Abstract
Background
People experiencing homelessness face a high risk of SARS-CoV-2 infection and transmission, as well as health complications and death due to COVID-19. Despite being prioritised for receiving the COVID-19 vaccine in many regions, little data are available on vaccine uptake in this vulnerable population. Using population-based health-care administrative data from Ontario, Canada—a region with a universal, publicly funded health system—we aimed to describe COVID-19 vaccine coverage (ie, the estimated percentage of people who have received a vaccine) and determinants of vaccine receipt among individuals with a recent history of homelessness.
Methods
We conducted a retrospective, population-based cohort study of adults (aged ≥18 years) with a recent experience of homelessness, inadequate housing, or shelter use as recorded in routinely collected health-care databases between June 14, 2020, and June 14, 2021 (a period within 6 months of Dec 14, 2020, when COVID-19 vaccine administration was initiated in Ontario). Participants were followed up from Dec 14, 2020, to Sept 30, 2021, for the receipt of one or two doses of a COVID-19 vaccine using the province's real-time centralised vaccine information system. We described COVID-19 vaccine coverage overall and within predefined subgroups. Using modified Poisson regression, we further identified sociodemographic factors, health-care usage, and clinical factors associated with receipt of at least one dose of a COVID-19 vaccine.
Findings
23 247 individuals with a recent history of homelessness were included in this study. Participants were predominantly male (14 752 [63·5%] of 23 247); nearly half were younger than 40 years (11 521 [49·6%]) and lived in large metropolitan regions (12 123 [52·2%]); and the majority (18 226 [78·4%]) visited a general practitioner for an in-person consultation during the observation period. By Sept 30, 2021, 14 271 (61·4%; 95% CI 60·8–62·0) individuals with a recent history of homelessness had received at least one dose of a COVID-19 vaccine and 11 082 (47·7%; 47·0–48·3) had received two doses; in comparison, over the same period, 86·6% of adults in the total Ontario population had received a first dose and 81·6% had received a second dose. In multivariable analysis, factors positively associated with COVID-19 uptake were one or more outpatient visits to a general practitioner (adjusted risk ratio [aRR] 1·37 [95% CI 1·31–1·42]), older age (50–59 years vs 18–29 years: 1·18 [1·14–1·22], ≥60 years vs 18–29 years: 1·27 [1·22–1·31]), receipt of an influenza vaccine in either of the two previous influenza seasons (1·25 [1·23–1·28]), being identified as homeless via a visit to a community health centre versus exclusively a hospital-based encounter (1·13 [1·10–1·15]), receipt of one or more SARS-CoV-2 tests between March 1, 2020, and Sept 30, 2021 (1·23 [1·20–1·26]), and the presence of chronic health conditions (one condition: 1·05 [1·03–1·08]; two or more conditions: 1·11 [1·08–1·14]). By contrast, living in a smaller metropolitan region (aRR 0·92 [95% CI 0·90–0·94]) or rural location (0·93 [0·90–0·97]) versus large metropolitan regions were associated with lower uptake.
Interpretation
In Ontario, COVID-19 vaccine coverage among adults with a recent history of homelessness has lagged and, as of Sept 30, 2021, was 25 percentage points lower than that of the general adult population in Ontario for a first dose and 34 percentage points lower for a second dose. With high usage of outpatient health services among individuals with a recent history of homelessness, better utilisation of outpatient primary care structures might offer an opportunity to increase vaccine coverage in this population. Our findings underscore the importance of leveraging existing health and service organisations that are accessed and trusted by people who experience homelessness for targeted vaccine delivery.
Funding
The Public Health Agency of Canada.
Translation
For the French translation of the abstract see Supplementary Materials section.
Research in context.
Evidence before this study
We searched MEDLINE, Scopus, PsycInfo, and CINAHL with the search terms (“homeless*” or “houseless” or “precariously housed” or “unhoused” or “no fixed address”) AND (“COVID*” or “coronavirus” or “SARS COV*”) AND (“vaccin*”or “immuniz*”) for articles published in any language from inception to Nov 30, 2021. Our search yielded 42 unique results. The available evidence quantifying vaccine uptake by people experiencing homelessness was found to be scarce. Most reports conducted qualitative assessments, or indirectly gauged the potential uptake of COVID-19 vaccination in this population through examination of vaccine intention or acceptability. Researchers commonly found that vaccine hesitancy in people experiencing homelessness was propagated by mistrust of the vaccine, misinformation spread in media, and lack of access to suitable health-care structures. One study examined COVID-19 vaccination coverage in homeless veterans who accessed Veterans Affairs health-care services in the USA, finding that coverage was similar to that of the US veteran population and lower than that of the general adult US population. They also found strong associations between veterans who used health-care and housing services and vaccination status. Furthermore, they found that female veterans, those who received the seasonal influenza vaccine, and those living with multiple comorbidities were more likely to be vaccinated. We did not find any other robust quantitative studies examining vaccination epidemiology in people experiencing homelessness.
Added value of this study
Our study of vaccine coverage in Ontario, Canada, between Dec 14, 2020, and Sept 30, 2021, provides population-level insights about vaccine uptake in people experiencing homelessness during the COVID-19 pandemic. The study cohort (n=23 247) was derived from a validated case ascertainment algorithm used to identify individuals with a recent history of homelessness from health-care administrative data of a provincial, single-payer publicly funded health-care system. Due to the nature of the data source, COVID-19 vaccination has been comprehensively captured by the province by use of a real-time tracking system, which allowed us to record the vaccination status of individuals with a recent history of homelessness in a timely and accurate manner. The cohort used in this study comprises a heterogeneous population of people experiencing homelessness living across the province, ranging in sociodemographic and health factors. We found that 14 271 (61·4%) of 23 247 individuals with a recent history of homelessness had received at least one COVID-19 vaccine by Sept 30, 2021, in comparison with 86·6% of the adult population of Ontario during the same timeframe. This study also showed that vaccine coverage among individuals with a recent history of homelessness is positively associated with accessing primary health care, being a previous recipient of a seasonal influenza vaccine or SARS-CoV-2 test, and the presence of chronic health conditions. Furthermore, identification as being homeless by a community-based primary health-care provider and previous mental health encounters were found to be important predictors of COVID-19 vaccination.
Implications of all the available evidence
Although people experiencing homelessness were denoted by the provincial government as a priority population to receive a COVID-19 vaccine, this study shows that coverage among individuals with a recent history of homelessness has lagged in comparison with that of the general population of Ontario, Canada. Also corroborating findings among homeless veterans in the USA, our results suggest that policy-related and social factors influence vaccine uptake in people experiencing homelessness, including trust in the health-care system, as evidenced by past influenza vaccination and involvement in primary care structures. Our findings underscore the importance of generating tailored and targeted outreach interventions that leverage existing health and service organisations that are accessed and trusted by people experiencing homelessness, including the potential development of mobile vaccination clinics to serve locations such as homeless encampments; warming and cooling centres; meal programmes; opioid replacement therapy and safe injection locations; and better utilisation of outpatient, primary, and community-based health-care structures as a location where people experiencing homelessness can receive COVID-19 vaccines.
