Abstract
Background
Acute appendicitis (AA) is one of the most common emergencies in general surgery worldwide. During the pandemic, a significant decrease in the number of accesses to the emergency department for AA has been recorded in different countries. A systematic review of the current literature sought to determine the impact of Coronavirus Disease 2019 (COVID-19) on hospital admissions and complications of AA.
Method
A systematic search was undertaken to identify repeated cross-sectional studies reporting the management of AA during the COVID-19 pandemic (index period) as compared to the previous year, or at the turn of lockdown (reference period). Data were abstracted on article (country of origin) and patients characteristics (adults, children [i.e. non adults, <18-year-old]), or mixed population) within the two given timeframes, including demographics, number of admissions for AA, number of appendectomies, and complicated appendectomies.
Results
Of 201 full-text articles assessed for eligibility, 54 studies from 22 world countries were included. In total, 27 (50%) were conducted on adults, 12 (22%) on children, and 15 (28%) on a mixed patients population. The overall rate ratio of admissions for AA between the two periods was 0.94 (95%CI, 0.75-1.17), with significant differences between studies on adults (0.90 [0.74-1.09]), mixed population (0.50 [0.27-0.90]), and children (1.50 [1.01-2.22]). The overall risk ratio of complicated AA was 1.65 (1.32-2.07), ranging from 1.32 in studies on children, to 2.45 in mixed population.
Conclusion
The pandemic has altered the rate of admissions for AA and appendectomy, with parallel increased incidence of complicated cases in all age groups.
Keywords: COVID-19, SARS-CoV-2, Acute appendicitis, Appendectomy
Two sentence summary
This systematic review identified 54 studies reporting on the management of acute appendicitis (AA) in the COVID-19 era. Our findings indicate that the effect of the pandemic on the rate of admissions for AA was different over age groups (i.e. declined in adults and increased in children), as opposed to an ubiquitous increase in complicated cases.
Introduction
Acute appendicitis (AA) is one of the most common emergencies in general surgery worldwide, with an incidence rate of 90–100 patients per 100,000 inhabitants per year in developed countries, and an estimated lifetime risk of 7–8% [1].
Appendectomy has long been the gold standard for treatment of AA. However, the use of antibiotic therapy as an alternative to surgery is enshrined in current guidelines [2], as supported by several high-quality studies. In a very recent trial, antibiotics were noninferior to appendectomy on the basis of results of a standard health-status measure [3].
AA has been traditionally regarded as a progressing disease, with a significant risk of perforation. However, a selection bias due to spontaneous resolution of non-perforated cases has vitiated this long-lasting assumption. Indeed, there is an increasing body of evidence suggesting a relationship between perforation and the pre-hospital (rather than in-hospital) delay [4].
During the Coronavirus Disease 2019 (COVID-19) pandemic, a significant decrease in the number of accesses to the emergency department (ED) for AA has been recorded in many institutions from different countries. The management of AA has become more challenging for surgeons facing hospital bed shortages and resource reallocation [5,6]. Non-operative management in the setting of COVID-19 has been advocated as a safe, short-term alternative to surgery with acceptably low failure and complication rates [7]. In this scenario, it remains unclear whether the increasing delay between the onset of symptoms and medical consultation has worsened outcomes in these patients.
Therefore, a systematic review of the current literature sought to determine the impact of COVID-19 on changes in the number of hospital admissions for AA and complicated cases.
Materials and methods
A systematic review was performed according to a predefined protocol. The study is reported in line with the PRISMA 2020 statement (Supplementary Table 1) [8].
A systematic search was undertaken to identify published articles relating to the management of patients with AA during the COVID-19 pandemic.
To be included in the review, papers needed to compare the number of admissions for AA and/or appendectomies within two time periods (i.e. repeated cross-sectional studies): (1) during the COVID-19 pandemic (index period), as compared to the previous year, or at the turn of lockdown (reference period). The latter may refer to the period shortly after or at the turn of lockdown, depending on studies. Only studies with full text in the English language were included. A minimum population sample of 20 patients in the index period was imposed for eligibility. Papers were excluded if they did not fit into the conceptual framework of the study.
To identify potentially relevant documents, the following bibliographic databases were searched from 1 December 2019 to 05 March 2021: MEDLINE, Embase, Scopus, Web of Science, and MedxRiv (including preprint publications). The final search strategy for each database is showed in Supplementary Table 2.
Two reviewers (MO and MP) sequentially evaluated the titles, abstracts and full text of all publications identified by our searches for potentially relevant studies. Any disagreements on study selection and data extraction were resolved by consensus and discussion with other authors (UG and GG).
A single investigator (NS) charted all data from eligible papers using a semi-structured charting pro-forma designed for the purpose of this study. Three other researchers verified the data for accuracy (UG, MO, MP and GG).
Data were abstracted on article (country of origin) and patients characteristics (adults, children [i.e. non adults, <18-year-old], or mixed population) within the two given study periods (in number of days), including demographics, number of admissions for AA, number of appendectomies, duration of symptoms (in days) prior to hospital admission, surgical approach (i.e. laparoscopic vs. open), perforated or complicated AA (intra-operative finding, defined as peritonitis, abscesses, or perforated AA), and length of stay. The number of COVID-19 active cases per million people on the day in the middle of the index period in the country where each study was conducted was also extrapolated.
Assessments of study quality was undertaken according to the Johanna Briggs Institute appraisal tool for analytical cross-sectionals studies [9]. Two reviewers (UG and NS) independently performed the risk of bias evaluation and categorized the included articles as ‘high risk’ when the study bias rating ‘yes’ score was between 0% and 49%, ‘moderate risk’ when the study ‘yes’ score was between 50% and 69%, and ‘low risk’ when the study ‘yes’ score was above 70%. Any disagreement was resolved by consensus with a third author (GG). A quantitative synthesis of data collected from eligible papers is presented and stratified by population (i.e. adults, children, or mixed).
Statistical analysis
A Hartung-Knapp-Sidik-Jonkman random effects meta-analysis allowed to pool the rate ratios of admissions for AA and appendectomies, and to compare rates between the pandemic and the matched pre-pandemic periods. Complications over the number of appendectomies were assessed across the two periods and pooled as risk ratios. Quantitative heterogeneity was determined by conducting a formal test of homogeneity and evaluating the proportion of variability due to heterogeneity (I2). Subgroup analyses were performed by type of population, i.e. adults, children, and mixed. Regression-based Egger test and eyeball evaluation of the contour-enhanced funnel plots were used to determine small-study effects.
The prediction intervals were reported along with pooled results (with 95% confidence intervals [CI])[10] to show the range of true rate and risk ratios that can be expected in future studies.
