Abstract
Evaluation of COVID-19 related complication is challenging in pregnancy, due to concerns about ionizing radiation risk to mother and the fetus. Although there are instances when diagnostic imaging is clinically warranted for COVID-19 evaluation despite the minimal risks of radiation exposure, often there are concerns raised by the patients and sometimes by the attending physicians. This article reviews the current recommendations on indications of chest imaging in pregnant patients with COVID-19, the dose optimization strategies, and the risks related to imaging exposure during pregnancy. In clinical practice, these imaging strategies are key in addressing the complex obstetrical complications associated with COVID-19 pneumonia.
Keywords: COVID-19, chest radiograph, computed tomography, pregnancy, optimization
Introduction
Corona virus disease of 2019 (COVID-19) is a viral disease caused by severe acute respiratory syndrome-Coronavirus-2 (SARS-COV-2). 1 The disease first originated in the Hubei province of China, later sweeping through the continents and evolving to become a global pandemic. The detailed insights into the disease manifestations, heterogeneity, and physiological behavior of the virus, including pulmonary and extra pulmonary manifestations of COVID-19, are being better understood with new research studies and clinical experiences.
There is a relative higher risk of COVID-19 infection during the time of pregnancy, 2 thereby creating constraints and clinical dilemma on proceeding with the use of an appropriate radiological investigation. 3 The clinical pathway for evaluating COVID-19 and its associated complications in pregnancy is highly variable, depending on the institutional preferences, availability of resources, practice pattern of referring clinicians, and interpreting radiologist. Imaging studies which involve radiation exposure like chest X-ray and chest CT scan are indispensable in the management of COVID-19 patients. Radiologists around the globe should be familiar with merits and limitations of various chest imaging modalities in evaluation of COVID-19 pneumonia and its complications during pregnancy. In this review, we aim to summarize the current recommendations on indications of chest imaging in pregnant COVID-19 patients including chest X-ray, CT chest, CT pulmonary angiogram, chest ultrasound, and cardiac MRI, with emphasis on imaging risks and dose optimization strategies.
Features of COVID-19 in pregnancy
Epidemiology
Recent surveillance data from the Centers for Disease Control and Prevention (CDC), in the women aged between 15 to 44 years, showed pregnant women were more likely to be hospitalized, requiring an intensive care unit (ICU) care or ventilation. 4 However, large cohort study from the United Kingdom observed that the rates of ICU admission or maternal mortality in severe disease were similar to non-pregnant women in the reproductive age group. 5 Pregnant women are more susceptible to infections owing to the immunity changes during the time of pregnancy. 6 There are guidelines from the CDC, the American College of Obstetricians and Gynaecologists (ACOG), the Society for Fetal-Medicine (SMFM), and the Royal College of Obstetrics and Gynaecologists (RCOG) related to the management of COVID-19 in pregnancy.7–13
Complications related to COVID-19 in pregnancy
Chest complications related to COVID-19 in general include a spectrum of findings related to airway, alveolar, vascular, and cardiac involvement. Recent studies have shown an increased incidence of complications in pregnancy due to COVID-19, especially preeclampsia, eclampsia, HELLP syndrome, and increased risk for maternal mortality. 14 Furthermore, the complications are augmented with pre-existing or underlying comorbidities like obesity, diabetes mellitus, systemic hypertension, and cardiac diseases. 15
Diagnosis and clinical severity classification in pregnancy with COVID-19
RT-PCR is considered the reference standard for diagnosis of COVID-19 in pregnancy. 16 Prior studies have reported the RT-PCR positive rates in asymptomatic pregnant women between 50 and 89%,17–19 while false negative rates varied from 17 to 63%. 20 The categorization of pregnant patients with COVID-19 based on the severity of illness is similar to other adult patients with COVID-19. They are categorized into asymptomatic, mild, moderate, severe or, critical 21 (Table 1). There are instances when the initial clinical presentation related to an upper or lower respiratory tract infection related to bacterial or other non-COVID-19 viral infection may raise the suspicion for COVID-19, 22 the imaging in such a scenario may be tailored according to the disease severity, clinical suspicion, and the trimester.
Table 1.
