data analysis association between tandem stance and prescribed mobility aid status and association between tandem stance time and gait parameters. The association between being prescribed a walking aid and ability to maintain tandem stance for 10 seconds was generated from dichotomized data using univariate logistic regression. Sensitivity and specificity estimates were derived from 2 × 2 tables according to standard formulae.
Gait parameters during unassisted walking were summarized as median (IQR) for each walking aid prescribed to participants, that is, no aid, walking stick, and 4-wheel walker. Between-condition differences for each parameter were assessed by Kruskal-Wallis tests. Correlations were assessed between 10-second tandem stance time and unassisted walking using Spearman ρ.
Correlations between tandem stance time and number of falls and FROP-Com scores were each calculated using Spearman ρ. Differences in tandem stance time according to fall history status were assessed using Wilcoxon rank-sum test. Inability to maintain tandem stance for 10 seconds was tabulated against occurrence of previous falls and odds ratios (ORs) calculated by univariate logistic regression. Calculation of ORs for the subgroup examination of falls and walking aid use of participants unable to maintain tandem stance for 10 seconds was performed by univariate logistic regression.
Based on the previous work of Hile et al,11 it was expected that a proportion of 0.32 of participants would be unable to complete 10 seconds of tandem stance. Using this proportion, α=0.05, and power = 0.8, we found a minimum sample size of 54 people was required for this study. To allow for any potential data loss, a final minimum sample size of 60 participants was established.
Results
Characteristics of study participants
Sixty-one participants were enrolled into the study, as shown in fig 1. Three participants had not been assessed for prescription of a mobility aid at the time of data collection. A description of the participants is provided in table 1. The study sample had a mean age of 76±9.8 years (range, 40-94) and 60% were female. Foot dominance was reported as right 86.8%, left 11.4%, and ambidextrous 1.6%. Thirty-eight participants (62%) reported having fallen at least once in the past 12 months. The mean FROP-Com score was 17.8±8.9.
Fig 1.
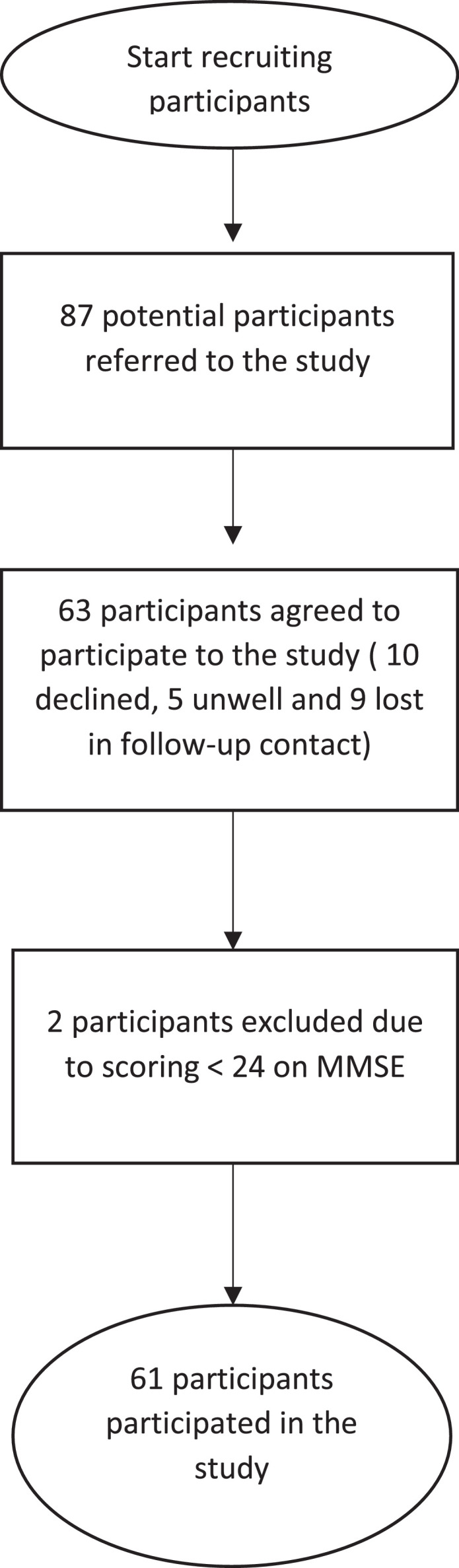
Flow of participants through the study.