Introduction
A survey administered by Nanos Research early in the COVID-19 pandemic (July, 2020) found that one in 20 Canadians, or an estimated 1·6 million Canadians, have experienced homelessness at some point in their lives, described as “the situation without safe, permanent, or appropriate housing, or the immediate prospect of acquiring it”.1 People experiencing homelessness commonly face physical and mental health challenges, increased health-care usage, morbidity, and premature mortality.2, 3 Unsurprisingly, numerous reports have documented high rates of SARS-CoV-2 infection and transmission, as well as health complications and mortality due to COVID-19 in this population.4, 5, 6, 7 In the Canadian province of Ontario, a population-based analysis found that between January and July, 2020, individuals with a recent history of homelessness were 20 times more likely to be admitted to hospital, ten times more likely to require critical care, and five times more likely to die within 21 days of a SARS-CoV-2 infection, compared to community-dwelling adults in Ontario.5 Recognising these risks, people experiencing homelessness, regardless of age, were prioritised for COVID-19 vaccine receipt in the second phase of Ontario's COVID-19 vaccine roll-out, which was scheduled to begin in April, 2021,8 with some health regions receiving authorisation to initiate targeted efforts in late February, 2021.9, 10 However, preliminary reports arising from that time period suggested barriers to vaccine delivery in people experiencing homelessness, including vaccine hesitancy,11 mistrust of organisations leading vaccination clinics,12 and various logistical barriers to offering clinics at shelters undergoing SARS-CoV-2 outbreaks.13
Although vaccine coverage (ie, the estimated percentage of people who have received a vaccine) has been well documented in other populations prioritised for early COVID-19 vaccine distribution (eg, older people and organ transplant recipients) and in the general population in Ontario,14, 15 little has been reported on vaccine uptake among people experiencing homelessness. Harnessing linked, routinely collected health-care data in Ontario, we sought to address this gap by describing COVID-19 vaccine coverage among individuals with a recent experience of homelessness as recorded during a health-care encounter, overall and within predefined subgroups, from Dec 14, 2020, to Sept 30, 2021; and the sociodemographic factors, health-care usage, and clinical factors associated with COVID-19 vaccine receipt in this population.
Methods
Study setting and design
We conducted a retrospective population-based cohort study using health-care administrative data in Ontario, Canada. Ontario is Canada's most populous province, with an estimated population of 14·8 million in 2021.16 Most residents of Ontario receive universal access to physician, hospital, and other health-care services through the single-payer Ontario Health Insurance Plan (OHIP).17 As an OHIP health card is presented at each health-care encounter, unique health card numbers enable linkage across patient encounters in all available databases. From Dec 14, 2020, onwards, COVID-19 vaccines were made freely available to anyone residing in Canada based on priority status as determined by their risk of developing health complications due to COVID-19.18 Initially (until May, 2021), vaccines authorised by Health Canada were indicated for individuals aged 16 years or older. This study follows the Reporting of Studies Conducted Using Observational Routinely Collected Data (RECORD) reporting guidelines (appendix 2 p 2).19
Data sources
Health-care administrative datasets used in this study were linked with encrypted health card numbers and analysed at ICES, an independent, non-profit research institute. Several data sources were used to define participants, outcomes, and covariates. These included the Canadian Institute for Health Information Discharge Abstract Database, Same Day Surgery database, National Ambulatory Care Reporting System, the Ontario Mental Health Reporting System; the Community Health Centres database; the Ontario Laboratories Information System; the COVID-19 vaccination information system, COVaxON; the Registered Persons Database demographic dataset; the OHIP claims database; the Ontario Drug Benefit database; and several population-surveillance datasets derived with validated case definitions, including the Chronic Obstructive Pulmonary Disease Database, the Ontario Asthma Database, the Ontario Diabetes Database, the Congestive Heart Failure Database, and the Ontario Hypertension Database. All data sources are further described in appendix 2 (p 8).
Participants
Study participants included adults (aged ≥18 years) in Ontario eligible for OHIP coverage who met the case definition of an individual with a recent history of homelessness as of Dec 14, 2020. The case definition, adapted from a recent validation study,20 included all individuals with an experience of homelessness, inadequate housing, or shelter use recorded as part of a health-care encounter among selected health-care service data sources that collect indicators of housing status (the Discharge Abstract Database, Same Day Surgery database, National Ambulatory Care Reporting System, Ontario Mental Health Reporting System, and the Community Health Centres database) between June 14, 2020, and June 14, 2021 (a period within 6 months before or after Dec 14, 2020). The validation study was evaluated against a representative sample of people experiencing homelessness across a range of living situations and found that a capture window of 6 months before or after an episode of known homelessness maximises sensitivity in determining the homeless experience within a 1-year period, while retaining excellent specificity.20 As such, this study retained the full accrual window despite overlap with the observation window in order to generate a cohort of individuals with contemporary evidence of homelessness. Indicators included the presence of the International Classification of Diseases, 10th revision (ICD-10) diagnosis codes for homelessness (Z590) or inadequate housing (Z591), a missing postal code (no address provided) or housing status indicative of homelessness, inadequate housing, or shelter use recorded in housing-specific data collection fields. A detailed case definition is provided in appendix 2 (p 17).
Characteristics of participants
We obtained various sociodemographic, health-care usage, and clinical characteristics available in the health-care administrative databases that were found to previously be associated with vaccine uptake in people experiencing homelessness, identified as barriers to accessing and accepting COVID-19 vaccines in people experiencing homelessness or aligned with domains of the WHO 3C model for the determinants of vaccine hesitancy.21, 22, 23, 24, 25 Characteristics and variable definitions are detailed in appendix 2 (p 18).
Outcome measures
Ontario records all COVID-19 vaccines administered in the province in a real-time centralised vaccine information system (COVaxON) that collects information including the date and location of administration, product type, and dose number. We extracted records pertaining to participants and assessed COVID-19 vaccine coverage by dose from Dec 14, 2020, to Sept 30, 2021. Coverage was measured as the cumulative percentage of people who had received one or two doses of a COVID-19 vaccine per day. We accepted any vaccine dose approved by Health Canada26 in classifying series initiation, regardless of whether it was received in Ontario or not. Participants were classified by vaccination status on the basis of the number of doses received as of Sept 30, 2021. Although third doses became available in Ontario in mid-August, 2021, eligibility was restricted to residents of long-term care homes and immunologically suppressed individuals in whom the response to a primary two-dose series was unlikely to be adequately protective. Because eligibility did not include the broader segment of people experiencing homelessness, we opted not to report on third doses in this study.27 Coverage was measured as a percentage in the complete cohort (overall) and among the prespecified subgroups based on age groupings, level of urbanicity, one or more visits to a general practitioner during the observation period, receipt of an influenza vaccination in at least one of the 2019–20 or 2020–21 influenza seasons, one or more mental health-care encounters in the previous year, the number of pre-existing medical conditions (zero, one, two, or more), and whether participants were recognised as homeless through a visit to a community health centre (vs exclusively via a hospital-based encounter).
