Abstract
Background:
Patients with substance use disorders are seven times more likely hospitalized than the general population. However, causes of death for recently hospitalized patients with Opioid Use Disorder (OUD) are not well described. This study describes causes of death in the year post-discharge among hospitalized patients with OUD.
Methods:
We analyzed data from participants who were at least 18 years old, with Medicaid insurance, and had a diagnosis of OUD during a general hospital admission in Oregon between April 2015 and December 2017.
Results:
During the study window, 6,654 Oregon Medicaid patients with an OUD diagnosis were hospitalized. Patients were predominately female (56.7%) and White (72.2%), an average age of 44.2 years (SD=15.4 years) and average hospital length of stay of 6.5 days (SD=10.9 days). In the 12 months post-discharge, 522 patients died (7.8%); 301 patients from a drug or substance related cause (4.5%), including 71 from drug overdose (1.1%). Stated another way, of those who died within 12 months, 58% of deaths were attributed to drug-related causes, including 13.6% of deaths attributed to overdose; 42% died of non-drug related causes. Drug-related death was the most frequent cause of mortality.
Conclusions:
Hospitalized patients with OUD are at high risk of death, from drug and non-drug related causes, in the year after discharge. Future research should consider not only overdose, but a more comprehensive definition of drug-related death in understanding post-discharge mortality among hospitalized patients with OUD, and care systems should work to mitigate the risk of death in this population.
Keywords: Medicaid, Oregon, Cause of Death, Opioid-Related Disorders, Drug Overdose, Hospitalization, Inpatients
1. Introduction
Patients with substance use disorders are seven times more likely hospitalized than the general population1 and hospitalizations among patients with opioid use disorder (OUD) are rising2. Hospitalization is a critical time to engage, treat, and support patients with OUD3. Support for these patients impacts not only OUD care, but also care for any illness both in and out of the hospital. Patients with OUD face high mortality from a variety of causes4. However, to date, causes of 12-month mortality for hospitalized patients with OUD are not well described, nor are the causes of death in this population beyond the immediate post-discharge period. Understanding causes of mortality among these patients is essential to identifying and addressing healthcare system gaps. The objective of this study was to describe causes of death in the year post-discharge among patients hospitalized with OUD.
2. Methods
2.1. Study setting and design
This analysis is part of a larger project modeling care trajectories for hospitalized patients with OUD in Oregon5. We used data from all Oregon Medicaid patients who were admitted to one of 62 Oregon hospitals at least once between April 2015 and December 2017. Encrypted IDs from these patients were linked to encrypted Oregon Vital Statistics mortality data through December 2018 by Medicaid Health Service Delivery in Oregon. All persons who die in Oregon are required to have death information submitted to Vital Statistics. Information is submitted by many sources, including by hospitals, nursing homes, counties and families6.The Oregon Health & Science University’s Institutional Review Board approved this study (#00010846).
2.2. Participants
This study included patients age 18 years old and older and had an ICD-9 (304.*) or ICD-10 (F11*) diagnosis code of OUD during a general hospital admission during the study window.
2.3. Measures
We extracted the following variables from Oregon Medicaid claims data: age (years), sex (male/female), race (white/Black/Asian/Other), ethnicity (Not Hispanic/Hispanic or Other), length of stay (days), concurrent Alcohol Use Disorder (yes/no), Amphetamine Use Disorder (yes/no), Sedative Use Disorder, including benzodiazepines (yes/no, and Chronic Illness and Disability Payment System Score, a surrogate estimate of comorbid burden available in Oregon Medicaid data. We selected these additional Use Disorders because of their high prevalence in Oregon7.
2.4. Outcome
We classified deaths using categories defined by ICD-10 codes from the National Center for Health Statistics8. We categorized drug-related deaths as all unintentional, intentional, and undetermined intent deaths from drug poisoning (ICD-10 codes X40-X49; X60-X69; Y10-Y19) and deaths attributed to mental and behavioral disorders because of substance use (F10–F19)8. Separately, we identified patients who had at least a code for a drug overdose. Participants were classified in each category of death for which they had codes; for example, a person with a code for drug-related death and for respiratory death was counted in both categories. Similarly, a patient who died from a drug overdose is counted as both a drug overdose death and drug-related death. A patient who died from endocarditis would be included as a drug-related death if a code for mental and behavioral disorders because of substance use (F10–F19) was also listed on their death certificate.
2.5. Data analysis
We calculated the cumulative monthly mortality rate and overall percentage of patients who died by different causes within 12-months of hospital discharge.