Clinical disease spectrum in patients with COVID-19.
| Illness severity | Clinical signs or symptoms |
|---|---|
| Asymptomatic or pre-symptomatic patients | Viral positive (RT-PCR or NAAT) without any symptoms |
| Mild illness | Patients with COVID-19 symptoms, without dyspnea, shortness of breath |
| Moderate illness * | Clinical or imaging assessment showing COVID-19 pneumonia with oxygen saturation (SpO2) >94% at room air or sea level |
| Severe illness * | Respiratory rate >30 per minute, SpO2 < 94% on room air or at sea level, ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) < 300, or chest X-ray showing lung infiltrates with >50% involvement |
| Critical illness * | Patients with respiratory failure, septic shock, or multiorgan dysfunction |
COVID-19-corona virus disease 2019; NAAT- nucleic acid amplification test, RT-PCR- reverse transcriptase polymerase chain reaction.* Disease severity that might require an imaging with chest X-ray, CT chest, or CT pulmonary angiogram depending on the clinical assessment and disease status
Evaluation of COVID-19 pneumonia in pregnancy
(1) Utility of chest X-ray
Recommendations
The position statement by Fleischner society and ACOG recommends that routine imaging should not be used in asymptomatic or mild illness severity patients and also in intubated stable patients with COVID-19.8,23 The ACOG and SMFM recommends chest X-ray in patients with moderate clinical risk based on illness severity and underlying comorbidities in all trimesters, 10 while the RCOG recommends that the radiographic investigations such as chest radiograph and CT chest should be performed in pregnant patient with COVID-19 as for the non-pregnant adult and chest imaging should be performed when indicated and should not be delayed over concerns of fetal radiation exposure, as the maternal well-being is paramount. 13 In practice, chest X-ray should not be used for arriving at a diagnosis of COVID-19 in pregnant patients, instead it is recommended to rely on RT-PCR confirmation of the disease status. Follow-up chest X-ray should be judiciously considered only when there is further clinical deterioration and situations that would impact patient care.
Optimization strategies in chest x-ray
In routine chest X-ray, the pelvis or gravid uterus is generally not exposed to direct X-ray beam, and can be safely performed with optimization strategies. 24 However, in third trimester due to gravid uterus reaching the upper abdomen, parts of fetus can get exposed to a direct X-ray beam, and this needs to be taken care of using an appropriate technique. Dose optimization strategies to reduce the maternal and fetal dose include collimating on the lungs and avoiding upper abdomen as much as possible with an abdominal lead shield 25 placed over the abdomen or back depending on Antero-Posterior (AP) or Postero-Anterior (PA) radiographs, respectively, and also to limit the chest radiograph to frontal view and avoiding a lateral radiograph. 24
(2) Utility of CT
Pattern of lung involvement in COVID-19 includes ground glass opacities (GGO), GGO with consolidation, and only consolidation are similar to non-pregnant patients.26–29 However, the imaging findings have close overlap with other viral lung infections like influenza virus, MERS-COV, SARS, H1N1, H5N1, and H7N9.26,27
Recommendations
The position statement by the American College of radiology (ACR) 30 recommends against the use of CT scan as a first-line investigation or for follow-up to assess progression of COVID-19. The Fleischner Society advocates CT scan only in patients with functional impairment, hypoxemia, or after recovery from infection. The SMFM, ACOG, and RCOG recommend that CT chest should not be withheld in pregnant patients when clinically indicated.10,13 Thus, in pregnant patients the CT chest should be undertaken only in instances where there is functional impairment, hypoxemia, or both.
Unlike other lower respiratory tract viral infections, respiratory decompensation in COVID-19 pneumonia happens later in the disease. 31 Hypoxemia related to acute respiratory failure in pregnancy manifests with partial pressure of oxygen (PaO2) <60 mmHg on room air, that corresponds to oxygen saturation (SpO2) <90 mmhg on room air or sea level.32,33
Optimization and dose reduction strategies in CT
Although CT chest do not directly expose the pelvis or gravid uterus to ionizing radiation and can be performed in pregnancy after justification of the benefits, the radiologists should be aware of the dose reduction descriptors 34 and strategies while performing a CT chest or CT pulmonary angiogram for pregnant patients with COVID-19 (Tables 2 and 3). The most common strategies include reducing mA, kVp, Z-axis of acquisition, and iterative reconstruction algorithms.21,35–37 Reduction in exposure parameters to a certain level is possible with trade-off in image quality without altering the diagnostic accuracy of images. Dose reduction strategies unrelated to CT imaging parameters include reducing the length of scan with strict collimation from the lung apices to diaphragm to minimize maternal and fetal dose and use of lead shield coverage over the maternal abdomen and bismuth breast shield to maternal breasts. Although, the lead shielding to wrap the abdomen during the CT chest scan may reassure the patient of the safety of fetus, the fetal dose received due to CT chest is primarily related to internal scatter, which is not altered by abdominal shielding. 38 The use of breast shielding is controversial as it can degrade the image quality due to increased noise and make the automatic exposure control unpredictable. However considering the increased radiosensitivity of breast parenchyma in pregnancy, breast shielding can be selectively used with proper training.39,40 In such a scenario, the dose reduction strategies implemented in pregnant patients should be utilized in non-pregnant young females undergoing COVID-19 imaging as well.