Table 1.
Characteristics of the Study Sample (N=61)
| Characteristic | Value |
|---|---|
| Age (y) Mean ± SD Range |
76.0±9.8 40-94 |
| Sex, n (%) Female Male |
37 (60.7) 24 (39.3) |
| Diagnoses, n Osteoarthritis Back pain Cerebral vascular accident Fall Pneumonia Coronary bypass Chronic obstructive pulmonary disease Non-ST-elevation myocardial infarction Deconditioned Fracture Balance impairment Decreased mobility Pancreatitis Tendinopathy Asthma Ascites Syncope Spinal fusion Hypotension Subdural hematoma Urinary tract infection Gout Ventral hernia repair Acute kidney injury Rheumatoid arthritis Polymyalgia rheumatica Sepsis Total knee replacement Pulmonary hypertension Acute knee pain Heart failure Parkinson disease Not specified |
10 6 5 4 2 2 2 2 2 2 2 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 |
| MMSE score, mean ± SD | 27.95±1.69 |
| Foot dominance, n (%) Right Left Ambidextrous |
53 (86.9) 7 (11.5) 1 (1.6) |
| Walking aid prescribed, n (%) None Walking stick 4 wheel walker |
21 (36.2) 13 (22.4) 24 (41.4) |
| FROP-Com score Mean ± SD Range |
17.89±8.87 1-36 |
Ten-second tandem stance test
When performing the test, 47 participants (77%) placed their left foot behind as their preferred stance position. The results of 10-second tandem stance test are presented in table 2. The median time the tandem stance position was maintained for all combinations of foot position was 10 seconds.
Table 2.
Results of 10-second tandem stance test listed by prescribed/regular walking aid
| All Participants(n=58) |
No Aid Users(n=21) |
Walking Stick Users (n=13) |
4-Wheel Walker Users (n=24) |
|||||
|---|---|---|---|---|---|---|---|---|
| Stance | Tandem Stance Time, median (IQR) | Maintaining Stance for 10 s, n (%) | Tandem Stance Time, median (IQR) | Maintaining Stance for 10 s, n (%) | Tandem Stance Time, median (IQR) | Maintaining Stance for 10 s, n (%) | Tandem Stance Time, median (IQR) | Maintaining Stance for 10, n (%) |
| Right foot positioned behind | 10 (3.4-10) | 37 (61) | 10 (10-10) | 17 (81) | 10 (9.6-10) | 9 (69) | 4 (2.25-10) | 8 (33) |
| Left foot positioned behind | 10 (4-10) | 34 (56) | 10 (10-10) | 17 (81) | 10 (7-10) | 8 (62) | 4.9 (2-10) | 8 (33) |
| Preferred foot behind | 10 (4-10) | 35 (57) | 10 (10-10) | 17 (81) | 10 (7-10) | 9 (69) | 4.8 (3.2-10) | 8 (33) |
| Nonpreferred foot behind | 10 (3.4-10) | 36 (59) | 10 (10-10) | 17 (81) | 10 (7-10) | 8 (62) | 3.7 (1.5-10) | 8 (33) |
Association between tandem stance and prescribed mobility aid status
For both preferred and nonpreferred foot behind, median (IQR) tandem stance time for participants assessed to be not requiring a walking aid was 10 seconds (10,10) and those prescribed a walking stick 10 seconds (7, 10) (see table 2). For those prescribed a 4-wheel walker stance time was 4.8 seconds (3.2, 10) for preferred foot and 3.7 seconds (1.5, 10) for nonpreferred foot behind. Hypothesis testing for the difference in medians showed a statistically significant difference between walking aid groupings for preferred foot behind (P=.02) and for nonpreferred foot behind (P=.01), with pairwise comparisons demonstrating the difference existing between the no aid and the 4-wheel walker groups for both foot combinations (P =.002). An inability to maintain tandem stance for 10 seconds significantly increased the odds of requiring a prescribed walking aid for preferred foot behind (OR, 5.19; 95% CI, 1.48-18.22; P=.01) and for nonpreferred foot behind (OR, 4.70; 95% CI, 1.34-16.45; P=.02). Sensitivity and specificity of the test when sustained for 10 seconds in relation to walking aid requirement for preferred foot behind and nonpreferred foot behind was 55% and 81% and 52.5% and 81%, respectively.
