Abstract
Aplastic or twig-like middle cerebral artery (Ap/T-MCA) is a rare vascular anomaly that can cause a hemorrhagic or ischemic event. We report a 38-year-old man who presented with intracerebral hemorrhage from a ruptured aneurysm associated with an Ap/T-MCA. After aneurysm trapping and resection, histopathological examination revealed an internal elastic lamina (IEL) disruption and a thin aneurysmal wall. The patient recovered well after surgery and rehabilitation. No hemorrhagic or ischemic events have occurred during 2 years of follow-up. Ap/T-MCA-associated aneurysms exhibit a disrupted IEL and thin wall, which demonstrates the fragility of the “twig-like” vessels.
Keywords: twig-like middle cerebral artery, anomaly, aneurysm, intracerebral hemorrhage
Introduction
Aplastic or twig-like middle cerebral artery (Ap/T-MCA) is a rare vascular anomaly with a prevalence of approximately 0.11%-0.67%.1-3) The embryological interruption of MCA trunk genesis is the cause, which results in the formation of a plexiform arterial network.1,2,4) Since the vessel walls of these arteries are fragile, flow-related aneurysms are formed and have a risk of rupture due to the continuous hemodynamic stress.5) However, little is known about the aneurysmal formation in the twig-like vessels. We report a case of Ap/T-MCA presented with intracerebral hemorrhage caused by aneurysm rupture and discuss the process of aneurysm formation and rupture in Ap/T-MCA from the angiographic and histological perspective.
Case Report
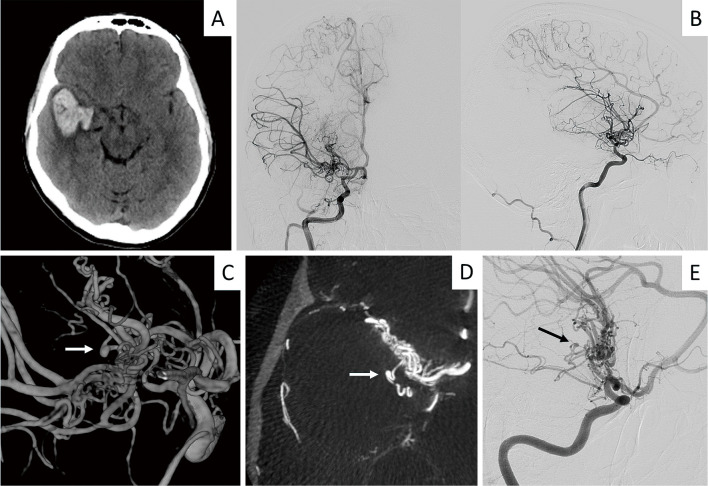
A previously healthy 38-year-old man presented with a sudden onset of severe headache and visual hallucinations. Computed tomography revealed a subcortical hematoma in the right temporal lobe (Fig. 1A). On examination, he was oriented but mildly drowsy with left hemianopia and no extremity weakness. Cerebral angiography showed “twig-like” vessels on M1 segment (Ap/T-MCA) arising from A1 segment of the anterior cerebral artery (ACA) with normal distal vasculature. MCA cerebral blood flow (CBF) was delayed due to the M1 stenosis. Leptomeningeal anastomoses from ACA were present (Fig. 1B). Three-dimensional rotational angiography and slab maximum intensity projection images of rotational angiography revealed a 1.9 × 1.9 mm aneurysm at a nonbranching point of the twig-like vessel deep in the hematoma, and the aneurysm is visualized at an oblique cerebral angiography view (Fig. 1C-E). The patient underwent a right pterional craniotomy to prevent rebleeding. After hematoma removal, the aneurysm was visualized on the surgical cavity rim; no other bleeding points were identified. The aneurysmal wall comprised dark red hematoma covered by a thin wall, thus appearing as a pseudoaneurysm. The aneurysm was trapped by applying clips to the feeding and draining arteries and then resected (Fig. 2A).
Fig. 1.
