Key Points
Question
In the US from 1988-2018, were tropical cyclones associated with increases in county-level cause-specific death rates in subsequent months?
Findings
In this retrospective observational analysis that included 33.6 million deaths in 1206 counties that experienced tropical cyclones from 1988-2018, each additional cyclone day per month was associated with increases in monthly county-level death rates in the month following a cyclone for several causes of death including injuries (3.7%), infectious and parasitic diseases (1.8%), respiratory diseases (1.3%), cardiovascular diseases (1.2%), and neuropsychiatric conditions (1.2%) but not for cancers.
Meaning
Among US counties that experienced at least 1 tropical cyclone from 1988-2018, each additional cyclone day per month was associated with modestly higher death rates in the months following the cyclone for several causes of death.
Abstract
Importance
Tropical cyclones have a devastating effect on society, but a comprehensive assessment of their association with cause-specific mortality over multiple years of study is lacking.
Objective
To comprehensively evaluate the association of county-level tropical cyclone exposure and death rates from various causes in the US.
Design, Setting, and Participants
A retrospective observational study using a Bayesian conditional quasi-Poisson model to examine how tropical cyclones were associated with monthly death rates. Data from 33.6 million deaths in the US were collected from the National Center for Health Statistics over 31 years (1988-2018), including residents of the 1206 counties in the US that experienced at least 1 tropical cyclone during the study period.
Exposures
Tropical cyclone days per county-month, defined as number of days in a month with a sustained maximal wind speed 34 knots or greater.
Main Outcomes and Measures
Monthly cause-specific county-level death rates by 6 underlying causes of death: cancers, cardiovascular diseases, infectious and parasitic diseases, injuries, neuropsychiatric conditions, and respiratory diseases. The model yielded information about the association between each additional cyclone day per month and monthly county-level mortality compared with the same county-month in different years, up to 6 months after tropical cyclones, and how these estimated associations varied by age, sex, and social vulnerability. The unit of analysis was county-month.
Results
There were 33 619 393 deaths in total (16 691 681 females and 16 927 712 males; 8 587 033 aged 0-64 years and 25 032 360 aged 65 years or older) from the 6 causes recorded in 1206 US counties. There was a median of 2 tropical cyclone days experienced in total in included US counties. Each additional cyclone day was associated with increased death rates in the month following the cyclone for injuries (3.7% [95% credible interval {CrI}, 2.5%-4.9%]; 2.0 [95% CrI, 1.3-2.7] additional deaths per 1 000 000 for 2018 monthly age-standardized median rate [DPM]; 54.3 to 56.3 DPM), infectious and parasitic diseases (1.8% [95% CrI, 0.1%-3.6%]; 0.2 [95% CrI, 0.0-0.4] additional DPM; 11.7 to 11.9 DPM), respiratory diseases (1.3% [95% CrI, 0.2%-2.4%]; 0.6 [95% CrI, 0.1-1.1] additional DPM; 44.9 to 45.5 DPM), cardiovascular diseases (1.2% [95% CrI, 0.6%-1.7%]; 1.5 [95% CrI, 0.8-2.2] additional DPM; 129.6 to 131.1 DPM), neuropsychiatric conditions (1.2% [95% CrI, 0.1%-2.4%]; 0.6 [95% CrI, 0.1-1.2] additional DPM; 52.1 to 52.7 DPM), with no change for cancers (−0.3% [95% CrI, −0.9% to 0.3%]; −0.3 [95% CrI, −0.9 to 0.3] additional DPM; 100.4 to 100.1 DPM).
Conclusions and Relevance
Among US counties that experienced at least 1 tropical cyclone from 1988-2018, each additional cyclone day per month was associated with modestly higher death rates in the months following the cyclone for several causes of death, including injuries, infectious and parasitic diseases, cardiovascular diseases, neuropsychiatric conditions, and respiratory diseases.
This study uses data on tropical cyclones in the US and mortality data from the National Center for Health Statistics to evaluate the association of county-level tropical cyclone exposure and mortality rates from various causes in the US from 1998-2018.
Introduction
In the US and worldwide, hurricanes and other tropical cyclones have had a devastating effect on society.1,2,3,4 Recent tropical cyclone seasons—which have yielded stronger,5 more active,6 and longer-lasting7 tropical cyclones than previously recorded—indicate that tropical cyclones will remain an important public health concern. States in the Atlantic and Gulf Coasts, most frequently exposed to tropical cyclones, have among the fastest-growing populations in the US and contain nearly half the population of the entire country.8 There is an intense concentration of economic and social activity in these states,9 which have also been particularly vulnerable to damage from climate change.10 While immediate coastal locations are often enclaves of wealth, an outsized proportion of low-income and historically disadvantaged communities in the US also reside in tropical cyclone–affected areas.11 Although tropical cyclones have not been selective of the communities they have affected, community characteristics have played an important role in their protection and resilience.12
Tropical cyclones have been associated with a wide range of hospital admissions in the US during 1999-2014.4 However, beyond a few case studies, including after Hurricane Maria in 201713 and after Hurricane Sandy in 2012,14 there remains a critical knowledge gap about cause-specific tropical cyclone–related mortality risks; a large-scale, multiyear study is needed to gain further insight and is an essential step in disaster risk reduction.15 This comprehensive study of tropical cyclones affecting the US over a 31-year period evaluated how tropical cyclones were associated with deaths from major causes up to 6 months after tropical cyclones in the US and how the associations varied by strength of tropical cyclone, age, sex, and social vulnerability.
Methods
This study was approved by the institutional review board at the Columbia University Mailman School of Public Health and was classified as exempt from needing to obtain informed consent (protocol IRB-AAAT9710).
Study Population
Data on deaths by age, sex, cause, and county of residence in US counties that experienced at least 1 tropical cyclone during 1988-2018 through the National Center for Health Statistics were used and are described in the Supplement. A subset of the data from counties that experienced at least 1 hurricane during the study period was used. County-level annual population data from the National Center for Health Statistics bridged-race data set for 1990-2018 and from the US Census Bureau before 1990 were used. Monthly population counts were calculated through linear interpolation of annual counts, assigning each yearly count to June. County-level data on social vulnerability from the Centers for Disease Control and Prevention Social Vulnerability Index (SVI) for 2018 were used, a relative measure of social vulnerability of every US county which incorporates data from the US Census on socioeconomic status; household composition and disability; minority status and language; and housing type and transportation.11 Included counties were divided into SVI tertiles (1 [low vulnerability] to 3 [high vulnerability]) (eAppendix and eFigures 4 and 5 in the Supplement).
