Abstract
Network analysis is an effective approach for examining complex relationships between psychiatric symptoms. This study was designed to examine item-level relationships between depressive and anxiety symptoms using network analysis in an adolescent sample and identified the most central symptoms within the depressive-anxiety symptoms network model. Depressive and anxiety symptoms were assessed using the Patient Health Questionire-9 (PHQ-9) and Generalized Anxiety Disorder Screener (GAD-7), respectively. The structure of depressive and anxiety symptoms was characterized using “Strength” and “Bridge Strength” as centrality indices in the symptom network. Network stability was tested using a case-dropping bootstrap procedure. Finally, a Network Comparison Test (NCT) was conducted to examine whether network characteristics differed on the basis of gender, school grade and residence. Network analysis revealed that nodes PHQ2 (“Sad mood”), GAD6 (“Irritability”), GAD3 (“Worry too much”), and PHQ6 (“Guilty”) were central symptoms in the network model of adolescents. Additionally, bridge symptoms linking anxiety and depressive symptoms in this sample were nodes PHQ6 (“Guilty”), PHQ2 (“Sad mood”), and PHQ9 (“Suicide ideation”). Gender, school grade and residence did not significantly affect the network structure. Central symptoms (e.g., Sad mood, Irritability, Worry too much, and Guilty) and key bridge symptoms (e.g., Guilty, Sad mood, and Suicide ideation) in the depressive and anxiety symptoms network may be useful as potential targets for intervention among adolescents who are at risk for or suffer from depressive and anxiety symptoms.
Subject terms: Depression, Scientific community
Introduction
Adolescence is a crucial period in life, characterized by many unique changes and challenges. One in six people fall within this age group (i.e., 10–19 years) and half of all psychiatric conditions start before 14 years of age [1]. It is estimated that one in seven adolescents experience mental health problems [2], of which anxiety and depression are the most common disturbances. For example, the estimated 1-year prevalence of depression among adolescents is 4–5% [3–5], while the corresponding figure for anxiety ranges between 5% and 10% [6]. Depression and anxiety often occur together in adolescents [7]. For instance, due to lockdown and school closures during the COVID-19 pandemic in early 2020 [8–10], prevalence estimates of depression and anxiety were 57.0% and 36.7%, respectively, among adolescents in China [10]. Depression and anxiety account for 16% of the global burden of disease for adolescents worldwide [1, 11, 12] and are among the major contributing factors for disability, substance use, self-harm, and suicide behaviors among adolescents [13–16].
Comorbid depression and anxiety have been widely examined with traditional conceptualizations of psychopathology that rely on total scale scores to describe symptom severity. Unfortunately, such approaches may obscure meaningful associations between individual symptoms [17]. Network analysis has emerged as a novel approach to conceptualizing psychological phenomena in a manner that addresses limitations of the traditional approach. In network theory, central symptoms are more likely to activate other symptoms and play a major role in causing the onset and/or maintenance of a syndrome/disorder. Network analysis has the potential to map specific relationships among individual symptoms of a disorder and identify targets for treatment [18]. Furthermore, network analysis can be used to extract the structure of psychiatric disturbances from clinical data [19, 20] and highlight meaningful associations between individual symptoms within and/or between disorders [21]. Additionally, network model is useful in understanding the mechanism of comorbidities and provide hints for clinicians to prevent and treat comorbidities [22].
Network analysis has been used to understand symptom-symptom relationships in psychiatric comorbidities. For example, a network analysis of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study revealed the importance of “Sad mood” and “Anhedonia” in non-psychotic depressive disorder [23]. In another network analysis study, “Sad mood” and “Worry” emerged as the most central symptoms in the depression-anxiety network among psychiatric patients [24, 25]. A network analysis on depressed US adolescents (N = 1409) revealed that “Self-hatred”, “Loneliness”, “Sadness”, and “Pessimism” were the most central symptoms [26]. Another network analysis on depressive and anxiety symptoms of adolescents in Sub-Saharan Africa found that the most central symptoms were “Guilty” and “Sad mood” in the depressive symptom community, while “Too much worry”, “Uncontrollable worry”, and “Nervousness” were the central symptoms in the anxiety symptom community [27].
Clinical features of depression and anxiety are closely associated with sociocultural and economic factors [28]. Therefore, findings based on samples from Western countries and Africa are not necessarily as applicable within sociocultural and economic contexts of highly populated, rapidly developing Asian countries such as China [29, 30]. To date, no network analysis studies have been published on comorbid depressive and anxiety symptoms in general samples of adolescents in China. Hence, this study examined the item-level relationships between depressive and anxiety symptoms using network analysis in a sample of Chinese adolescents.
Methods
Participants and procedure
Study design
This cross-sectional study was conducted between 8 August 2020 and 12 March 2021, using snowball sampling method through the collaborative research network of the National Clinical Research Center for Mental Disorders, China. Eligible participants were (1) secondary school students residing in China during the COVID-19 pandemic, who were (2) able to understand the purpose and contents of the assessment. To avoid contagion during the COVID-19 pandemic, following previous studies [31, 32] data were collected online using the WeChat-based “Questionnaire Star” program. WeChat is a widely used smartphone-based social communication APP, with more than 1.2 billion active users in China. All participants (and their caregivers for participants younger than 18 years) provided electronic written informed consent prior to participation in this study. This study was approved by the Institutional Review Board (IRB) of Beijing Anding Hospital.
Measures
Severity of the depressive symptoms was assessed using the Chinese version of the 9-item Patient Health Questionnaire (PHQ-9) [33, 34] each item reflected a symptom of depression and was rated from “0” (not at all) to “3” (nearly every day). Total PHQ-9 scores ranged from 0 to 27, with higher scores indicating more severe depressive symptoms. Severity of anxiety symptoms was measured using the Chinese version of the 7-item Generalized Anxiety Disorder Scale (GAD-7) [35, 36]. Each GAD-7, item described a common anxiety symptom and was scored from 0 (not at all) to 3 (nearly every day); total scores ranged from 0 to 21 with higher scores indicating more severe anxiety symptoms.