Table 2.
Dose descriptors relevant for dose optimization.
| Dose descriptor | Units | Definition | Calculation | Effect on radiation dose | Dependant CT parameters |
|---|---|---|---|---|---|
| CTDI (vol) | mGy | Measure of radiation from CT scanner assessed with 16 or 32 cm phantom | Weighted average to depict radiation across the phantom | Linear relationship between CTDI (vol) and exposure dose | Tube voltage, current, pitch, and phantom |
| Dose length product (DLP)mGy-cm | mGy-cm | Indicator of extend of Z-axis coverage and CTDI (vol) | CTDI (vol) x length of scan in cm | Linear relationship between CTDI (vol) and exposure dose | CTDI (vol), scan length, and number of acquisitions |
| Effective dose | mSv | Theoretical uniform whole body dose | DLP x conversion factor (k) | Linear relationship between mSv and absorbed dose | DLP, patient size, and radio sensitivity of involved organs |
| Size specific dose estimate (SSDE) | mGy | Dose measured for patient size/habitus | CTDI x correction factor dependant on patient diameter | Automated tube current modulation results in large dose for larger patients | Patient body contour along Z-axis and positioning within the gantry |
| Absorbed dose | mGy | Ionizing radiation absorbed (Joule) by tissue (kg) | Estimated from size specific dose estimate (SSDE) | — | DLP, patient size, and organ scanned |
Table 3.
Dose optimization strategies.
| CT parameter | Optimization recommendations |
|---|---|
| Tube current modulation | Check tube current saturation and adjust parameters like tube voltage and speed to attain maximal dose reduction |
| Optimal tube voltage at equivalent radiation dose | Selection of most efficient tube voltage that can reduce dose as much as possible depending on the scanner efficiency |
| Longitudinal scan range | Aortic arch to the diaphragm avoiding the upper abdomen as much as possible |
| Scan modes | Use low dose, ultra-low dose modes, high pitch dual energy modes |
| Noise reduction image reconstruction algorithms | Noise reducing, spatial resolution preserving algorithms like iterative reconstruction at low radiation dose |
| Body size regulated CT protocols | Using best-fit equation than dose table or charts |
| Other CT parameters independent dose reduction strategies | Elimination of lateral scout image |
| Fixed injection timing instead of bolus triggering | |
| Avoiding test run | |
| Single phase sequence | |
| Abdominal lead shielding |
Overall, the dose reduction strategies should be tailored depending on the resources available with the institution, and the focus should be on implementing a low dose or ultra-low dose strategies for CT imaging in pregnant patients with COVID-19 and to bring down the effective dose below 3 mSv. 41
(3) Utility of chest USG
The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) recommends using an ultrasound for lung examinations in pregnant patients with COVID-19 as it has the advantage of being radiation free and can be performed at the same time along with obstetric ultrasound which in turn saves time and improves the clinical workflow. Also it can be considered as an alternate when chest radiograph or CT scan is not available. 42 On ultrasound, the normal horizontal “A-lines” (A-lines refers to horizontal echogenic reverberation artefacts that occur in normal lungs, beneath the pleural line at multiples of distance between the ultrasound probe and visceral-parietal pleural interface) are replaced by abnormal “B-Lines” when there is early loss of aeration but not completely consolidated (B-Lines refers to artefact in ultrasound caused as a result of loss of aeration in alveolar-interstitial space). While a consolidation results in absence of A- and B-lines, with a hyperechoic “white lungs”.
Evaluation of pulmonary embolism in pregnancy with COVID-19
Utility of CT pulmonary angiogram
Pulmonary embolism is reported to occur commonly in patients with COVID-19 with a reported incidence ranging from 0.7–57%, more often associated with severe disease. 43 Pregnancy is associated with a five-fold increased risk for developing pulmonary embolism, due to decreased fibrinolysis, hypercoagulability status, venous stasis, and prolonged bed rest. Pulmonary embolism is also a leading cause of maternal death during pregnancy, and the diagnosis during pregnancy has significant implications in planning of delivery and anticoagulation therapy.44,45 In planning an imaging for COVID-19 to rule out pulmonary embolism, all patients should have been thoroughly evaluated on the pre-test probability of pulmonary embolism using Pulmonary embolism rule out criteria, 46 Wells score, 47 Geneva score, 48 and D-Dimer when indicated. The role of D-dimer assay is limited in pregnant patients as the value can arise above the reference levels as the pregnancy progresses. 49 However, normal D-dimer levels have a high negative predictive value in ruling out pulmonary embolism.
