Abstract
Little is known about the role of declarative memory in the ongoing perception of one’s personality. Seven individuals who developed a rare and severe type of anterograde amnesia following damage to their medial temporal lobes were identified from our neurological patient registry. We examined the stability of their personality ratings on the Big Five Inventory over five retest periods and assessed the accuracy of their ratings via analyses of self–caregiver agreement. The patients portrayed a stable sense of self over the course of 1 year. However, their self-ratings differed from those provided by the caregivers. Intriguingly, these discrepancies diminished when caregivers retrospectively rated the patients’ personalities prior to their brain injury, suggesting that patients’ perceptions of themselves were stuck in the past. We interpret our findings to indicate that the ability to form new declarative memories is not required for maintaining a stable sense of self but may be important for updating one’s sense of self over time.
Keywords: personality, amnesia, Big Five, medial temporal lobe, hippocampus, self–other agreement, personality stability, memory, neuropsychology
Philosophers and psychologists alike have long been interested in the concept of the “self” and how we conceptualize who we are. The self is a multifaceted construct that can be measured in various ways (Klein & Gangi, 2010; Philippi et al., 2012; Wilson, 2009). Although there is no gold standard for assessing the self, measuring personality traits has become one important proxy (Turner & Onorato, 1999). Personality traits are defined as relatively enduring patterns of thoughts, feelings, and behaviors (Tellegen, 1988); however, this does not imply that all traits are stagnant or unchanging. On the contrary, research has suggested that although traits demonstrate strong short-term rank-order stability (i.e., dependability), they may show significant change over longer time periods (e.g., greater than a year) because of the influence of major life experiences (Roberts et al., 2006; Vaidya et al., 2002; Watson, 2004).
The role of memory has been of interest in the study of how individuals create self-representations via personality ratings (Conway, 2005; Klein & Lax, 2010; Marquine, 2008; Rathbone et al., 2009). Individuals with acquired damage to the medial temporal lobes (MTLs) of the brain often have profound memory deficits, specifically in relation to learning facts and events that have occurred since the onset of brain damage (i.e., anterograde amnesia; Scoville & Milner, 1957; Zola-Morgan et al., 1986). But the question of how these memory deficits might affect how such individuals view who they “are” remains only partially tested. It is unclear whether amnesic patients would be able to form a stable, accurate, and updated perception of their personality without the ability to incorporate new declarative knowledge about life experiences and events, including details about their behavior in the context of new life circumstances.
The relevant neuropsychological literature largely consists of single case studies of amnesic patients, many of whom have noncircumscribed brain damage caused by traumatic brain injury (TBI) or Alzheimer’s disease (Duff et al., 2008; Grilli et al., 2018; Klein & Gangi, 2010; Marquine, 2008; Rathbone et al., 2009). Some studies have not used validated measures of personality, whereas others assessed personality at intervals very close to the onset of brain damage, without longitudinal follow-up, and without sufficient time for the patient to experience and integrate major life changes (e.g., loss of occupation, placement in an assisted living facility). Given that personality is fairly stable but is also influenced by major life events (Roberts et al., 2006; Vaidya et al., 2002; Watson, 2004), an important question is whether patients with amnesia would be capable of updating their self-ratings of personality in response to these sorts of significant life changes. Results from a small number of case studies that have attempted to address this question are equivocal. Specifically, three case studies of amnesic patients with MTL damage (resulting from TBI, anoxia, or unilateral temporal lobe resection, respectively) have shown that the patients were able to provide stable personality ratings that were consistent with ratings provided by their caregivers (Grilli et al., 2018; Klein et al., 2002; Tulving, 1993). Another case study of a patient with Alzheimer’s disease showed the opposite pattern, whereby current personality ratings were more consistent with the patient’s preamnesic self (Klein et al., 2003; for a review, see Klein & Gangi, 2010). In our patient Roger, who has extensive bilateral MTL damage caused by herpes simplex encephalitis, we found preliminary evidence that he maintained a stable sense of self over time, yet his ratings were discrepant with his caregivers and possibly more reflective of his preamnesic self (Philippi et al., 2012).
