Summary
Background
The identification and appropriate management of people with advanced HIV disease is a key component in the HIV response. People with HIV who are hospitalised are at a higher risk of death, a risk that might persist after discharge. The aims of this study were to estimate the frequency of negative post-discharge outcomes, and to determine risk factors for such outcomes in people with HIV.
Methods
Using a broad search strategy combining terms for hospital discharge and HIV infection, we searched MEDLINE via PubMed and Embase from Jan 1, 2003 to Nov 30, 2021 to identify studies reporting outcomes among people with HIV following discharge from hospital. We estimated pooled proportions of readmissions and deaths after hospital discharge using random-effects models. We also did subgroup analyses by setting, region, duration of follow-up, and advanced HIV status at admission, and sensitivity analyses to assess heterogeneity.
Findings
We obtained data from 29 cohorts, which reported outcomes of people living with HIV after hospital discharge in 92 781 patients. The pooled proportion of patients readmitted to hospital after discharge was 18·8% (95% CI 15·3–22·3) and 14·1% (10·8–17·3) died post-discharge. In sensitivity analyses, no differences were identified in the proportion of patients who were readmitted or died when comparing studies published before 2016 with those published after 2016. Post-discharge mortality was higher in studies from Africa (23·1% [16·5–29·7]) compared with the USA (7·5% [4·4–10·6]). For studies that reported both post-discharge mortality and readmission, the pooled proportion of patients who had this composite adverse outcome was 31·7% (23·9–39·5). Heterogeneity was moderate, and largely explained by patient status and linkage to care. Reported risk factors for readmission included low CD4 cell count at admission, longer length of stay, discharge against medical advice, and not linking to care following discharge; inpatient treatment with antiretroviral therapy (ART) during hospitalisation was protective of post-discharge mortality.
Interpretation
More than a quarter of patients with HIV had an adverse outcome after hospital discharge with no evidence of improvement in the past 15 years. This systematic review highlights the importance of ensuring post-discharge referral and appropriate management, including ART, to reduce mortality and readmission to hospital among this group of high-risk patients.
Funding
Bill & Melinda Gates Foundation.
Translations
For the French and Spanish translations of the abstract see Supplementary Materials section.
Introduction
The identification and appropriate management of people with advanced HIV disease is a key component in the HIV response to further reduce HIV-related mortality. Hospitalisations from complications associated with HIV infection, including coinfections associated with advanced HIV such as tuberculosis, cryptococcal meningitis, or severe bacterial infections remain substantial. A 2015 review found that HIV-related infections and bacterial infections are leading causes of hospital admission among people living with HIV.1 Low CD4 cell count and low antiretroviral coverage at admission are major contributors to this disease profile and associated mortality.1, 2
People with HIV who are hospitalised are at a higher risk of death,2, 3, 4, 5, 6, 7 and this risk might persist after discharge.5, 8 A systematic review of post-discharge mortality among general paediatric admissions in low-income settings found that post-discharge mortality rates often exceeded in-hospital mortality rates.9 A study from South Africa found that even with widespread access to antiretroviral therapy (ART), the majority of inpatient deaths were among patients with HIV.10 HIV is also commonly associated with readmission following discharge.11 Another study from South Africa reported that 6 months after discharge, half of patients had been readmitted at least once and a quarter had died.5 Several studies have identified factors associated with poor post-discharge outcomes among people living with HIV, including low CD4 cell count,12 lack of ART,13 and discharge against medical advice.14
The aims of this systematic review and meta-analysis were to assess post-discharge outcomes of people living with HIV and to summarise risk factors associated with poor outcomes.
Research in context.
Evidence before this study
There has been a renewed focus on advanced HIV disease in the past 5 years, with a need to improve outcomes to reduce HIV-related mortality. Individuals with advanced HIV disease (CD4 count <200 cells per μL) are at an increased risk of mortality from tuberculosis, cryptococcal meningitis, severe bacterial infections, and several other infectious diseases due to severely compromised immune function. In 2017, WHO recommended a package of care to be offered to individuals diagnosed with advanced HIV disease. Interventions in the package of care are directed at preventing, diagnosing, and treating the major causes of HIV-associated mortality and have been included in guidelines in many countries worldwide. Mortality among patients with HIV in hospital has been summarised, but the outcomes of patients after hospital discharge are less well understood.
Added value of this study
This systematic review provides summary estimates of the high rates of death or readmission following hospital discharge among people with HIV, and identified several studies reporting on risk factors that affect post-discharge outcomes. The proportion of patients with adverse outcomes has remained unchanged since 2016 and was similar in high-income and low-income settings. Post-discharge mortality and readmissions were associated with advanced HIV disease, lack of antiretroviral therapy, and discharge against medical advice among patients who were admitted to hospital.
Implications of all the available evidence
Ensuring adequate care for individuals with advanced HIV disease continues to be a significant challenge in many high burden settings. These findings emphasise the need for continued efforts to ensure that all people with HIV are taking antiretroviral therapy and that better support is provided for post-discharge referral and appropriate post-discharge linkage and management, particularly for individuals with low CD4 cell counts at discharge. It is important that programmes are able to collect data and report outcomes for people with HIV who are admitted to hospital to better inform progress towards global targets. Approaches are needed to identify individuals at the highest risk of poor outcomes and to provide adapted support.
Methods
Search strategy and selection criteria
This systematic review and meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.15 The study protocol is available in appendix 3 (pp 5–8).
To be included, studies had to report outcomes among people living with HIV following discharge from hospital. We were specifically interested in studies that reported outcomes following hospital discharge after Jan 1, 2003, when ART scale-up in low-income countries began. Studies had to report outcomes for at least 20 patients following discharge. We searched MEDLINE via PubMed and Embase from Jan 1, 2003 to Nov 30, 2021, using a highly sensitive search strategy that combined terms for HIV infection, hospital admission or readmission, and discharge, without language, geographical, or age restrictions. Full search strategies are available in the protocol (appendix 3 pp 5–8). We also screened references of review articles and all included full-text articles, and all articles that were included in a previous systematic review of outcomes after hospital admission.1 We searched conference abstracts from the International AIDS Society and Conferences on Retroviruses and Opportunistic Infections from 2016 onwards to identify studies that had been completed, but not yet published as full-text articles. Study inclusion was by consensus with disagreements resolved through discussion.
