Abstract
Objectives:
As the COVID-19 crisis evolves, it is important to understand COVID-19 worries and how they influence COVID-19 mitigation behaviours, especially in communities prior to case surges.
Methods:
Data related to COVID-19 impacts on life disruptions were collected from households in the Chitwan Valley Family Study, a 25-year community panel study, during February-April 2021. COVID-19 worry was measured by the extent of respondent concern for themselves or household members getting COVID-19 in the prior two weeks. Eleven items examined COVID-19 mitigation behaviours. Logistic regression models assessed associations between socio-demographic characteristics and COVID-19 worry and then the influence of worry on any mitigation behaviour and behaviour type adjusting for age, education, gender, ethnicity, and COVID-19 exposure, accounting for neighbourhood clustering.
Results:
Of 2,678 households with a responding adult, ages 18–88, 394 (14.7%) reported moderate to extreme COVID-19 worry and 1,214 (45.3%) engaged in three or more mitigation behaviours. Prevalence of mitigation behaviours was higher among those with COVID-19 worry (e.g., avoided crowds: 62.7% versus 40.5% in those with minimal worry). Respondents self-reporting COVID-19 had higher odds of worry (adjusted odds ratio [aOR]: 2.73, 95% confidence interval [CI]: 1.13, 6.57). Odds of any mitigation behaviour were higher amongst those with COVID-19 worry compared to those with minimal worry (aOR: 6.19, 95% CI=1.88, 20.35).
Conclusions:
COVID-19 mitigation behaviours were more common in people with COVID-19 worry. To address current and potential future waves of the pandemic, public health efforts should include informational campaigns about mitigation behaviours particularly for those unconcerned with COVID-19 risks.
Keywords: COVID-19, epidemiology, international health
INTRODUCTION
The COVID-19 pandemic has been ongoing for over a year now. At this phase in the pandemic, we know personal protective behaviour works, such as the use of face masks, distancing from others outside one’s household, and hand washing (1,2). In settings where people have evidence-based knowledge about COVID-19 protective strategies and access to resources, such as the use of face masks, we do not see face masks being used as widely as health professionals recommend. This is even true in communities with high case rates, due in part to differences in attitudes and beliefs (3). Evidence from high-income countries has documented variation in attitudes towards and the adoption of behaviours to reduce SARS-CoV-2 (i.e., the virus that causes COVID-19 disease (4)) transmission (5). In a high-risk sample of older adults in the United States, individuals that expressed less worry or concern about their own or their household risk of getting COVID-19 disease or other concerns about the impact of COVID-19 on disruptions to their lives (e.g., diminished access to food or medicines in stores, lifestyle disruptions) were less likely to adopt mitigation behaviours to protect themselves and their communities (6). Individual understanding of risk, which can be expressed partially through general worry about COVID-19, could help explain differential mitigation behaviour patterns. In low- and middle-income countries (LMICs), such as Nepal, relationships between COVID-19 worry and mitigation behaviours are understudied.
Nepal recorded its first COVID-19 case on January 24, 2020 and as of June 2021, has recorded estimates as high as 635,000 cases and 9,000 deaths (7). The country experienced a surge in October and November 2020, with incidence slowing in the early months of 2021, then sharply increasing in April 2021 in a major new wave of SARS-CoV-2 transmission and COVID-19 mortality. Although incidence has significantly decreased since May 2021, COVID-19 remains a significant public health threat in Nepal given low vaccination coverage and increasing prevalence of variants with greater transmissibility. The Nepalese population also has much in common with other high density Asian populations throughout South and South East Asia. Identifying responsive approaches to increasing use of effective mitigation strategies is thus a public health priority in this setting.
Beyond its direct health and mortality consequences, COVID-19 has created widespread social and economic impacts in Nepal and other LMICs, including job loss, education disruption, and food insecurity (8,9). The social and economic consequences of COVID-19 have been increasingly identified in many LMIC settings (10,11), including Nepal (12,13), but the predictors of mitigations strategies have not. Moreover, given significant disparities within Nepal in testing and case diagnosis (14) and healthcare system readiness to treat cases (15), there may also be socio-economic disparities in worry related to COVID-19 as well as in the practice of evidence-based mitigation behaviours.
Prior research has documented impacts of the COVID-19 pandemic on stress in Nepal with 76.4% of a cross-sectional convenience sample reporting feeling stressed during the early stages of the pandemic in May 2020 (16). Fear about infecting family members was high among Nepali healthcare workers in April 2020 (83.6%) (17). From April-June 2020, perceived risk of COVID-19 was high and access to protective equipment was limited among healthcare workers in Nepal (18). However, little is known about the extent of COVID-19 worry, mitigation behaviours, and concerns among the general population in Nepal. Few, if any, studies of COVID-19 in Nepal draw on population-representative, community-based samples. Moreover, prior studies have not examined COVID-19 related worry or mitigation behaviours in periods preceding COVID-19 surges, including the period just prior to the Spring 2021 surge of COVID-19 cases. Identifying prevalence of worry and mitigation behaviours prior to surge periods is critical for informing public health responses when they are needed most.