Exposure
Data were obtained on tropical cyclones in the US, indicated by windspeed, and categorized by county and month into all tropical cyclones (≥34 knots), as well as subset of the data including only hurricanes (≥64 knots) and are described fully in the Supplement.4,16 Data on county-level monthly mean temperature were obtained from the PRISM (Parameter-elevation Regressions on Independent Slopes Model) climate mapping system.17
Outcomes
The underlying cause of death, defined by the World Health Organization as the primary disease or injury that initiated the train of events leading directly to death,18 was coded according to the International Classification of Diseases system (9th revision before 1998 and 10th revision thereafter) and World Health Organization Global Health Estimate cause categories.19
Underlying causes of death were classified into 7 categories: cancers, cardiovascular diseases, infectious and parasitic diseases, injuries, neuropsychiatric conditions, respiratory diseases, and an aggregate set of other death causes (eTable 1 in the Supplement). The results of all of these categories were reported except other causes of death. The “other causes” category was not included because the diversity of causes it captures led to substantial heterogeneity, and the composition varied greatly by age, sex, county, and time.
Statistical Analysis
The county-level association between number of days in a month with tropical cyclone exposure and monthly death rates was analyzed by applying a Bayesian formulation of the conditional quasi-Poisson model,20 including unconstrained distributed lag terms up to 6 months after tropical cyclones. The quasi-Poisson model accounts for potentially overdispersed outcomes. This conditional approach examines contrasts within matched strata (in this case county-months, as described below), similar to a case-crossover study design, thus controlling for confounding bias that could arise by factors varying across strata, such as socioeconomic status, in a computationally efficient way.20 Bayesian inference allows for the full distributional estimation of the parameters of interest, as well as “borrowing of information” across county units.21 Bidirectional matching was made by county and month of the year, only comparing a tropical cyclone-exposed county-month in a particular year to the same county-month in all other included years, thus effectively controlling for any non–time-varying factors that varied across counties (such as seasonal hours of daylight) in the analyses, as well as seasonality. Although the conditional formulation adjusts for most sources of confounding by matching each county-month to itself, long-term trends (via a natural spline) and temperature (via a second-order random-walk term; equivalent to a spline with equally-spaced knots) were also specifically adjusted for. A county-month–specific population offset was included so that changes in death rates were analyzed. Unconstrained distributed lag terms for the exposure counts were included,22,23 to quantify the association between each additional day of tropical cyclone exposure in a month and death rates up to 6 months after cyclone. Therefore, a tropical cyclone in 1 particular month would be considered a lagged tropical cyclone in another month for the relevant distributed lag term.22,23 Full details on model terms are described in the Supplement.
Analyses were conducted separately by cause of death and class of tropical cyclone (all tropical cyclones, hurricanes), with further analyses stratified by broad age groups (0-64 and ≥65 years) (because older adults have been identified as vulnerable to being hospitalized from tropical cyclones4), finer age groups (0-24 years, 25-44 years, 45-64 years, 65-84 years and ≥85 years), sex (female/male), and county-level social vulnerability tertiles (1 [low vulnerability] to 3 [high vulnerability]), because death rates vary by these characteristics,24,25,26 as might their associations with tropical cyclones.
The sensitivity of the results to temperature adjustment (ie, including vs not including temperature in the model) and limiting the matched control period of tropical cyclone exposure to years in the same 5-year period, in addition to the month and county matching, were assessed.
Results are presented as relative (percentage) changes per 1-day increase in tropical cyclones in a month and as deaths per 1 000 000 for 2018 monthly age-standardized median rate (DPM) by multiplying the relative changes by the median (50th percentile) death rates for 2018 from eTables 2 and 3 in the Supplement. Any reported positive association was based on a positive point estimate with a 2-sided 95% credible interval (CrI) that excluded the null, with a negative association the same but with a negative point estimate. Any comparative analyses of effect estimates were obtained by a formal comparative analysis of 1000 draws from the posterior marginal distribution of each effect estimate; the proportion of draws that was higher than the other set of draws represented the probability that one effect estimate was higher than the one compared with.21
Statistical analyses were conducted using R version 3.6.3 (R Foundation for Statistical Computing), integrated nested Laplace approximation in R-INLA, version 21.03.17, and the ns function from the splines package, version 3.6.3. Study findings should be interpreted as exploratory because of numerous outcomes and issues related to multiple comparisons. There were no missing data.
Results
Tropical Cyclones
A total of 1206 counties, covering 48.1% of the 2018 population of the US, experienced at least 1 tropical cyclone during the 31-year study period (Figure 1; eFigure 1 in the Supplement), with a total of 4978 tropical cyclone county-days in 4842 county-months (Table). For included counties, the total number of tropical cyclone days across all years ranged from 1 to 26, with a median of 2 (mean, 4.1). Tropical cyclones occurred May-November, with greatest occurrence in September (n = 2188). Tropical cyclones were most frequent in the eastern and southeastern coastal counties. There were 233 hurricane county-days in 228 county-months across 153 counties, including 9.0% of the 2018 population of the US. The total number of hurricane days across all years ranged from 1 to 5, with a median of 1 (mean, 1.5). Hurricanes occurred July-October, with greatest occurrence in September (n = 99).
Figure 1. Counts of Tropical Cyclone Exposure by US County, 1988-2018.