Statistical analysis
We described the characteristics of vaccine administration by dose number (first vs second) and compared the demographic and health characteristics of participants by vaccination status as of Sept 30, 2021. Characteristics were summarised as counts and proportions, means and SDs, or medians and IQRs, as appropriate. Characteristics between participants who received zero doses and those who received one or more doses were compared with standardised differences, which assess differences between group means as a percentage of the pooled SD; standardised differences of 10% or more were considered meaningful.28
We calculated two measures of coverage: receipt of one or more doses of a COVID-19 vaccine and the receipt of two doses. COVID-19 vaccine coverage in the complete cohort was calculated as a percentage over time (from Dec 14, 2020, to Sept 30, 2021), whereas coverage in subgroups was presented as of Sept 30, 2021. 95% CIs for coverage percentages were calculated with the Wilson Score method for proportions.29 Differences in coverage within subgroups were calculated with χ2 tests.
We applied multivariable modified Poisson regression modelling to estimate the adjusted risk ratio (aRR) and 95% CI of receiving one or more doses of a COVID-19 vaccine as of Sept 30, 2021. Factors with standardised differences approaching 10% or more were considered for inclusion in the model, and multicollinearity was assessed with a correlation matrix and variance inflation factor. We did all analyses with SAS, version 9.4, and used two-sided p values throughout; p values less than 0·05 were considered significant.
Research ethics
ICES is a prescribed entity under Ontario's Personal Health Information Protection Act (PHIPA). Section 45 of PHIPA authorises ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management, evaluation, or monitoring of the allocation of resources to, or planning for, all or part of the health system. This project uses data collected by ICES under section 45 of PHIPA, and no other data, and is therefore exempt from research ethics review; the use of the data in this project is authorised under section 45 and was approved by ICES' Privacy and Legal Office.
Role of the funding source
The funder had no role in study design, data collection, data analysis, data interpretation, writing of the report, or the decision to submit this manuscript for publication.
Results
We identified 23 247 adult individuals with a recent history of homelessness for inclusion in this study (see appendix 2 p 1 for the study flowchart). Characteristics of study participants are summarised in table 1 ; data were complete for all variables, except for level of urbanicity, where a separate category of unknown or missing data was included. Participants were predominantly male, and nearly half were younger than 40 years (11 521 [49·6%] of 23 247), lived in large metropolitan regions, and were identified as homeless in the 2 years before accrual (table 1). Participants were active users of the health system, with 18 226 (78·4%) visiting a general practitioner for an in-person consultation during the observation window, 17 648 (75·9%) receiving a SARS-CoV-2 test between March 1, 2020, and Sept 30, 2021, and 2290 (9·9%) receiving an influenza vaccine in at least one of the previous two influenza seasons. 11 224 (48·3%) had one or more chronic conditions (eg, asthma, chronic obstructive pulmonary disease, hypertension, or diabetes), and 15 448 (66·5%) had a mental health-care encounter in the previous year.
Table 1.
Characteristics of adults in Ontario with a recent history of homelessness by COVID-19 vaccine doses received as of Sept 30, 2021
| Overall (n=23 247) | No doses*(n=8976) | One or more doses†(n=14 271) | Standardised difference (%) | ||
|---|---|---|---|---|---|
| Demographics | |||||
| Age, years (SD) | 43·20 (15·65) | 39·35 (13·46) | 45·61 (16·43) | 42% | |
| Age groups | |||||
| 18–29 years | 4435 (19·08%) | 2044 (22·77%) | 2391 (16·75%) | 15% | |
| 30–39 years | 7086 (30·48%) | 3335 (37·15%) | 3751 (26·28%) | 24% | |
| 40–49 years | 3919 (16·86%) | 1552 (17·29%) | 2367 (16·59%) | 2% | |
| 50–59 years | 3642 (15·67%) | 1172 (13·06%) | 2470 (17·31%) | 12% | |
| ≥60 years | 4165 (17·92%) | 873 (9·73%) | 3292 (23·07%) | 37% | |
| Sex | |||||
| Female | 8495 (36·54%) | 3048 (33·96%) | 5447 (38·17%) | 9% | |
| Male | 14 752 (63·46%) | 5928 (66·04%) | 8824 (61·83%) | 9% | |
| Level of urbanicity | |||||
| Large metropolitan region (population >500 000) | 12 123 (52·15%) | 4307 (47·98%) | 7816 (54·77%) | 14% | |
| Small to medium metropolitan region (population 10 000–500 000) | 9034 (38·86%) | 3815 (42·50%) | 5219 (36·57%) | 12% | |
| Rural regions (population <10 000) | 1503 (6·47%) | 594 (6·62%) | 909 (6·37%) | 1% | |
| Data unknown or missing | 587 (2·53%) | 260 (2·90%) | 327 (2·29%) | 4% | |
| Evidence of homelessness between June 14, 2018, and June 14, 2020 | 10 554 (45·40%) | 4140 (46·12%) | 6414 (44·94%) | 2% | |
| Identified as an individual with a recent history of homelessness via an outpatient community health centre visit | 6870 (29·55%) | 1976 (22·01%) | 4894 (34·29%) | 28% | |
| Health status | |||||
| Chronic health conditions | |||||
