Abstract
Background
Wearing facemasks is of proven efficacy as a public health protective measure against COVID-19. Currently there are no observational data concerning the wearing of facemasks and the adherence to guidelines concerning their handling.
Methods
Registration of the way passers-by were wearing facemasks at 26 different locations of five major cities in Greece. The results were correlated with the rate of COVID-19 deaths in the region.
Results
In total, 119,433 passers-by were registered, 57,043 females (47.8%) and 62,390 males (52.2%). From the total sample, 81.1% were wearing the mask properly, 10.8% had their nose out, 6.2% were wearing it under the jaw, and 1.9% had no mask at all . There was a significant difference between males and females concerning any use of mask. Inappropriate use of was correlated with COVID-19 death rate in the studied region.
Conclusion
Our findings suggest that under conditions of mandatory wearing and in central locations of major cities, during walking, proper use of masks is suboptimal, but still contributes with some protection. Fear and risk perception seem to be strong factors contributing to adherence to proper mask wearing.
Keyword: Facemasks, COVID-19, Health behavior
Background
The first to use a face mask for sanitary reasons with a modern theory in mind were Johann Mikulicz, head of the surgery department of the University of Breslau (now Wroclaw, Poland), and Paul Berger in Paris in 1897 [1]. Today it is known that when a contagious person coughs or sneezes, droplets containing infectious particles could be released [2, 3]. The importance of suppressing this potential source of pathogens was shown during the Manchurian plague of 1910–11, the influenza pandemic of 1918–19, and more recent 2003 and 2009 influenza pandemics [1].
Airborne transmission is probably the dominant way of COVID-19 transmission [4–9]; hence, wearing face masks is among the most efficacious, cheapest, and easiest measures to control it [10, 11]. Other measures include ventilation, air cleaning devices, and similar [12, 13]. Eventually, masks were recommended by government authorities and their usefulness was supported by scientific data [14–37], but unfortunately early in the course of the pandemic conflicting opinions and recommendations were made. This caused much confusion [38], and probably led to lower adherence with mask wearing or improper use of them. This in turn could have led to an at least partially cancel of their protective effect [39–41].
Many governments have implemented mandatory facemasks even in public open spaces. However, the efficacy of such measure depends on the material the mask is built upon as well as on the way masks are used. Also, as most public health sanitary measures, the protective effect of mask wearing tends to be more collective than personal; it demands that the overwhelming majority of the population will adopt the measure and will adhere to the rules and guidelines.
At the time of the study, there seems to be much uncertainty as well as a discrepancy. The uncertainty concerned the degree of adoption of the measure by the population. There are some poll data, but they are based on self-report online questionnaires and reports are anecdotal. Until now, there are no observational data concerning facemasks wearing of and the adherence to guidelines concerning its handling. Also, there are no data on the quality of facemasks and the materials they are made of.
The extent to which public health measures and appropriate health-related behaviors are adopted by the general public is a matter of great importance and should be the focus of mental health professionals. This kind of behaviors seem to stem from psychological characteristics and also follow the rules of mass psychology. In the future, managing of problematic attitudes and behaviors could be a prime target when facing a pandemic or other kinds of crises and mass destruction, and therefore, the studying these phenomena during the current pandemic is essential.
This study aimed at collecting observational data about the ways of wearing facemask in public, by observing and counting passers-by walking on the street under real-life situations. The outcome should be considered as reflecting the adherence to protective measures in general. The observational conditions chosen are considered to reflect the condition under which adherence is the maximum (walking in public, not socializing, mandatory use, monitoring by the police).
Methods
The aim of this study was to register the rates of passers-by wearing facemasks, their sex, and age group as well as the way they were wearing the mask, during a period of obligatory mask wearing in open spaces.
This study was an initiative by the School of Medicine under the auspice of the Rector of the Aristotle University of Thessaloniki in collaboration with the Panhellenic Medical Association. It took place between 18 November and 13 December 2020 and was approved by the Ethics committee, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki Greece.
