Abstract
The employees' psychological health and resilience in times of emergency and general uncertainty was chosen due to the immense implications for economics, entrepreneurs, psychologists and psychiatrists, and policymakers. This study aims to provide an insight into uncertainty-induced anxiety and depression among Chinese employees in the aftermath of the COVID-19 outbreak. Analysis performed in the context of China in the COVID-19 pandemic aftermath is significant due to the universal nature of external shock impact on psychological welfare, applicable across nations and business sectors and in similar contexts. The statistical analysis was performed with SEM software AMOS version 23. The research model consisting of fear of COVID-19, job insecurity, anxiety, depression, was empirically tested. A purposive sampling technique was applied with the online questionnaire shared with employees in companies located in China. Respondents were working in educational services, information technology, engineering, electronics, and other sectors on white-collar jobs. The data collection was conducted from May to August 2020, in the aftermath of the COVID-19 pandemic in China. The research sample consisting of 283 respondents was used for analysis. Path analysis was performed, and standardized parameter estimates, standard errors, and p-values were calculated. The results indicate a positive and significant impact of job insecurity on depression and anxiety. Furthermore, results indicate that the fear of COVID-19 significantly impacts anxiety and depression but does not impact job insecurity. The findings can be used in a multidisciplinary effort to mitigate the psychological damage. Furthermore, they complement the ongoing epidemiological and scientific discourse on people's personal health and choice of coping.
Keywords: COVID-19 mental health, Anxiety, Depression during COVID-19, Job insecurity, Fear of COVID-19
Introduction
The sudden outburst of COVID-19 pandemic engulfed major economies, health institutions and policymakers in an emergent contingency planning to manage adversities. Policies were introduced to mitigate consequences not solely from the financial and trading standpoint, but more importantly, proceeding from the more fundamental motivation to preserve the public welfare and sanity. As the crisis struck unexpectedly, policymakers were blindsided. Scientists from diverse disciplines were called upon to engage in a cooperative attempt to explore potential effects and uncover the remedy for the crisis's long-term effects on the human psyche. The unnerving uncertainty permeated all pillars of a healthy and sustainable society, calling into question the very stability of identities individuals' form of themselves and their surroundings during adversity (Van Bavel et al., 2020). Considering identity is partially fluctuating and inconstant, it is not surprising changes in the external environment perpetuate consequences for one’s internal mental states and influence individuals’ overall certainty perceptions (Kira et al., 2021). When people feel insecure, unsafe, or threatened, these fear-triggered emotions will shape their behavioral responses, be they adaptive or maladaptive (Kerahrodi & Michal, 2020). Self-identity, which is highly contextual and dependent on the appraisals drawn from collective identity, can be permanently altered by negative experiences and excessive anxiety, resulting in the formation of pathological coping patterns (Godinic & Obrenovic., 2020). So far, the research on the psychological consequences of COVID-19 has been extensive, especially concerning the occurrence of mental and mood disorders in the wake of instability-induced insecurity, accounting for the economic (Lund et al., 2018), psychological (Pfefferbaum & North, 2020) and psychiatric (Anjum et al., 2020) and policy-making (Zhang, 2020) perspective. Furthermore, as financial shocks shook economies, businesses were faced with several disruptions and many hindrances, including shutdowns, abrupt transitions to an online environment, changes in demand and supply shortages, and production closures (Shirahmadi et al., 2020). Consequently, unemployment rates increased dramatically, creating the atmosphere of general uncertainty wherein individuals questioned their employment and were faced with all the ramifications ambiguity brings about, such as worrying about not finding an alternative redeployment in case of displacement, loss of social outlet, affiliation-related status, structure, income, validation, purpose and opportunities for personal and professional development (Parolin et al., 2020). Apart from evident monetary loss, the stress of insecurity affects individuals' mood, relationships and general psychological and emotional health, leading to powerlessness, hurt, anger and depression. Changes in labor market dynamics caused employers to worry about liquidity and sustainability of operative activities and employees to dwell on their roles and responsibilities in the work setting.
Meanwhile, the pandemic influenced all labor market-related indicators, such as average salary (Qian & Fan, 2020), underemployment (Kawohl & Nordt, 2020), hiring rates, the occurrence of work-family conflict (Charoensukmongkol & Puyod, 2021; Novitasari et al., 2020), absenteeism (Der Feltz-Cornelis et al., 2020) and psychological impairment (Salman et al., 2020).
This paper aims to provide a preliminary insight into uncertainty-induced anxiety and depression among Chinese employees in the aftermath of the outbreak. As the phenomenon is still relatively new, the majority of data generated by prior research on threat outcomes on mental health and psychological impairment was collected during pandemic’ peaks. We created a framework encompassing the fear of COVID-19, uncertainty, anxiousness and depression. Our objective was to capture and measure the frequency and intensity of unhealthy and dysfunctional responses to fear using standard clinical inventory. Respondents were asked to self-reflect and assess according to personal subjective experience following the crisis. As Shramadi et al. (2020) well noted, public appraisals of the ongoing situation give a deeper understanding of personal experiences individuals undergo when subjected to an intense and volatile environment, and allow for comparison with the objective situation. Moreover, they enable us to better understand reckless behavioral responses during peril, considering people more often act on their emotions when striving for self-preservation, and are less likely to engage in an impartial, objective appraisal of the imminent danger.
Theory and Model Development
Fear of COVID-19
Sudden volatility and precariousness disrupting the common political, social, and economic functioning will likely have significant outcomes for psychological well-being (Reichert & Tauchmann, 2011). The intensity and impact of such instability will dictate the psychological vulnerability of the exposed population. Previous research on financial strain as a cause of mental impairment indicates that financial stressors during the economic decline translate to collective panic that is the social equivalent of a clinically significant depressive episode (Mahmud et al., 2021). Unpredictability and inconstancy-related stressors encompass restlessness over perceived, potential, or objective job loss which manifests as a depression layered with anxiety, unrest, dysthymia and dejection (Althouse et al., 2014; Catalano et al., 2011; Jesus et al., 2016). The association with a mood disorder was confirmed in the aftermath of prior monetary disasters, such as the Great Depression and the 2008 financial crisis (Lo & Cheng, 2014; Phillips & Nugent, 2014). A significant association between the pandemic and economic deterioration leads us to believe that the job uncertainty will have repercussions for psychological welfare and will, more specifically, lead to anxiety and depression (Dozois, 2021). Fear is conceptualized as an antecedent of maladaptive coping mechanisms and is thought to cause social and individual disintegration with two detrimental outcomes. It either inflicts intense psychological suffering, or it causes strain and dissociation wherein employees can disengage, lose focus or entirely fall back on their work assignments, thus risking discharge.
Accounting for Maslow's motivational hierarchy, we interpret hereinafter the ramifications of COVID-19 in light of such considerations that involve the negation or suspension of opportunities to realize physiological, relational and self-efficacy needs. The volatile nature of COVID-19 has significantly affected all economies, reducing the number of temporarily or full-time employed individuals (Zhang, 2020). As is now evident, the repercussions of COVID-19 are more extensive than those of similar crises and recovery will take much longer. Contrary to natural disasters or short-lived health challenges that entail short-term operational closures or confinement to mitigate the effects, the pandemic have been present for more than two years and are still an ongoing battle. It has affected all major economic segments, health, trading, and policy. Furthermore, it caused significant crashes and shook the Chinese economy, thus limiting employment and career opportunities and access to healthcare services.