3. Results
From April 2015 to December 2017, 6,654 Oregon Medicaid patients with an OUD diagnosis were hospitalized. Patients were predominately female (56.7%) and white (72.2%), with an average age of 44.2 years (SD=15.4 years) and average length of stay of 6.5 days in the hospital (SD=10.9 days). In the month after hospital discharge, 130 (2%) patients died. Sixty-five (1%) died from drug-related causes, including 0.2% who died from drug overdose. Sixty-five (1%) died from non-drug-related causes.
In the 12 months post-discharge, 522 patients died (7.8%); 301 patients died from a drug or substance related cause other than drug overdose (4.5%), and 71 died from a drug overdose (1.1%). Stated another way, of those who died within 12 months, 58% of deaths were attributed to drug-related causes, including 13.6% of deaths attributed to overdose; 42% of deaths were attributed to non-drug-related causes. After drug-related deaths, diseases of the circulatory system (39.5%), respiratory system (33.5%), other causes of death (24.3%), neoplasms (18.5%), endocrine, nutritional, and metabolic diseases (18.1%), and certain infectious and parasitic diseases (17.8%) were the next most frequently identified causes of death in the cohort at 12 months. Figure 1 displays cumulative mortality, by cause.
Figure 1.
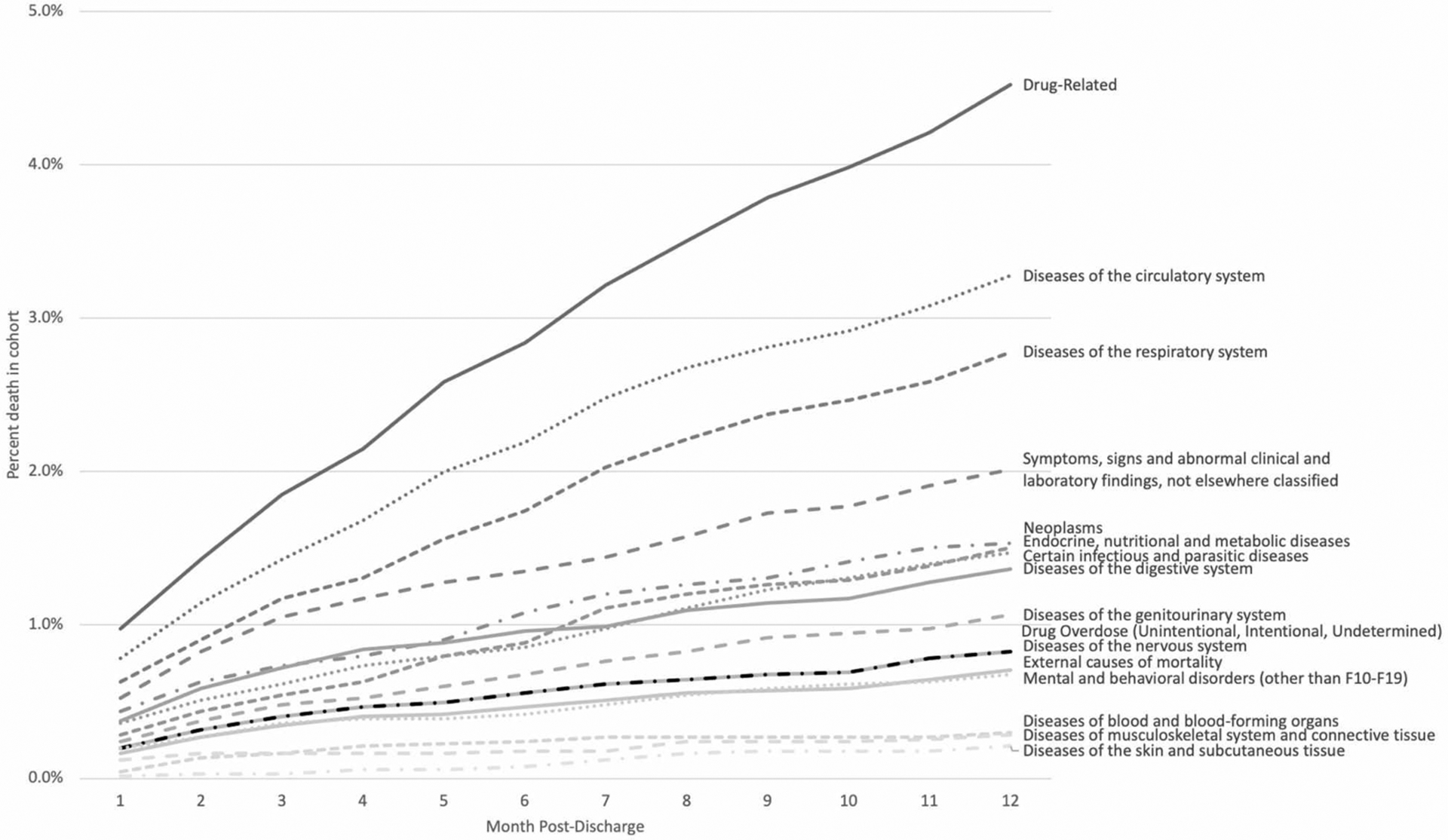
Cumulative mortality by cause among people hospitalized with OUD in Oregon, 2015–2018
Among patients who died from drug-related causes, the most common ICD-10 codes listed on death certificates in order of prevalence were F17.9 (Nicotine Dependence, n=182, 60.5%), J44.9 (Chronic obstructive pulmonary disease, unspecified, n=99, 32.9%), X42 (Accidental poisoning by and exposure to narcotics or hallucinogens, n=32, 10.6%), B182 (Chronic viral hepatitis C, n=32, 10.6%), and T401 (Opioid overdose, n=31, 10.3%). Among patients who were classified as not dying from drug-related causes, the most common ICD-10 codes listed on their death certificates in order of prevalence were A419 (Sepsis, unspecified organism, n-=23, 10.4%), I50 (Heart failure, n=22, 10.0%), I10 (Essential primary hypertension, n=20, 9.0%), J44.9 (Chronic obstructive pulmonary disease, unspecified, n=15, 6.8%), and B18.2 (Hepatitis C, n=14, 6.3%). In unadjusted analyses, there were differences in rates among patients who died from non-drug related deaths, drug-related non-overdose deaths, and overdose deaths by gender, age and co-occurring substance use disorder (Table 1).
Table 1.
Demographics of patients with OUD who died within 12 months of hospital discharge in Oregon, 2015–2018
| Non-drug related death (n=221) | Non-overdose drug-related death (n=230) | Overdose death (n=71) | p-value** | ||