Statistical analysis
Network analysis
All analyses were conducted using R (Version 4.0.3) [37]. Means, standard deviations (SDs), kurtosis, and skewness of all PHQ-9 and GAD-7 item scores were inspected. Following previous studies [26, 38], the informativeness of each item was estimated by the mean of the standard deviation, and then possible item redundancy was evaluated using “networktools” R package [39]. Due to controversies over the optimal method of modeling scale item scores in network analysis [40], following previous studies [20] the values of all PHQ-9 and GAD-7 items were dichotomized as “0” or “1”, representing the absence or presence of depressive and anxiety symptoms, respectively. Item values of 1, 2, or 3 were converted to “presence” of depressive and anxiety symptoms, respectively, while values of 0 reflected an “absence” of symptoms. An Ising model was used to assess the depressive-anxiety symptoms network structure based on binary data [20, 41]. Briefly, an Ising model can be conceived as a series of pairwise associations between binary variables, after controlling for the confounding effects of all other associations.
To estimate and visualize the network, R-package “qgraph” (Version 1.6.5) [42] and “bootnet” (Version 1.4.3) [43] were used. The network structure was estimated using the Enhanced Least Absolute Shrinkage and Selection Operator (eLASSO) method, which combines a logistic regression analysis with an optimization process to determine the best connection method for each symptom. To identify relationships between nodes, the eLASSO combined logistic regression with model selection based on a Goodness-of-Fit measure. This algorithm could result in a sparse network model which is more interpretable than the original model. Model selection was based on the Extend Bayesian Information Criterion (EBIC) [44, 45]. The binary network was fitted using the R-package “IsingFit” 0.3.1 [20]. When each node (representing a symptom) is connected to a range of other nodes through edges with different weights, the final network is constructed [46]. The thickness of an edge represents the strength of an association. The color of an edge indicates the direction of the association (e.g., green edges indicate positive associations; red edges indicate negative associations). The network is visualized using the Fruchterman-Reingold algorithm [43]. Nodes with stronger and more frequent associations with another node are placed closer with each other and are more concentrated in the network. Network analysis can provide quantitative centrality indicators for each node based on the unique configuration of the network. The predictability of each node was estimated using the R package “mgm”. Predictability was defined as the variance in a node that is explained by all other nodes in the network.
Following previous studies [43, 47], the centrality index of strength was used to indicate importance of individual symptoms in the model; certain other centrality indices, such as betweenness and closeness, are unsuitable as measure of node importance in psychological networks [48] and were excluded. Strength is the sum of the correlations of one node to all other nodes with higher values reflecting greater centrality in the network. Centrality measures are reported as standardized values (“z scores”).
Estimation of network accuracy and stability
According to recommendations of Epskamp et al. [43], the robustness of the network solution was assessed by estimating the accuracy of edge weights and the stability of centrality indices with the R-package “bootnet” (Version 1.4.3) [43]. The accuracy of edge weights was estimated by computing confidence intervals (CIs) with a non-parametric bootstrapping method [49]. Next, observations in the dataset were resampled randomly to create new datasets from which the 95% CIs were calculated. Larger CIs suggested reduced precision in the estimation of edges while narrower CIs indicated a more trustworthy network [43]. When “0” was included within the range of constructed CIs, this indicated the edge weights (or node strength) of two different symptoms did not significantly differ from each other. In this network analysis, we performed 1000 permutations and used a bootstrap differential test to evaluate differences in network properties, which were used to determine differences between edge weights and between node centrality indexes [26].
Correlation stability coefficients (CS-C) assessed the stability of centrality indexes (i.e., Strengths) using subset bootstraps [50]. If the strength of nodes did not change significantly after excluding a subset of the sample in the dataset, the network structure was considered to be stable. CS-C values represented the maximum proportion of samples that could be removed, while there was a 95% probability that the correlation between original centrality indices could reach at least 0.70 [43]. Generally, the CS-C should not be <0.25, and preferably above 0.50. Subsequently, the difference between two strength indices was considered significant if 1000-bootstrap 95% non-parametric CIs did not contain “0”. Bootstrapped difference tests were used to evaluate differences in network properties [43]. This test relied on 95% CIs to determine whether or not two edge weights or the strength of two nodes significantly differed from one-another. The R package “bootnet” was used to perform the analyses [51].
Comparison of network characteristics
Considering the moderating effects of gender, school grade, and residence on anxiety and depressive symptoms among adolescents [52], depression-anxiety network models were compared between genders, between school grades (junior/senior secondary school) and between residences (urban/rural areas). For these analyses, we used Network Comparison Tests (NCT), which are permutation tests that assess the difference between two networks, using the R-package “NetworkComparisonTest” 2.0.1 [53]. NCTs were performed on subsamples (i.e., females vs. males, junior secondary school vs. senior secondary school, and urban vs. rural areas) with 1000 permutations to assess global network strengths (absolute sums of all edge weights) and network structures (distributions of edge weights) between the two networks. In addition, the strength of each edge between the two networks was assessed using Holm-Bonferroni correlations for multiple comparisons.
Results
Study sample
Altogether, 1183 adolescents were invited to participate in this study; of these 1057 met study inclusion criteria and completed the assessment. A majority was female (60.3%) and their mean age was 16.30 years (SD = 3.61 years). The sample mean PHQ-9 and GAD-7 total scores were 3.98 (SD = 5.44) and 2.67 (SD = 4.40), respectively (Table 1). Means, SDs, skewness and kurtosis of all PHQ-9 and GAD-7 item scores are presented in Supplementary Table 1. Distribution of the answer to each PHQ-9 and GAD-7 question are presented in Supplementary Table 2. A correlation matrix of PHQ-9 and GAD-7 item scores is presented in Supplementary Table 3.