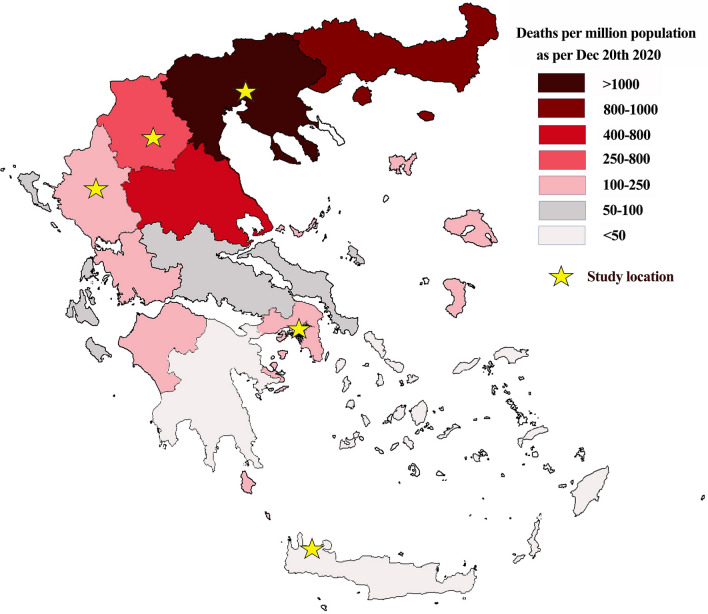
Data collection was performed by fourteen researchers at 26 different locations of five big cities in Greece, both in the morning and in the afternoon for periods of three hours each time. The five cities were in areas of the country with different standardized COVID-19 mortality rates (Fig. 1).
Fig. 1.
Map of Greece with the five centers and COVID-19 mortality rates per administrative region
The registration included gender and estimated age group. Field workers registered the way the person was using the mask as follows: (a) correctly, (b) nose out, (c) under the jaw, and (d) not at all. Age was classified into five age groups: 15–17 years, 18–30, 31–45, 46–60, and > 60. Age was registered according to the estimation by the rater; no contact with passers-by was initiated.
Only passers-by were registered; hence, there was no information collected for people standing, visiting any kind of shop, discussing with others, socializing etc., in order to have a homogenous result. The reason why the person was not wearing his/her mask properly (e.g., drinking or smoking while walking) was not taken into account. There were no questions concerning the material of the mask or the details of its use (cleaning, touching, etc.).
In cases passers-by were too many to register, the rater was instructed to register as many as possible in a consecutive but not selective sequence, and to record the instance. No such an instance was reported.
The composition of the study sample was compared with population data from the Greek Statistics Authority (ELSTAT) from www.statistics.gr, and expected numbers were calculated.
Official data on COVID-19 death rates until December 20, 2021, published by the Ministry of Health (Fig. 1) were used for the five locations.
The statistical analysis included Chi-square for the testing of frequencies and Spearman correlation coefficients were used to test for the relationship between mask wearing and COVID-19 deaths in the region at the time of data collection.
Results
In total, 119,433 passers-by were registered, 57,043 females (47.76%) and 62,390 males (52.24%).
From the total sample, 96,818 (81.06%) were wearing the mask properly, 12,906 (10.81%) had their nose out, 7451 (6.24%) were wearing it under the jaw, and 2258 (1.89%) had no mask at all. In detail the results are shown in Table 1.
Table 1.
Facemasks wearing by sex and age group and COVID-19 death rates in the five regional districts of the country
| N | Nose out | Jaw | Not at all | Total | % | Nose out | Jaw | Not at all | Jaw + not at all | Regional COVID-19 death rate | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Correctly | Correctly | Males | Females | |||||||||
| Males | 48,228 | 7630 | 5003 | 1529 | 62,390 | 77.30 | 12.23 | 8.02 | 2.45 | 10.47 | ||
| < 18 | 1943 | 553 | 328 | 233 | 3057 | 63.56 | 18.09 | 10.73 | 7.62 | 18.35 | ||
| 18–30 | 11,062 | 1877 | 1360 | 310 | 14,609 | 75.72 | 12.85 | 9.31 | 2.12 | 11.43 | ||
| 30–45 | 11,885 | 1775 | 1302 | 475 | 15,437 | 76.99 | 11.50 | 8.43 | 3.08 | 11.51 | ||
| 45–60 | 13,127 | 2037 | 1239 | 362 | 16,765 | 78.30 | 12.15 | 7.39 | 2.16 | 9.55 | ||
| > 60 | 10,211 | 1388 | 774 | 149 | 12,522 | 81.54 | 11.08 | 6.18 | 1.19 | 7.37 | ||
| Females | 48,590 | 5276 | 2448 | 729 | 57,043 | 85.18 | 9.25 | 4.29 | 1.28 | 5.57 | ||