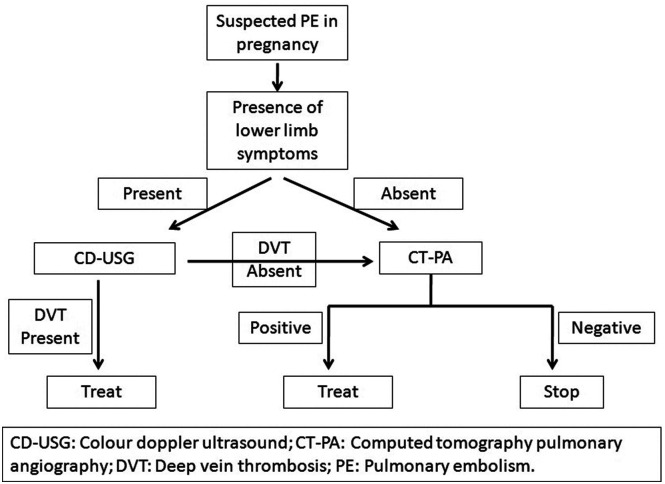
Diagnostic imaging with CT pulmonary angiography is considered a clinically warranted investigation in pregnant patients suspected of pulmonary embolism with COVID-19. 13 However, the initial workup should focus on non-ionizing imaging techniques like lower extremity color Doppler ultrasound. Although the prevalence of lower limb deep vein thrombosis with clinically suspected pulmonary embolism in COVID-19 is uncertain, the advantage of getting a positive deep vein thrombosis on duplex ultrasound is considered sufficient to justify the use of anticoagulation therapy, thereby eliminating the need for further CT pulmonary angiography. 50 If the initial tests are non-diagnostic, CT pulmonary angiography should be performed as a second line investigation. Figure 1 summarizes a practical diagnostic algorithm for evaluating a pregnant patient with suspected pulmonary embolism in COVID-19. 51 In a setting of COVID-19, the CT pulmonary angiography is preferred over V/Q scintigraphy as it can be used to assess the severity of lung changes for COVID-19 as well.
Figure 1.
Diagnostic algorithm for evaluation of pregnant patients with COVID-19 suspected of pulmonary embolism.
If there is a positive pulmonary embolism, deep vein thrombosis, or when there is maternal hypoxemia, an obstetric ultrasound for fetal growth, amniotic fluid, and color Doppler imaging should be performed when necessary to assess the extent of fetal hypoxemia. 52
Risks related to contrast media
The risks related to iodinated contrast material include the possibility of nephrotoxicity and allergic reactions, with similar relative risks for pregnant and general population. The contrast should not be administered when there is prior major allergic reaction to iodinated contrast material or an underlying impaired renal function. Although, the iodinated contrast crosses the placenta to reach the fetus, there are no reported risks for the fetus. There is a theoretical risk of contrast-induced thyroid dysfunction and hence thyroid function screening should be performed in neonates although there is no convincing evidence to support the same.53,54
The use of gadolinium should be restricted in pregnancy as few studies have shown association between gadolinium exposure in utero to still births and neonatal deaths. The US Food and Drug Administration (FDA) has categorized gadolinium as pregnancy class 3 drug. 55
Evaluation of myocarditis in pregnancy with COVID-19
Utility of Cardiac MRI
There is evidence of varying manifestation of myocardial injury associated with ongoing or recently recovered COVID-19 patients, with myocarditis being the most common pattern (in 40% cases) while other complications include myocardial ischemia, right ventricular strain, cardiac thromboembolism etc. 56 Few studies have indicated that the mapping abnormalities and cardiac involvement can be picked up early in the disease with cardiac MRI. 57 Cardiac MRI has shown to be a safe imaging in pregnancy with no risk to the mother. Theoretical concerns of teratogenesis, acoustic damage, and tissue heating have not been sufficiently proven in humans. Moreover in cardiac MRI, field of view is away from the fetus, thereby further reducing the potential harm. 58 There is no different risk in relation to different trimesters as per the American College of Radiology (ACR). 59 The information related to utility of cardiac MRI in pregnant patients with COVID-19 is limited, and with the absence of specific recommendations, the use of cardiac MRI can be considered in pregnancy on a case-to-case basis, and also on the resource availability.
