Abstract
Background:
Because older adults are particularly vulnerable to nonoptimal temperatures, it is expected that the progressive population aging will amplify the health burden attributable to heat and cold due to climate change in future decades. However, limited evidence exists on the contribution of population aging on historical temperature–mortality trends.
Objectives:
We aimed to a) assess trends in heat- and cold-related mortality in Switzerland between 1969 and 2017 and b) to quantify the contribution of population aging to the observed patterns.
Methods:
We collected daily time series of all-cause mortality by age group (, 65–79, and 80 y and older) and mean temperature for each Swiss municipality (1969–2017). We performed a two-stage time-series analysis with distributed lag nonlinear models and multivariate longitudinal meta-regression to obtain temperature–mortality associations by canton, decade, and age group. We then calculated the corresponding excess mortality attributable to nonoptimal temperatures and compared it to the estimates obtained in a hypothetical scenario of no population aging.
Results:
Between 1969 and 2017, heat- and cold-related mortality represented 0.28% [95% confidence interval (CI): 0.18, 0.37] and 8.91% (95% CI: 7.46, 10.21) of total mortality, which corresponded to 2.4 and 77 deaths per 100,000 people annually, respectively. Although mortality rates for heat slightly increased over time, annual number of deaths substantially raised up from 74 (12;125) to 181 (39;307) between 1969–78 and 2009–17, mostly driven by the age group. Cold-related mortality rates decreased across all ages, but annual cold-related deaths still increased among the , due to the increase in the population at risk. We estimated that heat- and cold-related deaths would have been 52.7% and 44.6% lower, respectively, in the most recent decade in the absence of population aging.
Discussion:
Our findings suggest that a substantial proportion of historical temperature-related impacts can be attributed to population aging. We found that population aging has attenuated the decrease in cold-related mortality and amplified heat-related mortality. https://doi.org/10.1289/EHP9835
Background
Exposure to nonoptimal ambient temperatures is considered to be among the most important environmental health hazards (Murray et al. 2020). It has been associated with approximately 9.4% of the total mortality burden globally, corresponding to 74 deaths per 100,000 people a year (Zhao et al. 2021). This estimate is similar to the relative contribution of other environmental risk factors, such as long-term exposure to air pollution, which has been associated with 7.3% of total mortality globally (Murray et al. 2020). Cold-related deaths, usually defined as deaths associated with nonoptimal temperature on days below the temperature of minimum mortality (MMT), represent the largest contribution of nonoptimal temperature-related mortality [8.5% vs. 0.9% of heat-related deaths (days with temperature above the MMT), globally (Zhao et al. 2021)]. However, recent projection studies suggest that climate change will further amplify the mortality burden attributed to heat and eventually outweigh current cold-related deaths in the future in most locations worldwide (Gasparrini et al. 2017; Zhao et al. 2021).
Along with the threatening projections of a warmer climate, the world’s population is projected to grow older. Current demographic trajectories reveal that the world’s population age 65 y and older will increase substantially from 9% to 16% by 2050 (United Nations 2019). This increase would pose additional societal challenges in the future, in particular for public health, because older adults are considered to be a population subgroup that is particularly susceptible to different environmental hazards, including heat and cold (Achebak et al. 2019). This increased vulnerability to heat and cold can be explained by physiological differences in thermoregulation (Basu and Samet 2002), as well as housing (Kim et al. 2019), prevalence of comorbidities (Bunker et al. 2016; Schneider et al. 2017), and social isolation, among others (Kim et al. 2020; Son et al. 2019). Projection studies published so far concluded that the trends in future burden attributed to nonoptimal temperatures are largely driven by the increase in the pool of susceptible population (i.e., population ) (Chen et al. 2020; Lee et al. 2018; Lee and Kim 2016; Li et al. 2016; Marsha et al. 2018; Vardoulakis et al. 2014). Therefore, understanding the role of future changes in the demographic structure of the population on projected health impacts is critical to formulating efficient strategies for adaptation to climate change. Additionally, quantifying the contribution of these factors in the observed impacts in the past would provide useful insights on the potential mechanisms of action, help to interpret the projected impacts, and help to assess the viability of the proposed adaptation policies.
When assessing the heat-related mortality during the last decades, studies found a decline in heat-related vulnerability, suggesting partial adaptation of the population, whereas for cold the evidence remains unclear (Achebak et al. 2019; Arbuthnott et al. 2016; Bobb et al. 2014; Chung et al. 2018; Sera et al. 2020; Vicedo-Cabrera et al. 2018). As reviewed by Sheridan and Allen, previous studies have attempted to assess the role of several factors as potential drivers of the attenuation of vulnerability, including socioeconomic indicators, changes in infrastructure, and demographic factors, including population aging (Sheridan and Allen 2018). In particular, the role of population aging has mostly been assessed through the evaluation of temporal trends in age-specific mortality fractions attributable to nonoptimal temperatures (Achebak et al. 2019). However, evidence from these assessments only reflect relative changes in the mortality burden across time and age groups and neither disentangle nor quantify the contribution of underlying changes in the populations at risk (i.e., population aging) and the corresponding societal impacts.
In Switzerland, progressive aging of the population is already evident, with almost 20% of the population over age 65 y, a share that is set to further increase up to 30% by 2060 (Lewis and Ollivaud 2020). Besides progressive population aging, the effects of climate change are directly visible, because 9 out of the 10 hottest years have occurred in the 21st century (National Centre for Climate Services 2018; Suarez-Gutierrez et al. 2018, 2020; Watts et al. 2021). Moreover, a recent international assessment found that 37% of heat-related deaths can be attributed to human-induced climate change (Vicedo-Cabrera et al. 2021). Thus, this study aimed to assess the role of the progressive aging of the population on the trends in heat- and cold-related mortality impacts in Switzerland over the past 49 y. Specifically, we a) comprehensively explored heat- and cold-related mortality trends in Switzerland during the last five decades using high-resolution mortality and weather data and b) quantified the contribution of population aging to the observed patterns. The main methodological novelty of this study is that we accounted for the changes in the demographic structure of the population across time (i.e., aging) when assessing the trends in excess mortality due to nonoptimal temperature, which was unlike approaches taken in previous studies. By doing so, we were able to disentangle and quantify the contribution of aging to the temporal trends driven by adaptation and/or acclimatization.
Methods and Data
Data
Mortality data.
We collected all-cause mortality data in Switzerland between the 1 January 1969 and 31 December 2017 from the Federal Statistical Office (BFS). Ethical approval was not required because data were gathered from administrative sources through the corresponding agreement between parties. For each Swiss municipality, we computed the daily count of all-cause deaths by age category (which was divided into , 65–79 y, and ). We used the 2019 Swiss Official Commune Register as the reference for the municipality boundaries (Federal Statistical Office 2020). From the 2,212 municipalities, we merged 156 smaller municipalities with recorded deaths in 49 y with neighboring municipalities based on similar neighborhood types as characterized by the BFS (Bundesamt für Statistik Statistischer Atlas der Schweiz 2020), which ultimately amounted to 2,056 units of analysis (Figure S1).
Temperature data.
We obtained daily mean temperatures on a grid across the full Swiss geography from a gridded climate data set (MeteoSwiss-grid-product) provided by MeteoSwiss (Federal Office of Meteorology and Climatalogy MeteoSwiss 2020). This high-resolution gridded data allowed us to capture the temperature exposures in areas with a sparse monitor network (i.e., rural and mountainous areas) and assign a unique exposure to each of the 2,056 municipalities in Switzerland (de Schrijver et al. 2021; Spangler et al. 2019). We included the grid cells that intersected the boundaries of the municipality to create the municipality-specific temperature series. To properly account for the heterogeneous distribution of the population due to the irregular orography (Figures S2 and S3), we derived population-weighted daily mean temperature series across the study period for each Swiss municipality, as explained in a previous study (de Schrijver et al. 2021).
Statistical Analysis
Overview of the statistical method and rationale.