Data analysis
Two reviewers (NF and AR), working independently in pairs, extracted data in accordance with a predefined data extraction sheet. If outcomes from the same cohort were published across different publications, each outcome was only reported once. Outcomes of interest were the proportion of patients who died, were readmitted to hospital, and were successfully linked to care after hospital discharge. We also extracted data about study setting, age, sex, length of hospital stay, diagnosis at index admission, history of previous admission, and CD4 cell count at discharge. Indicators of risk of bias were extracted using adapted items from the Newcastle-Ottawa scale.16 We calculated proportions and corresponding 95% CIs for all reported outcomes, and pooled data after transformation17, 18 using random-effects meta-analysis.19 We calculated a composite adverse outcome of death and hospital readmission. For studies in which loss to follow-up was reported, estimates were based on available cases. We did sensitivity analyses to assess differences in the proportion of patients who died following discharge or were readmitted to hospital by study location, duration of follow-up, advanced HIV disease status at admission, country economic status, and recency of publication (studies that reported outcomes up to the end of 2015 vs studies that reported outcomes from 2016 onwards); these subgroup proportions were compared using a two-sample z-test. Statistical tests for heterogeneity do not work well with pooled proportions, thus we assessed sources of heterogeneity through visual inspection of forest plot and exploration of outliers. We analysed all data with Stata (version 15.0).
Role of the funding source
The funder of the study had no role in study design, data interpretation, or writing of the report.
Results
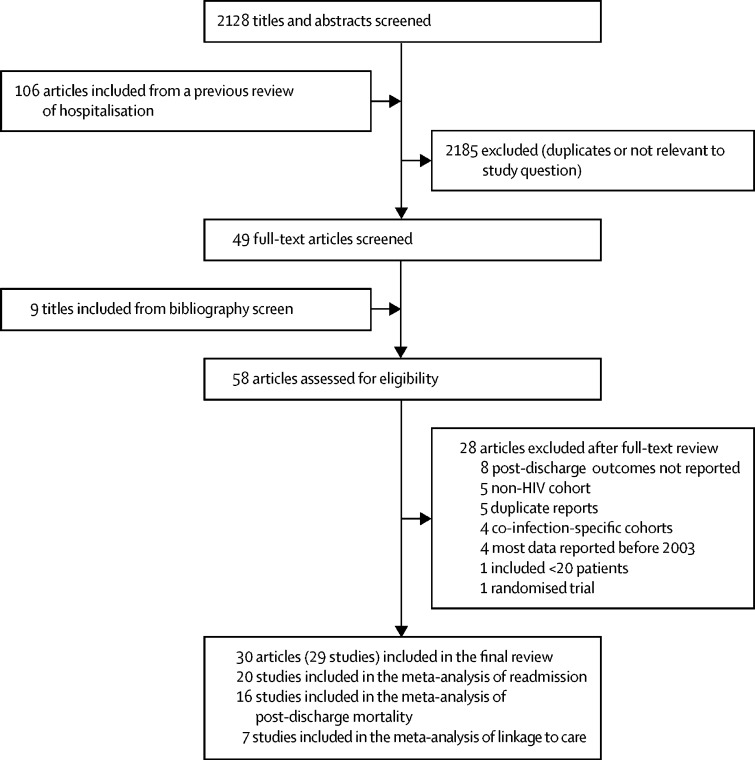
From an initial screen of 2128 papers, 29 studies met the eligibility criteria and were included in the systematic review, 20 of which were included in the meta-analysis of readmission, six were included in the meta-analysis of post-discharge mortality, and seven were included in the meta-analysis of linkage to care (figure 1);5, 11, 12, 13, 14, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44 one study reported outcomes in two separate publications.36, 37 Two studies were excluded because they reported post-discharge outcomes only for patients who were admitted for cryptococcal meningitis.45, 46 One study was excluded because it reported outcomes among children admitted with complicated severe acute malnutrition.47 Another study was excluded as it was a randomised trial assessing early initiation of ART among severely ill patients admitted to an intensive care unit in Brazil that was terminated due to slow recruitment.48 The 29 studies provided information about post-discharge outcomes for 92 781 patients. Most studies were from North America;11, 12, 13, 14, 20, 21, 24, 25, 29, 30, 31, 33, 34, 40, 44 nine studies were from Africa, including five from South Africa,5, 23, 27, 38, 43 one from Malawi,26 one from Mozambique,36, 37 one from Tanzania,41 and one from Zambia;32 two studies were from southeast Asia;22, 35 one study was from Latin America;28 and two studies were from Europe (table).39, 42 The study from Mozambique reported outcomes in children;36, 37 all other studies were done in adults. 11 studies reported the proportion of patients with advanced HIV disease (CD4 count <200 cells per μL),5, 11, 12, 13, 28, 29, 32, 35, 36, 37, 41 which ranged from 16% to 91%. 11 studies reported length of hospital stay,5, 11, 12, 13, 23, 26, 28, 29, 32, 43, 44 which ranged from 4 days to 12 days.
Figure 1.
Study selection
Table.