Evaluation of fetal hypoxemia due to maternal pulmonary compromise
Hypoxemia due to maternal respiratory failure in COVID-19 leading to poor oxygenation to placenta and fetus can result in fetal distress.60,61 Although the emerging evidence suggests vertical transmission is probable, the significance of the same to the neonate is yet to be ascertained. There are emerging data that indicate that this viral infection causes inflammation, villitis, and arteriopathy in placenta.62,63 Fetal distress and preterm pregnancy are common obstetrical complications of COVID-19. 64 Assessment for acute placental insufficiency and fetal hypoxia can be easily assessed with obstetric Doppler ultrasound.65,66 The placental and fetal consequences of COVID-19 including the utility of functional MRI in fetal hypoxemia related to COVID-19 remain to be explored.
Radiation exposure thresholds during pregnancy
During the time of pregnancy, the permitted radiation exposure limits are up to 50mGy. The absorbed dose of radiation in a fetus whose mother undergoes chest X-ray and CT scan is 0.002mGy and 0.2mGy, respectively.43,67 Although the data on the fetal risks from radiation is widely variable in the literature, it is generally agreed that at doses less than 50 mGy, there is no evidence of an increased risk of fetal malformations, developmental delay, or loss of pregnancy (Table 4). There is reported small increased risk of childhood cancer, 1 in 1500 to 2000 versus the 1 in 3000 background rate.68–70 In this context it is important to note that combined exposure to few chest radiograph or CT pulmonary angiography for evaluation of COVID-19 related complications, the cumulative dose falls well below the accepted limits of 50 mGy during the time of pregnancy.
Table 4.
Effects of radiation induced teratogenesis with gestational age.
| Gestational age | Effect on foetus | Estimated dose threshold |
|---|---|---|
| Prior to implantation (0–2 weeks after fertilization) | Embryonal death (or) no consequences at all | 50–100 mGy |
| Organogenesis (2–8 weeks after fertilization) | Congenital anomalies (skeleton, eyes, genitals) | 200 mGy |
| Growth restriction | 200–250 mGy | |
| 8–15 weeks | Severe intellectual disability (high risk) | 60–310 mGy |
| Intellectual deficit | 25 IQ points loss per 1000 mGy | |
| Microcephaly | 200 mGy | |
| 16–25 weeks | Severe intellectual disability (low risk) | 250–280 mGy |
Informed Consent and patient counseling
Informed consent and patient counseling are important to alleviate the anxiety of patients, while undergoing imaging modalities with radiation exposure like the chest X-ray or CT scan. The attending physician should convey the outweighed benefits of doing an imaging to assess the disease status or to evaluate the complications of COVID-19, as opposed to the risk on the fetus leading to congenital anomalies, birth defects, and miscarriage although negligible for the radiation dose received by the patient. The attending physician and the radiologist should confirm the patients understanding of the estimated risk to mother and fetus. In practice, patient can be explained about the imaging-related radiation exposure by comparing it with background population risk which is approximately 4%, 10%, 10%, and 20% for malformations, genetic diseases, growth retardation, and pregnancy loss, respectively. 71
Conclusion
Chest radiograph and CT examinations for COVID-19 evaluation deliver minimal radiation dose to the mother and fetus, and rarely exceed the permissible limit of 50mGy. Although this knowledge should reassure pregnant women and attending physician on the greater benefits of undergoing an imaging for COVID-19 evaluation, over the minimal radiation risks, the management strategy should focus on keeping the radiation exposure to both mother and fetus as low as reasonably achievable according to ALARA principles. Radiologists should be aware of the lack of understanding about the radiation risk among the non-radiologist physician who would be requesting an imaging during the care of a pregnant COVID-19 patient, and it’s the responsibility of radiologist to counsel the treating physician with regard to various options available for chest imaging including radiation-free modalities like chest USG and cardiac MRI when appropriate for evaluation of COVID-19 related chest complications in pregnancy and to improve patient care.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The publication of this article was funded by the Qatar National Library.
Informed consent: Informed consent was waived by IRB (Institutional Review Board) for this review article.
Guarantor: AN
Author contributions
Article concept, design, manuscript drafting/editing/revision for important intellectual content and Literature research all authors. Final version of manuscript is approved by all authors.