To our knowledge, there has been no systematic study investigating both the stability and accuracy of self-rated personality in a cohort of individuals with stable and chronic anterograde amnesia following lesions to the MTL. As noted, prior studies examining personality in patients with amnesia are single cases. Here, we expand on previous work by investigating both the stability and accuracy of personality ratings over short (1 day and 2 weeks), medium (2 months), and long (1 year) retest intervals in seven patients with severe anterograde amnesia caused by MTL damage. Caregivers provided additional retrospective ratings of what the patient was like prior to the onset of amnesia, which allowed us to examine the extent to which the amnesic patients’ self-ratings reflected their current personality as opposed to their preamnesic traits. In previous case studies (e.g., K. C., D. B., M. K., D. W., and Roger), it has been shown that despite profound anterograde amnesia, these individuals were able to consistently rate their personality traits over time, as indicated by retest reliabilities (r) ranging from .69 to .86 (Grilli et al., 2018; Klein & Gangi, 2010; Philippi et al., 2012). We hypothesized that patients in the current study would demonstrate item-level stability within this same (high) range across all time points measured. Regarding the ability to update the sense of self, on the basis of our prior finding in Roger (Philippi et al., 2012), we predicted that amnesic patients would fail to fully update their sense of self, and consequently, their current personality ratings would converge more closely with how the caregivers viewed their personality before the onset of amnesia.
Statement of Relevance.
Severe anterograde amnesia following focal bilateral brain damage to the medial temporal lobes is a rare condition that allows for the exploration of how an amnesic patient’s sense of self is maintained and updated in the context of their inability to form new declarative memories. In a study examining amnesic patients, we found that they all maintained a highly stable sense of self over the course of a year. There were substantial discrepancies between patients’ ratings and the ratings completed by their caregivers, but these differences were largely resolved when caregivers were asked to retrospectively rate the patient’s personality before the onset of their amnesia. Thus, the amnesic patients maintained a keen sense of who they were before their brain injury but were stuck in the past, in that they failed to form an accurate perception of who they are now. It appears that the brain’s medial temporal lobes (including the hippocampus) and their unique ability to form new declarative memories are not required for maintaining a stable sense of self but may be very important for updating one’s sense of self over time.
Method
Participants
All patients gave informed written consent before participating in the study, which was approved by the University of Iowa Institutional Review Board. In total, seven patients (six male, one female) with severe anterograde amnesia were recruited from the Iowa Neurological Patient Registry and took part in the study. For recruitment, we searched the database for all patients who had evidence of a brain lesion that impacted the MTL, as confirmed by neuroimaging (MRI or computed tomography), and had severe anterograde amnesia as defined by a minimum 25-point differential between their Full Scale IQ (as measured on the Wechsler Adult Intelligence Scale, Third Edition [WAIS-III]; Wechsler, 1997a) and their General Memory Index (GMI; as measured on the Wechsler Memory Scale, Third Edition [WMS-III]; Wechsler, 1997b). The etiology varied, but herpes simplex encephalitis and anoxia were the most common causes. Two patients who developed severe amnesia after herpes simplex encephalitis (Patients 1951 and 2308) had bilateral damage that spanned the entirety of the MTL, including the hippocampus and amygdala, in addition to other limbic and paralimbic structures (Cavaco et al., 2012; Feinstein et al., 2010). The four anoxic patients had damage that was largely limited to the hippocampus, as evidenced by significant bilateral volumetric reductions (Allen et al., 2006). For two of the anoxic patients (Patients 2563 and 3139), we were unable to obtain an MRI because the patients had pacemakers. In these cases, computed tomography imaging was used, and the findings were confirmed by an expert in neuroanatomy (blind to the hypotheses of the current study) to show damage to the MTLs bilaterally. In addition, we identified one patient (Patient 2367) with damage spanning the left MTL, caused by stroke and resulting in severe anterograde amnesia. Given that this patient’s neuropsychological profile closely matched that of the bilateral cases, we chose to include this patient in the study to bolster sample size. In summary, other than Patient 2367 (who had left unilateral MTL damage), all other amnesic patients had bilateral MTL damage. Notably, all seven patients had a severe deficit in their ability to form new declarative memories following the onset of their brain injury, but their overall cognition and intellectual functioning was largely preserved (see Table 1).