| < 18 | 2013 | 425 | 235 | 86 | 2759 | 72.96 | 15.40 | 8.52 | 3.12 | 11.63 | ||
| 18–30 | 13,659 | 1626 | 807 | 167 | 16,259 | 84.01 | 10.00 | 4.96 | 1.03 | 5.99 | ||
| 30–45 | 14,561 | 1570 | 777 | 271 | 17,179 | 84.76 | 9.14 | 4.52 | 1.58 | 6.10 | ||
| 45–60 | 12,230 | 1160 | 486 | 155 | 14,031 | 87.16 | 8.27 | 3.46 | 1.10 | 4.57 | ||
| > 60 | 6127 | 495 | 143 | 50 | 6815 | 89.90 | 7.26 | 2.10 | 0.73 | 2.83 | ||
| Athens | 19,322 | 1985 | 1565 | 873 | 23,745 | 81.37 | 8.36 | 6.59 | 3.68 | 10.27 | 272.53 | 156.35 |
| Thessaloniki | 57,168 | 7399 | 4494 | 1165 | 70,226 | 81.41 | 10.54 | 6.40 | 1.66 | 8.06 | 1330.13 | 840.71 |
| Ptolemaida | 8721 | 1416 | 633 | 122 | 10,892 | 80.07 | 13.00 | 5.81 | 1.12 | 6.93 | 500.78 | 472.13 |
| Ioannina | 9460 | 1193 | 646 | 91 | 11,390 | 83.06 | 10.47 | 5.67 | 0.80 | 6.47 | 205.10 | 122.75 |
| Chania | 2147 | 913 | 113 | 7 | 3180 | 67.52 | 28.71 | 3.55 | 0.22 | 3.77 | 51.84 | 19.08 |
From all the age groups, only females aged over 45 years old, manifested correct use of mask above 85%.
Chi-square test revealed a significant difference between males and females concerning any use of mask (chi-square = 1353.606, df = 3, p < 0.0001), and this was true in all sub-groups: correct vs not-correct use of the mask (Chi-square = 1205.583, df = 1, p < 0.0001), correct or nose out vs jaw or not at all (Chi-square = 958.039, df = 1, p < 0.0001), and any use vs not at all (Chi-square = 220.942, df = 1, p < 0.0001).
There was also a difference among the age groups both for males (Chi-square = 796.015, df = 16, p < 0.0001) and for females (Chi-square = 2439.912, df = 16, p < 0.0001).
Both for gender and for age groups, the differences were significant for all paired comparisons.
The comparison of the study population with the general population of the country revealed an excess of males and young females in our sample (Table 2).
Table 2.
Comparison of the study sample gender and age distribution with the general population
| General population | % | Observed in study sample | Expected | Difference % from expected | ||
|---|---|---|---|---|---|---|
| N | N | % | N | |||
| Males | 4,459,864 | 48.06 | 62,390 | 52.24 | 57,397.54 | 8.70 |
| 15–17 | 273,727 | 2.95 | 3057 | 2.56 | 3522.811 | – 13.22 |
| 18–30 | 599,106 | 6.46 | 14,609 | 12.23 | 7710.372 | 89.47 |
| 31–45 | 1,191,268 | 12.84 | 15,437 | 12.93 | 15,331.38 | 0.69 |
| 46–60 | 1,087,118 | 11.71 | 16,765 | 14.04 | 13,990.99 | 19.83 |
| > 60 | 1,308,645 | 14.10 | 12,522 | 10.48 | 16,842 | – 25.65 |
| Females | 4,820,236 | 51.94 | 57,043 | 47.76 | 62,035.46 | – 8.05 |
| 15–17 | 263,919 | 2.84 | 2759 | 2.31 | 3396.584 | – 18.77 |
| 18–30 | 587,150 | 6.33 | 16,259 | 13.61 | 7556.501 | 115.17 |
| 31–45 | 1,194,031 | 12.87 | 17,179 | 14.38 | 15,366.94 | 11.79 |
| 46–60 | 1,177,657 | 12.69 | 14,031 | 11.75 | 15,156.21 | – 7.42 |
| > 60 | 1,597,479 | 17.21 | 6815 | 5.71 | 20,559.23 | – 66.85 |
Spearman correlation coefficients between COVID-19 death rates per region and rates of mask wearing (data shown in Table 1) were below 0.3 for all correlations except from those concerning ‘mask under the jaw’ and ‘not at all,’ for both male and female death rates, which were above 0.7. No correlation was significant eventually due to the small size of the dataset; therefore, only the analysis of numerical values is possible.