ORCID iDs
Anirudh Venugopalan Nair https://orcid.org/0000-0001-7662-7668
Subramaniyan Ramanathan https://orcid.org/0000-0002-4317-2414
References
- 1.Nair AV, McInnes M, Jacob B, et al. Diagnostic accuracy and inter-observer agreement with the CO-RADS lexicon for CT chest reporting in COVID-19. Emerg Radiol 2021; 395: 1045–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet 2020; 395: 760–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wieseler KM, Bhargava P, Kanal KM, et al. Imaging in pregnant patients: examination appropriateness. Radiographics 2010; 30: 1215–1229. [DOI] [PubMed] [Google Scholar]
- 4.Ellington S, Strid P, Tong VT, et al. Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–June 7, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 769–775. DOI: 10.15585/mmwr.mm6925a1externalicon [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knight M, Bunch K, Vousden N, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ (Clin Res ed) 2020; 369: m2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mor G, Cardenas I, Abrahams V, et al. Inflammation and pregnancy: the role of the immune system at the implantation site. Ann New York Acad Sci 201; 1221: 80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID-19 Treatment Guidelines . [Internet]. 2021. Available from: https://www.covid19treatmentguidelines.nih.gov/. [accessed 2021 Jun 9]
- 8.Novel Coronavirus 2019 (COVID-19) | ACOG . [Internet]. 2021. Available from: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019. [accessed 2021 Jun 9]
- 9.Collin J, Byström E, Carnahan A, et al. Public health agency of sweden's brief report: pregnant and postpartum women with severe acute respiratory syndrome coronavirus 2 infection in intensive care in sweden. Acta Obstetricia Gynecologica Scand 2020; 99: 819–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol 2020; 222: 415–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Considerations for Inpatient Obstetric Healthcare Settings | CDC . [Internet]. 2021. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/inpatient-obstetric-healthcare-guidance.html. [acessed 2021 Jun 10]
- 12. Coronavirus (COVID-19) and Pregnancy: What Maternal-Fetal Medicine Subspecialists Need to Know . https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control- (accessed 15 February 2022). [Google Scholar]
- 13.Coronavirus (COVID-19) infection in pregnancy information for healthcare professionals, 2022. [Google Scholar]
- 14.Villar J, Ariff S, Gunier RB, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection. JAMA Pediatr 2021; 175: 817–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Savasi VM, Parisi F, Patanè L, et al. Clinical findings and disease severity in hospitalized pregnant women with coronavirus disease 2019 (COVID-19). Obstet Gynecol 2020; 136: 252–258. [DOI] [PubMed] [Google Scholar]
- 16.Savirón-Cornudella R, Villalba A, Zapardiel J, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) universal screening in gravids during labor and delivery. Eur J Obstet Gynecol Reprod Biol 2021; 256: 400–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sutton D, Fuchs K, D’Alton M, et al. Universal screening for SARS-CoV-2 in women admitted for delivery. New Engl J Med 2020; 382: 2163–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herraiz I, Folgueira D, Villalaín C, et al. Universal screening for SARS-CoV-2 before labor admission during Covid-19 pandemic in Madrid. J Perinatal Med 2020; 48: 981–984. [DOI] [PubMed] [Google Scholar]
- 19.Prabhu M, Cagino K, Matthews K, et al. Pregnancy and postpartum outcomes in a universally tested population for SARS‐CoV‐2 in new york city: a prospective cohort study. BJOG: Int J Obstet Gynaecol 2020; 127: 1548–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kelly JC, Dombrowksi M, O’Neil-Callahan M, et al. False-negative testing for severe acute respiratory syndrome coronavirus 2: consideration in obstetrical care. Am J Obstet Gynecol MFM 2020; 2: 100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clinical Spectrum | COVID-19 Treatment Guidelines . [Internet]. 2021. Available from: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/. [acessed 2021 Jun 10]
- 22.Inchingolo R, Smargiassi A, Moro F, et al. The diagnosis of pneumonia in a pregnant woman with coronavirus disease 2019 using maternal lung ultrasound. Am J Obstet Gynecol 2020; 223: 9–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubin GD, Ryerso CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Radiology. 2020; 296: 172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Acr. PRACTICE PARAMETER 1 Pregnant or Potentially Pregnant Patients. [Google Scholar]