A) A parenchymal hematoma in the right temporal lobe was seen on computed tomography. B) Cerebral angiography showed “twig-like” vessels of the M1 segment arising from A1 segment of the anterior cerebral artery with normal vessels distally. Pial anastomoses from the anterior cerebral artery were present, indicating insufficient blood supply from the middle cerebral artery. C) Three-dimensional rotational angiography showed a 1.9 × 1.9 mm aneurysm (white arrow) at a non-branching point of the twig-like vessel. D) Slab maximum intensity projection (MIP) images of rotational angiography showed the aneurysm (white arrow) located deep in the hematoma and arose from a tortuous segment of a “twig-like” vessel. E) The aneurysm (black arrow) is clearly visualized at an oblique cerebral angiography view.
Fig. 2.
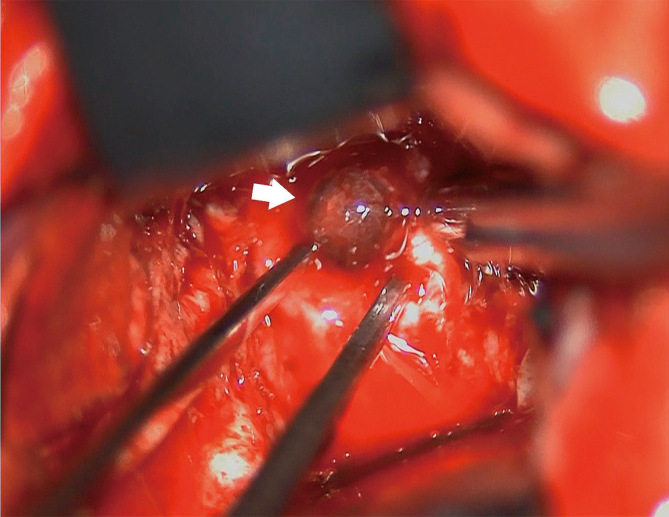
An intraoperative photograph shows the aneurysm (white arrow). The aneurysmal wall consisted of dark red hematoma covered by a thin fibrous wall and appeared to be a pseudoaneurysm associated with arterial dissection.
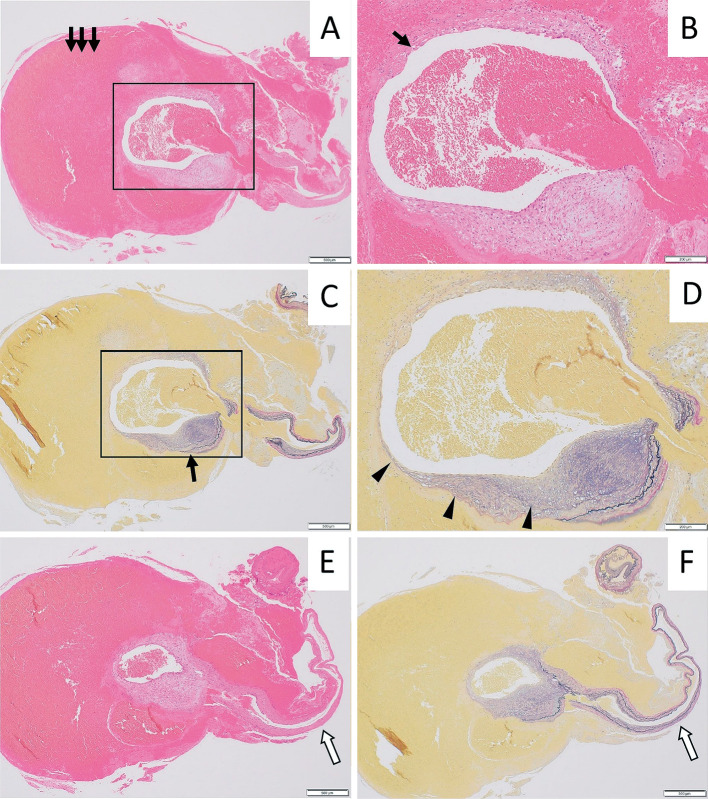
On histopathological examination, hematoxylin and eosin staining revealed a small aneurysmal dome with thick hematoma (Fig. 3A), which was observed like pseudoaneurysm intraoperatively, and a thin smooth muscle cell layer (Fig. 3B). Elastica van Gieson staining revealed an internal elastic lamina (IEL) disruption in the aneurysm neck and a thin aneurysmal wall with hematoma outside the outer layers of the arterial wall (Fig. 3C). Higher magnification revealed a thickened intima with disrupted IEL in the aneurysmal neck, which is formed by long-term wall share stress, and a thin intima in an aneurysmal dome (Fig. 3D). Hematoxylin and eosin staining and Elastica van Gieson staining of the parent artery revealed a normal vascular structure, and there are no abnormal histological findings, such as intimal thickness, tunica media thinning, or IEL tortuosity (Fig. 3E, F).
