Abstract
OBJECTIVES
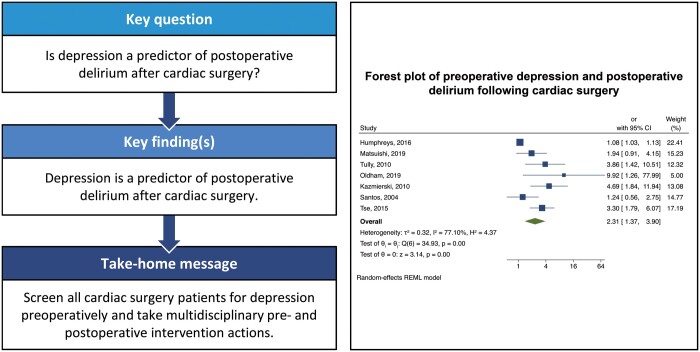
Depression is common in patients with cardiac disease. The importance of preoperative depression for development of postoperative delirium (POD) following cardiac surgery is not well known. The aim is to provide a summary estimate of depression as a predictor of POD following cardiac surgery.
METHODS
Systematic search of MEDLINE, EMBASE, Cochrane Library, Web of Science Core Collection and Psycinfo (Ovid) was performed from inception to October 2019, including cohort studies reporting odds ratios (ORs) and 95% confidence intervals (CIs) for POD following cardiac surgery in patients with preoperative depression compared to patients without depression. ORs and 95% CIs for POD were calculated using random-effects meta-analyses. Subgroup and sensitivity analyses were performed.
RESULTS
Seven studies were included with a combined study population of 2066 patients. The pooled prevalence of POD in the combined study population was 26% and preoperative depression was present in ∼9% of the total study population. All studies showed a positive association between preoperative depression and POD; and in 5 studies, the association was statistically significant. Patients with depression had a pooled OR of 2.31 (95% CI 1.37–3.90) for POD.
CONCLUSIONS
This systematic review and meta-analysis confirm the findings that the previous association between preoperative depression and increased risk for developing POD reported for other patient groups is found also in cardiac surgery. Depression screening prior to cardiac surgery may be effective in identifying patients at higher risk for POD.
Keywords: Depression, Postoperative delirium, Cardiac surgery, Meta-analysis
Depression is a common mental disorder affecting more than 264 million people in the world [1] with a higher prevalence in women who are more likely to develop depression during their life compared to men [2].
INTRODUCTION
Depression is a common mental disorder affecting more than 264 million people in the world [1] with a higher prevalence in women who are more likely to develop depression during their life compared to men [2]. Depression is a common comorbidity in patients with cardiovascular disease and in patients undergoing cardiac surgery, the incidence exceeds the general population by 2–3 times [3]. Moreover, 22–55% of cardiac surgery patients are affected by acute delirium postoperatively [4–7]. Delirium is a change in cognition or development of a perceptual disturbance that cannot be explained by pre-existing or evolving dementia. According to the Diagnostic and Statistical Manual of Mental Disorders, developed by the American Psychiatric Association, the definition includes an acutely evolved shift in attention, awareness and cognition not related to a reduced level of arousal such as a coma [8]. Hence, delirium develops over a short period of time, and tends to fluctuate during the day and the disturbance is caused by the direct physiological consequences of a medical condition [8]. Delirium with an onset of delirious symptoms shortly after surgery is defined as postoperative delirium (POD). POD can be further divided into 3 subgroups, namely hyperactive, hypoactive and mixed form. Symptoms of hyperactive POD are hypervigilance, restlessness, agitation and combativeness, whereas hypoactive POD is characterized by lack of awareness, lethargy and decreased motor activity and may therefore be difficult to detect. Hyper- and hypoactive forms of POD frequently coincide and the symptoms often fluctuate during the day [9]. POD after cardiac surgery is associated with adverse outcomes including higher rates of postoperative complications, poorer long-term outcomes and increased length of hospital stay [10]. Patients who develop POD are also more likely to experience depression and anxiety for the first 4–6 months after surgery [4, 6, 10–13]. Patients with depression prior to cardiac surgery as well as patients with delirium after cardiac surgery have poorer long-term prognosis after cardiac surgery [10, 13–16]. However, it is unknown whether depression precedes delirium, and more specifically POD. Chronic inflammation has proven to play a key role in the pathogenesis of several chronic disorders, including cardiovascular disease and depression [3]. Furthermore, neurocognitive disorders, including POD, correlate with and originate in a neuroinflammation triggered by a systemic inflammatory activation [17–19]. With common shared pathways, a correlation between cardiovascular disease, depression and POD is plausible. The aim of this systematic review and meta-analysis is to investigate whether depression is a predictor of POD after cardiac surgery. To our knowledge, this is the first meta-analysis to investigate depression as a predictor of POD after cardiac surgery.
MATERIALS AND METHODS
Study design
A systematic literature review and meta-analysis were performed following an established study protocol.