In this study, we used novel household panel survey data from the Chitwan Valley Family Study (CVFS), a general population representative sample of western Chitwan, Nepal. We aimd to characterize the experience of COVID-19 worry in the CVFS study population; assess predictors of COVID-19 worries; estimate associations between COVID-19 worry and mitigation behaviours; and then evaluate differences in types of concerns related to COVID-19 by COVID-19 worry.
METHODS
Data
We collected data from the Chitwan Valley Family Study (CVFS) sample, an ongoing multilevel panel study of social, demographic, and ecological change in Chitwan Valley of Nepal (19, 20). Launched in 1995, CVFS used a stratified cluster sample design and enrolled a representative probability sample of 151 neighborhoods (toles) with all the households within the sample neighborhoods and individuals (i.e., members of those households). Since 1997 CVFS has been tracking sample households and individual members of those households through a prospective monthly household registry system. This system is periodically refreshed to maintain representation of western Chitwan (most recently in 2015). CVFS has extraordinary cooperation from the sample households with response rates of well above 95% throughout the entire data collection period (19–21) and has complete and updated contact information of each of the sample households. Using the household contact information from the household registry, CVFS sample households were contacted via phone from February 1 to April 3, 2021 to discuss COVID-19 physical, economic, social, and education disruptions. One adult member who is knowledgeable about the household was selected to report on individual and household experiences, based on the availability of a valid phone number and participation in past CVFS data collection waves.
Interviews were conducted in tandem with ongoing household panel data collection, utilized computer assisted interviewing software, and took an average of 39 minutes to complete with a range of 20–70 minutes. Interviewers were trained and experienced staff members from the Institute for Social and Environmental Research in Nepal (ISER-N) who were familiar with CVFS study processes and protocols. From January 25–26, 2021, staff received additional study specific training in computer-assisted telephone interviewing (CATI). Interviews were conducted six days a week (Sunday-Friday), primarily in the morning. Interviewers were flexible to shift timing of interviews based on participant availability. Interviewers from ISER-N have been working with the CVFS study population communities for decades, enhancing community support and minimizing attrition over time.
To be interviewed participants had to have an active phone number. There were 40 households out of the 3,514 CVFS full sample households with no phone number during the time of the survey and another 40 with an inactive number. After excluding these 80 households, there were 3,434 households eligible from the CVFS to participate. Of these 3,434 households, there were 262 without complete interviews, specifically 208 who were unable to respond to the interview (i.e., busy or would not return calls), 41 who refused to participate, and 13 who moved out of the study’s geographic catchment area during data collection. In total, 3,172 households participated in the COVID-19 survey resulting in a 92% response rate. Of these 3,172 households, data from 2,678 households were collected during the study period (a second COVID-19 wave halted data collection activities in April 2021). These COVID-19 phone survey data were subsequently linked with prior CVFS household registry data to obtain information on demographic characteristics (e.g., gender, ethnicity). There was no item-specific missingness on any of the measures examined in this study.
This study followed both national and international ethical standards and was approved by the University of Michigan Institutional Review Board and the Nepal Health Research Council. All study participants gave verbal informed consent prior to the start of the interview.
Measures
Demographic characteristics:
Age was measured as a continuous variable (years). Education was dichotomized into passed school leaving certificate (SLC) versus did not pass SLC. SLC is awarded to those passing a national standardized test after finishing 10th grade in Nepal. Ethnicity was categorized into historically marginalized groups (Hill Janajati, Dalits, Newar, and Terai Janajati) versus historically privileged groups (Brahmin/Chhetri). Gender was measured as male or female.
COVID-19 concerns/disruptions:
Participants were asked to select all concerns from a list responding to the question “What do you think are the most important concerns for your household under the current circumstances?” COVID-19 concerns included shortage of food/increase in food prices, shortage of medicine/disruption in health services, disruption of schooling, getting sick, lack of work/disruption of livelihood, travel restrictions, other concerns, or no concerns. Concerns were summarized by total count: 0, 1, 2, 3 or more concerns.
COVID-19 prevalence:
Respondents self-reported whether they or anyone in their household had COVID-19 to their knowledge (yes/no).
COVID-19 worry:
Worrying about COVID-19 was measured by the following question “During the past two weeks, how worried have you been about being infected or someone in your household being infected with COVID-19?” Extent of respondent COVID-19 worry was categorized into not at all/slightly versus moderately/very/extremely.
