Abstract
We evaluated the activities of meropenem, imipenem, temocillin, piperacillin, and ceftazidime by determination of the MICs for 66 genotypically characterized Burkholderia cepacia isolates obtained from the sputum of cystic fibrosis patients. In vitro synergy assays, as performed by the time-kill methodology, of two- and three-drug combinations of the β-lactams with tobramycin, rifampin, and/or ciprofloxacin were also performed with 10 strains susceptible, intermediate, or resistant to fluoroquinolones. On the basis of the MICs, meropenem and temocillin were the most active β-lactam agents, with MICs at which 90% of isolates are inhibited of 8 and 32 μg/ml, respectively. The addition of ciprofloxacin significantly enhanced the killing activities of piperacillin, imipenem, and meropenem against the 10 strains tested (P < 0.05). The best killing activity was obtained with the combination of meropenem and ciprofloxacin, with bactericidal activity of 3.31 ± 0.36 log10 CFU/ml (P < 0.05). Compared to the activity of the two-drug β-lactam–ciprofloxacin combination, the addition of rifampin or tobramycin did not significantly increase the killing activity (P > 0.05). The three-drug combinations (with or without ciprofloxacin) significantly enhanced the killing activities of piperacillin, imipenem, and meropenem relative to the activities of the β-lactams used alone (P < 0.05). The combination β-lactam–ciprofloxacin–tobramycin was the combination with the most consistently synergistic effect.
Burkholderia cepacia, a phytopathogen first described in the 1950s (16), can cause opportunistic and nosocomial infections. When recovered from the sputum of cystic fibrosis (CF) patients, it is associated with a poor clinical prognosis, because fatal pulmonary infections occur in approximately 20% of colonized patients (16, 39). Isolates associated with acute clinical decline belong to genomovar III (42). B. cepacia is resistant to many of the traditional antipseudomonal antibiotics, and concomitant use of two or more drugs is often necessary to eradicate B. cepacia from CF patients.
Meropenem is a novel carbapenem antibiotic with good activity against B. cepacia (26, 33). In our study, we compared its efficacy against strains isolated from the sputum of CF patients with those of the antipseudomonal β-lactam agents temocillin, piperacillin, ceftazidime, and imipenem. The MICs and in vitro synergy, as determined by the time-kill methodology, of two- and three-drug combinations of the β-lactams with tobramycin, rifampin, and/or ciprofloxacin against genotypically characterized B. cepacia isolates were determined.
MATERIALS AND METHODS
Bacterial strains.
Ninety-five previously described (36) clinical B. cepacia isolates were studied. They were recovered from the sputum of 71 CF patients attending 13 French care centers located in nine regions from April 1988 to April 1995. The identities of the isolates were confirmed by standard biochemical procedures (API 20 NE; BioMérieux, Marcy l’Etoile, France).
Genotypic analysis.
Genotypic characterization was based on the analysis of ribosomal DNA regions (ribotyping) with EcoRI as described previously (4, 5).
Antimicrobial agents.
Susceptibility to the following antibiotics was tested: piperacillin, ceftazidime, imipenem, meropenem, temocillin, sulbactam, ciprofloxacin, rifampin, trimethoprim-sulfamethoxazole (TMP-SMZ), minocycline, and tobramycin.
Susceptibility testing. (i) Antibiotic susceptibility pattern.
Antibiotic susceptibility patterns were determined by the disk diffusion method according to the National Committee for Clinical Laboratory Standards (NCCLS) criteria (29, 31). Mueller-Hinton plates (Pasteur Diagnostic, Marnes la Coquette, France) were inoculated with a 0.5 McFarland standard suspension of organisms, and disks (Pasteur Diagnostic) were applied. Zones of growth inhibition were recorded in millimeters after overnight incubation at 35°C.
(ii) MIC determinations.
The antibiotics were obtained from the manufacturers as powders suitable for susceptibility testing. MICs were determined by the dilution method on Mueller-Hinton agar plates as recommended by NCCLS (30). The replicator prong delivered approximately 104 CFU per spot. The MIC50 and MIC90 were defined as the concentrations at which 50 and 90% of the strains were inhibited, respectively. NCCLS breakpoints for nonmembers of the family Enterobacteriaceae were used to define susceptibility to all drugs except temocillin and rifampin, for which there are no NCCLS recommendations (31). For temocillin and rifampin we used the breakpoints recommended by Fuchs et al. (14) and the Comité de l’Antibiogramme de la Société Française de Microbiologie (12), respectively. To avoid duplication, the MIC determination was not repeated when a strain with an identical ribotype and antibiotic susceptibility pattern was isolated twice in the same care center.
Synergy and killing activities.