- 25.Karimi MA, Radpour A, Sedaghat A, et al. Proposed imaging guidelines for pregnant women suspected of having COVID-19. Acad Radiol 2020; 27: 902–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-NCoV). Radiology 2020; 295: 202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song F, Shi N, Shan F, et al. Emerging 2019 novel coronavirus (2019-NCoV) pneumonia. Radiology 2020; 295: 210–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in wuhan, china: a descriptive study. Lancet Infect Dis 2020; 20: 425–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu H, Liu F, Li J, et al. Clinical and CT imaging features of the COVID-19 pneumonia: Focus on pregnant women and children. J Infect 2020; 80: e7–e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.(CT) for Suspected COVID-19 Infection . ACR recommendations for the use of chest radiography and computed tomography. American College of Radiology, [Internet]. 2021. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. [acessed 2021 Feb 22] [Google Scholar]
- 31.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, china. Jama 2020; 323: 1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.COVID-19: Overview of pregnancy issues - UpToDate . https://www.uptodate.com/contents/covid-19-overview-of-pregnancy-issues (accessed 15 February 2022). [Google Scholar]
- 33.Madan A. Correlation between the levels of SpO2and PaO2. Lung India: Offi Organ Indian Chest Soc 2017; 34: 307–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayo-Smith WW, Hara AK, Mahesh M, et al. How I do it: managing radiation dose in CT. Radiology 2014; 273: 657–672. [DOI] [PubMed] [Google Scholar]
- 35.Albrecht MH, Bickford MW, Nance JW, et al. State-of-the-art pulmonary CT angiography for acute pulmonary embolism. Am J Roentgenology 2017; 208: 495–504. [DOI] [PubMed] [Google Scholar]
- 36.Mayo J, Thakur Y. Pulmonary CT angiography as first-line imaging for PE: Image quality and radiation dose considerations. Am J Roentgenology 2013; 200: 522–528. [DOI] [PubMed] [Google Scholar]
- 37.Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol 2012; 13: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sowby Icrp FD, Bo Lindell P, Beninson DJ, et al. Published on behalf of the lnternational Commission on Radiological Protection International Commission on Radiological Protection 198l-1985 Members of the Main Commission of the ICRP Subscription Rates Annual subscription, including postage and insurance. 2021 [Google Scholar]
- 39.Chen J, Lee RJ, Tsodikov A, et al. Does radiotherapy around the time of pregnancy for Hodgkin’s disease modify the risk of breast cancer? Int J Radiat Oncology*Biology*Physics 2004; 58: 1474–1479. [DOI] [PubMed] [Google Scholar]
- 40.Colletti PM, Micheli OA, Lee KH, et al. To shield or not to shield: application of bismuth breast shields. AJR Am Journal Roentgenology 2013; 200: 503–507. [DOI] [PubMed] [Google Scholar]
- 41.Pahade JK, Litmanovich D, Pedrosa I, et al. Imaging pregnant patients with suspected pulmonary embolism: what the radiologist needs to know. Radiographics 2009; 29: 639–654. [DOI] [PubMed] [Google Scholar]
- 42.Poon LC, Yang H, Lee JCS, et al. ISUOG interim guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. Ultrasound Obstet Gynecol 2020; 55: 700–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Suh YJ, Hong H, Ohana M, et al. Pulmonary embolism and deep vein thrombosis in COVID-19: a systematic review and meta-analysis. Radiology 2021; 298: E70–E80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Knight M, Ukoss . Antenatal pulmonary embolism: risk factors, management and outcomes. BJOG: An International Journal of Obstetrics & Gynaecology. 2008; 115: 453–61. [DOI] [PubMed] [Google Scholar]
- 45.Campbell IA, Fennerty A, Miller AC, et al. British thoracic society guidelines for the management of suspected acute pulmonary embolism. Thorax 2003; 58: 470–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kline JA, Mitchell AM, Kabrhel C, et al. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost 2004; 2: 1247–1255. [DOI] [PubMed] [Google Scholar]
- 47.Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and D-dimer. Ann Intern Med 2001; 135: 98–107. [DOI] [PubMed] [Google Scholar]
- 48.Le Gal G, Righini M, Roy P-M, et al. Prediction of pulmonary embolism in the emergency department: the revised geneva score. Ann Intern Med 2006; 144: 165–171. [DOI] [PubMed] [Google Scholar]