COVID-19 mitigation behaviours:
Eleven items examined COVID-19 mitigation behaviours occurring during the prior two weeks: avoided crowded places, avoided public places, kept distance from others outside of one’s household (2 meters), used hand sanitizer, wore a face mask when going out and unable to physically distance (2 meters), wore gloves when going out and unable to physically distance (2 meters), wore a face shield when going out and unable to physically distance (2 meters), changed school or work arrangements, isolated from someone who had symptoms, or isolated from someone who did not have symptoms. Mitigation behaviours were summarized by total count: 0, 1, 2, or 3 or more behaviours. Mitigation behaviours were collapsed into the following seven categories (yes/no): avoided crowded/public places, kept distance from others, used hand sanitizer, wore face mask, wore gloves/face shield, work/school mitigation, and isolation measures.
Statistical Analyses
Descriptive statistics explored the prevalence of socio-demographic characteristics overall and by COVID-19 worry (moderately/very/extremely versus not at all/slightly). Patterning of responses to mitigation behaviours were explored with matrix cross-tabulations. Logistic regression models estimated characteristics associated with COVID-19 worry accounting for neighbourhood clustering. A series of logistic regression models assessed the relationship between COVID-19 worry and any COVID-19 mitigation behaviour (yes/no), then respondent endorsement of the seven specific types of mitigation practices as outcomes adjusting for age, education, gender, ethnicity, and COVID-19 exposure (respondent themselves and someone in their household, respectively) and accounting for clustering at the neighbourhood-level. Prevalence of COVID-19 type of concerns were explored overall and by COVID-19 worry, estimating differences by COVID-19 worry with independent t-tests and indicating significant differences at p < 0.05. Data were analysed in Stata 15.
RESULTS
Of the 2,678 CVFS respondents included in this analysis, 394 (14.71%) reported COVID-19 worry. The average age was 40.58 years, 30.99% reported less than SLC education, 43.76% reported being from historically privileged ethnic groups, and 34.06% were male. Among all respondents, 3.92% self-reported having COVID-19 themselves or someone in their household having COVID-19 prior to the time of the survey (Table 1). Socio-demographic characteristics were similar among those with and without COVID-19 worry (e.g., 32.99% male among those with COVID-19 worry versus 34.24% male among those without worry). Prevalence of all mitigation behaviours measured was higher among those with COVID-19 worry versus those without (e.g., avoided crowded/public places: 65.48% versus 43.04%, respectively). In the overall sample, 45.33% reported three or more COVID-19 mitigation behaviours and the prevalence was higher among those with COVID-19 worry (65.48% versus 41.86% in those without COVID-19 worry). Using hand sanitizer and wearing a mask (24.12%) was a frequently reported combination of mitigation behaviours, while wearing a mask without any additional mitigation behaviours was also common (17.14%, data not shown). Among those without COVID-19 worry, 19.26% reported wearing a mask as their only mitigation behaviour versus 4.82% with COVID-19 worry. Those with COVID-19 worry more commonly reported all of the following behaviours: avoiding crowded public spaces, distancing from others, using hand sanitizer, and wearing masks (23.35%) versus those without worry (11.12%).
Table 1:
Socio-demographic characteristics and COVID-19 concerns/mitigation behaviour measures, Nepal Chitwan Valley Family Study COVID-19 Survey 2021
| Characteristics | Overall N=2,678 N (column %) |
COVID-19 Worry N=394 N (column %) |
No COVID-19 Worry N=2,284 N (column %) |
|---|---|---|---|
| Age, mean (SD) | 40.58 (12.99) | 41.36 (12.96) | 40.47 (12.99) |
| Age group | |||
| 15–24 | 235 (8.78) | 32 (8.12) | 203 (8.89) |
| 25–34 | 705 (26.33) | 99 (25.13) | 606 (26.53) |
| 35–44 | 855 (31.93) | 117 (29.70) | 738 (32.31) |
| 45–54 | 482 (18.00) | 83 (21.07) | 399 (17.47) |
| 55+ | 401 (14.97) | 63 (15.99) | 338 (14.80) |
| Educationa | |||
| SLC pass | 1848 (69.01) | 277 (70.30) | 1571 (68.78) |
