Abstract
Submaximal exercise testing can be a feasible alternative to maximal testing within special populations to safely predict fitness levels; however, submaximal exercise testing has not been well-validated for use during pregnancy. The purpose of this study was to determine the concurrent validity of the 6-minute walk test (6MWT) and the YMCA submaximal cycle test (YMCAT) to predict VO2max in physically active women during mid-pregnancy. Thirty-seven (n=37) pregnant women (22.1 ±1.4 weeks gestation) and ten (n=10) non-pregnant women participated in the study. Participants completed a graded maximal treadmill test at one visit to measure maximal oxygen consumption (VO2max), then participants completed the 6MWT and YMCAT in randomized order during a separate visit. The predicted VO2max from each submaximal test were compared to the measured VO2max from the treadmill test to assess the validity of these tests during pregnancy. Among pregnant women, predicted VO2max from the YMCAT was not correlated to the measured VO2max (r=0.14, p=0.42), and the predicted VO2max from the 6MWT was only moderately correlated (r=0.40, p=0.016) to the measured VO2max. Among non-pregnant women, the predicted VO2max values from both the YMCAT and the 6MWT had strong correlations with the measured VO2max values (YMCAT: r=0.71, p=0.02; 6MWT: r=0.80, p=0.006). Neither test demonstrated concurrent validity among the pregnant sample. The main finding is that the YMCAT is not a valid method to estimate VO2max during mid-pregnancy (likely due to physiological changes in heart rate during pregnancy). The 6MWT has potential to be used clinically for estimating fitness as actual and predicted values did positively correlate and it is not dependent on heart rate responses to exercise. However, if a precise measure of fitness is needed, then neither test appears to have strong validity for use during mid-pregnancy.
Keywords: pregnancy, exercise testing, VO2max
INTRODUCTION
Maximal oxygen uptake (VO2max) upon graded exercise testing is the gold standard for measuring cardiorespiratory fitness (4, 5). However, directly measuring VO2max is not always feasible, particularly in higher-risk and/or special populations (e.g. pregnant women). Direct VO2max measurement also involves expensive machinery (metabolic cart, treadmill, cycle ergometer), physician oversight in higher-risk and/or special populations, trained personnel, and the ability of the test subject to exercise until volitional fatigue. Therefore, the ability to accurately predict VO2max using submaximal protocols is important.
Many submaximal tests can reasonably estimate or predict VO2max in apparently healthy individuals including the 6-and-12 minute walk tests, The Rockport One-Mile Fitness Walking Test, the Astrand-Rhyming cycle test, the YMCA cycle ergometry test, step tests, and submaximal treadmill protocols(32). However, none of these tests have been validated among pregnant women. Mottola et al. provided a validated equation for predicting VO2max during mid-pregnancy (16-22 weeks) (r=.71) using a progressive treadmill exercise test(28). Unfortunately, this submaximal protocol still requires expensive equipment and trained personnel to conduct the testing, limiting its utility for this clinical population.
The 6-minute walk test (6MWT) and YMCA submaximal cycle test (YMCAT) are two widely used submaximal tests that may be more practical tests for predicting cardiorespiratory fitness during pregnancy. The 6MWT is one of the most popular clinical exercise tests in other populations (e.g. heart disease, lung disease, hypertension, older adults) (22). The 6MWT evaluates integrated responses of all body systems involved in exercise including pulmonary, cardiovascular, neuromuscular, circulatory, and metabolic systems (21), which are all systems impacted by pregnancy. The 6MWT has been used among wide variety of populations to evaluate functional status as well as evaluate the effectiveness of medical interventions (21), and it may also serve useful to evaluate health status and effectiveness of exercise interventions/prescriptions during pregnancy. Fortunately, it is easy to administer (only requires a 100ft hallway and technicians do not need any advanced training), easy-to-tolerate by patients, and more reflective of activities of daily living than other tests (22, 40).
Further, The YMCAT is another popular submaximal test that utilizes the extrapolation method (heart rate and workload points are obtained and extrapolated to age-predicted maximal heart rate and from that, VO2max is predicted from maximal workload)(4). Previous literature suggests the extrapolation method is the best way to predict fitness among pregnant populations. Sady et al. concluded that “extrapolating the VO2-HR curve to an estimated maximal heart rate is the most accurate method of predicting VO2max in pregnant women”(37). In addition, stationary cycle exercise provides a safe modality for potentially high-risk patients who may be at risk for falling, and the YMCAT can be performed with minimal equipment and personnel training.
Validating one or both of these tests for use in pregnant populations is clinically important. Health care providers, particularly exercise professionals, need a validated test to predict the cardiorespiratory fitness and health status of pregnant patients. This will allow for appropriate individualized exercise prescriptions in order to maximize the well-established benefits of exercise in both the mother and her offspring (11, 34). Self-reported physical activity assessments should not be used to guide exercise prescriptions as they are subject to recall bias as well as require an understanding of exercise-related language (e.g. “moderate intensity”, “leisure time”)(38), and they do not correlate well with cardiorespiratory fitness in young adults(21). Therefore, prescriptions based on self-report would likely be erroneous. Further, objective assessments of cardiorespiratory fitness (such as maximal or submaximal exercise tests) are better alternatives to self-reported physical activity levels, as cardiorespiratory fitness is not subject to bias and is can be correlated to long-term health outcomes(39). Objective cardiorespiratory fitness tests will provide a stronger basis for designing personalized exercise programs for pregnant patients; thus, the ability to accurately assess cardiorespiratory fitness levels during pregnancy is important.
Therefore, the purpose of this study was to determine the concurrent validity of the 6MWT and the YMCAT to predict VO2max in physically-active women during mid-pregnancy.
METHODS
Experimental Approach to the Problem
In order to determine the validity of the 6MWT and the YMCAT, predicted VO2max values from each of these tests were compared to the gold standard, a measured VO2max from a treadmill test to volitional fatigue. A control group of age and activity level matched non-pregnant women were included to demonstrate the established validity of these two submaximal tests among non-pregnant women.