Search strategy
References for this systematic review—Depression as a predictor of POD after cardiac surgery—were searched with no language or year restrictions in the following databases: Medline (OVID®), Embase®, Cochrane Library (Wiley), Web of Science™ Core Collection (Thomson Reuters) and PsycINFO® (OVID®). Librarians at the Karolinska Institutet University Library performed the searches in October 2019, starting with identifying Medical Subject Headings (MeSH-terms) in MEDLINE. The search strategy comprised 3 concepts that were combined using the set operator AND. These 3 concepts were searched using the following MeSH-terms:
Mood Disorders OR Depression OR Type D Personality
Cardiovascular Surgical Procedures OR Anesthesia, Cardiac Procedures OR Cardiopulmonary Bypass OR Cardiovascular System/su
Confusion OR Hallucinations OR Illusions
Each search concept was also complemented by relevant free-text terms. For complete documentation of search strategies, see the Supplementary Material. We followed the preferred reporting items for systematic reviews and meta-analysis guidelines and the European Journal of Cardiothoracic Surgery statistical primer [20–22]. Article selection and data extraction were undertaken by 2 reviewers (A.F., J.K.) with disagreements resolved by consensus.
Selection criteria
We included all cohort studies investigating the association between preoperative depression and POD after cardiac surgery. Non-cohort studies were excluded, along with studies focusing on postoperative depression. Abstracts, case reports, conference presentations, editorials, reviews, expert opinions or animal studies were not included.
Data extraction
Data and characteristics of the included studies were extracted independently by 2 investigators (A.F. and J.K.) using separate spreadsheets. Any differences were resolved through dialogue until consensus was reached. The data extracted included the first author’s name, year of publication, study period, country, surgical procedure, assessment of depression, assessment of delirium, total number of patients, number of patients in the exposed and non-exposed groups, number of exposed patients with POD, number of unexposed patients with POD, unadjusted and multivariable adjusted odds ratios (ORs) and 95% confidence intervals (CIs).
Quality assessment
For quality assessment, the Newcastle–Ottawa scale was used. The Newcastle–Ottawa scale is a tool for quality assessment of non-randomized studies using a star system judged from 3 perspectives: selection of study groups, comparability of groups and ascertainment of either the exposure or outcome of interest for case-control or cohort studies. A study can be awarded stars for high quality in each area with a maximum of 4 stars for the selection category, 2 stars for comparability and 3 stars for outcome [23] (Supplementary Material). The Newcastle–Ottawa scale has been recommended as a tool for quality assessment of cohort and case–control studies [24]. In addition, the STROBE guidelines were used [25].
Exposure
The definition of exposure was preoperative depression. The assessment of depression differed between the studies using self-assessment questionnaires or ICD-diagnoses.
Outcome
The primary outcome was POD on postoperative days 1–7. The assessment of POD differed between the studies. All studies used the DSM diagnostic criteria for definition/classification of POD.
Data synthesis and statistical analysis
Unadjusted and adjusted ORs and CIs were extracted from the selected articles. In the studies lacking an OR, we manually calculated the number [26]. To take into account the clinical diversity and methodological variation among the studies, the random-effects model was used to calculate the summary statistics and their 95% CIs. Results of meta-analyses are displayed in forest plots. Publication bias was assessed through the visual examination of a funnel plot. Data management and statistical analyses were performed using Stata (Version.16.1 Stata Corp, College Station, TX, USA) [27].
Sensitivity analysis
To measure the impact of individual studies on the pooled estimate, a series of new meta-analyses were performed in which the pooled estimates were calculated omitting 1 study at a time using a random-effects model.
Subgroup analysis
Due to the different types of surgery, a separate meta-analysis without Matsuishi et al. [28] and Tse et al. [29] was performed, as these studies also included patients undergoing vascular surgery and transcatheter aortic valve implantation (TAVI).
RESULTS
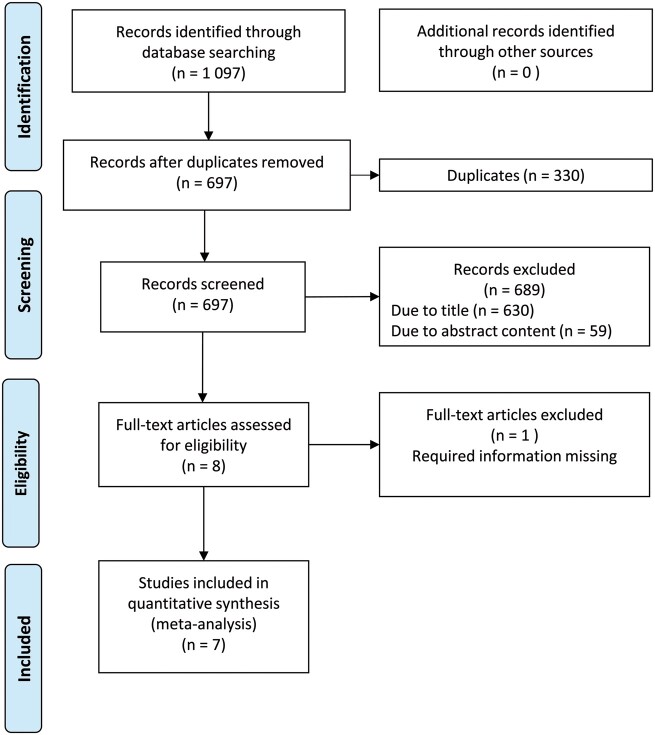
The literature search was finalized in October 2019. The total number of hits were 1027 before deduplication and 697 after deduplication. Of these, 689 articles were excluded due to title and abstract content. The remaining 8 full-text articles were assessed for eligibility. One study by Detroyer et al. [5] including 104 patients undergoing cardiac surgery showed no association between depressive symptoms and POD. Unfortunately, they did not present ORs or number of events in the depressed versus non-depressed group. After contacting the authors without getting a response, the study could not be included in the meta-analysis. A flow chart of the screening process is shown in Fig. 1. The articles included in the meta-analysis were published between 2004 and 2019 and comprised a total of 2.066 patients undergoing cardiovascular surgery in the USA, Australia, Japan, Brazil, Belgium and Poland. The number of patients in each study ranged from 131 to 563. The characteristics of the included studies are presented in Table 1. The quality of the included studies was assessed as moderate (Table 1).
