Abstract
OBJECTIVES
Our goal was to evaluate the impact of the adult congenital heart disease anatomical and physiological (ACHD AP) classification system on the surgical management of Ebstein anomaly (EA) in adult patients.
METHODS
From February 2000 through August 2017, data of patients aged at least 16 years, who underwent primary EA surgery, were retrospectively evaluated. The cohort was divided in 2 groups according to their ACHD AP classification: the moderate EA group (IIB, IIC) and the severe EA group (IID). Survival, freedom from reoperation and freedom from occurrence of major adverse advents were estimated.
RESULTS
There were 33 patients (21 women, 12 men). Eighteen belonged to the moderate group, 15 to the severe group. There were 12 female patients (80%) in the severe group. Patients in the moderate group were younger than those in the severe group (P = 0.02): 32 ± 12 vs 44 ± 15 years old. Thirty tricuspid valve repairs and 3 replacements were performed. Repair was mainly performed in the moderate group (P = 0.02). Overall survival was 90.1 ± 5.4% at 9 months after the operation and did not change in the later follow-up period. It was 100% for patients in the moderate group and 80.0 ± 10.3% in the severe group (P = 0.07), and 75.0 ± 12.5% for female patients of in the severe group compared to 100% for the remaining patients (P = 0.025). Survival free from major adverse events, including reoperation, at 10 years was 60.0 ± 12.6% in the moderate and 38.1% ± 12.9% in the severe group (P = 0.03). No patient in the moderate group evolved to be in the severe group at late follow-up.
CONCLUSION
Adult EA patients should undergo surgery earlier when they are still in the moderate ACHD AP classification.
Keywords: Ebstein anomaly, Adult congenital heart disease, Adult congenital heart disease anatomical and physiological classification, Adult congenital heart disease surgery, Operative outcomes
INTRODUCTION
The Ebstein anomaly (EA) is a rare congenital heart malformation involving the tricuspid valve. Its incidence per million live births was estimated by Hoffman and Kaplan to be 114 [1].
Four types have been described by Carpentier et al. [2], based on displacement of the posterior and septal leaflets of the tricuspid valve and the size of the right ventricle:
Type A: the posterior and the septal leaflets are dislocated in the direction of the right ventricle, the anterior leaflet is enlarged and mobile and a small part of the ventricle is atrialized.
Type B: a large part of the ventricle is atrialized and the anterior leaflet is mobile and enlarged.
Type C: in addition to having the morphological features of type B, the anterior leaflet is restrictive.
Type D: the right ventricle is almost completely atrialized and has a limited function (tricuspid sac).
Severe cases of Ebstein malformation present during the neonatal period with cyanosis and heart failure. Most patients present in infancy or childhood with a murmur, heart failure, cyanosis or arrhythmia; a few present as an adolescent or an adult with exercise intolerance [3]. Urgent surgery is usually required in symptomatic newborns. At other ages, an operation is usually indicated by progressive heart failure, increasing cyanosis and arrhythmias immune to medical treatment.
Several surgical modalities are applied to manage the EA: repair or replacement of the tricuspid valve, systemic-to-pulmonary shunt and partial or total univentricular palliation. In addition, repair of concomitant lesions and antiarrhythmic procedures are performed occasionally. Overall neonatal operative mortality is high: 27.4% in the series from the Society of Thoracic Surgeons Congenital Heart Surgery Database [4]. Operative risk in adults depends on their preoperative clinical condition and on the kind of surgical procedure that is carried out.
The new adult congenital heart disease anatomical and physiological (ACHD AP) classification [5] system defines EA as a lesion of anatomically moderate complexity (anatomical type II). A recent publication showed that such anatomical cardiac malformations carried an operative mortality risk varying from 1% (0.69–1.37%) in the physiologically lowest level of severity (IIA), to 5% (3.05–7.91%) in the highest level of severity (IID) [6].
Medical management and observation are often recommended for mildly/moderately symptomatic patients and are believed to be successful for many years. This study evaluates the possible impact of the ACHD AP classification system on this ‘wait-and-see’ strategy before surgical management.
METHODS
This is a single-centre, clinical, retrospective study of the surgical management of EA. This study was approved by the local institutional ethics committee: reference number EA2/256/18.