The synergy and killing activities of the drugs against 10 strains were determined. The 10 strains were genotypically unrelated on the basis of their ribotypes and antibiotic susceptibility patterns. Microtiter plates (Consortium de Matériel pour Laboratoires, Nemours, France) were used to perform the synergy assays and to determine the killing activities for these 10 strains, as described previously (13, 43, 44). A 24-h incubation period with an exponential-phase culture adjusted to approximately 105 CFU/ml in Mueller-Hinton broth with calcium and magnesium concentrations adjusted to 20 and 10 μg/ml, respectively, was used. Each β-lactam agent was tested alone and in two- and three-drug combinations with ciprofloxacin, tobramycin, or rifampin. The antibiotics were assessed for their synergistic effects and killing activities at 0.5 and 1× the MIC, respectively; these concentrations are close to the usual concentrations found in sputum (15, 19, 20, 25, 41). However, because the MICs of imipenem, rifampin, tobramycin, and ciprofloxacin (to which the strains are resistant) for B. cepacia are far higher than the achievable concentrations in sputum, we used imipenem, rifampin, and ciprofloxacin concentrations of 2 μg/ml and a tobramycin concentration of 1 μg/ml to approach the levels achieved in sputum (19, 23, 37, 38). Viability counts were made at 24 h by plating 50 μl from each well onto chocolate agar plates with a Spiral plater (Spiral Systems Inc., Cincinnati, Ohio). The numbers of viable bacteria were counted by the Spiral Systems quadrant counting method after 24 h of incubation at 37°C in room air. The detection limit was 20 CFU/ml. Given the drug concentrations used, significant antibiotic carryover could be ruled out (45).
Preliminary experiments indicated that resistant mutants were selected in the presence of the β-lactam antibiotics and ciprofloxacin at a frequency of about 10−6 at a concentration of 1× the MIC, and regrowth in the assay wells prevented the detection of antibiotic activity. Thus, an inoculum of 105 CFU/ml was used to assess the killing activity synergies of the various combinations of antibiotics. Moreover, to confirm that bacterial growth after 24 h of incubation was not due to the selection of resistant mutants, the susceptibilities of viable bacteria were compared with those of the initial strains (which were redetermined at the same time) by the disk diffusion method according to NCCLS criteria (29). When a significant reduction in the diameter of the inhibition zone (≥4 mm) was observed, survivors were considered to be resistant mutants and the killing activity results were not recorded. Indeed, preliminary experiments showed that the mean standard deviation of the inhibition zone diameter was 4 mm for a given strain when the disk diffusion test was repeated 10 times.
A synergistic effect was defined as a 100-fold (2 log10) fall in the numbers of CFU per milliliter induced by the drug combination relative to the value obtained with the single most effective antibiotic in the combination. Bactericidal activity was defined as a reduction of at least 3 log10 CFU/ml after 24 h. Student’s paired t test was used to test for statistical significance, and P values of less than 0.05 were considered significant.
RESULTS
Ribotyping generated 32 different patterns for the 95 clinical isolates; 29 isolates were considered duplicates and the MICs for those isolates were not determined.
The MICs of the antibiotics tested and the percentage of susceptible strains among the remaining 66 isolates are reported in Table 1. Among the β-lactam agents, temocillin and meropenem had the best inhibitory activities, with 82 and 67% of strains being susceptible to the two drugs, respectively (MIC90, 32 and 8 μg/ml, respectively). Among the non β-lactam agents, TMP-SMZ and minocycline had the best antimicrobial activities, with 62 and 47% of strains being susceptible, respectively (MIC90s, 8/152 and 64 μg/ml, respectively).
TABLE 1.
Susceptibilities of 66 B. cepacia strains to 11 antibiotics determined by the agar dilution method
| Antibiotic | MIC (μg/ml)
|
% Strainsa
|
||||
|---|---|---|---|---|---|---|
| 50% | 90% | Range | S | I | R | |
| Piperacillin | 32 | >128 | 2–>128 | 38 | 24 | 38 |
| Ceftazidime | 8 | 32 | 1–>64 | 42 | 46 | 12 |
| Imipenem | 16 | 64 | 4–>64 | 1 | 10 | 89 |
| Meropenem | 4 | 8 | 1–16 | 67 | 27 | 6 |
| Temocillin | 8 | 32 | 2–64 | 82 | — | 18 |
| Sulbactam | >64 | >64 | 4–>64 | ND | ND | ND |
| Ciprofloxacin | 16 | 64 | 1–>64 | 6 | 9 | 85 |
| Rifampin | 64 | >64 | 32–>64 | 0 | 0 | 100 |
| TMP-SMZ | 2/38 | 8/152 | 0.25/4–>8/152 | 62 | — | 38 |
| Minocycline | 8 | 64 | 0.5–64 | 47 | 17 | 36 |
| Tobramycin | >64 | >64 | >64 | 0 | 0 | 100 |
S, I, and R, susceptible, intermediate, and resistant, respectively. The respective breakpoints for susceptible, intermediate, and resistant were as follows: piperacillin, ≤16, 32 to 64, and ≥128 μg/ml; ceftazidime, ≤8, 16, and ≥32 μg/ml; imipenem and meropenem, ≤4, 8, and ≥16 μg/ml; temocillin, ≤16 and ≥32 μg/ml; ciprofloxacin ≤1, 2, and ≥4 μg/ml; rifampin ≤4, 8, and >16 μg/ml; TMP-SMZ ≤2/38 and ≥4/76 μg/ml; minocycline ≤4, 8, and ≥16 μg/ml; and tobramycin ≤4, 8, and ≥16 μg/ml. ND, not determined. For temocillin and TMP-SMZ there is no intermediate category.