Fig. 3.
A) A thick hematoma (arrows) was observed within the aneurysmal wall (hematoxylin and eosin (HE) staining, ×40). B) The smooth muscle cell layer was prominently thin (arrow) (HE staining, ×100). C) The internal elastic lamina (IEL) was disrupted in the aneurysm neck (arrow) and an mural hematoma was seen adjacent to layers of the arterial wall (Elastica van Gieson (EVG) staining, ×40). D) Higher magnification showed that the thickened intima in the neck became extremely thin (arrowheads) and without IEL in the aneurysmal wall (EVG staining, ×100). E, F) The parent artery of aneurysm (white arrow) showed a normal vascular structure with no tunica media thinning or tortuosity of the internal elastic lamina (HE staining, ×40 and EVG staining, ×40).
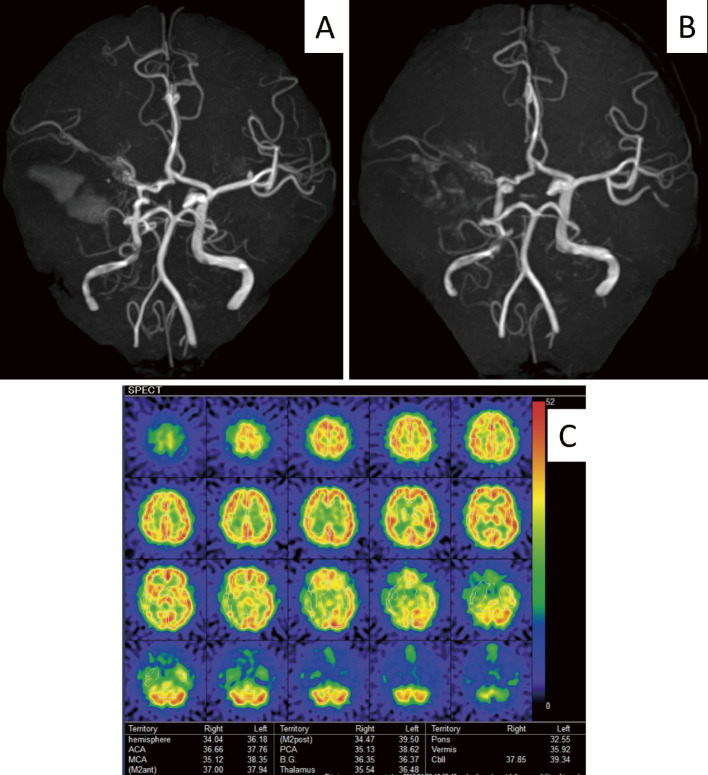
The patient recovered well after surgery and required rehabilitation due to visual disturbance and speech disorder. Compared to preoperative MRA (Fig. 4A), postoperative MRA (Fig. 4B) showed no obvious intensity decrease on the distal MCA area. Follow-up single photon emission computed tomography (SPECT) revealed no significant reduction of CBF on the affected side, other than the hematoma area (Fig. 4C). No hemodynamic or ischemic event has occurred in 2 years of follow-up.
Fig. 4.
A) Preoperative MRA showed decreased signal intensity on the right MCA area, B) which was not further affected postoperatively. C) Follow-up single photon emission computed tomography (SPECT) showed no significant reduction of CBF on the affected side other than the area of hematoma.