Subjects
All study procedures were approved by the University’s Institutional Review Board. All participants were informed of the benefits and risks of study participation prior to signing an institutional review board approved informed consent document. Participants were recruited from local obstetric outpatient clinics, campus-wide emails at the University, and pregnancy fairs sponsored through the local hospital. Inclusion criteria included: obstetric provider written consent for study participation, confirmed singleton viable pregnancy with no identified fetal abnormalities (as determined by routine standard of care ultrasonography), age 18-44 years, self-reported physically active lifestyle (i.e. exercise for ≥30 minutes on 3 or more days per week) at the time of recruitment, and between 18-24 weeks pregnant at time of study participation. The gestational age of 18-24 weeks was chosen due to the greatly reduced risk of miscarrying(44), in addition to the fact that this is a time point during pregnancy in which health care providers may wish to prescribe exercise(36). Exclusion criteria included: restrictive lung disease, incompetent cervix/cerclage, multiple gestation at risk for premature labor, persistent 2nd trimester bleeding, ruptured membranes, preeclampsia/pregnancy-induced hypertension, hemodynamically-significant heart disease, inability to provide voluntary informed consent, currently using illegal drugs (cocaine, methamphetamine, opiates, etc.), current smoker, or any other reason why exercise may be contraindicated.
In addition, ten (n=10) non-gravid women participated in identical study procedures and served as a control group to demonstrate the validity of these two submaximal tests among non-gravid women. Inclusion criteria included: age 18-44 years and self-reported physically active lifestyle (i.e. exercise for ≥30 minutes on 3 or more days per week). Control participants were excluded if there were any contraindications to exercise testing.
Procedures
Each participant completed two exercise sessions (maximal and submaximal) in randomized order between 18 and 24 weeks gestation. All exercise sessions took place in the Exercise Physiology Lab of the Health Sciences Building.
Maximal Testing Session:
To assess VO2max, participants completed a graded exercise test according to the Bruce Protocol on a treadmill with the initial settings at 1.7 mph and grade at 10%. Both speed and grade were increased incrementally according to the established protocol every three minutes until volitional fatigue. During the test, heart rate was monitored via a chest mounted heart rate monitor (Polar, USA) and oxygen consumption and carbon dioxide (CO2) production were assessed using the K4b2 portable metabolic system (COSMED, USA)(15). The portable metabolic analyzer was used to determine VO2max and respiratory exchange ratio (RER). Rating of Perceived Exertion (RPE) was assessed at each stage during the exercise testing using the Borg Scale6-20 rating system. Participants were informed that they could stop the test at any time, but they were encouraged to reach maximal effort. All maximal tests were conducted to volitional exhaustion or the participant requesting to stop or rest by straddling the belt. In order to ensure maximal effort was achieved, heart rate, RPE, RER, lactate (pregnant group only), and participant self-report were obtained. Blood pressure was assessed before the test, as well as immediately after, and 15 minutes post-test completion. In the pregnant group only, blood was drawn via intravenous catheter before and immediately post-exercise to assess glucose and lactate levels. All pregnancy study visits were supervised by a nurse practitioner and completed in close proximity to the hospital for safety.
Submaximal Testing Session:
At this session, participants completed the 6MWT and YMCAT. Half of the participants completed the YMCAT first and the other half completed the 6MWT first. Between tests, participants rested quietly until heart rate (HR) and blood pressure (BP) returned to baseline values (~10-20min). In order to make the study more feasible for participants, both submaximal tests were performed on the same day in randomized order; however, both tests targeted submaximal effort and all vitals returned to baseline during the rest period before the second test was performed.
For the 6MWT, previously cited procedures were followed (7, 22). Briefly, participants began in a chair while baseline HR and BP were taken. Two cones were set up 30 meters apart. Participants were instructed to walk between the cones for six minutes as fast as they were able to without running. The total distance walked during the six minutes was measured and recorded. Immediately post-test, the patient was seated and vitals were taken again.
VO2max was predicted by using the equation developed for healthy working-aged adults(7) [Equation 1].
| [1] |
For the YMCAT protocol(32), the Monark cycle ergometer was adjusted for each individual so that there was a slight bend in the knee when the participant was sitting on the cycle with their foot centered on the pedal with the pedal in the bottom position. A standard load (1.5 kg) was applied to the flywheel and all participants cycled at 50 RPM for three minutes. Based on HR responses, additional stages and workloads were applied in order to achieve two stages of cycling above 110 beats per minute but below 85% of age-predicted maximum heart rate. These two submaximal workloads were then extrapolated to the maximal workload in order to predict VO2max.
Statistical analysis
Sample size for the pregnant group was based on data from studies synthesized by Ross et al., who found that VO2max and the 6MWT were moderately correlated at R2=.55 or higher in other clinical populations tested to date(35). Using a normal, bivariate correlation model, an alpha value of .05, required a sample size of 20 participants in order to adequately power our study at β=0.95. However, a larger sample was utilized as the original power calculation was based on data from a non-pregnant population due to lack of data on the relationship between predicted and actual VO2max values for either test among pregnant women. A larger sample would be more apt to detect the level of significance in this untested population.