|---|---|---|---|---|---|
| Sex | Male | 92 (41.6%) | 123 (53.5%) | 41 (57.7%) | 0.012 |
| Female | 129 (58.4%) | 107 (46.5%) | 30 (42.3%) | ||
| Age (years) | 58.1 (15.9) | 58.0 (12.4) | 43.2 (13.2) | 0.0012 | |
| Race | Black | 9 (4.1%) | 9 (3.9%) | * | 0.80 |
| White | 176 (79.6%) | 186 (80.9%) | 55 (77.5%) | ||
| Asian | 6 (2.7%) | 6 (2.6%) | 0 | ||
| Other | 30 (13.6%) | 29 (12.6%) | 13 (18.3%) | ||
| Ethnicity | Not Hispanic | 192 (86.9%) | 205 (89.1%) | 56 (78.9%) | 0.083 |
| Hispanic/Other | 29 (13.1%) | 25 (10.9%) | 15 (21.1%) | ||
| Length of stay (days) | 10.1 (14.0) | 9.7 (17.3) | 7.7 (13.9) | 0.39 | |
| Alcohol use disorder | Yes | * | 14 (6.1%) | 6 (8.5%) | 0.004 |
| Amphetamine use disorder | Yes | 10 (4.5%) | * | 13 (18.3%) | <0.001 |
| Sedative use disorder | Yes | * | 7 (3.0%) | * | 0.042 |
| Chronic Illness & Disability Payment System Score | 4.3 (2.0) | 4.1 (1.8) | 3.0 (1.5) | <0.0001 | |
Cells suppressed if n<=5
Assessed using Chi-squared tests, Fisher’s exact test, or Analysis of Variance
4. Discussion
Patients with OUD are at high-risk of death from a myriad of causes in the year after hospital discharge. Overdose deaths represent the tip of the iceberg; causes of death spanned nearly every medical specialty, reflecting the burden of comorbid medical conditions among people with OUD. Mortality in our study is similar to acute coronary syndrome (estimated 5–9% one-year mortality), a condition which has garnered enormous attention from providers, policy-makers, and payers to achieve high quality care9. And yet, most hospitals do not offer medication for OUD (MOUD)10, patients with OUD frequently have stigmatizing healthcare experiences, providers receive little training to address OUD11, 12, and there are no widely accepted hospital standards or metrics for OUD. This underscores key needs: first, healthcare providers in many disciplines should learn about and offer OUD treatment, regardless of whether the patient’s illness is attributable to their substance use. Healthcare providers can support increased treatment engagement in OUD treatment3, and MOUD reduces overdose risk13. Second, healthcare systems and policymakers must create systems that destigmatize OUD and better care for patients at risk of death. This might include implementing inpatient addiction consult services3; integrating OUD care in primary care14; and removing barriers to methadone that limit access for people with serious medical illness15. Finally, we must invest in broad program and policy solutions that drive integration across hospital and community settings for people with OUD, including hospital-quality metrics.