Discussion
Most articles on Ap/T-MCA were published from East Asia, such as Korea and Japan.2,6,7) The pathogenesis of Ap/T-MCA is not yet well known. During embryonic development, the trunk of the MCA is formed by the fusion and regression of numerous plexiform arterial twigs that arise just distal to the anterior choroidal artery.4) Authors speculated that Ap/T-MCA might result from interruption during the MCA evolution.1,2,5,8) The most important consideration in the differential diagnosis of Ap/T-MCA is MMD.1,3-5,7) MMD typically presents with progressive steno-occlusion of the arteries of the circle of Willis, particularly the terminal portion of the internal cerebral artery and the proximal MCA and ACA, which are associated with unusual collaterals (moyamoya vessels).9,10) The shared angiographic features with Ap/T-MCA include steno-occlusive lesion of the MCA, plexiform arterial network with perforators, and normal cortical branches beyond the occluded MCA trunk.1,4) In our case, the Ap/T-MCA was unilateral and confined to the M1 segment with normal cortical branches without associated moyamoya vessels.
Since the aneurysm was located on an elongated tortuous vessel, we presume that it was formed due to increased hemodynamic stress, and the histological findings suggested that the hemorrhage source was the aneurysm associated with the Ap/T-MCA. Shin et al. proposed that hemodynamic stress on the twig-like fragile vessels induces a flow-related aneurysm and subsequent rupture.5) Hemodynamic stress and wall shear stress (WSS) may contribute to the formation and rupture of Ap/T-MCA-associated aneurysms as in saccular aneurysms.11) In our case, we speculated that a flow-related aneurysm was formed in a tortuous and aplastic/twig-like vessel of MCA due to WSS, and that an aneurysm was ruptured after intima and media thinning and IEL disruption. On the parent artery of a cerebral aneurysm, an obvious abnormal vessel structure was not seen. Intimal thickening, tunica media thinning, and IEL tortuosity seen in Moyamoya disease are not prominent.
Previously, only one pathological finding of Ap/T-MCA-associated aneurysm was reported. The parent artery of the previously reported case had a similar vascular structure with that of our case, but there is no information about the cause of intracerebral hemorrhage. Our case report revealed that the cause of hemorrhage is a rupture of flow-related aneurysm arising from “twig-like” vessels on M1 segment (Ap/T-MCA).12) However, in the mother vessel on the proximal side of the aneurysm, there is evidence of stratification of the intimal elastic plate, and the intimal elastic plate is disrupted with intimal thickening at the aneurysm neck (disruption and laceration). These findings are caused by prolonged WSS to the medial elastic plate. After a flow-related aneurysm with intimal elastic plate rupture occurred, the intimal thickening of the aneurysm neck progressed due to the repair process of the aneurysm wall (healing process), but the aneurysm wall ruptured at the aneurysm dome where the arterial wall became thinner, causing cerebral hemorrhage. Such a cerebral aneurysm is called a dissecting cerebral aneurysm or pseudoaneurysm.13,14) The RNF213 p.R 4810K gene polymorphism has been associated with intracranial steno-occlusive cerebrovascular disease, including Moyamoya disease.15,16) Fukuyama et al. reported a case of Ap/T-MCA with heterozygous mutation of RNF213 (c.14429 G>A p.R4810K)17); however, there are no clinical studies to clarify the clinical significance of Ap/T-MCA with heterozygous mutation of RNF213. In our case, RNF213 p.R 4810K gene polymorphism has not been evaluated, and clinical research of gene analysis and follow-up are needed to evaluate the pathogenesis of Ap/T-MCA and RNF213.
Ap/T-MCA can present with hemorrhagic stroke in 27%-40% and ischemic stroke in 33%-46% cases.1,2,8) Among hemorrhagic strokes due to Ap/T-MCA, 26.6%-46% are caused by aneurysmal rupture.8,18) Ruptured Ap/T-MCA-associated aneurysms have been successfully treated via endovascular coil embolization and surgical clipping.3,5,6,8,18,19) Additionally, direct bypass surgery for patients with hemorrhagic stroke has reportedly shown satisfactory outcomes and reduction of abnormal “twig-like” vasculature.12,19) Direct bypass surgery in patients with an Ap/T-MCA may decrease hemodynamic stress on the fragile vessels and increase CBF, preventing future hemorrhagic and ischemic events12,19-22) as in MMD.23-25) In our case, CBF delay was observed before surgery in the MCA territory. After successful aneurysm trapping and resection, cortical CBF was not significantly decreased, except for the hematoma area. If follow-up magnetic resonance imaging or CBF-SPECT reveals a de novo aneurysm arising from the abnormal “twig-like” vasculature or decreased CBF in the MCA territory, revascularization surgery should be considered.