Discussion
During 2020, almost 95% of the world population was living in countries where the use of facemasks in public places was mandatory at some time and for prolonged periods of time, in order to contain the COVID-19 pandemic. There are specialized medical facemasks and cloth facemasks with the latter being washable and reusable and aiming to be used by the general population [42, 43].
Although, eventually, masks were recommended by government authorities and their usefulness was supported by scientific data [14–37], early in the course of the pandemic conflicting opinions and recommendations were made, leading to long-lasting confusion [38]. Improper wearing or mishandling of masks could at least partially cancel their protective effect [39–41]. The extent of this problem in the real world is unknown; however, models of the protective effect under different conditions have been proposed [40, 41]. Until now there was no report on the actual adoption of mask wearing especially in European countries, which is a determining factor for the real-world success of such a measure of public health. To our knowledge, the only study concerning the efficacy of facemasks in open spaces was underpowered and its methodology conceived masks as if they are an independent measure of self-protection [44], which is one of the most faulty ways of studying their usefulness. An additional problem was that around the world, the overall quality of these masks is relatively unknown [45].
To our knowledge, the current is one of the first studies in the literature to register the real-world use of facemasks under mandatory conditions. Unfortunately, our findings do not agree with the positive speculation for an excellent adoption of facemasks by the public in front of a deadly pandemic [46]. They suggest that in the middle of the second wave of the pandemic, under conditions of mandatory wearing, and in central places of major cities, during walking, proper use of masks is on average around 80% and only in females aged over 45 the percentage climbs above 85%. It is reasonable to assume that in almost all other conditions the adherence would be significantly lower. We should add the unknown specifications of mask fabric and the unknown adherence to guidelines on how to handle the mask. These findings, together with their most probable interpretation, suggest that the measure of mask wearing may be working but at a suboptimal level, and in combination with a reasonable lockdown they probably lead to a 50% reduction in death rates [40, 41], but it proved to be insufficient to prevent the third wave of the pandemic which eventually hit the country.
The second finding of this study was that percentage of people not wearing masks correlates with both male and female COVID-19 death rates in the region. This implies that the determining factor for adherence behavior is fear and risk perception rather than information, or at least it constitutes a very strong element [47–50].
The third important finding was related with sex and age composition of the study sample in comparison to the general population. While the composition of circulating people under normal conditions is unknown, the results of the current study suggest that middle aged and older females (all aged > 45) have probably reduced their time outside home. In males this was also evident maybe only in those above 60 years of age. It is to be noted, however, that the age was roughly estimated, so there is some kind of uncertainty concerning this variable and this should be considered as a limitation of the current study.
Taking all these together, the conclusion should be that the use of mask by the public is suboptimal but still probably partially efficacious. This should be considered together with the finding that cases and deaths were steadily going downwards even after more than a month after the end of the data collection of the current study.
Mask wearing is culturally strange in western societies in contrast to east Asian ones who consider this kind of behavior as social and collective responsibility [51]. Still, the pandemic has changed radically western views but the extent of this is largely unknown and of unknown influence on the end-efficacy [52]. There are reports suggesting better adherence to facemask wearing with increasing age [53] and with higher rates in females (54). Both these are confirmed by our findings, which additionally suggest the relationship with age is linear. The gender difference is impressive; no male age group has higher rate from any female group except from the very young aged < 18 (Table 1).
Apart from sociocultural elements, psychological characteristics are important in the adoption of health-related behaviors, and in this specific situation probably the cognitive style is of high importance. Emotions probably play a significant role and anger together with high level of anxiety was prominent in the general population during the period of the gathering of the data for the current study.
Conclusions
The results of the current study
suggest that mandatory mask wearing produced suboptimal results, but still probably exerted a significant effect on COVID-19 death rate;
provide a possible explanation why almost all countries around the world were eventually obliged to utilize some form of lockdown; and
suggest that difference in adherence between genders is at least one of many contributing factors in the observed difference between males and females concerning morbidity and mortality from COVID-19.