Hypothesis 1 The fear of COVID-19 leads to job insecurity
The Relationship Between Uncertainty and Depression
Prior research exploring the extent and intensity of depression phenomenon found individuals experiencing the mood disorder to be living in a state of constant distrust, caution and apprehension over specific stressors, such as one’s current or overall life situation, whereby the mood swing feels like a creature with a life of its own (American Psychological Association, 2020a; Karp, 1996, pp. 124–5). Such a condition is characterized by an acute awareness that one lacks control and has little or no influence over the issue at hand. The underlying unease and waywardness causing the depressive episode often become a trigger for the chronic mental illness. The severity of the depression is evident in that it causes a vicious cycle in people's lives, where the profound lack of autonomy is simultaneously the root cause and the predominant feature of the disorder (Kira et al., 2021). The idea that depression affects the Self was long recognized by psychoanalysis. The low mood can lead to the disintegration of the Self by virtue of personal and social atrophy. The malady is felt as a prevalent sensation of melancholy arising from the disappointment in the objective world, eventually resulting in depreciation, devaluation and contentious retraction (Freud, 1957). Moreover, the explanation of the Self as being actualized through continuous communication with the real world and as a consequence of such interaction, as Heidegger, (1927/1962), Freud (1957) and Fuchs (2002) argued, presupposes the contextual socio-economic and circumstantial origin of the disorder.
Under main indications of clinical depression, vulnerable individuals experience extreme dissociation, retraction, or avoidance that manifests in causalities in the social, professional, or personal province. The excessive irritability aspect of depression arises from implicit angst that is latent in such a state (Dobson, 1985), so relevant scales often include anxiousness measurements to determine the condition (Svenaeus, 2007, 2008). The most common pattern includes severe retraction from the majority of or all activities individuals previously considered meaningful. The pathology spreading across cognitive processes causes continuous intrusion of harmful obsessive thoughts and influences the behavior.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) defines depression as a disorderly state with a clinically significant negative and dysfunctional repetitive behavioral and emotional pattern in reaction to a specific stressor that the individual perceives as especially problematic or as a general disability encompassing one or more crucial aspects of an individual’s life (American Psychiatric Association, 2000a, b, xxxi). Work serves to fill more than one purpose in life, as it not only allows individuals to make ends meet but also enables them to plan for the future, provides social support and recognition, facilitates career and personal growth and provides a sense of achievement. To lose such an asset is to lose a pillar of well-being, as psychological well-being is obtained through safe, rewarding and beneficial employment (Charoensukmongkol & Suthatorn, 2021).
Job Insecurity
Uncertainty arises as a consequence of a volatile, inconstant, erratic and unmanageable environment wherein individuals not only feel discomposed and unsure, but start to question their reasoning and the very ground they base their decisions upon, including thinking skills, knowledge, and information appraisal (Brashers, 2001). Following Herzberg’s (1968) definition, job certainty entails stable and secure employment with accompanying benefits, monetary or otherwise, in a particular status, income, career development and training, retirement and bonuses, and it extends beyond occupational characterization to include current and prospect development opportunities and socio-economic situation (Herzberg, 2017). According to the Conservation of Resources (COR) theory, people always seek to multiply their resources, and when some are threatened, they will use other less relevant available assets to retain those that are considered essential (Vander Elst et al., 2014). In other words, to maintain sanity and curb anxiety, they will use the energy, strength, skills, and knowledge to devise an effective strategy for preserving their well-being, to the employer's detriment (Jesus et al., 2016). An extensive amount of stamina and energy is invested in maintaining the coping strategy, and the association between coping behavior related to economic stress and psychological welfare is empirically substantiated in the literature (Stein et al., 2013).
The social aspect of job certainty concerns a complex network of intimate, professional, friendly and mentorship bonds employee forms with coworkers, partners, clients, leaders and managers. Unexpected closures and social distancing measures during COVID-19 national threat management enforcing lockdowns and proscribing the remote working policy forced employees into isolation. Such a sudden transition from a community-based environment to solitude leaves repercussions for mental health, leading to slow deterioration, irritability, anxiousness, and pervasively negative attitude or obsessive thoughts (Casale & Flett, 2020).
Job certainty plays a pivotal role in ensuring individuals' psychological well-being. For instance, under the proper leadership, employees experience less stress and are therefore able to fully engage in creative endeavors and drive an organization towards success (Huang et al., 2020; Puyod & Charoensukmongkol, 2021). To fulfill this objective, employees should first and foremost be fed transparent and accurate information that will enable for more precise assessment of the impending danger (Lin, 2020; Puyod & Charoensukmongkol, 2021). Sudden volatility in the organizational and business environment has both socio-economic and psycho-somatic repercussions (Stanisławski, 2019). The precondition for framing negativity into the opportunity for self-development and awareness lies upon the presumed individuals' capacity to differentiate between self-oriented fears and the industrial resentment due to the weak organizational constitution and poor resilience. Failing to acknowledge underlying emotions and fears contributing to anxiety and strain leads to negative thinking patterns. Job uncertainty can cause significant damage to employees' psyche as it consumes one's essential resources, blocks creativity and leads to workplace rigidity that can be detrimental in market volatility (Jofre-Bonet et al., 2018). As a central concern in organizational psychology, the uncertainty phenomenon was previously investigated in terms of adversities anxiety and strain bring to the organizational performance (Bert et al., 2021; Ganson et al., 2021; San Too et al., 2021). When it's key that the organization runs smoothly, where agility and flexibility are essential when responsiveness to sudden changes matters the most, a phenomenon of decline in performance and turnover increases. Instead of proving that they are crucial for organizational success and up to the challenge, employees disengage from their assignments, lack concentration, lack vision and willingness to take on the challenge, and fall back on their performance. This phenomenon is commonly known as reaction distress employed by individuals as an avoidance strategy. It represents a lack of motivation for active engagement when the action should be taken (Labrague & de los Santos, 2021). Furthermore, once the fear of losing employment kicks in, employees may detach from tasks or organization in general and focus their efforts on devising an alternative strategy that may ease their fears, such as creating a spending plan, seeking out supplementary income and taking on additional freelance projects, searching out information on qualifying for aid in case of a layoff, such as insurance, loans and tax reliefs. While this may be a useful coping strategy for individuals, namely adaptive fear control, it is damaging for organizations. During adversity and general ambiguity, people either assume an adaptive manner to cope with stress or engage in maladaptive coping, resulting in heightened paranoia, depression, angst, and anxiety (Liao et al., 2014). Either of these coping mechanisms requires resources. Consequently, we conclude the following hypothesis:
Hypothesis 2: Job insecurity leads to depression
Anxiety
Anxiety refers not only to a specific feeling of irritability, uncertainty and fear but on a more fundamental level, it represents an internal state of a human being coping to manage and manipulate surroundings to ensure survival (Banerjee, 2020). Way back before psychology and psychiatry emerged as specialized disciplines, many great existentialists have pondered the issue of existential dread, how it relates to one’s perception, and to what extent it changes in response to external stimuli (Kierkegaard, 1843/1954, 1849/1954; Sartre, 1939/1994, 1989; Husserl, 1954). However, fear and anxiety should be delineated with regard to their reference (Barlow, 2002). For instance, following Tillich (1952a, b), fear is directed towards a particular issue while anxiety has no specific object but is rather an underlying precondition for all action. Therefore, it is incitement and stimuli for growth and development when balanced and managed adequately. Whenever a person is dwelling on the future, transience, meaning, and sustenance the Self is always inevitably bemused by its fate.