| <SLC | 830 (30.99) | 117 (29.70) | 713 (31.22) |
| Ethnicityb | |||
| Historically privileged groups | 1172 (43.76) | 153 (38.83) | 1019 (44.61) |
| Historically marginalized groups | 1506 (56.24) | 241 (61.17) | 1265 (55.39) |
| Gender | |||
| Female | 1766 (65.94) | 264 (67.01) | 1502 (65.76) |
| Male | 912 (34.06) | 130 (32.99) | 782 (34.24) |
| COVID-19 exposure | |||
| Respondent or household had COVID-19 | 105 (3.92) | 22 (5.58) | 83 (3.63) |
| Respondent had COVID-19 | 34 (1.27) | 11 (2.79) | 23 (1.01) |
| Someone in household had COVID-19 | 90 (3.36) | 18 (4.57) | 72 (3.15) |
| COVID-19 mitigation behavioursb | |||
| Avoid crowded places | 1172 (43.76%) | 247 (62.69%) | 925 (40.50%) |
| Avoid public places | 966 (36.07%) | 219 (55.58%) | 747 (32.71%) |
| Physical distance outside household | 571 (21.32%) | 160 (40.61%) | 411 (17.99%) |
| Used hand sanitizer | 1,685 (62.92%) | 309 (78.43%) | 1376 (60.25%) |
| Wore a face maskc | 2,392 (89.32%) | 369 (93.65%) | 2,023 (88.57%) |
| Wore glovesc | 150 (5.60%) | 40 (10.15%) | 110 (4.82%) |
| Wore a face shieldc | 23 (0.86%) | 5 (1.27%) | 18 (0.79%) |
| Changed school or work arrangements | 143 (5.34%) | 35 (8.88%) | 108 (4.73%) |
| Isolated someone with symptoms | 11 (0.41%) | 4 (1.02%) | 7 (0.31%) |
| Isolated someone even without symptoms | 7 (0.26%) | 2 (0.51%) | 5 (0.22%) |
| COVID-19 mitigation behaviours, categorizedd | |||
| Avoid crowded/public places | 1241 (46.34) | 258 (65.48) | 983 (43.04) |
| Kept distance from others | 571 (21.32) | 160 (40.61) | 411 (17.99) |
| Used hand sanitizer | 1685 (62.92) | 309 (78.43) | 1376 (60.25) |
| Wore face mask | 2392 (89.32) | 369 (93.65) | 2023 (88.57) |
| Wore gloves/face shield | 161 (6.01) | 44 (11.17) | 117 (5.12) |
| School/work mitigations | 143 (5.34) | 35 (8.88) | 108 (4.73) |
| Isolation measures | 15 (0.56) | 5 (1.27) | 10 (0.44) |
| COVID-19 mitigation behaviours, counte | |||
| 0 | 136 (5.08) | 4 (1.02) | 132 (5.78) |
| 1 | 536 (20.01) | 32 (8.12) | 504 (22.07) |
| 2 | 792 (29.57) | 100 (25.38) | 692 (30.30) |
| 3+ | 1214 (45.33) | 258 (65.48) | 956 (41.86) |
SLC= school leaving certificate (i.e., awarded to those passing a national standardized test after finishing 10th grade in Nepal).
Ethnicity categorized as historically privileged (Brahmin/Chhetri), as compared to historically marginalized (Hill Janjati, Dalits, Newar, and Terai Janjati).
These behaviours were specifically when going out and unable to physically distance (2 meters).
Indicates respondents could select more than one mitigation behaviour and thus estimates do not all sum to 100%.
Counts were based on individual mitigation behaviour items and not broader categorized groups.
Select socio-demographic and COVID-19 exposure variables were associated with COVID-19 worry (Table 2). Respondents who self-reported ever having COVID-19 themselves reported higher odds of COVID-19 worry compared with those who did not have COVID-19 (adjusted odds ratio [aOR]= 2.73, 95% confidence interval [CI]= 1.13, 6.57), whereas reporting that anyone in a respondent’s household other than themselves had COVID-19 was not associated with significantly higher odds of COVID-19 worry after accounting for other characteristics (aOR= 1.17, 95% CI= 0.68, 2.01). Historically marginalized ethnic groups had 1.37 times the odds of COVID-19 worry (95% CI= 1.03, 1.83) compared with historically privileged ethnic groups.
Table 2:
Associations between characteristics and COVID-19 worry, Nepal Chitwan Valley Family Study COVID-19 Survey 2021 (N=2,678)
| Characteristics | COVID-19 Worry | |
|---|---|---|
|
| ||
| uOR (95% CI) | aOR (95% CI) | |
|
|
||
| Age (continuous) | 1.00 (1.00, 1.01) | 1.01 (1.00, 1.02) |
| Gender (ref: male) | ||
| Female | 1.06 (0.84, 1.33) | 1.13 (0.88, 1.44) |
| Ethnicitya (ref: historically privileged groups) | ||
| Historically marginalized groups | 1.27 (0.96, 1.68) | 1.37 (1.03, 1.83) |
| Educationb (ref: SLC pass) | ||
| No SLC pass | 0.93 (0.73, 1.19) | 1.05 (0.82, 1.37) |
| Respondent had COVID-19 (ref: no COVID-19) | 2.82 (1.31, 6.07) | 2.73 (1.13, 6.57) |
| Someone in respondent’s household had COVID-19 (ref: no COVID-19) | 1.47 (0.91, 2.38) | 1.17 (0.68, 2.01) |
uOR= unadjusted odds ratio; aOR= adjusted odds ratio; CI= confidence interval.