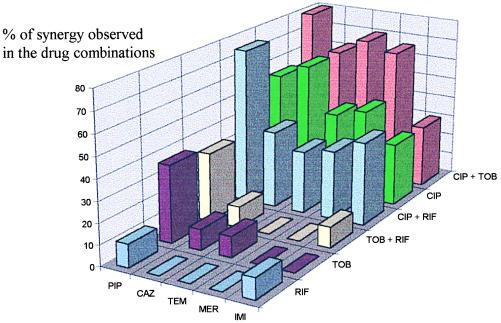
The synergistic effects and killing activities of the antibiotics alone and in combination were determined with 10 strains distinguished by their ribotypes and antibiotic susceptibility patterns. The 10 strains used were all susceptible to the β-lactam agents tested (except for imipenem). Preliminary experiments showed that the use of resistant strains resulted in their growth in the assay well and prevented the detection of antibiotic activity at clinically achievable concentrations in sputum. The ranges of MICs for the 10 strains were as follows: piperacillin, 2 to 16 μg/ml; ceftazidime, 1 to 4 μg/ml; imipenem, 8 to 32 μg/ml; meropenem, 1 to 4 μg/ml; and temocillin, 2 to 8 μg/ml. Seven strains were susceptible or intermediate to ciprofloxacin, with MICs ranging from 1 to 2 μg/ml. Synergistic effects and killing activities, determined at 0.5 and 1× the MIC, respectively, are reported in Fig. 1 and Table 2, respectively.
FIG. 1.
Proportion of strains against which a synergistic effect was observed with double or triple antibiotic combinations. PIP, piperacillin; CAZ, ceftazidime; TEM, temocillin; MER, meropenem; IMI, imipenem; RIF, rifampin; TOB, tobramycin; CIP, ciprofloxacin.
TABLE 2.
Killing activities of temocillin, piperacillin, ceftazidime, imipenem, and meropenem alone or in combination with ciprofloxacin and/or tobramycin or rifampin after 24 h of incubationa
| Antibiotic(s) | Mean ± SD change in log10 CFU/ml after 24 h of incubation
|
|||||
|---|---|---|---|---|---|---|
| Alone | Temocillin | Piperacillin | Ceftazidime | Imipenem | Meropenem | |
| Alone | −0.96 ± 1.89 | −0.23 ± 2.12 | −1.14 ± 2.10 | 2.8 ± 1.49 | 0.41 ± 2.58 | |
| With ciprofloxacin | ||||||
| Asb | 1.44 ± 1.94 | −2.05 ± 1.6c | −2.7 ± 0.77d | −2.42 ± 1.24c | −0.24 ± 3.14d | −3.31 ± 0.36de |
| Ciprf | 3.8 ± 0.8 | −1.0 ± 2.4 | −1.9 ± 1.55 | −1.9 ± 2.55 | 2.4 ± 1.94 | −2.7 ± 0.0 |
| With tobramycin | NDg | −1.32 ± 2.26c | −1.37 ± 1.70c | −1.22 ± 2.07c | 2.14 ± 2.18c | −0.62 ± 2.55c |
| With rifampin | ND | 0.56 ± 1.89c | −1.20 ± 1.65c | −0.65 ± 1.84c | 0.84 ± 3.44c | 0.03 ± 3.19c |
| With ciprofloxacin and tobramycin | ||||||
| As | 1.4 ± 2.0 | −2.6 ± 1.72ch | −2.92 ± 0.33dh | −3.1 ± 0.74dh | −0.85 ± 2.49dh | −3.15 ± 0.59dh |
| Cipr | 3.88 ± 0.83 | −0.4 ± 3.2 | −2.7 ± 0.42 | −2.83 ± 1.25 | 1.3 ± 2.2 | −2.61 ± 0.55 |
| With ciprofloxacin and rifampin | ||||||
| As | 1.24 ± 2.1 | −2.4 ± 1.94ci | −2.98 ± 0.14di | −2.61 ± 1.0di | −1.47 ± 2.28di | −3.04 ± 0.89di |
| Cipr | 3.88 ± 0.83 | −0.05 ± 3.74 | −3.05 ± 0.1 | −1.97 ± 1.8 | 0.3 ± 3.0 | −2.85 ± 0.21 |
| With rifampin and tobramycin | ND | −1 ± 1.98c | −2.1 ± 1.13d | −2.3 ± 1.73c | 0.01 ± 3.2d | −2.4 ± 2.28d |
| Growth control | 4.5 ± 0.4 | 4.34 ± 0.4 | 4.55 ± 0.4 | 4.44 ± 0.35 | 4.3 ± 0.6 | |
Unless indicated otherwise, all antibiotics were tested at 1× the MIC. Imipenem, rifampin, and ciprofloxacin (for ciprofloxacin-resistant strains) and tobramycin were tested at the usual concentrations achieved in sputum (2 and 1 μg/ml, respectively).