Several authors have employed Terror Management Theory (TMT) to address the issue and empirically substantiate these theoretical assumptions. According to TMT, anxiety is a result of human fear of death, final extinction that emerges from the mixture of self-preservation instinct and acknowledgment of impermanence (Solomon et al., 1991). Failure to account for the influence of both ends can result in pathology. Prior studies found the threat to be predictive of one’s coping strategy choice, anxiety to be predictive of willingness to engage in prevention and the level of panic indicative of self-preservation (Cypryańska & Nezlek, 2020). Due to COVID-19 being a significant threat on more than one frontier, the pandemic are more likely to harm public psychological welfare (Ahorsu et al., 2020). At the onset researchers eagerly engaged in investigating the association of pandemic-induced anxiety with other mood disturbances and the occurrence of psycho-somatic diseases (Stanton et al., 2020).
As was already demonstrated in the literature, financial disadvantage and lack of resources for satisfying rudimentary physiological needs lead to mental deterioration, be it from fear and psychological uncertainty or actual shortage of sources for preservation (Fabian, 2013; Flores et al., 2017). The job can be represented as the reservoir of conveniences, as it is a means of acquiring essential skills and knowledge that can be an asset in obtaining additional opportunities for income and resource accumulation. However, during the COVID-19 threat not only related to job security but to health concerns as well (Blustein et al., 2019; Lai et al., 2020), people invest significant effort into coping with challenges, managing daily obligations under highly stressful conditions and confronting trepidation with protective action, which drains the psyche. Therefore, we conclude the following:
Hypothesis 3: Job insecurity leads to anxiety
Our paper moves past the purely biological and neurological annotation of depression to encompass more comprehensive causation, such as socio-economic and occupational factors that contribute to the occurrence of depressive episodes. To make an association more explicit, we posit the environmental conditioning of depression, arguing for the considerable role external factors exert on a human psyche. The rationale for such reasoning is based upon numbers concerning the increase in depressive states during major financial, natural and health disasters(Almeida & Xavier, 2013; Liao et al., 2014). Empirical evidence points to a major increase in depressed, anxious, paranoid and suicidal populations (Branas et al., 2015; De Vogli et al., 2013). In this lieu, major crises, disasters, pandemic, and related instability and volatility can cause a frenzy, resulting in mental illness (Taylor, 2019). Economic decline leads to low mood and anxiety through prospect or actual job loss (Mahmud et al., 2021).
During adversity and major disastrous events, the need for relatedness comes to the fore as individuals facing a challenge strive for social support (Krug et al., 2021). Furthermore, one draws a sense of Self from social identity, i.e., the role the individual assumes in collectives, and cultural and political association he or she makes, affiliations one acquires (Ryand & Deci, 2000). All partial identifications by affiliation constitute personal identity (Haslam et al., 2018). Identity can be threatened either by the sudden collapse in a socio-economic environment that indirectly affects personal identity via closures, layoff, loss of status, etc. or by a personal identity crisis, whereby individuals' personal challenges and self-doubt reflect on their work or ability to perform a specific role in a broader community (Burke, 2020). Therefore, it is pretty logical to assume that employment is crucial for psychological well-being considering it allows for actualization and fulfillment of several human needs, such as the need for relatedness, social support, self-development, self-accomplishment, self-efficacy and serves as the tool for ensuring life quality (Thompson et al., 2017).
Furthermore, the implementation of lockdown policies and restrictions on social gatherings imposed during the COVID-19 outbreak peaks drained people of much required social support that is considered a pillar to psychological well-being, leaving individuals lonesome, alienated, and isolated (Jahangiry et al., 2020). As social beings people are in constant need of interaction and mutual validation (Zhao & Wu, 2021). Breaking of affiliations, even for short periods, especially those that are considered constitutive of one’s identity may lead to severe mental downfall, burning out the energy and striping individuals of their sense of purpose (Killgore et al., 2020; Tull et al., 2020). Fear can function both as a facilitator or impediment (Pollock et al., 2020), i.e., it can serve as a stimulus for abiding by protective rules and taking preventive measures with the end goal being a desire to end the threatening situation as soon as possible. However, excessive fear may paralyze and lead to personality collapse, wherein each action may seem futile and meaningless. There is now already extensive empirical support for the claim that job uncertainty during COVID-19 leads to strain and depression (Blanuša et al., 2021; Godinic et al., 2020; Nelson & Kaminsky, 2020).
Hypothesis 4: The fear of COVID-19 leads to depression
Hypothesis 5: The fear of COVID-19 leads to anxiety
Materials and Methods
The study used the survey strategy with cross-sectional data collection via an online questionnaire. Spector (2019) suggested that a cross-sectional research design can provide support for relationships between variables. A purposive sampling technique was applied with the online questionnaire distributed to white-collar employees in organizations located in China, Jiangsu province. Respondents were working in knowledge-intensive sectors related to educational services, information technology, engineering, and electronics on white-collar jobs, to ensure the homogeneity of the sample. The research sample was accessed with the help of the companies management. The data collection was conducted anonymously from May to August 2020 in the aftermath of the COVID-19 pandemic. The questionnaire consisted of questions and scales capturing demographic data, fear of COVID-19, job insecurity, anxiety, and depression. The multi-item scales were evaluated on a 5-point Likert scale. The link to access the online questionnaire was distributed to 400 employees. A total of 301 respondents completed the questionnaire. The missing values were eliminated, followed by the analysis that was performed on the sample of 283 respondents. Out of 283 respondents, 150 were male (53%) and 133 were female (47%). All the respondents were of Chinese nationality. Most of the respondents were were between 21 and 29 years old, 43.4% respectively and between 30 and 39 years old, 32.5% respectively. 21.9 percent were older than 40, and only 3.2% of the respondents were under 21 years of age. In terms of educational background, 90% of the participants have a bachelor's degree or above. Specifically, 40.6% of the respondents have a bachelor's degree, 49.4% hold a postgraduate and Ph.D. degree. The remaining 10% hold a high school degree. As for employment status, among all the respondents, 54.1% worked 40 h or more per week, and the other 45.9% worked less than 40 h per week. The demographic information is displayed in Table 1.
Table 1.
Demographic information
| Demographic categories | Frequency | Value percentage |
|---|---|---|
| Gender | ||
| Male | 150 | 53.0% |
| Female | 133 | 47.0% |
| Age | ||
| 18–21 | 9 | 3.2% |
| 21–29 | 123 | 43.4% |
| 30–39 | 92 | 32.5% |
| 40–49 | 45 | 15.9% |
| 50–59 | 14 | 5.0% |
| Nationality | 100.0% | |
| Chinese | 283 | |
| Education level | ||
| Postgraduate degree | 140 | 49.4% |
| Bachelor's degree | 115 | 40.6% |
| High school degree | 28 | 10% |
| Employment status | ||
| Fulltime—40 h or more per week | 153 | 54.1% |
| Part time—Less than 40 h per week | 130 | 45.9% |
| Total respondents | 283 | |
Measurements
Fear of COVID 19
The Fear of COVID-19 was taken from Blakey et al. (2015), who adapted the Wheaton et al. (2012) scale. The scale was used to assess the fear of Ebola. The Fear of COVID 19 scale consists of 9 items measured on a 5 point Likert scale ranging from "Not at all" (1) to "Very much" (5). Scale includes sample items: "How quickly do you believe contamination from COVID-19 is spreading in your country?"; "To what extent has the threat of COVID-19 influenced your decisions to be around people?" and "To what extent has the threat of COVID-19 influenced your travel plans?".
Job Insecurity
We adopted the job insecurity (JIS) scale from De Witte (2000). The items were evaluated on a 5-point Likert scale ranging from "strongly disagree" to "strongly agree". The scale consists of four items that include: "(1) Chances are, I will soon lose my job, (2) I am sure I can keep my job, (3) I feel insecure about the future of my job, and (4) I think I might lose my job in the near future."