Acknowledgements
None.
Disclaimer
PT and JB are staff members of the World Health Organization. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Authors’ contributions
KNF, PT, PP, and SK conceived and designed the study. All the rest authors participated in data collection, creation, and certification of the dataset and made interim and preliminary analyses. KNF, EM, PT, PP, JB, and SK participated in data analysis. KNF wrote the first draft of the paper. All authors participated in interpreting the data and developing further stages of the paper. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Availability of data and materials
The data are available upon request from the first author.
Declarations
Ethical approval and consent to participate
This study was approved by the Ethics committee, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki Greece.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Konstantinos N. Fountoulakis, Email: Kostasfountoulakis@gmail.com
Joao Breda, Email: rodriguesdasilvabred@who.int.
Marianna P. Arletou, Email: marianna_arl29@hotmail.com
Anastasios I. Charalampakis, Email: charalampakisanastasios@gmail.com
Maria G. Karypidou, Email: mariakarupidou@gmail.com
Konstantina S. Kotorli, Email: konstantinaki134@gmail.com
Christina G. Koutsoudi, Email: christinaakoutsoudi@gmail.com
Eleftheria S. Ladia, Email: eleftherialadia@gmail.com
Calypso A. Mitkani, Email: m.calypso11@gmail.com
Vasiliki N. Mpouri, Email: bouribasia@gmail.com
Anastasia C. Samara, Email: anastasia_sama@yahoo.gr
Aikaterini S. Stravoravdi, Email: kate_st@outlook.com
Ioannis G. Tsiamis, Email: drtsiamis@gmail.com
Aphrodite Tzortzi, Email: afrotzw1@gmail.com.
Maria A. Vamvaka, Email: maria.vamv1@gmail.com
Charikleia N. Zacharopoulou, Email: charikleiazaxar@gmail.com
Panagiotis E. Prezerakos, Email: prezerpot@gmail.com
Sotirios A. Koupidis, Email: sotirioskoupidis@yahoo.gr
Nikolaos K. Fountoulakis, Email: nikolasfountoulakis@gmail.com.
Eva Maria Tsapakis, Email: emtsapakis@doctors.org.uk.
Anastasia Konsta, Email: tetakonsta322@gmail.com.
Pavlos N. Theodorakis, Email: theodorakisp@who.int
References
- 1.Strasser BJ, Schlich T. A history of the medical mask and the rise of throwaway culture. Lancet. 2020;396(10243):19–20. doi: 10.1016/S0140-6736(20)31207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chao CYH, Wan MP, Morawska L, Johnson GR, Ristovski ZD, Hargreaves M, et al. Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. J Aerosol Sci. 2009;40(2):122–133. doi: 10.1016/j.jaerosci.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicas M, Nazaroff WW, Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J Occup Environ Hyg. 2005;2(3):143–154. doi: 10.1080/15459620590918466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci USA. 2020;117(26):14857–14863. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu W, Tang F, Fang L-Q, de Vlas SJ, Ma H-J, Zhou J-P, et al. Risk factors for SARS infection among hospital healthcare workers in Beijing: a case control study. Tropical Med Int Health. 2009;14(s1):52–59. [Google Scholar]
- 6.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burke RM, Midgley CM, Dratch A, Fenstersheib M, Haupt T, Holshue M, et al. Active monitoring of persons exposed to patients with confirmed COVID-19—United States, January–February 2020. MMWR Morb Mortal Wkly Rep. 2020;69(9):245–246. doi: 10.15585/mmwr.mm6909e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jefferson T, Del Mar CB, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev. 2020;11(11):CD006207. doi: 10.1002/14651858.CD006207.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Sande M, Teunis P, Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS ONE. 2008;3(7):e2618. doi: 10.1371/journal.pone.0002618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen C, Zhao B, Cui W, Dong L, An N, Ouyang X. The effectiveness of an air cleaner in controlling droplet/aerosol particle dispersion emitted from a patient's mouth in the indoor environment of dental clinics. J R Soc Interface. 2010;7(48):1105–1118. doi: 10.1098/rsif.2009.0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Y, Leung GM, Tang JW, Yang X, Chao CY, Lin JZ, et al. Role of ventilation in airborne transmission of infectious agents in the built environment—a multidisciplinary systematic review. Indoor Air. 2007;17(1):2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 14.Brooks JT, Butler JC, Redfield RR. Universal masking to prevent SARS-CoV-2 transmission—the time is now. JAMA. 2020;324(7):635–637. doi: 10.1001/jama.2020.13107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization 2020;Pages: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak. Accessed 5 Mar 2022.