Table 1.
Demographic characteristics of the study sample (n = 1057).
| Variables | |
|---|---|
| Age, mean (SD) | 16.30 (3.61) |
| Female gender, n (%) | 637 (60.3%) |
| School grade, n (%) | |
| Junior secondary school | 479 (45.3%) |
| Senior secondary school | 578 (54.7%) |
| PHQ-9 total, mean (SD) | 3.98 (5.44) |
| GAD total, mean (SD) | 2.67 (4.40) |
PHQ-9 nine-item Patient Health Questionnaire, GAD-7 seven-item Generalized Anxiety Disorder scale.
Network structure and centrality measures analysis
Tests of item informativeness and redundancy indicated no item ratings were <2.5 SD from the mean level for informativeness (MSD = 0.44 ± 0.04); as such, none of the items were poor vis a vis informativeness. Moreover, no items were redundant with any other items (<25% of statistically different correlations). Therefore, all PHQ-9 and GAD-7 items were retained in the analyses.
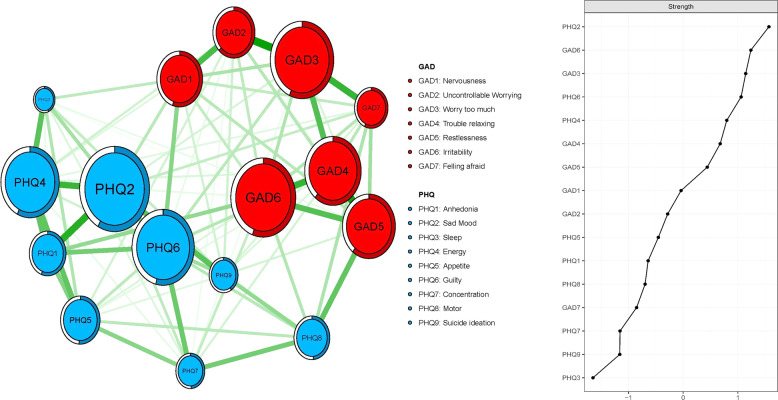
Figure 1 shows the network analysis of depressive and anxiety symptoms using the Ising model. The predictability of symptoms is shown in the form of ring-shaped pie charts in Fig. 1. Mean predictability was 0.54 in this adolescent sample. Within the depressive symptom community, node PHQ1 (“Anhedonia”) had the most direct connection with the node PHQ2 (“Sad mood”), followed by the connection between nodes PHQ2 (“Sad mood”) and PHQ4 (“Energy”), and the connection between nodes PHQ3 (“Sleep”) and PHQ4 (“Energy”).
Fig. 1. Estimated network model for depressive and anxiety symptoms in adolescents.
Ring-shaped pie charts represent predictability (a fully filled dark ring would indicate that 100% of the symptom’s variance is explained by its intercorrelations with the other symptoms in the network). In the diagram symptom node with stronger connections are closer to each other. The blue node denotes the PHQ-9 items (9 -items Patients Health Questionnaire); the red node denotes the GAD-7 items (7-items Generalized Anxiety Disorder scale). The dark green lines represent positive correlations. The edge thickness represents the strength of the association between symptom nodes.
Within the anxiety symptom community, the node GAD3 (“Worry too much”) had the most direct connection with node GAD2 (“Uncontrollable Worrying”), followed by the connection between nodes GAD4 (“Trouble relaxing”) and GAD5 (“Restlessness”), the connection between nodes GAD3 (“Worry too much”) and GAD7 (“Feeling afraid”) and the connection between nodes GAD4 (“Trouble relaxing”) and GAD6 (“Irritability”). In the depressive and anxiety symptoms network model of Chinese adolescents, node GAD5 (“Restlessness”) was most strongly associated with node PHQ8 (“Motor”) (average edge Weight=1.09), followed by connections between nodes GAD1 (“Nervousness”) and PHQ6 (“Guilty”) (average edge weight = 0.84), and nodes PHQ1 (“Anhedonia”) and GAD6 (“Irritability”) (average edge Weight=0.79) (Fig. 1 and Supplementary Table S3).
In terms of strength, node PHQ2 (“Sad mood”) had the highest strength. Nodes GAD6 (“Irritability”), GAD3 (“Worry too much”), and PHQ6 (“Guilty”) were also statistically stronger than most other symptoms in the network (Fig. 1). Therefore, these four symptoms were central symptoms for understanding the association between depressive and anxiety symptoms in this sample. In contrast, several other symptoms were marginal including nodes PHQ7 (“Concentration”), PHQ9 (“Suicide ideation”) and PHQ3 (“Sleep”) (Fig. 1).
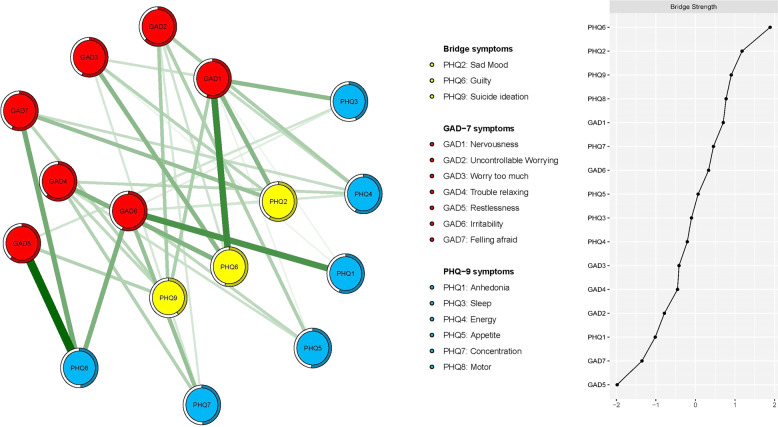
Following previous studies [22, 54], bridge strength, the best index for identifying nodes in which deactivation could prevent activation spread from one disorder to another was used to identify bridge symptoms. Nodes PHQ6 (“Guilty”), PHQ2 (“Sad mood”) and PHQ9 (“Suicide ideation”) emerged as the three most prominent bridge symptoms (Fig. 2).