All statistical analyses were performed using Stata 16 (StataCorp LLC, College Station, TX, USA).
Results
Selection of sources of evidence
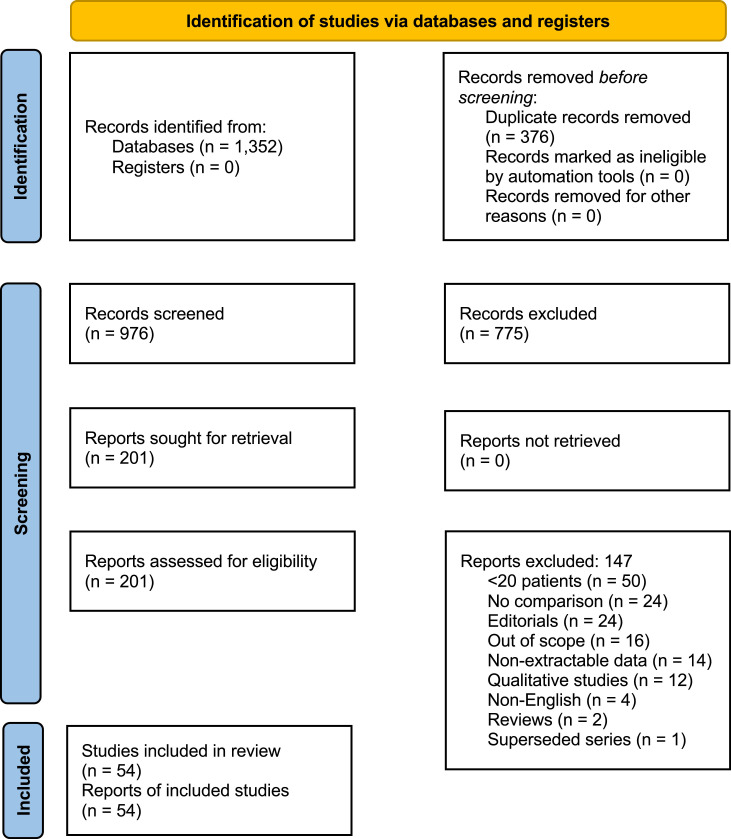
After 376 duplicates were removed, a total of 976 citations were identified from searches of electronic databases and review article references. Based on the title and the abstract, 775 were excluded, with 201 full text articles to be retrieved and assessed for eligibility. Of these, 147 were excluded, with 54 repeated cross-sectional studies from 22 world countries considered eligible for this review (Fig. 1 ). In total, 27 (50%) were conducted on adults (Table 1 ), 12 (22%) on children (Table 2 ), and 15 (28%) on a mixed patients’ population (Table 3 ).
Fig. 1.
Prisma diagram
Table 1.
Cross sectional studies comparing the number of admissions for acute appendicitis in the adult population
| Author | Country | Index period |
Pre-pandemic period |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. COVID cases per 106 people at mid index period^ | No. days | No. patients | Age* | Perforated or complicated# | No. days | No. patients | Age* | Perforated or complicated# | ||
| Allen [22] | New Zealand | 189 | 72 | 75 | NR | NR | 72 | 68 | NR | NR |
| Angeramo [23] | Argentina | 490 | 150 | 60 | 37 | 38% | 150 | 142 | 39 | 19% |
| Antakia [24] | United Kingdom | 2,637 | 115 | 91 | 38.2 | 20% | 129 | 116 | 40.3 | 20% |
| Anteby [25] | Israel | 1 | 60 | 33 | NR | NR | 60 | 22 | NR | NR |
| Aviran [26] | Israel | 499 | 29 | 42 | NR | NR | 29 | 31 | NR | NR |
| Baral [27] | Nepal | 2 | 90 | 50 | 32.3 | 21% | 90 | 42 | 30.2 | 16% |
| Butt [28] | Qatar¶ | 140 | 30 | 92 | NR | NR | 30 | 113 | NR | NR |
| English [29] | United Kingdom¶ | 1,279 | 40 | 79 | NR | NR | 24 | 63 | NR | NR |
| Fallani [11] | Italy¶ | 1,717 | 41 | NR | NR | NR | 41 | NR | NR | NR |
| Finkelstein [30] | United States | 2,098 | 55 | 48 | 44 | 37% | 55 | 59 | 41 | 18% |
| Fonseca [20] | Turkey | 718 | 61 | 42 | NR | 43% | 61 | 155 | NR | 19% |
| Gao [31] | China | 25 | 119 | 58 | 42.8 | NR | 210 | 105 | 41.6 | NR |
| Goksoy [32] | Turkey | 759 | 60 | 45 | NR | 20% | 60 | 48 | NR | 10% |
| Griffith [33] | United States | 1,726 | 29 | 21 | NR | NR | 29 | 13 | NR | NR |
| Ho [34] | China | 8 | 179 | 188 | 43.7 | 46% | 179 | 160 | 44.6 | 41% |
| Honeyford [35] | United Kingdom | 641 | 26 | 41 | NR | NR | 26 | 144 | NR | NR |
| Mathur [36] | Singapore | 6 | 58 | 61 | NR | NR | 58 | 44 | NR | NR |
| McGuinness [37] | New Zealand | 185 | 31 | 39 | NR | NR | 33 | 49 | NR | NR |
| Neufeld [38] | United States¶ | 1,602 | 65 | 91 | 38.4 | 30% | 99 | 840 | 37.3 | 25% |
| O'Connell [39] | Ireland | 2,452 | 59 | 24 | NR | NR | 59 | 35 | NR | NR |
| Patel [40] | United States | 2,180 | 76 | 75 | NR | 45% | 76 | 111 | NR | 22% |
| Perea del Pozo [41] | Spain | 1,248 | 36 | 20 | NR | NR | 36 | 42 | NR | NR |
| Romero [42] | Colombia | 48 | 41 | 25 | 36.6 | NR | 41 | 42 | 38.2 | NR |
| Surek [43] | Turkey | 718 | 61 | 42 | NR | 43% | 61 | 155 | NR | 19% |
| Turanli [44] | Turkey | 638 | 90 | NR | NR | 26% | 90 | NR | NR | 29% |
| Wang [19] | United States | 8 | 105 | 32 | 24.8 | 31% | 105 | 48 | 27.3 | 13% |
| Wichmann [45] | Germany | 533 | 75 | 46 | 38.5 | 47% | 75 | 43 | 42.7 | 30% |
NR: not reported
Reported as mean or median across studies
Data extrapolated in each country from www.worldometers.info/coronavirus/
As a percentage of appendectomies
Multicenter
Table 2.