Demographic and exercise characteristics were compared between pregnant and control participants using independent samples t-tests for continuous variables or chi-square tests for categorical variables. To estimate the concurrent validity of predicted VO2max values from each of the two submaximal tests in comparison to the gold standard, measured VO2max values from the maximal graded treadmill test using the Bruce Protocol, Pearson Product Moment Correlation Coefficients were used. Paired t-test were also conducted to compare actual and predicted values for each test for pregnant and non-pregnant control groups. Because assessments can correlate but not necessarily agree, Intra-Class Correlation Coefficients (ICC) were used to analyze agreement between the actual and predicted values. A model 3,k ICCs (ICC3,1was used to determine if each test of estimated VO2max produced comparable results with the measured VO2max ). Reference values used for the interpretation of ICC values for concurrent validity were as follows: < 0.50, poor; .50-.75, moderate; > 0.75 good(2). Confidence intervals (95% CI) were calculated around the ICC point estimate. To further examine the agreement between predicted and measured values of VO2max, the 95% limits of agreement (LOA) from Bland Altman Plots were calculated using the formula 95% LOA = MD * 2SDd(3) where MD is the mean difference between measures of VO2max and SDd is the standard deviation of the difference scores between VO2max measures(6).
Data entry, export, and cleaning were conducted using REDcap software(19). All data analyses were done using SPSS (Version 24) and the alpha level for statistical significance was set at p <0.05.
RESULTS
Demographic characteristics on all participants are reported in Table 1. With the exception of BMI at the time of the study and education level, there were no differences in demographic characteristics between the pregnant and non-pregnant women. However, when pre-pregnancy BMI in the pregnant group and BMI in the non-pregnant control group were compared, there was no difference. Thus, the women had similar body types; the reason for the difference in BMI at the time of the study appeared to be due to gestational weight gain (i.e. pregnancy).
Table 1.
Demographic characteristics (mean ±SD; number of women (%))
| Pregnant (n=37) | Controls (n=10) | p-value | |
|---|---|---|---|
|
| |||
| Age (years) | 31.0±3.9 | 29.7±9.6 | 0.53 |
|
| |||
| Gestation Age (weeks) | 22.1 ±1.4 | N/A | |
|
| |||
| BMI (kg/m2) | 26.1±3.8 | 23.2±3.8 | 0.03┼ |
|
| |||
| Pre-pregnancy BMI (kg/m2) | 23.5± 3.3 | N/A | |
|
| |||
| Weight (kg) | 71.0±9.6 | 66.0±9.3 | 0.15 |
|
| |||
| Height (cm) | 165.3±8.9 | 168.4±7.2 | 0.31 |
|
| |||
| Resting Systolic Blood Pressure (mmHg) | 118.7±10.0 | 113.6±9.1 | 0.17 |
|
| |||
| Resting Diastolic Blood Pressure (mmHg) | 70.2±6.9 | 72.7±11.0 | 0.40 |
|
| |||
| Resting Heart Rate (bpm) | 80.1.3±10.3 | 76.3±14.5 | 0.44 |
|
| |||
| Baseline Glucose (mg/dL) | 100.5±17.9 | DNC | |
|
| |||
| Ethnicity | 0.78 | ||
| Caucasian | 36 (97%) | 10 (100%) | |
| Hispanic | 1 (3%) | 0 (0%) | |
|
| |||
| Education | 0.02 | ||
| Some college | 1 (2.7%) | 3 (30%) | |
| Bachelor’s degree | 18 (48.7%) | 2 (20%) | |
| Post graduate degree | 17 (45.9%) | 5 (50%) | |
| Unknown | 1 (2.7%) | 0 (0%) | |
|
| |||
| Exercise Level | 0.09 | ||
| None | 1 (2.7%) | 0 (0%) | |
| Once a week | 5 (13.5%) | 1 (10%) | |
| 2-3 times per week | 15 (40.5%) | 2 (20%) | |
| 4-6 times per week | 14 (37.8%) | 4 (40%) | |
| Daily | 1 (2.7%) | 3 (30%) | |
| Unknown | 1 (2.7%) | 0 (0%) | |
DNC: data not collected
When comparing pre-pregnancy BMI in the pregnancy group to BMI in the control group, there was no difference in BMI (p=0.81).
Thirty-seven (n=37) pregnant women (gestation age: 22.1 ±1.4 weeks, age: 31.0±3.9 years, BMI at time of study visit: 26.1±3.8 kg/m2) participated in the study. All women were considered physically active (via self-report) at the time of recruitment (i.e. exercise for ≥30 minutes on 3 or more days per week) which ensured they met inclusion criteria. However, seven women reported only exercising 0-1 time per week at the time of study participation, suggesting some women reduced ongoing exercise levels in the time between recruitment and study participation which is likely due to the rapid growth and change that occur during the second trimester of pregnancy (Table 1). Among pregnant women, predicted VO2max from the YMCAT was not correlated to the measured VO2max (r=0.14, p=0.42) (Figure 1). VO2max predicted from the 6MWT and the measured VO2max were moderately correlated during pregnancy (r=0.40, p=0.016) (Figure 2).
Figure 1.
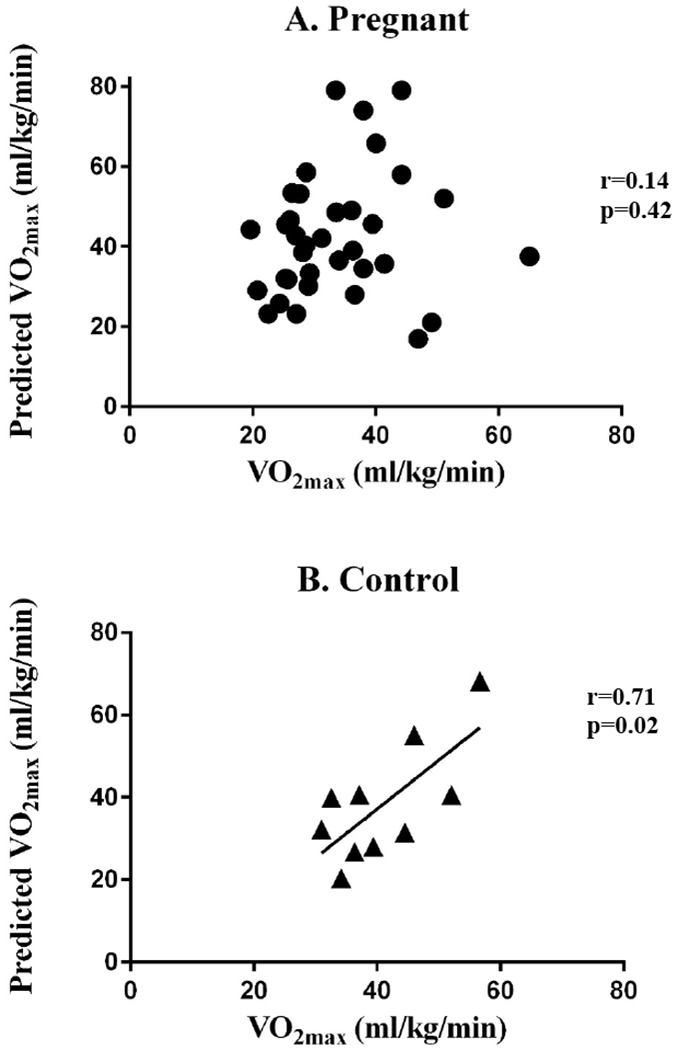
Predicted VO2max and measured VO2max for the YMCA submaximal cycle test were not correlated among pregnant women (A), but were significantly correlated among control women (B).