Fig. 2. Network structure of depressive and anxiety in adolescents only showing bridge connection.
Ring-shaped pie charts represent predictability (a fully filled dark ring would indicate that 100% of the symptom’s variance is explained by its intercorrelations with the other symptoms in the network). In the diagram symptom node with stronger connections are closer to each other. The blue node denotes the PHQ-9 items (9-items Patients Health Questionnaire); the red node denotes the GAD-7 items (7-items Generalized Anxiety Disorder scale). The dark green lines represent positive correlations. The edge thickness represents the strength of the association between symptom nodes.
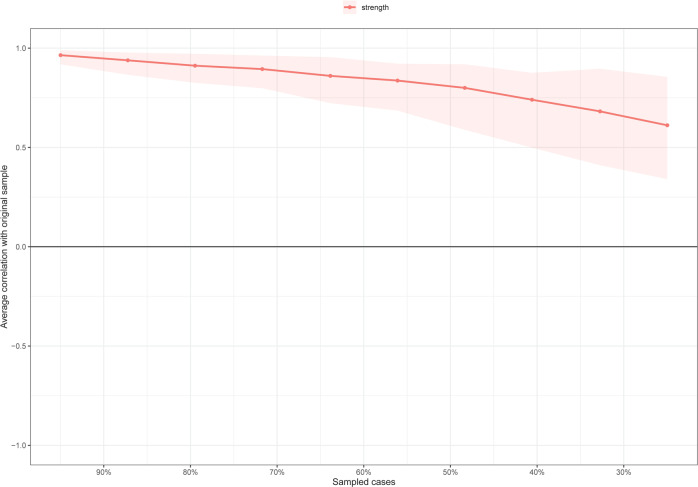
For stability of the network analysis, strength had an excellent level of stability (i.e., CS-coefficient = 0.517), indicating that 51% of the sample could be dropped without significant changes in the network structure (Fig. 3). Bootstrapped 95% CIs for estimated edge-weights suggested that the estimates were reliable and stable (Fig. S1). The bootstrap difference test showed that most of the comparisons between edge weights are statistically significant.
Fig. 3. Stability of centrality indices by case dropping subset bootstrap.
The x-axis represents the percentage of cases of the original sample used at each step. The y-axis represents the average of correlations between the centrality indices in the original network and the centrality indices from the re-estimated networks after excluding increasing percentages of cases. The line indicates the correlations of strength and bridge strength.
Network Comparison Tests
In the comparison of network models between female and male adolescents, there were no significant differences in network global strength (network strength among male participants: 7.52 versus female participants: 7.60, S = 0.08, p = 0.484), but there was a significant difference in edge weights (M = 0.28, p = 0.022; Supplementary Figs. S2–S4). Three edge weights, PHQ4 (“Energy”) – PHQ8 (“Motor”), PHQ9 (“Suicide ideation”) – GAD1 (“Nervousness”), and PHQ1(“Anhedonia”) - GAD5 (“Restlessness”) were stronger in female than in male adolescents. Conversely, two edge weights, PHQ1 (”Anhedonia”) – PHQ4 (“Energy”) and PHQ8 (“Motor”) - GAD5 (“Restlessness”) were stronger in male than in female adolescents. Subdividing the sample according to junior versus senior secondary school grade, no significant differences were found in network global strength (network strength among junior participants: 7.47; among senior participants: 7.40; S = 0.07, p = 0.527) or the distribution of edge weights (M = 0.18, p = 0.626, Supplementary Figs. S5–S7). Subdividing the sample according to urban versus rural residence, no significant differences were found in network global strength (network strength among urban participants: 7.36; among rural participants: 7.61; S = 0.25, p = 0.108) or the distribution of edge weights (M = 0.23, p = 0.222, Supplementary Figs. S8–S10).
Discussion
To our knowledge, this is the first network analysis study of depressive and anxiety symptoms in a general sample of adolescents in China. Analyses indicated nodes PHQ2 (“Sad mood”), GAD6 (“Irritability”), GAD3 (“Worry too much”) and PHQ6 (“Guilty”) were central symptoms in the network model. Additionally, bridge symptoms linking anxiety and depressive symptoms in this sample were nodes PHQ6 (“Guilty”), PHQ2 (“Sad mood”) and PHQ9 (“Suicide ideation”). Gender, school grade and residence did not significantly affect the overall network structure.
“Sad mood” (PHQ2) was one of the most central symptoms to emerge within the depression-anxiety network of Chinese adolescents. Similar findings have been reported in previous studies on depressive and anxiety symptom networks of adults with psychiatric disorders [24, 55], adults with depression [23, 56], a sample of US children and adolescents [25], and adolescents in Sub-Saharan Africa [27]. Our findings also supported sad mood as a required, core symptom for the diagnosis of major depressive disorder (MDD) in line with the Diagnostic and Statistical Manual of Mental Disorder-5 (DSM-5); [57] and International Classification of Diseases, Tenth Revision (ICD-10) [58]. Other studies have also reported the presence of sad mood contributes to the prediction of MDD and increases risk for MDD onset or recurrence [23, 59, 60]. Furthermore, a substantial proportion of Chinese adolescents are “left-behind children” (e.g., children who are left at home for at least half a year while one or both parents move elsewhere to work) who often suffered from financial, social-emotional, behavioral, and educational difficulties [61, 62], which could increase the likelihood of sad mood in adolescents.