Cross sectional studies comparing the number of admissions for acute appendicitis in the pediatric population
| Author | Country | Index period |
Pre-pandemic period |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. COVID cases per 106 people at mid index period^ | No. days | No. patients | Age* | Perforated or complicated# | No. days | No. patients | Age* | Perforated or complicated | ||
| Bonilla [46] | Spain | 1,643 | 60 | 49 | 9.2 | 33% | 60 | 41 | 9.2 | 34% |
| Fisher [47] | United States¶ | 873 | 66 | 55 | 10 | 50% | 1,800 | 1,291 | 10.7 | 27% |
| Gaitero Tristán [15] | Spain | 1,698 | 45 | 77 | 10.7 | 39% | 240 | 74 | 10.5 | 28% |
| Gerall [48] | United States | 1,726 | 90 | 48 | 11.1 | 19% | 90 | 41 | 13.1 | 11% |
| Kvasnovsky [49] | United States | 1,783 | 33 | 55 | 12.4 | 43% | 33 | 41 | NR | 32% |
| La Pergola [50] | Italy¶ | 707 | 60 | 86 | 10 | 31% | 60 | 92 | 10 | 25% |
| Lee-Archer [12] | Australia | 216 | 49 | 48 | NR | 48% | 49 | 57 | NR | NR |
| Montalva [51] | France | 1,405 | 54 | 69 | 11.1 | 74% | 56 | 39 | 8.9 | 85% |
| Pines [52] | United States¶ | 11 | 179 | 921 | NR | NR | 179 | 1,144 | NR | NR |
| Place [53] | United States | 2,477 | 81 | 90 | 10 | 43% | 81 | 70 | 11 | 19% |
| Raucci [46] | Italy¶ | 953 | 69 | 61 | NR | 28% | 69 | 57 | NR | 44% |
| Velayos [54] | Spain | 1,766 | 46 | 25 | 9.3 | 32% | 73 | 41 | 10.7 | 7% |
NR: not reported
Reported as mean or median across studies
Data extrapolated in each country from www.worldometers.info/coronavirus/
As a percentage of appendectomies
Multicenter
Table 3.
Cross sectional studies comparing the number of admissions for acute appendicitis in a mixed population of children and adults
| Author | Country | Index period |
Pre-pandemic period |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. COVID cases per 106 people at mid index period^ | No. days | No. patients | Age* | Perforated or complicated# | No. days | No. patients | Age* | Perforated or complicated | ||
| Bajomo [55] | United Kingdom | 1,222 | 60 | 36 | 26.5 | 29% | 60 | 42 | 30.5 | 21% |
| Baugh [56] | United States¶ | 611 | 59 | 150 | NR | NR | 59 | 191 | NR | NR |
| Burgard [57] | Switzerland¶ | 712 | 84 | 65 | 29 | 52% | 84 | 241 | 30 | 8% |
| Ganesh [58] | United Kingdom | 1,407 | 414 | 32 | 37 | NR | 139 | 64 | 37 | NR |
| Mai [59] | United Kingdom | 1,916 | 61 | 39 | 34.4 | 61% | 62 | 50 | 29.1 | 38% |
| Maneck [60] | Germany¶ | 841 | 40 | 2,914 | 34.5 | NR | 42 | 3591 | 32.7 | NR |
| Meriç [61] | Turkey | 680 | 60 | 40 | 34 | 18% | 60 | 110 | 29.1 | 6% |
| Orthopoulos [62] | United States | 1,100 | 44 | 37 | 27 | 31% | 44 | 54 | 23 | 8% |
| Steinman [63] | Brazil¶ | 439 | 99 | 160 | NR | NR | 441 | 706 | NR | NR |
| Tankel [64] | Israel¶ | 21 | 48 | 141 | 23.3 | 22% | 48 | 237 | 23.1 | 15% |
| Toale [65] | Ireland | 1,158 | 65 | 62 | 27.1 | 38% | 84 | 122 | 21.9 | 10% |
| Verma [66] | India | 38 | 97 | 91 | NR | 28% | 97 | 126 | NR | NR |
| Walker [67] | United States¶ | 14 | 72 | 73 | NR | NR | 34 | 140 | NR | NR |
| Willms [5] | Germany¶ | 721 | 69 | 888 | 36 | 64% | 69 | 1027 | 35 | 58% |
| Zhou [68] | China | 26 | 64 | 81 | 40.9 | 19% | 64 | 121 | 37.7 | 8% |
NR: not reported
Reported as mean or median across studies
Data extrapolated in each country from www.worldometers.info/coronavirus/
As a percentage of appendectomies
Multicenter
Of the included studies, 15 (28%) were multicenter. Gender prevalence was available from 31/54 (57%) studies, with a slight male prevalence across the three groups of study population in both periods (median index period, 58% [interquartile range limits, IQRL, 52%-68%]; reference period, 55% [48%-63%]). No substantial differences in age were found between the two study periods across the three groups.
The timing of the outbreak differed in each country at the time of data collection. Indeed, the number of COVID-19 cases ranged from 1 (in Israel) to 2,637 (in the United Kingdom) per 106 people in the middle of the index period (median, 718; IQRL, 174-718), with no major differences across the three study groups of adults, children, and mixed populations.
The duration of symptoms prior to hospital admission (n = 9[17%] studies) and length of stay (n = 14 [26%] studies) were similar between the two periods.