Data of all patients aged at least 16 years who underwent surgical treatment from February 2000 through August 2017 were analysed. Patients previously operated on for this malformation were excluded.
Demographic, clinical, echocardiographic and surgical (preoperative, operative and postoperative) findings were compiled. The last follow-up included a check-up in our department or an answered questionnaire. The occurrence of postoperative major complications was noted. They were defined as any 1 or more of the following 6 events [7]: (i) postoperative acute renal failure requiring temporary or permanent dialysis; (ii) postoperative neurological deficit persisting at discharge; (iii) postoperative atrioventricular block requiring a permanent pacemaker; (iv) postoperative mechanical circulatory support; (v) phrenic nerve injury/paralyzed diaphragm; and (vi) unplanned reoperation or catheter intervention. Subsequent reoperations and episodes during the follow-up period of myocardial infarction, cerebrovascular accident and infective endocarditis were recorded as major adverse events. Early survival was defined as survival until discharge from the hospital or within 30 days after the operation.
The patients were grouped according to their preoperative physiological condition in conformity with the ACHD AP classification [5]. Physiological variables included aortopathy, arrhythmia, concomitant valvular heart disease, end-organ dysfunction, exercise capacity, hypoxaemia/hypoxia/cyanosis, New York Heart Association functional class, pulmonary hypertension, a haemodynamically significant shunt and venous and aortic stenosis. Details are given in the appendix as supplemental material.
The clinical condition of patients presenting with physiological status B and C was defined as ‘moderate’. It was designed as ‘severe’ in the presence of D physiological features.
The primary end-point of this study was a comparison of postoperative early and late survival for the 2 groups of patients in the moderate and severe physiological conditions. Secondary end-points were incidence of postoperative major complications and, in the follow-up period, survival free from major adverse events and evolution of ACHD AP classes.
Groups were compared using the Student’s t-test, Fisher’s exact test and McNemar’s test, as indicated. Late survival and freedom from events were estimated according to the Kaplan–Meier method; the log-rank test (Mantel–Cox test) was used to compare curves. Means are given with standard deviations (SD). Normality was determined by the Shapiro–Wilk test. For statistical analyses, SPSS for Windows (Version 25, IBM, Armonk, NY, USA) was utilized. The statistical significance level was set at P < 0.05 and the confidence interval, at 95%.
RESULTS
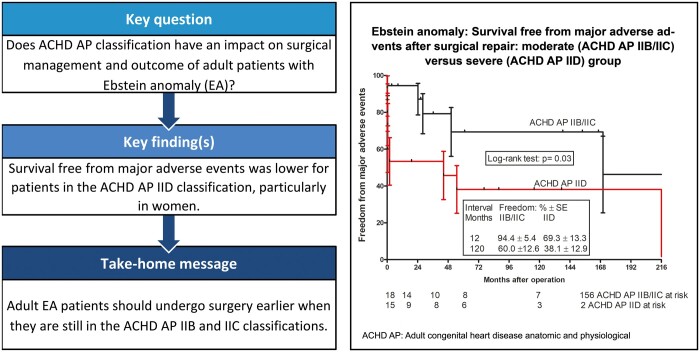
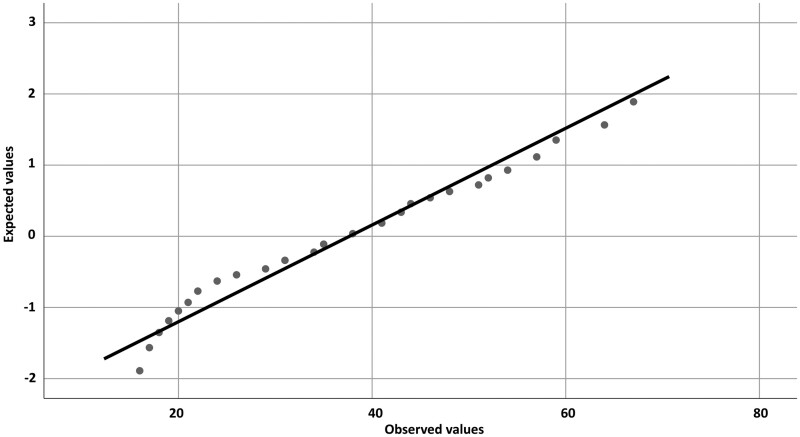
Forty-two patients were operated on for EA in the period from February 2000 to August 2017. Nine were excluded because they previously underwent a surgical procedure for this malformation. Therefore, 33 patients were included in this study. Their mean age at the time of the operation was 38 years with a SD of 15 years. Confirmation of the normal age distribution at the time of the operation is shown graphically in Fig. 1. All continuous variables included in this study passed the Shapiro–Wilk normality test.