As, all strains.
P > 0.05 compared with the β-lactam tested alone.
P < 0.05 compared with the β-lactam tested alone.
P < 0.05 (meropenem-ciprofloxacin compared with other β-lactam agent–ciprofloxacin).
Ciprofloxacin-resistant strains (n = 3).
ND, not determined.
P > 0.05 (β-lactam–ciprofloxacin–tobramycin compared with β-lactam–ciprofloxacin).
P > 0.05 (β-lactam–ciprofloxacin–rifampin compared with β-lactam–ciprofloxacin).
The effects of two-drug combinations comprising a β-lactam agent (at 0.5× the MIC) and ciprofloxacin, rifampin, or tobramycin were synergistic against 30 to 62%, 0 to 10%, and 0 to 37% of the strains, respectively (Fig. 1). The two-drug combination observed to have the most synergistic effect was ceftazidime-ciprofloxacin. At 1× the MIC (Table 2), the maximal fall in bacterial counts was 1.14 log10 CFU/ml with the β-lactams tested alone. The addition of ciprofloxacin significantly enhanced the mean killing activities of piperacillin, imipenem, and meropenem against the 10 tested strains (P < 0.05). The best killing activity at 1× the MIC was obtained with the combination of meropenem and ciprofloxacin, with bactericidal activity of 3.31 ± 0.36 log10 CFU/ml (P < 0.05). However, the addition of ciprofloxacin to the β-lactams did not enhance their killing activities against the three fluoroquinolone-resistant strains (MICs, 32 to 64 μg/ml) except in the cases of meropenem and piperacillin, which caused decreases of 2.7 ± 0 and 1.9 ± 1.55 log10 CFU/ml, respectively. The addition of tobramycin or rifampin did not enhance the killing activities against any of the strains compared to those of the β-lactams alone (P > 0.05).
The three-drug β-lactam–tobramycin–rifampin combinations showed synergistic effects against 0 to 33% of the strains. A greater synergistic effect (30 to 80% of strains) was obtained with the β-lactam–ciprofloxacin–rifampin or β-lactam–ciprofloxacin–tobramycin combinations (Fig. 1). The combination of β-lactams (except imipenem) with ciprofloxacin and tobramycin was the one with the most consistently synergistic effects (against more than 60% of the strains). The addition of tobramycin to the combination of meropenem or temocillin plus rifampin did not result in a greater synergistic effect (Fig. 1).
Compared to the two-drug β-lactam–ciprofloxacin combination, the addition of rifampin or tobramycin did not significantly increase the mean killing activity (P > 0.05) when 1× the MIC was used (Table 2). The three-drug combinations at 1× the MIC (with or without ciprofloxacin) significantly enhanced the killing activities of piperacillin, imipenem, and meropenem relative to those of the β-lactams used alone (P < 0.05). The killing activity of ceftazidime combined with ciprofloxacin and rifampin or tobramycin was significantly superior to that of ceftazidime alone (P < 0.05). In contrast, the killing activity of temocillin in any of the two- or three-drug combinations was not significantly enhanced (P > 0.05).