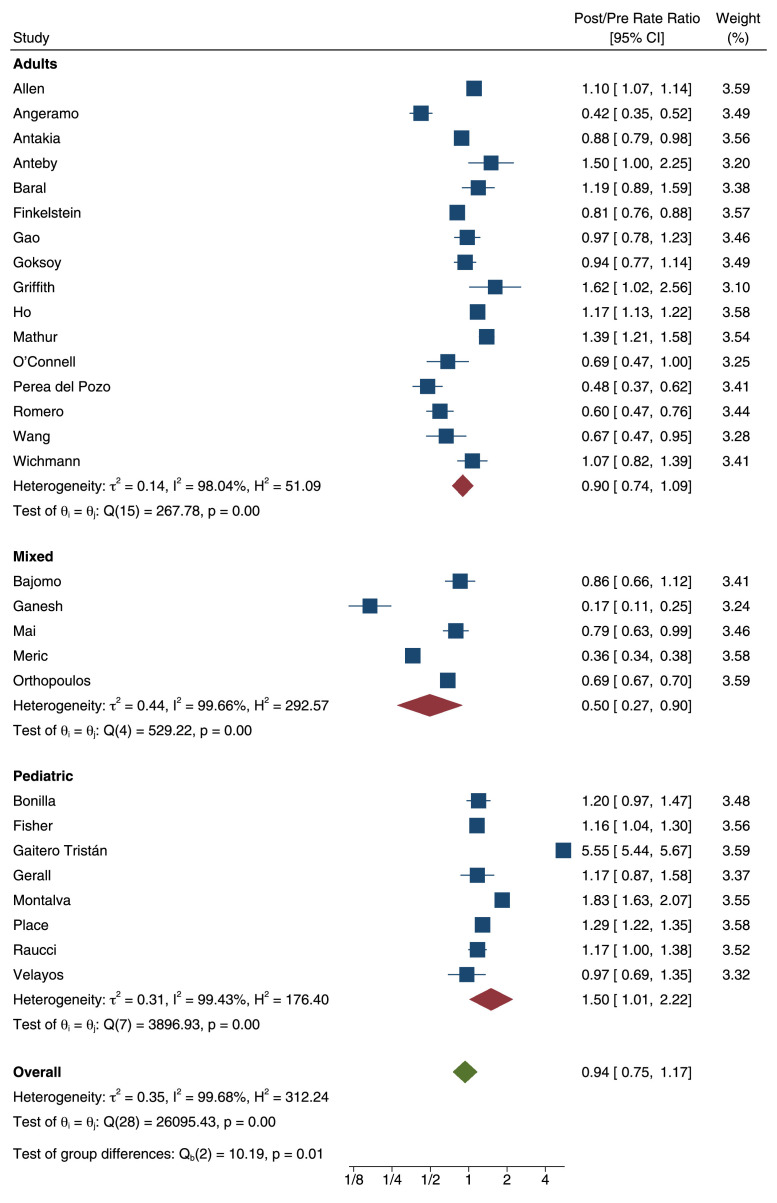
Rate ratio of admissions for AA
The overall rate ratio of admissions for AA between the index and reference periods was 0.94 (95%CI, 0.75-1.17), with statistically significant differences (homogeneity test P<0.0001) between studies on adults (0.90 [0.74-1.09]), mixed population (0.50 [0.27-0.90]), and children (1.50 [1.01-2.22]) (Fig. 2 ). Taking into account the heterogeneity across studies, the 95% prediction interval was 0.27-3.23. No small study effect was observed (P = 0.195; Supplementary Fig. 1).
Fig. 2.
Forest plot showing the overall pooled rate ratio of admissions for acute appendicitis with subgroup analysis according to population included.
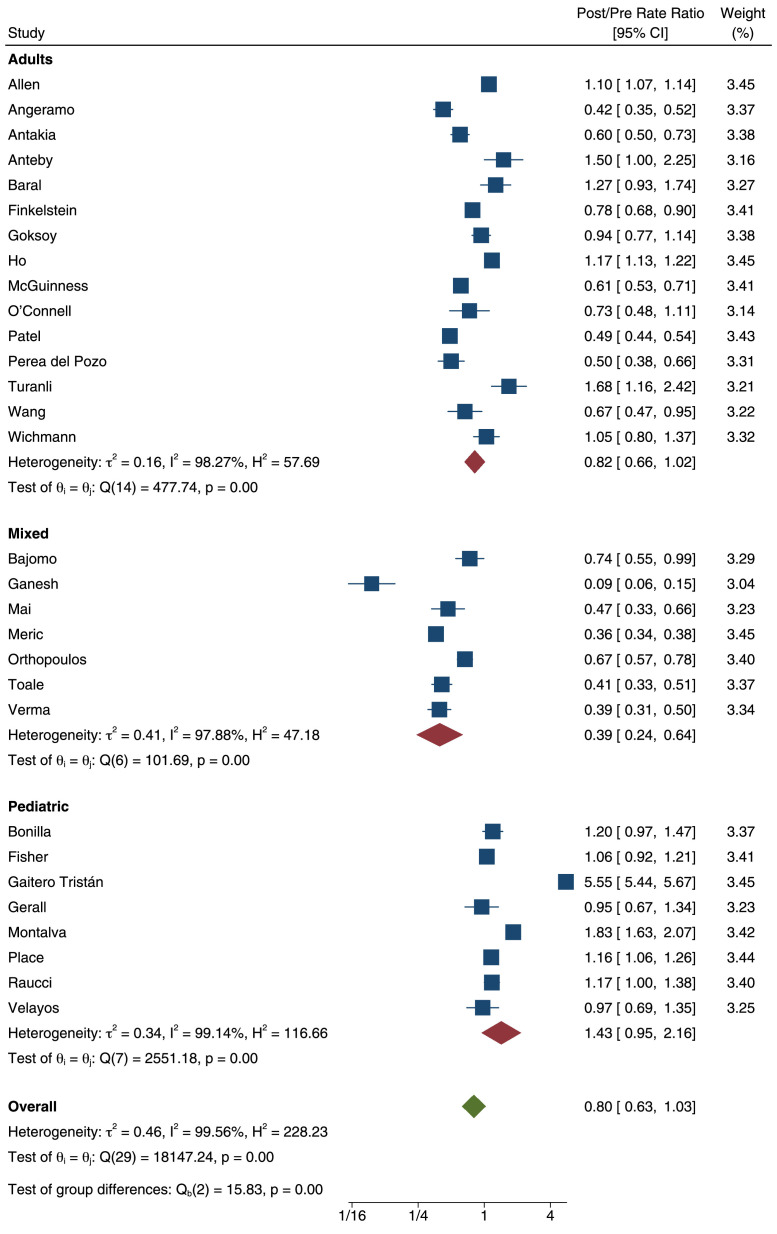
Rate ratio of appendectomies
The overall rate ratio of appendectomies between the index and reference periods was 0.80 (0.63-1.03), with lower estimates in studies on a mixed population (0.39 [0.24-0.64]) and adults (0.82 [0.66-1.02]), compared to children (1.43 [0.95-2.16]) (Fig. 3 ). The 95% prediction interval was 0.195-3.312. Some degree of small study effect was observed (P = 0.062; Supplementary Figure 2).
Fig. 3.
Forest plot showing the overall pooled rate ratio of appendectomies with subgroup analysis according to population included.