We assessed the temporal trends in heat- and cold-related mortality impacts in Switzerland and the influence of population aging in three steps. In brief, we first performed a two-stage time-series analysis to derive the decadal temperature–mortality associations for each canton and age category. We estimated the canton-specific association using temperature–mortality series in each municipality by decade while accounting for heterogeneity between municipalities and cantons. Second, we estimated the corresponding overall and decade-specific heat- and cold-related excess mortality for each canton and age category. The statistical framework for these two first steps has been previously applied in recent works (e.g., Gasparrini et al. 2015a). Finally, we quantified the excess heat- and cold-related mortality attributed to population aging by rescaling the observed impacts in each decade to the age structure of the population in the first decade (1969–1978), thus assuming a hypothetical scenario of no population aging. Differently from previous assessments of temporal trends, we accounted for changes in the demographic structure of the population across time by estimating the age-specific excess mortality using the corresponding baseline mortality in each age category, decade, and canton. This approach mimics the method used in assessments of projections of health impacts to account for socioeconomic and demographic scenarios (Vicedo-Cabrera et al. 2019).
Estimation of the heat- and cold-related mortality associations.
We applied an extension of the usual two-stage time-series approach to estimate the geographical and temporal variation in age-specific heat- and cold-related mortality association using high-resolution data. First, we performed separate first-stage models for each combination of canton, age category, and decade (1969–1978, 1979–1988, 1989–1998, 1999–2008, and 2009–2017). We applied the novel case time-series design, a method which allows the application of flexible time series techniques without the need of aggregating the data in a single series (Gasparrini 2021). Specifically, we defined multiple series of mortality and temperature at the municipality level within each canton and modeled them all together using a conditional quasi-Poisson regression (Armstrong et al. 2014; Gasparrini et al. 2010). We defined matching strata defined by year, month, and day of the week, which is similar to the idea of the bidirectional time-stratified case-crossover design, and municipality. This analytical approach provides a common exposure–response function for all municipalities in a canton using temperature and mortality data at a higher resolution (i.e., municipality level), thus increasing the precision of the estimates.
We modeled the temperature–mortality association using distributed lag nonlinear models. We defined a quadratic B-spline with three internal knots placed at the 10th, 75th, and 90th percentile of the canton-specific temperature distribution in the exposure dimension of the so-called cross-basis term of temperature (Gasparrini et al. 2010). We modeled the lag-response curve using a natural cubic B-spline with three internal knots placed at equally spaced values on the log scale up to 21 d to capture the long-lagged associations and short-term harvesting. We reduced the bidimensional exposure-lag-response curve to a one-dimensional overall cumulative exposure–response association to reduce the number of parameters while preserving complexity of the dependencies.
Then, we pooled the overall cumulative exposure–response associations derived in the previous step by decade, age category, and canton through a multivariate multilevel longitudinal meta-regression model (Sera et al. 2019a). This model included as fixed-effect predictors a factor variable of time (i.e., decade) and age category, and mean temperature (as numeric variable) in each canton and period. We tested for other variables (i.e., time-variant and invariant contextual variables); however, these did not end up being relevant based on the Wald test, Akaike criterion, and the assessment of the heterogeneity (Cochran Q bidimensional test and the statistic) (see the Supplementary Material for details, Table S1). We derived from the meta-analytic model the best linear unbiased predictions (BLUPs), which are improved estimates of temperature–mortality associations (Gasparrini et al. 2012; Sera et al. 2019a). For each combination of canton, age, and decade we derived the MMT, used as the reference, and the corresponding minimum mortality percentile (MMP) (defined between the 60th and 98th percentile of the decade-specific temperature distribution). The MMT corresponds to the temperature value for which the temperature-mortality risk is minimum, usually considered as optimal temperature (Gasparrini et al. 2015a).
Estimation of excess mortality impacts.
We calculated the excess mortality attributed to nonoptimal temperatures using the decade- and age-specific BLUPs and corresponding baseline mortality and temperature series in each canton, as described elsewhere (Gasparrini and Leone 2014). We computed the cold- and heat-related excess mortality by summing the daily contributions on days with temperatures lower or higher than the decade-age-canton–specific MMT. We calculated the corresponding 95% empirical confidence interval (eCI) using Monte Carlo simulations (Gasparrini and Leone 2014). We first reported the impacts as the total number of excess deaths attributed to cold and heat, and the average annual per subperiod. We also calculated the heat and cold mortality rates (per 100,000 people) by age category and decade. We collected historical population data per canton and age group from Historical Statistics of Switzerland (HSSO 2012). We used the population in the first year of the decade for each of the subperiods (e.g., 1970 for the 1969–1978 period, 1980 for the 1979–1988). To obtain comparable estimates across cantons, we calculated the heat- and cold-related age-standardized mortality rates using the average population distribution in each decade. We also estimated the overall mortality rates by age group (i.e., for the full study period) and the overall rate as an average of the corresponding decade-specific estimates.
Assessment of the impact of population aging on the observed trends.
We assessed the role of population aging in two ways. First, we compared the trends in average annual number of deaths and mortality rates by age group to disentangle the influence of changes in the size of the population at risk in each age group. Second, we compared the estimated all-age heat/cold mortality rates (observed) in each decade with the corresponding mortality rates calculated assuming the demographic structure of the population in the first decade, which is assuming that no changes in the population age composition had occured (i.e., no aging). In brief, we restructured the decade-specific population according to the relative age-group contribution in the first decade (1969–1978). In this way, we rescaled the observed population for each decade according to the age structure of 1969–1978 (i.e., assuming no population aging), while keeping constant the total population for the corresponding decade. We then calculated the heat- and cold-related deaths over the rescaled population by using the corresponding age- and decade-specific mortality rates estimated in the main analysis. This approach yielded the number of heat- and cold-related excess mortality in the hypothetical scenario of no population aging. We then expressed the difference percent between the excess mortality calculated with and without the population aging to quantify the contribution of population aging to the observed trend. As the population between the observed and the hypothetical scenario in each decade remained constant, the differences would only reflect the influence of the changes in demographic structure across decades (i.e., distribution of the population across age groups).
We used R software (version 4.01; R Development Core Team) for this data analysis. The dlnm package was used to create distributed lag nonlinear model (Gasparrini 2011), and the mixmeta package was used to fit the longitudinal multivariate meta-analysis (Sera et al. 2019a).
Results
Description of the Mortality and Temperature Series
Table 1 provides a summary description of the mortality and temperature data by decade from 1969 to 2017 aggregated by region in Switzerland (Table S2 reports the corresponding summary description for each canton; for further details on the spatial boundaries see Figure S1 and Table S3). We analyzed 2,986,581 death records throughout the 2,212 municipalities (2,056 aggregated units) covering the full Swiss geography. The age distribution of the total mortality changed over time, with the age group contributing 27.8% of the total annual deaths in 1969 and 60.8% in 2017 (Figure S4), which equates to an increase from 16,000 to 40,000 annual deaths in this age group. However, for the and 65–79-y-old age groups this proportion decreased from 29.8% to 13.6% and from 42.4% to 25.6%, respectively. The population size of the group also substantially increased from 111,285 to 372,894 people, the equivalent of 235%, between 1970 and 2010 (Figures S5 and S6). As shown in Table 1, we observe the warmest mean temperatures in the regions of northwest Switzerland and Ticino, and the coldest temperatures were registered in less populated and mountainous regions of eastern and central Switzerland. The daily mean temperature distribution progressively shifted toward warmer temperatures in all regions, with an average of approximately 2°C increase in 2009–2017 vs. 1969–1978.
Table 1.