Figure 2.
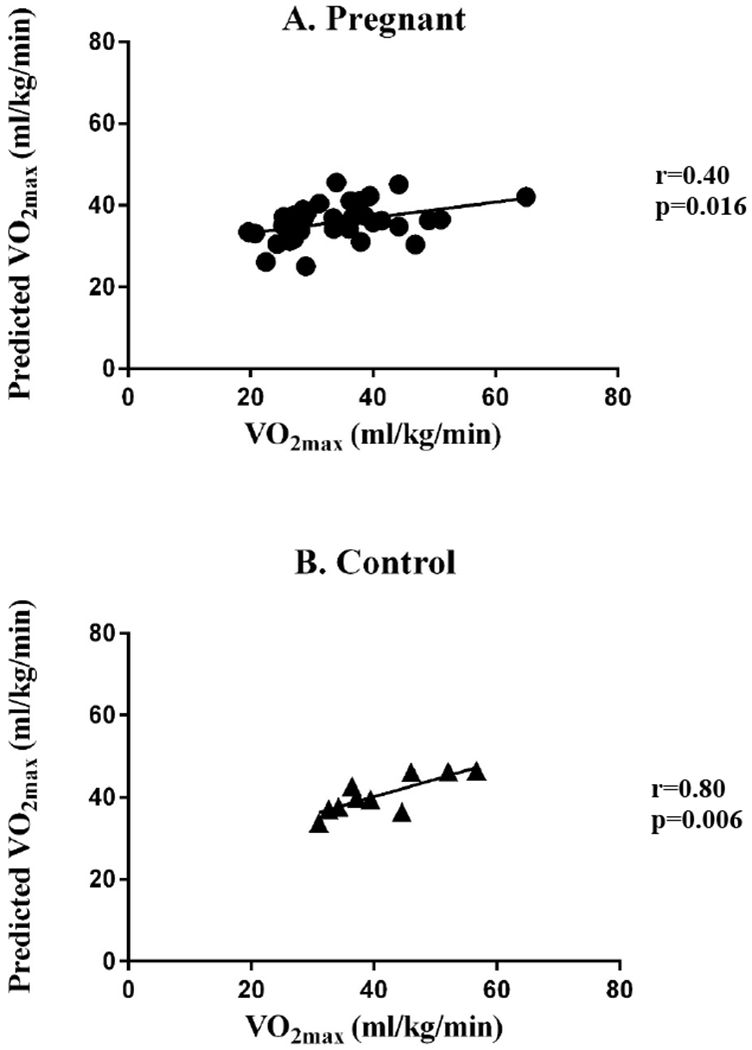
Predicted VO2max and measured VO2max for the 6-minute walk test were significantly correlated among pregnant (A) and control women (B). The correlation between actual and predicted VO2max was stronger among control women compared to pregnant women (r=0.80 vs. r=0.40, respectively).
Ten (n=10) non-pregnant women (age: 29.7 ± 9.6 years, BMI: 23.2±3.8 kg/m2) also participated. In this group, the predicted VO2max values from both the YMCAT and the 6MWT had strong correlations with the measured VO2max values (YMCAT: r=0.71, p=0.02 (Figure 1); 6MWT: r=0.80, p=0.006 (Figure 2)).
Paired t-tests revealed a statistical difference between predicted VO2max from the YMCAT and measured VO2max values for the pregnant group (p=0.004), but not for the control group (p=0.42). For the 6MWT, t-tests revealed no statistical difference between predicted VO2max values and measured VO2max values (pregnant group: p=0.21, control group: p=0.81).
Concurrent validity of measured VO2max values and estimated VO2max values from 6MWT were moderate for controls (ICC=.661) (95% CI for the ICC: 0.099, 0.904) and poor for the pregnant group (ICC=.301) (95% CI for the ICC:−0.032,0.573). Concurrent validity of measured VO2max values and estimated VO2max values from YMCAT were moderate for controls (ICC=.629) (95% CI for the ICC: 0.043, 0.893) and poor for the pregnant group (ICC=.133) (95% CI for the ICC: −0.210, 0.447). The 95% Limits of Agreement (LOA) from Bland-Altman plots suggest that the difference between VO2max values estimated with the 6MWT and measured from maximal graded treadmill test measurements varied between −10.7 to 11.6 ml/kg/min for controls and −19.54 to 15.74 ml/kg/min for the pregnant group. The 95% LOA suggest that the difference between VO2max values estimated with the YMCAT and measured from maximal graded treadmill test measurements varied between −17.1 to 22.5 ml/kg/min for controls and −43.4 to 24.8 ml/kg/min for the pregnant group.