| Asthma | 3804 (16·36%) | 1425 (15·88%) | 2379 (16·67%) | 2% | |
| Chronic obstructive pulmonary disease | 3315 (14·26%) | 852 (9·49%) | 2463 (17·26%) | 23% | |
| Congestive heart failure | 775 (3·33%) | 169 (1·88%) | 606 (4·25%) | 14% | |
| Hypertension | 4673 (20·10%) | 1088 (12·12%) | 3585 (25·12%) | 34% | |
| Diabetes | 3575 (15·38%) | 849 (9·46%) | 2726 (19·10%) | 28% | |
| Dementia | 627 (2·70%) | 95 (1·06%) | 532 (3·73%) | 18% | |
| Autoimmune diseases (multiple sclerosis, psoriasis, rheumatoid arthritis, Crohn's disease, or ulcerative colitis) | 1027 (4·42%) | 253 (2·82%) | 774 (5·42%) | 13% | |
| Immunocompromised state (cancer, sickle-cell disease, HIV, or other) | 1156 (4·97%) | 392 (4·37%) | 764 (5·35%) | 5% | |
| Number of chronic conditions‡ | |||||
| 0 | 12 023 (51·72%) | 5461 (60·84%) | 6562 (45·98%) | 30% | |
| 1 | 6412 (27·58%) | 2402 (26·76%) | 4010 (28·10%) | 3% | |
| ≥2 | 4812 (20·70%) | 1113 (12·40%) | 3699 (25·92%) | 35% | |
| Historical use of health services | |||||
| Visits to an emergency department in the past 2 years | 7·29 (15·79) | 6·99 (14·13) | 7·48 (16·75) | 3% | |
| Outpatient visits to a general practitioner§ in the past 2 years | 16 (6–39) | 11 (3–30) | 19 (7–44) | 32% | |
| Receipt of an influenza vaccine in 2019–20 or 2020–21 seasons | 2290 (9·85%) | 275 (3·06%) | 2015 (14·12%) | 34% | |
| Mental health-care encounter in the past year | 15 448 (66·45%) | 5744 (63·99%) | 9704 (68·00%) | 9% | |
| Specific mental health conditions | |||||
| Psychotic disorder | 2817 (12·12%) | 997 (11·11%) | 1820 (12·75%) | 5% | |
| Mood disorder | 8018 (34·49%) | 2628 (29·28%) | 5390 (37·77%) | 18% | |
| Substance use-related disorder | 9686 (41·67%) | 3889 (43·33%) | 5797 (40·62%) | 6% | |
| Other mental health-related care | 5094 (21·91%) | 1626 (18·11%) | 3468 (24·30%) | 15% | |
| Recent use of health services | |||||
| ≥1 SARS-CoV-2 test (March 1, 2020, to Sept 30, 2021) | 17 648 (75·92%) | 6311 (70·31%) | 11 337 (79·44%) | 21% | |
| Infection or hospital admission for COVID-19 (March 1, 2020, to Sept 30, 2021) | 2067 (8·89%) | 715 (7·97%) | 1352 (9·47%) | 5% | |
| Outpatient visits to a general practitioner§ (Dec 14, 2020, to Sept 30, 2021) | 5 (1–14) | 3 (1–10) | 7 (2–16) | 42% | |
| ≥1 in-person outpatient visit to a general practitioner§ (Dec 14 2020, to Sept 30, 2021), | 18 226 (78·40%) | 6311 (70·31%) | 11 915 (83·49%) | 32% | |
| Visits to an emergency department (Dec 14, 2020, to Sept 30, 2021) | 3·09 (7·15) | 2·96 (6·25) | 3·17 (7·66) | 3% | |
| ≥1 visit to an emergency department (Dec 14, 2020, to Sept 30, 2021) | 15 327 (65·93%) | 6059 (67·50%) | 9268 (64·94%) | 5% | |
Data are mean (SD), median (IQR), or n (%).
Individuals with a recent history of homelessness (adults) with no record of a COVID-19 vaccine in COVaxON.
Individuals with a recent history of homelessness (adults) with one or two vaccine doses recorded in COVaxON.
Sum of the specific chronic health conditions.
General practitioner visits include outpatient visits to a physician with the Ontario Health Insurance Plan (OHIP) designation of “FAMILY PRACTICE AND GENERAL PRACTICE” or any visit to a community health centre.
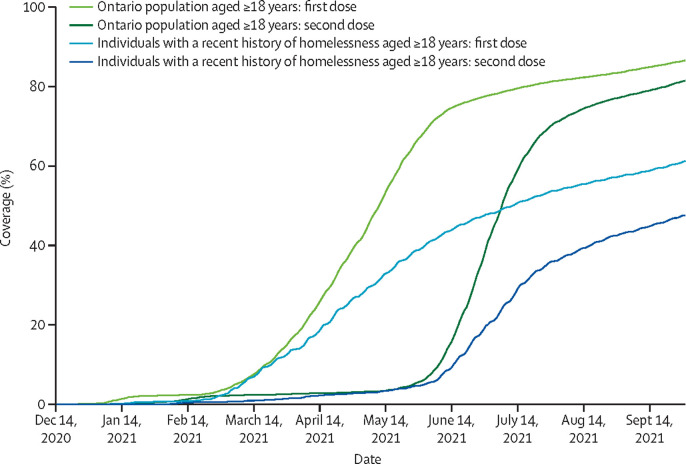
By Sept 30, 2021, 14 271 (61·4%; 95% CI 60·8–62·0) participants had received a first dose of a COVID-19 vaccine and 11 082 (47·7%; 47·0–48·3) had received two doses (figure 1 ). Vaccination coverage for first doses increased steadily from early March (564 participants; 2·4%) to mid-June (10 269 participants; 44·2%), with moderate additional uptake to the end of September (61·4%). Participants who received a second dose did so a median of 61 days (IQR 38–84) following their first dose. Among individuals with a recent history of homelessness who received a maximum of one dose, 41·6% (1327 of 3189) received their first dose in August or September and so would not have met the 8-week interval eligibility requirement for a second dose by the end of September (appendix 2 p 27).
Figure 1.
COVID-19 vaccine coverage from Dec 14, 2020, to Sept 30, 2021 among adults in Ontario with a recent history of homelessness compared to the general adult population of Ontario, by dose
In contrast to the COVID-19 vaccine coverage observed in individuals with a recent history of homelessness, by Sept 30, 2021, 86·6% (10 468 820 of 12 083 325) of the total adult population of Ontario had received their first dose of the COVID-19 vaccine, and 81·6% (9 855 523) had received two doses (appendix 2 p 23). Although a similar pattern in the timing of vaccine uptake occurred among adults in Ontario, coverage in the general population increased at a quicker rate between early March and mid-June (from 447 721 [3·7%] to 9 051 844 [74·9%]; figure 1).
Individuals with a recent history of homelessness were predominantly administered an mRNA vaccine (13 533 [95·0%] administered an mRNA vaccine as a first dose; 10 935 [98·7%] administered an mRNA vaccine as a second dose), with the remainder receiving a viral vector vaccine (table 2 ). When receiving their first dose, participants were most often distributed among the age-eligibility, congregate setting, or at-risk priority groups, with varied locations of administration.
Table 2.