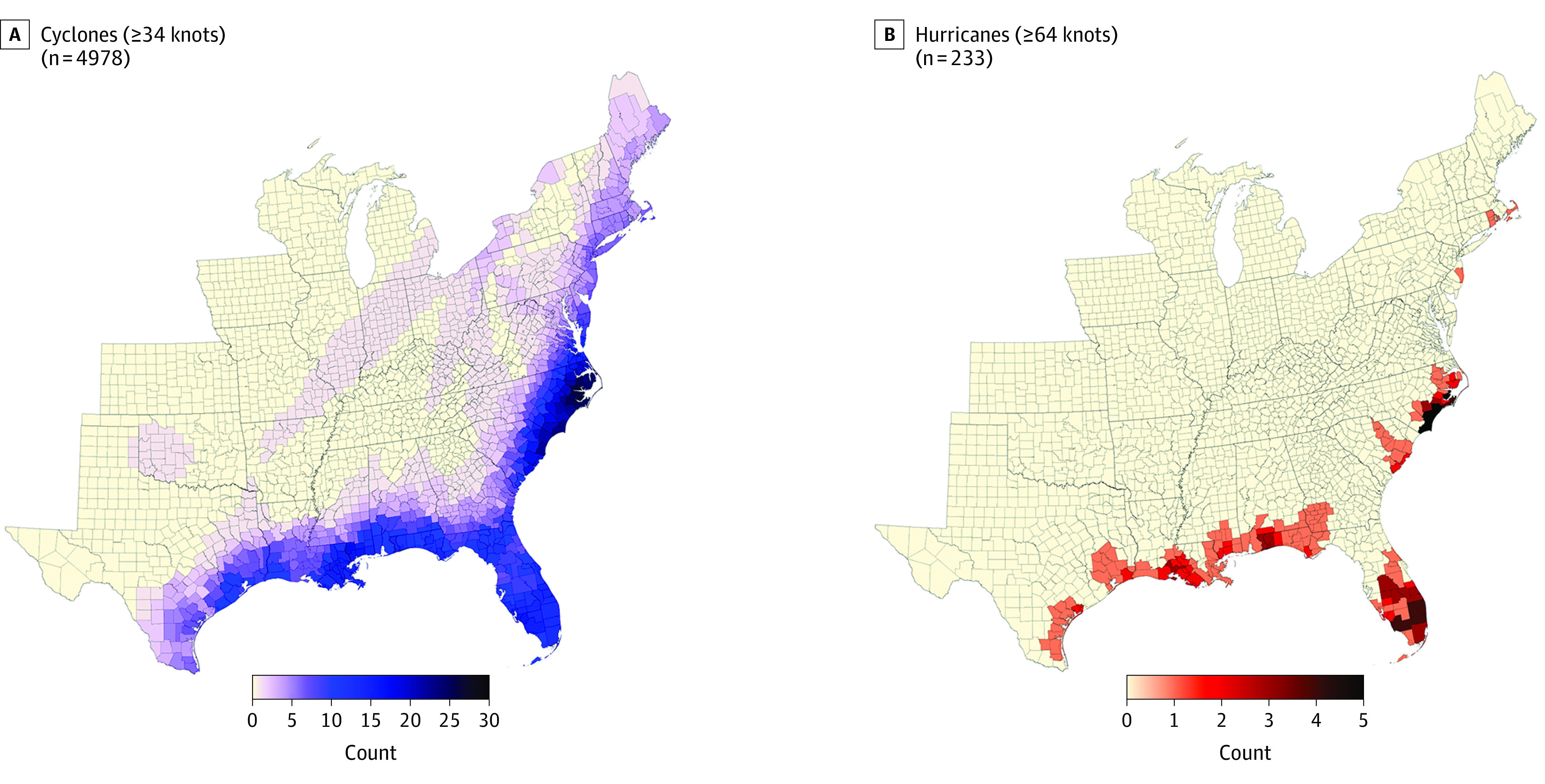
Table. Tropical Cyclones From 1988-2018 and Their Maximal Intensities Recorded in the US (in knots), With Number of Tropical Cyclone Exposures in the US and Total Deaths in Included Counties per Year.
| Year | Tropical cyclones (maximal intensity in US, knots) | Tropical cyclone exposures | Total deaths in analysis from included counties |
|---|---|---|---|
| 1988 | Beryl (44.8), Chris (34.1), Florence (51.4), Keith (47.8), AL13 (11.3),a AL14 (27.8),a AL17 (12.6),a Alberto (22.8),a Gilbert (33.0)a | 53 | 1 009 179 |
| 1989 | Allison (45.0), Chantal (59.0), Hugo (94.1),b Jerry (60.2) | 244 | 994 218 |
| 1990 | Marco (46.7), AL01 (16.7),a Bertha (11.0)a | 12 | 993 622 |
| 1991 | Bob (75.6),b AL12 (30.9) a Ana (20.0),a Fabian (22.8)a | 100 | 1 002 601 |
| 1992 | Andrew (110.0),b Danielle (46.8), AL02 (25.0),a Earl (19.2)a | 101 | 1 007 167 |
| 1993 | Emily (57.9), AL01 (9.8),a Arlene (31.4)a | 35 | 1 044 692 |
| 1994 | Alberto (44.4), Beryl (49.4), Gordon (50.5), AL02 (27.0)a | 55 | 1 049 668 |
| 1995 | Allison (49.8), Dean (34.4), Erin (72.4), Jerry (35.0), Opal (82.9),b Gabrielle (21.9)a | 282 | 1 063 748 |
| 1996 | Bertha (81.8), Edouard (34.4), Fran (88.3), Josephine (49.5), Arthur (25.5)a | 383 | 1 061 303 |
| 1997 | Danny (58.4), AL01 (19.0),a Ana (12.3)a | 57 | 1 054 165 |
| 1998 | Bonnie (93.1), Charley (36.5), Earl (64.8), Frances (43.6), Georges (83.3),b Mitch (51.5),b Hermine (30.6)a | 300 | 1 058 349 |
| 1999 | Bret (91.7), Dennis (54.5), Floyd (75.8),b Harvey (44.7), Irene (65.0), AL07 (16.0)a | 247 | 1 079 454 |
| 2000 | Gordon (46.8), Helene (39.9), AL04 (17.8),a AL09 (24.4),a Beryl (25.5),a Leslie (29.9)a | 35 | 1 083 674 |
| 2001 | Allison (41.3),b Barry (51.8), Gabrielle (54.9), Karen (14.6),a Michelle (24.6)a,b | 71 | 1 083 045 |
| 2002 | Fay (45.2), Gustav (36.9), Hanna (42.4), Isidore (50.5),b Kyle (34.0), Lili (69.9),b Arthur (20.3),a Bertha (31.0),a Cristobal (13.4),a Edouard (31.3)a | 96 | 1 089 933 |
| 2003 | Bill (45.3), Claudette (66.2), Erika (47.9), Grace (34.7), Isabel (81.7),b AL07 (21.8),a Henri (28.7)a | 227 | 1 087 587 |
| 2004 | Alex (51.7), Charley (107.3),b Frances (87.4),b Gaston (59.3), Ivan (85.4),b Jeanne (98.1),b Bonnie (28.9),a Hermine (32.3),a Matthew (26.2)a | 303 | 1 067 225 |
| 2005 | Arlene (43.5), Cindy (54.3), Dennis (87.0),b Emily (45.3), Katrina (97.0),b Ophelia (54.6), Rita (82.0),b Tammy (39.3), Wilma (79.5),b Twenty-Two (27.0)a | 268 | 1 082 681 |
| 2006 | Alberto (37.2), Beryl (34.3), Ernesto (47.0), Chris (9.3)a | 114 | 1 069 021 |
| 2007 | Barry (37.7), Erin (47.7), Gabrielle (42.4), Humberto (67.6), Andrea (21.9),a Noel (31.0),a,b Ten (23.2)a | 89 | 1 065 336 |
| 2008 | Dolly (64.3), Edouard (50.6), Fay (58.7), Gustav (87.1),b Hanna (55.2), Ike (88.8),b Kyle (35.3), Cristobal (31.7),a Paloma (8.9)a,b | 544 | 1 084 664 |
| 2009 | Claudette (37.8), One (10.4),a Ida (30.7)a | 6 | 1 068 770 |
| 2010 | Hermine (51.8), Alex (32.0),a Bonnie (30.6),a Earl (31.4),a Five (24.9),a Nicole (19.9),a Paula (16.1),a Two (24.8)a | 22 | 1 083 043 |
| 2011 | Irene (68.5),b Lee (39.9), Bret (18.3),a Don (26.6),a Emily (14.3)a | 193 | 1 099 280 |
| 2012 | Beryl (51.0), Isaac (63.3), Sandy (64.5),b Alberto (25.2),a Debby (30.2)a | 196 | 1 111 594 |
| 2013 | Andrea (40.5), Dorian (16.0),a Karen (16.9)a | 81 | 1 135 359 |
| 2014 | Arthur (76.2) | 55 | 1 148 798 |
| 2015 | Ana (38.7), Bill (49.9), Claudette (19.7)a | 19 | 1 182 341 |
| 2016 | Colin (44.9), Hermine (63.1), Julia (44.1), Matthew (68.0),b Bonnie (29.1),a Eight (16.5)a | 270 | 1 196 221 |
| 2017 | Cindy (44.1), Emily (37.4), Harvey (103.2),b Irma (91.9),b Nate (60.6),b Jose (23.9),a Philippe (8.6)a | 166 | 1 226 793 |
| 2018 | Alberto (36.8), Florence (79.4),b Gordon (57.4), Michael (130.5),b Chris (15.7)a | 354 | 1 235 862 |
| Total | 4978 | 33 619 393 |
Did not contribute any tropical cyclone exposures in the US.