Exercise data for both groups can be found in Table 2. Pregnant women had lower measured VO2max values during the maximal exercise test (p=0.04) and predicted VO2max values during the 6MWT test (p=0.005) compared to non-pregnant women. In addition, maximal heart rates during the maximal treadmill test were lower among pregnant women compared to non-pregnant women (p=0.003). Further, when pregnant women who did not achieve ≥85% of age-predicted maximal heart rate (n=7) were removed and the analysis was re-run, the correlation values were similar (measured VO2max and predicted VO2max from the YMCAT: r=0.17, p=0.37; measured VO2max and predicted VO2max from the 6MWT: r=0.43, p=0.17). In addition, there were no differences in RPE or RER between the two groups, and both RPEs and RERS would suggest all participants achieved maximal effort.
Table 2.
Exercise Characteristics (mean ± SD)
| Pregnant | Controls | p-value | 95% CI of mean difference | |
|---|---|---|---|---|
| VO2max (ml/kg/min) | 33.7±9.6 | 41.0±8.6 | 0.04 | 0.52 – 14.1 |
| HRmax (bpm) | 167.6±12.7 | 182.0±11.0 | 0.003 | 5.5 – 24.1 |
| RPEmax | 17.3±1.8 | 17.9±1.7 | 0.39 | −0.72 – 1.9 |
| Lactatemax (mmol/L) | 6.7± 2.5 | DNC | ||
| Glucosemax (mg/dL) | 86.7±18.9 | DNC | ||
| RERmax | 1.20±0.19 | 1.24±0.13 | 0.62 | −0.19 - 0.1 |
| 6MWT predicted VO2max (ml/kg/min) | 35.7±4.5 | 40.6±4.6 | 0.006 | 1.60 – 8.2 |
| YMCA predicted VO2max (ml/kg/min) | 42.9±15.8 | 38.3±14.2 | 0.43 | −15.9 – 6.7 |
DNC: data not collected
CI: confidence interval
DISCUSSION
The purpose of this study was to determine the validity of the 6MWT and the YMCAT to predict VO2max in physically active women during mid-pregnancy.
The main findings of this study are that neither test appear to be valid for use during mid-pregnancy. For both tests, the ICCs for the pregnant group were poor while it was moderate for the controls. The range of 95% LOA were much larger for the pregnant group for both tests, suggesting poor agreement between predicted and measured values. To elaborate, the 95% LOA for the 6MWT and the YMCAT among pregnant women were >20 ml/kg/min. Clinically, a test that only ensures a value within 20 ml/kg/min from the mean is not very valuable as a difference of >20ml/kg/min may change one’s cardiorespiratory fitness level classification from very poor to superior.
Health care providers, specifically exercise professionals, need an accurate submaximal test to predict cardiorespiratory fitness during pregnancy. Assessments to objectively measure fitness will provide a much stronger basis for patients and providers to build an exercise prescription and predict future health outcomes such as cardiovascular health, diabetes risk, and even longevity(10, 13). Accurate fitness assessments will allow providers to tailor their patients’ exercise prescriptions in order to maximize the well-established benefits of exercise in both the mother and her offspring(11, 34). Our findings suggest the 6MWT, while not ideal, did have a positive correlation with actual VO2max values. The 6MWT could still be used in clinical settings when an estimated value can be used in place of a self-reported assessments. Values from the this test could also be useful when the objective is to measure the changes in cardiorespiratory fitness over time within one person as their effort, age, heart rate responses, and understanding of the test instructions are more likely to be consistent from test-to-test (e.g. if a pregnant woman wants to begin an exercise routine and assess her cardiorespiratory fitness at multiple time points over the course of her pregnancy). Demonstrating to a pregnant woman an improvement in fitness, despite progression of their pregnancy, could prove to be a powerful motivational tool. In such a case, the ability to accurately assess the improvements in fitness are more important than the validity of the fitness test itself. Despite several situations in which the 6MWT could be useful, our results suggest caution should be taken using either test to draw conclusions regarding fitness (based on estimated VO2max values) in clinical settings or within clinical research studies.
The 6MWT is easy to administer and requires minimal testing equipment. The only required equipment is a hallway or walkway (30m), cones or markers, and a timer. It is also a very safe test for potentially at-risk populations (e.g. heart disease, lung disease, hypertension), and it is widely used in clinical settings among individuals with a wide variety of conditions and medical co-morbidities(9). Thus, it has potential to be used clinically during pregnancy, even among high-risk women with significant medical concerns such as obesity, diabetes, or hypertension. These women are experiencing high-risk pregnancies making a VO2max test even less feasible; however, future studies to determine the validity of these tests among overweight/obese, diabetic, and/or hypertensive pregnant women are warranted to determine their generalizability for these groups. The benefits of validating these tests among high-risk pregnant populations could be substantial as they have the most to gain from a personalized exercise prescription, as many studies support the maternal and fetal benefits of beginning or continuing exercise in the presence of risk factors such as diabetes, obesity, and/or hypertension (3, 12, 14, 18, 31, 34, 42). Obesity, diabetes, and hypertension are three very common pregnancy complications that may be modified with an exercise intervention(43).
The predicted VO2max from the 6MWT had a moderate correlation (r=0.40) with measured VO2max. In previous studies, the 6MWT has significantly correlated with VO2peak in patients with heart failure (r=.64, r=.59, r=.59, r=.58, r=.78)(9, 17, 23, 26, 33), end-stage lung disease (r=.69)(8), pulmonary hypertension (r=.68)(27), chronic obstructive pulmonary disorder (r=.55)(41), and dilated cardiomyopathy (r=.69)(45). The correlation between actual and predicted VO2max was much weaker among in our pregnant women than the previously studied populations (r=0.55-0.78), as well as among the control group in the present study (r=0.80). However, due to the moderate validity and the lack of other validated submaximal exercise tests during pregnancy, the 6MWT still likely has clinical utility among women with uncomplicated pregnancies.
