Abstract
Background:
Persulfate is an oxidizing agent used for multiple purposes, including bleaching hair, bleaching flour, and as pool/spa water disinfectant.
Objective:
To identify the prevalence and clinical characteristics of patients allergic to ammonium persulfate (APS) among patients who underwent patch testing in our clinic.
Methods:
A retrospective chart review of 2138 patients who underwent patch testing at Brigham and Women's hospital in Boston between July 2015 to November 2019. All patients were tested to our standard series including APS 2.5% petrolatum. Given the irritant nature of APS, we included for analysis only patients with 2+ or 3+ reactions.
Results:
Among 2138 patients, 61 (2.85%) had 2+ or 3+ reactions to APS. In this study, 72% were female. 75% had an atopic diathesis; 56% had 2+ reactions, and 44% had 3+ reactions. Clinical relevance was definite in 11%, probable in 10%, and unknown/possible in 79%. In patients with definite clinical relevance, 6/7 had occupational allergic contact dermatitis: 4 hairdressers, 1 hair salon cleaner, and 1 aquarium worker; 1/7 was bleaching her hair.
Conclusion:
Prevalence of 2+ or 3+ APS reactions in this single-center study was higher than that reported by the North American Contact Dermatitis Group, 2015–2016, (0.75% vs. 2.85% in our study). APS is an important occupational allergen, and clinicians should be aware of this when treating patients with exposure to APS.
KEY WORDS: Allergic dermatitis, ammonium persulfate, contact dermatitis, persulfate
Introduction
Ammonium persulfate (APS) is a white crystalline solid. It is a strong oxidizing agent used as a bleaching agent to bleach hair and flour.[1] Potassium peroxymonosulfate (PPMS) is commonly used as a water disinfectant. APS and PPMS are structurally related and likely cross-react with each other. Persulfate salts are considered strong sensitizers and can cause both delayed-type and immediate-type skin reactions.[2] Gilligan et al.[3] reported 6 patients diagnosed with widespread allergic contact dermatitis due to potassium peroxymonosulfate (PPMS) used as a shock treatment in hot tubs. Five out of these six patients had positive patch test reactions to both PPMS and APS, which most likely indicates cross-reactivity between these related compounds.[3] There were two other cases reported with allergic contact dermatitis to potassium persulfate after spa treatment with evidence of cross-reaction with ammonium persulfate (APS) in one of them.[4,5] Kanerva and colleagues reported a case of occupational allergic dermatitis to potassium persulfate in a water quality laboratory technician.[6] Veien N et al.[7] reported a case of allergic contact dermatitis in a patient who was exposed to potassium persulfate while working in a potato-flour factory with positive patch test to both potassium persulfate and ammonium persulfate.
The North American Contact Dermatitis Group (NACDG), 2015–2016 reported 97 out of 5594 patients (1.7%) allergic to persulfate, with one patient (1%) as having definite clinical relevance.[8] We sought to analyze persulfate reactions in our single center over a 51-month period.
Methods
A retrospective chart review was conducted in 2138 consecutive patients patch-tested for suspected allergic contact dermatitis in our contact dermatitis clinic at Brigham and Women's hospital in Boston between July 2015 and November 2019. This study was approved by the Brigham and Women's Hospital Institutional Review Board (no. 2016P000718). All patients were patch-tested to a modified American Contact Dermatitis Society core “standard” series, as well as additional series based on the clinical history and physical examination. Our standard series included APS at 2.5% in petrolatum (Chemotechnique MB Diagnostics AB, Vellinge, Sweden). Allergens were tested in Finn Chambers (SmartPractice, Phoenix, AZ.) At 48 hours, patches were removed and patients were evaluated for an initial reading. Final readings were performed from 72 hours to 168 hours after placement. Given the irritant nature of APS, we included for analysis only patients with 2+ (strong reactions; edematous papules and/or vesicles within the disc site) or 3+ (extreme reactions; coalescing vesicles, bullous, or extreme reactions spreading beyond the disc site) reactions. Clinical relevance for APS reactions was designated as definite (definite exposure and clinical signs and symptoms consistent with exposure), probable (exposure to ammonium persulfate but with no direct causation established), possible/unknown (no known exposure to allergen, or possible exposure to allergen but distribution of dermatitis or clinical symptoms not consistent with APS as the causative agent). The ethics committee was approved and I listed the IRB number (no. 2016P000718) and the date was August 10,2019.
Results
Among 2138 patients, 61 (2.85%) had 2+ or 3+ reactions to APS. Here, 44 (72%) patients were females, and 17 (28%) were males; 34 out of 61 patients (56%) had 2+ reaction, and 27 (44%) had 3+ reaction. The average age was 50 years. 75% of patients had an atopic diathesis. Clinical relevance was determined to be definite in 11% of patients, probable in 10%, and possible/unknown in 79%.