Descriptive statistics by region for the total number of all-cause deaths, number of municipalities, and average daily mean temperature distributions (median and IQR) for the overall study period and by decade.
| Region | Deaths (n) | Municipalities (n) | ||||||
|---|---|---|---|---|---|---|---|---|
| 1969–2017 | 1969–1978 | 1979–1988 | 1989–1998 | 1999–2008 | 2009–2017 | |||
| 1. Lake Geneva | 511,754 | 418 | 7.9 (, 19.3) | 6.7 (, 18.1) | 6.9 (, 18.7) | 8.0 (, 19.0) | 8.6 (, 20.3) | 8.7 (, 20.2) |
| 2. Espace Mitteland | 747,935 | 617 | 8.1 (, 19.5) | 7.2 (, 18.6) | 7.6 (, 19.2) | 8.4 (, 19.5) | 8.9 (, 20.6) | 9.1 (, 20.7) |
| 3. Northwest Switzerland | 403,450 | 288 | 9.6 (, 21.2) | 8.4 (, 19.8) | 8.9 (, 20.5) | 9.8 (, 21.0) | 10.5 (, 22.2) | 10.6 (, 22.2) |
| 4. Zurich | 506,099 | 163 | 9.1 (, 21.1) | 8.0 (, 19.8) | 8.5 (, 20.5) | 9.3 (, 20.9) | 10.0 (, 22.2) | 10.1 (, 22.2) |
| 5. Eastern Switzerland | 439,438 | 304 | 7.0 (, 18.4) | 6.0 (, 17.3) | 6.4 (, 18.0) | 7.1 (, 18.2) | 7.7 (, 19.3) | 7.9 (, 19.3) |
| 6. Central Switzerland | 200,599 | 158 | 6.4 (, 17.6) | 5.4 (, 16.5) | 5.9 (, 17.2) | 6.6 (, 17.3) | 7.1 (, 18.6) | 7.5 (, 18.7) |
| 7. Ticino | 131,763 | 108 | 9.2 (, 21.1) | 8.2 (, 19.8) | 8.3 (, 20.5) | 9.3 (, 20.8) | 9.9 (, 22.0) | 10.3 (, 22.3) |
| Overall | 2,986,581 | 2,056 | 8.1 (, 19.7) | 7.0 (, 18.5) | 7.3 (, 19.1) | 8.3 (, 19.4) | 8.8 (, 20.6) | 9.0 (, 20.7) |
Note: IQR, interquartile range.
Overall Heat- and Cold-Related Excess Mortality
Total all-cause excess mortality associated with nonoptimal temperatures was 9.19% [95% confidence interval (CI): 7.72, 10.47], which translates to 274,578 (95% CI: 230,657, 312,761) temperature-related excess deaths in Switzerland between 1969 and 2017 (Table 2; Table S4). Cold-related mortality represented a larger fraction in comparison with heat, with 8.91% (95% CI: 7.46, 10.21) vs. 0.28% (95% CI: 0.18, 0.37). The corresponding annual all-age rates were 2.4 deaths (95% CI: 1.4, 3.4) and 77 deaths (95% CI: 63, 88) per 100,000 people, with heterogeneous impacts across age groups. The average heat-related mortality rate per 100,000 people between 1969 and 2017 was lower in the group, with 0.3 deaths (95% CI: 01, 0.5), followed by the 65–79 age group with 4.3 deaths (95% CI: 1.5, 6.6), and 48.2 deaths (95% CI: 33.3, 61.8) per 100,000 people for the group. For cold, the group is also most vulnerable, with on average 1,275 deaths (95% CI: 1,097, 1,431) per 100,000 people, although this was substantially lower for the 65–79-y-old and groups, with 239 deaths (95% CI: 193, 281) and 7 deaths (95% CI: 3, 11) per 100,000 people, respectively. The mortality fractions by age group are shown in Table 2.
Table 2.
Excess all-cause mortality related to nonoptimal temperature (heat, cold, and total), by age group and decade between 1969 and 2017 in Switzerland [number of deaths and fractions (%), and 95% confidence interval]. represents the corresponding total all-cause mortality for each study period and age group.
| Category | Sub-category | Measure of impact | Heat-related mortality (95% CI) | Cold-related mortality (95% CI) | Non-optimal temperature-related mortality (95% CI) |
|---|---|---|---|---|---|
| Total | 1969–2017 | Total () | 8,385 (5,482, 10,937) | 266,193 (222,842, 304,815) | 274,578 (230,657, 312,761) |
| () | Fraction (%)* | 0.28 (0.18, 0.37) | 8.91 (7.46, 10.21) | 9.19 (7.72, 10.47) | |
| Rate (per 100,000)* | 2.4 (1.4, 3.4) | 77 (63, 88) | 79 (66, 90) | ||
| Age | Total () | 953 (158, 1,645) | 21,418 (8,354, 32,540) | 22,372 (9,625, 33,316) | |
| () | Fraction (%)* | 0.16 (0.03, 0.27) | 3.55 (1.38, 5.38) | 3.71 (1.59, 5.52) | |
| Rate (per 100,000)* | 0.3 (0.1, 0.5) | 7 (3, 11) | 8 (3, 11) | ||
| 65–79 y | Total () | 1,508 (572, 2,530) | 92,903 (74,085, 107,898) | 93,227 (75,520, 109,623) | |
| () | Fraction (%)* | 0.17 (0.06, 0.26) | 9.26 (7.49, 10.90) | 9.42 (7.63, 11.07) | |
| Rate (per 100,000)* | 4.3 (1.5, 6.6) | 239 (193, 281) | 243 (197, 286) | ||
| Total () | 5,794 (4,003, 7,423) | 153,185 (131,787, 171,906) | 158,797 (137,495, 177,816) | ||
| () | Fraction (%)* | 0.42 (0.29, 0.53) | 10.99 (9.46, 12.34) | 11.41 (9.87, 12.76) | |
| Rate (per 100,000)* | 48.2 (33.3, 61.8) | 1,275 (1,097, 1,431) | 1,323 (1,145, 1,480) | ||
| Decade | 1969–1978 | Annual () | 74 (12, 125) | 6,559 (5,009, 7,985) | 6,633 (5,041, 8,096) |
| () | Fraction (%) | 0.13 (0.02, 0.22) | 11.52 (8.80, 14.03) | 11.65 (8.86, 14.22) | |
| Rate (per 100,000) | 1.2 (0.2, 2.0) | 105 (80, 127) | 106 (80, 129) | ||
| 1979–1988 | Annual () | 158 (76, 236) | 4,780 (3,780, 5,789) | 4,939 (3,941, 5,954) | |
| () | Fraction (%) | 0.27 (0.13, 0.40) | 8.03 (6.36, 9.73) | 8.30 (6.63, 10.01) | |
| Rate (per 100,000) | 2.5 (1.2, 3.7) | 75 (59, 91) | 78 (62, 94) | ||
| 1989–1998 | Annual () | 104 (10, 193) | 5,145 (3,839, 6,325) | 5,250 (3,918, 6,386) | |
| () | Fraction (%) | 0.17 (0.02, 0.31) | 8.22 (6.13, 10.11) | 8.39 (6.26, 10.21) | |
| Rate (per 100,000) | 1.5 (0.1, 2.8) | 75 (56, 92) | 76 (57, 93) | ||
| 1999–2008 | Annual () | 338 (239, 432) | 6,306 (5,052, 7,533) | 6,645 (5,360, 7,918) | |
| () | Fraction (%) | 0.55 (0.39, 0.70) | 10.23 (8.20, 12.23) | 10.78 (8.70, 12.85) | |
| Rate (per 100,000) | 4.7 (3.3, 6.0) | 87 (70, 105) | 92 (74, 110) | ||
| 2009–2017 | Annual () | 181 (39, 307) | 4,254 (2,642, 5,757) | 4,435 (2,807, 5,976) | |
| () | Fraction (%) | 0.28 (0.06, 0.48) | 6.59 (4.10, 8.92) | 6.87 (4.35, 9.26) | |
| Rate (per 100,000) | 2.1 (0.4, 3.5) | 49 (30, 66) | 51 (32, 68) |
The results of the excess mortality fractions and rates (per 100,000 people) over the total study period (1969–2017) should be interpreted with caution because these have been averaged over the total deaths and total population, respectively.