Characteristics of COVID-19 vaccines received, by dose, for adults with a recent history of homelessness
| First dose (n=14 271) | Second dose (n=11 082) | |
|---|---|---|
| Vaccine product | ||
| Pfizer–BioNTech (BNT162b2) | 7865 (55·11%) | 5744 (51·83%) |
| Moderna (mRNA-1273) | 5688 (39·86%) | 5191 (46·84%) |
| Oxford–AstraZeneca (ChAdOx1 nCoV-19), Covishield, or Janssen (Ad26.CoV2.S) | 718 (5·03%) | 147 (1·33%) |
| Priority status under which vaccine was administered | ||
| Age-based eligibility | 6296 (44·21%) | 4587 (41·48%) |
| Congregate setting | 2370 (16·64%) | 1816 (16·42%) |
| Priority populations | 3655 (25·67%) | 3087 (27·92%) |
| Essential workers (health-care workers) | 170 (1·19%) | 161 (1·46%) |
| Essential workers (others) | 106 (0·74%) | 97 (0·88%) |
| Other | 1644 (11·54%) | 1310 (11·85%) |
| Location of vaccine administration | ||
| Public health unit delivered clinic | 6057 (42·44%) | 4748 (42·84%) |
| Congregate living or care | 2762 (19·35%) | 1691 (15·25%) |
| Hospital | 2183 (15·30%) | 1411 (12·73%) |
| Pharmacy | 2064 (14·46%) | 2156 (19·45%) |
| Physician's office | 1091 (7·64%) | 962 (8·68%) |
| Other | 115 (0·80%) | 114 (1·04%) |
Data are n (%).
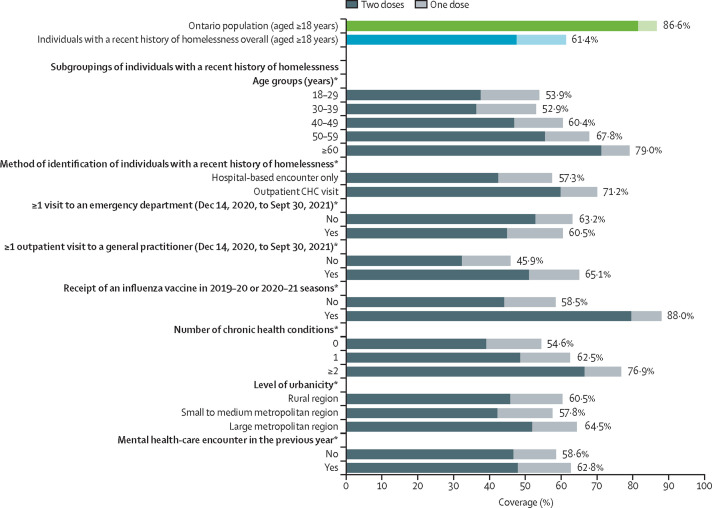
Variation in vaccine coverage was observed among subgroups of individuals with a recent history of homelessness (figure 2 ; appendix 2 p 23). A gradient in coverage was apparent among age groups (ranging from 52·9% to 53·9% in those aged 18–39 years to 79·0% in those aged ≥60 years) and chronic health conditions (ranging from 54·6% for those with no conditions to 76·9% for those with two or more conditions). Coverage was markedly higher among individuals identified as homeless via an outpatient community health centre visit compared to those with an exclusively hospital-based encounter (71·2% vs 57·3%), those who had one or more visits to a general practitioner during the observation window compared with those who reported no visits (65·1% vs 45·9%), and those who received an influenza vaccine in at least one of the previous two influenza seasons compared with those who did not (88·0% vs 58·5%). Smaller differences were observed according to the level of urbanicity (ranging from 57·8% in those living in small to medium metropolitan regions to 64·5% in those living in large metropolitan regions) or if the participant had a mental health-care encounter in the previous year (58·6% coverage in those with no encounter vs 62·8% coverage in those with an encounter).
Figure 2.
COVID-19 vaccine coverage as of Sept 30, 2021, in overall adult population of Ontario, in adults with a recent history of homelessness, and in predefined subgroups of people with a recent history of homelessness
Source: Public Health Ontario, 2021. *p value of χ2 tests comparing within-group coverage of one or more doses less than 0·05. Darker shades represent receipt of two doses; lighter shades represent receipt of one dose. CHC=community health centre. Detailed values, 95% CIs, and p values are summarised in the appendix (p 23).
In the unadjusted analysis, compared to unvaccinated individuals (table 1), adult individuals with a recent history of homelessness who received one or more doses of a COVID-19 vaccine were more often older (mean age 45·6 years vs 39·4 years), lived in large metropolitan regions (54·8% vs 47·9%), were identified as homeless via a community health centre visit (34·3% vs 22·0%), had one or more pre-existing chronic health conditions (54·0% vs 39·2%), more often visited a general practitioner in the previous 2 years (median visits 19 vs 11), received an influenza vaccine in at least one of the previous two influenza seasons (14·1% vs 3·1%), received one or more SARS-CoV-2 tests between March 1, 2020, and Sept 30, 2021 (79·4% vs 70·3%), and had one or more general practitioner visits on an outpatient basis between Dec 14, 2020, and Sept 30, 2021 (83·5% vs 70·3%).
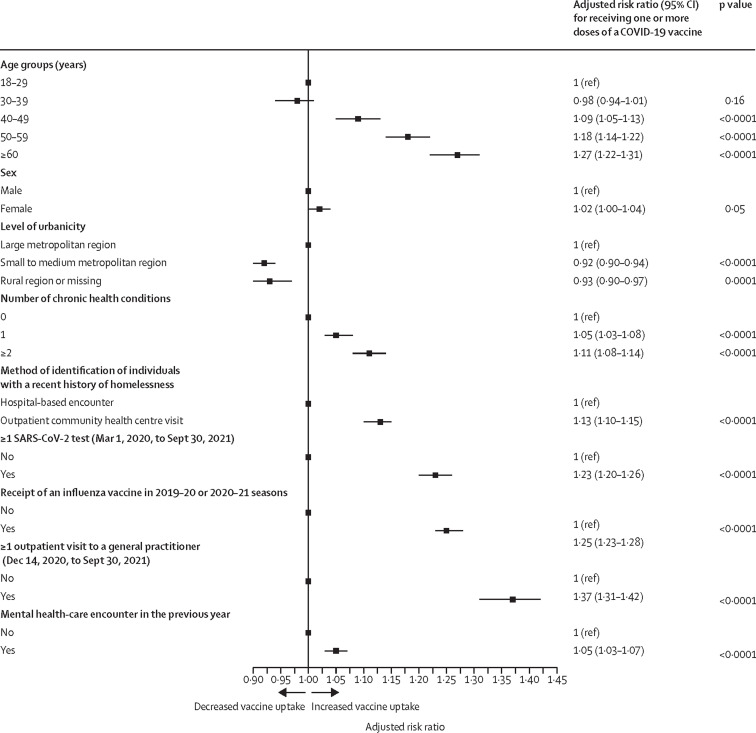
In the multivariable analysis (figure 3 ), factors positively associated with COVID-19 vaccine uptake were one or more outpatient visits to a general practitioner during the observation window (aRR 1·37 [95% CI 1·31–1·42]), older age (50–59 years vs 18–29 years: 1·18 [1·14–1·22]; ≥60 years vs 18–29 years: 1·27 [1·22–1·31]), receipt of an influenza vaccine in at least one of the previous two influenza seasons (1·25 [1·23–1·28]), being identified as homeless via a visit to a community health centre versus exclusively having a hospital-based encounter (1·13 [1·10–1·15]), receipt of one or more SARS-CoV-2 tests between March 1, 2020, and Sept 30, 2021 (1·23 [1·20–1·26]), the presence of chronic health conditions (one condition: 1·05 [1·03–1·08]; two or more conditions: 1·11 [1·08–1·14]) and one or more mental health-care encounters in the previous year (1·05 [1·03–1·07]). By contrast, living in a smaller metropolitan region (aRR 0·92 [95% CI 0·90–0·94]) or rural location (0·93 [0·90–0·97]) were associated with lower uptake. No appreciable differences in uptake were apparent by biological sex (aRR 1·02 [95% CI 1·00–1·04]). A sensitivity model excluding multimorbidity (having a correlation of 0·46 with age, indicating mild to moderate collinearity) showed only small changes to the aRR and no changes in the significance or direction of the results (data not shown).