Cyclone name subsequently retired by the World Meteorological Organization because of destruction caused in the US or elsewhere.
Deaths
During 1988-2018, in included counties, there were 38 756 460 deaths. For the 6 studied causes (cancers, cardiovascular diseases, infectious and parasitic diseases, injuries, neuropsychiatric conditions, and respiratory diseases) there were 33 619 393 deaths (Table) (86.7% of total deaths in tropical cyclone–exposed counties); 16 691 681 females and 16 927 712 males died from the 6 studied causes, and 81.1% of female deaths and 67.9% of male deaths were among those 65 years or older (eFigures 2 and 3 in the Supplement). Cardiovascular diseases were the leading cause of death overall (129.6 DPM), by sex (98.9 and 157.1 DPM for females and males), for age 65 years or older (1053.7 DPM), and social vulnerability tertile (109.0 DPM for SVI tertitle 1; 130.4 for tertile 2; 156.8 for tertile 3) (eTables 2 and 3 in the Supplement). Deaths from injuries were mostly among those aged 0 to 64 years (59.2% for females and 78.1% for males) and were the leading cause of death for this age group (43.7 DPM).
Association of Tropical Cyclones and Hurricanes With Total Death Rates
Highest overall increases were observed in injury-related mortality after tropical cyclones, peaking 1 month after cyclone (3.7% [95% CrI, 2.5%-4.9%]; 2.0 [95% CrI, 1.3-2.7] additional DPM; 54.3 to 56.3 DPM) and the month of a hurricane (33.4% [95% CrI, 28.3%-38.8%]; 18.2 [95% CrI, 15.4-21.1] additional DPM; 54.5 to 72.7 DPM) (Figure 2; eTable 4 in the Supplement).
Figure 2. Percentage Change in Death Rates per 1-Day Increase in Monthly Tropical Cyclone or Hurricane-Only Exposure by Cause of Death, and Lag Time.
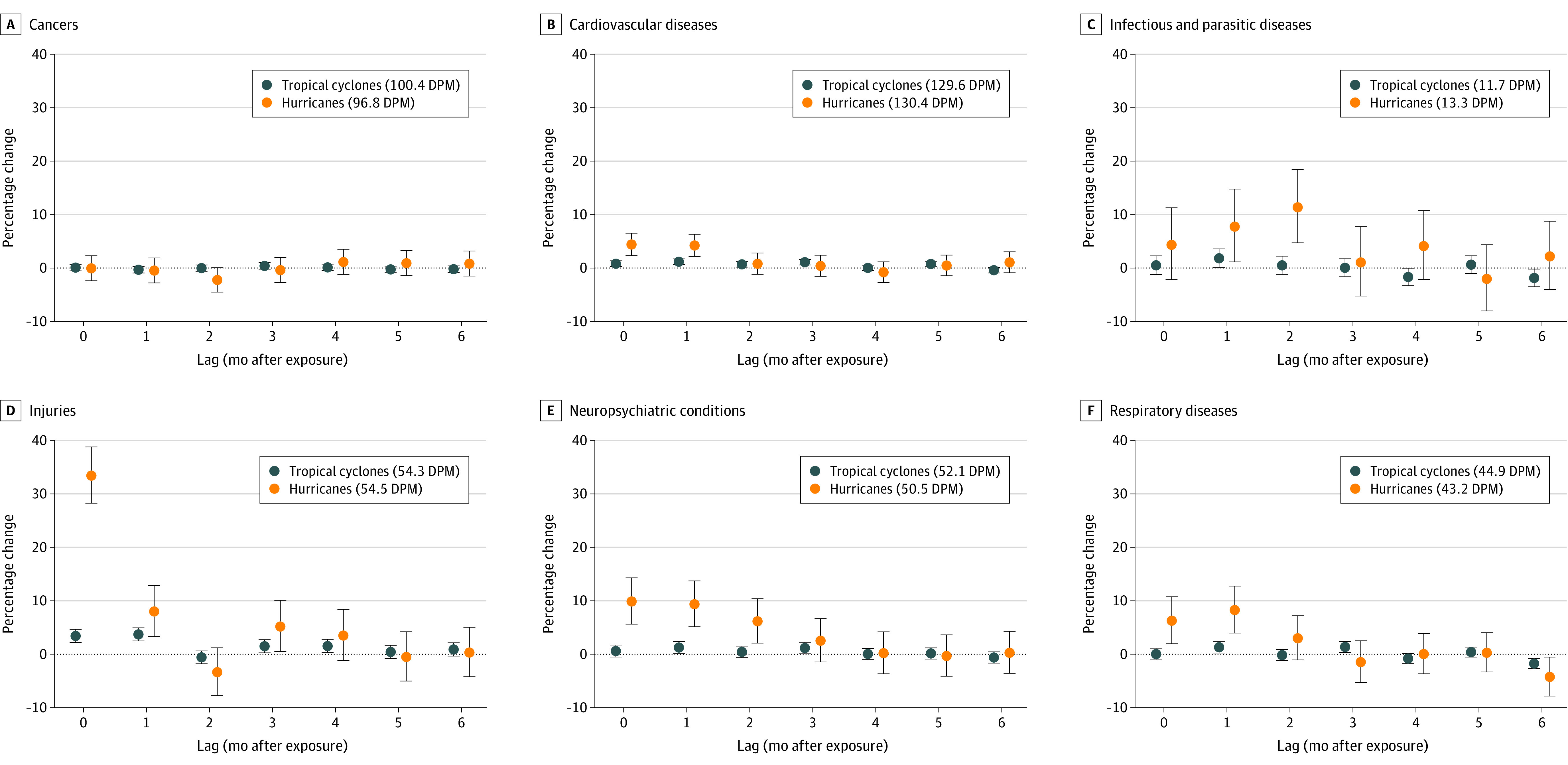
Dots indicate point estimates; whiskers, 95% credible intervals. Values in parentheses indicate overall deaths per 1 000 000 for 2018 monthly age-standardized median rate (DPM). Pneumonia-type deaths were classified as respiratory diseases.