The symptom, “worry too much” (GAD3), was another prominent central symptom in the depressive-anxiety symptom network of Chinese adolescents as indicated by its strength. This finding is also consistent with previous findings of depressive and anxiety symptoms network in an adult psychiatric sample [24, 55] and adolescents in Sub-Saharan Africa [27]. “Worry too much” is a hallmark symptom required for a generalized anxiety disorder diagnosis in the DSM-5 [57] and ICD-10 [58]. In this sample, sources of worry could include concerns of academic performance during the COVID-19 pandemic [8, 63–66], infection risk for oneself, one’s family, classmates, and friends [67, 68], and further COVID-19 outbreaks [63]. Together, stressors associated with COVID-19 may increase uncertainty and ambiguity in negotiating tasks of adolescences such as the completion of academic requirements and transitions to further education or work and contribute to chronic worry [69, 70], particularly among already distressed cohorts.
“Irritability” (GAD3) was another prominent central symptom in this network analysis, and is also a key criterion, both for depression in children and adolescents and anxiety disorders in the DSM-5 [57]. In addition, irritability was found to be a predictor of future depression and anxiety disorders in a 20-year follow-up study of a community-based sample [71]. Irritability in adolescents has been linked to increased activity in the insula, prefrontal cortex, and inferior parietal lobule [72]. Abnormalities in both reward and threat processing underlie the clinical presentation of irritability, which includes a greater propensity toward affective (e.g., frustration and anger) and behavioral (e.g., motor activity and aggression) responses [73].
Guilt or negative self-referential thinking has also been implicated in the onset and/or maintenance of depression among adolescents [74, 75]. The emergence of Guilty (PHQ6) as a central symptom in the network of our adolescent sample parallels findings in depressed adolescents in Sub-Saharan Africa [27] and North America [26] and suggests regret about having done or not done something one believes should be done is common among depressed-anxious adolescents across different cultures. Guilt and/or negative self-concept are key features in the DSM-5 diagnosis of major depression [57]. Negative self-evaluations reflecting regrets may increase rumination and attentional focus toward negative self-information [76]. Therefore, negative self-evaluations may contribute to the development and/or maintenance of a depressive episode with co-occurring anxiety [76].
Comorbid depressive and anxiety symptoms are often associated with poor treatment efficacy, and increased rates of hospitalization and disability [77]. We found that “Guilty” (PHQ6), “Sad mood” (PHQ2) and “Suicide ideation” (PHQ9) were key bridge symptoms in the current depression-anxiety network. Similar findings have been found in previous studies wherein “guilty” and “sad mood” have had a role linking the depression and anxiety of between ages 5 and 14 years old [25]. These bridge symptoms do not necessarily extend to older groups, however, as another study found that psychomotor agitation, concentration problems, and restlessness were the bridge symptoms in depression and anxiety network of adults [56]. The discrepancy between studies could be partly due to using different measures of depression and anxiety, though an intriguing hypothesis for future work is the possibility that different clinical features are critical to the co-occurrence of depression within samples of adolescents versus adults. Some studies also found that uncaring family environments, parental rejection, and over-control, unhealthy living style, peer victimization and hopelessness are associated with higher risk of sad mood, suicidal ideation and guilt in adolescents [78–82].
Previous meta-analysis on depressive and anxiety symptoms in children and adolescents found that female sex was associated with increased risk of depressive and anxiety symptoms during COVID-19 pandemic [52]. However, network analysis revealed that only certain edges were different between genders during the late stage of the COVID-19 pandemic, which may be partly due to gender differences involving biological susceptibility, self-esteem, experience of interpersonal violence, and exposure to stress [83].
Identifying central symptoms and bridge symptoms within the depressive-anxiety symptom network model has possible clinical significance; targeting these symptoms may contribute to prevention among at-risk adolescents and improve the effectiveness of treatments targeting co-occurring depressive and anxiety symptom [56]. For example, cognitive behavioral therapies (CBTs) targeting central symptoms and bridge symptoms including “Guilty”, “Excessive worry”, “Sad mood”, and “Irritability” via strategies such as cognitive restructuring and distribution may rapidly improve depressive and anxiety symptoms among adolescents and reduce risk of comorbidity [84, 85]. Furthermore, a recent meta-analysis of 17 randomized control trials (RCTs) concluded that antidepressants are more effective than CBT in treating specific symptoms of depression including “depressed mood”, “feelings of guilt”, “suicidal thoughts”, and “psychic anxiety” [86], though this difference was limited to those patients with the highest elevations on these symptoms and it was not clear how applicable these results were to adolescents given the mean age of just under 40 years across the set of studies. Nonetheless, such findings underscore the need for further research on antidepressants as a potentially viable alternative for targeting key symptoms of depressive and anxiety among adolescents.
Possible implications aside, the main limitations of this study should be noted. First, findings may not be generalized to adolescents in clinical settings, as previous studies have suggested differences in network connectivity may exist in different populations or samples [87]. Furthermore, although some parallels were observed between the network characteristics of the current sample and of adolescents in other countries, generalizations across cultures and contexts (e.g., to a post-COVID-19 world) are tentative at best. Second, due to the cross-sectional research design, dynamic changes and causality between individual symptoms could not be explored. The “snapshot” of the depressive-anxiety symptom network of adolescents provided in this research provides a foundation for more costly, time-consuming longitudinal extensions in future. Third, because symptom assessments were based on self-reports, biases in recall and/or social desirability cannot be ruled out as influences on the results. Fourth, data collected by snowball sampling were used to construct a network model, which could limit the sample representativeness. Fifth, for logistical reasons, data prior to and in the early stage of the COVID-19 pandemic were not collected; therefore, comparisons of symptom patterns in adolescents between different stages of the pandemic could not be conducted.