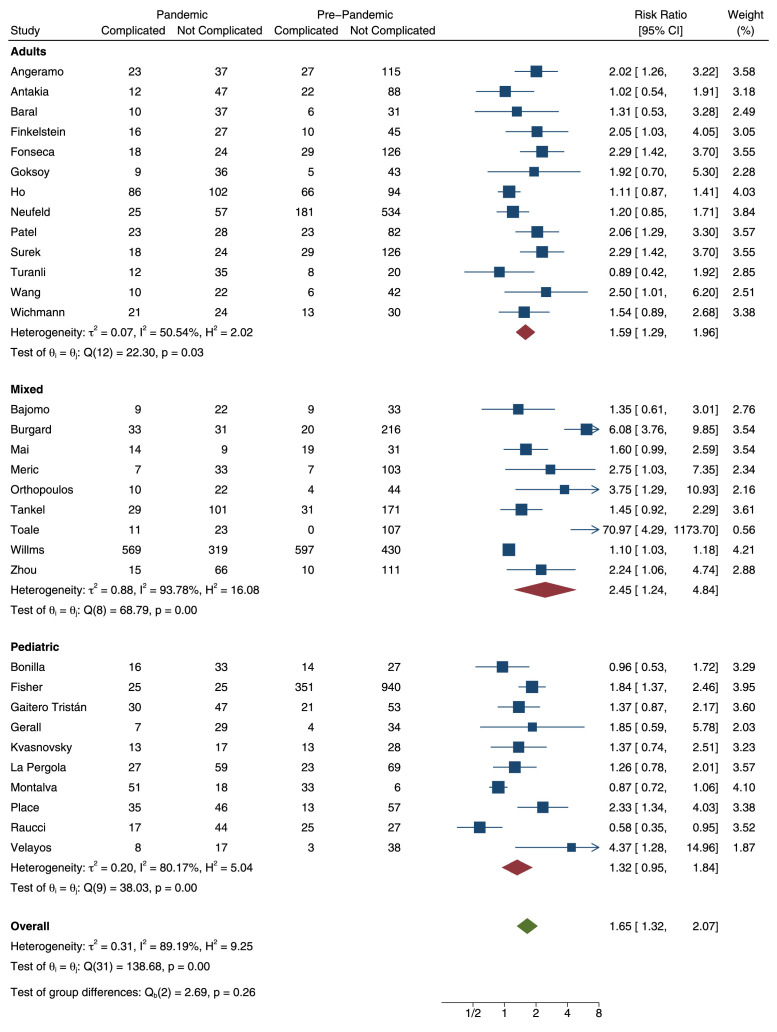
Risk ratio of complicated AA
The overall risk ratio of complicated AA was 1.65 (1.32-2.07), ranging from 1.32 (0.95-1.84) in studies on children, to 1.59 (1.29-1.96) and 2.45 (1.24-4.84) in studies on adults and mixed population, respectively (Fig. 4 ). The 95% prediction interval was 0.515-5.295. A small study effect was found with some asymmetry of the funnel plot (P = 0.004; Supplementary Figure 3).
Fig. 4.
Forest plot showing the overall pooled risk ratio of complicated appendectomies with subgroup analysis according to population included.
The meta-regression showed that the number of COVID-19 cases per million people had a negligible association with the rate ratios of admissions for AA (P = 0.737) and appendectomies (P = 0.883), nor risk ratio of complicated AA (P = 0.847).
Risk of bias within studies
Only 7 articles presented high risk of bias, while the other studies presented low risk of bias. The question which most commonly elevated the risk of bias was ‘Were confounding factors identified?’. More details are provided in Supplementary Figure 4.
Discussion
Summary of evidence
This systematic review identified 54 studies reporting on the management of AA in the COVID-19 era, and published until the beginning of March 2021. Our findings indicate that the effect of the pandemic on the rate of admissions for AA was different over age groups. In accordance with previous series [11,12], a decrease in hospital attendances by 10% was observed in adult patients, although not reaching statistical significance. Beside national lockdowns and isolation measures [13], a further reason behind this decline is likely to be the fear of contracting COVID-19, which may have restrained patients from seeking medical care even in instances of acute illnesses [14]. The striking decline in ED visits worldwide registered the highest peaks in April 2020 in the worst-hit areas by the scourge of the pandemic, marking a dramatic shift in the use of the ED by the public. Our meta-regression showed that COVID-19 cases per million (at mid-pandemic period, per nation) was not associated with any of three pooled outcomes. Several reasons may account for this finding, with the main being considering such measure as an imperfect proxy for burden on the healthcare system, which subsequently affects management patterns.
Nevertheless, AA remained among the top reasons for seeking emergency care even during the pandemic as being one of the most common causes of abdominal pain [13]. However, compared to the pre-pandemic period, the increased rate of admissions for AA observed in the pediatric population was rather unexpected. Such finding may reflect a growing self-awareness of wellbeing that made parents more apprehensive to avoid diagnostic delays [15].
Secondly, a solidly reported curb in surgical activities was observed both in elective and emergency settings [16,17], as a result of decreased hospital attendances and nonemergent surgeries amid lack of resources. Although not reaching statistical significance, this can somehow explain the 18% reduction in appendectomy rate observed in the pandemic period in the adult population. Podda et al [18]. highlighted how surgeons facing hospital services curtailed or suspended have become more keen to consider antibiotic treatment alone in patients with AA. The decline in appendectomies is therefore most likely attributable both to lower number of admissions an.d more active use of antibiotics for uncomplicated AA.
As opposed to the adult population, our meta-analysis showed a 43% increase in the rate of appendectomies in the pediatric counterpart, which mirrors the hike in admission rates for AA in this patients’ group.
On the other hand, the deferred pursuit of medical attention by the adult population may have caused diagnostic delays eventually leading to an increase in the rate of complicated AA (as high as 59% in this group, although not significant). Indeed, a significant increase in the time interval from symptom onset to admission has been reported during the pandemic [19], while other studies overly reported late presentations and complicated disease [20]. Similar figures were observed, although to a lesser extent (32%), in the pediatric population, and became even more pronounced when considering studies on mixed populations.
Nevertheless, a steep decrease in the rate of negative appendectomy was observed during the pandemic [18], likely as consequence of a more accurate selection of surgical candidates.
Changes in AA treatment during the COVID-19 pandemic has been recently explored in two systematic reviews [7,21]. The number of studies identified by Köhler at al [21]. was lower compared to our work (46 vs. 54), in line with a literature search ended one month before (Feb 1st vs. Mar 5th 2021). Similar to our findings, they demonstrated an overall significant reduction of AA cases by 21% in adults and an increase of 13% in children. Also, higher rates of complicated appendicitis were observed in adults. Emile et al [7]. demonstrated a 7-time higher application of non-operative management during than before the pandemic.
This systematic review has several limitations. First, the low quality of included studies, all being retrospective in nature, with relatively small sample size. Second, the incidence of AA was not normalized to any population data. It remains unknown whether the population from which AA cases were extrapolated was consistent between the reference and index periods. Despite controlling for the number of COVID-19 active cases per million people on the day in the middle of the index period in the country where each study was conducted, several further factors may have played a role in the epidemiological trend of admissions for AA and appendectomies. Ultimately, the exclusion of studies at high risk of bias (13%) would have unlikely changed the results of this systematic review.