Infectious and parasitic disease death rate increases peaked 1 month after cyclone (1.8% [95% CrI, 0.1%-3.6%]; 0.2 [95% CrI, 0.0-0.4] additional DPM; 11.7 to 11.9 DPM) and 2 months after hurricane (11.4% [95% CrI, 4.7%-18.4%]; 1.5 [95% CrI, 0.6-2.4] additional DPM; 13.3 to 14.8 DPM). Respiratory disease death rate increases peaked 1 month after cyclone (1.3% [95% CrI, 0.2%-2.4%]; 0.6 [95% CrI, 0.1-1.1] additional DPM; 44.9 to 45.5 DPM), and 1 month after hurricane (8.3% [95% CrI, 4.0%-12.7%]; 3.6 [95% CrI, 1.7-5.5] additional DPM; 43.2 to 46.8 DPM). Cardiovascular disease death rate increases peaked 1 month after cyclone (1.2% [95% CrI, 0.6%-1.7%]; 1.5 [95% CrI, 0.8-2.2] additional DPM; 129.6 to 131.1 DPM) and the month of a hurricane (4.4% [95% CrI, 2.3%-6.5%]; 5.7 [95% CrI, 3.0-8.5] additional DPM; 130.4 to 136.1 DPM). Neuropsychiatric condition death rate increases peaked 1 month after cyclone (1.2% [95% CrI, 0.1%-2.4%]; 0.6 [95% CrI, 0.1-1.2] additional DPM; 52.1 to 52.7 DPM) and the month of a hurricane (9.9% [95% CrI, 5.6%-14.3%]; 5.0 [95% CrI, 2.8-7.2] additional DPM; 50.5 to 55.5 DPM). Cancer death rates did not change in the 6 months after tropical cyclones or hurricanes (eg, 1 month after cyclone, −0.3% [95% CrI, −0.9% to 0.3%]; −0.3 [95% CrI, −0.9 to 0.3] additional DPM; 100.4 to 100.1 DPM).
Association of Tropical Cyclones With Death Rates by Age Group and Sex
Increases in injury death rates were larger for persons 65 years or older in the first 2 months after a tropical cyclone (Figure 3; eTable 5 in the Supplement) (>99% posterior probability) (eg, 1 month after cyclone, 6.4% [95% CrI, 4.2%-8.7%]; 6.2 [95% CrI, 4.0-8.4] additional DPM; 96.6 to 102.8 DPM for 65 years or older and 2.7% [95% CrI, 1.3%-4.2%]; 1.2 [95% CrI, 0.6-1.8] additional DPM; 43.7 to 44.9 DPM for age 0-64 years).
Figure 3. Percentage Change in Death Rates per 1-Day Increase in Monthly Tropical Cyclone Exposure by Cause of Death, Age Group (0-64 Years, ≥65 Years), and Lag Time.
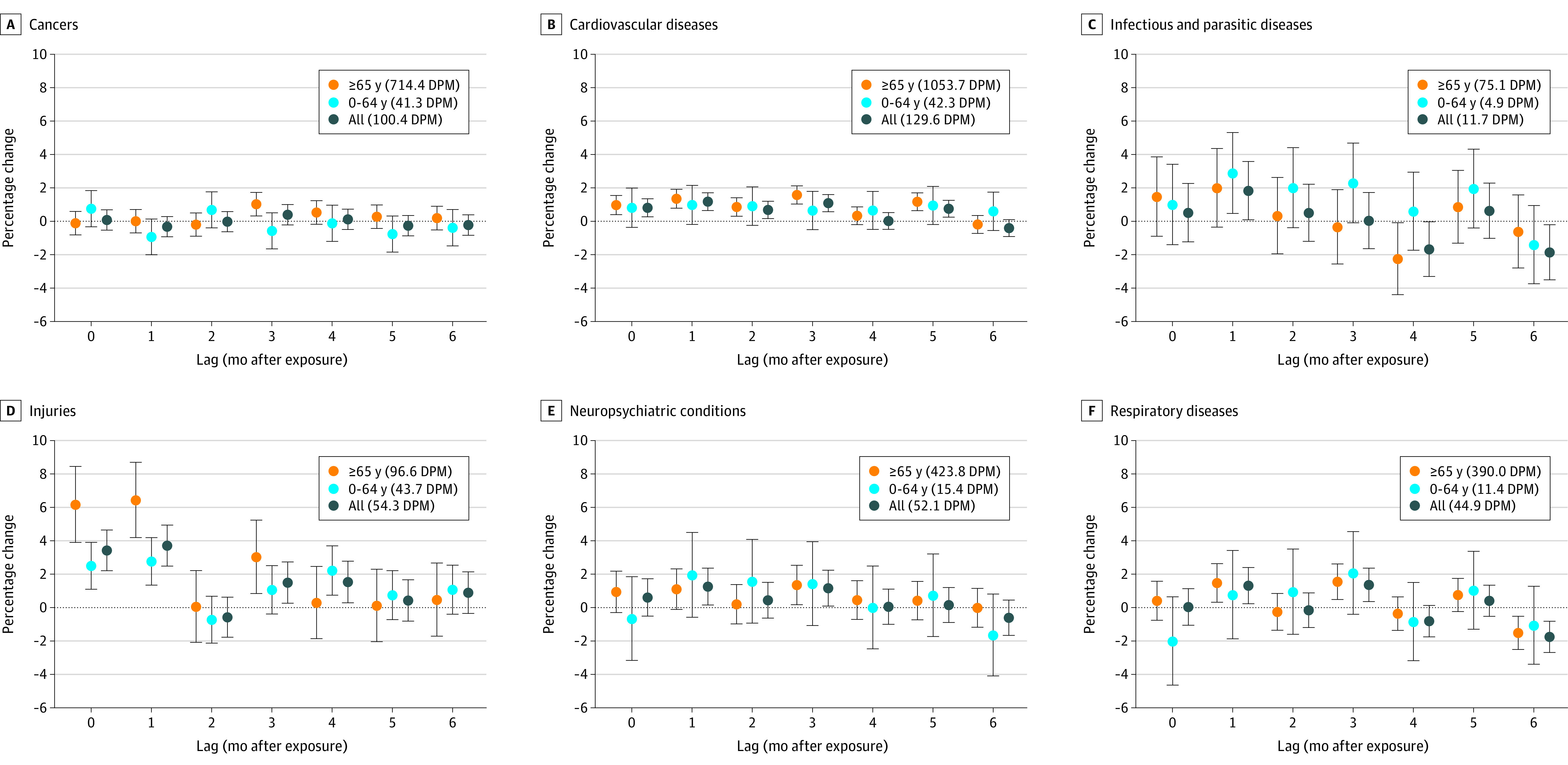
Dots indicate point estimates; whiskers, 95% credible intervals. Values in parentheses indicate overall deaths per 1 000 000 for 2018 monthly age-standardized median rate (DPM). Pneumonia-type deaths were classified as respiratory diseases.