Studies included in the systematic review
| Setting | Population | Study period | HIV-positive patients with outcomes, n | Men | Women | Age, years | Patients on ART, n (%) |
CD4 count |
Length of stay, days | Primary index admission | Post-discharge follow-up, days | Risk factors for readmission or post-discharge mortality | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | <200 cells per μL | |||||||||||||
| Alfandre et al20 | USA | Adults | 2012–13 | 33 270 | 17 896 | 15 374 | >40 (81% of study population) | .. | .. | .. | .. | .. | 30 | Discharged against medical advice |
| Antoniou et al21 | Canada | Medically complex and socially vulnerable adults | 2009–15 | 268 | 222 | 46 | 49 | .. | .. | .. | .. | .. | 30 | .. |
| Ayudhya et al22 | Thailand | Adults | 2013 | 140* | 76 | 44 | 40 | .. | 160 (52–407) | .. | .. | .. | 30 | .. |
| Beckwith et al23 | South Africa | Adults | 2013–15 | 151 | 73 | 78 | 39 | 92 (61%)† | .. | 91% (<100 cells μL) | 5 | AIDS-related illness; tuberculosis | 30 | .. |
| Berry et al24 | USA | Adults | 2013–15 | 45 382 admissions (33 556 individuals) | 30 086 | 15 296 | 37% 45–54 (37% of study population) | .. | .. | .. | .. | Non-AIDS defining infection | 30 | .. |
| Campbell et al25 | USA | HIV-positive patients | 2019 | 389 | .. | .. | (78%) | .. | .. | .. | .. | 30 | .. | |
| Chawla et al26 | Malawi | Adults | 2013 | 1001 | 475 | 526 | 31–40 (38% of study population) | .. | .. | .. | 4 | .. | 30 | .. |
| Cichowitz et al27 | South Africa | Adults | 2014 | 168 (136 HIV-positive at admission) | 61 | 76 | 37 | 88 (65%) | 56 (23–372) | .. | .. | 180 | .. | |
| Coelho et al28 | Brazil | Adults | 2007–13 | 1861 admitted to hospital; 1442 index hospitalisations | 932 | 510 | 40 | 1080 (75%) | .. | 47% | 12 | AIDS-related illness | 30 | Low CD4 cell count at admission; longer length of stay; discharged against medical advice |
| Colasanti et al29 | USA | Adults newly diagnosed with HIV in hospital | 2011–12 | 94 | 72 | 22 | 43 | 0 | 134 (30–307) | .. | 10 | .. | 730 | .. |
| Davy-Mendez et al12 | USA | Adults (41% men who have sex with men) | 1996–2016 | 2006 | 1376 | 630 | 37 | .. | .. | 16% | 7 | .. | 30 | Low CD4 cell count at admission |
| English et al30 | USA | Adults | 2010–13 | 417 | 304 | 113 | <50 (75% of study population) | .. | .. | 65% | .. | .. | .. | |
| Gibson et al14 | USA | Adults | 2015–16 | 918 | 652 | 266 | 43 | .. | .. | .. | AIDS-related illness | 30 | Discharged against medical advice | |
| Gupta and Dhanireddy31 | USA | HIV-positive patients | 2007–12 | 850 | − | .. | .. | .. | .. | .. | .. | .. | 90 | .. |
| Haachambwa et al32 | Zambia | Adults | 2017–18 | 239 | 96 | 143 | 36 | 206 (86%) | 181 (52–301) | .. | 12 | Pulmonary (including tuberculosis) | 74 | |
| Hadlock et al33‡ | USA | Adults | 2010–14 | 908 | .. | 48 | .. | .. | 55% | .. | .. | 30 | ||
| Hoffmann et al5 | South Africa | Adults | 2016 | 121 | 54 | 67 | 40 | 81 (67%) | 260 (113–464) | .. | 6 | Pulmonary (including tuberculosis) | 180 | Longer length of stay; no linkage to care following discharge |
| Hsieh et al34 | USA | Febrile adults who inject drugs | 1998–2004 | 82 | .. | .. | .. | .. | 248 (2–1033) | .. | .. | .. | 90 | |
| Khawcharoenporn et al35 | Thailand | Adults | 2013–15 | 240 | 138 | 102 | 37 | 103 (43%) | 158 (72–382) | .. | .. | ..- | 30 | |
| Madrid et al36, 37 | Mozambique | Children | 2000–16 | 258 | .. | .. | 1–5 (57% of study population) | .. | .. | .. | .. | .. | 90 | |
| Meintjes et al38 | South Africa | Adults | 2012–13 | 585 | 247 | 338 | 35 | 263 (45%) | 134 (53–275) | .. | Tuberculosis (33·5%) | 90 | ||
| Morquin et al39 | France | Adults in intensive care unit | 1997–2008 | 98 | 69 | 29 | 43 | 53 (54%) | .. | 55% | .. | Respiratory and neurological failure | 365 | Low CD4 cell count at admission |
| Nijhawan et al13 | USA | Adults | 2011 | 930 | .. | .. | 45 | .. | .. | 62% | 5·5 | .. | 30 | Not being on ART |
| Nijhawan et al11 | USA | Adults | 2006–08 | 1509 | 1102† | 407† | 43 | .. | .. | 52% | 7 | AIDS-related illness | 30 | |
| Parent et al40 | Canada | Adults | 1996–2015 | 7013 | 5649 | 1364 | 43 | 7013 (100%) | .. | 28% | .. | .. | 30 | Discharged against medical advice |
| Peck et al41 | Tanzania | Adults | 2013 | 143 | 47 | 58 | 47 | 105 (100%) | .. | .. | .. | .. | 365 | Longer length of stay or lack of linkage <1 month post discharge |
| Shaaban et al42 | Portugal | Adults | 2009–14 | 37 134 | 25 060 | 12 074 | 44 | .. | .. | .. | .. | .. | 30 | Discharged against medical advice |
| Stuart-Clark et al43 | South Africa | Adults | 2009 | 146 | .. | 39 | 56 (38%) | 111 (61–231) | .. | 6 | .. | 365 | ||
| Tang et al44 | USA | Adults | 2009–12 | 185 | .. | 50 | .. | .. | .. | 5 | .. | 30 | .. | |
ART=antiretroviral therapy.
140 patients admitted to hospital, but data on characteristics only provided for 120 patients.
Estimated from overall sample (numbers not reported in original study).
Characteristics provided for the 60 patients who were readmitted to hospital.
Overall, studies were rated as being at moderate risk of bias. 16 studies reported outcomes for all patients, 19 studies reported disaggregated outcomes per patient, and all 29 studies reported outcomes for at least 30 days after discharge. 13 studies reported vital status for all discharged patients and 12 studies either reported previous admission status or excluded patients with previous admissions from the study (appendix 3 p 2). There was moderate heterogeneity in outcomes, consistent with differences in disease severity at discharge, duration between discharge and readmission, and post-discharge planning and linkage to care. In subgroup analysis, outcomes also differed by geographical region and country income level.