Figure 1:
Graphical confirmation of the normal distribution of patients’ ages at the time of the operation. The graph is a quantile–quantile plot of the standardized data against the standard normal distribution. The points plotted in the graph fall approximately on a straight line, indicating high positive correlation.
Grouping and preoperative characteristics
Variables leading to classification in different ACHD AP classes are detailed in Table 1. Among the 33 patients, 7 belonged in class IIB, 11 in IIC and 15 in IID. Therefore, 18 cases were categorized as the EA moderate group and 15, as the EA severe group.
Table 1:
Variables of the adult congenital heart disease anatomical and physiological classification system
| II B | II C | II D | |
|---|---|---|---|
| NYHA FC II symptoms, mild valvular disease | 7 | ||
| NYHA FC II symptoms, mild valvular disease, moderate hypoxaemia, cyanosis | 1 | ||
| NYHA FC II symptoms, moderate valvular disease | 2 | ||
| NYHA FC II symptoms, arrhythmia requiring treatment, mild valvular disease | 1 | ||
| NYHA FC II symptoms, moderate valvular disease, cyanosis | 1 | ||
| NYHA FC III symptoms, moderate valvular disease | 4 | ||
| NYHA FC III symptoms, arrhythmia requiring treatment, moderate valvular disease | 2 | ||
| NYHA FC II symptoms, moderate hypoxaemia, cyanosis, moderate valvular disease, refractory kidney failure immune | 1 | ||
| NYHA FC III symptoms, arrhythmia refractory to treatment, greater valvular disease, haemodynamically significant shunt | 1 | ||
| NYHA FC III symptoms, severe hypoxaemia, moderate valvular disease, haemodynamically significant shunt | 1 | ||
| NYHA FC IV symptoms, severe hypoxaemia, greater valvular disease, arrhythmia requiring treatment | 1 | ||
| NYHA FC IV symptoms, arrhythmia refractory to treatment, greater valvular disease | 4 | ||
| NYHA FC IV symptoms, moderate hypoxaemia, cyanosis, arrhythmia requiring treatment, greater valvular disease, haemodynamically significant shunt | 1 | ||
| NYHA FC IV symptoms, cyanosis, greater valvular disease | 2 | ||
| NYHA FC IV symptoms, greater valvular disease, haemodynamically significant shunt | 1 | ||
| NYHA FC IV symptoms, moderate hypoxaemia, cyanosis, moderate valvular disease | 1 | ||
| NYHA FC IV symptoms, severe hypoxaemia, cyanosis, arrhythmia requiring treatment, greater valvular disease | 1 | ||
| NYHA FC IV symptoms, severe hypoxaemia, cyanosis, greater valvular disease, haemodynamically significant shunt | 1 |
NYHA FC: New York Heart Association functional class.
Twenty-one patients (64%) were women and 12 of these (80%) were in the severe group (Table 2). Patients in the moderate group were younger than those in the severe group (P = 0.02): 32 (SD = 12) vs 44 (SD = 15) years old. Re-partition of Carpentier types was similar: P = 0.60. In particular, there were 5 with Carpentier type C in the moderate group and 7 in the severe group. This re-partition did not change during the study period: P = 0.94.
Table 2:
General characteristics of the cohorts
| Characteristics | Moderate EA (n = 18) | Severe EA (n = 15) | P-value |
|---|---|---|---|
| Male/female | 9/9 | 3/12 | 0.145 |
| Age (years) | 32.44 ± 12.16 | 43.93 ± 15.44 | 0.023 |
| Body mass index | 23.37 ± 2.74 | 24.79 ± 4.03 | 0.24 |
| Carpentier type A | 5 | 1 | 0.60* |
| Carpentier types A and B | 1 | 0 | |
| Carpentier type B | 3 | 2 | |
| Carpentier types B and C | 0 | 2 | |
| Carpentier type C | 5 | 7 | |
| Carpentier types C and D | 1 | 1 | |
| Carpentier type D | 1 | 1 | |
| Carpentier type unclear | 2 | 1 |
EA: Ebstein anomaly.
