Abstract
Atresia of the left main coronary artery is a rare coronary anomaly. We describe the case of a 5-year-old child presenting in emergency in extremis. Clinical findings of haemodynamic collapse, malignant ventricular tachyarrhythmias and severe mitral regurgitation were indicative of a possible ischaemic aetiology. Surgical revascularization of the atretic left main coronary artery segment using an interposition autologous saphenous vein graft was successfully performed.
Keywords: Left main coronary artery atresia, Coronary artery anomalies, Mitral regurgitation, Coronary artery bypass grafting
Coronary artery anomalies are a diverse group of congenital cardiac malformations.
INTRODUCTION
Coronary artery anomalies are a diverse group of congenital cardiac malformations. Although they are seen in 0.64–5.6% of adult patients undergoing coronary angiography, there are limited data regarding the paediatric population, with an estimated prevalence of 0.9% [1–3]. Atresia of the left main coronary artery (LMCA) is one of its least frequently observed variations. It has been suggested that the aetiology may be either an infection or systemic disease that causes fibrotic changes in the media, thus leading to obstruction or thrombosis. However, evidence of these could not be determined in most of the cases.
CASE REPORT
A 5-year-old male child presented to our department with ventricular arrhythmias (doublets, triplets and Torsade de points) causing haemodynamic instability. On examination, a grade II/VI systolic murmur was heard at the apex. Transthoracic echocardiography showed a dilated left atrium with severe mitral regurgitation. The ventricular septum and the anterolateral papillary muscle appeared hyper-echogenic, thus raising suspicion of chronic ischaemia. The left ventricular ejection fraction was slightly reduced (45%). The right coronary artery (RCA) was dominant while the left coronary artery (LCA) could not be conclusively visualized. Due to refractory cardiac arrhythmias with haemodynamic collapse, the child needed extracorporeal life support. A veno-arterial extracorporeal membrane oxygenation (ECMO) stabilized the haemodynamics and a cardiac catheter examination revealed atresia of the LMCA (Fig. 1A).
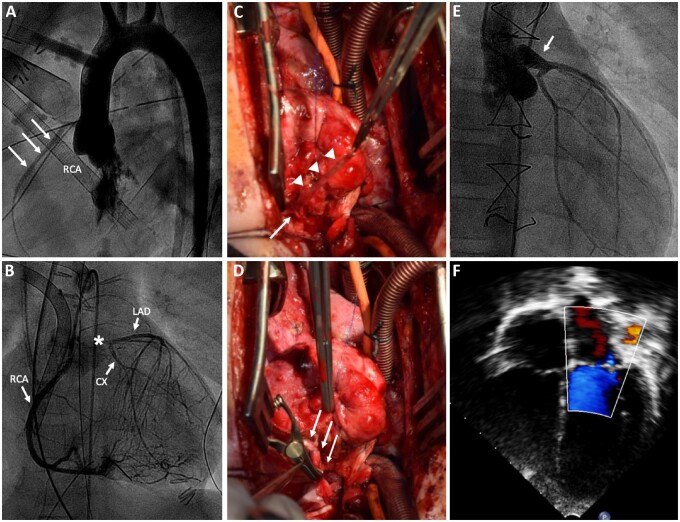
Figure 1:
(A) Preoperative angiogram showing a large RCA (arrows). The origin of the left coronary artery fails to contrast on aortic root injection. (B) Preoperative coronary angiogram: large RCA with late retrograde filling of the left coronary artery system through multiple collaterals. Retrograde contrast filling of the left main coronary artery ends up in a blind stump (asterisk). (C) Picture showing the atretic left coronary artery (arrow) with the distal anastomosed vein graft (arrowheads). (D) Autologous great saphenous vein interposition graft (arrows) from aortic sinus to the left anterior descending coronary artery. (E) Selective angiography at 1-year follow-up showing a well revascularized left coronary artery system. (F) Echo Doppler image showing trivial mitral regurgitation at 1 year follow-up. CX: circumflex branch of the left coronary artery; LAD: left anterior descending coronary artery; RCA: right coronary artery.