Ethnicity categorized as historically privileged (Brahmin/Chhetri), as compared to historically marginalized (other ethnicities Hill Janjati, Dalits, Newar, and Terai Janjati).
SLC= school leaving certificate (i.e., awarded to those passing a national standardized test after finishing 10th grade in Nepal). All models adjusted for age, education, gender, ethnicity, and COVID-19 exposure (respondent themselves and someone in their household, respectively). Models accounted for neighbourhood-level clustering. Bold values indicate significant at p < 0.05.
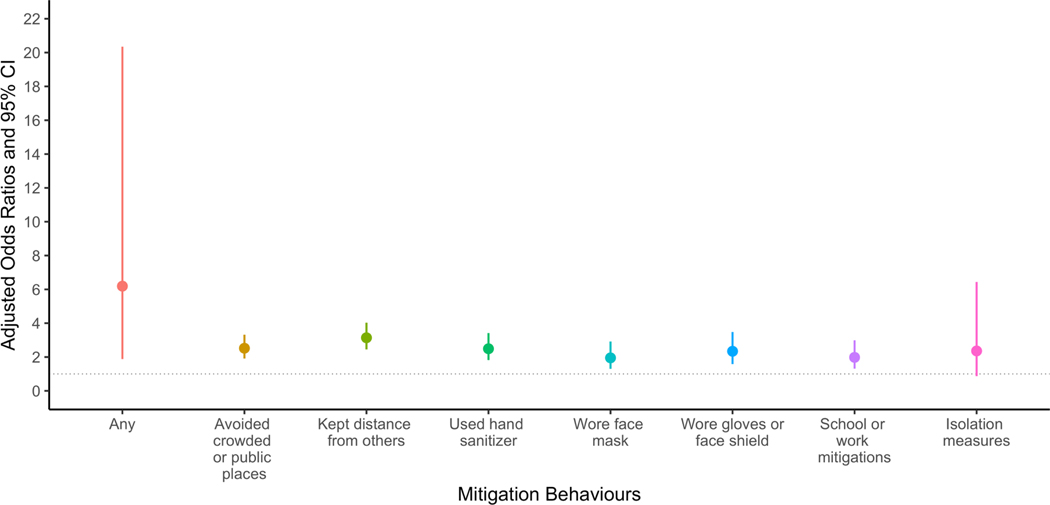
COVID-19 worry was associated with any COVID-19 mitigation behaviour (aOR=6.19, 95% CI=1.88, 20.35) after accounting for socio-demographic and COVID-19 characteristics (Figure 1). COVID-19 worry was associated with keeping distance from others (aOR=3.14, 95% CI=2.45, 4.03), avoiding crowded public spaces (aOR=2.52, 95% CI=1.91, 3.32), using hand sanitizer (aOR=2.49, 95% CI=1.82, 3.42), school/work mitigation practices (aOR=1.98, 95% CI=1.31, 2.99), wearing gloves or a face shield (aOR=2.34, 95% CI=1.58, 3.48), and wearing a face mask (aOR=1.95, 95% CI=1.30, 2.92).
Figure 1:
COVID-19 Mitigation Behaviours Association with COVID-19-related Worry, Nepal Chitwan Valley Family Study COVID-19 Survey 2021(N=2,678)
All models adjusted for age, education, gender, ethnicity, and COVID-19 exposure (respondent themselves and someone in their household, respectively). Models accounted for neighbourhood-level clustering. Respondents could endorse more than one mitigation behaviour.
To contextualize findings and understand which domains worry pertained to, types of COVID-19-related concerns were explored descriptively overall and by COVID-19 worry (Figure 2). The main concerns respondents had regarded education (20.69%), food availability/security (18.19%), and employment (10.75%). A higher prevalence of people without COVID-19 worry reported no concerns (60.99%), compared to people with COVID-19 worry (39.34%). Those with COVID-19 worry were more likely to report more concerns (e.g., 22.84% reported two concerns), compared with those without COVID-19 worry (13.09% reported two concerns).
Figure 2:
Type of COVID-19 concerns by COVID-19 worry, Nepal Chitwan Valley Family Study COVID-19 Survey 2021(N=2,678)
*Indicates significant difference between those with and without COVID-19 worry at p < 0.05. Respondents could select more than one type of COVID-19 concern. Overall N=2,678, COVID-19 worry n=394, and no COVID-19 worry n=2,284. Medical concerns pertained to shortage of medicine/disruption in health services, whereas sick concerns pertained to getting sick.
DISCUSSION
Our study explores COVID-19 worry and mitigation behaviours during the period immediately before Nepal’s second COVID-19 surge in April 2021. Before this second wave in Nepal, most of the participants were not worried about COVID-19. If they were worried, respondents generally worried about potential disruptions to food and education. Individual participants who reported having COVID-19 themselves had a higher likelihood of COVID-19 worry compared with participants who reported that another household member had COVID-19. A large proportion of the population reported mask and hand sanitizer usage; however, other mitigation behaviours, such as avoiding crowded and public places, were not often employed. Those who were more worried about COVID-19 employed more mitigation behaviours.