P-value for re-partition of Carpentier types.
Patients in the severe group presented more often with cyanosis. Arrhythmia affected both groups similarly. Atrial septal defect was frequently associated (n = 26, 79%) with EA in the cohort. Ventricular septal defect was also present in 2 cases, as was partial anomalous pulmonary venous connection in 1 case. Re-partition among both EA groups with these concomitant anomalies was similar: P = 0.60.
Surgical procedures and cardiopulmonary bypass data
A total of 30 tricuspid valve repairs were performed. They comprised different methods of annuloplasty (n = 16) and the Sebening procedure (n = 9) in the early period under review and the Cone procedure (n = 5) as of 2013. The tricuspid valve was replaced in 3 patients with the biological St. Jude Medical (n = 2) prosthesis and 1 Hancock prosthesis.
An antiarrhythmic procedure was used in 6 cases: the Maze procedure (n = 4) and ablation at the atrial level (n = 2). Twenty-two of the 26 associated atrial septal defects were closed. The Glenn procedure was added on 5 occasions: 2 after tricuspid valve annuloplasty, 2 after valve replacement and 1 after the Cone procedure. As shown in Table 3, tricuspid valve repair as the sole procedure was performed more frequently in the moderate EA group (n = 16) than in the severe group (n = 7) (P = 0.02).
Table 3:
Main surgical procedures
| Main surgical procedure | Moderate EA | Severe EA | Total |
|---|---|---|---|
| Tricuspid valve replacement | 3 | ||
| + Glenn procedure | 1 | 0 | 1 |
| + Antiarrhythmia procedure | 0 | 1 | 1 |
| + Glenn procedure + antiarrhythmia procedure | 0 | 1 | 1 |
| Tricuspid valve repair | 30 | ||
| Sole* | 16 | 7 | 23 |
| + Glenn procedure | 0 | 2 | 2 |
| + Antiarrhythmia procedure | 1 | 3 | 4 |
| + Glenn procedure + antiarrhythmia procedure | 0 | 1 | 1 |
EA: Ebstein anomaly.
P-value = 0.02.
Cardiopulmonary bypass and aortic cross-clamping lasted in the moderate EA group 109 ± 81 and 64 ± 57 min, respectively. These procedures lasted 156 ± 218 and 54 ± 19 min, respectively, in the severe group. The differences were not statistically different (P-values: 0.4 and 0.6).
Early postoperative outcomes
Two patients died early after the operation: The early mortality was 6% (95% CI: 0.74–20.2%). Both were women and both belonged to the severe group. The first patient had undergone tricuspid valve repair and needed a pacemaker because she had heart block and a univentricular assist device for 3 days to overcome cardiogenic shock. She died 1 month after the operation of ventricular fibrillation. The second deceased patient similarly presented with poor cardiac function, postoperative heart block and arrhythmias after surgery. The cause of death was also ventricular fibrillation 1 month after surgery. The difference in early mortality between the 2 EA groups was, however, not statistically significant: P = 0.20.
One patient in the moderate group and 6 patients belonging to the severe group had at least 1 major postoperative complication (Table 4): a significantly different postoperative morbidity: P = 0.03. One early valve re-repair was required. The most frequent complication was heart block requiring a permanent pacemaker implant, which occurred overall 6 times, but only once in the moderate group. It was observed in 3 cases after tricuspid valve annuloplasty and on 3 occasions after the Sebening procedure.
Table 4:
Postoperative major complications within 30 days after surgery
| Complications | Moderate EA | Severe EA |
|---|---|---|
| Neurological deficit | 0 | 2 |
| A-V block + PM implant | 1 | 5 |
| Sick sinus + PM Implant | 0 | 1 |
| Mechanical circulatory support | 0 | 1 |
| Tricuspid valve reoperation | 0 | 1 |
| Total* | 1 | 6a |
A-V: atrioventricular; EA: Ebstein anomaly; PM: pacemaker.
Four patients with severe EA experienced 2 postoperative major complications.
P-value = 0.03.