The angiogram showed a robust contrasting RCA with a diameter of 2.8 mm and a conspicuously absent left coronary ostium and LMCA. A retrograde contrast-filled left coronary system through multiple collaterals from the RCA could be observed. The retrogradely filled LCA stump extended up to 7 mm upwards from the potential site of the LCA ostium (Fig. 1B). An urgent surgical revascularization of the LMCA was undertaken. A moderately hypothermic bicaval–aortic cardiopulmonary bypass was instituted. Antegrade as well as retrograde cold blood cardioplegia was administered. Aortotomy confirmed the absence of the left coronary ostium as well as the proximal 1 cm of the LMCA. Surgical revascularization was performed using a short autologous great saphenous vein interposition graft (Fig. 1C and D). The patient was weaned off ECMO on postoperative day 4. Angiography at 1 year showed a nicely revascularized LCA system (Fig. 1E). Transthoracic echocardiography showed a normalized left ventricular ejection fraction, with residual dyskinesia of the interventricular septum and a trivial mitral regurgitation (Fig. 1F). The child is in New York Heart Association class I.
DISCUSSION
Congenital atresia of the LMCA is a rare coronary anomaly in which there is no left coronary ostium. The proximal left main stem ends blindly and blood flows retrogradely from the RCA via small collaterals [4]. The diagnosis is usually delayed because of the non-specific symptoms. Typical signs such as syncope, tachyarrhythmia and heart failure may be variably absent, depending on the amount of collaterals perfusing the atretic territory.
Our patient did report 2 syncopal events under physical strain, 1 and 2 years ago. A cardiac evaluation to rule out coronary aetiology was not sought for until the present admission. Except for these episodes, the child was healthy and showed normal development and growth. Coronary angiography remains the gold diagnostic standard, and restoring a 2-coronary system-based myocardial perfusion can achieve the goal of normal coronary flow reserve. In the present case, the short atretic segment was best amenable to a short autologous vein interposition graft. Successful coronary revascularization using the left internal mammary artery has been reported; however, there are little data on the long-term outcome of coronary revascularization in children [5]. Under these circumstances, an initial end-to-end revascularization of the left main segment is expected to provide a good long-term patency, while allowing the option of a later internal mammary coronary artery bypass operation.
CONCLUSION
While persistent malignant cardiac arrhythmias, severe mitral valve regurgitation or low cardiac output syndrome obviously warrant an emergency ischaemia work-up, even symptoms such as syncope and seizures should be looked at with suspicion. Diagnostic coronary imaging, including conventional angiography, is essential to rule out coronary artery anomalies. Surgical revascularization is the best option for atresia of the LMCA.
Conflict of interest: none declared.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Antonios Kallikourdis and the other, anonymous reviewer(s) for their contribution to the peer-review process of this article.
REFERENCES
- 1. Kardos A, Babai A, Rudas L, Gaál T, Horváth T, Tálosi L. et al. Epidemiology of congenital coronary artery anomalies: a coronary arteriography study on a Central European population. Cathet Cardiovasc Diagn 1997;42:270–5. [DOI] [PubMed] [Google Scholar]
- 2. Angelini P, Villason S, Chan AV, Diez JG.. Humans normal and anomalous coronary arteries in humans. In: Coronary Artery Anomalies: A Comprehensive Approach. Philadelphia, PA: Lippincott Williams and Wilkins, 1999. [Google Scholar]
- 3. Uysal F, Bostan O, Semizel E, Signak I, Asut E, Ergun C.. Congenital anomalies of coronary arteries in children: the evaluation of 22 patients. Pediatr Cardiol 2014;35:778–84. [DOI] [PubMed] [Google Scholar]
- 4. Musiani A, Cernigliaro C, Sansa M, Maselli D, De Gasperis C.. Left main coronary artery atresia: literature review and therapeutical considerations. Eur J Cardiothorac Surg 1997;11:505–14. [DOI] [PubMed] [Google Scholar]
- 5. Gebauer R, Cerny S, Vojtovic P, Tax P.. Congenital atresia of the left coronary artery—myocardial revascularization in two children. Interact CardioVasc Thorac Surg 2008;7:1174–5. [DOI] [PubMed] [Google Scholar]