Temporal Trends in Heat- and Cold-Related Mortality
For heat, the average annual excess deaths more than doubled between 1969–1978 and 2009–2017 [from 74 (95% CI: 12, 125) to 181 deaths (95% CI: 39, 307)], whereas the overall heat-related mortality rate also increased but at a lower magnitude from 1.2 deaths (95% CI: 0.2, 2.0) to 2.1 deaths (95% CI: 0.4, 3.5) per 100,000 people. The 1999–2008 decade reported substantially higher annual heat-related deaths with 338 deaths (95% CI: 239, 432), which corresponds to 4.7 (95% CI: 3.3, 6.0) deaths per 100,000 people (Table 2; Table S4). When excluding the excess mortality in the year 2003 (when the massive European heat wave occured), annual heat-related mortality burden in this decade decreased to 234 deaths (95% CI: 153, 298), thus suggesting that the steep increase could partially be attributed to the 2003 heat wave (Table S5). Similar patterns can be observed in the group (Figure 1A and B), with the largest increase in annual excess deaths from 33 deaths (95% CI: , 59) in 1969–1978 to 162 (95% CI: 36, 278) deaths in 2009–2017, whereas the increase in mortality rates was not as substantial, from 29.4 deaths (95% CI: , 52.9) in 1969–1978 to 39.1 deaths (95% CI: 8.7, 67.1) per 100,000 people in 2009–2017. For the and 65–79 age groups, both the annual excess mortality as well as the mortality rates remained constant over time (See Table S4 for the corresponding figures).
Figure 1.
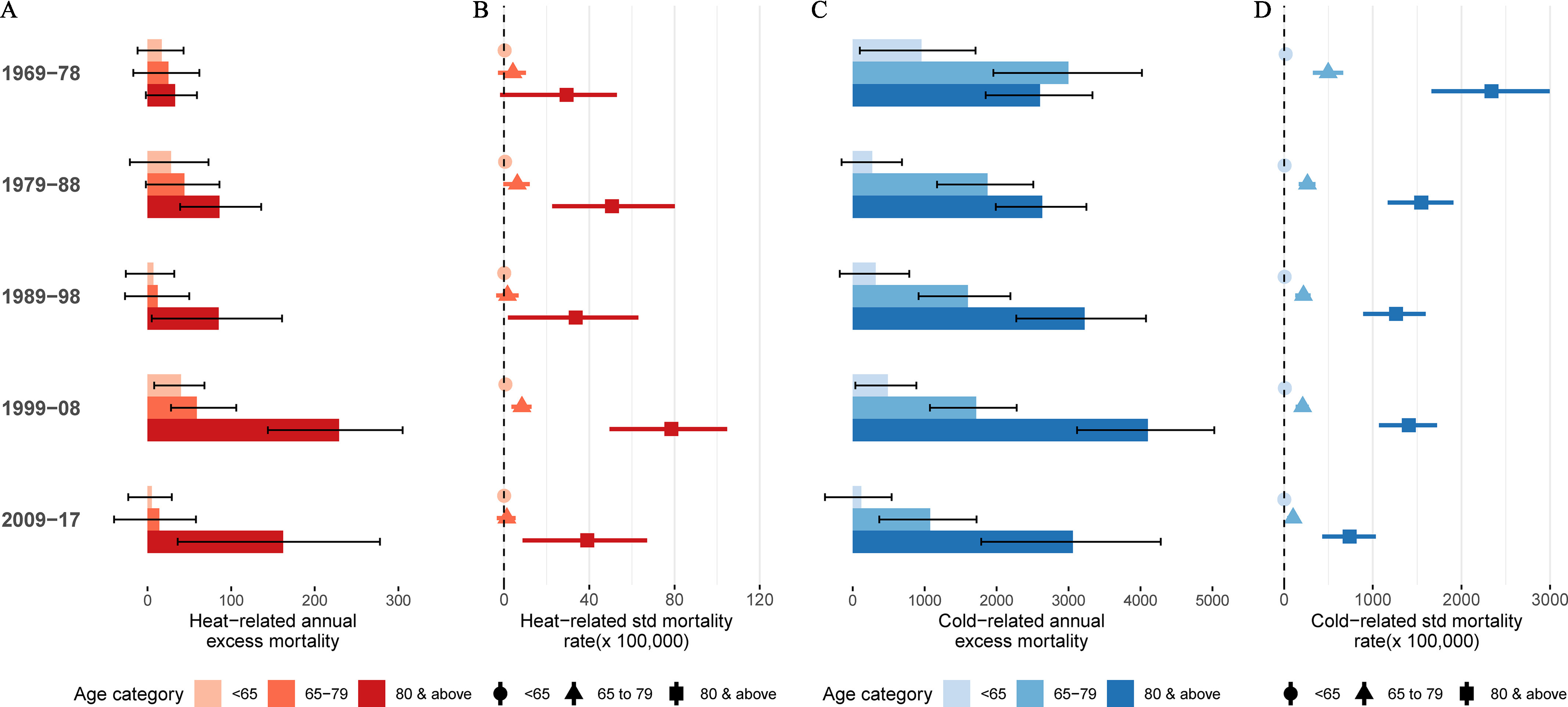
Annual excess mortality for heat (A,B) and cold (C,D) by decade and age group. Panels A and C report the age-specific annual excess deaths for heat and cold respectively, and panels B and D show the corresponding heat and cold-related mortality rates per 100,000 people. The point estimates with the corresponding 95% confidence interval are provided in Table S7.
Conversely, cold-related mortality decreased in Switzerland during the study period, from 6,559 (95% CI: 5,009, 7,985) in 1969–1978 to 4,254 (95% CI: 2,642, 5,757) annual deaths in 2009–2017, corresponding to a decrease in the overall rate from 105 deaths (95% CI: 80, 127) to 49 deaths (95% CI: 30, 66) per 100,000 people, respectively (Figure 1C,D; Table 2). All numbers illustrated in Figure 1 have been reported in the supplementary file (Table S4). The most substantial decrease in the cold-related excess mortality was among the 65–79 y age group, from 2,999 (95% CI: 1,955, 4,020) in 1969–1978 to 1,076 annual deaths (95% CI: 37, 1,722) in the 2009–2017 decade (Table S4). Similarly, mortality rates decreased from 497 deaths (95% CI: 324, 666) to 101 deaths (95% CI: 35, 161) in 2009–2017. Interestingly, among the , although mortality rates decreased from 2,339 deaths (95% CI: 1,663; 2,995) in 1969–1978 to 1,408 deaths (95% CI: 1,070, 1,725) per 100,000 people per year in 1999–2008, the corresponding annual number of deaths substantially increased from 2,603 (95% CI: 1,850, 3,333) to 4,102 deaths (95% CI: 3,119, 5,026) in the fourth decade (1999–2008). Both rates and number of deaths decreased from the fourth to the last decade. Furthermore, at the beginning of the study period, there were more annual cold-related deaths of the 65–79 y age group [2,999 annual deaths (95% CI: 1,955, 4,020)], whereas at the end of the period, the group reported the largest number, with 3,059 annual deaths (95% CI: 1,787, 4,283) in 2009–2017. For the group, the cold-related mortality rate has remained small and even close to null in the 2009–2017 decade, with 2 deaths (95% CI: , 11) per 100,000 people.
The observed trends in excess mortality align with the changes in risk and evolution of the MMT/MMP across decades in each age group (Figures S7–S8; Tables S6–S8). Overall, heat-related mortality risk remained fairly stable in all age groups across all decades, except for the 1999–2008 decade in which the risk substantially increased. For cold, mortality risk decreased in all age groups across the study period. Additionally, we found that the MMT for the and 65–79 age groups has increased over time, whereas the MMP has remained constant (Figure S7). For the group, the MMT has remained constant over time, whereas the MMPs decreased.