Table 1.
Demographic and Neuropsychological Characteristics
| Patient | Sex | Age at testing | Onset age | Years since lesion onset | Years of education | FSIQ | GMI | FSIQ – GMI | WMI | AVLT: total recall (Time 1 – Time 5) | AVLT: 30-min delayed recall | Lesion location | Etiology |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1846 | F | 45 | 30 | 15 | 14 | 84 | 57 | 27 | 85 | 24 | 2 | Bilateral hippocampus | Anoxia-status epilepticus |
| 1951 | M | 56 | 28 | 28 | 16 | 106 | 57 | 49 | 108 | 35 | 1 | Bilateral medial temporal lobe+ | Herpes simplex encephalitis |
| 2308 | M | 51 | 42 | 9 | 18 | 87 | 45 | 42 | 91 | 28 | 0 | Bilateral medial temporal lobe+ | Herpes simplex encephalitis |
| 2363 | M | 52 | 43 | 9 | 18 | 98 | 73 | 25 | 88 | 32 | 0 | Bilateral hippocampus + cortical atrophy | Anoxia-cardiac arrest |
| 2367 | M | 54 | 45 | 9 | 13 | 104 | 79 | 25 | 93 | 32 | 0 | Left medial temporal lobe | Stroke |
| 2563 | M | 52 | 44 | 8 | 16 | 94 | 63 | 31 | 90 | 32 | 2 | Bilateral hippocampus | Anoxia |
| 3139 | M | 56 | 52 | 4 | 20 | 107 | 78 | 29 | 93 | 37 | 2 | Bilateral hippocampus | Anoxia |
Note: All patients identified as non-Hispanic White. Full Scale IQ (FSIQ) scores were obtained from the Wechsler Adult Intelligence Scale, Third Edition (Wechsler, 1997a); General Memory Index (GMI) and Working Memory Index (WMI) scores were obtained from the Wechsler Memory Scale, Third Edition (Wechsler, 1997b). AVLT = Auditory Verbal Learning Test; F = female; M = male.
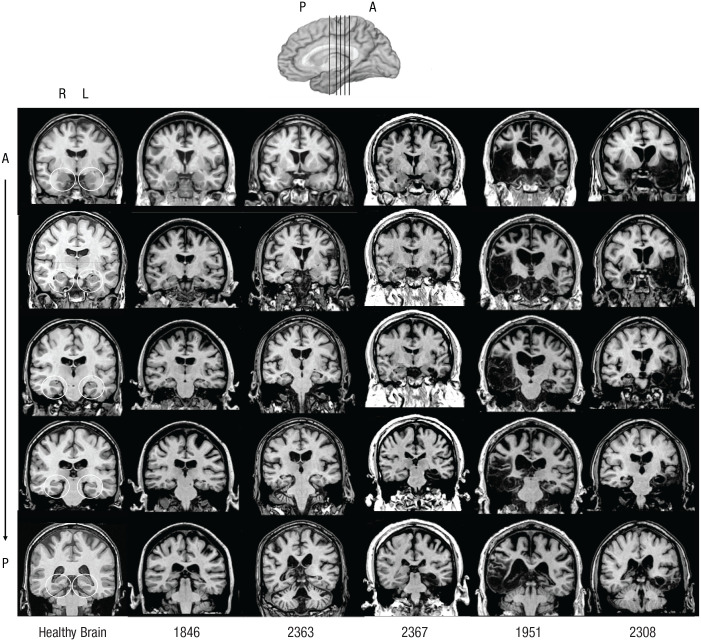
The seven patients were in the chronic phase of recovery; their brain injury had occurred many years prior to this study (range = 4–28 years). Because of the debilitating nature of their amnesic condition, all patients had undergone significant changes to their lifestyle and ability to function independently and care for themselves. All seven patients had severe and selective memory impairments. IQ scores on the WAIS-III (Wechsler, 1997a) were largely in the normal range, whereas GMI scores from the WMS-III (Wechsler, 1997b) were substantially lower. Across all patients, GMI scores were at least 25 points lower than Full Scale IQ scores (mean difference = 32.6 points). In addition, performances on the WMS Working Memory Index were largely in the normal range, indicating that the patients were able to hold information on-line even though that information was quickly forgotten after a short delay. Full demographic and neuropsychological characteristics are presented in Table 1. Further semantic and episodic memory data are provided in Table S1 in the Supplemental Material available online. MRI findings are provided in Figure 1. Some data from Patient 1951 have been previously published (Philippi et al., 2012); however, the current study provides new data on this patient regarding levels of self–other agreement.