Six studies (4487 admissions) reported in-hospital mortality; these studies were done in the USA,12, 25 South Africa,5, 38 Tanzania,41 and Zambia.32 Mortality prior to discharge ranged from 1·7% (95% CI 1·2–2·3) to 26·7% (19·9–34·2), indicating substantial heterogeneity, with an overall pooled proportion of 6·1% (3·1–9·1).
Seven studies5, 21, 22, 29, 30, 35, 41 (1296 admissions) reported the proportion of patients who were successfully linked to care after hospital discharge (defined as linkage to HIV care, outpatient care, or community care). The proportion of patients who were successfully linked to care after discharge ranged from 10·9% (95% CI 7·0–15·5) to 79·1% (71·5-85·8%), with an overall pooled proportion of 41·6% (23·6–59·6).
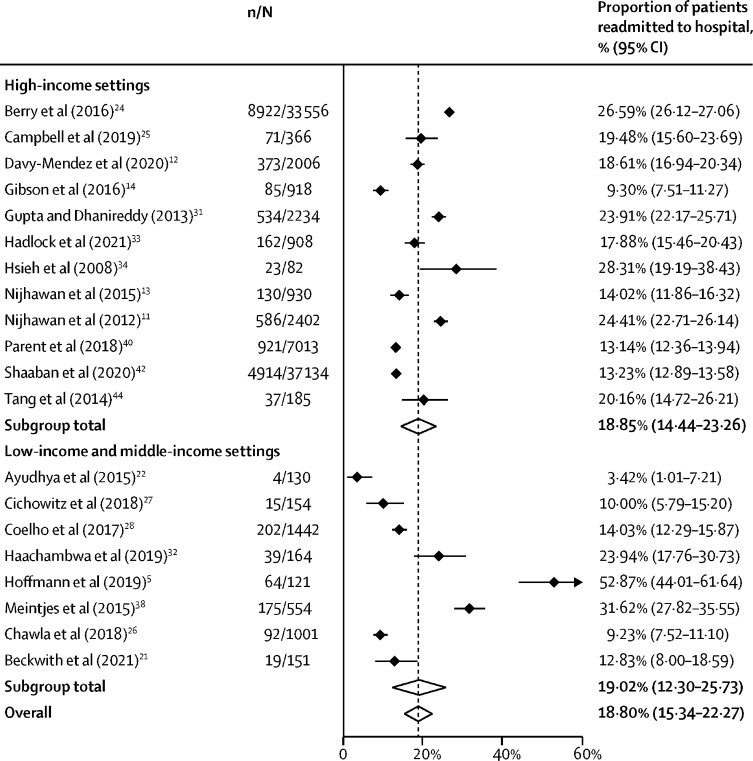
20 studies (91451 admissions) reported the number of patients readmitted to care after hospital discharge,5, 11, 12, 13, 14, 22, 23, 24, 25, 26, 27, 28, 31, 32, 33, 34, 38, 40, 42, 44 of which, 14 studies reported readmission within 30 days of discharge. The proportion of patients readmitted post-discharge ranged from 3·4% (1·0–7·2) to 52·9% (44·0–61·6), with an overall pooled proportion of 18·8% (15·3–22·3; figure 2). The pooled proportion of patients readmitted to hospital was also higher for studies that reported readmissions that occurred after 30 days (figure 3). One study reported that the risk of readmission within 30 days of discharge was higher for people living with HIV who had been discharged against medical advice; however, there were insufficient data to include this in the meta-analysis.20
Figure 2.
Post-discharge readmission by study setting
n=number of readmissions. N=total number of patients. Black diamonds show point estimates, white diamonds show pooled estimates, and the dashed line shows the overall pooled estimate.
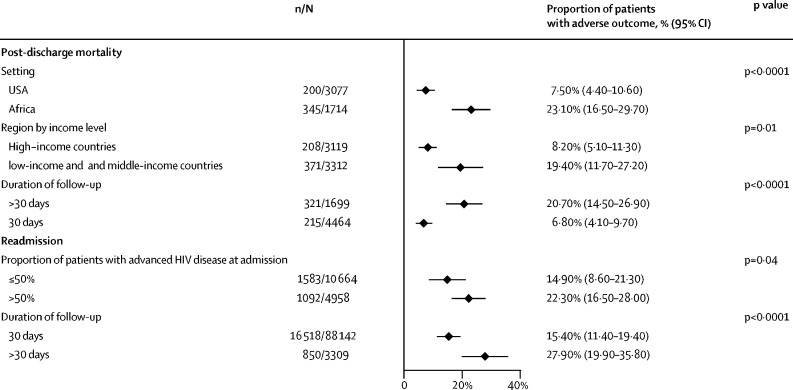
Figure 3.
Post-discharge mortality and readmissions by setting, region, duration of follow-up, and advanced HIV status at admission
n=number of events. N=total number of patients.
In sensitivity analysis, no differences were identified in the proportion of patients readmitted to hospital comparing studies published before 2016 and those published after 2016, when universal ART was introduced. No differences in the proportion of patients readmitted to hospital were identified when comparing studies from the USA and Africa, and high-income countries compared with low-income and middle-income settings. The proportion of readmissions was higher in studies in which the majority of patients had advanced HIV disease at admission than those in which less than half of patients had advanced HIV disease at admission (figure 3).