Anxiety
The seven-item Generalized Anxiety Disorders (GAD-7) scale is used to evaluate worry and anxiety symptoms. The GAD-7 scale consists of seven items that are measured with a 5-point Likert scale ranging from “1” represented “not at all” to “5” represented “nearly every day.” The sample items include: "Worrying too much about different things"; "Trouble relaxing" and "Being so restless that it's hard to sit still “.
Depression
The Center for Epidemiology Scale for Depression (CES-D) was utilized to evaluate the frequency of depression symptoms. The scale was created by the National Institute of Mental Health for epidemiological research (Radloff, 1977) and consists of 20 items. Four independent factors: depressive affect, positive affect, somatic symptoms, and interpersonal relations comprise the CES-D scale. A 5-point Likert scale ranging from “1” for “rarely or none of the time (< 1 week)” to “5” for “almost or all of the time (the whole month)” was used to measure the items that captured how the respondents felt during the last month. Sample items include: “I felt depressed"; "I felt that everything I did was an effort" and "My sleep was restless “.
Statistical Analysis and Results
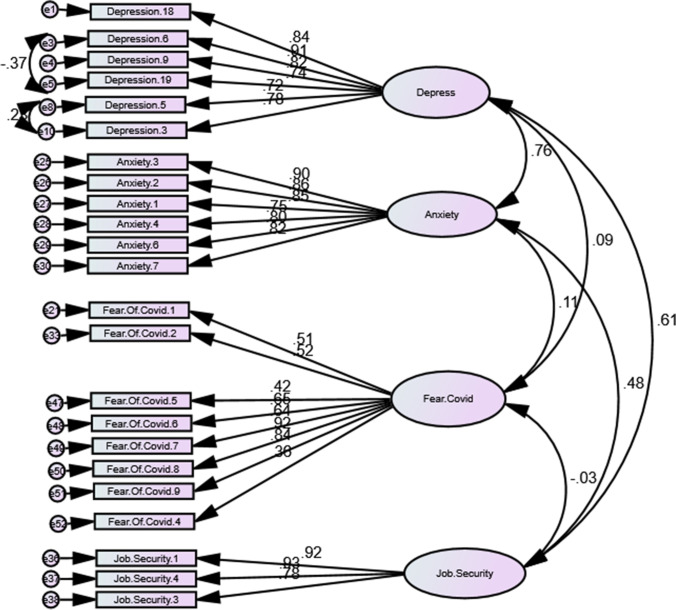
The statistical analysis was performed with SEM software AMOS version 23. The research model consisting of four variables, including fear of COVID-19, job insecurity, anxiety, depression was tested (Fig. 1). The research sample consisting of 283 respondents was used for analysis. The validity check of the measurement tool was performed using confirmatory factor analysis (CFA). Maximum likelihood estimation was done, and the goodness-of-fit indices were calculated for the observed model to assess the model and data fit. Indices that were calculated include χ2/df (normed chi-square statistic); RMSEA (root mean square error of approximation); NFI (normed fit index); CFI (comparative fit index); GFI (goodness-of-fit index); RMR (root-mean-square residual) and TLI (Tucker–Lewis Index). The confirmatory factor analysis was performed indicating that model requires improvement (χ2/df = 3.813; CFI = 0.784; SRMR = 0.077; RMSEA = 0.053). Factor loadings below 0.55 were deleted (Fornell and Larcker, 1981), and CFA was performed (Fig. 2). After deleting Depression 7, 10, 11, 12, 14, 16, 17 and 20 and Anxiety 5 due to high correlation between depression and anxiety and adding two covariances the model fit became better (χ2/df = 3.788; CFI = 0.89; SRMR = 0.062; RMSEA = 0.053). That was justified by Byrne (2010) due to synonymous formulation.
Fig. 1.
Research model of the study
Fig. 2.
Measurement model (CFA)
Composite reliability (CR), average variance extracted (AVE), and correlation matrix aimed to confirm the convergent and discriminant validity were calculated (Table 2). AVE coefficients of all the variables is above 0.6, whereas CR was above 0.8, indicating consistency. Thus, the convergent validity was confirmed. Furthermore, as indicated in the table AVE is higher than maximum shared variance (MSV) of each construct, thus confirming discriminant validity.
Table 2.
CR, AVE, and correlation matrix
| Validity testing | ||||||||
|---|---|---|---|---|---|---|---|---|
| CR | AVE | MSV | MaxR(H) | Fear.Covid | Depress | Anxiety | Job.Insecurity | |
| Fear.Covid | 0.905 | 0.547 | 0.043 | 0.915 | 0.740 | |||
| Depress | 0.907 | 0.621 | 0.612 | 0.925 | 0.098 | 0.788 | ||
| Anxiety | 0.945 | 0.740 | 0.612 | 0.948 | 0.207 | 0.782 | 0.860 | |
| Job.Insecurity | 0.884 | 0.719 | 0.141 | 0.908 | -0.033 | 0.376 | 0.248 | 0.848 |
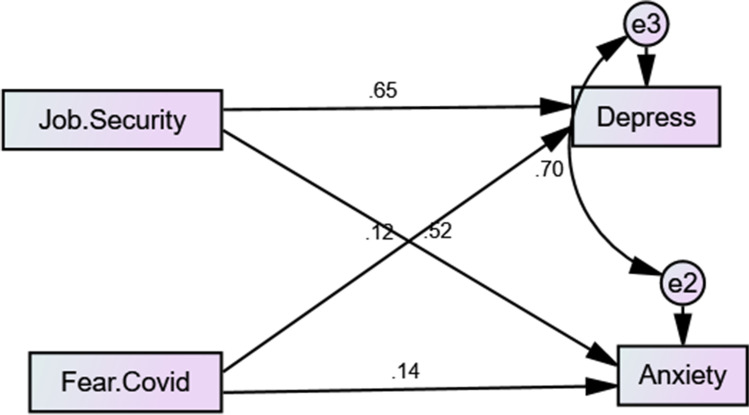
Next, structural equation modeling (SEM) was applied to test the structural model. The hypothesized model was evaluated for the fit, with the results suggesting fit improvements. To achieve a better fit a covariance between e3 and e2 was added and a path between Fear and Job Insecurity was removed due to poor significance (p = 0.427). Consequently, Hypothesis 1 is rejected. The manipulations allowed to attain an excellent model fit (χ2/df = 0.309; CFI = 1; SRMR = 0.017; RMSEA = 0) as shown in Table 3.
Table 3.
Model fit measures
| Measure | Estimate | Threshold | Interpretation |
|---|---|---|---|
| CMIN | 0.927 | – | – |
| DF | 3 | – | – |
| CMIN/DF | 0.309 | Between 1 and 3 | Excellent |
| CFI | 1 | > 0.95 | Excellent |
| SRMR | 0.017 | < 0.08 | Excellent |
| RMSEA | 0 | < 0.06 | Excellent |
| Pclose | 0.992 | > 0.05 | Excellent |
Path analysis was performed and standardized parameter estimates, standard errors, and p-values were calculated (Table 4). Fear of COVID-19, job insecurity, anxiety and depression relationships were assessed. The results indicate a positive and significant impact of Job insecurity on Depression (β = 0.644; p < 0.001) and Anxiety (β = 0.506; p < 0.001). Consequently, Hypotheses 2 and Hypotheses 3 are accepted. The analysis showed that the fear of COVID-19 has a significant impact on Anxiety (β = 0.235; p < 0.005) and Depression (β = 0.208; p < 0.005). Thus, Hypotheses 4 and 5 are accepted. Standardized parameter estimates, standard errors, and p values for the structural model are displayed in Table 3. The SEM model is depicted in Fig. 3.
Table 4.