For patients with definite clinical relevance, the most common locations affected were hands (40%), followed by upper extremities (20%), scattered generalized (20%), face (10%), and eyelids (10%) [Diagram 1]. Polysensitization (3 or > distinct positive allergic reactions) was seen in 77% of patients with definite and probable clinical relevance, while 79% of patients with possible/unknown relevance showed polysensitization [Table 1].
Diagram 1.
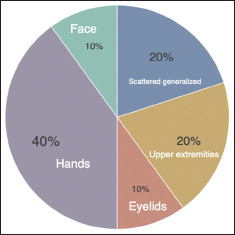
Location of rash in patients with definite clinical relevance
Table 1.
Clinical characteristics of patients allergic to ammonium persulfate with definite clinical relevance
| Occupation | Polysensitization | Clinical Relevance | Location of rash | Type I symptoms |
|---|---|---|---|---|
| Hairdresser | No | Definite; exposed to hair bleach | face, arms, legs, chest, and back generalized | +SOB |
| Administrative assistant | Yes | Definite; gets hair bleached and also scalp itches | Under eyes | No respiratory symptoms |
| Hairdresser-Part time | Yes | Definite; exposed to hair bleach | Face and hands | No respiratory symptoms |
| Hairdresser | Yes | Definite; exposed to and uses persulfate | Hands, upper and lower extremities, back generalized | +Rhinorrea, No SOB |
| Aquarium worker | Yes | Definite; exposed to potassium peroxomonosulfate in disinfectant at work | Arms and hands; Recall phenomenon after patch test | No respiratory symptoms |
| Hairdresser | No | Definite; Gets cough and throat symptoms when she uses persulfate | Hands and forearms | + respiratory symptoms (cough) and throat irritation |
| Hair salon cleaner | Yes | Definite; gets hand itching as soon as he enters the salon | Started on hands then spread | No respiratory symptoms |
SOB=Shortness of breath
History of childhood eczema was reported in 33% of patients with possible/unknown clinical relevance compared to 23% in patients with definite and probable relevance. This was not statistically significant (P-value = 0.73, Fisher's exact test, two-tailed).
All patients were questioned about the history of type 1 immediate hypersensitivity symptoms (cough, shortness of breath, rhinorrhea, or throat irritation), but prick testing was not done as our main focus was on the delayed-type hypersensitivity to APS.
Type 1 immediate hypersensitivity symptoms were seen in 31% of patients with probable and definite relevance and in 17% of patients with possible/unknown clinical relevance [Table 1]. This was also not statistically significant (P-value = 0.71, Fisher's exact test, two-tailed). It is possible that statistical significance was not reached due to the small sample size.
Discussion
APS is known to cause immediate and delayed-type hypersensitivity reactions.[9,10] Piapan et al.[11] investigated sensitization in hairdressers from north-eastern Italy, who were patch-tested with a hairdressing series (n = 140). Sensitization to APS was seen in 13.6% of hairdressers testing positive. In our cohort of patients with 2+ and 3+ reactions to APS, 4 (6.6%) were hairdressers and all of them had reactions of definite clinical relevance. Of those with definite clinical relevance, 6/7 (86%) were occupational. Of the occupations, (4/6) 66.7% were hairdressers, 1/6 was a salon cleaner, and 1/6 was an aquarium worker; 3/4 (75%) of hairdressers had immediate hypersensitivity symptoms such as cough, shortness of breath, rhinorrhea, or throat irritation [Table 1].
The NACDG patch test study in 2015–2016[8] reported total positive reactions to APS of 97 out of 5594 patients with 42 patients (0.75%) having 2+/3+ allergic reactions to persulfate. The prevalence of 2+/3+ APS reactions in this single-center study was higher (2.85%) than that reported by the NACDG, 2015–2016 [Table 2]. However, our combined definite and probable relevance 13/61 (21%) aligns with the NACDG group (26.8%).
Table 2.
Comparison between our study and NACDG study*
| Our study | NACDG study* | |
|---|---|---|
| Number of patients (sample size) | 2138 | 5594 |
| Prevalence of 2+/3+ammonium persulfate reactions | 2.7% | 0.75% |
| Patients with definite and probable clinical relevance of ammonium persulfate allergy | 3/61 (21%) | 26/97 (26.8%) |
*North American Contact Dermatitis Group Patch Test Results: 2015-2016[8]
None of our nonoccupational patients (definite and probable group) nor our aquarium worker had associated immediate hypersensitivity symptoms in comparison to our hairdressers in whom immediate hypersensitivity symptoms were more common (P-value = 0.26, Fisher exact test, 2-tailed). The association did not reach statistical significance, which is likely because of our small sample size. We postulated that airborne exposure to persulfate on a constant basis in our hairdressers was responsible for the high prevalence of type I symptoms in this group. In patients with definite clinically relevant allergy to persulfate, the most common location of rash was on hands which corresponded to areas that would be exposed to APS [Diagram 1].