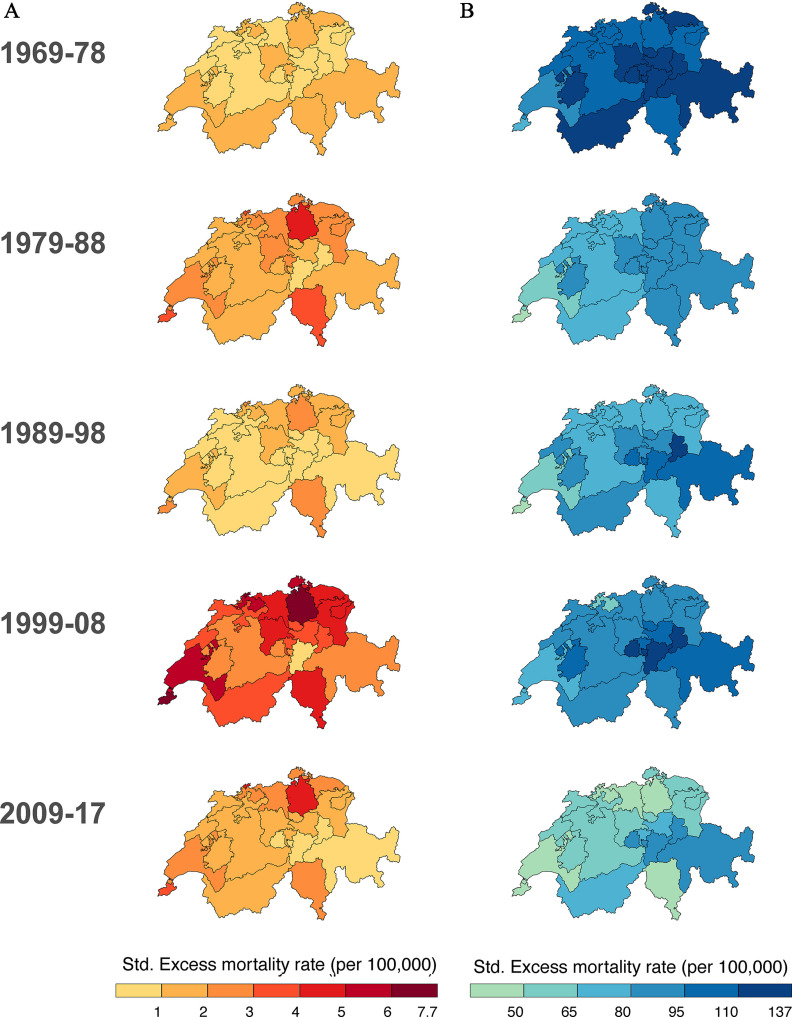
Furthermore, as shown in Figure 2, the geographical distribution of the heat-related excess mortality rates changed over the study period. Specifically, we can see that rates were similar across cantons in the first decades and started to spatially diverge in the 1980s with larger rates in northern and western Switzerland and lower rates in central Switzerland. For cold, a more homogenous decline among all cantons can be observed, with large spatial heterogeneity.
Figure 2.
Age-standardized (std.) excess mortality rate for heat (A) and cold (B) by decade per 100,000 people.
Impact of Population Aging
First, we found that the relative contribution of heat- and cold-related deaths in the group (over the all-age heat- and cold-related deaths) substantially increased across the study period (from 36.3% to 90.2% and from 39.0% to 70.8% for heat and cold, respectively) (Table S9). Figure 3 illustrates the contribution of population aging in the observed trend over the study period, as depicted by the difference between the dark and bright bars and the shown percentage on top. The contribution of population aging to the overall heat- and cold-related mortality trend increased from 21.7% in the 1979–1988 decade to 52.7% in the most recent decade and from 23.9% to 44.6%, respectively.
Figure 3.
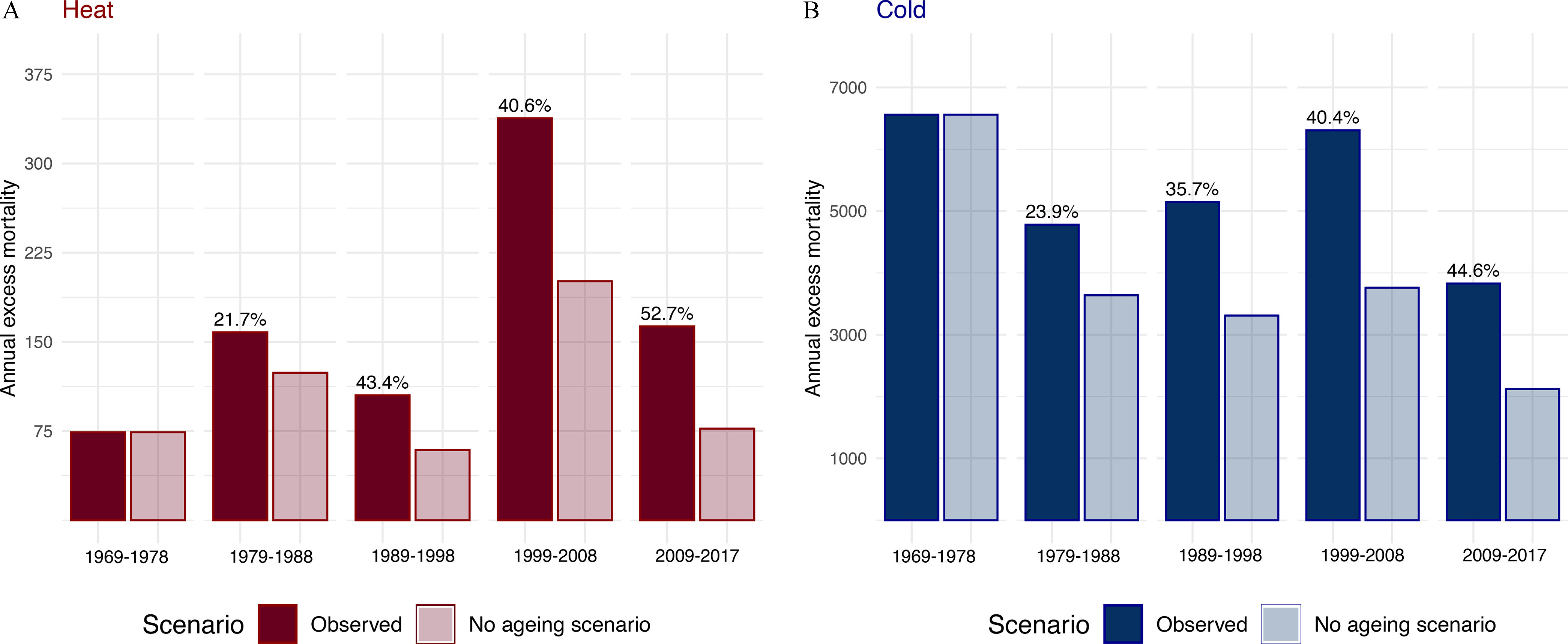
Panels A and B compare the observed annual heat- and cold-related number of excess deaths, respectively, with the excess mortality estimated in a scenario of no population aging. The percent reported on the “observed” bars illustrate the corresponding decade-specific percent difference between the observed annual heat and cold-related excess mortality and the scenario of no population aging in comparison with 1969–1978. The point estimates and difference percent between the observed and counter-factual scenario are provided in Table S9.
Discussion
In this nationwide study, we found evidence that population aging could have altered the temporal patterns in heat- and cold-related mortality between 1969 and 2017 in Switzerland. In particular, our results first confirm that a large proportion of heat- and cold-related mortality happens among the age groups above 65 y of age. We estimated that 0.28% and 8.91% of all-cause mortality, which corresponds to 2.4 and 77 deaths per 100,000 people per year, could be attributed to heat and cold, respectively. More than half of these were in the population of old. Second, vulnerability to heat increased for the group over the past 50 y, whereas the and 65–79-y-old populations showed signs of resilience. In contrast, although vulnerability to cold decreased across all age groups, the cold-related mortality burden, in terms of number of deaths, has continuously increased among the age group amid the increase in the pool of vulnerable individuals due to population aging. Finally, our findings suggest that a substantial proportion of temperature–mortality impacts can be attributed to population aging, amounting to 52.7% and 44.6% of heat- and cold-related mortality for the most recent decade.