This study provides further evidence around the relationship between worry and behaviour change activities related to COVID-19. With a six-fold increase in adoption of any COVID-19 protective behaviours, those who were worried about COVID-19 before the most recent surge adopted more protective measures. In LMIC settings, such as Nepal, those with fewer socio-economic resources, such as those without complete secondary school education, are often unable to adopt personal protective strategies (11). Individuals in these groups frequently lack sufficient financial resources or income generating activities that would allow them to stay home if sick or avoid public and crowded environments (22). Structural barriers (e.g., economic, housing) that inhibit individuals from adopting risk mitigation behaviours could contribute to increased worry in historically marginalized ethnic groups, similar to findings from underserved and marginalized communities in other settings (11,23). Thus, increased worry could function as an imprecise approximation of increased risk of COVID-19, and an inability to adopt all risk mitigating behaviours could contribute to increased worry (e.g., cannot avoid crowds because of jobs). Future studies should explore relationships between existing behaviours, behavioural intent, and ideal behaviours if barriers were removed, to better understand the factors predicting risk mitigation behaviours in order to provide the means for improved preventive messaging and risk mitigation uptake.
Distinguishing between COVID-19-specific worry and general worry that may be associated with anxiety is potentially useful. COVID-19 worry as a construct can reflect knowledge and understanding of community risk. Too little worry can translate into lack of mitigation behaviours, as our study demonstrated, similar to research from settings in high-income countries (6). When worry is high, it can become maladaptive and develop into anxiety and/or depressive symptoms and disorders for a subset of the population (24). Extensive research has identified negative mental health consequences of the pandemic on populations throughout the world (25). Specifically in Nepal, mental health consequences have been documented in healthcare worker populations (26,27) and the general population (28,29). Future research should assess the development of psychiatric symptoms and disorders in individuals with very high COVID-19 worry.
This study provides additional evidence that individual COVID-19 protective behaviours vary. This underscores the importance of understanding and communicating personal risk to motivate behaviour change. When individual risk is perceived to be higher and mitigation strategies are considered effective, this can translate into increased behaviour change (30,31). Given inequality in ability to employ individual-based protective measures, increased locally-informed and population-based wide-scale vaccine and education campaigns are essential to increasing capacity for enhancing such behaviours in low-resource settings (32). Additionally, a combination of government policies to protect the most vulnerable, global support to increase access to key resources (i.e., protective equipment, testing, and vaccines), and targeted informational campaigns are essential to manage and prevent future COVID-19 outbreaks in LMIC.
COVID-19 protective behaviours should be contextualized within the public health guidelines at the time. By creating a COVID-19 Crisis Management Committee (CCMC) at the national level, Nepal responded COVID-19 pandemic in a well-coordinated manner. The CCMC was composed of several government ministries (e.g., Ministry of Health) and led by the deputy prime minister who was primarily responsible to monitor pandemic situation, develop the plan of action, and provide directives to local government agencies. The local governments were the responsible for monitoring the pandemic situation locally, adopting CCMC directives or developing and implementing local guidelines based on local pandemic situation. In general, these guidelines were reviewed and new directives were provided in a biweekly basis. As our study area lies in Chitwan district these guidelines were issued, enforced and monitored by the Chitwan District Administration Office through the district COVID-19 crisis management coordination committee. The CVFS COVID-19 survey was conducted in Nepal in early 2021 between the first and second waves. There were some public health guidelines in place, but there was not a complete lock down. In March 2020 lock downs began in Nepal including the closing of schools and limiting of large gatherings and these guidelines were loosened in July 2020 (33). While the public administration was primarily focused on the enforcement of the lock down (closing and stay home); public health communities were focused on raising awareness about COVID-19 risk factors, symptoms, and best practices for mitigating the risk and seeking treatment through various modes, including radio, television, and by phone (33). COVID-19 protective behaviours could have changed from the start of the pandemic as risk was communicated to be lower compared with spring of 2020. This survey was conducted months after the initial strict public health measures were lifted and before cases began rising again.
Our study has many strengths, including timely data on COVID-19 disruptions from a LMIC immediately before a major COVID-19 surge among a population-representative sample rather than a convenience sample, on which most studies on COVID-19 worry have relied (8,24). Our study has limitations worth noting as well. We did not have data on COVID-19 test results and relied on self-report. Given that COVID-19 testing access is low (34), self-reported estimates of having COVID-19 are likely under-estimates. Our study did not examine psychiatric symptoms or disorders, but rather assessed worry as a broader construct. Future studies should examine the relationship between COVID-19 worry and development of psychiatric disorders in Nepal. As a cross-sectional study, our study is not able to determine whether COVID-19 worry preceded mitigation behaviours or vice versa. Given that those with higher levels of worry reported increased preventive measure usage, it is possible that increased worry leads to increased behaviour adoption, that increased behaviour adoption leads to increased worry, or that the two increase together. Future research should focus on household relationships, how they may have changed during the pandemic, and their influence on COVID-19 worry, as a household member having COVID-19 appeared to influence worry less than a respondent having COVID-19 themselves.