Illustrative case
A 31-year-old female had a history of an itchy rash on her dorsal hands and arms for 4 years. She was working full-time at the aquarium when her symptoms started and there was a temporal relationship between her symptoms and working at the aquarium. When she began working there less frequently as a volunteer only, she cleared. She was completely clear when patch testing began and had been clear for several months. She had patch testing that showed the following reactions: 1+-p-tert-butyl phenol-formaldehyde resin (PTBPFR), 3+ mixed dialkyl thiourea, 2+ benzalkonium chloride (BAK); 3+ diethyl thiourea; 3+ APS [Photo 1]. She developed a “recall phenomenon” at day 2 post-placement of patches, with flaring on her arms in the areas of her previous dermatitis, despite having no dermatitis when patch testing began and despite being away from work [Photo 2]. When she was previously working full-time at the aquarium, she had been exposed to potassium peroxymonosulfate, which was present in the disinfectant used to clean surfaces at the aquarium. We meant that her allergic reaction to thiourea is relevant to her past when she gets a reaction when her suits get wet at work as thiourea present in swimsuits. Her reactions to PTBPFR and BAK were of unknown clinical relevance.
Photo 1.

3+ allergic reaction to ammonium persulfate
Photo 2.

Recall phenomenon during patch testing
Limitations of our study include the retrospective nature of this study and the fact that it is a single-center study compared to the NACDG study.
In conclusion, the prevalence of allergy to APS reactions in this single-center study was higher than that reported by the NACDG. APS is an important occupational contact allergen in hairdressers and is associated with a high prevalence of immediate hypersensitivity symptoms. Strategies need to be instituted to prevent occupational sensitization to persulfate. It is important for clinicians to be aware of persulfate allergy to best counsel their patients about potential exposures and symptoms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pang S, Fiume MZ. Final report on the safety assessment of Ammonium, Potassium, and Sodium Persulfate. Int J Toxicol. 2001;20(Suppl 3):7–21. doi: 10.1080/10915810152630710. [DOI] [PubMed] [Google Scholar]
- 2.Cruz MJ, De Vooght V, Muñoz X, Hoet PH, Morell F, Nemery B, et al. Assessment of the sensitization potential of persulfate salts used for bleaching hair. Contact Dermatitis. 2009;60:85–90. doi: 10.1111/j.1600-0536.2008.01477.x. [DOI] [PubMed] [Google Scholar]
- 3.Gilligan P, Horst AV. Allergy to a hot tub water treatment chemical: An unexpectedly common cause of generalized dermatitis in men. J Clin Aesthet Dermatol. 2010;3:54–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Yankura JA, Marks JG, Jr, Anderson BE, Adams DR. Spa contact dermatitis. Dermatitis. 2008;19:100–1. [PubMed] [Google Scholar]
- 5.Kagen MH, Wolf J, Scheman A, Nedorost S. Potassium peroxymonosulfate-induced contact dermatitis. Contact Dermatitis. 2004;51:89–90. doi: 10.1111/j.0105-1873.2004.0396b.x. [DOI] [PubMed] [Google Scholar]
- 6.Kanerva L, Alanko K, Jolanki R, Aalto-Korte K, Estlander T. Occupational allergic contact dermatitis from potassium persulfate. Contact Dermatitis. 1999;40:116–7. doi: 10.1111/j.1600-0536.1999.tb06007.x. [DOI] [PubMed] [Google Scholar]
- 7.Veien NK, Hattel T, Laurberg G. Contact dermatitis due to potassium persulfate. Contact Dermatitis. 2001;45:176. doi: 10.1034/j.1600-0536.2001.045003176.x. [DOI] [PubMed] [Google Scholar]
- 8.DeKoven JG, Warshaw EM, Zug KA, Maibach HI, Belsito DV, Sasseville D, et al. North American Contact Dermatitis Group patch test results: 2015-2016. Dermatitis. 2018;29:297–9. doi: 10.1097/DER.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 9.Borelli S, Wüthrich B. Immediate and delayed hypersensitivity to ammonium persulfate. Allergy. 1999;54:893–4. doi: 10.1034/j.1398-9995.1999.00281.x. [DOI] [PubMed] [Google Scholar]
- 10.Hoekstra M, van der Heide S, Coenraads PJ, Schuttelaar ML. Anaphylaxis and severe systemic reactions caused by skin contact with persulfates in hair-bleaching products. Contact Dermatitis. 2012;66:317–22. doi: 10.1111/j.1600-0536.2012.02047.x. [DOI] [PubMed] [Google Scholar]
- 11.Piapan L, Mauro M, Martinuzzo C, Larese Filon F. Characteristics and incidence of contact dermatitis among hairdressers in north-eastern Italy. Contact Dermatitis. 2020;83:458–65. doi: 10.1111/cod.13687. [DOI] [PubMed] [Google Scholar]