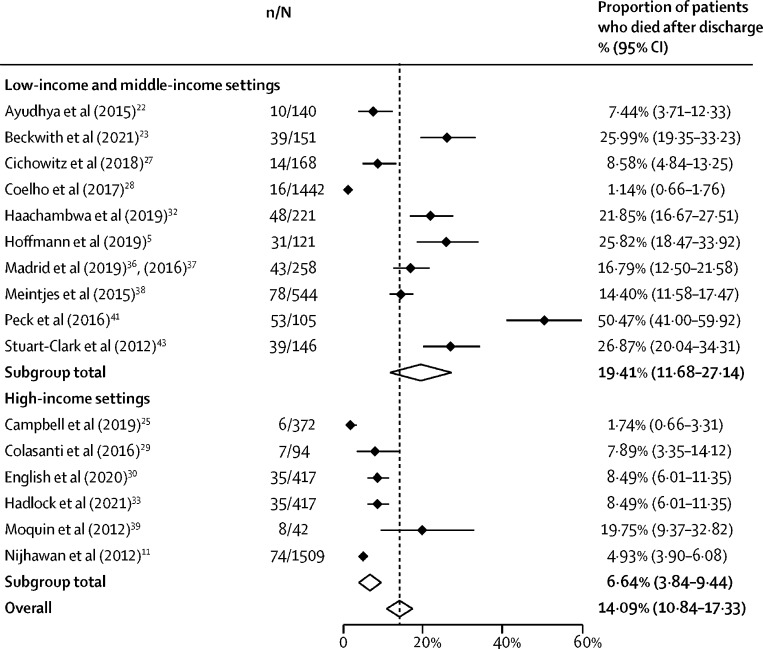
16 studies (6163 patients) reported the number of patients who died after discharge.5, 13, 22, 23, 25, 27, 28, 29, 30, 32, 33, 36, 38, 39, 41, 43 The proportion of patients who died after discharge ranged from 1·1% (95% CI 0·7–1·7) to 50·5% (41·0–59·9), with an overall pooled proportion of 14·1% (10·8–17·3) (figure 4). In sensitivity analysis, no difference was identified in the proportion of patients who died following discharge when comparing studies published before 2016 and studies published after 2016. Post-discharge mortality was higher in studies from Africa than studies from the USA, and from studies done in low-income countries and middle-income countries compared with high-income countries. Post-discharge mortality was higher in studies in which people were followed up for longer than 30 days (figure 3).
Figure 4.
Post-discharge mortality by study setting
n=number of deaths. N=total number of patients. Black diamonds show point estimates, white diamonds show pooled estimates, and the dashed line shows the overall pooled estimate.
11 studies (6598 admissions) provided data on both the number of patients who were readmitted and the number who died following discharge.5, 11, 21, 22, 23, 25, 27, 28, 32, 33, 38 The proportion of patients with this composite adverse outcome ranged from 11·0% (95% CI 6·3–17·0) to 78·3% (70·6–85·1), with a pooled proportion of 31·7% (23·9–39·5).
Post-discharge mortality was associated with a lower CD4 cell count11, 39 and lack of linkage to care within 1 month after discharge.41 A US study reported that inpatient treatment with ART during hospitalisation reduced the risk of short-term mortality.25 A study from Tanzania reported that more than half of adults living with HIV had died within 12 months of hospital discharge, and nearly a third had died within the first 3 months, with a 2 times higher adjusted risk of post-discharge mortality compared with HIV-negative adults.41 The high mortality in this study might be the result of the condition of advanced HIV disease among individuals who were admitted, and although this study did not report information on CD4 cell count, early linkage to primary HIV care was associated with a 75% lower incidence of post-discharge mortality. Reported risk factors for readmission included low CD4 cell count at admission,12, 28 longer length of stay,5, 28 not being on ART,13 discharge against medical advice,14, 20, 28, 40, 42 and not linking to care after discharge.5 A US study of febrile people who inject drugs reported a higher rehospitalisation rate among those with newly diagnosed HIV infection than those with known HIV infection (40% vs 26%), highlighting the importance of tailored support for this patient group as part of discharge plans.34
Six studies reported outcomes for people living with HIV and those who were HIV-negative. In Tanzania, 28·9% of adults with HIV-infected died within the first 3 months after discharge compared with 17·7% of HIV-negative adults.41 In Mozambique, children with HIV had a higher rate of post-discharge mortality than did children without HIV (hazard ratio [HR] 1·77 [95% CI 1·07–2·91]).36, 37 Two US studies found that HIV infection was associated with readmission. The first study found the risk of readmission was 1·5 times higher (95% CI 1·46–1·54) among adults with HIV than those without HIV.24 The second study was among people who inject drugs and reported a HR of 2·90 (1·20–7·02) for readmission comparing people with HIV with those without HIV.34 A study from Malawi reported that patients with HIV who were discharged from hospital had a higher risk of readmission than HIV-negative individuals (adjusted risk ratio 2·41 [95% CI 1·64–3·53]).26 In contrast, a study from South Africa found no difference in readmission, death, or loss to follow-up by HIV status.27
Discussion
This systematic review summarises outcomes of a population of people living with HIV at high risk of death. We found that almost a third of patients with HIV had an adverse outcome after hospital discharge, (mortality or readmission to hospital), mostly within 30 days of discharge. Where comparative information by serostatus was available, outcomes were generally worse for people living with HIV. This finding is consistent with a previous study, not included in this review, among children admitted with complicated severe acute malnutrition in Zambia and Zimbabwe; in this study, children who were HIV-positive had an almost four times higher risk of post-discharge mortality than HIV-negative children, regardless of ART initiation.47 This finding represents a missed opportunity to reduce HIV-associated mortality, and results in increased utilisation of health-care resources. Post-discharge mortality was higher in low-income and middle-income countries, in particular when comparing Africa and the USA. No apparent decrease was observed in the proportion of people with HIV who had adverse outcomes post-discharge when comparing studies done before 2016 with those done from 2016 onwards, when initiation of ART is recommended as soon as a positive HIV diagnosis is confirmed.49
The majority of adverse outcomes occurred within 30 days following discharge, but the proportion of patients who had an adverse outcome overall was higher in studies that followed up patients for longer durations. 30-day readmission rate is commonly used as an indicator for quality of hospital care, but follow-up over a longer time period provides a better estimate of adverse events after discharge and helps to identify a larger proportion of patients at risk of mortality and readmission. Programmes should consider patient follow-up after the 30-day discharge period to account for adverse outcomes and to enable intervention to reduce such outcomes, similar to that recommended for other areas of patient care.50