Fig. 1.
Magnetic resonance images of five amnesic patients and a normal healthy comparison brain. For each amnesic patient, a series of coronal MRI slices shows damage to the medial temporal lobes following anoxia (Patients 1846 and 2363), stroke (Patient 2367), or herpes simplex encephalitis (Patients 1951 and 2308). (Patients 2563 and 3139 could not undergo MRI because of the presence of a pacemaker.) R = right; L = left; A = anterior; P = posterior.
Informant ratings about the patients were also obtained from at least one first-degree relative or significant other who was in close contact with the patient both before and after the brain injury and who played an active role in taking care of the patient following the onset of amnesia. Each caregiver either lived with the patient or saw them on at least a weekly basis following the injury. Three patients had two caregivers who provided ratings.
Procedures
Self-report ratings were obtained at baseline and then again at four other time points (1 day, 2 weeks, 2 months, and 1 year later). Informant ratings were obtained at baseline and then again at 2 months. At 1 year after baseline, caregivers used the same questionnaires to rate how they remembered the patients during the year before their brain injury. Because retrospective ratings were obtained at the end of the study, the data in all relevant tables and figures are presented with retrospective ratings listed last.
We examined ratings on the Big Five Inventory (BFI), a widely used and well-validated measure of the Big Five traits: Neuroticism (eight items), Extraversion (eight items), Openness (10 items), Agreeableness (nine items), and Conscientiousness (nine items; John & Srivastava, 1999). The BFI has demonstrated acceptable internal consistencies across all subscales (α = .79–.87; John et al., 2008) and has shown suitable levels of convergent and discriminant validity (John et al., 2008; John & Srivastava, 1999; Soto & John, 2009). The existing evidence indicates that the Big Five traits display similar levels of rank-order stability, both in the short term (e.g., from 2 weeks up to 2 months; Gnambs, 2014) and over longer term intervals (e.g., decades; Roberts & DelVecchio, 2000; Soldz & Vaillant, 1999). Each item begins with the stem, “I see myself as someone who . . .” (for patients) or “I see this person as someone who . . .” (for caregivers), which is followed by one of 44 phrases. Patients are asked to rate each item using a 5-point scale (1 = strongly disagree, 5 = strongly agree). For ratings at baseline and 2 months, caregivers were given the following instructions: “Answer all questions with regard to how the patient acts, behaves, and feels currently, NOT how they were before the brain injury.” In contrast, at the 1-year follow-up, caregivers were asked to “describe the patient as you remember him or her during the year before their brain injury.”
Analyses
Stability analyses
Personality stability was estimated using two different kinds of analyses. For person-centered analyses, Pearson’s r correlation coefficients were computed using item-level BFI data for each patient. Specifically, the ratings of the 44 BFI items at each patient’s baseline were correlated with their ratings on the same 44 items at each retest interval (1 day, 2 weeks, 2 months, and 1 year). Thus, four correlation coefficients were computed for each patient (n = 44 for each correlation). This same process was used to examine the stability of caregiver ratings over time. For each caregiver, the 44 BFI items answered at baseline were correlated with the same 44 items rated at the 2-month follow-up using Pearson’s r correlation coefficients.