Association between tandem stance time and gait parameters
Gait parameters with no walking aid, measured over the 20-m course and listed by prescribed walking aid, and correlations between tandem stance test position time and each gait parameter are provided in table 3. Tandem stance test time displayed moderate positive correlations with stride length, gait speed, peak angle velocity, and maximal swing speed during the gait cycle (table 4).
Table 3.
Gait parameters measured during unassisted 20-m walk test categorized by the users prescribed walking aid
| Gait Parameter | Walking Aid Used for Assessment |
||||
|---|---|---|---|---|---|
| No Walking Aid (n=21), median (IQR) | Walking Stick (n=13), median (IQR) | 4-Wheel Walker (n=24), median (IQR) | P Value for Between-Group Difference | Explanation of Between-Group Difference | |
| Gait cycle time (s) | 1.12 (1.07-1.15) | 1.20 (1.10-1.25) | 1.21 (1.04-1.37) | .12 | Difference between no aid walking stick (P=.62) Difference between no aid and 4WW (P=.13) Difference between walking stick and 4WW (p=1.00) |
| Cadence (steps/min) | 106.98 (104.29-112.57) | 100.20 (96.19-108.84) | 99.68 (89.81-115.82) | .26 | Difference between no aid walking stick (P=.70) Difference between no aid and 4WW (P=.37) Difference between walking stick and 4WW (p=1.00) |
| Stance phase (% of cycle duration) | 61.53 (60.02-63.53) | 64.39 (62.04-66.19) | 63.30 (61.79-69.07) | .03 | Difference between no aid walking stick (P=.31) Difference between no aid and 4WW (P=.02) Difference between walking stick and 4WW (p=1.00) |
| Swing phase (% of gait cycle) | 38.47 (36.47-39.98) | 35.61 (33.81-37.96) | 36.41 (30.94-38.21) | .03 | Difference between no aid walking stick (P=.31) Difference between no aid and 4WW (P=.02) Difference between walking stick and 4WW (P>.99) |
| Double support (% of cycle duration) | 23.31 (19.89-27.13) | 28.74 (24.01-32.28) | 27.24 (23.51-38.16) | .02 | Difference between no aid walking stick (P=.30) Difference between no aid and 4WW (P=.02) Difference between walking stick and 4WW (p=1.00) |
| Stride length (m) | 1.23 (1.11-1.33) | 0.92 (0.87-1.14) | 0.82 (0.58-0.94) | <.01 | Difference between no aid and walking stick (P<.01). Difference between no aid and 4WW (P<.01). Difference between walking stick and 4WW (P=.03) |
| Speed (m/s) | 1.15 (0.90-1.24) | 0.82 (0.71-1.01) | 0.69 (0.50-0.83) | <.01 | Difference between no aid and walking stick (P=.02). Difference between no aid and 4WW (P<.01). Difference between walking stick and 4WW (P=.18) |
| Peak angle velocity (degrees/s) | 379.00 (337.30-390.30) | 332.40 (289.40-351.10) | 278.45 (228.35-335.40) | <.01 | Difference between no aid walking stick (P=.35) Difference between no aid and 4WW (P<.01) Difference between walking stick and 4WW (P=.10) |
| Max heel clearance (m) | 0.28 (0.26-0.29) | 0.28 (0.25-0.32) | 0.23 (0.20-0.26) | <.01 | Difference between no aid walking stick (p=1.00) Difference between no aid and 4WW (P=.02) Difference between walking stick and 4WW (P=.03) |
Abbreviation: 4WW, 4-wheel walker.
Table 4.