The association of hurricanes by broad age group as well as by finer age groupings (eFigures 6-8 in the Supplement) was also examined in stratified analyses. For females and males, associations were largely consistent and similar (eFigures 9 and 10 in the Supplement), although relative increases in injury death rates in the month of a hurricane were higher for females than for males (>99% posterior probability) (46.5% [95% CrI, 37.3%-56.4%]; 13.7 [95% CrI, 11.0-16.6] additional DPM; 29.5 to 43.2 DPM for females and 27.6% [95% CrI, 21.9%-33.6%]; 21.0 [95% CrI, 16.7-25.6] additional DPM; 76.1 to 97.1 DPM for males).
Association of Tropical Cyclones With Death Rates by Social Vulnerability
For injuries, death rates in the most vulnerable tertile (3) were larger than the least vulnerable tertile (1) 1 month after cyclone (5.5% [95% CrI, 3.1%-7.8%]; 3.3 [95% CrI, 1.9-4.8] additional DPM; 60.8 to 64.1 DPM for most vulnerable [tertile 3] and 2.6% [95% CrI, 0.1%-5.0%]; 1.2 [95% CrI, 0.1-2.4] additional DPM; 46.7 to 47.9 DPM for least vulnerable [tertile 1]; 96% posterior probability that rates in tertile 3 were greater than those in tertile 1) (Figure 4; eTable 6 in the Supplement). The association of hurricanes by social vulnerability was also examined, with greater than 99% posterior probability that increases in injury death rates in tertile 3 were greater than those in tertile 1 in the month of a hurricane (eFigure 11 in the Supplement). There was a correlation of 0.91 between the first year available of SVI data (2000) and the SVI data used in this analysis (2018) (eFigure 5 in the Supplement).
Figure 4. Percentage Change in Death Rates per 1-Day Increase in Monthly Tropical Cyclone Exposure by Cause of Death, Social Vulnerability Tertiles, and Lag Time.
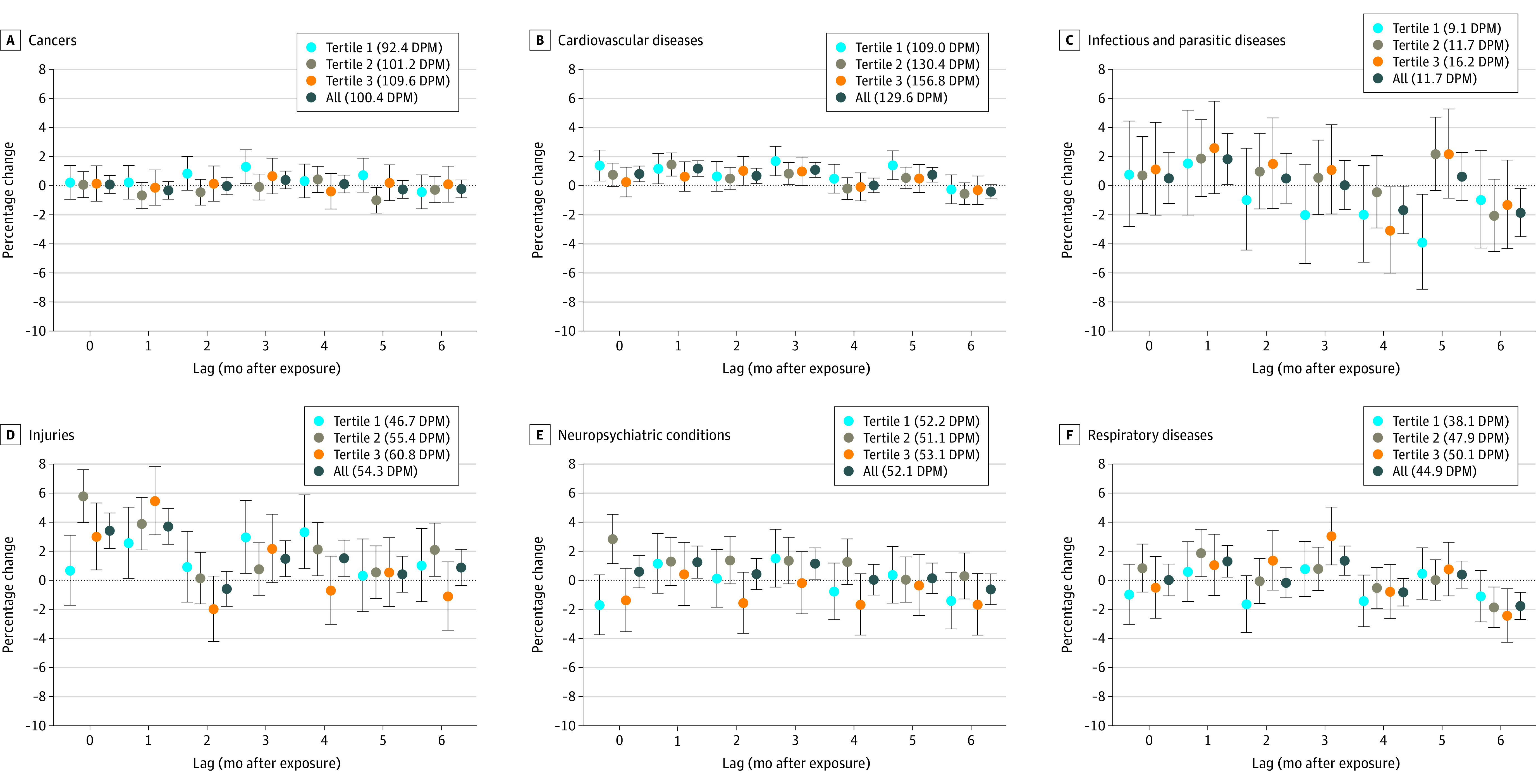
Tertile 1 represents lowest social vulnerability; tertile 3, highest social vulnerability. Dots indicate point estimates; whiskers, 95% credible intervals. Values in parentheses indicate overall deaths per 1 000 000 for 2018 monthly age-standardized median rate (DPM). Pneumonia-type deaths were classified as respiratory diseases.
Full results of formal comparisons by posterior draws of model parameters are reported in eTables 7-12 in the Supplement.