Figure 1:
PRISMA flow chart for systematic review of preoperative depression and postoperative delirium following cardiac surgery. PRISMA: preferred reporting items for systematic reviews and meta-analysis.
Table 1:
Characteristics of included studies
| First author, year | Study period | Country | Procedure | Assessment of depression | Assessment of delirium | Number of patients, (depressed/non-depressed) | Crude OR | Multivariable adjustment | Adjusted OR (95% CI) | Nos |
|---|---|---|---|---|---|---|---|---|---|---|
| Humphreys, 2016 | 2003–2011 | Australia | CABG | DASS | DSI, SPMSQ | 173 | Not reported | Male gender, hyper-cholesterolemia, diabetes, urgent surgery | 1.08 (1.03–1.13) | 5 |
| Kazmierski, 2009 | 2004–2007 | Poland | CABG, CABG + valve surgery, valve surgery | MINI | DSM-IV | 563 (35/528) | 3.85 (1.87–7.88) | Age, MMSE <25, MD, anaemia, AF, intubation >24 h, pO2 <60 mmHg | 4.69 (1.84–11.93) | 7 |
| Oldham, 2018 | 2012–2016 | USA | CABG | DISH, HDRS, PHQ-9, GDS | CAM, MMSE, DSI | 131 (13/118) | 3.98 (1.16–13.71) | Age, sex, MCI, preoperative depression, MCA stenosis >50%, CCI, Lawton score | 9.92 (1.26–77.88) | 6 |
| Tully, 2010 | 2007–2009 | Australia | CABG, concomitant valve surgery | MINI | DSI | 158 (27/131) | 3.49 (1.48–8.26) | Sex, age, cross-clamp time, Hb, psychotropic drug use | 3.86 (1.42–10.52) | 7 |
| Santos, 2004 | 1996–1999 | Brazil | CABG | GDS | DSM-IV | 220 (29/191) | 1.24 (0.56–2.75) | Not reported | Not reported | 6 |
| Matsuishi, 2019 | 2015–2016 | Japan | Cardio-vascular, thoracic and abdominal artery surgery | HADS | RASS, CAM-ICU | 142 (37/105) | 1.94 (0.91–4.16) | Not reported | Not reported | 6 |
| Tse, 2015 | 2008 | Canada | CABG, CABG + other, TAVI | DSM IV | CAM, DSM-IV | 679 (57/622) | Not reported | Age, history of delirium, stroke/TIA, cognitive impairment, depression, preop beta-blocker use | 3.3 (1.8–6.1) | 6 |
AF: atrial fibrillation; CABG: coronary artery bypass grafting; CAM: confusion assessment method; CAM-ICU: confusion assessment method for the intensive care unit; CI: confidence interval; DASS: depression anxiety and stress scales; DISH: Depression Interview and Structured Hamilton; DSI: Delirium Symptom Interview; DSM-IV: diagnostic and statistical manual of mental disorders fourth edition; GDS: the Geriatric Depression Scale; HADS: Hospital Anxiety and Depression Scale; Hb: haemoglobin; HDRS: the Hamilton Depression Rating Scale; MCA: middle cerebral artery; MCI: mild cognitive impairment; MD: major depression; MINI: the Mini International Neuropsychiatric Interview; NOS: Newcastle–Ottawa scale; OR: odds ratio; PHQ-9: the Patient Health Questionnaire-9; Preop: preoperative; RASS: Richmond Agitation-Sedation Scale; SPMSQ: short portable mental status questionnaire; TAVI: transcatheter aortic valve implantation; TIA: trans-ischaemic attack.
Assessment of depression
Preoperative depression was present in ∼198 patients, i.e. 9% of the combined study population. Humphreys et al. [30] did not account for the ratio of depression prior to surgery. When excluding the patients from this study (173 patients), the prevalence of preoperative depression reached 10%. Six studies defined depression through self-assessment from questionnaires and 1 study through ICD-diagnoses. In the Humphreys et al. [30] study, depression was assessed before surgery using the depression anxiety and stress scales. In 2 of the studies, Kazmierski et al. [31] and Tully et al. [32], depression was assessed using the Mini International Neuropsychiatric Interview. Oldham et al. [33] used 3 different depression scales to evaluate depression before surgery: the Depression Interview and Structured Hamilton the Hamilton Depression Rating Scale and the Patient Health Questionnaire-9. Santos et al. [34] evaluated depression using the Geriatric Depression Scale. Matsuishi et al. [28] assessed depressive symptoms using the Hospital Anxiety and Depression Scale. In the Tse et al. [29] study, depression was diagnosed by physicians using the DSM IV criteria.