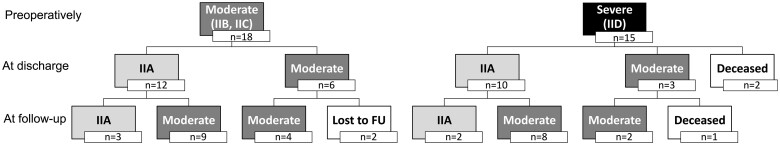
The hospital stay was 11 days (SD = 5 days) for patients with moderate EA. It was significantly longer for those with severe EA: 19 days (SD = 14 days); P-value = 0.03. At the time of discharge from the hospital, the survivors were in ACHD AP class IIA (n = 22), IIB (n = 8) and IIC (n = 1) (Fig. 2).
Figure 2:
Physiological evolution of adult congenital heart disease anatomical and physiological moderate and severe groups. Follow-up diagram depicting the physiological evolution of patients, starting from the preoperative condition (first line), continuing with postoperative status (second line) and ending with the adult congenital heart disease anatomical and physiological grouping at the time of the last follow-up (third line). FU: follow-up.
Late survival and freedom from adverse events
One woman from the severe group died 8 months after the first operation. She had already undergone an unplanned reoperation 16 days after the first procedure (tricuspid valve re-repair and a pacemaker implant due to a complete heart block). The cause of death in this case is unknown.
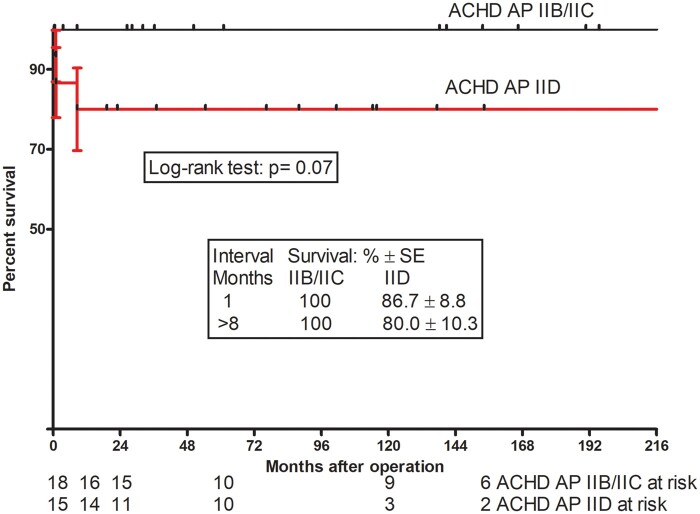
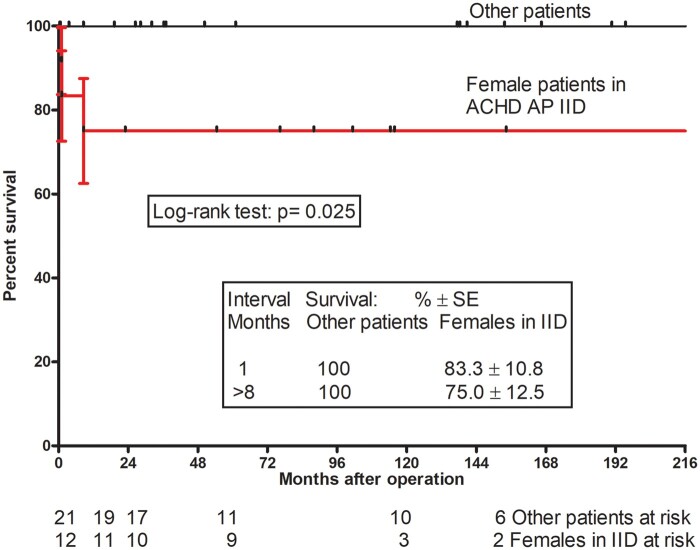
Survival for the whole cohort was 90.1% [standard error (SE) = 5.4%] at 9 months after the operation and did not change in the later follow-up period. It was 100% for the patients in the moderate group and 80.0% (SE = 10.3%) in the severe group (Fig. 3): The difference in survival did not reach the level of statistical significance: P = 0.07. It was 75.0% (SE = 12.5%) for female patients in the severe group and 100% for the remaining patients (female patients in moderate group + male patients), a significant difference: P = 0.025 (Fig. 4).