In conclusion, this study is the first to identify central symptoms (e.g., Sad mood, Irritability, Worry too much, Guilty) and key bridge symptoms (e.g., Guilty, Sad mood, Suicide ideation) within the depression-anxiety network of Chinese adolescents. Findings may provide an impetus for future studies examining symptom networks in other groups of adolescents as a means of clarifying key symptoms that extend across adolescents from different cultures and those that are unique to particular groups. In addition, central symptoms and bridge symptoms identified in this study may be useful targets for interventions designed to prevent these disturbances among at-risk Chinese adolescents and treat those who are currently suffering from co-occurring depressive and anxiety symptoms.
Supplementary information
Acknowledgements
The study was supported by the Beijing Municipal Science & Technology Commission (Grant No.: Z181100001718124), Beijing Talents Foundation (Grant No.: 2017000021469G222), and the University of Macau (MYRG2019-00066-FHS).
Author contributions
Study design: Y-TX, HC, and WB. Collection, analysIs, and interpretation of data: HC, WB, HL, XC, HQ, RL, ZS, and JL. Drafting of the manuscript: HC, TC, and Y-TX. Critical revision of the manuscript: YT and TJ. Approval of the fill version for publication: all the authors.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hong Cai, Wei Bai, Huanzhong Liu, Xu Chen.
Supplementary information
The online version contains supplementary material available at 10.1038/s41398-022-01838-9.
References
- 1.World health organization. Adolescent mental health. 2021.
- 2.World Health Organization. Ensuring mental health an well-being in an adolescent’s formative years can foster a better transition from childhood to adulthood. 2021.
- 3.Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44:972–86. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 4.Jane Costello E, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry. 2006;47:1263–71.. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen MS, Clausen CE, Hirota T, Kumperscak H, Guerrero A, Kaneko H, et al. A comparison of child and adolescent psychiatry in the Far East, the Middle East, and Southeast Europe. Asia‐Pac Psychiatry 2021:e12490. [DOI] [PubMed]
- 6.Bodden DH, Dirksen CD, Bögels SM. Societal burden of clinically anxious youth referred for treatment: a cost-of-illness study. J Abnorm Child Psychol. 2008;36:487–97.. doi: 10.1007/s10802-007-9194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol Bull. 2014;140:816. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang S, Xiang M, Cheung T, Xiang Y-T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J Affect Disord. 2021;279:353–60.. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen F, Zheng D, Liu J, Gong Y, Guan Z, Lou D, et al. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav Immun. 2020;88:36. doi: 10.1016/j.bbi.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen X, Qi H, Liu R, Feng Y, Li W, Xiang M, et al. Depression, anxiety and associated factors among Chinese adolescents during the COVID-19 outbreak: a comparison of two cross-sectional studies. Transl Psychiatry. 2021;11:148. doi: 10.1038/s41398-021-01271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86.. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 12.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–8. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 13.Zubrick SR, Hafekost J, Johnson SE, Sawyer MG, Patton G, Lawrence D, et al. The continuity and duration of depression and its relationship to non-suicidal self-harm and suicidal ideation and behavior in adolescents 12–17. J Affect Disord. 2017;220:49–56. doi: 10.1016/j.jad.2017.05.050. [DOI] [PubMed] [Google Scholar]
- 14.Davidson LL, Grigorenko EL, Boivin MJ, Rapa E, Stein A. A focus on adolescence to reduce neurological, mental health and substance-use disability. Nature. 2015;527:S161–S6.. doi: 10.1038/nature16030. [DOI] [PubMed] [Google Scholar]
- 15.Feigelman W, Gorman BS. Prospective predictors of premature death: evidence from the National Longitudinal Study of Adolescent Health. J Psychoactive Drugs. 2010;42:353–61. doi: 10.1080/02791072.2010.10400698. [DOI] [PubMed] [Google Scholar]
- 16.Vijayakumar L, Ray S, Fernandes TN, Pathare S. A descriptive mapping review of suicide in vulnerable populations in low and middle countries. Asia‐Pac Psychiatry. 2021;13:e12472. doi: 10.1111/appy.12472. [DOI] [PubMed] [Google Scholar]
- 17.Fried EI, Nesse RM. The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS ONE. 2014;9:e90311. doi: 10.1371/journal.pone.0090311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fried EI, Nesse RM, Zivin K, Guille C, Sen S. Depression is more than the sum score of its parts: individual DSM symptoms have different risk factors. Psychol Med. 2014;44:2067–76.. doi: 10.1017/S0033291713002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- 20.Van Borkulo CD, Borsboom D, Epskamp S, Blanken TF, Boschloo L, Schoevers RA, et al. A new method for constructing networks from binary data. Sci Rep. 2014;4:5918. doi: 10.1038/srep05918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Epskamp S, Kruis J, Marsman M. Estimating psychopathological networks: be careful what you wish for. PLoS ONE. 2017;12:e0179891. doi: 10.1371/journal.pone.0179891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. 2019;56:1–15. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- 23.Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D, et al. What are’good’depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J Affect Disord. 2016;189:314–20.. doi: 10.1016/j.jad.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 24.Beard C, Millner AJ, Forgeard MJ, Fried EI, Hsu KJ, Treadway M, et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol Med. 2016;46:3359–69.. doi: 10.1017/S0033291716002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McElroy E, Fearon P, Belsky J, Fonagy P, Patalay P. Networks of depression and anxiety symptoms across development. J Am Acad Child Adolesc Psychiatry. 2018;57:964–73.. doi: 10.1016/j.jaac.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mullarkey MC, Marchetti I, Beevers CG. Using network analysis to identify central symptoms of adolescent depression. J Clin Child Adolesc Psychol. 2019;48:656–68.. doi: 10.1080/15374416.2018.1437735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Osborn TL, Campbell S, Ndetei D, Weisz J. Network analysis reveals central symptoms of adolescent depression and anxiety in sub-Saharan Africa. 2020.