- 16.MacIntyre CR, Chughtai AA. A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int J Nurs Stud. 2020;108:103629. doi: 10.1016/j.ijnurstu.2020.103629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitze T, Kosfeld R, Rode J, Walde K. Face masks considerably reduce COVID-19 cases in Germany. Proc Natl Acad Sci USA. 2020;117(51):32293–32301. doi: 10.1073/pnas.2015954117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hendrix MJ, Walde C, Findley K, Trotman R. Absence of Apparent transmission of SARS-CoV-2 from two stylists after exposure at a hair salon with a universal face covering policy—Springfield, Missouri, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):930–932. doi: 10.15585/mmwr.mm6928e2. [DOI] [PubMed] [Google Scholar]
- 19.Leffler CT, Ing E, Lykins JD, Hogan MC, McKeown CA, Grzybowski A. Association of country-wide coronavirus mortality with demographics testing, lockdowns, and public wearing of masks. Am J Trop Med Hyg. 2020;103(6):2400–2411. doi: 10.4269/ajtmh.20-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan JF, Yuan S, Zhang AJ, Poon VK, Chan CC, Lee AC, et al. Surgical mask partition reduces the risk of noncontact transmission in a golden Syrian hamster model for coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2020;71(16):2139–2149. doi: 10.1093/cid/ciaa644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gandhi M, Beyrer C, Goosby E. Masks do more than protect others during COVID-19: reducing the inoculum of SARS-CoV-2 to protect the wearer. J Gen Intern Med. 2020;35(10):3063–3066. doi: 10.1007/s11606-020-06067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schunemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5(5):e002794. doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Payne DC, Smith-Jeffcoat SE, Nowak G, Chukwuma U, Geibe JR, Hawkins RJ, et al. SARS-CoV-2 infections and serologic responses from a sample of US navy service members—USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):714–721. doi: 10.15585/mmwr.mm6923e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doung-Ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Case-control study of use of personal protective measures and risk for SARS-CoV 2 infection Thailand. Emerg Infect Dis. 2020;26(11):2607–2616. doi: 10.3201/eid2611.203003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aiello AE, Murray GF, Perez V, Coulborn RM, Davis BM, Uddin M, et al. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: a randomized intervention trial. J Infect Dis. 2010;201(4):491–498. doi: 10.1086/650396. [DOI] [PubMed] [Google Scholar]
- 28.Aiello AE, Perez V, Coulborn RM, Davis BM, Uddin M, Monto AS. Facemasks, hand hygiene, and influenza among young adults: a randomized intervention trial. PLoS ONE. 2012;7(1):e29744. doi: 10.1371/journal.pone.0029744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Canini L, Andreoletti L, Ferrari P, D'Angelo R, Blanchon T, Lemaitre M, et al. Surgical mask to prevent influenza transmission in households: a cluster randomized trial. PLoS ONE. 2010;5(11):e13998. doi: 10.1371/journal.pone.0013998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cowling BJ, Chan KH, Fang VJ, Cheng CK, Fung RO, Wai W, et al. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann Intern Med. 2009;151(7):437–446. doi: 10.7326/0003-4819-151-7-200910060-00142. [DOI] [PubMed] [Google Scholar]
- 31.Cowling BJ, Fung RO, Cheng CK, Fang VJ, Chan KH, Seto WH, et al. Preliminary findings of a randomized trial of non-pharmaceutical interventions to prevent influenza transmission in households. PLoS ONE. 2008;3(5):e2101. doi: 10.1371/journal.pone.0002101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Larson EL, Ferng YH, Wong-McLoughlin J, Wang S, Haber M, Morse SS. Impact of non-pharmaceutical interventions on URIs and influenza in crowded, urban households. Public Health Rep. 2010;125(2):178–191. doi: 10.1177/003335491012500206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacIntyre CR, Cauchemez S, Dwyer DE, Seale H, Cheung P, Browne G, et al. Face mask use and control of respiratory virus transmission in households. Emerg Infect Dis. 2009;15(2):233–241. doi: 10.3201/eid1502.081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simmerman JM, Suntarattiwong P, Levy J, Jarman RG, Kaewchana S, Gibbons RV, et al. Findings from a household randomized controlled trial of hand washing and face masks to reduce influenza transmission in Bangkok Thailand. Influenza Other Respir Viruses. 