In conclusion, the pandemic has altered the rate of admissions for AA and appendectomy, with parallel increased incidence of complicated cases. These findings will inform future efforts to develop and implement guidelines for this condition in time of emergency.
Author contributions
UG, GG and MO conceived the study; UG, GG, MO, MP, NS, CF, GAS and GZ designed and performed the research; UG and GLDT analyzed the data; UG, MO, MP, CF, GAS and GG wrote the paper; MG, GS, SDS and GZ supervised the paper; all authors read and approved the final manuscript
Supplementary Table 1. PRISMA Checklist.
Supplementary Table 2. Search strategy.
Supplementary Figure 1. Funnel plot showing the standard error for the effect sizes for rate ratio of admissions for acute appendicitis.
Supplementary Figure 2. Funnel plot showing the standard error for the effect sizes of rate ratio of appendectomies.
Supplementary Figure 3. Funnel plot showing the standard error for the effect sizes for risk ratio of complicated appendectomies.
Supplementary Figure 4. Risk of bias summary, assessed by Joanna Briggs Institute Critical Appraisal Checklist for Analytical Cross-Sectional Studies: authors' judgments for each included study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding
None
Ethical approval
This article does not contain any study with human participants performed by any of the authors
Informed consent
For this type of study, formal consent is not required
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.hsr.2022.100021.
Appendix. Supplementary materials
References
- 1.Bhangu A, Soreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 2.Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J. Emerg. Surg. 2020;15:27. doi: 10.1186/s13017-020-00306-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collaborative C, Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N. Engl. J. Med. 2020;383:1907–1919. doi: 10.1056/NEJMoa2014320. [DOI] [PubMed] [Google Scholar]
- 4.Andersson RE. The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J. Surg. 2007;31:86–92. doi: 10.1007/s00268-006-0056-y. [DOI] [PubMed] [Google Scholar]
- 5.Willms AG, Oldhafer KJ, Conze S, Thasler WE, von Schassen C, Hauer T, et al. Appendicitis during the COVID-19 lockdown: results of a multicenter analysis in Germany. Langenbecks Arch. Surg. 2021;406:367–375. doi: 10.1007/s00423-021-02090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ceresoli M, Coccolini F, Magnone S, Lucianetti A, Bisagni P, Armao T, et al. The decrease of non-complicated acute appendicitis and the negative appendectomy rate during pandemic. Eur. J. Trauma Emerg. Surg. 2021 doi: 10.1007/s00068-021-01731-y. [DOI] [PubMed] [Google Scholar]
- 7.Emile SH, Hamid HKS, Khan SM, Davis GN. Rate of application and outcome of non-operative management of acute appendicitis in the setting of COVID-19: systematic review and meta-analysis. J. Gastrointest. Surg. 2021;25:1905–1915. doi: 10.1007/s11605-021-04988-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aromataris E, Munn Z. JBI; 2020. JBI Manual for Evidence Synthesis.https://synthesismanual.jbi.global (Editors) Available from. 2020. [Google Scholar]
- 10.IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fallani G, Lombardi R, Masetti M, Chisari M, Zanini N, Cattaneo GM, et al. Urgent and emergency surgery for secondary peritonitis during the COVID-19 outbreak: an unseen burden of a healthcare crisis. Updates Surg. 2021;73:753–762. doi: 10.1007/s13304-020-00943-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee-Archer P, Blackall S, Campbell H, Boyd D, Patel B, McBride C. Increased incidence of complicated appendicitis during the COVID-19 pandemic. J. Paediatr. Child Health. 2020;56:1313–1314. doi: 10.1111/jpc.15058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jantti S, Ponkilainen V, Kuitunen I, Hevonkorpi TP, Paloneva J, Ukkonen M, et al. Trends in appendicectomy during the COVID-19 pandemic. Br. J. Surg. 2021;108:e35–ee6. doi: 10.1093/bjs/znaa086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ponkilainen V, Kuitunen I, Hevonkorpi TP, Paloneva J, Reito A, Launonen AP, et al. The effect of nationwide lockdown and societal restrictions due to COVID-19 on emergency and urgent surgeries. Br. J. Surg. 2020;107:e405–e4e6. doi: 10.1002/bjs.11847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaitero Tristan J, Souto Romero H, Escalada Pellitero S, Espinera CR, Andina Martin D, Espinosa Gongora R, et al. Acute appendicitis in children during the COVID-19 pandemic: neither delayed diagnosis nor worse outcomes. Pediatr. Emerg. Care. 2021;37:185–190. doi: 10.1097/PEC.0000000000002364. [DOI] [PubMed] [Google Scholar]
- 16.Bracale U, Podda M, Castiglioni S, Peltrini R, Sartori A, Arezzo A, et al. Changes in surgicaL behaviOrs dUring the CoviD-19 pandemic. The SICE CLOUD19 Study. Updates Surg. 2021;73:731–744. doi: 10.1007/s13304-021-01010-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santoro GA, Grossi U, Murad-Regadas S, Nunoo-Mensah JW, Mellgren A, Di Tanna GL, et al. DElayed COloRectal cancer care during COVID-19 pandemic (DECOR-19): global perspective from an international survey. Surgery. 2021;169:796–807. doi: 10.1016/j.surg.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Podda M, Pata F, Pellino G, Ielpo B, Di Saverio S. Acute appendicitis during the COVID-19 lockdown: never waste a crisis! Br. J. Surg. 2021;108:e31–ee2. doi: 10.1093/bjs/znaa073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang AW, Prieto J, Ikeda DS, Lewis PR, Benzer EM, Van Gent JM. Perforated appendicitis: an unintended consequence during the coronavirus-19 pandemic. Mil. Med. 2021;186:e94–ee7. doi: 10.1093/milmed/usaa527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumaira Fonseca M, Trindade EN, Costa Filho OP, Nacul MP, Seabra AP. Impact of COVID-19 outbreak on the emergency presentation of acute appendicitis. Am. Surg. 2020;86:1508–1512. doi: 10.1177/0003134820972098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kohler F, Muller S, Hendricks A, Kastner C, Reese L, Boerner K, et al. Changes in appendicitis treatment during the COVID-19 pandemic - a systematic review and meta-analysis. Int. J. Surg. 2021;95 doi: 10.1016/j.ijsu.2021.106148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allen MT, Thompson BC, Atkinson B, Fyfe CE, Scanlan MJ, Stephen RE, et al. Emergency department presentations in the Southern District of New Zealand during the 2020 COVID-19 pandemic lockdown. Emerg. Med. Australas. 