DISCUSSION
The multiple-antibiotic resistance of B. cepacia has been attributed to an impermeable selective outer membrane (1, 28, 32), an efflux pump mechanism (7), and/or the production of an inducible chromosomal β-lactamase (3, 34). Given the reported spread of epidemic strains (17, 33, 36), we determined the MICs for all the strains that were isolated from patients within the same care center and that had different ribotypes and/or antibiotic susceptibility patterns. The MICs observed in our study are consistent with those reported elsewhere for all the drugs tested except sulbactam (10, 21, 26, 27, 33, 44). Contrary to Jacoby and Sutton (21), we found that sulbactam was poorly active, with MIC50s above 64 μg/ml, possibly because we tested isolates from CF patients. On the basis of the MICs, temocillin and meropenem were the most active β-lactam agents, with no cross-resistance with imipenem, in agreement with Lewin et al. (26) and Pitt et al. (33). Meropenem also had the narrowest MIC range. This may be explained by its recent introduction in France. However, the long-term impact of meropenem use on resistance rates among B. cepacia is unknown. The other antibacterial agents used to treat CF patients, such as piperacillin, ceftazidime, imipenem, and ciprofloxacin, had wider MIC ranges, probably because of the emergence of resistant mutants in vivo. This has been documented with Pseudomonas aeruginosa (15, 18) but may also occur with B. cepacia, because the migration of insertion sequences within the chromosome can affect the expression of genes that modulate antibiotic resistance (35).
Previous studies have shown the value of antibiotic combinations such as β-lactam–ciprofloxacin, β-lactam–ciprofloxacin–rifampin, and β-lactam–aminoglycoside against B. cepacia (2, 6, 10, 24, 27) and β-lactam–aminoglycoside–rifampin against P. aeruginosa (46, 47). We therefore tested the activities of two- and three-drug combinations of these antibiotics against our strains. Among the aminoglycosides, we chose tobramycin, the MICs of which are lower than those of gentamicin and amikacin (27, 33). The antibiotics were tested at 0.5 and 1× the MICs to improve the detection of synergy (13) and to reflect clinical conditions. Except for imipenem, rifampin, tobramycin, and ciprofloxacin (to which strains were resistant), the achievable concentrations in sputum were close to the relevant MICs (15, 19, 20, 23, 25, 37, 38, 41).
The potential of the use of β-lactam–ciprofloxacin combinations against B. cepacia has been investigated previously (6, 24, 27). Most of the latter studies were based on fractional inhibitory concentration indexes and gave variable results. In this study, which was based on the time-kill method, the addition of ciprofloxacin significantly increased the killing activities of piperacillin and meropenem and, to a lesser extent, that of imipenem against all strains susceptible or intermediate to fluoroquinolones. The synergistic effect of such combinations was superior to that of β-lactam combinations with aminoglycosides or rifampin. The results are consistent with those of Kumar et al. (24) but are in disagreement with those of Lu et al. (27); those investigators tested imipenem plus rifampin or ciprofloxacin and ceftazidime plus ciprofloxacin or amikacin, respectively. The discrepancies may be explained by the origins of the strains (isolates from CF patients in the study of Kumar et al. [24] and invasive strains in the work of Lu et al. [27]) and by the methodology used to detect synergistic effects. Indeed, no correlation between the results obtained by the killing curve method used by Kumar et al. (24) and the results obtained by the checkerboard method used by Lu et al. (27) has been reported (9). However, synergy is best detected by the time-kill methodology, which is more able to predict the outcome of antibiotic treatment (22).
A bactericidal effect was achieved by adding meropenem to ciprofloxacin. However, with the three ciprofloxacin-resistant strains tested, the decrease was less than 3 log10 CFU/ml.
Clinical trial data on the eradication of B. cepacia from CF patients are highly limited (8, 11, 15, 18, 40). Published results from trials involving small numbers of patients suggest a potential value of temocillin and the disappointing activity of ceftazidime (15, 40). The two- and three-drug combinations proposed in our study and the use of meropenem may be of interest in this setting. Clinical trials are required to corroborate our in vitro data.
ACKNOWLEDGMENTS
We are indebted to O. Bajolet-Laudinat, Reims, France; G. Berthelot, Dieppe, France; J. Carrère, Giens, France; G. Chabanon, Toulouse, France; C. de Champs, Clermont-Ferrand, France; P. Honderlick, Suresnes, France; G. Paul, Paris, France; D. Tande, Brest, France; J. Texier-Maugein, Pessac, France; J. Thubert, Roscoff, France; H. Vu Thien, Paris; and M. Weber, Nancy, France, for providing strains and to A. Munck and J. Navarro, Paris, for helpful discussion.
This work was supported by a grant from the Association Française de Lutte contre la Mucoviscidose, 1995.