In addition to running person-centered analyses to characterize the overall stability in self-reported personality, we were interested in the degree of stability for each of the Big Five personality traits. Trait stability was computed by averaging raw scores across all seven patients for each personality trait at each time point. Average baseline trait scores were then correlated with average trait scores at each retest period. Given that we had seven patients in our sample, Spearman ρ nonparametric rank-order stability coefficients were used for these variable-centered analyses.
Agreement analyses
To examine the degree of self–other agreement, we computed bivariate correlations between self and caregiver ratings at three time points: baseline, 2-month follow-up, and 1-year follow-up. For these analyses, the effective sample size for each patient–caregiver pair was the number of BFI items (n = 44). At baseline and 2-month follow-up, caregivers rated the patients as they currently viewed them (i.e., concurrent ratings). Retrospective ratings included only the 1-year follow-up when caregivers were asked to rate the patient’s personality during the year prior to the injury. For the patients who had two caregivers providing ratings, raw caregiver data were first averaged at the item level, and then the average item-level data and the patient raw item-level data were correlated to create a single value. We then transformed patient–caregiver correlations at all three time points into a z score using Fisher’s r-to-z transformation before averaging across the entire sample. Significant differences between the average z scores were then assessed at each of the time points using Fisher’s z tests (baseline vs. 2 months, baseline vs. retrospective, and 2 months vs. retrospective).
Trait self–other consistency was examined using difference scores in which the patient’s raw trait scores were subtracted from their caregiver’s raw trait scores at baseline (concurrent) and at the 1-year follow-up (retrospective). For the three patients for whom more than one caregiver provided ratings, the two caregivers’ trait scores were first averaged, and their individual difference score was then created from this average value. All difference scores were averaged across the entire sample to create an average difference score for each trait.
Multiple-rater analyses
For patients for whom multiple caregivers provided ratings, analyses were run to examine the level of agreement between the two caregivers. Pearson’s r bivariate correlations between Informant 1 and Informant 2 were computed using item-level BFI data (n = 44).
Results
Stability
For the person-centered analyses, stability coefficients across the four retest intervals—Time 1 to Time 2 (1 day), Time 1 to Time 3 (2 weeks), Time 1 to Time 4 (2 months), and Time 1 to Time 5 (1 year)—are provided in Table 2. Individual mean Pearson’s r correlations (using Fisher’s z transformation) across the four retest intervals ranged from .51 to .94 (ps < .01; Table 2). Similarly, item-level data were used to assess the stability of caregiver ratings across the two time points in which caregivers were asked to rate the patients according to how they viewed them currently (baseline and 2 months). Caregiver stability correlations ranged from .49 to .85 (ps < .01; see Table S2 in the Supplemental Material).
Table 2.
Stability of Patients’ Ratings on the Big Five Inventory at the Item Level
| Patient | Time point | M | Mdn | |||
|---|---|---|---|---|---|---|
| 1 day | 2 weeks | 2 months | 1 year | |||
| 1846 | .45 [.17, .66] | .45 [.18, .66] | .62 [.39, .77] | .52 [.26, .71] | .51 | .49 |
| 1951 | .74 [.56, .85] | .75 [.58, .86] | .71 [.53, .83] | .75 [.59, .86] | .74 | .75 |
| 2308 | .95 [.92, .97] | .94 [.89, .97] | .95 [.91, .97] | .93 [.88, .96] | .94 | .95 |
| 2363 | .81 [.68, .89] | .73 [.55, .84] | .82 [.68, .90] | .67 [.47, .81] | .76 | .77 |
| 2367 | .78 [.63, .87] | .85 [.74, .92] | .84 [.72, .91] | .79 [.65, .88] | .82 | .82 |
| 2563 | .88 [.79, .93] | .76 [60, .86] | .88 [.79, .93] | .80 [.65, .88] | .84 | .84 |
| 3139 | .80 [.66, .89] | .87 [.78, .93] | .81 [.68, .89] | .81 [.67, .89] | .82 | .81 |
| M | .81 | .80 | .83 | .78 | ||
| Mdn | .80 | .76 | .82 | .79 | ||
Note: The table shows Pearson’s r stability coefficients across four retest intervals; all correlations are significant at p < .01. Values in brackets are 95% confidence intervals. Means are averages using Fisher’s z transformation. All individual correlations were transformed to z scores using Fisher’s z-transformation method. These values were then averaged and transformed back to a Pearson’s correlation using Fisher’s inverse transformation.