2021 doi: 10.1111/1742-6723.13749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Angeramo CA, Dreifuss NH, Schlottmann F, Rotholtz NA. More severe presentations of acute appendicitis during COVID-19. J. Gastrointest. Surg. 2021 doi: 10.1007/s11605-020-04892-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Antakia R, Xanthis A, Georgiades F, Hudson V, Ashcroft J, Rooney S, et al. Acute appendicitis management during the COVID-19 pandemic: A prospective cohort study from a large UK centre. Int. J. Surg. 2021;86:32–37. doi: 10.1016/j.ijsu.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anteby R, Zager Y, Barash Y, Nadler R, Cordoba M, Klang E, et al. The Impact of the Coronavirus Disease 2019 outbreak on the attendance of patients with surgical complaints at a tertiary hospital emergency department. J. Laparoendosc. Adv. Surg. Tech. A. 2020;30:1001–1007. doi: 10.1089/lap.2020.0465. [DOI] [PubMed] [Google Scholar]
- 26.Aviran E, Laks S, Benvenisti H, Khalilieh S, Assaf D, Aviran N, et al. The Impact of the COVID-19 pandemic on general surgery acute admissions and urgent operations: a comparative prospective study. Isr. Med. Assoc. J. 2020;11:673–679. [PubMed] [Google Scholar]
- 27.Baral S, Chhetri RK, Thapa N. Comparison of acute appendicitis before and within lockdown period in COVID-19 era: a retrospective study from rural Nepal. PLoS One. 2021;16 doi: 10.1371/journal.pone.0245137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Butt AA, Kartha AB, Masoodi NA, Azad AM, Asaad NA, Alhomsi MU, et al. Hospital admission rates, length of stay, and in-hospital mortality for common acute care conditions in COVID-19 vs. pre-COVID-19 era. Public Health. 2020;189:6–11. doi: 10.1016/j.puhe.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.English W, Habib Bedwani N, Smith C, Doganay E, Marsden M, Muse S, et al. Suspected appendicitis and COVID-19, a change in investigation and management-a multicentre cohort study. Langenbecks Arch. Surg. 2021;406:357–365. doi: 10.1007/s00423-020-02023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finkelstein P, Picado O, Muddasani K, Wodnicki H, Mesko T, Unger S, et al. A retrospective analysis of the trends in acute appendicitis during the COVID-19 pandemic. J. Laparoendosc. Adv. Surg. Tech. A. 2021;31:243–246. doi: 10.1089/lap.2020.0749. [DOI] [PubMed] [Google Scholar]
- 31.Gao Z, Li M, Zhou H, Liang Y, Zheng C, Li S, et al. Complicated appendicitis are common during the epidemic period of 2019 novel coronavirus (2019-nCoV) Asian J. Surg. 2020;43:1002–1005. doi: 10.1016/j.asjsur.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goksoy B, Akca MT, Inanc OF. The impacts of the COVID-19 outbreak on emergency department visits of surgical patients. Ulus Travma Acil. Cerrahi. Derg. 2020;26:685–692. doi: 10.14744/etd.2020.67927. [DOI] [PubMed] [Google Scholar]
- 33.Griffith AM, Ockerse P, Shaaban A, Kelly C. Effect of the COVID-19 pandemic on CT scans ordered from the emergency department for abdominal complaints. Emerg. Radiol. 2021;28:485–495. doi: 10.1007/s10140-021-01907-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ho S-L, Lau J, Wang C-T, Cheung S-L, Wong K-F, Leung S-K. Impact of Coronavirus disease 2019 (COVID-19) on acute appendicitis in Hong Kong: Retrospective cohort study in a local cluster hospital. Surg. Pract. 2021;25:25–31. [Google Scholar]
- 35.Honeyford K, Coughlan C, Nijman R, Expert P, Burcea G, Maconochie I, et al. Changes in Emergency Department attendances before and after COVID-19 lockdown implementation: a cross sectional study of one urban NHS Hospital Trust. medRxiv. 2020 [Google Scholar]
- 36.Mathur S, Jeremy Ng CF, Koh F, Cai M, Palaniappan G, Linn YL, et al. Development of an enhanced acute care surgery service in response to the COVID-19 global pandemic. Injury. 2020;51:2135–2141. doi: 10.1016/j.injury.2020.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGuinness MJ, Hsee L. Impact of the COVID-19 national lockdown on emergency general surgery: Auckland City Hospital’s experience. ANZ J. Surg. 2020;90:2254–2258. doi: 10.1111/ans.16336. [DOI] [PubMed] [Google Scholar]
- 38.Neufeld MY, Bauerle W, Eriksson E, Azar FK, Evans HL, Johnson M, et al. Where did the patients go? Changes in acute appendicitis presentation and severity of illness during the coronavirus disease 2019 pandemic: a retrospective cohort study. Surgery. 2021;169:808–815. doi: 10.1016/j.surg.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Connell RM, Khan MA, Amir M, Bucheeri M, Khan W, Khan IZ, et al. The impact of COVID-19 on emergency general surgery admissions and operative volumes: a single centre experience. Surgeon. 2020 doi: 10.1016/j.surge.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patel VK, Ye K, In H, Scheinfeld MH. Non-operative management for acute appendicitis during the COVID-19 pandemic does not increase the rate of complications. J. Gastrointest. Surg. 2021;25:1327–1329. doi: 10.1007/s11605-020-04844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Perea Del Pozo E, Aparicio-Sanchez D, Hinojosa Ramirez F, Pareja Ciuro F, Duran Munoz-Cruzado V, Sanchez Arteaga A, et al. A prospective cohort study of the impact of COVID19 world pandemic on the management of emergency surgical pathology. Br. J. Surg. 2020;107:e463–e4e4. doi: 10.1002/bjs.11918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Romero J, Valencia S, Guerrero A. Acute Appendicitis During Coronavirus Disease 2019 (COVID-19): changes in clinical presentation and CT findings. J. Am. Coll. Radiol. 2020;17:1011–1013. doi: 10.1016/j.jacr.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Surek A, Ferahman S, Gemici E, Dural AC, Donmez T, Karabulut M. Effects of COVID-19 pandemic on general surgical emergencies: are some emergencies really urgent? Level 1 trauma center experience. Eur. J. Trauma Emerg. Surg. 2020 doi: 10.1007/s00068-020-01534-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Turanli S, Kiziltan G. Did the COVID-19 pandemic cause a delay in the diagnosis of acute appendicitis? World J. Surg. 2021;45:18–22. doi: 10.1007/s00268-020-05825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wichmann D, Schweizer U, Wulff D, Thiel K, Beltzer C, Konigsrainer A, et al. Incidence of perforated appendicitis during the COVID-19 pandemic: lessons to be considered in the second wave. J. Gastrointest. Surg. 2021 doi: 10.1007/s11605-021-04915-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bonilla L, Galvez C, Medrano L, Benito J. [Impact of COVID-19 on the presentation and course of acute appendicitis in paediatrics] An. Pediatr. (Engl. Ed.) 2021;94:245–251. doi: 10.1016/j.anpedi.