Correlation between tandem stance time and unassisted gait parameters
| Gait Parameter | Correlation Between Tandem Stance Time and Unassisted Gait Parameter ρ (P Value) |
|
|---|---|---|
| Preferred Foot Behind | Nonpreferred Foot Behind | |
| Gait cycle time (s) | −0.28 (.03) | −0.19 (.14) |
| Cadence (steps/min) | 0.27 (.04) | 0.18 (.15) |
| Stance phase (% of cycle duration) | −0.33 (<.01) | −0.37 (<.01) |
| Swing phase (% of gait cycle) | 0.33 (<.01) | 0.37 (<.01) |
| Double support (% of cycle duration) | −0.34 (<.01) | −0.37 (<.01) |
| Stride length (m) | 0.48 (<.01) | 0.58 (<.01) |
| Speed (m/s) | 0.50 (<.01) | 0.54 (<.01) |
| Peak angle velocity (degrees/s) | 0.50 (<.01) | 0.44 (<.01) |
| Max. heel clearance (m) | 0.42 (<.01) | 0.36 (<.01) |
Association between tandem stance test, retrospective falls, and falls risk
A total of 101 independent discreet fall episodes in the previous 12 months occurred, affecting 38 of the 61 participants. The number of falls per individual ranged from 0-10 (median, 1 [IQR, 0, 2]. The correlation between tandem stance time and number of falls was not significant and weak for preferred foot behind (P=.14, ρ=−0.19) but was significant and weak for nonpreferred foot behind (P=.01, ρ=−0.31). Furthermore, based upon dichotomized data on whether the tandem stance position was maintained for 10 seconds or less than 10 seconds, the difference in median tandem stance time between the participants who had fallen in the past 12 months and those who had not was significant for tandem stance testing with the nonpreferred foot behind position (P=.04) but not when the preferred foot was behind (P=.16). Almost 90% (34/38) of people who fell reported that they were not using a walking aid at the time of their fall. The correlation between tandem stance time and FROP-Com score for falls risk was negative and moderate (ρ=−0.52, P<.01 for preferred foot behind and ρ=− 0.58, P<.01 for nonpreferred foot behind).
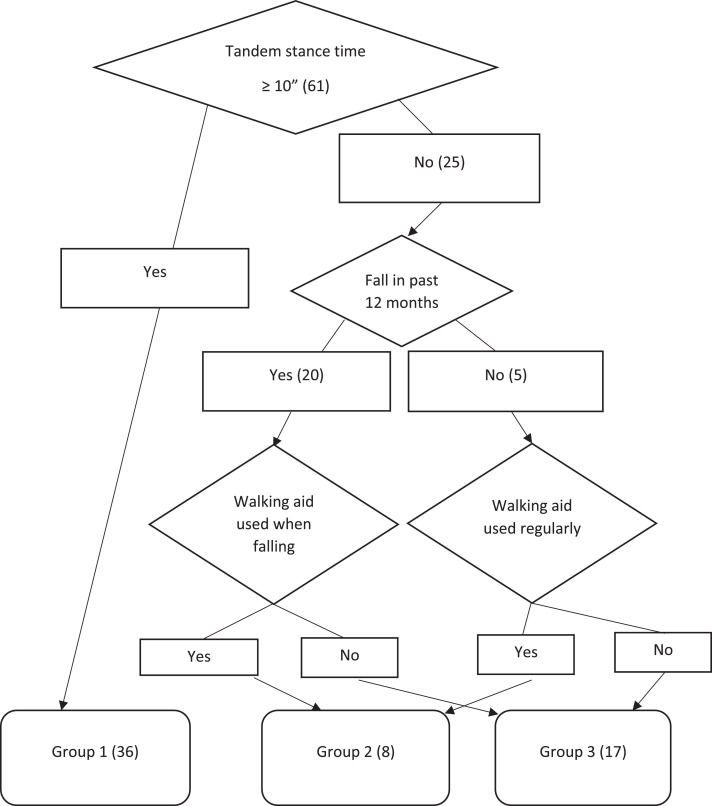
Association between tandem stance test and falling history
Twenty of 25 participants (80%) unable to maintain tandem stance for 10 seconds sustained a fall in the preceding 12 months compared with 18 of 36 participants (50%) able to sustain the position (fig 2 and table 5). The odds of having had a fall in the previous 12 months was 4 times higher if the participant was unable to maintain tandem stance with the nonpreferred foot behind for 10 seconds as opposed to being able to maintain for 10 seconds (OR, 4.00; 95% CI, 1.23-13.00; P=.02).
Fig. 2.
Grouping by tandem stance (nonpreferred foot behind), falls history, and walking aid use (N=61).
Table 5.