Figure 3:
Survival after repair of Ebstein anomaly: moderate (adult congenital heart disease anatomical and physiological IIB/IIC) versus severe (adult congenital heart disease anatomical and physiological IID) group. Kaplan–Meier survival curve after repair of Ebstein anomaly. Percent survival in the severe group was lower (albeit not statistically significant) than % survival in the mild group: log-rank test: P = 0.07. Vertical bars present standard errors. ACHD AP: adult congenital heart disease anatomical and physiological; SE: standard error.
Figure 4:
Postoperative survival of female patients in the adult congenital heart disease anatomical and physiological severe physiological group (IID) compared with survival of other patients. The Kaplan–Meier curve for postoperative survival of female patients in the adult congenital heart disease anatomical and physiological severe physiological group (IID) compared with the survival of other patients. Survival of female patients in the adult congenital heart disease anatomical and physiological IID group was significantly lower: log-rank test: P = 0.025. Vertical bars present standard errors. ACHD AP: adult congenital heart disease anatomical and physiological.
Two of the 31 early survivors were lost to follow-up. For the remaining 28 late survivors who could be traced, the mean duration of follow-up was 101 months (SD = 95 months) (median = 95 months). Seven patients underwent reoperations. The tricuspid valve was replaced in 2 patients in the severe EA group. It was re-repaired in 2 cases of moderate EA. Valvuloplasty was associated with a Glenn procedure in both patients and also with a Maze procedure in 1 case.
Overall, 5 patients had pacemaker implants during the follow-up period. They were carried out late after tricuspid valve annuloplasty in 3 cases, after the Sebening procedure in 1 patient and after tricuspid valve replacement in 1 case. One patient had sick sinus syndrome, and 1 patient had an implantable cardioverter-defibrillator implant because of recurrent ventricular tachyarrhythmia.
Survival free from reoperation at the 10-year follow-up for patients in the moderate EA group was somewhat higher compared to those in the severe group: 71.9% (SE = 12.1%) vs 45.7% (SE = 13.10%), but the difference did not reach statistical difference: P = 0.07.
One patient in the severe EA group had a neurological deficit (cerebral infarction in the left middle cerebral artery, hemiparesis). No episodes of infective endocarditis or of myocardial infarction occurred during the follow-up period. Survival free from major adverse event from the day of operation onwards is depicted in the Central Image. At 10 years, it was 60.0% (SE = 12.6%) for the moderate EA group, which was higher than the 38.1% (SE = 12.9%) for patients affected by the severe form of EA: P = 0.03.
Clinical status and adult congenital heart disease anatomic and physiological class at the last follow-up
The mean age of the 28 patients at the time of follow-up was 49 years (SD = 22 years). Five patients presented in ACHD AP IIA, 19 in IIB and 4 in IIC class. Therefore, 23 patients belonged to the moderate EA (IIB, IIC) group. Five enjoyed the best physiological condition of IIA class.
Figure 2 depicts how patients evolved clinically after the operation. In the moderate group, 3 patients evolved to be currently in class IIA; the other 13 stayed in the moderate IIB/IIC classes after the operation. Overall, 2 patients from the severe group improved to be in class IIA and 10, to be in moderate IIB/IIC classes over time. One female patient, currently in class IIC, has been listed for a heart transplant.
DISCUSSION
The timing of surgery in adult patients with EA is still uncertain. A wait-and-see approach is usually recommended for those with mild/moderate symptoms. So far, no age limit for intervention in mildly/moderately symptomatic patients has been set or proposed.
There is general agreement that an operation should be advised before significant right ventricular dysfunction occurs, which is not always easy to ascertain. Brown et al. [8], in 1 of the largest series of neonates and adults (539 patients), assumed that preoperative cyanosis and lower right and left ventricular systolic function predict a higher postoperative mortality and are important considerations when considering a surgical procedure. We relied on the new ACHD AP classification and divided the EA cohort into a moderate and a severe group, which may be the right choice when considering surgery. Ombelet et al. [9], using this classification, just showed that the probability of death after surgery for moderate heart defects increased in relation to the physiological status at the 15-year follow-up. EA is classified as being of moderate anatomical complexity (II). The impact of the ACHD AP classification on the EA postoperative outcome was therefore expected.