CONCLUSION
This study provides unique insight into a region in Nepal immediately preceding a COVID-19 surge, and the general mitigation strategies commonly employed. Public health messaging and informational campaigns should focus on individualizing messages so that the apparent risk within a community is better understood, as an individual’s COVID-19 concern is strongly associated with their protective behaviours.
ACKNOWLEDGEMENTS
The authors thank the survey staff of the Institute for Social and Environmental Research–Nepal for collecting the data reported here; the staff of the Survey Research Operations unit of the University of Michigan’s Survey Research Center for development and support of the technical systems that made the fieldwork in Nepal possible; and the respondents of the CVFS, whose generous contributions made this research possible. The authors thank Erika Arias for her copyediting support. The authors alone remain responsible for any errors or omissions in this manuscript. This work was supported by the National Institute of Mental Health (R01MH110872) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development funded Population Dynamics and Health Program Pilot Project Seed Grant (P2CHD041028). The sponsors played no direct role in study design, data collection, analysis, interpretation, manuscript preparation, or the decision to submit the paper for publication. Dr. Ghimire is the Director of the Institute for Social and Environmental Research Nepal (ISER-N) in Nepal that collected the data for the research reported here. Dr. Ghimire’s conflict of interest management plan is approved and monitored by the Regents of the University of Michigan.
References
- 1.Hutchins HJ. COVID-19 Mitigation Behaviors by Age Group — United States, April–June 2020. MMWR Morb Mortal Wkly Rep [Internet]. 2020. [cited 2021 Jul 18];69. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6943e4.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, van der Westhuizen H-M, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci [Internet]. 2021. Jan 26 [cited 2021 Jul 18];118(4). Available from: https://www.pnas.org/content/118/4/e2014564118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Timpka T, Nyce JM. Face mask use during the COVID-19 pandemic—the significance of culture and the symbolic meaning of behavior. Ann Epidemiol. 2021. Jul 1;59:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.V’kovski P, Kratzel A, Steiner S, Stalder H, Thiel V. Coronavirus biology and replication: implications for SARS-CoV-2. Nat Rev Microbiol. 2021. Mar;19(3):155–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benham JL, Lang R, Burns KK, MacKean G, Léveillé T, McCormack B, et al. Attitudes, current behaviours and barriers to public health measures that reduce COVID-19 transmission: A qualitative study to inform public health messaging. PLOS ONE. 2021. Feb 19;16(2):e0246941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barber SJ, Kim H. COVID-19 Worries and Behavior Changes in Older and Younger Men and Women. J Gerontol B Psychol Sci Soc Sci. 2021. Jan 18;76(2):e17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020. May 1;20(5):533–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh DR, Sunuwar DR, Adhikari B, Szabo S, Padmadas SS. The perils of COVID-19 in Nepal: Implications for population health and nutritional status. J Glob Health. 2020. Jun;10(1):010378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thapa P. Building Back Better (BBB) from COVID-19 [Internet]. Kathmandu, Nepal: World Vision Nepal; 2020. May p. 16. Available from: https://www.wvi.org/publications/policy-briefing/nepal/building-back-better-covid-19 [Google Scholar]
- 10.Rohwerder B. Social Impacts and Responses Related to COVID-19 in Low- and Middle-income Countries. 2020. Jul [cited 2021 Jul 7]; Available from: https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/15625 [Google Scholar]
- 11.Coetzee BJ, Kagee A. Structural barriers to adhering to health behaviours in the context of the COVID-19 crisis: Considerations for low- and middle-income countries. Glob Public Health. 2020. Aug;15(8):1093–102. [DOI] [PubMed] [Google Scholar]
- 12.Bhatt N, Bhatt B, Gurung S, Dahal S, Jaishi AR, Neupane B, et al. Perceptions and experiences of the public regarding the COVID-19 pandemic in Nepal: a qualitative study using phenomenological analysis. BMJ Open. 2020. Dec 1;10(12):e043312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poudel K, Subedi P. Impact of COVID-19 pandemic on socioeconomic and mental health aspects in Nepal. Int J Soc Psychiatry. 2020. Dec 1;66(8):748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma K, Banstola A, Parajuli RR. Assessment of COVID-19 Pandemic in Nepal: A Lockdown Scenario Analysis. Front Public Health. 2021. Apr 8;9:599280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhattarai S, Dhungana J, Ensor T, Shrestha UB. Assessment of service availability and Infection prevention measures in hospitals of Nepal during the transition phase of COVID-19 case surge. medRxiv. 2020. May 19;2020.05.13.20097675. [Google Scholar]