Falls history in the preceding 12 mo in relation to tandem stance performance with nonpreferred foot behind and walking aid use
| Group | Fell in Past 12-mo | Did Not Fall in Past 12 mo |
| Group 1: Able to maintain tandem stance for 10 s | 18 | 18 |
| Group 2: Unable to maintain tandem stance for 10 s and walking aid used | 3 | 5 |
| Group 3: Unable to maintain tandem stance for 10 s and walking aid not used | 17 | 0 |
Association between tandem stance test, falling history, and walking aid use history
Participants were divided into 3 groups based on their tandem stance time on the nonpreferred foot behind, falling history, and mobility aid use history (see fig 2). Table 5 shows the distribution of the participants in these groupings based on falls history. The odds of having had a fall in the preceding 12 months was 55 times higher if the participant was unable to maintain tandem stance with the nonpreferred foot behind for 10 seconds and had not used a walking aid as opposed to being unable to maintain for 10 seconds and having used a walking aid (OR, 55.00; 95% CI, 2.44-1238.46; P=.01).
Discussion
This study investigated the association between performance of the10-second tandem stance test; and (1) prescription of mobility aid, (2) gait parameters with prescribed walking aid, and (3) fall and walking aid use history. The 10-second tandem stance test showed associations with the need for mobility aid use with all 3 objectives.
In the absence of a criterion standard tool for mobility aid prescription, professional prescription of mobility aid was used as a reference standard. Individuals who were unable to hold a tandem stance position for 10 seconds were 5 times more likely require a walking aid. The 10-second tandem stance test appears to be a reasonable indicator of the need for a potentially balance impaired individual for walking aid prescription, although it is not sensitive enough to discriminate between walking aid requirements. The high specificity derived from the analysis of this test suggests that an inability to maintain for 10 seconds indicates the requirement for a walking aid is likely. However, this may be used with an additional assessment to suggest between walking stick and walking frame.
Placing preferred or nonpreferred foot behind did not demonstrate a difference in association with walking aid prescription or gait parameters. However, placing the nonpreferred foot behind displayed a stronger association than preferred foot behind for all fall-related outcome measures. This may indicate that this is a preferred method when using the tandem stance test with a view to prescribing an aid explicitly to mitigate against falls.
Subgrouping based on falls history and walking aid use history illustrates that walking aid use provides strong protection against falls because while every participant in group 3 fell in the past 12 months, only 38% in group 2 and 50% in group 1 sustained a recorded fall. This may indicate when capturing fall-related outcome measures on balance impaired individuals, including walking aid use history may be worthwhile. This may also indicate a greater need for patient education on the use of their walking aid.
Study limitations
In the absence of a criterion standard for walking aid prescription this study used clinician walking aid prescription as a reference standard. This carries an assumption that the current prescription of walking aids by health professionals is accurate and appropriate to each patient's need. Additional limitations includes using a sample of convenience, its small size, a single site, and absence of comparison with criterion standards such as the Berg or Dynamic Gait Index.
Future
Finding additional tools that may distinguish between walking stick and walking frame prescription to augment the 10-second tandem stance test may provide a more powerful method.
Implication of findings
Having a quick screening tool that does not require a large space or equipment may maximize efficiency, reduce time in assessment, and increase confidence of decision making in recommending mobility aid use.
Conclusions
The results of the 10-second tandem stance test are aligned with therapist prescription of walking aids, gait parameters, falls risk, falls, and history of walking aid use. This quick test can be easily administered in most settings and may be useful in guiding mobility aid prescription.
Supplier
-
a
PhysiGait Lab; Gait Up, Renens, Switzerland.
Footnotes
Presented on Rehabilitation Grand Rounds of New South Wales Health to the clinicians on June 30, 2021, via Skype. Otherwise, this study has not been presented elsewhere.
Supported in part by a 2018 NSW Rural Allied Health Postgraduate Scholarship under the Health Education and Training Institute. This funding supported the purchase of the gait analyzing system for the study.
Disclosures: none.