Figure 3.
Factors associated with receipt of one or more doses of a COVID-19 vaccine by Sept 30, 2021
Discussion
In this population-based analysis of more than 23 000 adults with a recently recorded experience of homelessness, we found that 61·4% were at least partially vaccinated against COVID-19 by Sept 30, 2021, which was 25% lower than the general adult population in Ontario (86·6%). We also found that higher vaccine uptake was associated with older age, increased number of comorbidities, and indicators of increased engagement with outpatient health services (eg, visits to a general practitioner, receipt of a seasonal influenza vaccine, and SARS-CoV-2 testing).
Our study provides population-level insights about vaccine uptake of adults experiencing homelessness during the COVID-19 pandemic. The study cohort analysed was derived from the population-level, provincial health-care administrative database in a region with a universal, publicly funded health system, and applied a validated case ascertainment algorithm designed to identify individuals with a recent history of homelessness.20 Direct linkage of individuals who had a recent history of homelessness with COVID-19 vaccination status was also done, providing timely and near comprehensive vaccination status of people experiencing homelessness in the province of Ontario, Canada. At the time of reporting (December, 2021), the only other comparable study to assess COVID-19 vaccine uptake in people experiencing homelessness was among veterans experiencing homelessness in the USA.30 Despite the differing source populations, settings, and political ideologies that might have influenced COVID-19 vaccine uptake in the two nations, several of our findings corroborated the findings among homeless veterans in the USA: homeless veterans were found to have lower vaccination coverage compared to the general population (45·8% vs 64·3%); homeless veterans who were older, used health-care services, received the seasonal influenza vaccine, and lived with multiple comorbidities were also found to have higher vaccination coverage.
Contemporary research has shown that adults experiencing homelessness are disproportionately affected by COVID-19 and its associated complications.5 For this reason, after the first COVID-19 vaccine was approved by Health Canada in December, 2020, the provincial vaccine prioritisation strategy responsible for allocation of the then-limited supply of vaccines listed people experiencing homelessness of all age categories as a priority population for vaccination.8 Although people experiencing homelessness were identified as a priority demographic for vaccination, the significantly lower coverage of vaccination in comparison with the general population observed in this study is of considerable policy and practice concern. Although it is not possible to fully ascertain the mechanisms behind this lagged vaccination coverage from the study findings alone, past work has identified a range of hesitancy factors related to obtaining vaccination in people experiencing homelessness, including fear or mistrust of the vaccine, misinformation spread in media, uncertainties about personal risk of COVID-19, and elements related to access to health-care structures and trust within the patient–provider relationship.21, 23, 24, 31, 32 Furthermore, systematic structural barriers commonly faced by people experiencing homelessness33 possibly also acted as obstacles to COVID-19 vaccination in the study population. For instance, during the study period, many of the centralised provincial vaccination clinics required advanced scheduling of appointments through online websites or portals. This requirement could generate considerable barriers to access for individuals with limited internet access or digital literacy, and further impede individuals without access to, or the ability to travel to, these centralised clinics.33 Furthermore, although specialised clinics were offered (eg, mobile clinics and clinics in shelters) to people experiencing homelessness, these depended on the availability of resources at the municipal level and would have favoured larger centres. Together, this might also explain why vaccination coverage was found to be moderately lower outside of larger urban settings.
Overall, the largest factor associated with COVID-19 vaccine uptake in individuals with a recent history of homelessness uncovered in our study was visiting a community-based general practitioner during the study timeframe. Older age, living with comorbidities, and past receipt of a seasonal influenza vaccine or a SARS-CoV-2 test were also associated with higher vaccination coverage, highlighting segments of the population that are also more likely to access primary health-care services. These findings suggest that connection and access to primary health care is a crucial factor in facilitating uptake of COVID-19 vaccination among people experiencing homelessness. Although the causal mechanisms of this association are not fully clear, the literature exploring COVID-19 vaccination approaches in people experiencing homelessness has outlined that trust and relationship building with this population is central to a successful vaccination strategy.30, 32, 33 As a historically marginalised population, people experiencing homelessness face considerable and ongoing barriers towards accessing health-care services34 that have only been further exacerbated by the pandemic.35 Community-based primary health-care models that provide priority populations such as people experiencing homelessness with more accessible avenues to health care (eg, community health centres and outreach teams) should be further investigated and leveraged to support vaccination efforts in people experiencing homelessness, along with other targeted vaccination interventions (ie, mobile vaccination clinics at encampments, as well as opioid replacement therapy and safe injection locations).33, 36 Although a visit to a general practitioner was found to be a strong factor associated with vaccine uptake, unvaccinated individuals were also found to access these services at a high rate (70·3% visited a general practitioner in person between Dec 14, 2020, and Sept 30, 2021, with a median of three visits). Minimal opportunities for family medical practices in Ontario to participate in vaccine delivery early in the vaccination effort (until July, 2021)37 might have also played a role in the lower vaccination coverage observed in this population.
Despite our study's strengths, the following limitations, also discussed in more detail elsewhere,38 should be considered. First, our study relies on health administrative data, which comprises the population of Ontario eligible for provincial health insurance. Although more than 99% of people in Ontario have health-care coverage through this provincial insurance plan (ie, OHIP), specific cross-sections of the provincial population are not covered by OHIP, including: Indigenous people living on reserves; certain refugee claimants who do not meet the refugee definition in the 1951 Geneva Convention; and active military and some veteran groups.39 These excluded groups generally receive health-care coverage through federal programmes. As such, our results can only be generalised to people in Ontario with provincial health insurance coverage. Furthermore, our results can only be generalised to individuals in Ontario with a recent history of homelessness who access hospital or primary health-care structures, as the case definition used in this study only allowed us to identify adult individuals with a recent history of homelessness who had an eligible health system encounter. As comprehensive demographics of people experiencing homelessness in Ontario are unavailable, we were unable to assess how the study cohort differs from the broader population of people experiencing homelessness. Additionally, the case definition did not allow us to distinguish the timing of episodes of homelessness and so participants might have moved in and out of homelessness within the accrual or follow-up periods. The same reliance on administrative data sources made it impossible for us to distinguish between individuals who experienced homelessness chronically or more episodically, or the living situations of these individuals (eg, living on the streets or in a shelter), among whom vaccination coverage might differ.