ACHD AP class IIC indicates a need for surgery. The timing of surgical intervention is still debated for patients in class IIB, even if a number of contemporary surgical teams would accept them for a Cone procedure. But postoperative outcomes of patients in classes IIB and IIC, grouped as moderate, were similar. Early and late survival was 100%. Patients had fewer postoperative complications (P = 0.03), had shorter stays in the hospital (P = 0.03) and enjoyed higher survival free from major adverse advents (P = 0.03) than patients affected by severe physiological EA (IID).
It is known that a better preoperative condition results in a better outcome. The ACHD AP classification carries the advantage of summarizing parameters that are often used to indicate surgery for EA. Concomitant valvular heart disease, exercise capacity, cyanosis, New York Heart Association functional class and a haemodynamically significant shunt are included. Grade of tricuspid valve insufficiency, oxygen saturation and exercise capacity testing by spiroergometry were therefore not specifically referred to in this study.
The finding of worse outcomes for female patients presenting with severe physiological EA raises questions. All 3 deceased patients were women in the severe EA group, and survival was much lower (P = 0.025) (see Fig. 4). This new result needs to be confirmed by further observation and studies. We could not find any report in the literature to corroborate this finding. We do not have any factors that could explain such an unfavourable outcome.
The younger age of patients in the moderate EA group (P = 0.023) is noteworthy: They were in their 30s. Age at surgery was a strong (P = 0.007) univariate predictor of death during the follow-up period in the series of Attenhofer et al. [10] of 81 patients with EA operated on when they were at least 50 years old. The 20-year survival was 65% vs 74% for age- and sex-matched controls (P = 0.001). Given the better outcome enjoyed by the moderate EA group in our study, 1 may consider advocating surgery earlier for moderately symptomatic patients, i.e. before the age of 40. This recommendation may apply specifically to female patients. This endorsement remains pertinent considering that younger age was associated with a higher rate of tricuspid valve repair (P = 0.02), a fact noted by other groups [11]. No patient presenting preoperatively in a moderate group evolved to be in the severe group in late follow-up.
This retrospective study essentially used the ACHD AP classification system to help guide surgical indications and the timing of repair. We did not have the goal of discussing the role of various procedures involved in EA surgery. The study covers a long period during which different techniques were used to repair the tricuspid valve. In the later study period, we were unable to assess in particular the implementation of alternative strategies, such as placing a bidirectional cavopulmonary anastomosis or leaving a restrictive atrial-level shunt in order to unload a deficient right ventricle, in patients belonging to class IID. The high incidence of complete AV block requiring pacemaker implants that occurred after annuloplasty and the Sebening procedure is noteworthy. This complication was not observed after the Cone procedure, which was performed beginning with the year 2013. An arrhythmia substrate prior to tricuspid valve repair has been identified in ∼70% of patients by Shivapour et al. [12]. Rhythm disturbances are a problem in long-term follow-up, and sudden death presumably related to arrhythmia has been reported [13].
Limitations
A relatively small number of patients with EA were included in our single-centre study, which prohibited us from correcting for potential confounders. The small number of events also prevented us from performing a multivariable analysis. Female gender is known to be more frequently affected by EA, which might explain the unequal distribution of female patients in different classes of the ACHD AP classification system. It was inevitable that some data were missing due to the retrospective nature of this study. In particular, echocardiographic data such as left ventricular function and right atrium surface were missing in patients who had operations from 2000 to 2008. Therefore, the Great Ormond Street Echocardiography score could not be estimated [14]. We relied on the re-partition of Carpentier types, which was similar for both moderate and severe groups. The differences in outcomes between tricuspid valve repair and replacement also could not be estimated, because only 3 patients underwent valve replacement. The mortality score based on the ACHD AP classification is new and needs validation. The proposition to indicate surgery before the age of 40 for mildly/moderately symptomatic patients, although suggested by the study, is empirical.
CONCLUSION
The ACHD AP classification system provides important hints for risk stratification and outcomes after repair of EA in adult patients. Patients with EA should undergo surgery earlier, when they are still in a moderate ACHD AP condition. Larger scale, possibly multicentric studies are needed to confirm suggestions set forth in this study using a multivariable analysis.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
Author contributions
Laura Homzova: Conceptualization; Data curation; Formal analysis; Writing—original draft. Joachim Photiadis: Supervision; Validation; Writing—review & editing. Nicodème Sinzobahamvya: Formal analysis; Validation; Writing—original draft; Writing—review & editing. Stanislav Ovroutski: Supervision; Validation. Mi-Young Cho: Data curation. Antonia Schulz: Data curation; Validation; Writing—review & editing.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks the anonymous reviewers for their contribution to the peer review process of this article.