We suspect that the YMCAT may be even less accurate for predicting VO2max during pregnancy because it is well-established that heart rate responses during exercise are altered during pregnancy(20, 24, 25, 28). The YMCAT relies on heart rate responses to workloads to determine the subsequent stage as well as uses steady state heart rates in each stage to extrapolate the heart rate/work rate relationship in order to predict VO2max. Pregnancy has been shown to alter the linear relationship between heart rate and workload(24), it is logical that the extrapolation method used among non-pregnant populations would not be accurate among pregnant women. However, this was an important test to study as Sady et al. concluded that extrapolating the VO2-Heart Rate curve to an estimated maximal heart rate was the most accurate way to predict VO2max in pregnancy(37). On the contrary, our findings suggest that methods relying heavily on heart rate responses to exercise loads may not be the best choice for predicting fitness among pregnant women. Our results agreed with Lotgering et al. who determined several different methods used to estimate VO2max (Astrand’s nomogram, linear extrapolation to maximal heart rate of the linear regression line between heart rate and VO2 measured at submaximal intensities, and by linear regression line of the individual values of heart rate and VO2 measured between 30 and 70% of VO2max) cannot accurately predict measured VO2max during pregnancy(24). Although the YMCAT is one of the most popular assessment methods for VO2max prediction among non-pregnant populations (32)(1), it does not appear to be a useful assessment during pregnancy.
Of note, the pregnant women had lower overall cardiorespiratory fitness levels compared to non-pregnant women, as well as lower maximal heart rates during the maximal treadmill test (which is consistent with previous research(25)). These findings could suggest that the explanation for the lack-of correlation between actual and predicted VO2max tests among pregnant women are due to the pregnant women not reaching a true physiological max. Fortunately, no differences were detected in rating of perceived exertion (RPE) or respiratory exchange ratio (RER) between the two groups. Further, among pregnant women (and control women) RER values were ≥1.1mmol/L and RPE values were ≥17(16), both of which would indicate our pregnant participants reached maximal effort(16). In addition, mean lactate values for the pregnant women were 6.7mmol/L, and recent data by Edvardsen et al. suggests that for females of childbearing age a lactate concentration of 7.0mmol/L signifies maximal effort(16). Thus, pregnant females with a mean lactate value of 6.7mmol/L, as found in the present study, would be at or very near maximal capacity. Due to the significant difference in maximal heart rates between pregnant women and controls, all women who did not reach ≥85% of age-predicted maximal heart rate (another criteria for determining VO2max) were removed and correlations were performed a second time. Even with these women excluded, the relationships between actual and predicted VO2max from both the YMCA test and the 6-minute walk tests did not change substantially among pregnant women (Measured VO2max and predicted VO2max from the YMCAT: r=0.17, p=0.37; Measured VO2max and predicted VO2max from the 6MWT: r=0.43, p=0.17), and all other comparisons were similar between groups with these women excluded. Taken together, these data suggest our participants did reach their maximal effort, and that the lower maximal heart rate does not explain the lack of correlation between actual and predicted VO2max values among pregnant women. Our findings also suggest maximal heart rate responses may be blunted during pregnancy, which is consistent with previous studies(25).
A strength of the present study is that identical procedures were performed by a group of non-gravid women, and we found that both submaximal tests had similar accuracies in predicting VO2max to what has been previously reported in the literature among non-pregnant women(32). This finding suggests the lack of (or reduced) associations between actual and predicted VO2max values among pregnant women in our study are likely due to physiological changes associated with pregnancy and not methodological issues with our study protocol. Another strength of the present study is that successful maximal exercise testing was conducted safely in low-risk pregnant women during mid-pregnancy. No adverse maternal or fetal/infant outcomes were reported by any participants as a result of this testing.
A limitation of the present study is that pregnant women were assessed during mid-pregnancy (2nd trimester), so our results are not generalizable to all trimesters of pregnancy as physiological changes, including heart rate, change throughout the entire pregnancy. However, we believe this is an important time for assessment as it is when many women are likely to initiate an exercise program as many of the risks and discomforts of the first trimester are over yet the mechanical barriers to exercise during late pregnancy are not yet of concern. Further, this is the time point in which providers initiate gestational diabetes screening, and often times, exercise may be part of the recommended plan for improving sugars during pregnancy. Another limitation that restricts the generalizability of our results is that we only tested physically active pregnant women. However, this was an important inclusion criteria for the current study as we felt it was safer to conduct maximal exercise testing with pregnant women who were accustomed to the physiological stresses of exercise. Another limitation is that the pregnant group was slightly less fit and had lower maximal heart rates than controls; however, a secondary analysis was performed to ensure these differences did not have a significant impact on the relationships reported. An additional limitation is conducting the two submaximal tests on the same day (in order to lower participant burden), as this may have influenced results; however, both tests were submaximal, performed in randomized order, and caution was taken to ensure vitals returned to normal between tests to minimize issues with the quality of the data collection.
Healthcare providers need a safe and feasible submaximal exercise test that accurately measures cardiorespiratory fitness. This will allow them to tailor their patients’ exercise prescriptions in order to maximize the well-established benefits of exercise (11, 29, 30). In addition, healthcare providers need a test they can safely perform with high-risk pregnancies, which is common among U.S. women give the high prevalence of obesity, diabetes, and high blood pressure during pregnancy (1, 4, 21). Not only are these women experiencing high-risk pregnancies (making a VO2max test less feasible), but this population has the most to gain from a personalized exercise prescription, as many studies support the maternal and fetal benefits of beginning or continuing exercise in the presence of risk factors(14, 18, 31, 34, 42). Therefore, an important future direction of this research is to test the validity of submaximal exercise testing among women with relative contraindications to exercise during pregnancy such as obesity, diabetes, and/or hypertension. The 6MWT be useful among these populations as these conditions may be the same or mimic other conditions in which the 6MWT has been indicated (21). Findings from the present study suggest that neither submaximal test should be used for accurately predicting cardiorespiratory fitness among pregnant women.