Sensitivity Analyses
For temperature sensitivity analyses (eFigure 12 in the Supplement), there was correlation of R = 0.99 and a slope of 1.00 (95% CrI, 0.98-1.01) between estimates of associations with (main analysis) and without (sensitivity analysis) temperature in the model. For sensitivity analyses limiting county-month matching to control periods in nearby years (eFigure 13 in the Supplement), there was a correlation of R = 0.95 and a slope of 0.95 (95% CrI, 0.88-1.05) between estimates of associations without (main analysis) and with (sensitivity analysis) the 5-year matching control period restriction. The same conclusions would be drawn from the main and sensitivity analyses.
Discussion
Among US counties that experienced at least 1 tropical cyclone from 1988-2018, each additional cyclone day per month was associated with modestly higher death rates in the months following the cyclone for several causes of death.
There were generally county-level increases in death rates on the month of and months after tropical cyclones when compared with the same months in years without tropical cyclones. Directly related deaths are caused by the physical forces of tropical cyclones, whereas indirect deaths are caused by unsafe or unhealthy conditions in their aftermath.1 Well-known direct threats to lives include drowning while driving motor vehicles in shallow water, being mortally wounded from flying objects, and electrocution from downed power lines.1,27,28,29 The observed increases up to 6 months after tropical cyclones for some outcomes indicates that some associations could be due to indirect pathways, such as cardiovascular failure, medical equipment outage, and disruption of normal care for persons already vulnerable.1,28
After a tropical cyclone, injury deaths could result from direct causes, such as drowning,27,30 and indirect causes, such as mortal injuries sustained in cleanup efforts or intentional self-harm from economic hardship after destruction of property.1 Infectious and parasitic diseases may spread from compromised drinking water and sanitation, damage to water pipes, and disruption to treatment plants, as well as standing water.1 Cardiovascular disease death increases have been linked to heart attacks and cardiac arrests from physical overexertion,28 as well as increases in stress31 and disruption in treatment of chronic conditions.32 Traumatic psychological consequences and a high prevalence of anxiety-mood disorders were evident after Hurricane Harvey and Hurricane Katrina.30 There was increased risk of dementia diagnosis after natural disasters such as earthquakes and tsunamis in Japan.33 Respiratory disease deaths could be related to disrupted power supplies for breathing aids.34,35 High winds during tropical cyclones may spread dust and other particulates into the air, exacerbating chronic respiratory diseases.36 Residents in low-income and historically disadvantaged communities have been differentially affected after disasters,37 consistent with some findings in the current study of larger relative and absolute increases in death rates in socially vulnerable counties.
Leveraging complete death data from 33.6 million deaths and a curated tropical cyclone data set over a 31-year period, this study is the first, to our knowledge, comprehensive investigation of the association of tropical cyclones with cause-specific deaths and by age group, sex, and social vulnerability.
Limitations
This study has several limitations. First, a potential limitation is exposure misclassification, if decedents’ recorded county of residence differs from the actual location during a tropical cyclone. Exposure misclassification, however, is likely nondifferential, as it is not expected to be correlated with the outcomes assessed, potentially biasing toward the null.38 Second, the analysis may have been susceptible to confounding. By matching on county-month of tropical cyclone occurrence and using the conditional Poisson model to account for the matching, this design controls for factors varying across counties, as well as month and season, but the possibility of residual confounding by unknown or unmeasured factors cannot be ruled out. Long-term trends, such as temperature and population age composition, were also adjusted for by temperature terms and in age-stratified models, respectively. Any variable would have to covary with both death rates and tropical cyclones in counties and be independent of the variables included in analyses to induce residual confounding.
Third, wind speed was used as an identifier of hurricanes and tropical cyclones; the causal pathways will include other environmental hazards and should be further explored. Fourth, this study was focused on the continental US, although devastating effects of hurricanes, such as Hurricane Maria in Puerto Rico, have also been recorded.13
Fifth, the overall association of tropical cyclone exposure with death rates over more than 3 decades was examined; however, like any exposure, results may have variations over time, space, and communities, which future work should highlight and examine further, as well as examine excess mortality by specific events. Sixth, the spatial unit of analysis was US county. Counties contain disparities within them, which was not captured by the analysis. Future work may be able to study associations by smaller areal units, eg, zip code, as appropriate exposure and outcome data become available.
Seventh, analysis of social vulnerability used 2018 values for the entire study period; however, rankings of social vulnerability change over time, although there was a high correlation of social vulnerability when comparing first available (2000) and last available (2018) years. Eighth, the data used extended only through 2018, and it is unknown whether the findings of this study reflect more recent cyclone activity and mortality following cyclones.
Conclusions
Among US counties that experienced at least 1 tropical cyclone from 1988-2018, each additional cyclone day per month was associated with modestly higher death rates in the months following the cyclone for several causes of death, including injuries, infectious and parasitic diseases, cardiovascular diseases, neuropsychiatric conditions, and respiratory diseases.