REFERENCES
- 1.Aronoff S C. Outer membrane permeability in Pseudomonas cepacia diminished porin content in a β-lactam-resistant mutant and in resistant cystic fibrosis isolates. Antimicrob Agents Chemother. 1988;32:1636–1639. doi: 10.1128/aac.32.11.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aronoff S C, Klinger J. In vitro activities of aztreonam, piperacillin, and ticarcillin with amikacin against amikacin-resistant Pseudomonas aeruginosa and Pseudomonas cepacia isolates from children with cystic fibrosis. Antimicrob Agents Chemother. 1984;25:279–280. doi: 10.1128/aac.25.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beckman W, Lessie T G. Abstracts of the 80th Annual Meeting of the American Society for Microbiology 1980. Washington, D.C: American Society for Microbiology; 1980. Multiple forms of Pseudomonas cepacia β-lactamase, abstr. K-128; p. 148. [Google Scholar]
- 4.Bingen E H, Denamur E, Elion J. use of ribotyping in epidemiological surveillance of nosocomial outbreaks. Clin Microbiol Rev. 1994;7:311–327. doi: 10.1128/cmr.7.3.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bingen E H, Weber M, Derelle J, Brahimi N, Lambert-Zechovsky N Y, Vidailhet M, Navarro J, Elion J. Arbitrarily primed polymerase chain reaction as a rapid method to differentiate crossed from independent Pseudomonas cepacia infections in cystic fibrosis patients. J Clin Microbiol. 1993;31:2589–2593. doi: 10.1128/jcm.31.10.2589-2593.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosso J A, Saxon B A, Matsen J M. In vitro activities of combinations of aztreonam, ciprofloxacin, and ceftazidime against clinical isolates of Pseudomonas aeruginosa and Pseudomonas cepacia from cystic fibrosis patients. Antimicrob Agents Chemother. 1990;34:487–488. doi: 10.1128/aac.34.3.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burns J L, Wadsworth C D, Barry J J, Goodall C P. Nucleotide sequence analysis of a gene from Burkholderia (Pseudomonas) cepacia encoding an outer membrane lipoprotein involved in multiple antibiotic resistance. Antimicrob Agents Chemother. 1996;40:307–313. doi: 10.1128/aac.40.2.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Byrne, S., J. Maddison, P. Connor, I. Doughty, M. Jenney, A. K. Webb, and T. J. David. 1995. Clinical evaluation of meropenem versus ceftazidime for the treatment of Pseudomonas spp. infections in cystic fibrosis patients. J. Antimicrob. Chemother. 36(Suppl. A):135–143. [DOI] [PubMed]
- 9.Cappellety D M, Rybak M J. Comparison of methodologies for synergism testing of drug combinations against resistant strains of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1996;40:677–683. doi: 10.1128/aac.40.3.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chin N X, Neu H C. Synergy of new C-3 substituted cephalosporins and tobramycin against Pseudomonas aeruginosa and Pseudomonas cepacia. Diagn Microbiol Infect Dis. 1989;12:343–349. doi: 10.1016/0732-8893(89)90101-6. [DOI] [PubMed] [Google Scholar]
- 11.Ciofu O, Jensen T, Pressler T, Johansen H K, Koch C, Hoiby N. Meropenem in cystic fibrosis patients infected with resistant Pseudomonas aeruginosa or Burkholderia cepacia and with hypersensitivity to β-lactams antibiotics. Clin Microbiol Infect. 1996;2:91–98. doi: 10.1111/j.1469-0691.1996.tb00212.x. [DOI] [PubMed] [Google Scholar]
- 12.Comité de l’Antibiogramme de la Société Française de Microbiologie. Communiqué 1997. Pathol Biol. 1997;45:1–12. [Google Scholar]
- 13.Eliopoulos G M, Moellering R C., Jr . Antimicrobial combinations. In: Lorian V, editor. Antibiotics in laboratory medicine. 4th ed. Baltimore, Md: The Williams & Wilkins Co.; 1996. pp. 330–396. [Google Scholar]
- 14.Fuchs P C, Barry A L, Thornsberry C, Jones R N. Interpretive criteria for temocillin disk diffusion susceptibility testing. Eur J Clin Microbiol. 1985;4:30–33. doi: 10.1007/BF02148656. [DOI] [PubMed] [Google Scholar]
- 15.Gold, R., E. Jin, H. Levinson, A. Isles, and P. C. Fleming. 1983. Ceftazidime alone and in combination in patients with cystic fibrosis: lack of efficacy in treatment of severe respiratory infections caused by Pseudomonas cepacia. J. Antimicrob. Chemother. 12(Suppl. A):331–336. [DOI] [PubMed]