Definition/classification and assessment of postoperative delirium
In the total study population, the pooled prevalence of POD was 26%. When removing 2 articles that also included non-cardiac surgery patients [28, 29], the pooled prevalence of POD was 24%. All studies used the DSM diagnostic criteria for definition/classification of POD [8]. For the assessment of delirium, different tools were applied. Humphreys et al. [30] and Tully et al. [32] used the Delirium Symptom Interview to assess POD. The Delirium Symptom Interview combines interview questions with behavioural observations and has good sensitivity (0.90) and specificity (0.80), as well as strong inter-rater reliability (0.90) [30, 35]. Tse et al. [29] used the confusion assessment method (CAM). The CAM is a standardized tool, based on the DSM criteria, that helps non-psychiatrically trained clinicians to identify and recognize delirium [36]. In the Oldham et al. [33] study, POD was assessed by a psychiatrist at baseline and on postoperative days 2–5 using the CAM and the delirium index, which is a tool for evaluating the severity of POD [37]. Matsuishi et al. [28] used the Richmond Agitation-Sedation Scale and the confusion assessment method for the intensive care unit (ICU), which is a development of the CAM for use in an ICU. In 2 studies [31, 34], psychiatrists evaluated POD using the DSM criteria [8].
Surgical procedure
In 3 of the studies, only patients undergoing coronary artery bypass grafting (CABG) were included [30, 33, 34]. In the Kazmierski et al. [31] study, the participants underwent CABG, cardiac valve replacement and combined procedures. Tully et al. [32] included patients undergoing CABG with or without cardiac valve replacement. In addition to cardiac surgery, Matsuishi et al. [28] included abdominal blood vessel replacement (n = 5) and endovascular aortic repair (n = 16). Tse et al. [29] comprised cardiac surgery patients and patients undergoing percutaneous TAVI.
The impact of POD on length of hospital stay and long-term mortality
Three of the studies investigated the impact of POD on length of hospital stay. In the Kazmierski et al. [31] study, the patients who developed POD had a longer total duration of hospitalization (18 vs 15 days) compared to patients without POD. In the Tully et al. [32] study, patients with POD had longer hospital stay compared to patients without POD, but the difference was not statistically significant (P 0.13). Tse et al. [29] reported a prolonged hospital stay of 5 days for patients who developed POD. Tse et al. [29] was the only study reporting mortality. No difference was noticed in 1-year mortality between patients with POD compared to patients without POD.
Sex and gender aspects
In the overall results, more men than women underwent cardiac surgery which is in line with the current sex distribution among cardiac surgery patients [38]. The prevalence of POD according to sex was presented in 5 of the studies [29, 30, 32–34] with various results. In one of the studies [33], women were over-represented among the patients who developed POD. In the other 4 studies, however, [29, 30, 32, 34], men developed POD to a larger extent than women.
Preoperative depression and postoperative delirium
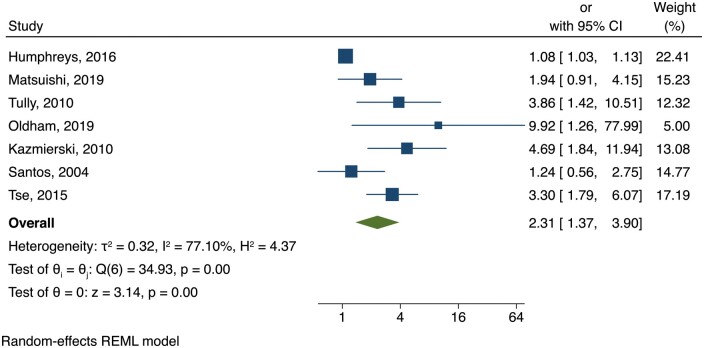
As presented in Fig. 2, the overall pooled OR for preoperative depression and POD was 2.31 (95% CI 1.37–3.90) according to a random-effects model with a high heterogeneity (I2 = 77.10%). Publication bias was assessed through the visual examination of a funnel plot (Fig. 3).
Figure 2:
Forest plot of preoperative depression and postoperative delirium following cardiac surgery.
Figure 3:
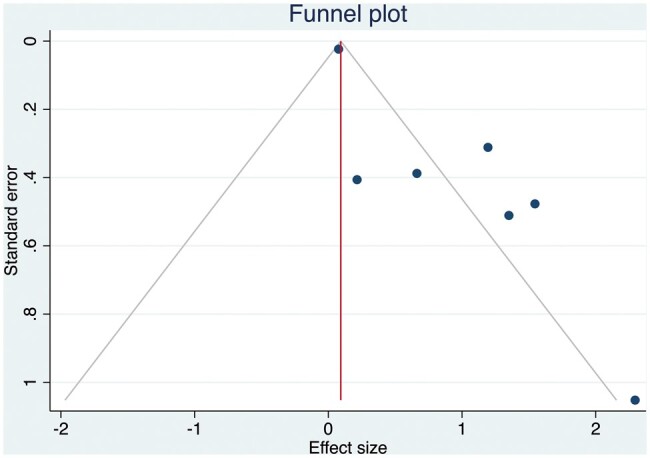
Publication bias was assessed through the visual examination of a funnel plot.