We estimated that 9.2% of all-cause mortality during the last five decades in Switzerland can be attributed to nonoptimal temperatures. This amounted to 8,385 and 266,193 excess deaths in total for heat and cold, of which 64% were among the group. Additionally, we found that heat-related deaths almost tripled between 1969–1978 and 2009–2017, which was largely a result of an increase in the group, whereas it slightly decreased in the y and 65–79 y age groups. The observed increase in heat vulnerability contradicts findings in other retrospective studies, which found a reduction of risks, suggesting a partial adaptation of the population to the increase in temperature (Achebak et al. 2019; Gasparrini et al. 2015b; Nordio et al. 2015; Vicedo-Cabrera et al. 2018). In particular, a recent multicountry study found an overall decline in heat-related excess mortality in Switzerland (Vicedo-Cabrera et al. 2018). However, it should be noted that this study included a shorter study period (1995–2012), coinciding with the period between 1999–2008 and 2009–2017 decades in which we found a similar decline in heat-related mortality. In our analysis, the 2003 heat wave was shown to partially drive the exceptionally high annual heat-related mortality for the 1999–2008 decade (Grize et al. 2003). However, when excluding the year 2003, we still observed higher excess heat-related mortality in comparison with the period 2009–2017. For cold, we observed an overall decreasing trend in excess mortality rates between 1969–1978 and 2009–2017, which is consistent with existing findings (Achebak et al. 2019; Vicedo-Cabrera et al. 2018). This decline is a result of changes in vulnerability and relative risk for cold temperatures, commonly attributable to changes in infrastructure, changes in health care access, and other improved vulnerability factors (Arbuthnott et al. 2016).
Our findings support the conclusion that climate change and aging populations constitute a dual challenge for future generations in terms of health burden attributed to nonoptimal temperatures. We found that population aging could have been responsible for an increase in annual mortality burden due to cold in the age group, despite the decrease in vulnerability (i.e., decrease in relative risk and mortality rates). The progressive increase in the pool of vulnerable individuals could have partially counteracted the potential benefits of the progressive adaption of the population to cold temperatures. In the case of heat, population aging could have led to an amplification of the impacts. We observe that rates slightly increased over the past 50 y, whereas the annual number of deaths is 5 times more in the recent decade among the group. No previous study has attempted to compare the contribution of both changes in vulnerability and population at risk to the historical temperature–mortality burden. If current aging trends persist in Switzerland, the pool of susceptible population at risk for extreme temperatures (i.e., elders) will double by 2060 (Lewis and Ollivaud 2020). Thus, the combination of a warming climate and population aging will likely exacerbate the impact of heat and possibly attenuate the potential decrease in cold-related deaths in future decades (Chen et al. 2020). For instance, when projection studies assumed a constant population over time, they estimated an overall net decrease (or lower increase) in temperature-related mortality burden; however, when accounting for demographic change, a larger net increase in heat- and cold-related mortality was observed (Åström et al. 2017; Chen et al. 2020; Lee et al. 2018; Lee and Kim 2016; Li et al. 2016; Liu et al. 2019; Marsha et al. 2018; Vardoulakis et al. 2014).
The observed progressive population aging we observed in Switzerland follows the current trends in developed northern regions of the globe. Thus, it is likely that the impact of population aging on historical temperature–mortality trends in these regions could be similar. However, these findings should not be directly extrapolated to these geographical locations, because other factors driving changes in vulnerability are highly heterogeneous and diverge from one place to another. Although we assessed several potential factors driving changes in vulnerability over time (e.g., percent of population above 80 y of age and population density), none of them resulted in relevance in the statistical model. However, we acknowledge that other relevant time-varying factors were not assessed due to the lack of data, such as access to air conditioning (Nordio et al. 2015; Sera et al. 2020), socioeconomic status (Ng et al. 2016; Sera et al. 2019a), or changes in land use (Murage et al. 2020; Sera et al. 2019b). Similarly, regions currently having a large proportion of young population, such as in some low- and middle-income countries, will also likely experience population aging in the future, according to current population projections (United Nations 2019). Thus, our findings suggest that the impact of population aging that we observed in past decades in Switzerland could be potentially relevant for the coming decades in these regions.
Our findings also suggest large differences in vulnerability between age groups, with populations and 65–79 y of age being more resilient to nonoptimal temperatures in comparison with the group. Considerably larger risks were found in the oldest age category for both heat and cold (Figure S8). Another proxy for vulnerability often used is the difference in MMT between age groups and over time (Achebak et al. 2019; Åström et al. 2016; Todd and Valleron 2015). First, we observed higher MMPs among the and 65–79-y-old age groups compared to category (Figure S7). This observation would suggest that the effect of heat is restricted to more extreme temperature ranges in the two younger subpopulations, whereas increased risks are already present in milder temperatures in the category. Second, MMTs increased among the -y-old and 65–79-y-old age groups in time, whereas MMPs remained constant, which would suggest resilience to the progressive shift toward warmer temperatures due to climate change. In contrast, the age group showed no signs of adaptation because the MMT has remained constant despite the increase in temperature. The trends in the -y-old and 65–79-y-old age groups are consistent with findings reported in previous literature; however, a stagnation in the MMT among the group has not been reported before (Achebak et al. 2019).
This study has several strengths. We assessed temperature–mortality trends by properly accounting for changes in the age structure of population, as reported in health impact projection studies in which different socioeconomic development pathways are compared. Previous studies estimated the overall temperature–mortality associations (i.e., across all ages) and applied them over the all-ages baseline daily mortality (Gasparrini et al. 2016; Vicedo-Cabrera et al. 2018). This approach does not take into account that temperature–mortality risks and baseline mortality (or population at risk) change in time but also between population subgroups (i.e., age groups), because of different degrees of adaptation/acclimatization and demographic changes. Additionally, this study used the state-of-the-art methodologies recently developed in climate change epidemiology, which allowed us to obtain robust estimations of impacts while accounting for complex temporal and geographical patterns in the risks. We also made use of historical high-quality daily mortality and temperature data defined at each municipality in Switzerland along almost 50 y of time. Regarding the latter, municipality-level series were derived from the combination of high-resolution temperature and population maps. As shown in a previous publication (de Schrijver et al. 2021), this methodology provides more accurate exposure series and reduced exposure misclassification, in particular for large municipalities located in rural areas with a sparse population distribution. By assessing almost 50 y of data, we were able to better capture temporal patterns and potential drivers happening at a longer time scale (i.e., adaptation and population aging).
Some limitations must be acknowledged. We could not assess temporal pattern by combinations of sex and age category due to the lack of statistical power. Although previous studies found heterogeneous trends by sex (Achebak et al. 2019), we assume that the role of population aging might have been the same in the temperature–mortality impacts for both sexes. Apart from the role of population aging, we assessed other potential time-varying factors (e.g., population density, spatial terms, and interaction terms) in the meta-analytical model, which could have partially explained the observed trends, although none of the tested variables were found to be relevant. It should be noted that other relevant factors such as air conditioning or other infrastructural measures (Sera et al. 2020) were not considered, because data was not available for the whole country at different time points. Understanding changes in the temperature vulnerability over time and its drivers is critical for projection studies and public health (Hess and Ebi 2016). Thus, future studies should aim to specifically identify those relevant factors that could help to design effective adaptation strategies in the future. We did not test for other environmental factors as potential confounders of the temperature–mortality, such as air pollution, humidity, and influenza epidemics. However, we believe that their impact would be, if present, minimal because the role of these variables as confounders remains debatable (Armstrong et al. 2019; Buckley et al. 2014; von Klot et al. 2012). Last, although we explored only trends in mortality, mortality is hypothesized to be only the tip of the iceberg with large morbidity and economic costs associated with nonoptimal temperatures; yet, underlying changes in morbidity and other societal costs have remained largely unexplored in the current literature (Wellenius et al. 2017; Wondmagegn et al. 2021).