- 28.Kleinman A. Culture and depression. New Engl J Med. 2004;351:951–3. doi: 10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- 29.Baxter AJ, Scott K, Vos T, Whiteford H. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- 30.Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC, et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8:1–10. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luo H, Lie Y, Prinzen FW. Surveillance of COVID-19 in the general population using an online questionnaire: report from 18,161 respondents in China. JMIR Public Health Surveill. 2020;6:e18576. doi: 10.2196/18576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou J, Liu L, Xue P, Yang X, Tang X. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry. 2020;177:574–5. doi: 10.1176/appi.ajp.2020.20030304. [DOI] [PubMed] [Google Scholar]
- 33.Zhang YL, Liang W, Chen ZM, Zhang HM, Zhang JH, Weng XQ, et al. Validity and reliability of Patient Health Questionnaire‐9 and Patient Health Questionnaire‐2 to screen for depression among college students in China. Asia‐Pac Psychiatry. 2013;5:268–75.. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 36.He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients (in Chinese) Shanghai Arch Psychiatry. 2010;22:200–3. [Google Scholar]
- 37.R Core Team. R: A language and environment for statistical computing. 2020. https://www.R-project.org/.
- 38.Marchetti I. Hopelessness: a network analysis. Cogn Ther Res. 2019;43:611–9. [Google Scholar]
- 39.Jones P. Networktools: Assorted tools for identifying important nodes in network. R package version 120. 2018.
- 40.Fried EI. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front Psychol. 2015;6:309. doi: 10.3389/fpsyg.2015.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barber RF, Drton M. High-dimensional Ising model selection with Bayesian information criteria. Electron J Stat. 2015;9:567–607.. [Google Scholar]
- 42.Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Stat Softw. 2012;1:2012. [Google Scholar]
- 43.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Foygel R, Drton M. Extended Bayesian information criteria for Gaussian graphical models. Adv Neural Inf Process Syst. 2010;2010:604–12. [Google Scholar]
- 45.Chen J, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95:759–71.. [Google Scholar]
- 46.van Rooijen G, Isvoranu AM, Meijer CJ. A symptom network structure of the psychosis spectrum. Schizophr Res. 2017;189:75–83. doi: 10.1016/j.schres.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 47.Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Netw. 2010;32:245–51.. [Google Scholar]
- 48.Bringmann LF, Elmer T, Epskamp S. What do centrality measures measure in psychological networks? J Abnorm Psychol. 2019;128:892. doi: 10.1037/abn0000446. [DOI] [PubMed] [Google Scholar]
- 49.Chernick MR. Bootstrap methods: a guide for practitioners and researchers. John Wiley & Sons; 2011.
- 50.Costenbader E, Valente TW. The stability of centrality measures when networks are sampled. Soc Netw. 2003;25:283–307. [Google Scholar]
- 51.Epskamp S. Fried EI Package ‘bootnet’. 2018. https://cran.r-project.org/web/packages/bootnet/index.html.
- 52.Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S, et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142–50. [DOI] [PMC free article] [PubMed]
- 53.van Borkulo C, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ, Schoevers R, et al. Association of symptom network structure with the course of depression. JAMA Psychiatry. 2015;72:1219–26. doi: 10.1001/jamapsychiatry.2015.2079. [DOI] [PubMed] [Google Scholar]
- 54.Garabiles MR, Lao CK, Xiong Y, Hall BJ. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: a network approach. J Affect Disord. 2019;250:85–93. doi: 10.1016/j.jad.2019.02.062. [DOI] [PubMed] [Google Scholar]
- 55.Park S-C, Kim D. The centrality of depression and anxiety symptoms in major depressive disorder determined using a network analysis. J Affect Disord. 2020;271:19–26. doi: 10.1016/j.jad.2020.03.078. [DOI] [PubMed] [Google Scholar]
- 56.Kaiser T, Herzog P, Voderholzer U, Brakemeier EL. Unraveling the comorbidity of depression and anxiety in a large inpatient sample: network analysis to examine bridge symptoms. Depression Anxiety. 2021;38:307–17.. doi: 10.1002/da.23136. [DOI] [PubMed] [Google Scholar]
- 57.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (Edition, Fifth). Am Psychiatric Assoc. 2013;21:160–8.
- 58.World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization; 1992.