There are some limitations to this work. First, our study only uses death data from Oregon Vital Statistics and ICD-10 codes which likely underestimate mortality incidence and causes of death. Second, OUD may be underdiagnosed in patient data. Third, Oregon has low racial and ethnic diversity, and may not be generalizable to other populations.
Hospitalized patients with OUD are at high risk of death in the year after discharge. Care systems must work to mitigate the risk of death in this population.
Funding:
This research was supported through grants from the National Institutes of Health, National Institute on Drug Abuse (UG1DA015815, UG3DA044831). Grant UL1TR002369 provided support of REDCap, the web application this study used for data collection. Caroline King was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Award Number TL1TR002371 and the National Institute On Drug Abuse of the National Institutes of Health under Award Number F30DA052972. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest:
No authors have financial conflicts of interest. Dr. Korthuis serves as principal investigator for NIH-funded trials that accept donated study medications from Alkermes (extended-release naltrexone) and Indivior (buprenorphine-naloxone).
References
- 1.Lewer D, Freer J, King E, et al. Frequency of health-care utilization by adults who use illicit drugs: a systematic review and meta-analysis. Addiction. Jun 2020;115(6):1011–1023. doi: 10.1111/add.14892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peterson C, Xu L, Florence C, Mack KA. Opioid-related US hospital discharges by type, 1993–2016. J Subst Abuse Treat. Aug 2019;103:9–13. doi: 10.1016/j.jsat.2019.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Englander H, Dobbertin K, Lind BK, et al. Inpatient Addiction Medicine Consultation and Post-Hospital Substance Use Disorder Treatment Engagement: a Propensity-Matched Analysis. Journal of General Internal Medicine Aug 13 2019;doi: 10.1007/s11606-019-05251-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hser YI, Mooney LJ, Saxon AJ, et al. High Mortality Among Patients With Opioid Use Disorder in a Large Healthcare System. J Addict Med. Jul/Aug 2017;11(4):315–319. doi: 10.1097/ADM.0000000000000312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King CA, Englander H, Korthuis PT, Barocas JA, McConnell KJ, Morris CD, Cook R. Designing and validating a Markov model for hospital-based addiction consult service impact on 12-month drug and non-drug related mortality. MedRxiv (Preprint). 2020;doi: 10.1101/2020/12/01/20242164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.OHA. Oregon Vital Statistics. https://www.oregon.gov/oha/PH/BIRTHDEATHCERTIFICATES/VITALSTATISTICS/DEATH/Pages/index.aspx
- 7.King C, Nicolaidis C, Korthuis PT, Priest KC, Englander H. Patterns of substance use before and after hospitalization among patients seen by an inpatient addiction consult service: A latent transition analysis. J Subst Abuse Treat. Nov 2020;118:108121. doi: 10.1016/j.jsat.2020.108121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. ICD-10* Recodes of Selected Causes of Death for Deaths Occuring in 1999 and Beyond. https://simba.isr.umich.edu/restricted/docs/Mortality/icd_10_recodes.pdf
- 9.Bradley EH, Herrin J, Elbel B, et al. Hospital quality for acute myocardial infarction: correlation among process measures and relationship with short-term mortality. JAMA. Jul 5 2006;296(1):72–8. doi: 10.1001/jama.296.1.72 [DOI] [PubMed] [Google Scholar]
- 10.Priest KC, Lovejoy T, Englander H, Shull S, McCarty D Opioid agonist therapy during hospitalization within the Veterans Health Administration: A retrospective cohort analysis. . JGIM. 2019;doi:Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. Mar 2014;105:59–66. doi: 10.1016/j.socscimed.2014.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biancarelli DL, Biello KB, Childs E, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug and Alcohol Dependence. May 1 2019;198:80–86. doi: 10.1016/j.drugalcdep.2019.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wakeman SE, Larochelle MR, Ameli O, et al. Comparative Effectiveness of Different Treatment Pathways for Opioid Use Disorder. JAMA Netw Open. Feb 5 2020;3(2):e1920622. doi: 10.1001/jamanetworkopen.2019.20622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Korthuis PT, McCarty D, Weimer M, et al. Primary Care-Based Models for the Treatment of Opioid Use Disorder: A Scoping Review. Ann Intern Med. Feb 21 2017;166(4):268–278. doi: 10.7326/M16-2149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregg JL. Dying To Access Methadone. Health Aff (Millwood). Jul 2019;38(7):1225–1227. doi: 10.1377/hlthaff.2019.00056 [DOI] [PubMed] [Google Scholar]