- 49.Anderson BL, Mendez-Figueroa H, Dahlke JD, et al. Pregnancy-induced changes in immune protection of the genital tract: defining normal. Am J Obstet Gynecol 2013; 208: e1–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patel SJ, Reede DL, Katz DS, et al. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics 2007; 27: 1705–1722. [DOI] [PubMed] [Google Scholar]
- 51.Leung AN, Bull TM, Jaeschke R, et al. An official american thoracic society/society of thoracic radiology clinical practice guideline: evaluation of suspected pulmonary embolism in pregnancy. Am J Respir Crit Care Med 2011; 184: 1200–1208. [DOI] [PubMed] [Google Scholar]
- 52.Stanczyk P, Jachymski T, Sieroszewski P. COVID-19 during pregnancy, delivery and postpartum period based on EBM. Ginekologia Polska 2020; 91: 417–423. [DOI] [PubMed] [Google Scholar]
- 53.Webb JAW, Thomsen HS, Morcos SK, et al. The use of iodinated and gadolinium contrast media during pregnancy and lactation. Eur Radiol 2005; 15: 1234–1240. [DOI] [PubMed] [Google Scholar]
- 54.Dembinski J, Arpe V, Kroll M, et al. Thyroid function in very low birthweight infants after intravenous administration of the iodinated contrast medium iopromide. Arch Disease Childhood. Fetal Neo Edit 2000; 82: F215–F217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ray JG, Vermeulen MJ, Bharatha A, et al. Association between MRI exposure during pregnancy and fetal and childhood outcomes. Jama 2016; 316: 952–961. [DOI] [PubMed] [Google Scholar]
- 56.Ojha V, Verma M, Pandey NN, et al. Cardiac magnetic resonance imaging in coronavirus disease 2019 (COVID-19). J Thorac Imaging 2021; 36: 73–83. [DOI] [PubMed] [Google Scholar]
- 57.Huang L, Zhao P, Tang D, et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC: Cardiovasc Imaging 2020; 13: 2330–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen MM, Coakley FV, Kaimal A, et al. Guidelines for computed tomography and magnetic resonance imaging use during pregnancy and lactation. Obstet Gynecol 2008; 112: 333–340. [DOI] [PubMed] [Google Scholar]
- 59.Kanal E, Kanal E, Barkovich AJ, et al. ACR guidance document on MR safe practices: 2013. JMRI 2013; 37: 501–530. [DOI] [PubMed] [Google Scholar]
- 60.Putbrese B, Kennedy A. Findings and differential diagnosis of fetal intracranial haemorrhage and fetal ischaemic brain injury: what is the role of fetal MRI? Br J Radiol 2017; 90: 20160253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Düppers AL, Bohnhorst B, Bültmann E, et al. Severe fetal brain damage subsequent to acute maternal hypoxemic deterioration in COVID-19. Ultrasound Obstet Gynecol 2021; 58: 490–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Algarroba GN, Rekawek P, Vahanian SA, et al. Visualization of severe acute respiratory syndrome coronavirus 2 invading the human placenta using electron microscopy. Am J Obstet Gynecol 2020; 223: 275–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shanes ED, Mithal LB, Otero S, et al. Placental pathology in COVID-19. Am J Clin Pathol 2020; 154: 23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sule GA, Aysegul A, Selcan S, et al. Effects of SARS-COV-2 infection on fetal pulmonary artery Doppler parameters. Echocardiography (Mount Kisco, N.Y.) 2021; 38: 1314–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Turgut E, Ayhan SG, Oluklu D, et al. Fetal pulmonary artery doppler evaluation in pregnant women after recovery from COVID‐19. Int J Gynecol Obstet 2021; 155: 450–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rabiei M, Soori T, Abiri A, et al. Maternal and fetal effects of COVID-19 virus on a complicated triplet pregnancy: a case report. J Med Case Rep 2021; 15: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davarpanah AH, Mahdavi A, Sabri A, et al. Novel screening and triage strategy in iran during deadly coronavirus disease 2019 (COVID-19) epidemic: value of humanitarian teleconsultation service. J Am Coll Radiol 2020; 17: 734–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gynecol AC on OP-O . ACOG committee opinion. number 299, September 2004 (replaces no. 158, September 1995). Guidelines for diagnostic imaging during pregnancy. unboundmedicine.com, 2004. [DOI] [PubMed] [Google Scholar]
- 69.McCollough CH, Schueler BA, Atwell TD, et al. Radiation exposure and pregnancy: when should we be concerned? Radiographics 2007; 27: 909–917. [DOI] [PubMed] [Google Scholar]
- 70.Guidelines for diagnostic imaging during pregnancy and lactation . Obstetrics and Gynecology. 130, Lippincott Williams and Wilkins; 2017. p. e210–6. [DOI] [PubMed] [Google Scholar]
- 71.Diagnostic imaging in pregnant and nursing patients - UpToDate . https://www.uptodate.com/contents/diagnostic-imaging-in-pregnant-and-nursing-patients (accessed 15 February 2022). [Google Scholar]