Conclusion
In conclusion, our findings suggest that population aging could have been a relevant driver of historic trends in temperature-related mortality impacts during the last five decades in Switzerland. In particular, we found that progressive aging of the population might have attenuated the decrease in cold-related mortality expected from the warming of the climate and exacerbated the burden attributed to heat. This evidence supports the hypothesis that population aging combined with climate change is likely to further amplify the mortality burden attributed to heat and cold if no further adaptation measures are introduced, putting an additional strain on health care systems across countries with an aging population. Therefore, protecting elders from the effects of climate change could be crucial to reducing the health impacts and building populations resilient to the threatening adverse health impacts of a warming climate.
Supplementary Material
Acknowledgments
The authors would like to thank the BFS for providing data on the daily mortality in Switzerland used in this study.
E.S. has received funding from The European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement No. 801076, through the Swiss School of Public Health (SSPH) Global PhD Fellowship Programme in Public Health Sciences (GlobalP3HS) of the SSPH. A.G. has received funding from The Medical Research Council-UK (Grant ID: MR/R013349/1), The Natural Environment Research Council UK (Grant ID: NE/R009384/1), The European Union’s Horizon 2020 Project Exhaustion (Grant ID: 820655), and The Joint Research Center of the European Union (JRC/SVQ/2020/MVP/1654).
References
- Achebak H, Devolder D, Ballester J. 2019. Trends in temperature-related age-specific and sex-specific mortality from cardiovascular diseases in Spain: a national time-series analysis. Lancet Planet Health 3(7):e297–e306, PMID: , 10.1016/S2542-5196(19)30090-7. [DOI] [PubMed] [Google Scholar]
- Arbuthnott K, Hajat S, Heaviside C, Vardoulakis S. 2016. Changes in population susceptibility to heat and cold over time: assessing adaptation to climate change. Environ Health 15(suppl 1):33, PMID: , 10.1186/s12940-016-0102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong BG, Gasparrini A, Tobias A. 2014. Conditional Poisson models: a flexible alternative to conditional logistic case cross-over analysis. BMC Med Res Methodol 14(1):122, PMID: , 10.1186/1471-2288-14-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong B, Sera F, Vicedo-Cabrera AM, Abrutzky R, Åström DO, Bell ML, et al. 2019. The role of humidity in associations of high temperature with mortality: a multicountry, multicity study. Environ Health Perspect 127(9):97007, PMID: , 10.1289/EHP5430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Åström C, Åström DO, Andersson C, Ebi K, Forsberg B. 2017. Vulnerability reduction needed to maintain current burdens of heat-related mortality in a changing climate—magnitude and determinants. Int J Environ Public Health 14(7):741, PMID: , 10.3390/ijerph14070741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Åström DO, Tornevi A, Ebi KL, Rocklöv J, Forsberg B. 2016. Evolution of minimum mortality temperature in Stockholm, Sweden, 1901–2009. Environ Health Perspect 124(6):740–744, PMID: , 10.1289/ehp.1509692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, Samet JM. 2002. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev 24(2):190–202, PMID: , 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- Bobb JF, Peng RD, Bell ML, Dominici F. 2014. Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect 122(8):811–816, PMID: , 10.1289/ehp.1307392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley JP, Samet JM, Richardson DB. 2014. Commentary: does air pollution confound studies of temperature? Epidemiology 25(2):242–245, PMID: , 10.1097/EDE.0000000000000051. [DOI] [PubMed] [Google Scholar]
- Bundesamt für Statistik Statistischer Atlas der Schweiz. 2020. Räumliche Gliederungen der Schweiz/Räumliche Typologien/Gemeindetypologie 2012 mit 9 Kategorien. https://www.atlas.bfs.admin.ch/maps/13/de/12360_12482_3191_227/20593.html [accessed 12 March 2020].
- Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklöv J, Hajat S, et al. 2016. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6:258–268, PMID: , 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Vicedo-Cabrera AM, Dubrow R. 2020. Projections of ambient temperature- and air pollution-related mortality burden under combined climate change and population aging scenarios: a review. Curr Environ Health Rep 7(3):243–255, PMID: , 10.1007/s40572-020-00281-6. [DOI] [PubMed] [Google Scholar]
- Chung Y, Yang D, Gasparrini A, Vicedo-Cabrera AM, Fook Sheng Ng C, Kim Y, et al. 2018. Changing susceptibility to non-optimum temperatures in Japan, 1972–2012: the role of climate, demographic, and socioeconomic factors. Environ Health Perspect 126(5):057002, PMID: , 10.1289/EHP2546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Schrijver E, Folly CL, Schneider R, Royé D, Franco OH, Gasparrini A, et al. 2021. A comparative analysis of the temperature‐mortality risks using different weather datasets across heterogeneous regions. Geohealth 5(5):e2020GH000363, PMID: , 10.1029/2020GH000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Office of Meteorology and Climatalogy MeteoSwiss. 2020. Spatial Climate Analysis. https://www.meteoswiss.admin.ch/home/climate/swiss-climate-in-detail/raeumliche-klimaanalysen.html [accessed 5 January 2020].
- Federal Statistical Office. 2020. Swiss Official Commune Register. https://www.bfs.admin.ch/bfs/en/home/basics/swiss-official-commune-register.html [accessed 12 March 2020].
- Gasparrini A. 2011. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Soft 43(8), 10.18637/jss.v043.i08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A. 2021. The case time series design. Epidemiology 32(6):829–837, PMID: , 10.1097/EDE.0000000000001410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2010. Distributed lag non-linear models. Stat Med 29(21):2224–2234, PMID: , 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2012. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat Med 31(29):3821–3839, PMID: , 10.1002/sim.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Tobias A, Zanobetti A, et al. 2016. Changes in susceptibility to heat during the summer: a multicountry analysis. Am J Epidemiol 183(11):1027–1036, PMID: , 10.1093/aje/kwv260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. 2015a. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386(9991):369–375, PMID: , 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Kinney PL, Petkova EP, Lavigne E, et al. 2015b. Temporal variation in heat–mortality associations: a multicountry study. Environ Health Perspect 123(11):1200–1207, PMID: , 10.1289/ehp.1409070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Sera F, Vicedo-Cabrera AM, Huber V, Tong S, et al. 2017. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health 1(9):e360–e367, PMID: , 10.1016/S2542-5196(17)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Leone M. 2014. Attributable risk from distributed lag models. BMC Med Res Methodol 14(1):55, PMID: , 10.1186/1471-2288-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grize L, Huss A, Thommen O, Schindler C, Braun-Fahrländer C. 2003. Heat Wave 2003 and Mortality in Switzerland. https://m4.ti.ch/fileadmin/DSS/DSP/GOSA/documenti/smw2005-135-200-205.pdf. [DOI] [PubMed]
- Hess JJ, Ebi KL. 2016. Iterative management of heat early warning systems in a changing climate: iterative management of heat early warning systems. Ann NY Acad Sci 1382(1):21–30, PMID: , 10.1111/nyas.13258. [DOI] [PubMed] [Google Scholar]
- HSSO (Historische statistik der Schweiz). 2012. Wohnbevölkerung der Kantone nach Fünfjahresaltersklassen (annähernde Altersjahre) 1860–1870 und 1880–1990: absolute Zahlen und Prozentzahlen. https://hsso.ch/2012/b/7 [accessed 18 August 2021].