To determine whether the stability coefficients obtained from the current sample were within the range of values obtained from healthy, non-brain-damaged individuals, we compared their item-level reliability with the reliability in a large normative database of individuals who were also assessed on the BFI across a 1-year interval (samples described by Costello et al., 2018). We performed the same person-centered analyses on two age bands of this normative sample: individuals who were no longer in emerging adulthood (i.e., 26+ years old; mean age = 38.75 years; n = 300) and a smaller subset of individuals who were within the same age range as our current sample (i.e., 45–56 years old; mean age = 50.09 years; n = 86). At the item level, our cohort of amnesic patients demonstrated similarly high stability (r = .78) in comparison with both age bands of the normative sample (r = .75 in individuals 26+ years old, r = .78 in individuals 45–56 years old).
Trait stability
For the next set of analyses, we examined the rank-order stability of the BFI traits using Spearman’s ρ nonparametric correlations. For the self-ratings, stability coefficients were obtained for four retest intervals: Time 1 to Time 2 (1 day), Time 1 to Time 3 (2 weeks), Time 1 to Time 4 (2 months), and Time 1 to Time 5 (1 year). As shown in Table 3, Extraversion had the highest mean stability (ρ = .98), and all stability coefficients were significant (ps < .05). In contrast, none of the stability coefficients were significant for Neuroticism, which had the lowest mean stability of the Big Five traits (ρ = .72). Overall, rank-order stability across the five traits was relatively well maintained over time. In comparison with a large sample of adults from the Life Outcomes of Personality Replication (LOOPR) Project (Soto, 2019; N = 488; mean age = 52.5 years), our sample generally had stability coefficients that were consistent with short-term normative results on the BFI-2 (Soto & John, 2017). Normative stability (r) at 1 month in the comparison sample ranged from .80 (Agreeableness) to .86 (Neuroticism; Soto, 2020), whereas our sample’s trait stability (ρ) ranged from .60 (Agreeableness) to .96 (Extraversion) at 2 weeks and .72 (Neuroticism) to .96 (Extraversion) at 2 months. Additionally, we examined long-term BFI trait stability (i.e., 1 year) from a large sample of healthy individuals (described by Costello et al., 2018). Analyses were conducted on two age bands from this sample: individuals who were no longer in emerging adulthood (i.e., 26+ years old; mean age = 38.75 years; n = 300) and only individuals within the age range of our current sample (i.e., 45–56 years old; mean age = 50.09 years; n = 86). At the trait level, stability correlations (rs) ranged between .82 and .87 and between .78 and .89 for each respective age subset, whereas our sample’s trait stability (ρ) ranged from .66 (Neuroticism) to .99 (Extraversion) at 1 year. Notably, at both comparison time points (1 month and 1 year), the current sample showed heightened levels of stability on Extraversion and lower levels of stability on Neuroticism relative to the normative data sets.
Table 3.
Stability of Patients’ Ratings on the Big Five Inventory at the Trait Level
| Trait | Time point | M | |||
|---|---|---|---|---|---|
| 1 day | 2 weeks | 2 months | 1 year | ||
| Neuroticism | .74 [−.03, .96] | .74 [−.03, .96] | .72 [−.08, .96] | .66 [−.18, .95] | .72 |
| Extraversion | 1.00 a [1.00, 1.00] | .96 [.77, 1.00] | .96 [.72, .99] | .99 [.94, .99] | .98 |
| Openness | .96 [.77, 1.00] | .90 [.46, .99] | .81 [.15, .97] | .90 [.46, .99] | .91 |
| Agreeableness | .93 [.58, .99] | .60 [−.15, .95] | .79 [.09, .97] | .88 [.94, .99] | .83 |
| Conscientiousness | .91 [.49, .99] | .87 [.34, .98] | .91 [.49, .99] | .80 [.13, .97] | .88 |
Note: The table shows rank-order stability (Spearman’s ρ coefficients) across four retest intervals. Significant coefficients are in boldface (p < .05). Values in brackets are 95% confidence intervals. Means are averages using Fisher’s z transformation.