- 16.Kandel S, Lamsal M, Yadav SA, Bhandari D, Adhikari G, Poudel S, et al. Lifestyle, behavior, perception and practices of Nepalese during lockdown due to COVID-19 pandemic. JNMA J Nepal Med Assoc. 2020. Sep;58(229):690–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajbhandari P, Maharjan K. Willingness of emergency and medicine department doctors to work during surge of COVID-19 patients, Patan Hospital, Nepal. J Patan Acad Health Sci. 2020. Apr 30;7(1):25–30. [Google Scholar]
- 18.Sharma B, Shrestha N, Gurung N, Banstola S. Perceived risk, preventive behavior and enabling environment among health workers during COVID-19 pandemic in Nepal: an Online Survey. J Gandaki Med Coll-Nepal [Internet]. 2020. Nov 6 [cited 2021 Jul 7]; Available from: https://www.nepjol.info/index.php/JGMCN/article/view/31166 [Google Scholar]
- 19.Thornton A, Ghimire D, Young-DeMarco L, Bhandari P. The Reliability and Stability of Measures of Individuals’ Values and Beliefs Concerning Developmental Idealism in Nepal. Sociol Dev. 2019. Sep 1;5(3):314–36. [Google Scholar]
- 20.Axinn WG, Ghimire D, Williams NE. Collecting Survey Data during Armed Conflict. J Off Stat. 2012. Jun;28(2):153–71. [PMC free article] [PubMed] [Google Scholar]
- 21.Ghimire DJ, Williams NE, Thornton A, Young-DeMarco L, Bhandari P. Strategies for origin-based surveying of international migrants. J Ethn Migr Stud. 2019. May 19;45(7):1185–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soleimanvandi NA, Irandoost SF, Ahmadi S, Xosravi T, Ranjbar H, Mansourian M, et al. Explaining the reasons for not maintaining the health guidelines to prevent COVID-19 in high-risk jobs: a qualitative study in Iran. BMC Public Health. 2021. May 3;21(1):848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Papageorge NW, Zahn MV, Belot M, van den Broek-Altenburg E, Choi S, Jamison JC, et al. Socio-demographic factors associated with self-protecting behavior during the Covid-19 pandemic. J Popul Econ. 2021. Apr 1;34(2):691–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020. Dec 1;277:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lange KW. Coronavirus disease 2019 (COVID-19) and global mental health. Glob Health J Amst Neth. 2021. Mar;5(1):31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob Health. 2020. Sep 25;16(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta AK, Mehra A, Niraula A, Kafle K, Deo SP, Singh B, et al. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID-19 pandemic. Asian J Psychiatry. 2020. Dec;54:102260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta AK, Sahoo S, Mehra A, Grover S. Psychological impact of ‘Lockdown’ due to COVID-19 pandemic in Nepal: An online survey. Asian J Psychiatry. 2020. Dec;54:102243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sigdel A, Bista A, Bhattarai N, Pun BC, Giri G, Marqusee H, et al. Depression, Anxiety and Depression-anxiety comorbidity amid COVID-19 Pandemic: An online survey conducted during lockdown in Nepal. medRxiv. 2020. May 6;2020.04.30.20086926. [Google Scholar]
- 30.Dryhurst S, Schneider CR, Kerr J, Freeman ALJ, Recchia G, Bles AM van der, et al. Risk perceptions of COVID-19 around the world. J Risk Res. 2020. Aug 2;23(7–8):994–1006. [Google Scholar]
- 31.Bruine de Bruin W, Bennett D. Relationships Between Initial COVID-19 Risk Perceptions and Protective Health Behaviors: A National Survey. Am J Prev Med. 2020. Aug;59(2):157–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kusuma D, Pradeepa R, Khawaja KI, Hasan M, Siddiqui S, Mahmood S, et al. Low uptake of COVID-19 prevention behaviours and high socioeconomic impact of lockdown measures in South Asia: Evidence from a large-scale multi-country surveillance programme. SSM - Popul Health. 2021. Feb 13;13:100751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Responding to COVID-19, Health sector preparedness, response and lessons learnt.pdf [Internet]. [cited 2021 Nov 21]. Available from: https://mohp.gov.np/attachments/article/703/Responding%20to%20COVID-19,%20Health%20sector%20preparedness,%20response%20and%20lessons%20learnt.pdf
- 34.Giri AK, Rana DR. Charting the challenges behind the testing of COVID-19 in developing countries: Nepal as a case study. Biosaf Health. 2020. Jun 1;2(2):53–6. [DOI] [PMC free article] [PubMed] [Google Scholar]