Sensitivity analysis
To measure the influence of separate studies on the primary outcome, a series of meta-analyses were carried out, omitting 1 study at a time. The results were robust with an OR between 2.06 (95% CI 1.20–3.51) and 2.78 (95% CI 1.76–4.40). When removing the largest study by Tse et al. [29] comprising 679 patients, the results changed slightly (OR 2.18, 95% CI 1.20–3.97). When omitting Humphreys et al. [30] the OR was 2.78 (95% CI 1.76–4.40) (Supplementary Material, Table S1).
Subgroup analysis
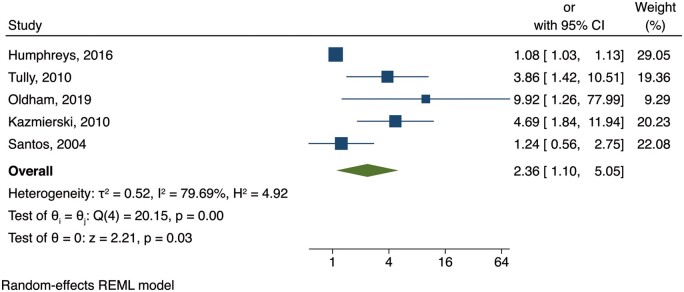
A pooled OR was calculated separately for studies that only included CABG patients. As shown in Fig. 4, the OR in this analysis was 2.36 (95% CI 1.10–5.05).
Figure 4:
In a subgroup analysis, the pooled estimates were calculated including studies of coronary artery bypass grafting surgery only using a random effects model.
DISCUSSION
In this systematic review and meta-analysis, preoperative depression was found to be a significant predictor of POD in patients treated with cardiac surgery, which confirms reports on other surgical patient groups. The correlation between depression and POD was significant even in a subgroup analysis that included studies of CABG patients only.
The definition of depression differed between the studies, as 6 of the studies [28, 30–34] defined preoperative depression using different questionnaires and 1 study [29] used ICD codes for depression. A meta-analysis is an objective evaluation and pooling of different study populations. Previous reports indicate an association between depression and POD, which is in line with the findings of this meta-analysis [39–42]. However, these previous reports have investigated POD after general surgery [39–42], not specifically cardiac surgery. Depression is common in patients with cardiac disease, but the association between depression and POD in cardiac surgery patients has been sparsely studied. Various studies report a POD prevalence of between 22% and 55% after cardiac surgery [4, 6, 7]. The pooled POD prevalence in the total study population was 26%. Adequate delirium assessment tools have been used throughout the majority of the studies [28–30, 32, 33], rendering the POD prevalence reliable. However, 2 studies [31, 33] reported a lower POD prevalence compared to the other studies. Possible explanations could be that the average age of the patients in these studies was relatively low and that assessment tools to detect POD were not used properly. Timing of assessment is important. To assess POD once a day is not sufficient to detect POD as the symptoms tend to fluctuate during the day.
Previous studies show that patients developing POD have worse long-term outcomes, such as increased length of hospital stay, more hospital readmissions, reduced quality of life, dementia and increased mortality [4, 6, 10, 13]. An equal aggravation of long-term outcomes and increased length of hospital stay have been demonstrated among patients with preoperative depression undergoing cardiac surgery [14, 15, 43]. It has been suggested that depression and delirium share common pathophysiological pathways [44]. Stress response systems such as the limbic-hypothalamic-pituitary-adrenal axis, inflammatory response and sympathetic nervous system are known to affect cognition, mood and motivation, increasing fatigue, anhedonia, reducing appetite [17] and an activated immune response with increased expression of inflammatory factors that activate pattern recognition receptors is strongly correlated with depression [18, 45]. Furthermore, it has been demonstrated that perioperative neurocognitive disorders, including POD, correlate with and originate in a neuroinflammation triggered by a systemic inflammatory activation [19, 46]. With common shared pathways, a correlation between depression and POD is plausible and should therefore be explored more in more detail. In this respect, cardiac surgery patients should be screened for depression prior to surgery in order to identify those high-risk patients who require preventive strategies to avoid developing POD [47]. Preventive interventions such as the use of antipsychotics, dexmedetomidine treatment and monitoring of bispectral index during anaesthesia can reduce the incidence and severity of POD in elderly patients undergoing elective surgery [48]. Furthermore, being aware of the increased risk of POD could motivate the healthcare staff to be particularly meticulous in exercising preventive caring activities such as using delirium assessment tools properly, reorienting the patient, providing good sleep hygiene, maintaining nutrition and hydration, offering therapeutic activities and cognitive stimulation, removing catheters and chest tubes as early as possible and focusing on early mobilization after surgery [5, 44, 49]. Delays in preventive caring activities can prolong POD, which is associated with worse functional and cognitive recovery and higher morbidity and mortality [49]. It is of value to increase the understanding about the complexity of POD to raise a more patient-centred approach regarding the increased risk of developing POD among cardiac surgery patients.