PRACTICAL APPLICATIONS
Exercise during pregnancy is an important topic among health care providers, and research suggests it is both safe and effective for improving maternal and infant health. The basis for any exercise prescription should be an accurate assessment of cardiorespiratory fitness. The results of this study suggest that commonly used submaximal exercise tests may not be valid for predicting fitness among pregnant women, particularly those that rely on submaximal heart rate responses (e.g. the YMCAT). Therefore, clinicians and health care providers should be cautious about test selection during pregnancy in order to obtain an accurate prediction of fitness. This will help to ensure an appropriate, personalized exercise program to maximize the well-established benefits of exercise during pregnancy.
Acknowledgments
Funding: This research was funded by NIH NIGMS IDeA Grant 5P20GM103436 and Western Kentucky University Faculty Undergraduate Student Engagement Grant #SP16-212.
Footnotes
Conflicts of Interest: The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The authors have no conflicts of interest to disclose.
References
- 1.Golding L, Sinning W. Y’s Way to Physical Fitness: The Complete Guide to Fitness Testing and Instruction: YMCA of the USA. Champaign, IL: Human Kinetics Publishers; 1989. pp. 89–106. [Google Scholar]
- 2.Portney LG and Watkins MP (2009) Foundations of Clinical Research: Applications to Practice. 3rd Edition, Pearson Education, Inc., New Jersey. [Google Scholar]
- 3.Barakat R, Perales M, Bacchi M, Coteron J, and Refoyo I. A program of exercise throughout pregnancy. Is it safe to mother and newborn? Am J Health Promot 29: 2–8, 2014. [DOI] [PubMed] [Google Scholar]
- 4.Beekley MD, Brechue WF, deHoyos DV, Garzarella L, Werber-Zion G, and Pollock ML. Cross-validation of the YMCA submaximal cycle ergometer test to predict VO2max. Res Q Exerc Sport 75: 337–342, 2004. [DOI] [PubMed] [Google Scholar]
- 5.Blair SN, Kohl HW 3rd, Paffenbarger RS Jr., Clark DG, Cooper KH, and Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 262: 2395–2401, 1989. [DOI] [PubMed] [Google Scholar]
- 6.Bland JM and Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1: 307–310, 1986. [PubMed] [Google Scholar]
- 7.Burr JF, Bredin SS, Faktor MD, and Warburton DE. The 6-minute walk test as a predictor of objectively measured aerobic fitness in healthy working-aged adults. Phys Sportsmed 39: 133–139, 2011. [DOI] [PubMed] [Google Scholar]
- 8.Cahalin L, Pappagianopoulos P, Prevost S, Wain J, and Ginns L. The relationship of the 6-min walk test to maximal oxygen consumption in transplant candidates with end-stage lung disease. Chest 108: 452–459, 1995. [DOI] [PubMed] [Google Scholar]
- 9.Cahalin LP, Mathier MA, Semigran MJ, Dec GW, and DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest 110: 325–332, 1996. [DOI] [PubMed] [Google Scholar]
- 10.Chen CN, Chuang LM, and Wu YT. Clinical measures of physical fitness predict insulin resistance in people at risk for diabetes. Phys Ther 88: 1355–1364, 2008. [DOI] [PubMed] [Google Scholar]
- 11.Clapp JF 3rd and Capeless EL. Neonatal morphometrics after endurance exercise during pregnancy. Am J Obstet Gynecol 163: 1805–1811, 1990. [DOI] [PubMed] [Google Scholar]
- 12.Clapp JF 3rd and Little KD. Effect of recreational exercise on pregnancy weight gain and subcutaneous fat deposition. Med Sci Sports Exerc 27: 170–177, 1995. [PubMed] [Google Scholar]
- 13.Clausen JSR, Marott JL, Holtermann A, Gyntelberg F, and Jensen MT. Midlife Cardiorespiratory Fitness and the Long-Term Risk of Mortality: 46 Years of Follow-Up. J Am Coll Cardiol 72: 987–995, 2018. [DOI] [PubMed] [Google Scholar]
- 14.Dempsey JC, Sorensen TK, Williams MA, Lee IM, Miller RS, Dashow EE, and Luthy DA. Prospective study of gestational diabetes mellitus risk in relation to maternal recreational physical activity before and during pregnancy. Am J Epidemiol 159: 663–670, 2004. [DOI] [PubMed] [Google Scholar]
- 15.Duffield R, Dawson B, Pinnington HC, and Wong P. Accuracy and reliability of a Cosmed K4b2 portable gas analysis system. J Sci Med Sport 7: 11–22, 2004. [DOI] [PubMed] [Google Scholar]
- 16.Edvardsen E, Hem E, and Anderssen SA. End criteria for reaching maximal oxygen uptake must be strict and adjusted to sex and age: a cross-sectional study. PLoS One 9: e85276, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faggiano P, D’Aloia A, Gualeni A, Lavatelli A, and Giordano A. Assessment of oxygen uptake during the 6-minute walking test in patients with heart failure: preliminary experience with a portable device. Am Heart J 134: 203–206, 1997. [DOI] [PubMed] [Google Scholar]
- 18.Genest DS, Falcao S, Gutkowska J, and Lavoie JL. Impact of exercise training on preeclampsia: potential preventive mechanisms. Hypertension 60: 1104–1109, 2012. [DOI] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, and Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: 377–381, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heenan AP, Wolfe LA, and Davies GA. Maximal exercise testing in late gestation: maternal responses. Obstet Gynecol 97: 127–134, 2001. [DOI] [PubMed] [Google Scholar]