Standardized parameter estimates, standard errors, and p values for the structural model
| Dep. Var | Path | Indep. Var | Std Estimate |
Estimate | S.E | C.R | P | Label |
|---|---|---|---|---|---|---|---|---|
| Depress | < –- | Job.Insecurity | 0.648 | 0.644 | 0.058 | 11.189 | *** | |
| Depress | < –- | Fear.Covid | 0.119 | 0.208 | 0.102 | 2.05 | ** | |
| Anxiety | < –- | Job.Insecurity | 0.519 | 0.506 | 0.063 | 7.982 | *** | |
| Anxiety | < –- | Fear.Covid | 0.136 | 0.235 | 0.112 | 2.097 | ** |
Fig. 3.
Improved structural model
Discussion
The post-pandemic environment surely brought about calamities with regard to many causalities for individuals' socio-economic functioning and psychosocial states. The actual picture should be of the utmost relevance for organizational psychologists and general managers as the outcomes of the distraught population are directly dealing with a critical workforce that is to be employed post hoc weak economic recovery. In the aftermath of the COVID-19 outburst, we are becoming able to generate much more accurate data on the actual number of psychologically impaired and vulnerable Chinese individuals and assess the extent and intensity retrospectively. As other studies have eagerly engaged in conducting and confirming reports on mood disorders and related traumatic disturbances on a macro-level, our paper allows for comparison between gathered reports and self-assessment survey responses, including a break-down for clarification of key antecedents of depression and anxiety during adversity. Our framework accounted for two possible fear responses: maladaptive and adaptive behavior. One hinges on fear and leads to retraction and avoidance, which is damaging for the human psyche and creates a negative pattern in organizational citizenship behavior. In contrast, adaptive responses entail high threat perception and high efficacy beliefs, e.g.e, individuals' beliefs in the efficaciousness of the preventive action, which is taken for the sole purpose of curbing the spread. They are willing to sacrifice socializing, status, affiliations, capital, knowledge, incomes, and bonuses when they believe the action is attainable and will be very effective. We draw our inferences from prior works by Teasdale et al. (2012) and Van Bavel et al. (2020). Each of the two strategies requires a significant investment of core resources, be it actual financial assets and cognitive capital and skills for obtaining additional income and advancing carrier opportunities or resorting to a reservoir of psychological resources one uses to counter the threat and create a buffer against traumatic events. Respiratory diseases require transparent, quick and responsive communication on desirable behavioral modifications, and prior study attempts focused on risk evaluation such as perceived plausibility, while the emotional aspect of the measurement itinerary was directed towards capturing the perceived and objective possibility of getting sick, a latent idea layered with excessive worry, angst and avoidance. The coinciding of psychological and behavioral factors during previous health challenges was long before posited from experience with preceding crisis (Liao et al., 2014).
We have therefore ascertained that the financial shock has a negative impact on the human psyche by means of rising job insecurity, i.e., the phenomenon is not exclusively related to the unemployed and poor, but also to those who are under the real or perceived threat of getting layoff or are missing career opportunities and long-term projects they would generally have. Furthermore, apart from other short-lived health challenges, the COVID-19 pandemic differs in that it has been ongoing for two years now and we are still are at odds with managing its ramifications. To remedy the consequences, the introduction of somewhat controversial policies and restrictions on social gatherings is rigorous and universal, draining individuals of psychological resources that would otherwise be employed as an asset for acquiring additional advantageous sources. Unlike other related epidemics and disasters, the outbreak has touched upon all frontiers – personal, social, monetary, physiological (Aguiar-Quintana et al., 2021; Godinic et al., 2020). Contrary to our assumption that the fear brought on by the pandemic will increase the job insecurity, we were not able to establish statistically significant relationship between the two, which is at odds with findings gathered by Blanuša et al. (2021) and Ruffolo et al. (2021).
According to Blanuša et al. (2021), the psychological strain becomes more and more prominent as the job becomes less secure. Workplace volatility increases the dilemma and general mistrust and leads to occupational and personal psychopathology (Bünnings et al., 2017). Monetary preoccupation and not knowing what the future holds, combined with doubt in subsequent employability and a severe lack of control, results in employees being alienated, distracted, distant and disengaged (Huang et al., 2012). According to observations prevalence of the maladaptive coping is recorded in our survey. As it turns out, even those compliant with enforced norms and aware of challenges ahead that did abide by restrictions and regulations still experienced symptoms of anxiousness and depression, such as discouragement, obsessive thinking, burnout, tension and discontent. Psychological welfare is always at risk when one is presented with a substantial threat. Events that qualify as such include catastrophes, disasters, breakdowns, recession, health challenges, tensions and market crashes. Without precedent, these lead to depression and anxiety (Burgard et al., 2012; Caramanica et al., 2014; IMF, 2020; Li et al., 2020) Therefore, the hypotheses 2 and 3 stating job insecurity leads to depression and anxiety, are accepted. Our results are fully in line with Stanisławski (2019), Bert et al. (2021), and San Too et al. (2021).
The majority of Chinese workers experienced adverse emotional rollercoasters due to uprising ambiguity and comprehensive lifestyle change consisting for the most of constrain and isolation. Almost revolutionary, the transition to an online environment and shifting all social and occupational activities to an online mode lacking clear indication of 'going back to normal' lead to panic, angst and depressive thinking.
In this study, we tested the precaution measures taken by respondents and the fear imposed by social distancing and related policies. Not surprisingly, those with significant threat awareness due to high susceptibility and possible exposure to the virus were also concerned with the response efficacy. Hypothesis 4 and 5 stating fear of COVID-19 leads to anxiety and depression are accepted, and thus we in the aftermath of the infection corroborate findings generated by LaMontagne et al. (2020), and Rossi et al. (2020), Nelson and Kaminsky (2020) and Ganson et al. (2021) during peaks of the pandemic. Furthermore, we have corroborated COVID-19 induced trauma results of Aguiar-Quintana et al. (2021) and Ganson et al. (2021)
Conclusion
The topic of employees' psychological health and resilience in times of emergency and general uncertainty was chosen due to the immense implications for economics, entrepreneurs, psychologists and psychiatrists, and policymakers. Results gathered from the Chinese sample are, due to the universal nature of external shock impact on psychological welfare, applicable across nations and business sectors and in similar contexts. Considering COVID-19 is a global challenge, notwithstanding the difference in restrictions choice and implementation timeline, repercussions for workforce and labor market concerning possible challenges coincide. Governmental and organizational failure to recognize potential hindrances and timely provide support and resources often results in a low success rate of creative endeavors and reduced performance. A support system is often not set in advance, and employees are left struggling with their new roles, obligations, expectations, and a whole new business model. They may easily engage in skepticism or lower the organizational outcome by looking into alternative possibilities for acquiring income. Such reactions stem from fear and even lead to high turnover intention. Even those who aren't considering plan b, if not adequately addressed, become less of a success factor and more a hindrance. All these reflections are relevant during the crisis. However, the attention is shifted from prevention to post-crisis healing in the aftermath. Infrastructural support, guidance, training, counseling, and pre-qualifications become a viable option to ensure labor adequacy. Our results add to the existing literature and further elaborate on the major shocks ramifications on mental health and latent drivers of mental disorders arising from stressful circumstances. Practically, our findings can be contrasted to prior studies and included in a multidisciplinary effort to mitigate the psychological damage. It aligns with the ongoing epidemiological and scientific discourse on people's intimate health and coping choices.
Study Limitations and Future Research
The research suffers from several limitations. The study uses a cross-sectional research design, which is widely considered inferior to longitudinal research when establishing causal relationships between variables. Thus, future studies can use longitudinal research to validate the study results. Additionally, the data collection was carried out during the aftermath stage of the COVID-19 pandemic in China. Future studies can investigate the relationships during other stages of the COVID-19 pandemic. Another limitation is that the study relies on self-reported measures to collect data. Future studies may use content analysis and experimentation to investigate the impact of social media on mental health.