Depression screening is recommended by the American Heart Association for all patients scheduled for cardiac surgery [50]. Thus, screening for depression is one way of identifying patients at risk of POD and may be used together with other multi-disciplinary interventions during the preoperative phase to reduce the incidence and severity of POD [47]. Being aware of the strong association between depression and POD in cardiac patients emphasizes the importance of depression screening prior to cardiac surgery, as depression, besides predicting POD, is associated with worse postoperative outcomes, increased mortality and hospital readmission [3, 15, 43]. Even though women are depressed to a larger extent than men [2], men seem to develop POD more frequently than women. It has been hypothesized that depression is under-diagnosed in men [51]. The higher prevalence of POD among men might reflect this under-diagnosing. This emphasizes the importance of depression screening in both men and women.
Limitations
In this meta-analysis, data from 2.066 patients were collected. The relatively high number of patients and strict inclusion criteria represent a strength of this study. However, systematic reviews and meta-analyses are associated with various biases. To minimize the risk of bias, a strict study protocol and the STROBE checklist were used. Only cohort studies were included; the main limitation of observational studies is the non-randomization of exposure. As with any meta-analysis, there is a possibility that studies were missed during the literature search, or that studies observing no association between depression and POD never have been published (publication bias). The studies have a high heterogeneity primarily regarding the type of surgery that the patients underwent. This possible publication bias is visually demonstrated by a funnel plot. Two of the studies [28, 34] did not report adjusted ORs. Thus, unadjusted ORs were included in the meta-analysis. The variety in the used definitions of the diagnosis depression, mainly by using validated evaluation tools for depression (depression anxiety and stress scales, the Mini International Neuropsychiatric Interview, Depression Interview and Structured Hamilton, Hamilton Depression Rating Scale, Patient Health Questionnaire-9, Geriatric Depression Scale, Hospital Anxiety and Depression Scale) does introduce varying thresholds of the extent of disease, a misclassification of exposure. However, it is probable that by requesting such tools, an underestimation of the prevalence of depression is also plausible. Furthermore, information on the number of patients exposed (depressed) prior to surgery is missing in one of the studies [30]. Regarding POD, it was assessed multiple times a day in some of the studies and in others, only once a day. The assessment tools differed between the Delirium Symptom Interview, delirium index, CAM and the confusion assessment method for the ICU. In 2 of the studies [31, 34], no specific assessment tool was used. Instead, physicians set the diagnosis according to the DSM IV criteria for delirium. One study could not be included as the OR and number of events in the depressed versus non-depressed group were not presented [5].
CONCLUSION
The findings confirm a strong association between preoperative depression and POD, which is a common and costly condition in the postoperative care trajectory for cardiac patients. Findings emphasize the need for structured implementation of depression screening preoperatively in cardiac patients to identify high-risk patients and take multi-disciplinary pre- and postoperative intervention actions such as providing information to the patient, dexmedetomidine treatment, monitoring of bispectral index during anaesthesia, using delirium assessment tools properly, reorienting the patient, providing good sleep hygiene, maintaining nutrition and hydration, offering therapeutic activities and cognitive stimulation and removing catheters and chest tubes as early as possible after surgery. One could foresee improved quality of life in patients, better outcome and shorter hospital stay by such preoperative identifications, which needs to be confirmed in prospective trials.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank the librarians Carl Gornitzki and Sabina Gillsund at the Karolinska Institutet University Library for excellent help with the systematic literature search. They received no compensation for their contribution.
Funding
This work was supported by the Mats Kleberg Foundation grant number: 4-2953/2019 [to M.S.].
Conflict of interest: none declared.
Author contributions
Anna Falk: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Validation; Visualization; Writing—original draft; Writing—review & editing. Jessica Kåhlin: Conceptualization; Investigation; Methodology; Project administration; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing. Carolin Nymark: Conceptualization; Investigation; Methodology; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing. Rebecka Hultgren: Conceptualization; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing. Malin Stenman: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Vito Domenico Bruno, Milan Milojevic, Mate Petricevic and the other, anonymous reviewer(s) for their contribution to the peer-review process of this article.
Abbreviations
- CABG
Coronary artery bypass grafting
- CAM
Confusion assessment method
- CI
Confidence interval
- ICU
Intensive care unit
- OR
Odds ratios
- POD
Postoperative delirium
- TAVI
Transcatheter aortic valve implantation
These authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
REFERENCES
- 1. Spencer LJ, Degu A, Kalkidan HA, Solomon MA, Cristiana A, Nooshin A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry 2017;4:146–58. [DOI] [PubMed] [Google Scholar]
- 3. Celano CM, Huffman JC.. Depression and cardiac disease: a review. Cardiol Rev 2011;19:130–42. [DOI] [PubMed] [Google Scholar]
- 4. Nguyen Q, Uminski K, Hiebert BM, Tangri N, Arora RC.. Midterm outcomes after postoperative delirium on cognition and mood in patients after cardiac surgery. J Thorac Cardiovasc Surg 2018;155:660–7.e2. [DOI] [PubMed] [Google Scholar]
- 5. Detroyer E, Dobbels F, Verfaillie E, Meyfroidt G, Sergeant P, Milisen K.. Is preoperative anxiety and depression associated with onset of delirium after cardiac surgery in older patients? A prospective cohort study. J Am Geriatr Soc 2008;56:2278–84. [DOI] [PubMed] [Google Scholar]
- 6. Kotfis K, Szylińska A, Listewnik M, Strzelbicka M, Brykczyński M, Rotter I. et al. Early delirium after cardiac surgery: an analysis of incidence and risk factors in elderly (>/=65 years) and very elderly (>/=80 years) patients. Clin Interv Aging 2018;13:1061–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smulter N, Lingehall HC, Gustafson Y, Olofsson B, Engstrom KG.. Delirium after cardiac surgery: incidence and risk factors. Interact CardioVasc Thorac Surg 2013;17:790–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5 (R)). 5th edn. Arlington, VA: American Psychiatric Association, 2013. 10.1176/appi.books.9780890425596.