- 21.Jakicic JM, King WC, Gibbs BB, Rogers RJ, Rickman AD, Davis KK, Wahed A, and Belle SH. Objective Versus Self-Reported Physical Activity in Overweight and Obese Young Adults. J Phys Act Health 12: 1394–1400, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laboratories ATSCoPSfCPF. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166: 111–117, 2002. [DOI] [PubMed] [Google Scholar]
- 23.Lipkin DP, Scriven AJ, Crake T, and Poole-Wilson PA. Six minute walking test for assessing exercise capacity in chronic heart failure. Br Med J (Clin Res Ed) 292: 653–655, 1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lotgering FK, Struijk PC, van Doorn MB, and Wallenburg HC. Errors in predicting maximal oxygen consumption in pregnant women. J Appl Physiol (1985) 72: 562–567, 1992. [DOI] [PubMed] [Google Scholar]
- 25.Lotgering FK, van Doorn MB, Struijk PC, Pool J, and Wallenburg HC. Maximal aerobic exercise in pregnant women: heart rate, O2 consumption, CO2 production, and ventilation. J Appl Physiol (1985) 70: 1016–1023, 1991. [DOI] [PubMed] [Google Scholar]
- 26.Lucas C, Stevenson LW, Johnson W, Hartley H, Hamilton MA, Walden J, Lem V, and Eagen-Bengsten E. The 6-min walk and peak oxygen consumption in advanced heart failure: aerobic capacity and survival. Am Heart J 138: 618–624, 1999. [DOI] [PubMed] [Google Scholar]
- 27.Miyamoto S, Nagaya N, Satoh T, Kyotani S, Sakamaki F, Fujita M, Nakanishi N, and Miyatake K. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. Comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med 161: 487–492, 2000. [DOI] [PubMed] [Google Scholar]
- 28.Mottola MF, Davenport MH, Brun CR, Inglis SD, Charlesworth S, and Sopper MM. VO2peak prediction and exercise prescription for pregnant women. Med Sci Sports Exerc 38: 1389–1395, 2006. [DOI] [PubMed] [Google Scholar]
- 29.Muktabhant B, Lawrie TA, Lumbiganon P, and Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst Rev 6: CD007145, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nascimento SL, Surita FG, and Cecatti JG. Physical exercise during pregnancy: a systematic review. Curr Opin Obstet Gynecol 24: 387–394, 2012. [DOI] [PubMed] [Google Scholar]
- 31.Nathanielsz PW, Ford SP, Long NM, Vega CC, Reyes-Castro LA, and Zambrano E. Interventions to prevent adverse fetal programming due to maternal obesity during pregnancy. Nutr Rev 71 Suppl 1: S78–87, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Noonan V and Dean E. Submaximal exercise testing: clinical application and interpretation. Phys Ther 80: 782–807, 2000. [PubMed] [Google Scholar]
- 33.Opasich C, Pinna GD, Mazza A, Febo O, Riccardi R, Riccardi PG, Capomolla S, Forni G, Cobelli F, and Tavazzi L. Six-minute walking performance in patients with moderate-to-severe heart failure; is it a useful indicator in clinical practice? Eur Heart J 22: 488–496, 2001. [DOI] [PubMed] [Google Scholar]
- 34.Price BB, Amini SB, and Kappeler K. Exercise in pregnancy: effect on fitness and obstetric outcomes-a randomized trial. Med Sci Sports Exerc 44: 2263–2269, 2012. [DOI] [PubMed] [Google Scholar]
- 35.Ross RM, Murthy JN, Wollak ID, and Jackson AS. The six minute walk test accurately estimates mean peak oxygen uptake. BMC Pulm Med 10: 31, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Russo LM, Nobles C, Ertel KA, Chasan-Taber L, and Whitcomb BW. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Obstet Gynecol 125: 576–582, 2015. [DOI] [PubMed] [Google Scholar]
- 37.Sady SP, Carpenter MW, Sady MA, Haydon B, Hoegsberg B, Cullinane EM, Thompson PD, and Coustan DR. Prediction of VO2max during cycle exercise in pregnant women. J Appl Physiol (1985) 65: 657–661, 1988. [DOI] [PubMed] [Google Scholar]
- 38.Sallis JF and Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport 71: S1–14, 2000. [PubMed] [Google Scholar]
- 39.Sandvik L, Erikssen J, Thaulow E, Erikssen G, Mundal R, and Rodahl K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med 328: 533–537, 1993. [DOI] [PubMed] [Google Scholar]
- 40.Solway S, Brooks D, Lacasse Y, and Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 119: 256–270, 2001. [DOI] [PubMed] [Google Scholar]
- 41.Starobin D, Kramer MR, Yarmolovsky A, Bendayan D, Rosenberg I, Sulkes J, and Fink G. Assessment of functional capacity in patients with chronic obstructive pulmonary disease: correlation between cardiopulmonary exercise, 6 minute walk and 15 step exercise oximetry test. Isr Med Assoc J 8: 460–463, 2006. [PubMed] [Google Scholar]
- 42.Sui Z, Moran LJ, and Dodd JM. Physical activity levels during pregnancy and gestational weight gain among women who are overweight or obese. Health Promot J Austr 24: 206–213, 2013. [DOI] [PubMed] [Google Scholar]
- 43.Tinius RA, Cahill AG, and Cade WT. Origins in the Womb: Potential Role of the Physical Therapist in Modulating the Deleterious Effects of Obesity on Maternal and Offspring Health Through Movement Promotion and Prescription During Pregnancy. Phys Ther 97: 114–123, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tong S, Kaur A, Walker SP, Bryant V, Onwude JL, and Permezel M. Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit. Obstet Gynecol 111: 710–714, 2008. [DOI] [PubMed] [Google Scholar]
- 45.Zugck C, Kruger C, Durr S, Gerber SH, Haunstetter A, Hornig K, Kubler W, and Haass M. Is the 6-minute walk test a reliable substitute for peak oxygen uptake in patients with dilated cardiomyopathy? Eur Heart J 21: 540–549, 2000. [DOI] [PubMed] [Google Scholar]