Several studies included provide insights into risk factors for adverse outcomes and potential interventions to reduce mortality and readmission following discharge. In subgroup analyses, readmissions were more common in studies in which a higher proportion of index admissions had advanced HIV disease. Several studies reported that mortality post-discharge was associated with a lower CD4 cell count,11, 38 whereas initiation of ART in hospital25 was associated with decreased mortality. Risk factors for readmission included discharge against medical advice,14, 20, 28 not being on ART,13 having an AIDS-defining illness,11 low CD4 cell count,12, 28 high viral load,12 and no support for linkage to care.5 One study reported that 18% of patients on ART were readmitted within 30 days compared with 26% of patients who were not on ART, highlighting the importance of ensuring patients who are not on ART and have no contraindications are started on treatment before being discharged.25
The provision of patient support for linkage to care after discharge is an important strategy to reduce readmission and improve outcomes. This systematic review included a study from Thailand, which found that an intervention bundle including enhanced care during admission and appointment scheduling and reminders post-discharge was associated with significantly higher HIV care engagement post-discharge.35 These observations are consistent with findings from a systematic review, which found that patient-centred discharge instructions and telephone follow-up calls were common components of effective intervention bundles to reduce 30-day readmission.51
We used a broad search to identify a large number of studies reporting readmission and death after discharge across a range of settings. Post-discharge mortality was higher in studies that reported outcomes over a longer follow-up period, suggesting that the pooled estimate of post-discharge mortality would be higher if studies had longer follow-up periods. There are several other limitations to note. Because this systematic review was not primarily focused on mortality during admission, the reported estimates are not representative of all studies reporting this outcome—eg, a previous systematic review of causes of hospital admission found that mortality among individuals admitted to hospital was 20% for adults and 14% for children.1 Importantly, many programmes will underestimate negative post-discharge outcomes because these outcomes have not been detected in routine information systems or patients attended a clinic outside the catchment area of the information system. Reporting from research settings that have interventions in place to improve ascertainment of outcomes might not be representative of outcomes within routine programmes with fewer resources. We investigated risk of readmission post-discharge, but it is likely that some of the index admissions were in fact readmissions from a recent hospital discharge. Previous hospitalisation, a risk factor for readmission,52 was infrequently reported but might explain some of the adverse outcomes reported. Palliative care provision was not reported; anticipated deaths following discharge to palliative care might have occurred but were not reported and their inclusion effectively misclassifies post-discharge mortality as an adverse outcome.53 Most studies included were from high-income countries and reported outcomes among adults; no studies from west and central Africa, and few studies from southeast Asia or the Western Pacific region were included. Although this paucity of reported information from these regions does not necessarily represent publication bias, it does highlight the need for data from a broader set of patient populations and countries. A number of studies did not account for outcomes among patients who were lost to follow-up after discharge, thus estimates of adverse outcomes are likely to be an underestimate, particularly because studies were unable to correct status ascertainment through linkage to vital registration systems.54, 55 Outcomes were inconsistently reported by the studies, with only around a quarter of studies reporting linkage to care and around a half reporting mortality after discharge. Key study characteristics were also inconsistently reported, such as length of hospital stay, CD4 cell count, and ART status.
In conclusion, this systematic review found high rates of mortality and readmission after hospital discharge of people living with HIV, highlighting the importance of ensuring post-discharge referral and appropriate post-discharge management to improve outcomes among these vulnerable patients. Further research and investment is needed to identify feasible approaches targeting individuals at highest risk of poor outcomes after discharge and to provide adapted support to ensure appropriate linkage and continuity of support post-discharge, including ART.
Date sharing
All data are available in the original published articles included in this systematic review, and are available upon request from the corresponding author.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
We would like to thank Kavita Kothari and Tomas Allen for their support in designing the search strategy, Steve Kanters for statistical advice, and José Imbernon, Carmen Pérez Casas, and Omar Sued for support with translations.
Contributors
NF, TE, and GP conceptualised and designed the study. NF, GP, and AR were involved with data acquisition, analysis, or interpretation. NF and AR verified the data. NF drafted the manuscript. All authors critically revised and drafted the manuscript for important intellectual content, including data interpretation in the broader context. TE oversaw the study. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Supplementary Material
References
- 1.Ford N, Shubber Z, Meintjes G, et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. Lancet HIV. 2015;2:e438–e444. doi: 10.1016/S2352-3018(15)00137-X. [DOI] [PubMed] [Google Scholar]
- 2.Wajanga BM, Webster LE, Peck RN, et al. Inpatient mortality of HIV-infected adults in sub-Saharan Africa and possible interventions: a mixed methods review. BMC Health Serv Res. 2014;14:627. doi: 10.1186/s12913-014-0627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akinkuotu A, Roemer E, Richardson A, et al. In-hospital mortality rates and HIV: a medical ward review, Lilongwe, Malawi. Int J STD AIDS. 2011;22:465–470. doi: 10.1258/ijsa.2011.011021. [DOI] [PubMed] [Google Scholar]
- 4.Myer L, Smith E, Mayosi BM. Medical inpatient mortality at Groote Schuur Hospital, Cape Town, South Africa, 2002-2009. S Afr Med J. 2012;103:28–31. doi: 10.7196/samj.6285. [DOI] [PubMed] [Google Scholar]