eAppendix
eTables 1-12
eFigures 1-13
References
- 1.Shultz JM, Russell J, Espinel Z. Epidemiology of tropical cyclones: the dynamics of disaster, disease, and development. Epidemiol Rev. 2005;27(1):21-35. doi: 10.1093/epirev/mxi011 [DOI] [PubMed] [Google Scholar]
- 2.Peduzzi P, Chatenoux B, Dao H, et al. Global trends in tropical cyclone risk. Nature Climate Change. 2012;2(4):289-294. doi: 10.1038/nclimate1410 [DOI] [Google Scholar]
- 3.Weinkle J, Landsea C, Collins D, et al. Normalized hurricane damage in the continental United States 1900–2017. Nat Sustain. 2018;1(12):808-813. doi: 10.1038/s41893-018-0165-2 [DOI] [Google Scholar]
- 4.Parks RM, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, Kioumourtzoglou MA. Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat Commun. 2021;12(1):1545. doi: 10.1038/s41467-021-21777-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang S, Toumi R. Recent migration of tropical cyclones toward coasts. Science. 2021;371(6528):514-517. doi: 10.1126/science.abb9038 [DOI] [PubMed] [Google Scholar]
- 6.National Oceanic and Atmospheric Administration . Atlantic Hurricane season takes infamous top spot for busiest on record. Published 2020. Accessed November 24, 2020. https://www.noaa.gov/news/2020-atlantic-hurricane-season-takes-infamous-top-spot-for-busiest-on-record
- 7.Li L, Chakraborty P. Slower decay of landfalling hurricanes in a warming world. Nature. 2020;587(7833):230-234. doi: 10.1038/s41586-020-2867-7 [DOI] [PubMed] [Google Scholar]
- 8.US Census Bureau . Coastal areas. Published 2020. Accessed May 13, 2021. https://www.census.gov/topics/preparedness/about/coastal-areas.html
- 9.National Oceanic and Atmospheric Administration . National Coastal Population Report: Population Trends From 1970 to 2020. Published 2021. Accessed May 13, 2021. https://coast.noaa.gov/digitalcoast/training/population-report.html
- 10.Hsiang S, Kopp R, Jina A, et al. Estimating economic damage from climate change in the United States. Science. 2017;356(6345):1362-1369. doi: 10.1126/science.aal4369 [DOI] [PubMed] [Google Scholar]
- 11.Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the Centers for Disease Control and Prevention’s Social Vulnerability Index. J Environ Health. 2018;80(10):34-36. [PMC free article] [PubMed] [Google Scholar]
- 12.Bodenreider C, Wright L, Barr O, Xu K, Wilson S. Assessment of social, economic, and geographic vulnerability pre- and post-Hurricane Harvey in Houston, Texas. Environ Justice. 2019;12(4):182-193. doi: 10.1089/env.2019.0001 [DOI] [Google Scholar]
- 13.Kishore N, Marqués D, Mahmud A, et al. Mortality in Puerto Rico after Hurricane Maria. N Engl J Med. 2018;379(2):162-170. doi: 10.1056/NEJMsa1803972 [DOI] [PubMed] [Google Scholar]
- 14.Kim S, Kulkarni PA, Rajan M, et al. Hurricane Sandy (New Jersey): mortality rates in the following month and quarter. Am J Public Health. 2017;107(8):1304-1307. doi: 10.2105/AJPH.2017.303826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shultz JM, Galea S. Preparing for the next Harvey, Irma, or Maria—addressing research gaps. N Engl J Med. 2017;377(19):1804-1806. doi: 10.1056/NEJMp1712854 [DOI] [PubMed] [Google Scholar]
- 16.Anderson GB, Ferreri J, Al-Hamdan M, et al. Assessing United States county-level exposure for research on tropical cyclones and human health. Environ Health Perspect. 2020;128(10):107009. doi: 10.1289/EHP6976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.PRISM Climate Group . The PRISM Climate and Weather System—An Introduction. Published 2013. Accessed February 2, 2022. https://prism.oregonstate.edu/documents/PRISM_history_jun2013.pdf
- 18.World Health Organization . Medical Certification of Cause of Death: Instructions for Physicians on Use of International Form of Medical Certificate of Cause of Death. World Health Organization; 1979. [PMC free article] [PubMed] [Google Scholar]
- 19.Boerma T, Mathers CD. The World Health Organization and global health estimates: improving collaboration and capacity. BMC Med. 2015;13(1):50. doi: 10.1186/s12916-015-0286-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Armstrong BG, Gasparrini A, Tobias A. Conditional Poisson models: a flexible alternative to conditional logistic case cross-over analysis. BMC Med Res Methodol. 2014;14:122. doi: 10.1186/1471-2288-14-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, Rubin DB. Bayesian Data Analysis. 3rd ed. CRC Press; 2013. doi: 10.1201/b16018 [DOI] [Google Scholar]
- 22.Schwartz J. The distributed lag between air pollution and daily deaths. Epidemiology. 2000;11(3):320-326. doi: 10.1097/00001648-200005000-00016 [DOI] [PubMed] [Google Scholar]
- 23.Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA. 2014;312(24):2659-2667. doi: 10.1001/jama.2014.15715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095-2128. doi: 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parks RM, Bennett JE, Foreman KJ, Toumi R, Ezzati M. National and regional seasonal dynamics of all-cause and cause-specific mortality in the USA from 1980 to 2016. Elife. 2018;7:e35500. doi: 10.7554/eLife.35500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murray CJ, Kulkarni S, Ezzati M. Eight Americas: new perspectives on US health disparities. Am J Prev Med. 2005;29(5)(suppl 1):4-10. doi: 10.1016/j.amepre.2005.07.031 [DOI] [PubMed] [Google Scholar]
- 27.Rappaport EN. Fatalities in the United States from Atlantic tropical cyclones: new data and interpretation. Bull Am Meteorological Soc. 2014;95(3):341-346. doi: 10.1175/BAMS-D-12-00074.1 [DOI] [Google Scholar]
- 28.Rappaport EN, Blanchard BW. Fatalities in the United States indirectly associated with Atlantic tropical cyclones. Bull Am Meteorological Soc. 2016;97(7):1139-1148. doi: 10.1175/BAMS-D-15-00042.1 [DOI] [Google Scholar]
- 29.Tellman B, Schank C, Schwarz B, Howe PD, de Sherbinin A. Using disaster outcomes to validate components of social vulnerability to floods: flood deaths and property damage across the USA. Sustainability. 2020;12(15):6006. doi: 10.3390/su12156006 [DOI] [Google Scholar]
- 30.Shultz JM, Galea S. Mitigating the mental and physical health consequences of Hurricane Harvey. JAMA. 2017;318(15):1437-1438. doi: 10.1001/jama.2017.14618 [DOI] [PubMed] [Google Scholar]
- 31.Cruz-Cano R, Mead EL. Causes of excess deaths in Puerto Rico after Hurricane Maria: a time-series estimation. Am J Public Health. 2019;109(7):1050-1052. doi: 10.2105/AJPH.2019.305015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB; Myocardial Infarction Data Acquisition System (MIDAS 24) Study Group . The effect of Hurricane Sandy on cardiovascular events in New Jersey. J Am Heart Assoc. 2014;3(6):e001354. doi: 10.1161/JAHA.114.001354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hikichi H, Aida J, Kondo K, et al. Increased risk of dementia in the aftermath of the 2011 Great East Japan Earthquake and Tsunami. Proc Natl Acad Sci U S A. 2016;113(45):E6911-E6918. doi: 10.1073/pnas.1607793113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lane K, Charles-Guzman K, Wheeler K, Abid Z, Graber N, Matte T. Health effects of coastal storms and flooding in urban areas: a review and vulnerability assessment. J Environ Public Health. 2013;2013:913064. doi: 10.1155/2013/913064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu H, Davidson RA, Rosowsky DV, Stedinger JR. Negative binomial regression of electric power outages in hurricanes. J Infrastructure Syst. 2005;11(4):258-267. doi: 10.1061/(ASCE)1076-0342(2005)11:4(258) [DOI] [Google Scholar]
- 36.World Meteorological Organization . Sand and dust storms. Published 2017. Accessed November 17, 2021. https://public.wmo.int/en/https%3A//www.wmo.int/sdswas
- 37.Fothergill A, Peek LA. Poverty and disasters in the United States: a review of recent sociological findings. Natural Hazards. 2004;32(1):89-110. doi: 10.1023/B:NHAZ.0000026792.76181.d9 [DOI] [Google Scholar]
- 38.Carroll RJ, Ruppert D, Stefanski LA, Crainiceanu CM. Measurement Error in Nonlinear Models: A Modern Perspective. CRC Press; 2006. doi: 10.1201/9781420010138 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix
eTables 1-12
eFigures 1-13