References
- 1.Hardi I, Bridenbaugh SA, Gschwind YJ, Kressig RW. The effect of three different types of walking aids on spatio-temporal gait parameters in community-dwelling older adults. Aging Clin Exp Res. 2014;26:221–228. doi: 10.1007/s40520-014-0204-4. [DOI] [PubMed] [Google Scholar]
- 2.Sudarsky L. Geriatrics: gait disorders in the elderly. N Engl J Med. 1990;322:1441–1446. doi: 10.1056/NEJM199005173222007. [DOI] [PubMed] [Google Scholar]
- 3.Verghese J, Holtzer R, Lipton RB, Wang C. Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci. 2009;64:896–901. doi: 10.1093/gerona/glp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Australian Commission on Safety and Quality in Health Care. Preventing falls and harm from falls in older people: best pratice guidelines for Australian community care 2009. Australian Commission on Safety and Quality in Healthcare, editors. 2009 Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/Guidelines-COMM.pdf. Accessed December 30, 2021. [Google Scholar]
- 5.Australian Commission on Safety and Quality in Health Care. Preventing falls and harm from falls in older people in Austalian hospitals 2009. Australian Commission on Safety and Quality in Healthcare, editors. 2009 Available at: https://www.safetyandquality.gov.au/sites/default/files/migrated/Guidelines-HOSP.pdf. Accessed December 30, 2021. [Google Scholar]
- 6.Nandapalan V, Smith CA, Jones AS, Lesser TH. Objective measurement of the benefit of walking sticks in peripheral vestibular balance disorders, using the Sway Weigh balance platform. J Laryngol Otol. 1995;109:836–840. doi: 10.1017/s0022215100131457. [DOI] [PubMed] [Google Scholar]
- 7.Resnik L, Allen S, Isenstadt D, Wasserman M, Iezzoni L. Perspectives on use of mobility aids in a diverse population of seniors: implications for intervention. Disabil Health J. 2009;2:77–85. doi: 10.1016/j.dhjo.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gell N, Wallace R, LaCroix A, Mroz T, Patel K. Mobility device use in older adults and incidence of falls and worry about falling: findings from the 2011-2012 National Health and Aging Trends Study. J Am Geriatr Soc. 2015;63:853–859. doi: 10.1111/jgs.13393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen SM, Foster A, Berg K. Receiving help at home: the interplay of human and technological assistance. J Gerontol B Psychol Sci Soc Sci. 2001;56:S374–S382. doi: 10.1093/geronb/56.6.s374. [DOI] [PubMed] [Google Scholar]
- 10.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 11.Hile ES, Brach JS, Perera S, Wert DM, VanSwearingen JM, Studenski SA. Interpreting the need for initial support to perform tandem stance tests of balance. Phys Ther. 2012;92:1316–1328. doi: 10.2522/ptj.20110283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berg K, Wood-Dauphinee S, Williams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311. [Google Scholar]
- 13.Fregly AR, Smith MJ, Graybiel A. Revised normative standards of performance of men on a quantitative ataxia test battery. Acta Otolaryngol. 1973;75:10–16. doi: 10.3109/00016487309139631. [DOI] [PubMed] [Google Scholar]
- 14.Jonsson E, Seiger A, Hirschfeld H. Postural steadiness and weight distribution during tandem stance in healthy young and elderly adults. Clin Biomech (Bristol, Avon) 2005;20:202–208. doi: 10.1016/j.clinbiomech.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Rossiter-Fornoff JE, Wolf SL, Wolfson LI, Buchner DM. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and injuries: cooperative studies of intervention techniques. J Gerontol A Biol Sci Med Sci. 1995;50:M291–M297. doi: 10.1093/gerona/50a.6.m291. [DOI] [PubMed] [Google Scholar]
- 16.Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci. 2001;56:M644–M649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- 17.Dick JP, Guiloff RJ, Stewart A, et al. Mini-Mental State Examination in neurological patients. J Neurol Neurosurg Psychiatry. 1984;47:496–499. doi: 10.1136/jnnp.47.5.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rougier PR, Marsande J, James M, Brachet M. Biomechanical study of tandem stance in healthy young adults: effects of weight-bearing and limb dominance. J Mot Behav. 2019;51:603–609. doi: 10.1080/00222895.2018.1545217. [DOI] [PubMed] [Google Scholar]
- 19.Mariani B, Hoskovec C, Rochat S, Bula C, Penders J, Aminian K. 3D gait assessment in young and elderly subjects using foot-worn inertial sensors. J Biomech. 2010;43:2999–3006. doi: 10.1016/j.jbiomech.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Mariani B, Rochat S, Bula CJ, Aminian K. Heel and toe clearance estimation for gait analysis using wireless inertial sensors. IEEE Trans Biomed Eng. 2012;59:3162–3168. doi: 10.1109/TBME.2012.2216263. [DOI] [PubMed] [Google Scholar]
- 21.Russell MA, Hill KD, Blackberry I, Day LM, Dharmage SC. The reliability and predictive accuracy of the Falls Risk for Older People in the Community assessment (FROP-Com) tool. Age Ageing. 2008;37:634–639. doi: 10.1093/ageing/afn129. [DOI] [PubMed] [Google Scholar]