Conclusion
We presented a case of Ap/T-MCA-associated aneurysm rupture. Histological analysis of a resected aneurysm showed a prominently thin aneurysmal wall and disrupted IEL in the aneurysmal neck. The cause of aneurysmal formation and rupture was speculated to be a flow-related aneurysm with long-term WSS in a tortuous and aplastic or twig-like vessel of MCA. Long-term follow-up should be done to detect a de novo aneurysm and a cerebral ischemic event related to the abnormal “twig-like” vasculature.
Ethics Declarations
The current study has been performed in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of University of Tsukuba Hospital (registration number: R01-216). Informed consent was obtained from the patient.
Conflicts of Interest Disclosure
The authors declare no conflicts of interest associated with this manuscript. Authors who are members of the Japan Neurosurgical Society have registered online Self-reported COI Disclosure Statement Forms.
Acknowledgments
This work was supported by JSPS KAKENHI Grant-in-Aid for Scientific Research (C) under Grant Number JP17K10819 and Grant-in-Aid for Scientific Research (B) No. 20H03787.
The authors thank Crimson Interactive Japan Co., Ltd. for native English revision.
References
- 1). Akkan K, Ucar M, Kilic K, Celtikci E, Ilgit E, Onal B: Unfused or twig-like middle cerebral artery. Eur J Radiol 84: 2013-2018, 2015 [DOI] [PubMed] [Google Scholar]
- 2). Cho KC, Kim JJ, Jang CK, Hong CK, Joo JY, Kim YB: Rete middle cerebral artery anomalies: a unifying name, case series, and literature review. J Neurosurg 131: 453-461, 2018 [DOI] [PubMed] [Google Scholar]
- 3). Liu HM, Lai DM, Tu YK, Wang YH: Aneurysms in twig-like middle cerebral artery. Cerebrovasc Dis 20: 1-5, 2005 [DOI] [PubMed] [Google Scholar]
- 4). Uchiyama N: Anomalies of the middle cerebral artery. Neurol Med Chir (Tokyo) 57: 261-266, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Shin HS, Lee SH, Ryu CW, Koh JS: Flow-related intracranial aneurysms associated with unfused arterial twigs relevant to different vascular anomalies: embryologic and hemodynamic considerations. Acta Neurochir (Wien) 156: 1637-1646, 2014 [DOI] [PubMed] [Google Scholar]
- 6). Fukuda Y, Matsunaga Y, Hirayama K, et al. : A case of aplastic or twig-like middle cerebral artery associated with a ruptured A1 aneurysm at the origin of the anomalous collateral artery. Jpn J Stroke 40: 75-80, 2018 [Google Scholar]
- 7). Goto Y, Oka H, Hiraizumi S, et al. : Aplastic or twig-like middle cerebral artery presenting with intracerebral hemorrhage during pregnancy: report of two cases. World Neurosurg X 2: 100018, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Seo BS, Lee YS, Lee HG, Lee JH, Ryu KY, Kang DG: Clinical and radiological features of patients with aplastic or twiglike middle cerebral arteries. Neurosurgery 70: 1472-1480, 2012 [DOI] [PubMed] [Google Scholar]
- 9). Takahashi JC, Miyamoto S: Moyamoya disease: recent progress and outlook. Neurol Med Chir (Tokyo) 50: 824-832, 2010 [DOI] [PubMed] [Google Scholar]
- 10). Yamamoto S, Kashiwazaki D, Uchino H, et al. : Clinical and radiological features of childhood onset adult Moyamoya disease: implication for hemorrhagic stroke. Neurol Med Chir (Tokyo) 60: 360-367, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Chalouhi N, Hoh BL, Hasan D: Review of cerebral aneurysm formation, growth, and rupture. Stroke 44: 3613-3622, 2013 [DOI] [PubMed] [Google Scholar]