- 16.Govan J R W, Hugues J E, Vandamme P. Burkholderia cepacia: medical, taxonomic and ecological issues. J Med Microbiol. 1996;45:395–407. doi: 10.1099/00222615-45-6-395. [DOI] [PubMed] [Google Scholar]
- 17.Govan J R W, Brown P H, Maddison J, Doherty C J, Nelson J W, Dodd M, Greening A P, Webb A K. Evidence for transmission of Pseudomonas cepacia by social contact in cystic fibrosis. Lancet. 1993;342:15–19. doi: 10.1016/0140-6736(93)91881-l. [DOI] [PubMed] [Google Scholar]
- 18.Hoiby N, Ciofu O, Jensen T, Pressler T, Johansen H K, Koch C. Use of carbapenems and other antibiotics for pulmonary infections in patients with cystic fibrosis. Pediatr Infect Dis J. 1996;15:738–743. doi: 10.1097/00006454-199608000-00035. [DOI] [PubMed] [Google Scholar]
- 19.Hoogkamp-Korstanje J A A, van der Laag J. Piperacillin and tobramycin in the treatment of Pseudomonas lung infections in cystic fibrosis. J Antimicrob Chemother. 1983;12:175–183. doi: 10.1093/jac/12.2.175. [DOI] [PubMed] [Google Scholar]
- 20.Hutchinson, M., K. L. Faulkner, P. J. Turner, S. J. Haworth, W. Sheik, H. Nadler, and D. H. Pitkin. 1995. A compilation of meropenem tissue distribution data. J. Antimicrob. Chemother. 36(Suppl. A):43–56. [DOI] [PubMed]
- 21.Jacoby G A, Sutton L. Pseudomonas cepacia susceptibility to sulbactam. Antimicrob Agents Chemother. 1989;33:583–584. doi: 10.1128/aac.33.4.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson C C. In vitro testing: correlations between bacterial susceptibility, body fluids levels, and effectiveness of antibacterial therapy. In: Lorian V, editor. Antibiotics in laboratory medicine. 4th ed. Baltimore, Md: The Williams & Wilkins Co.; 1996. pp. 813–834. [Google Scholar]
- 23.Kucers A, Bennett N M. Rifampicin. In: Bennett N M, editor. The use of antibiotics. 4th ed. Oxford, United Kingdom: Heinemann Medical Books; 1987. pp. 914–970. [Google Scholar]
- 24.Kumar A, Wofford-McQueen R, Gordon R C. Ciprofloxacin, imipenem and rifampicin: in-vitro synergy of two and three drug combinations against Pseudomonas cepacia. J Antimicrob Chemother. 1989;23:831–835. doi: 10.1093/jac/23.6.831. [DOI] [PubMed] [Google Scholar]
- 25.Legge, J. S., T. M. Reid, and J. B. Palmer. 1985. Clinical efficacy, tolerance and pharmacokinetics of temocillin in patients with respiratory tract infections. Drugs 29(Suppl. 5):118–121. [DOI] [PubMed]
- 26.Lewin C, Doherty C, Govan J. In vitro activities of meropenem, PD 127391, PD 131628, ceftazidime, chloramphenicol, co-trimoxazole, and ciprofloxacin against Pseudomonas cepacia. Antimicrob Agents Chemother. 1993;37:123–125. doi: 10.1128/aac.37.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lu D C T, Chang S C, Chen Y C, Luh K T, Hsieh W C. In vitro activities of antimicrobial agents, alone and in combinations against Burkholderia cepacia isolated from blood. Diagn Microbiol Infect Dis. 1997;28:187–191. doi: 10.1016/s0732-8893(97)00069-2. [DOI] [PubMed] [Google Scholar]
- 28.Moore R A, Hancock R E W. Involvement of outer membrane of Pseudomonas cepacia in aminoglycoside and polymyxin resistance. Antimicrob Agents Chemother. 1986;30:923–926. doi: 10.1128/aac.30.6.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Committee for Clinical Laboratory Standards. Performance for antimicrobial disk susceptibility tests. 5th ed. Approved standard M2-A5. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1993. [Google Scholar]
- 30.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. 4th ed. Approved standard M7 A4. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 31.National Committee for Clinical Laboratory Standards. Performance for antimicrobial susceptibility testing. Eighth informational supplement. M100 S8. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1998. [Google Scholar]
- 32.Parr T R, Jr, Moore R A, Moore L V, Hancock R E W. Role of porins in intrinsic antibiotic resistance of Pseudomonas cepacia. Antimicrob Agents Chemother. 1987;31:121–123. doi: 10.1128/aac.31.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pitt T L, Kaufmann M E, Patel P S, Benge L C A, Gaskin S, Livermore D M. Type characterisation and antibiotic susceptibility of Burkholderia (Pseudomonas) cepacia isolates from patients with cystic fibrosis in the United Kingdom and the Republic of Ireland. J Med Microbiol. 1996;44:203–210. doi: 10.1099/00222615-44-3-203. [DOI] [PubMed] [Google Scholar]