The actual coefficient was 0.999 and was rounded up to 1.00.
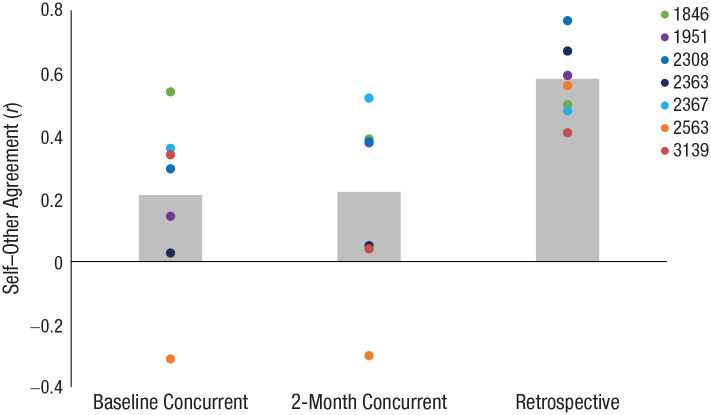
Concurrent and retrospective self–other agreement
Mean retrospective self–other agreement (r = .58) was significantly higher than baseline concurrent self–other agreement (r = .21, z = −2.04, p = .041; see Fig. 2). Comparisons between retrospective self–other agreement (r = .58) and 2-month concurrent self–other agreement (r = .22) showed a similar significant pattern (z = −1.99, p = .047), in which there was a higher degree of agreement in retrospective than in concurrent ratings. There was no difference in the level of self–other agreement on the two concurrent ratings (baseline and 2 months; z = −0.05, p = .958). Correlation coefficients for concurrent and retrospective self–other agreement are displayed for each patient–caregiver pair in Table S3 in the Supplemental Material. We compared patient–caregiver ratings with ratings obtained in two previous studies from large normative samples of close dyads (i.e., married couples; n = 148, mean age = 47.1 years, average length of marriage = 17 years, described by Watson et al., 2000; and n = 170, mean age = 39.4 years, average length of marriage = 11 years, described by Longley et al., 2005). The dyad members from these normative samples rated themselves and each other on the NEO Five-Factor Inventory and BFI scales, respectively. These dyad studies suggested that normative levels of item-level self–other agreement (r) fall within a range of .52 to .60. Thus, in comparison with these normative data, data from our patient–caregiver pairs showed lower levels of self–other agreement when ratings were made concurrently (r = .21 at baseline and r = .22 at 2 months) and typical levels of agreement when caregivers made ratings retrospectively (r = .58).
Fig. 2.
Mean correlation between patient and caregiver ratings at three time points, both separately for each patient and averaged across all patient–caregiver pairs. Retrospective ratings reflect average correlations between self-report ratings at 1 year and caregiver retrospective ratings at 1 year.