- 9. Evans AS, Weiner MM, Arora RC, Chung I, Deshpande R, Varghese R. et al. Current approach to diagnosis and treatment of delirium after cardiac surgery. Ann Card Anaesth 2016;19:328–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Koster S, Hensens AG, Schuurmans MJ, van der Palen J.. Consequences of delirium after cardiac operations. Ann Thorac Surg 2012;93:705–11. [DOI] [PubMed] [Google Scholar]
- 11. Zhang WY, Wu WL, Gu JJ, Sun Y, Ye XF, Qiu WJ. et al. Risk factors for postoperative delirium in patients after coronary artery bypass grafting: a prospective cohort study. J Crit Care 2015;30:606–12. [DOI] [PubMed] [Google Scholar]
- 12. Hollinger A, Siegemund M, Goettel N, Steiner LA.. Postoperative delirium in cardiac surgery: an unavoidable menace? J Cardiothorac Vasc Anesth 2015;29:1677–87. [DOI] [PubMed] [Google Scholar]
- 13. Brown CH. Delirium in the cardiac surgical ICU. Curr Opin Anaesthesiol 2014;27:117–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stenman M, Holzmann MJ, Sartipy U.. Relation of major depression to survival after coronary artery bypass grafting. Am J Cardiol 2014;114:698–703. [DOI] [PubMed] [Google Scholar]
- 15. Stenman M, Holzmann MJ, Sartipy U.. Association between preoperative depression and long-term survival following coronary artery bypass surgery—a systematic review and meta-analysis. Int J Cardiol 2016;222:462–6. [DOI] [PubMed] [Google Scholar]
- 16. Blumenthal JA, Lett HS, Babyak MA, White W, Smith PK, Mark DB. et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet 2003;362:604–9. [DOI] [PubMed] [Google Scholar]
- 17. Maclullich AM, Ferguson KJ, Miller T, de Rooij SE, Cunningham C.. Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses. J Psychosom Res 2008;65:229–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Franklin TC, Wohleb ES, Zhang Y, Fogaca M, Hare B, Duman RS.. Persistent increase in microglial RAGE contributes to chronic stress-induced priming of depressive-like behavior. Biol Psychiatry 2018;83:50–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Danielson M, Wiklund A, Granath F, Blennow K, Mkrtchian S, Nellgard B. et al. Neuroinflammatory markers associate with cognitive decline after major surgery: findings of an explorative study. Ann Neurol 2020;87:370–82. [DOI] [PubMed] [Google Scholar]
- 20. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Buccheri S, Sodeck GH, Capodanno D.. Statistical primer: methodology and reporting of meta-analyses. Eur J Cardiothorac Surg 2018;53:708–13. [DOI] [PubMed] [Google Scholar]
- 22. Hickey GL, Dunning J, Seifert B, Sodeck G, Carr MJ, Burger HU. et al. Statistical and data reporting guidelines for the European Journal of Cardio-Thoracic Surgery and the Interactive CardioVascular and Thoracic Surgery. Eur J Cardiothorac Surg 2015;48:180–93. [DOI] [PubMed] [Google Scholar]
- 23. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- 24. Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F. et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 2015;8:2–10. [DOI] [PubMed] [Google Scholar]
- 25. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ. et al. (eds). Cochrane Handbook for Systematic Reviews and Interventions. 2nd edn. Chichester: John Wiley and Sons, 2019. [Google Scholar]
- 27. Quaranta, L. STATA programs for using the intermediate data structure (IDS) to construct files for statistical analysis. Hist Life Course Stud 2016;3:1–19. [Google Scholar]
- 28. Matsuishi Y, Shimojo N, Unoki T, Sakuramoto H, Tokunaga C, Yoshino Y. et al. Type D personality is a predictor of prolonged acute brain dysfunction (delirium/coma) after cardiovascular surgery. BMC Psychol 2019;7:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tse L, Schwarz SK, Bowering JB, Moore RL, Barr AM.. Incidence of and risk factors for delirium after cardiac surgery at a quaternary care center: a retrospective cohort study. J Cardiothorac Vasc Anesth 2015;29:1472–9. [DOI] [PubMed] [Google Scholar]
- 30. Humphreys JM, Denson LA, Baker RA, Tully PJ.. The importance of depression and alcohol use in coronary artery bypass graft surgery patients: risk factors for delirium and poorer quality of life. J Geriatr Cardiol 2016;13:51–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kazmierski J, Kowman M, Banach M, Fendler W, Okonski P, Banys A. et al. Incidence and predictors of delirium after cardiac surgery: results from The IPDACS Study. J Psychosom Res 2010;69:179–85. [DOI] [PubMed] [Google Scholar]