- 59.Coyne JC, Schwenk TL. The relationship of distress to mood disturbance in primary care and psychiatric populations. J Consult Clin Psychol. 1997;65:161. doi: 10.1037//0022-006x.65.1.161. [DOI] [PubMed] [Google Scholar]
- 60.Georgiades K, Lewinsohn PM, Monroe SM, Seeley JR. Major depressive disorder in adolescence: the role of subthreshold symptoms. J Am Acad Child Adolesc Psychiatry. 2006;45:936–44.. doi: 10.1097/01.chi.0000223313.25536.47. [DOI] [PubMed] [Google Scholar]
- 61.Hu BY, Wu H, Winsler A, Fan X, Song Z. Parent migration and rural preschool children’s early academic and social skill trajectories in China: are ‘left-behind’children really left behind? Early Child Res Q. 2020;51:317–28.. [Google Scholar]
- 62.Dai Q, Chu R-X. Anxiety, happiness and self-esteem of western Chinese left-behind children. Child Abus Negl. 2018;86:403–13.. doi: 10.1016/j.chiabu.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 63.Magson NR, Freeman JY, Rapee RM, Richardson CE, Oar EL, Fardouly J, et al. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50:44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, Simoes-e-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct. 2020;51:101845. doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, Wang J-Q, Chen J-C, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29:749–58. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kılınçel Ş, Kılınçel O, Muratdağı G, Aydın A, Usta MB. Factors affecting the anxiety levels of adolescents in home‐quarantine during COVID‐19 pandemic in Turkey. Asia‐Pac Psychiatry. 2021;13:e12406. doi: 10.1111/appy.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Estévez Lópe E, Moreno D, Jiménez T. Aggressive behavior in adolescence as a predictor of personal, family, and school adjustment problems. Psicothema. 2018;30:66–73. doi: 10.7334/psicothema2016.294. [DOI] [PubMed] [Google Scholar]
- 68.Nie X-D, Wang Q, Wang M-N, Zhao S, Liu L, Zhu Y-L, et al. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int J Psychiatry Clin Pract. 2020;25:109–14. doi: 10.1080/13651501.2020.1791345. [DOI] [PubMed] [Google Scholar]
- 69.Li X, Tang X, Wu H, Wang M, Li L. COVID-19-related stressors and Chinese adolescents’ adjustment: the moderating role of coping and online learning satisfaction. Front Psychiatry. 2021;12:241. doi: 10.3389/fpsyt.2021.633523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Van Loon AW, Creemers HE, Vogelaar S, Miers AC, Saab N, Westenberg PM, et al. Prepandemic risk factors of COVID‐19‐related concerns in adolescents during the COVID‐19 pandemic. J Res Adolesc. 2021;31:531–45. doi: 10.1111/jora.12651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166:1048–54. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kircanski K, White LK, Tseng W-L, Wiggins JL, Frank HR, Sequeira S, et al. A latent variable approach to differentiating neural mechanisms of irritability and anxiety in youth. JAMA Psychiatry. 2018;75:631–9. doi: 10.1001/jamapsychiatry.2018.0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brotman MA, Kircanski K, Stringaris A, Pine DS, Leibenluft E. Irritability in youths: a translational model. Am J Psychiatry. 2017;174:520–32. doi: 10.1176/appi.ajp.2016.16070839. [DOI] [PubMed] [Google Scholar]
- 74.Dainer-Best J, Trujillo LT, Schnyer DM, Beevers CG. Sustained engagement of attention is associated with increased negative self-referent processing in major depressive disorder. Biol Psychol. 2017;129:231–41. doi: 10.1016/j.biopsycho.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hards E, Ellis J, Fisk J, Reynolds S. Negative view of the self and symptoms of depression in adolescents. J Affect Disord. 2020;262:143–8. doi: 10.1016/j.jad.2019.11.012. [DOI] [PubMed] [Google Scholar]
- 76.Black SW, Pössel P. The combined effects of self-referent information processing and ruminative responses on adolescent depression. J Youth Adolesc. 2013;42:1145–54. doi: 10.1007/s10964-012-9827-y. [DOI] [PubMed] [Google Scholar]
- 77.Fava M, Rush AJ, Trivedi MH. Background and rationale for the sequenced treatment alternatives to relieve depression (STAR∗ D) study. Psychiatr Clin North Am. 2003;26:457–94. doi: 10.1016/s0193-953x(02)00107-7. [DOI] [PubMed] [Google Scholar]
- 78.Yang Y, Wang Q. Culture in emotional development. Handbook of emotional development: Springer; 2019. p. 569-93.
- 79.Ai T, Xu Q, Li X, Li D. Interparental conflict and Chinese adolescents’ suicide ideation and suicide attempts: the mediating role of peer victimization. J Child Fam Stud. 2017;26:3502–11. [Google Scholar]
- 80.Li D, Li X, Wang Y, Bao Z. Parenting and Chinese adolescent suicidal ideation and suicide attempts: the mediating role of hopelessness. J Child Fam Stud. 2016;25:1397–407. [Google Scholar]
- 81.Jeon GS, Choi K, Cho SI. Gender differences in exposure and vulnerability to psychosocial and behavioral factors of suicide attempt among Korean adolescents. Asia‐Pac Psychiatry. 2017;9:e12272. doi: 10.1111/appy.12272. [DOI] [PubMed] [Google Scholar]
- 82.Wasserman D, Carli V, Iosue M, Javed A, Herrman H. Suicide prevention in childhood and adolescence: a narrative review of current knowledge on risk and protective factors and effectiveness of interventions. Asia‐Pac Psychiatry 2021;13:e12452. [DOI] [PubMed]
- 83.Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry. 2017;4:8–9. doi: 10.1016/S2215-0366(16)30348-0. [DOI] [PubMed] [Google Scholar]
- 84.Ebert DD, Zarski A-C, Christensen H, Stikkelbroek Y, Cuijpers P, Berking M, et al. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PLoS ONE. 2015;10:e0119895. doi: 10.1371/journal.pone.0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rasing S, Creemers DH, Janssens JM, Scholte RH. Depression and anxiety prevention based on cognitive behavioral therapy for at-risk adolescents: a meta-analytic review. Front Psychol. 2017;8:1066. doi: 10.3389/fpsyg.2017.01066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Boschloo L, Bekhuis E, Weitz ES, Reijnders M, DeRubeis RJ, Dimidjian S, et al. The symptom‐specific efficacy of antidepressant medication vs. cognitive behavioral therapy in the treatment of depression: Results from an individual patient data meta‐analysis. World Psychiatry. 2019;18:183–91. doi: 10.1002/wps.20630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Santos H, Jr, Fried EI, Asafu‐Adjei J, Ruiz RJ. Network structure of perinatal depressive symptoms in Latinas: relationship to stress and reproductive biomarkers. Res Nurs Health. 2017;40:218–28. doi: 10.1002/nur.21784. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.