- 5.Hoffmann CJ, Milovanovic M, Cichowitz C, Kinghorn A, Martinson NA, Variava E. Readmission and death following hospitalization among people with HIV in South Africa. PLoS One. 2019;14 doi: 10.1371/journal.pone.0218902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laher AE, Paruk F, Venter W, Ayeni OA, Richards GA. Predictors of in-hospital mortality among HIV-positive patients presenting with an acute illness to the emergency department. HIV Med. 2021;22:557–566. doi: 10.1111/hiv.13097. [DOI] [PubMed] [Google Scholar]
- 7.Matoga MM, Rosenberg NE, Stanley CC, et al. Inpatient mortality rates during an era of increased access to HIV testing and ART: a prospective observational study in Lilongwe, Malawi. PLoS One. 2018;13 doi: 10.1371/journal.pone.0191944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nemetchek B, English L, Kissoon N, et al. Paediatric postdischarge mortality in developing countries: a systematic review. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2018-023445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiens MO, Pawluk S, Kissoon N, et al. Pediatric post-discharge mortality in resource poor countries: a systematic review. PLoS One. 2013;8 doi: 10.1371/journal.pone.0066698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Long LC, Evans D, Rosen S, et al. Can routine inpatient mortality data improve HIV mortality estimates? Inpatient mortality at an urban hospital in South Africa. S Afr Med J. 2018;108:870–875. doi: 10.7196/SAMJ.2018.v108i10.13002. [DOI] [PubMed] [Google Scholar]
- 11.Nijhawan AE, Clark C, Kaplan R, Moore B, Halm EA, Amarasingham R. An electronic medical record-based model to predict 30-day risk of readmission and death among HIV-infected inpatients. J Acquir Immune Defic Syndr. 2012;61:349–358. doi: 10.1097/QAI.0b013e31826ebc83. [DOI] [PubMed] [Google Scholar]
- 12.Davy-Mendez T, Napravnik S, Wohl DA, et al. Hospitalization rates and outcomes among persons living with human immunodeficiency virus in the southeastern United States, 1996–2016. Clin Infect Dis. 2020;71:1616–1623. doi: 10.1093/cid/ciz1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nijhawan AE, Kitchell E, Etherton SS, Duarte P, Halm EA, Jain MK. Half of 30-day hospital readmissions among HIV-infected patients are potentially preventable. AIDS Patient Care STDS. 2015;29:465–473. doi: 10.1089/apc.2015.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gibson MP, Nijhawan AE, Jain MK, Halm E. Thirty-day readmissions among HIV-infected individuals at a safety-net hospital: predictors and preventability. Open Forum Infect Dis. 2016;3(suppl 1):3. [Google Scholar]
- 15.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells G, Shea B, O'Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 17.Freeman MFTJ, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21:607–611. [Google Scholar]
- 18.Miller J. The inverse of the Freeman-Tukey double arcsine transformation. Am Stat. 1978;32:138. [Google Scholar]
- 19.Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res. 1993;2:121–145. doi: 10.1177/096228029300200202. [DOI] [PubMed] [Google Scholar]
- 20.Alfandre D, Yang J, Harwood K, et al. “Against medical advice” discharges among HIV-infected patients: health and health services outcomes. J Assoc Nurses AIDS Care. 2017;28:95–104. doi: 10.1016/j.jana.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Antoniou T, Graves E, Plumptre L, Stewart A, Chan Carusone S. Antiretroviral prescription pick-up and physician follow-up after hospital discharge among medically complex people with HIV. Open Forum Infect Dis. 2019;6 doi: 10.1093/ofid/ofz009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayudhya DPN, Khawcharoenporn T. HIV care engagement within 30 days after hospital discharge among patients from a Thai tertiary-care centre. Int J STD AIDS. 2015;26:467–469. doi: 10.1177/0956462414543843. [DOI] [PubMed] [Google Scholar]
- 23.Beckwith PG, Tlali M, Charalambous S, et al. Causes and outcomes of admission and investigation of tuberculosis in adults with advanced HIV in South African hospitals: data from the TB Fast Track Trial. Am J Trop Med Hyg. 2021;105:1662–1671. doi: 10.4269/ajtmh.21-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berry SA, Fleishman JA, Moore RD, Gebo KA. Thirty-day hospital readmissions for adults with and without HIV infection. HIV Med. 2016;17:167–177. doi: 10.1111/hiv.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell J, Polk C, Roshdy D, Leonard M. Inpatient initiation of art improves short-term mortality in people living with HIV. Open Forum Infect Dis. 2019;6(suppl 2):S479. [Google Scholar]
- 26.Chawla KS, Rosenberg NE, Stanley C, et al. HIV and early hospital readmission: evaluation of a tertiary medical facility in Lilongwe, Malawi. BMC Health Serv Res. 2018;18:225. doi: 10.1186/s12913-018-3050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cichowitz C, Pellegrino R, Motlhaoleng K, Martinson NA, Variava E, Hoffmann CJ. Hospitalization and post-discharge care in South Africa: a critical event in the continuum of care. PLoS One. 2018;13 doi: 10.1371/journal.pone.0208429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coelho LE, Ribeiro SR, Japiassu AM, et al. Thirty-day readmission rates in an HIV-infected cohort from Rio de Janeiro, Brazil. J Acquir Immune Defic Syndr. 2017;75:e90–e98. doi: 10.1097/QAI.0000000000001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colasanti J, Goswami ND, Khoubian JJ, et al. The perilous road from HIV diagnosis in the hospital to viral suppression in the outpatient clinic. AIDS Res Hum Retroviruses. 2016;32:729–736. doi: 10.1089/aid.2015.0346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.English K, May SB, Davila JA, et al. Retention in care and viral load improvement after discharge among hospitalized out-of-care people with HIV infection: a post hoc analysis of a randomized controlled trial. Open Forum Infect Dis. 2020;7 doi: 10.1093/ofid/ofaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gupta R, Dhanireddy S. Hospital readmissions among indigent HIV-infected patients: a movement toward medical home model interventions. J Gen Intern Med. 2013;28:S90–S91. [Google Scholar]