- Kim Y, Kim H, Gasparrini A, Armstrong B, Honda Y, Chung Y, et al. 2019. Suicide and ambient temperature: a multi-country multi-city study. Environ Health Perspect 127(11):117007, 10.1289/EHP4898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Lee W, Kim H, Cho Y. 2020. Social isolation and vulnerability to heatwave-related mortality in the urban elderly population: a time-series multi-community study in Korea. Environment International 142:105868, 10.1016/j.envint.2020.105868. [DOI] [PubMed] [Google Scholar]
- Lee JY, Kim H. 2016. Projection of future temperature-related mortality due to climate and demographic changes. Environ Int 94:489–494, PMID: , 10.1016/j.envint.2016.06.007. [DOI] [PubMed] [Google Scholar]
- Lee J, Kim E, Lee W-S, Chae Y, Kim H. 2018. Projection of future mortality due to temperature and population changes under representative concentration pathways and shared socioeconomic pathways. Int J Environ Public Health 15(4):822, PMID: , 10.3390/ijerph15040822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis C, Ollivaud P. 2020. Policies for Switzerland’s Ageing Society. OECD Economics Department Working Papers No. 1600. Paris, France: OECD Publishing. 10.1787/3f8a12c6-en [accessed 28 August 2020]. [DOI] [Google Scholar]
- Li T, Horton RM, Bader DA, Zhou M, Liang X, Ban J, et al. 2016. Aging will amplify the heat-related mortality risk under a changing climate: projection for the elderly in Beijing, China. Sci Rep 6(1):28161, PMID: , 10.1038/srep28161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T, Ren Z, Zhang Y, Feng B, Lin H, Xiao J, et al. 2019. Modification effects of population expansion, ageing, and adaptation on heat-related mortality risks under different climate change scenarios in Guangzhou, China. Int J Environ Public Health 16(3):376, PMID: , 10.3390/ijerph16030376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsha A, Sain SR, Heaton MJ, Monaghan AJ, Wilhelmi OV. 2018. Influences of climatic and population changes on heat-related mortality in Houston, Texas, USA. Climatic Change 146(3–4):471–485, 10.1007/s10584-016-1775-1. [DOI] [Google Scholar]
- Murage P, Kovats S, Sarran C, Taylor J, McInnes R, Hajat S. 2020. What individual and neighbourhood-level factors increase the risk of heat-related mortality? A case-crossover study of over 185,000 deaths in London using high-resolution climate datasets. Environ Int 134:105292, PMID: , 10.1016/j.envint.2019.105292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. 2020. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease study 2019. Lancet 396(10258):1223–1249, PMID: , 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Centre for Climate Services. 2018. Climate Scenarios for Switzerland: CH2018 Technical Report. Zurich, Switzerland: National Centre for Climate Services. https://www.nccs.admin.ch/nccs/en/home/climate-change-and-impacts/swiss-climate-change-scenarios/technical-report.html [accessed 5 January 2020]. [Google Scholar]
- Ng CFS, Boeckmann M, Ueda K, Zeeb H, Nitta H, Watanabe C, et al. 2016. Heat-related mortality: effect modification and adaptation in Japan from 1972 to 2010. Global Environ Change 39:234–243, 10.1016/j.gloenvcha.2016.05.006. [DOI] [Google Scholar]
- Nordio F, Zanobetti A, Colicino E, Kloog I, Schwartz J. 2015. Changing patterns of the temperature–mortality association by time and location in the US, and implications for climate change. Environ Int 81:80–86, PMID: , 10.1016/j.envint.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider A, Rückerl R, Breitner S, Wolf K, Peters A. 2017. Thermal control, weather, and aging. Curr Environ Health Rep 4(1):21–29, PMID: , 10.1007/s40572-017-0129-0. [DOI] [PubMed] [Google Scholar]
- Sera F, Armstrong B, Blangiardo M, Gasparrini A. 2019a. An extended mixed‐effects framework for meta‐analysis. Stat Med 38(29):5429–5444, PMID: , 10.1002/sim.8362. [DOI] [PubMed] [Google Scholar]
- Sera F, Armstrong B, Tobias A, Vicedo-Cabrera AM, Åström C, Bell ML, et al. 2019b. How urban characteristics affect vulnerability to heat and cold: a multi-country analysis. Int J Epidemiol 48(4):1101–1112, PMID: , 10.1093/ije/dyz008. [DOI] [PubMed] [Google Scholar]
- Sera F, Hashizume M, Honda Y, Lavigne E, Schwartz J, Zanobetti A, et al. 2020. Air conditioning and heat-related mortality: a multi-country longitudinal study. Epidemiology 31(6):779–787, PMID: , 10.1097/EDE.0000000000001241. [DOI] [PubMed] [Google Scholar]
- Sheridan SC, Allen MJ. 2018. Temporal trends in human vulnerability to excessive heat. Environ Res Lett 13(4):043001, 10.1088/1748-9326/aab214. [DOI] [Google Scholar]
- Son J-Y, Liu JC, Bell ML. 2019. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ Res Lett 14(7):073004, 10.1088/1748-9326/ab1cdb. [DOI] [Google Scholar]
- Spangler KR, Weinberger KR, Wellenius GA. 2019. Suitability of gridded climate datasets for use in environmental epidemiology. J Expo Sci Environ Epidemiol 29(6):777–789, PMID: , 10.1038/s41370-018-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suarez-Gutierrez L, Li C, Müller WA, Marotzke J. 2018. Internal variability in European summer temperatures at 1.5°C and 2°C of global warming. Environ Res Lett 13(6):064026, 10.1088/1748-9326/aaba58. [DOI] [Google Scholar]
- Suarez-Gutierrez L, Müller WA, Li C, Marotzke J. 2020. Dynamical and thermodynamical drivers of variability in European summer heat extremes. Clim Dyn 54(9–10):4351–4366, 10.1007/s00382-020-05233-2. [DOI] [Google Scholar]
- Todd N, Valleron A-J. 2015. Space–time covariation of mortality with temperature: a systematic study of deaths in France, 1968–2009. Environ Health Perspect 123(7):659–664, PMID: , 10.1289/ehp.1307771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. 2019. World Population Prospects 2019: Highlights. https://www.un.org/development/desa/publications/world-population-prospects-2019-highlights.html [accessed 6 January 2021].
- Vardoulakis S, Dear K, Hajat S, Heaviside C, Eggen B, McMichael AJ. 2014. Comparative assessment of the effects of climate change on heat- and cold-related mortality in the United Kingdom and Australia. Environ Health Perspect 122(12):1285–1292, PMID: , 10.1289/ehp.1307524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicedo-Cabrera AM, Scovronick N, Sera F, Royé D, Schneider R, Tobias A, et al. 2021. The burden of heat-related mortality attributable to recent human-induced climate change. Nat Clim Chang 11(6):492–500, PMID: , 10.1038/s41558-021-01058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicedo-Cabrera AM, Sera F, Gasparrini A. 2019. Hands-on tutorial on a modeling framework for projections of climate change impacts on health. Epidemiology 30(3):321–329, PMID: , 10.1097/EDE.0000000000000982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicedo-Cabrera Sera F, Guo Y, Chung Y, Arbuthnott K, Tong S, Tobias A, et al. 2018. A multi-country analysis on potential adaptive mechanisms to cold and heat in a changing climate. Environ Int 111:239–246, PMID: , 10.1016/j.envint.2017.11.006. [DOI] [PubMed] [Google Scholar]
- von Klot S, Zanobetti A, Schwartz J. 2012. Influenza epidemics, seasonality, and the effects of cold weather on cardiac mortality. Environ Health 11(1):74, PMID: , 10.1186/1476-069X-11-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, et al. 2021. The 2020 report of the lancet countdown on health and climate change: responding to converging crises. Lancet 397(10269):129–170, PMID: , 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellenius GA, Eliot MN, Bush KF, Holt D, Lincoln RA, Smith AE, et al. 2017. Heat-related morbidity and mortality in new England: evidence for local policy. Environ Res 156:845–853, PMID: , 10.1016/j.envres.2017.02.005. [DOI] [PubMed] [Google Scholar]
- Wondmagegn BY, Xiang J, Dear K, Williams S, Hansen A, Pisaniello D, et al. 2021. Increasing impacts of temperature on hospital admissions, length of stay, and related healthcare costs in the context of climate change in Adelaide, South Australia. Sci Total Environ 773:145656, PMID: , 10.1016/j.scitotenv.2021.145656. [DOI] [PubMed] [Google Scholar]
- Zhao Q, Guo Y, Ye T, Gasparrini A, Tong S, Overcenco A, et al. 2021. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health 5(7):e415–e425, PMID: , 10.1016/S2542-5196(21)00081-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.