- 12). Inoue A, Kohno K, Fukumoto S, et al. : [A case of ECA-MCA double anastomoses for hemorrhagic type of twig-like MCA]. No Shinkei Geka 44: 463-471, 2016(Japanese) [DOI] [PubMed] [Google Scholar]
- 13). Mizutani T, Kojima H, Asamoto S: Healing process for cerebral dissecting aneurysms presenting with subarachnoid hemorrhage. Neurosurgery 54: 342-347, 2004 [DOI] [PubMed] [Google Scholar]
- 14). Mizutani T, Miki Y, Kojima H, Suzuki H: Proposed classification of nonatherosclerotic cerebral fusiform and dissecting aneurysms. Neurosurgery 45: 253-259, 1999 [DOI] [PubMed] [Google Scholar]
- 15). Kamada F, Aoki Y, Narisawa A, et al. : A genome-wide association study identifies RNF213 as the first Moyamoya disease gene. J Hum Genet 56: 34-40, 2011 [DOI] [PubMed] [Google Scholar]
- 16). Liu W, Morito D, Takashima S, et al. : Identification of RNF213 as a susceptibility gene for Moyamoya disease and its possible role in vascular development. PLOS ONE 6: e22542, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Fukuyama R, Yamamura K, Murata H, Miyatake S, Matsumoto N, Abe H: [Ruptured aneurysm of an aplastic or twig-like middle cerebral artery with ring finger protein 213 mutation: a case report]. No Shinkei Geka 48: 533-540, 2020(Japanese) [DOI] [PubMed] [Google Scholar]
- 18). Miura S, Katsube T, Nakamizo S, Sakagami Y: [A case of aplastic or twig-like middle cerebral artery with a ruptured aneurysm at an anomalous collateral artery]. Brain Nerve 70: 1033-1036, 2018(Japanese) [DOI] [PubMed] [Google Scholar]
- 19). Seno T, Kohno K, Tanaka H, et al. : [A case of ruptured distal anterior choroidal artery aneurysm associated with a twig-like middle cerebral artery, treated with single-stage aneurysm clipping and STA-MCA double anastomoses in the acute phase]. No Shinkei Geka 45: 691-697, 2017(Japanese) [DOI] [PubMed] [Google Scholar]
- 20). Sakai K, Hiu T, Fukuda Y, et al. : [A rare case of a ruptured de novo aneurysm arising from the twig-like networks of an anomalous collateral artery associated with hypoplasia of the M1 segment of the middle cerebral artery 4 years after the rupture of an A1 aneurysm at the origin of the collateral artery]. No Shinkei Geka 46: 713-722, 2018(Japanese) [DOI] [PubMed] [Google Scholar]
- 21). Uchiyama T, Okamoto H, Koguchi M, Tajima Y, Suzuyama K: [A case of aplastic or twig-like middle cerebral artery presenting with an intracranial hemorrhage two years after a transient ischemic attack]. No Shinkei Geka 44: 143-148, 2016(Japanese) [DOI] [PubMed] [Google Scholar]
- 22). Matsunaga Y, Izumo T, Morofuji Y, Horie N, Hayashi K, Matsuo T: Revascularization for aplastic or twiglike middle cerebral artery: a case report. J Stroke Cerebrovasc Dis 27: e78-e79, 2018 [DOI] [PubMed] [Google Scholar]
- 23). Cho WS, Kim JE, Kim CH, et al. : Long-term outcomes after combined revascularization surgery in adult moyamoya disease. Stroke 45: 3025-3031, 2014 [DOI] [PubMed] [Google Scholar]
- 24). Miyamoto S, Yoshimoto T, Hashimoto N, et al. : Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan Adult Moyamoya Trial. Stroke 45: 1415-1421, 2014 [DOI] [PubMed] [Google Scholar]
- 25). Morimoto M, Iwama T, Hashimoto N, Kojima A, Hayashida K: Efficacy of direct revascularization in adult Moyamoya disease: haemodynamic evaluation by positron emission tomography. Acta Neurochir (Wien) 141: 377-384, 1999 [DOI] [PubMed] [Google Scholar]