- 34.Prince A, Wood M S, Cacalano G S, Chin N X. Isolation and characterization of a penicillinase from Pseudomonas cepacia 249. Antimicrob Agents Chemother. 1988;32:838–843. doi: 10.1128/aac.32.6.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scordilis G E, Ree H, Lessie T G. Identification of transposable elements which activate gene expression in Pseudomonas cepacia. J Bacteriol. 1987;169:8–13. doi: 10.1128/jb.169.1.8-13.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Segonds C, Bingen E, Couetdic G, Mathy S, Brahimi N, Marty N, Plesiat P, Michel-Briand Y, Chabanon G. Genotypic analysis of Burkholderia cepacia isolates from 13 French cystic fibrosis centers. J Clin Microbiol. 1997;35:2055–2060. doi: 10.1128/jcm.35.8.2055-2060.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith M J, White L O, Bowyer H, Willis J, Hodson M E, Batten J C. Pharmacokinetics and sputum penetration of ciprofloxacin in patients with cystic fibrosis. Antimicrob Agents Chemother. 1986;30:614–616. doi: 10.1128/aac.30.4.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Strandvik B, Malmborg A S, Bergan T, Michalsen H, Storrosten O T, Wretlind B. Imipenem/cilastatin, an alternative treatment of Pseudomonas infection in cystic fibrosis. J Antimicrob Chemother. 1988;21:471–480. doi: 10.1093/jac/21.4.471. [DOI] [PubMed] [Google Scholar]
- 39.Tablan O C, Chorba T L, Schidlow D V, White J W, Hardy K A, Gilligan P H, Morgan W M, Carson L A, Martone W J, Jason J M, Jarvis W R. Pseudomonas cepacia colonization in patients with cystic fibrosis: risks factors and clinical outcome. J Pediatr. 1985;107:382–387. doi: 10.1016/s0022-3476(85)80511-4. [DOI] [PubMed] [Google Scholar]
- 40.Taylor R F H, Gaya H, Hodson M E. Temocillin and cystic fibrosis. outcome of intravenous administration in patients infected with Pseudomonas cepacia. J Antimicrob Chemother. 1992;29:341–344. doi: 10.1093/jac/29.3.341. [DOI] [PubMed] [Google Scholar]
- 41.Turner A, Pedler S J, Carswell F, Spencer G R, Speller D C E. Serum and sputum concentrations of ceftazidime in patients with cystic fibrosis. J Antimicrob Chemother. 1984;14:521–527. doi: 10.1093/jac/14.5.521. [DOI] [PubMed] [Google Scholar]
- 42.Vandamme P, Holmes B, Vancanneyt M, Coenye T, Hoste B, Coopman R, Revets H, Lauwers S, Gillis M, Kersters K, Gowan J R W. Occurrence of multiple genomovars of Burkholderia cepacia in cystic fibrosis patients and proposal of Burkholderia multivorans sp. nov. Int J Syst Bacteriol. 1997;47:1188–1200. doi: 10.1099/00207713-47-4-1188. [DOI] [PubMed] [Google Scholar]
- 43.Visalli M, A, Jacobs M R, Appelbaum P C. Activities of three quinolones alone and in combination with extended-spectrum cephalosporins or gentamicin against Stenotrophomonas maltophilia. Antimicrob Agents Chemother. 1998;42:2002–2005. doi: 10.1128/aac.42.8.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Visalli M, A, Bajaksouzian S, Jacobs M R, Appelbaum P C. Comparative activity of trovafloxacin, alone and in combination with other agents, against gram-negative nonfermentative rods. Antimicrob Agents Chemother. 1997;41:1475–1481. doi: 10.1128/aac.41.7.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yourassovsky E, Van der Linden M P, Crokaert F, Glupczynski Y. Effect of antibiotics carry-over on bacterial counting by “spiral plating.”. J Antimicrob Chemother. 1988;21:138–140. doi: 10.1093/jac/21.1.138. [DOI] [PubMed] [Google Scholar]
- 46.Yu V L, Zuravleff J J, Peacock J E, Dehertogh D, Tashjian L. Addition of rifampin to carboxypenicillin-aminoglycoside combination for the treatment of Pseudomonas aeruginosa infection: clinical experience with four patients. Antimicrob Agents Chemother. 1984;26:575–577. doi: 10.1128/aac.26.4.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zuravleff J J, Yu V L, Yee R B. Ticarcillin-tobramycin-rifampin: in vitro synergy of the triplet combination against Pseudomonas aeruginosa. J Lab Clin Med. 1983;101:896–902. [PubMed] [Google Scholar]