Furthermore, due to the limited sample size, we could not account for the differences in anxiety and depression levels among different occupational groups and across industries. Future studies are advised to address the limitation by examining the occurrence of mental disorders and the effects of job insecurity in the COVID-19 aftermath among individuals from specific industries and diverse occupations. We could not confirm the impact of fear of COVID-19 on job insecurity. Nevertheless, we recommend future research to assess the relationship and mediation effects of job insecurity. Other factors, such as personality and proneness to fear and anxiety, tenure and professional qualification, confidence in leadership, may interfere to reduce responsiveness to fear of COVID-19. Future studies should further look into these factors. This study offers preliminary insight into psychological aftereffects and lays the ground for future investigation on how job insecurity relates to fear, identity disturbance, and anxiety.
Data Availability
The datasets, models created during this research can be provided by the corresponding authors upon the reasonable request.
Declarations
Consent to Participate
Informed consent from participants was acquired online, before they started the investigation.
Ethical Statement
Approval was obtained from the ethics committee of Huazhong University of Science and Technology. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Akmal Khudaykulov, Email: ahudaykulov@live.com.
Zheng Changjun, Email: 631795110@qq.com.
Bojan Obrenovic, Email: bojan@inovatus-usluge.hr.
Danijela Godinic, Email: danijela.godinic5@gmail.com.
Ilimdorjon Jakhongirov, Email: jahongirov@inbox.ru.
References
- Aguiar-Quintana, T., Nguyen, H., Araujo-Cabrera, Y., & Sanabria-Díaz, J. M. (2021). Do job insecurity, anxiety and depression caused by the COVID-19 pandemic influence hotel employees’ self-rated task performance? The moderating role of employee resilience. International Journal of Hospitality Management,94, 102868. 10.1016/j.ijhm.2021.102868. [DOI] [PMC free article] [PubMed]
- Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction, 1–9. [DOI] [PMC free article] [PubMed]
- Almeida JMC, Xavier M. Estudo epidemiológico nacional de saúde mental: 1° relatório [National Epidemiological Study of Mental Health: 1st report] Faculdade de Ciências Médicas, Universidade Nova de Lisboa; 2013. [Google Scholar]
- Althouse B, Allem J, Childers M, Dredze M, Ayers J. Population health concerns during the United States' great recession. American Journal of Preventive Medicine. 2014;46:166–170. doi: 10.1016/j.amepre.2013.10.008. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2000a). Diagnostic and Statistical Manual of Mental Disorders (4th ed., Text Revision). Washington, DC: American Psychiatric Association.
- American Psychological Association. (2020b). Depression. https://www.apa.org/topics/depression/.
- Anjum, S., Ullah, R., Rana, M. S., Ali Khan, H., Memon, F. S., Ahmed, Y., … Faryal, R. (2020). COVID-19 pandemic: A serious threat for public mental health globally. Psychiatria Danubina,32(2), 245–250. [DOI] [PubMed]
- Banerjee, D. (2020). The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian journal of psychiatry, 50, 102014. [DOI] [PMC free article] [PubMed]
- Bert F, Gualano MR, Thomas R, Vergnano G, Voglino G, Siliquini R. Exploring the possible health consequences of job insecurity: A pilot study among young workers. Gaceta Sanit. 2021;34:385–392. doi: 10.1016/j.gaceta.2018.08.011. [DOI] [PubMed] [Google Scholar]
- Blakey SM, Reuman L, Jacoby RJ, Abramowitz JS. Tracing “Fearbola”: psychological predictors of anxious responding to the threat of ebola. Cognitive Therapy and Research. 2015;39(6):816–825. doi: 10.1007/s10608-015-9701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanuša J, Barzut V, KneŽević J. Intolerance of uncertainty and fear of COVID-19 moderating role in the relationship between job insecurity and work-related distress in The Republic of Serbia. Frontiers in Psychology. 2021;12:647972. doi: 10.3389/fpsyg.2021.647972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blustein DL, Kenny ME, Di Fabio A, Guichard J. Expanding the impact of the psychology of working: Engaging psychology in the struggle for decent work and human rights. Journal of Career Assessment. 2019;27:3–28. doi: 10.1177/1069072718774002. [DOI] [Google Scholar]
- Branas CC, Kastanaki AE, Michalodimitrakis M, Tzougas J, Kranioti EF, Theodorakis PN, et al. The impact of economic austerity and prosperity events on suicide in Greece: A 30-year interrupted time-series analysis. British Medical Journal Open. 2015;5:e005619. doi: 10.1136/bmjopen-2014-005619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brashers DE. Communication and uncertainty management. The Journal of Communication. 2001;51:477–497. doi: 10.1111/j.1460-2466.2001.tb02892.x. [DOI] [Google Scholar]
- Bünnings C, Kleibrink J, Weßling J. Fear of unemployment and its effect on the mental health of spouses. Health Economics. 2017;26:104–117. doi: 10.1002/hec.3279. [DOI] [PubMed] [Google Scholar]
- Burgard SA, Kalousova L, Seefeldt KS. Perceived job insecurity and health: The Michigan Recession and Recovery Study. Journal of Occupational and Environmental Medicine. 2012;54:1101–1106. doi: 10.1097/JOM.0b013e3182677dad. [DOI] [PubMed] [Google Scholar]
- Burke PJ. Identity dispersion: flexibility, uncertainty, or inconsistency? In: Serpe RT, Stryker R, Powell B, editors. Identity and symbolic interaction. Springer; 2020. pp. 89–117. [Google Scholar]
- Byrne BM. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming. Abingdon, VA: Routledge; 2010. [Google Scholar]
- Caramanica K, Brackbill RM, Liao T, Stellman SD. Comorbidity of 9/11-related PTSD and depression in the World Trade Center Health Registry 10–11 years postdisaster. Journal of Traumatic Stress. 2014;27:680–688. doi: 10.1002/jts.21972. [DOI] [PubMed] [Google Scholar]
- Casale S, Flett GL. Interpersonally-based fears during the covid-19 pandemic: reflections on the fear of missing out and the fear of not mattering constructs. Clin. Neuropsychiatry. 2020;17:88–93. doi: 10.36131/CN20200211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano R, Goldman-Mellor S, Saxton K, Margerison-Zilko C, Subbaraman M, LeWinn K, et al. The health effects of economic decline. Annual Review of Public Health. 2011;32:431–450. doi: 10.1146/annurev-publhealth-031210-101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charoensukmongkol, P., & Puyod, J. V. (2021). Influence of transformational leadership on role ambiguity and work–life balance of Filipino University employees during COVID-19: does employee involvement matter?. International Journal of Leadership in Education, 1–20.
- Charoensukmongkol, P., & Suthatorn, P. (2021). How managerial communication reduces perceived job insecurity of flight attendants during the COVID-19 pandemic. Corporate Communications: An International Journal.