2011;5(4):256–267. doi: 10.1111/j.1750-2659.2011.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Suess T, Remschmidt C, Schink SB, Schweiger B, Nitsche A, Schroeder K, et al. The role of facemasks and hand hygiene in the prevention of influenza transmission in households: results from a cluster randomised trial; Berlin, Germany, 2009–2011. BMC Infect Dis. 2012;12:26. doi: 10.1186/1471-2334-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.MacIntyre CR, Zhang Y, Chughtai AA, Seale H, Zhang D, Chu Y, et al. Cluster randomised controlled trial to examine medical mask use as source control for people with respiratory illness. BMJ Open. 2016;6(12):e012330. doi: 10.1136/bmjopen-2016-012330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu J, Xu F, Zhou W, Feikin DR, Lin CY, He X, et al. Risk factors for SARS among persons without known contact with SARS patients, Beijing. China Emerg Infect Dis. 2004;10(2):210–216. doi: 10.3201/eid1002.030730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fauci A. Dr. Fauci Says, “With All Due Modesty, I Think I’m Pretty Effective.”. In: O’Donnell N, ed. InStyleNew York; 2020.
- 39.Wolff R. At “Half Mask” or “Nose Commando:” A note demonstrating nasal breaths can spread microorganisms when improperly wearing a mask during COVID-19. MDPI AG; 2020.
- 40.Worby CJ, Chang HH. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nat Commun. 2020;11(1):4049. doi: 10.1038/s41467-020-17922-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang K, Vilches TN, Tariq M, Galvani AP, Moghadas SM. The impact of mask-wearing and shelter-in-place on COVID-19 outbreaks in the United States. Int J Infect Dis. 2020;101:334–341. doi: 10.1016/j.ijid.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MacIntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;350:h694. doi: 10.1136/bmj.h694. [DOI] [PubMed] [Google Scholar]
- 43.Gralton J, McLaws ML. Protecting healthcare workers from pandemic influenza: N95 or surgical masks? Crit Care Med. 2010;38(2):657–667. doi: 10.1097/ccm.0b013e3181b9e8b3. [DOI] [PubMed] [Google Scholar]
- 44.Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, Norsk JB, et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers : a randomized controlled trial. Ann Intern Med. 2020 doi: 10.7326/M20-6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clase CM, Fu EL, Ashur A, Beale RCL, Clase IA, Dolovich MB, et al. Forgotten technology in the COVID-19 pandemic: filtration properties of cloth and cloth masks—a narrative review. Mayo Clin Proc. 2020;95(10):2204–2224. doi: 10.1016/j.mayocp.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L. Face masks for the public during the covid-19 crisis. BMJ. 2020;369:m1435. doi: 10.1136/bmj.m1435. [DOI] [PubMed] [Google Scholar]
- 47.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 48.Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull. 2014;140(2):511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- 49.Brewer NT, Weinstein ND, Cuite CL, Herrington JE. Risk perceptions and their relation to risk behavior. Ann Behav Med. 2004;27(2):125–130. doi: 10.1207/s15324796abm2702_7. [DOI] [PubMed] [Google Scholar]
- 50.Slovic P, Finucane ML, Peters E, MacGregor DG. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Anal. 2004;24(2):311–322. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- 51.Cheng KK, Lam TH, Leung CC. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. Lancet. 2020;S0140–6736(20):30918–30921. doi: 10.1016/S0140-6736(20)30918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barceló J, Sheen G. Voluntary adoption of social welfare-enhancing behavior: mask-wearing in Spain during the COVID-19 outbreak. PLoS ONE. 2020;15(12):e0242764. doi: 10.1371/journal.pone.0242764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hutchins HJ, Wolff B, Leeb R, Ko JY, Odom E, Willey J, et al. COVID-19 mitigation behaviors by age group—United States, April–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1584–1590. doi: 10.15585/mmwr.mm6943e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Howard MC. Gender, face mask perceptions, and face mask wearing: are men being dangerous during the COVID-19 pandemic? Pers Individ Dif. 2021;170:110417. doi: 10.1016/j.paid.2020.110417. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available upon request from the first author.