- 32. Tully PJ, Baker RA, Winefield HR, Turnbull DA.. Depression, anxiety disorders and Type D personality as risk factors for delirium after cardiac surgery. Aust N Z J Psychiatry 2010;44:1005–11. [DOI] [PubMed] [Google Scholar]
- 33. Oldham MA, Hawkins KA, Lin IH, Deng Y, Hao Q, Scoutt LM. et al. Depression predicts delirium after coronary artery bypass graft surgery independent of cognitive impairment and cerebrovascular disease: an analysis of the neuropsychiatric outcomes after heart surgery study. Am J Geriatr Psychiatry 2019;27:476–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Santos FS, Velasco IT, Fraguas R Jr.. Risk factors for delirium in the elderly after coronary artery bypass graft surgery. Int Psychogeriatr 2004;16:175–93. [PubMed] [Google Scholar]
- 35. Albert MS, Levkoff SE, Reilly C, Liptzin B, Pilgrim D, Cleary PD. et al. The delirium symptom interview: an interview for the detection of delirium symptoms in hospitalized patients. J Geriatr Psychiatry Neurol 1992;5:14–21. [DOI] [PubMed] [Google Scholar]
- 36. Smulter N, Lingehall HC, Gustafson Y, Olofsson B, Engstrom KG.. Validation of the confusion assessment method in detecting postoperative delirium in cardiac surgery patients. Am J Crit Care 2015;24:480–7. [DOI] [PubMed] [Google Scholar]
- 37. McCusker J, Cole MG, Dendukuri N, Belzile E.. The delirium index, a measure of the severity of delirium: new findings on reliability, validity, and responsiveness. J Am Geriatr Soc 2004;52:1744–9. [DOI] [PubMed] [Google Scholar]
- 38.Swedeheart. Årsrsapport 2018. 2019. https://www.ucr.uu.se/swedeheart/dokument-sh/arsrapporter-sh/1-swedeheart-annual-report-2019/download
- 39. Elsamadicy AA, Adogwa O, Lydon E, Sergesketter A, Kaakati R, Mehta AI. et al. Depression as an independent predictor of postoperative delirium in spine deformity patients undergoing elective spine surgery. J Neurosurg Spine 2017;27:209–14. [DOI] [PubMed] [Google Scholar]
- 40. McGuire JM. The incidence of and risk factors for emergence delirium in U.S. military combat veterans. J Perianesth Nurs 2012;27:236–45. [DOI] [PubMed] [Google Scholar]
- 41. Greene NH, Attix DK, Weldon BC, Smith PJ, McDonagh DL, Monk TG.. Measures of executive function and depression identify patients at risk for postoperative delirium. Anesthesiology 2009;110:788–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Smith PJ, Attix DK, Weldon BC, Greene NH, Monk TG.. Executive function and depression as independent risk factors for postoperative delirium. Anesthesiology 2009;110:781–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Stenman M, Holzmann MJ, Sartipy U.. Antidepressant use before coronary artery bypass surgery is associated with long-term mortality. Int J Cardiol 2013;167:2958–62. [DOI] [PubMed] [Google Scholar]
- 44. Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Audisio R, Borozdina A. et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 2017;34:192–214. [DOI] [PubMed] [Google Scholar]
- 45. Franklin TC, Xu C, Duman RS.. Depression and sterile inflammation: essential role of danger associated molecular patterns. Brain Behav Immun 2018;72:2–13. [DOI] [PubMed] [Google Scholar]
- 46. Forsberg A, Cervenka S, Jonsson Fagerlund M, Rasmussen LS, Zetterberg H, Erlandsson Harris H. et al. The immune response of the human brain to abdominal surgery. Ann Neurol 2017;81:572–82. [DOI] [PubMed] [Google Scholar]
- 47. Raats JW, Steunenberg SL, de Lange DC, van der Laan L.. Risk factors of post-operative delirium after elective vascular surgery in the elderly: a systematic review. Int J Surg 2016;35:1–6. [DOI] [PubMed] [Google Scholar]
- 48. Janssen TL, Alberts AR, Hooft L, Mattace-Raso F, Mosk CA, van der Laan L.. Prevention of postoperative delirium in elderly patients planned for elective surgery: systematic review and meta-analysis. Clin Interv Aging 2019;14:1095–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sharon KI, Tom R, Caroline B, Jan B-W, Malaz B, Ara C, et al. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc 2015;63:142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sowden G, Mastromauro CA, Januzzi JL, Fricchione GL, Huffman JC.. Detection of depression in cardiac inpatients: feasibility and results of systematic screening. Am Heart J 2010;159:780–7. [DOI] [PubMed] [Google Scholar]
- 51. Thunander Sundbom L, Bingefors K, Hedborg K, Isacson D.. Are men under-treated and women over-treated with antidepressants? Findings from a cross-sectional survey in Sweden. BJPsych Bull 2017;41:145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.