Second, vaccine uptake is likely to be influenced by other behaviours and attitudes that are not captured or measurable within the health-care administrative data source. For instance, although past influenza vaccination and use of primary health-care services were interpreted as proxies for access to or trust in health-care providers, or both, these variables represent inaccurate proxies for such constructs. Similarly, because of the limitations of the data available to us, we could not assess the impact of intersectionality between gender, race, education, and other social factors with homelessness, which might have influenced vaccination uptake among this cohort of individuals with a recent history of homelessness. Finally, although all residents of Ontario were eligible to receive a COVID-19 vaccine, an OHIP health card was not required to be presented for vaccine receipt. Although efforts were made to link vaccine recipients to their health insurance account by use of other identifiers (ie, last name, first name, date of birth, or sex), it is possible that vaccination records of eligible individuals could have been missed where specific identifying information was not present (eg, health card number), or other identifiers were insufficient for accurate linkage. This limitation could lead to an underestimate of vaccine coverage in the study population.
In conclusion, despite the province recognising people experiencing homelessness as a priority population for early vaccination receipt, this study found that COVID-19 vaccine coverage among adults with a recent history of homelessness has lagged and, as of Sept 30, 2021, was 25 percentage points lower than that of the general adult population in Ontario for a first dose and 34 percentage points lower than that of the general adult population in Ontario for a second dose. With the return of the winter weather, circulating and emerging SARS-CoV-2 variants such as delta (B.1.617.2) and omicron (B.1.1.529) becoming active in community spread across Ontario (as of the end of December, 2021), and public health guidelines recommending third doses of COVID-19 vaccines,27 it is imperative that vaccination coverage among people experiencing homelessness is increased to curb widespread infections and the ever-increasing burden of COVID-19 on this population. More concerted and informed efforts are needed to enhance vaccination coverage. Leveraging relationships with existing organisations that provide health care for people experiencing homelessness might offer a solution. For example, integration of community-based primary care providers such as general practitioners and community health centres in vaccination efforts and other tailored interventions (eg, mobile vaccination clinics to serve homelessness encampments, no-appointment vaccination clinics, warming and cooling centres, meal programmes, and opioid replacement therapy and safe injection locations) might assist in improving COVID-19 vaccination uptake among people experiencing homelessness. Findings from this study could also be used to inform future human and health resource planning, enabling better and more efficient resource allocation to support the ongoing pandemic and future pandemic responses.
Data sharing
The dataset from this study is held securely in coded form at ICES. Although legal data sharing agreements between ICES and data providers (eg, health-care organisations and government) prohibit ICES from making the dataset publicly available, access could be granted to those who meet pre-specified criteria for confidential access, either online or via email (das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the corresponding author upon request, understanding that the syntax might rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or might require modification.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
This study was supported by ICES (formerly the Institute for Clinical Evaluative Sciences), which is funded by an annual grant from the Ontario Ministry of Health and Ministry of Long-Term Care. The study was completed at the ICES Western site, where core funding is provided by the Academic Medical Organization of Southwestern Ontario, the Schulich School of Medicine and Dentistry, Western University, and the Lawson Health Research Institute. This study was funded by the Public Health Agency of Canada. Parts of this material are based on data and information compiled and provided by the Ontario Ministry of Health, Ministry of Long-term Care, Canadian Institute for Health Information, Public Health Ontario, and Statistics Canada. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding sources or data providers; no endorsement is intended or should be inferred. We thank IQVIA Solutions Canada for use of their Drug Information File. We thank Boniface Harerimana and Harry Hyunteh Kim for their support in preparing the French translation of the abstract.
Contributors
SZS conceived the study, did the initial literature review, and developed the initial study plan. LR analysed the data. All authors contributed to the analysis plan and interpreted the results. LR and SZS accessed and verified the underlying data. SZS, RB, and LR drafted the initial manuscript, and all authors revised the manuscript critically for important intellectual content, gave final approval, and agreed to be accountable for all aspects of the work. SZS and LR had access to the individual-level data, and all authors had access to summary data (aggregate data) generated from the individual-level data.
Supplementary Materials
References
- 1.Nanos One in five Canadians have a friend or acquaintance who has been homeless; majority support building new affordable housing. August, 2020. https://nanos.co/wp-content/uploads/2020/08/2020-1698-CND-Alliance-to-End-Homelessness-FINAL-with-Tabs.pdf
- 2.Hwang SW, Chambers C, Chiu S, et al. A comprehensive assessment of health care utilization among homeless adults under a system of universal health insurance. Am J Public Health. 2013;103(suppl 2):S294–S301. doi: 10.2105/AJPH.2013.301369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martens WH. A review of physical and mental health in homeless persons. Public Health Rev. 2001;29:13–33. [PubMed] [Google Scholar]
- 4.McFarling UL. The uncounted: people who are homeless are invisible victims of Covid-19. March 11, 2021. https://www.statnews.com/2021/03/11/the-uncounted-people-who-are-homeless-are-invisible-victims-of-covid-19/
- 5.Richard L, Booth R, Rayner J, Clemens KK, Forchuk C, Shariff SZ. Testing, infection and complication rates of COVID-19 among people with a recent history of homelessness in Ontario, Canada: a retrospective cohort study. CMAJ Open. 2021;9:e1–e9. doi: 10.9778/cmajo.20200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohsenpour A, Bozorgmehr K, Rohleder S, Stratil J, Costa D. SARS-Cov-2 prevalence, transmission, health-related outcomes and control strategies in homeless shelters: systematic review and meta-analysis. EClinicalMedicine. 2021;38 doi: 10.1016/j.eclinm.2021.101032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duffy A. How Ottawa's homeless shelters vaccinated their way out of a massive COVID-19 outbreak. Ottawa Citizen. Aug 28, 2021. https://ottawacitizen.com/news/local-news/how-ottawas-homeless-shelters-vaccinated-their-way-out-of-a-massive-covid-19-outbreak
- 8.Government of Ontario Ontario's COVID-19 vaccination plan. Sept 14, 2021. https://covid-19.ontario.ca/ontarios-covid-19-vaccination-plan