- Cypryańska M, Nezlek JB. Anxiety as a mediator of relationships between perceptions of the threat of COVID-19 and coping behaviors during the onset of the pandemic in Poland. PLoS ONE. 2020;15:e0241464. doi: 10.1371/journal.pone.0241464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vogli R, Marmot M, Stuckler D. Excess suicides and attempted suicides in Italy attributable to the great recession. The Journal of Epidemiology and Community Health. 2013;67:378–379. doi: 10.1136/jech-2012-201607. [DOI] [PubMed] [Google Scholar]
- De Witte H. Work ethic and job insecurity: Assessment and consequences for well-being, satisfaction and performance at work. Group Communication. 2000;52:325–350. [Google Scholar]
- Der Feltz-Cornelis V, Maria C, Varley D, Allgar VL, De Beurs E. Workplace stress, presenteeism, absenteeism, and resilience amongst university staff and students in the COVID-19 lockdown. Frontiers in Psychiatry. 2020;11:1284. doi: 10.3389/fpsyg.2020.01284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobson KS. The relationship between anxiety and depression. Clinical Psychology Review. 1985;5(4):307–324. doi: 10.1016/0272-7358(85)90010-8. [DOI] [Google Scholar]
- Dozois DJ. Anxiety and depression in Canada during the COVID-19 pandemic: A national survey. Canadian Psychology/psychologie Canadienne. 2021;62(1):136. doi: 10.1037/cap0000251. [DOI] [Google Scholar]
- Fabian E. Work and disability. In: Blustein DL, editor. The Oxford handjournal of the psychology of working. Oxford University Press; 2013. pp. 185–201. [Google Scholar]
- Flores L, Navarro R, Ali S. The state of SCCT research in relation to social class: Future directions. Journal of Career Assessment. 2017;25:6–23. doi: 10.1177/1069072716658649. [DOI] [Google Scholar]
- Freud S. Mourning and melancholia. The Standard Edition of the Complete Psychological Works of Sigmund Freud. Hogarth; 1957. [Google Scholar]
- Fornell C, Larcker DF. Structural equation models with unobservable variables and measurement error: algebra and statistics. J. Mark. Res. 1981;18:382–388. doi: 10.1177/002224378101800313. [DOI] [Google Scholar]
- Fuchs T. The phenomenology of shame, guilt and the body in body dysmorphic disorder and depression. Journal of Phenomenological Psychology. 2002;33:223–243. doi: 10.1163/15691620260622903. [DOI] [Google Scholar]
- Ganson KT, Tsai AC, Weiser SD, Benabou SE, Nagata JM. Job insecurity and symptoms of anxiety and depression among US young adults during COVID-19. Journal of Adolescent Health. 2021;68:53–56. doi: 10.1016/j.jadohealth.2020.10.008. [DOI] [PubMed] [Google Scholar]
- Godinić, D., & Obrenovic, B. (2020). Effects of economic uncertainty on mental health in the COVID-19 pandemic context: social identity disturbance, job uncertainty and psychological well-being model. International Journal of Innovation and Economic Development, 6(1)
- Godinic D, Obrenovic B, Khudaykulov A. Effects of economic uncertainty on mental health in the COVID-19 pandemic context: Social identity disturbance, job uncertainty and psychological well-being model. International Journal of Business and Management. 2020;6:61–74. doi: 10.18775/ijied.1849-7551-7020.2015.61.2005. [DOI] [Google Scholar]
- Haslam C, Jetten J, Cruwys T, Dingle G, Haslam SA, editors. The New Psychology of Health: Unlocking the Social Cure. Routledge; 2018. [Google Scholar]
- Heidegger, M. (1927/1962). Being and Time (Macquarrie, J. and Robinson, E. trans.). Blackwell.
- Herzberg F. Motivation to Work. Routledge; 2017. [Google Scholar]
- Herzberg F. One More Time: How Do You Motivate Employees. Boston, MA: Harvard Business Review; 1968. [PubMed] [Google Scholar]
- Huang GH, Niu X, Lee C, Ashford SJ. Differentiating cognitive and affective job insecurity: Antecedents and outcomes. Journal of Organizational Behavior. 2012;33:752–769. doi: 10.1002/job.1815. [DOI] [Google Scholar]
- Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192–195. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- Husserl, E. (1954). Die Krisis der europäischen Wissenschaften und die transzendentale Phänomenologie, ed W. Biemel and Husserliana VI. Den Haag: Martinus Nijhoff.
- IMF (2020). World Economic Outlook Update, October 2020: A Long and Difficult Ascend.
- Jahangiry L, Bakhtari F, Sohrabi Z, Reihani P, Samei S, Ponnet K, et al. Risk perception related to COVID-19 among the Iranian general population: An application of the extended parallel process model. BMC Public Health. 2020;20:1–8. doi: 10.1186/s12889-020-09681-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesus SN, Leal AR, Viseu JN, Valle P, Matavelli RD, Pereira J, et al. Coping as a moderator of the influence of economic stressors on psychological health. AnálisePsicológica. 2016;34:365–376. doi: 10.14417/ap.1122. [DOI] [Google Scholar]
- Jofre-Bonet M, Serra-Sastre V, Vandoros S. The impact of the Great Recession on health-related risk factors, behaviour and outcomes in England. Soc. Sci. Med. 2018;197:213–225. doi: 10.1016/j.socscimed.2017.12.010. [DOI] [PubMed] [Google Scholar]
- Karp DA. Speaking of Sadness: Depression, Disconnection, and the Meanings of Illness. Oxford University Press; 1996. [Google Scholar]
- Kawohl W, Nordt C. COVID-19, unemployment, and suicide. The Lancet Psychiatry. 2020;7(5):389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerahrodi, J. G., & Michal, M. (2020). The fear-defense system, emotions, and oxidative stress. Redox Biology, 101588. [DOI] [PMC free article] [PubMed]
- Kierkegaard, S. (1843/1954). Fear and trembling. Princeton University Press.
- Kierkegaard, S. (1849/1954). The sickness unto death. Princeton University Press.
- Killgore, W. D., Cloonen, S. A., Taylor, E. C., & Dailey, N. S. (2020). Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res.,290,. [DOI] [PMC free article] [PubMed]
- Kira IA, Shuwiekh HA, Alhuwailah A, Ashby JS, Sous Fahmy Sous M, Baali SBA, Jamil HJ. The effects of COVID-19 and collective identity trauma (intersectional discrimination) on social status and well-being. Traumatology. 2021;27(1):29. doi: 10.1037/trm0000289. [DOI] [Google Scholar]
- Krug, H., Haslam, S. A., Otto, K., & Steffens, N. K. (2021). Identity leadership, social identity continuity, and well-being at work during COVID-19. Frontiers in Psychology, 12. [DOI] [PMC free article] [PubMed]
- Labrague LJ, de Los Santos JAA. Fear of Covid-19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management. 2021;29(3):395–403. doi: 10.1111/jonm.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wu J, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMontagne AD, Too LS, Laura Punnett L, Milner AJ. Changes in job security and mental health: An analysis of 14 annual waves of an Australian working population panel survey. American Journal of Epidemiology. 2020;190:207–215. doi: 10.1093/aje/kwaa038. [DOI] [PubMed] [Google Scholar]
- Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain, Behavior, and Immunity. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Q, Cowling BJ, Lam WW, Ng DM, Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: Ten cross-sectional surveys. BMC Infectious Diseases. 2014;14:169. doi: 10.1186/1471-2334-14-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CY. Social reaction toward the 2019 novel coronavirus (COVID-19) Social Health and Behavior. 2020;3(1):1. doi: 10.4103/SHB.SHB_11_20. [DOI] [Google Scholar]
- Lo C, Cheng T. Race, unemployment, and chronic mental illness: A 15 year trend analysis. Social Psychiatry and Psychiatric Epidemiology. 2014;49:1119–1128. doi: 10.1007/s00127-014-0844-x. [DOI] [PubMed] [Google Scholar]
- Lund, C., Brooke-Sumner, C., Baingana, F., Baron, E. C., Breuer, E., Chandra, P., … Saxena, S. (2018). Social determinants of mental disorders and the Sustainable Development Goals: A systematic review of reviews. The Lancet Psychiatry,5(4), 357–369. [DOI] [PubMed]
- Mahmud MS, Talukder MU, Rahman SM. Does ‘Fear of COVID-19’trigger future career anxiety? An empirical investigation considering depression from COVID-19 as a mediator. The International Journal of Social Psychiatry. 2021;67(1):35. doi: 10.1177/0020764020935488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson B, Kaminsky DB. COVID-19's multipronged attack on mental health. Cancer Cytopathology. 2020;128:679–680. doi: 10.1002/cncy.22364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novitasari D, Sasono I, Asbari M. Work-family conflict and worker’s performance during Covid-19 pandemic: What is the role of readiness to change mentality. International Journal of Science and Management Studies (IJSMS) 2020;3(4):122–134. doi: 10.51386/25815946/ijsms-v3i4p112. [DOI] [Google Scholar]
- Parolin, Z., Curran, M., Matsudaira, J., Waldfogel, J., & Wimer, C. (2020). Monthly Poverty Rates in the United States During the COVID-19 Pandemic. Center on Poverty and Social Policy at Columbia University.
- Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. New England Journal of Medicine. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Phillips J, Nugent C. Suicide and the great recession of 2007–2009: The role of economic factors in the 50 U.S. states. Social Science and Medicine. 2014;116:22–31. doi: 10.1016/j.socscimed.2014.06.015. [DOI] [PubMed] [Google Scholar]
- Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed-methods systematic review. Cochrane Database of Systematic Reviews. 2020;11:CD013779. doi: 10.1002/14651858.CD013779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puyod, J. V., & Charoensukmongkol, P. (2021). Effects of workplace rumors and organizational formalization during the COVID-19 pandemic: a case study of universities in the Philippines. Corporate Communications: An International Journal.
- Qian Y, Fan W. Who loses income during the COVID-19 outbreak? Evidence from China. Research in Social Stratification and Mobility. 2020;68:100522. doi: 10.1016/j.rssm.2020.100522. [DOI] [Google Scholar]
- Radloff, L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306
- Reichert, A., & Tauchmann, H. (2011). The Causal Impact of Fear of Unemployment on Psychological Health, No 266. Ruhr Economic Papers, RWI - Leibniz-Institut für Wirtschaftsforschung, Ruhr-University Bochum, TU Dortmund University, University of Duisburg-Essen.
- Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffolo M, Price D, Schoultz M, Leung J, Bonsaksen T, Thygesen H, et al. Employment uncertainty and mental health during the COVID-19 pandemic initial social distancing implementation: A cross-national study. Global Social Welfare. 2021;8:141–150. doi: 10.1007/s40609-020-00201-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55:68–78. doi: 10.1037/0003-066X.55.1.68. [DOI] [PubMed] [Google Scholar]
- Salman, M., Asif, N., Mustafa, Z. U., Khan, T. M., Shehzadi, N., Tahir, H., ... & Mallhi, T. H. (2020). Psychological impairment and coping strategies during the COVID-19 pandemic among students in Pakistan: a cross-sectional analysis. Disaster Medicine and Public Health Preparedness, 1–7. [DOI] [PMC free article] [PubMed]
- San Too L, Leach L, Butterworth P. The cumulative impact of high job demands, low job control and high job insecurity on midlife depression and anxiety: A prospective cohort study of Australian employees. Occupational and Environmental Medicine. 2021;78:400–408. doi: 10.1136/oemed-2020-106840. [DOI] [PubMed] [Google Scholar]
- Sartre, J. P. (1989). Being and Nothingness, Barnes, H.E. (trans.). Routledge.
- Sartre, J.-P. (1939/1994). Sketch for a theory of the emotions. Routledge.
- Shirahmadi, S., Seyedzadeh-Sabounchi, S., Khazaei, S., Bashirian, S., Miresmæili, A. F., Bayat, Z., & Dadae, N. (2020). Fear control and danger control amid COVID-19 dental crisis: Application of the Extended Parallel Process Model. PloS one,15(8). [DOI] [PMC free article] [PubMed]
- Solomon S, Greenberg J, Pyszczynski T. A terror management theory of social behavior: The psychological functions of self-esteem and cultural worldviews. Advances in Experimental Social Psychology. 1991;24:93–159. doi: 10.1016/S0065-2601(08)60328-7. [DOI] [Google Scholar]
- Spector PE. Do Not Cross Me: Optimizing the Use of Cross-Sectional Designs. Journal of Business and Psychology. 2019;34:125–137. doi: 10.1007/s10869-018-09613-8. [DOI] [Google Scholar]
- Stanisławski K. The coping circumplex model: An integrative model of the structure of coping with stress. Frontiers in Psychology. 2019;10:694. doi: 10.3389/fpsyg.2019.00694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. International Journal of Environmental Research and Public Health. 2020;17:4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein C, Hoffmann E, Bonar E, Leith J, Abraham K, Hamill A, et al. The United States economic crisis: Young adults' reports of economic pressures, financial and religious coping and psychological well-being. Journal of Family and Economic Issues. 2013;34:200–210. doi: 10.1007/s10834-012-9328-x. [DOI] [Google Scholar]
- Svenaeus F. Do antidepressants affect the Self? A phenomenological approach. Medicine, Health Care and Philosophy. 2007;10:153–166. doi: 10.1007/s11019-007-9060-8. [DOI] [PubMed] [Google Scholar]
- Svenaeus, F. (2008). Tabletter för Känsliga Själar: Den Antidepressiva Revolutionen. Nora: Nya Doxa · Herzberg, F. (1968). One More Time: How Do You Motivate Employees, Vol. 65. Boston, MA: Harvard Business Review [PubMed]
- Taylor S. (2019). The psychology of pandemic: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing.
- Teasdale E, Yardley L, Schlotz W, Michie S. The importance of coping appraisal in behavioural responses to pandemic flu. The British Journal of Health Psychology. 2012;17:44–59. doi: 10.1111/j.2044-8287.2011.02017.x. [DOI] [PubMed] [Google Scholar]
- Thompson M, Nitzarim R, Her P, Sampe M, Diestelmann J. Financial stress and work hope beliefs among adolescents. Journal of Career Assessment. 2017;25:254–267. doi: 10.1177/1069072715621517. [DOI] [Google Scholar]
- Tillich P. The courage to be. Yale University Press; 1952. [Google Scholar]
- Tillich P. Anxiety, religion, and medicine. Pastoral Psychology. 1952;3:11–17. doi: 10.1007/BF01769082. [DOI] [Google Scholar]
- Tull MT, Edmonds KA, Scamaldo K, Richmond JR, Rose JP, Gratz K. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Research. 2020;289:113098. doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bavel, J. J., Baicker, K., Boggio, P. S., Capraro, V., Cichocka, A., Cikara, M., et al. (2020). Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour,1–12,. 10.31234/osf.io/y38m9. [DOI] [PubMed]
- Vander Elst T, Van den Broeck A, De Cuyper N, De Witte H. On the reciprocal relationship between job insecurity and employee well-being: Mediation by perceived control? Journal of Occupational and Organizational Psychology. 2014;87:671–693. doi: 10.1111/joop.12068. [DOI] [Google Scholar]
- Wheaton MG, Abramowitz JS, Berman NC, Fabricant LE, Olatunji BO. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research. 2012;36:210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- Zhang, H. (2020). China's employment stabilization policies in response to the impact of the COVID-19 pandemic. International Journal of Sociology and Social Policy.
- Zhao S, Wu X. From information exposure to protective behaviors: Investigating the underlying mechanism in COVID-19 outbreak using social amplification theory and extended parallel process model. Frontiers in Psychology. 2021;12:1351. doi: 10.3389/fpsyg.2021.631116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets, models created during this research can be provided by the corresponding authors upon the reasonable request.