- 32.Haachambwa L, Kandiwo N, Zulu PM, et al. Care continuum and postdischarge outcomes among HIV-infected adults admitted to the hospital in Zambia. Open Forum Infect Dis. 2019;6 doi: 10.1093/ofid/ofz336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hadlock GC, Moleres KA, Pineda LJ, Jakeman B. Risk factors for potentially preventable hospital readmissions among persons living with human immunodeficiency virus infection. AIDS Care. 2021;33:306–310. doi: 10.1080/09540121.2019.1709613. [DOI] [PubMed] [Google Scholar]
- 34.Hsieh YH, Rothman RE, Bartlett JG, Yang S, Kelen GD. HIV seropositivity predicts longer duration of stay and rehospitalization among nonbacteremic febrile injection drug users with skin and soft tissue infections. J Acquir Immune Defic Syndr. 2008;49:398–405. doi: 10.1097/qai.0b013e318183ac84. [DOI] [PubMed] [Google Scholar]
- 35.Khawcharoenporn T, Damronglerd P, Chunloy K, Sha BE. Enhanced inpatient rounds, appointment reminders, and patient education improved HIV care engagement following hospital discharge. Int J STD AIDS. 2018;29:641–649. doi: 10.1177/0956462417749420. [DOI] [PubMed] [Google Scholar]
- 36.Madrid L, Casellas A, Sacoor C, et al. Postdischarge mortality prediction in sub-Saharan Africa. Pediatrics. 2019;143 doi: 10.1542/peds.2018-0606. [DOI] [PubMed] [Google Scholar]
- 37.Madrid L, Sitoe A, Aldea M, et al. Mortality following discharge in children admitted to a rural mozambican hospital: development of a prediction model to identify children at risk of death. Am J Trop Med Hyg. 2016;95:531. [Google Scholar]
- 38.Meintjes G, Kerkhoff AD, Burton R, et al. HIV-related medical admissions to a South African district hospital remain frequent despite effective antiretroviral therapy scale-up. Medicine. 2015;94 doi: 10.1097/MD.0000000000002269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morquin D, Le Moing V, Mura T, et al. Short- and long-term outcomes of HIV-infected patients admitted to the intensive care unit: impact of antiretroviral therapy and immunovirological status. Ann Intensive Care. 2012;2:25. doi: 10.1186/2110-5820-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parent S, Barrios R, Nosyk B, et al. Impact of patient-provider attachment on hospital readmissions among people living with HIV: a population-based study. J Acquir Immune Defic Syndr. 2018;79:551–558. doi: 10.1097/QAI.0000000000001857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peck RN, Wang RJ, Mtui G, et al. Linkage to primary care and survival after hospital discharge for HIV-infected adults in Tanzania: a prospective cohort study. J Acquir Immune Defic Syndr. 2016;73:522–530. doi: 10.1097/QAI.000000000001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shaaban AN, Dias SS, Muggli Z, Peleteiro B, Martins MRO. Risk of readmission among HIV patients in public Portuguese hospitals: longitudinal multilevel population-based study. Front Public Health. 2020;8:15. doi: 10.3389/fpubh.2020.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stuart-Clark H, Vorajee N, Zuma S, et al. Twelve-month outcomes of patients admitted to the acute general medical service at Groote Schuur Hospital. S Afr Med J. 2012;102:549–553. doi: 10.7196/samj.5615. [DOI] [PubMed] [Google Scholar]
- 44.Tang N, Maselli JH, Gonzales R. Variations in 30-day hospital readmission rates across primary care clinics within a tertiary referral center. J Hosp Med. 2014;9:688–694. doi: 10.1002/jhm.2243. [DOI] [PubMed] [Google Scholar]
- 45.Kitonsa J, Mayanja Y, Aling E, et al. Factors affecting mortality among HIV positive patients two years after completing recommended therapy for cryptococcal meningitis in Uganda. PLoS One. 2019;14 doi: 10.1371/journal.pone.0210287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sathirapanya P, Ekpitakdamrong N, Chusri S, Pruphetkaew N, Chongphattararot P, Nanphan P. Predictors of hospital discharge outcome from the presenting clinical characteristics and the first cerebrospinal fluid analysis among the patients with cryptococcal meningitis. Clin Neurol Neurosurg. 2019;186 doi: 10.1016/j.clineuro.2019.105539. [DOI] [PubMed] [Google Scholar]
- 47.Bwakura-Dangarembizi M, Dumbura C, Amadi B, et al. Risk factors for postdischarge mortality following hospitalization for severe acute malnutrition in Zimbabwe and Zambia. Am J Clin Nutr. 2021;113:665–674. doi: 10.1093/ajcn/nqaa346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boniatti MM, Pellegrini JAS, Marques LS, et al. Early antiretroviral therapy for HIV-infected patients admitted to an intensive care unit (EARTH-ICU): a randomized clinical trial. PLoS One. 2020;15 doi: 10.1371/journal.pone.0239452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.WHO . World Health Organization; Geneva: 2016. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations.https://www.who.int/hiv/pub/guidelines/keypopulations-2016/en/ [PubMed] [Google Scholar]
- 50.Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day readmissions: the clock is ticking. JAMA. 2013;309:345–346. doi: 10.1001/jama.2012.205110. [DOI] [PubMed] [Google Scholar]
- 51.Sawan MJ, Wennekers D, Sakiris M, Gnjidic D. Interventions at hospital discharge to guide caregivers in medication management for people living with dementia: a systematic review. J Gen Intern Med. 2021;36:1371–1379. doi: 10.1007/s11606-020-06442-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Feller DJ, Akiyama MJ, Gordon P, Agins BD. Readmissions in HIV-infected inpatients: a large cohort analysis. J Acquir Immune Defic Syndr. 2016;71:407–412. doi: 10.1097/QAI.0000000000000876. [DOI] [PubMed] [Google Scholar]
- 53.Vasilevskis EE, Kuzniewicz MW, Cason BA, et al. Predictors of early postdischarge mortality in critically ill patients: a retrospective cohort study from the California Intensive Care Outcomes project. J Crit Care. 2011;26:65–75. doi: 10.1016/j.jcrc.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anderegg N, Johnson LF, Zaniewski E, et al. All-cause mortality in HIV-positive adults starting combination antiretroviral therapy: correcting for loss to follow-up. AIDS. 2017;31(suppl 1):S31–S40. doi: 10.1097/QAD.0000000000001321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Van Cutsem G, Ford N, Hildebrand K, et al. Correcting for mortality among patients lost to follow up on antiretroviral therapy in South Africa: a cohort analysis. PLoS One. 2011;6 doi: 10.1371/journal.pone.0014684. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are available in the original published articles included in this systematic review, and are available upon request from the corresponding author.