Supplementary Material
ABBREVIATIONS
- ACHD AP
Adult congenital heart disease anatomical and physiological
- EA
Ebstein anomaly
- SD
Standard deviation
- SE
Standard error
REFERENCES
- 1. Hoffman JIE, Kaplan S.. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890–900. [DOI] [PubMed] [Google Scholar]
- 2. Carpentier A, Chauvaud S, Mace L, Relland J, Mihaileanu S, Marino JP. et al. A new reconstructive operation for Ebstein’s anomaly of the tricuspid valve. J Thorac Cardiovasc Surg 1988;96:92–101. [PubMed] [Google Scholar]
- 3. O’Learly PW, Dearini JA, Anderson RH, Spicer DE, Srivastana D.. Diseases of the tricuspid valve. In W Gil (ed). Anderson’s Pediatric Cardiology, 4th edn; Philadelphia: Elsevier, 2019, 585–603. [Google Scholar]
- 4. Holst KA, Dearani JA, Said SM, Davies RR, Pizarro C, Knott-Craig C. et al. Surgical management and outcomes of Ebstein anomaly in neonates and infants: a Society of Thoracic Surgeons Congenital Heart Surgery Database analysis. Ann Thorac Surg 2018;106:785–91. [DOI] [PubMed] [Google Scholar]
- 5. Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM. et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol 2019;73:1494–563. [DOI] [PubMed] [Google Scholar]
- 6. Cho MY, Weidenbach M, Sinzobahamvya N, Grafe K, Murin P, Berger F. et al. Adult congenital open-heart surgery: emergence of a new mortality score. Eur J Cardiothorac Surg 2020;58:171–6. [DOI] [PubMed] [Google Scholar]
- 7. Jacobs JP, Jacobs ML, Austin EH 3rd, Mavroudis C, Pasquali SK, Lacour-Gayet FG. et al. Quality measures for congenital and pediatric cardiac surgery. World J Pediatr Congenit Heart Surg 2012;3:32–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brown M, Dearani JA, Danielson GK, Cetta F, Connolly HM, Warnes CA. et al. The outcomes of operations for 539 patients with Ebstein anomaly. J Thorac Cardiovasc Surg 2008;135:1120–36. [DOI] [PubMed] [Google Scholar]
- 9. Ombelet F, Goossens E, Van de Bruaene A, Budts W, Moons P.. Newly developed adult congenital heart disease anatomic and physiological classification: first predictive validity evaluation. J Am Heart Assoc 2020;9:e014988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Attenhofer Jost CH, Connolly HM, Scott CG, Burkhart HM, Warnes CA, Dearani JA.. Outcome of cardiac surgery in patients 50 years of age or older with Ebstein anomaly: survival and functional improvement. J Am Coll Cardiol 2012;59:2101–6. [DOI] [PubMed] [Google Scholar]
- 11. Holst KA, Dearani JA, Said SM, Pike RB, Connolly HM, Cannon BC. et al. Improving results of surgery for Ebstein anomaly: where are we after 235 Cone repairs? Ann Thorac Surg 2018;105:160–8. [DOI] [PubMed] [Google Scholar]
- 12. Shivapour JK, Sherwin ED, Alexander ME, Cecchin F, Mah DY, Triedman JK. et al. Utility of preoperative electrophysiologic studies in patients With Ebstein's anomaly undergoing the Cone procedure. Heart Rhythm 2014;11:182–6. [DOI] [PubMed] [Google Scholar]
- 13. Morray B. Preoperative physiology, imaging, and management of Ebstein’s anomaly of the tricuspid valve. Semin Cardiothorac Vasc Anesth 2016;20:74–81. [DOI] [PubMed] [Google Scholar]
- 14. Celermajer DS, Bull C, Till JA, Cullen S, Vassillikos VP, Sullivan ID. et al. Ebstein's anomaly: presentation and outcome from fetus to adult. J Am Coll Cardiol 1994;23:170–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.