- 9.City of Toronto City of Toronto, hospital and community health partners to begin vaccinating people experiencing homelessness and other priority populations as part of phase 1 community vaccination plan. Feb 28, 2021. https://www.toronto.ca/news/city-of-toronto-hospital-and-community-health-partners-to-begin-vaccinating-people-experiencing-homelessness-and-other-priority-populations-as-part-of-phase-1-community-vaccination-plan/
- 10.Raymond T, Szperling P. Ottawa to begin vaccinations for homeless population Thursday. CTV News. March 3, 2021. https://ottawa.ctvnews.ca/ottawa-to-begin-vaccinations-for-homeless-population-thursday-1.5331624
- 11.Gibson V. ‘It feels like we're behind’: slow pace of vaccinating Toronto's homeless causes alarm — and a strategy rethink. Toronto Star. April 11, 2021. https://www.thestar.com/news/gta/2021/04/11/it-feels-like-were-behind-slow-pace-of-vaccinating-torontos-homeless-causes-alarm-and-a-strategy-rethink.html
- 12.Casey L. Vaccination of Toronto's homeless well underway with about 1,000 getting a shot. CTV News. March 11, 2021. https://toronto.ctvnews.ca/vaccination-of-toronto-s-homeless-well-underway-with-about-1-000-getting-a-shot-1.5343715
- 13.Leung W. Toronto faces obstacles in vaccinating homeless populations while COVID-19 outbreaks erupt in shelters. The Globe and Mail. May 4, 2021. https://www.theglobeandmail.com/canada/toronto/article-toronto-faces-obstacles-in-vaccinating-homeless-populations-while/
- 14.ICES ICES COVID-19 Dashboard, Applied Health Research Questions (AHRQ) # 2021 0950 080 000. 2020. https://www.ices.on.ca/DAS/AHRQ/COVID-19-Dashboard#priority-groups
- 15.Ontario Agency for Health Protection and Promotion (Public Health Ontario) Surveillance report: COVID-19 vaccine uptake in Ontario: December 14, 2020 to October 3, 2021. https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-vaccine-uptake-ontario-epi-summary.pdf?sc_lang=en
- 16.Government of Ontario. Ministry of Finance Ontario demographic quarterly: highlights of first quarter. Sept 22, 2021. https://www.ontario.ca/page/ontario-demographic-quarterly-highlights-first-quarter
- 17.Government of Ontario. Ministry of Health and Long-Term Care What OHIP covers. Oct 21, 2021. https://www.ontario.ca/page/what-ohip-covers
- 18.Government of Canada Vaccines for COVID-19: how to get vaccinated. Feb 24, 2022. https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19/vaccines/how-vaccinated.html#a2
- 19.Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richard L, Hwang SW, Forchuk C, et al. Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-030221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodriguez RM, Torres JR, Chang AM, et al. The rapid evaluation of COVID-19 vaccination in emergency departments for underserved patients study. Ann Emerg Med. 2021;78:502–510. doi: 10.1016/j.annemergmed.2021.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knight KR, Duke MR, Carey CA, et al. COVID-19 testing and vaccine acceptability among homeless-experienced adults: qualitative data from two samples. J Gen Intern Med. 2021 doi: 10.1007/s11606-021-07161-1. published online Oct 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Longchamps C, Ducarroz S, Crouzet L, et al. COVID-19 vaccine hesitancy among persons living in homeless shelters in France. Vaccine. 2021;39:3315–3318. doi: 10.1016/j.vaccine.2021.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuhn R, Henwood B, Lawton A, et al. COVID-19 vaccine access and attitudes among people experiencing homelessness from pilot mobile phone survey in Los Angeles, CA. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The SAGE Vaccine Hesitancy Working Group What influences vaccine acceptance: a model of determinants of vaccine hesitancy. March 18, 2013. http://www.who.int/immunization/sage/meetings/2013/april/1_Model_analyze_driversofvaccineConfidence_22_March.pdf?ua=1
- 26.Government of Ontario. Ministry of Health COVID-19 guidance for individuals vaccinated outside of Ontario/Canada. Feb 1, 2022. https://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/vaccine/COVID-19_guidance_for_individuals_vaccinated_outside_of_ontario.pdf
- 27.Government of Ontario. Ministry of Health COVID-19 vaccine third dose recommendations. Feb 17, 2022. https://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/vaccine/COVID-19_vaccine_third_dose_recommendations.pdf
- 28.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38:1228–1234. [Google Scholar]
- 29.Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat. 1998;52:119–126. [Google Scholar]
- 30.Balut MD, Chu K, Gin JL, Dobalian A, Der-Martirosian C. Predictors of COVID-19 vaccination among veterans experiencing homelessness. Vaccines. 2021;9 doi: 10.3390/vaccines9111268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meehan AA, Yeh M, Gardner A, et al. COVID-19 vaccine acceptability among clients and staff of homeless shelters in Detroit, Michigan, February 2021. Health Promot Pract. 2022;23:35–41. doi: 10.1177/15248399211049202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogers JH, Cox SN, Hughes JP, et al. Trends in COVID-19 vaccination intent and factors associated with deliberation and reluctance among adult homeless shelter residents and staff, 1 November 2020 to 28 February 2021 – King County, Washington. Vaccine. 2022;40:122–132. doi: 10.1016/j.vaccine.2021.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paudyal V, Racine M, Hwang SW. COVID-19 vaccination amongst persons experiencing homelessness: practices and learnings from UK, Canada and the US. Public Health. 2021;199:e2–e3. doi: 10.1016/j.puhe.2021.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu M, Hwang SW. Health care for homeless people. Nat Rev Dis Primers. 2021;7:5. doi: 10.1038/s41572-020-00241-2. [DOI] [PubMed] [Google Scholar]
- 35.Harris MTH, Young S, Barocas J, et al. A descriptive comparison of substance use services in recovery and isolation sites for people experiencing homelessness during the COVID-19 pandemic, Boston and Toronto. Public Health Rep. 2021;136:532–537. doi: 10.1177/00333549211032974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghosh SM, Turnbull J, Macdonald N, Bond A, April AO. Key strategies to vaccinating homeless populations. April 12, 2021. https://rsc-src.ca/fr/voix-de-la-src/key-strategies-to-vaccinating-homeless-populations
- 37.CTV News Ontario family doctors want clear plan on their future COVID-19 vaccination role. July 10, 2021. https://toronto.ctvnews.ca/ontario-family-doctors-want-clear-plan-on-their-future-covid-19-vaccination-role-1.5504327
- 38.Booth R, Richard L, Forchuk C, Shariff SZ. Utility, limitations and opportunities for using linked health administrative data to study homelessness in Ontario. Healthc Q. 2022;24:7–10. doi: 10.12927/hcq.2022.26718. [DOI] [PubMed] [Google Scholar]
- 39.Government of Ontario. Ministry of Health Apply for OHIP and get a health card. Jan 19, 2022. https://www.ontario.ca/page/apply-ohip-and-get-health-card
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset from this study is held securely in coded form at ICES. Although legal data sharing agreements between ICES and data providers (eg, health-care organisations and government) prohibit ICES from making the dataset publicly available, access could be granted to those who meet pre-specified criteria for confidential access, either online or via email (das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the corresponding author upon request, understanding that the syntax might rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or might require modification.