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fisher JC, Tomita SS, Ginsburg HB, Gordon A, Walker D, Kuenzler KA. Increase in pediatric perforated appendicitis in the New York City metropolitan region at the epicenter of the COVID-19 outbreak. Ann. Surg. 2021;273:410–415. doi: 10.1097/SLA.0000000000004426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gerall CD, DeFazio JR, Kahan AM, Fan W, Fallon EM, Middlesworth W, et al. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J. Pediatr. Surg. 2021;56:905–910. doi: 10.1016/j.jpedsurg.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kvasnovsky CL, Shi Y, Rich BS, Glick RD, Soffer SZ, Lipskar AM, et al. Limiting hospital resources for acute appendicitis in children: Lessons learned from the U.S. epicenter of the COVID-19 pandemic. J. Pediatr. Surg. 2021;56:900–904. doi: 10.1016/j.jpedsurg.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.La Pergola E, Sgro A, Rebosio F, Vavassori D, Fava G, Codrich D, et al. Appendicitis in children in a large Italian COVID-19 pandemic area. Front. Pediatr. 2020;8 doi: 10.3389/fped.2020.600320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Montalva L, Haffreingue A, Ali L, Clariot S, Julien-Marsollier F, Ghoneimi AE, et al. The role of a pediatric tertiary care center in avoiding collateral damage for children with acute appendicitis during the COVID-19 outbreak. Pediatr. Surg. Int. 2020;36:1397–1405. doi: 10.1007/s00383-020-04759-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pines JM, Zocchi MS, Black BS, Carlson JN, Celedon P, Moghtaderi A, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am. J. Emerg. Med. 2021;41:201–204. doi: 10.1016/j.ajem.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Place R, Lee J, Howell J. Rate of pediatric appendiceal perforation at a Children’s Hospital during the COVID-19 pandemic compared with the previous year. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.27948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Velayos M, Munoz-Serrano AJ, Estefania-Fernandez K, Sarmiento Caldas MC, Moratilla Lapena L, Lopez-Santamaria M, et al. Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis. An. Pediatr. (Engl. Ed.) 2020;93:118–122. doi: 10.1016/j.anpede.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bajomo O, Hampal R, Sykes P, Miah A. Managing appendicitis during the COVID-19 era: a single centre experience & implications for future practice. Ann. Med. Surg. (Lond.) 2021;63 doi: 10.1016/j.amsu.2021.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Baugh JJ, White BA, McEvoy D, Yun BJ, Brown DFM, Raja AS, et al. The cases not seen: patterns of emergency department visits and procedures in the era of COVID-19. Am. J. Emerg. Med. 2020 doi: 10.1016/j.ajem.2020.10.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Burgard M, Cherbanyk F, Nassiopoulos K, Malekzadeh S, Pugin F, Egger B. An effect of the COVID-19 pandemic: significantly more complicated appendicitis due to delayed presentation of patients! medRxiv. 2021 doi: 10.1371/journal.pone.0249171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ganesh R, Lucocq J, Ekpete NO, Ain NU, Lim SK, Alwash A, et al. Management of appendicitis during COVID-19 pandemic; short-term outcomes. Scott. Med. J. 2020;65:144–148. doi: 10.1177/0036933020956316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mai DVC, Sagar A, Menon NS, Claydon O, Park JY, Down B, et al. A local experience of non-operative management for an appendicitis cohort during COVID-19. Ann. Med. Surg. (Lond.) 2021;63 doi: 10.1016/j.amsu.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maneck M, Gunster C, Meyer HJ, Heidecke CD, Rolle U. Influence of COVID-19 confinement measures on appendectomies in Germany-a claims data analysis of 9797 patients. Langenbecks Arch. Surg. 2021;406:385–391. doi: 10.1007/s00423-020-02041-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Meriç S, Vartanoglu Aktokmakyan T, Tokocin M, Aktimur YE, Hacım NA, Gülcicek OB. Comparative analysis of the management of acute appendicitis between the normal period and COVID-19 pandemic. Ulus Travma Acil. Cerrahi. Derg. 2021;27:22–25. doi: 10.14744/tjtes.2020.46487. [DOI] [PubMed] [Google Scholar]
- 62.Orthopoulos G, Santone E, Izzo F, Tirabassi M, Perez-Caraballo AM, Corriveau N, et al. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am. J. Surg. 2021;221:1056–1060. doi: 10.1016/j.amjsurg.2020.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Steinman M, de Sousa JHB, Tustumi F, Wolosker N. The burden of the pandemic on the non-SARS-CoV-2 emergencies: A multicenter study. Am. J. Emerg. Med. 2021;42:9–14. doi: 10.1016/j.ajem.2020.12.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tankel J, Keinan A, Blich O, Koussa M, Helou B, Shay S, et al. The decreasing incidence of acute appendicitis during COVID-19: a retrospective multi-centre study. World J. Surg. 2020;44:2458–2463. doi: 10.1007/s00268-020-05599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Toale C, Westby D, O’Callaghan M, Nally D, Burke P, Peirce C, et al. Appendicitis and the COVID pandemic; new challenges in the management of a familiar foe. Br. J. Surg. 2020;107:e605–e6e6. doi: 10.1002/bjs.12058. [DOI] [PubMed] [Google Scholar]
- 66.Verma S, Garg P, Verma A, Sirohi V. Careful non-operative management with surveillance of acute appendicitis during COVID-19 pandemic. Indian J. Surg. 2020:1–2. doi: 10.1007/s12262-020-02620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Walker LE, Heaton HA, Monroe RJ, Reichard RR, Kendall M, Mullan AF, et al. Impact of the SARS-CoV-2 pandemic on emergency department presentations in an integrated health system. Mayo Clin. Proc. 2020;95:2395–2407. doi: 10.1016/j.mayocp.2020.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhou Y, Cen LS. Managing acute appendicitis during the COVID-19 pandemic in Jiaxing, China. World J. Clin. Cases. 2020;8:4349–4359. doi: 10.12998/wjcc.v8.i19.4349. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.