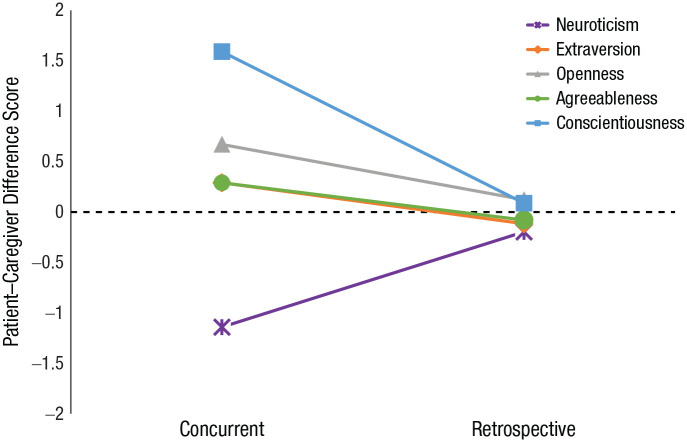
Self–other consistency in mean trait levels
To examine the level of self–other consistency across all individual personality traits, we computed difference scores between self and caregiver trait ratings at baseline (concurrent) and 1-year follow-up (retrospective) and averaged them across all patients. Average self–other consistency by trait is reported in Figure 3. Given that each BFI scale consists of varying numbers of items, average raw scores for each scale were used as a replacement for summed scale scores in order to facilitate more direct comparisons. Larger differences indicate larger discrepancies in self–other ratings, whereas scores near zero reflect greater convergence. Retrospective ratings yielded discrepancies closer to zero across all five traits (see Fig. 3). The largest discrepancies were evident for Neuroticism (patient ratings were lower than caregiver ratings) and Conscientiousness (patient ratings were higher than caregiver ratings). Patient-level self–other consistency and stability for each of the five traits are reported in Figures S1 to S7 in the Supplemental Material. As can be seen in those graphs, there was an appropriate level of variance in patients’ and caregivers’ ratings across the different personality traits, providing evidence against the notion of potential range restriction or stereotype effects.
Fig. 3.
Average difference score on each of the Big Five traits when patients and caregivers made ratings concurrently and retrospectively. Difference scores between patient and average caregiver raw trait ratings were calculated at baseline (concurrent) and 1-year follow-up (retrospective). Individual difference scores were then averaged across the seven patients to create an average difference score for each trait. Larger differences indicate larger discrepancies in patient–caregiver ratings, whereas scores near zero suggest greater convergence. Positive values signify higher ratings by the patient on a given trait than the caregiver, whereas negative values indicate lower ratings by the patient than the caregiver.
Multiple-rater agreement
To address the possibility that the caregiver, rather than the patient, was inaccurately reporting personality traits, we assessed the similarity between caregiver ratings for patients for whom more than one individual provided collateral ratings. To examine the degree of agreement between multiple raters for a given patient, we computed bivariate correlations between Caregiver 1 and Caregiver 2 using item-level BFI data (n = 44). Correlations, provided in Table S4 in the Supplemental Material, ranged from .56 to .75, and all were significant (p < .05). Average rater–rater agreement (r) was .59 for concurrent baseline ratings, .69 for concurrent 2-month ratings, and .65 for retrospective ratings.
Discussion
We conducted the first systematic examination of personality stability and accuracy in a group of rare amnesic patients with bilateral (n = 6) or unilateral left (n = 1) MTL damage by comparing self-reported and caregiver-reported personality ratings over the course of a year. Consistent with previously reported case studies, results suggested a high degree of stability across self-report ratings at five time points. Results also indicated a relatively high level of stability on each of the individual personality traits, Extraversion being highest and Neuroticism being lowest. For the two time points at which caregivers provided concurrent collateral ratings, we saw similarly high stability, suggesting that over the time points measured, the patients did not exhibit any major changes in personality.
To address the patients’ accuracy in reporting their personality traits, we compared self-ratings with concurrent and retrospective ratings made by caregivers. Results consistently showed a higher degree of convergence with retrospective than with concurrent ratings, both at an item level and across individual personality traits. Furthermore, when more than one caregiver provided ratings (n = three patients), the high degree of convergence between the two caregiver ratings (see Table S4) suggests that the patients, rather than the caregivers, inaccurately reported their current personality. Together, these findings suggest that declarative memory may not be necessary for maintaining a stable sense of self. However, maintaining an accurate and up-to-date sense of self may in fact be reliant on the ability to integrate new life experiences into one’s memory. A person’s view of their own personality is developed and refined over time in response to life events. The patients in this study experienced extreme and drastic life changes following their brain injury (e.g., loss of relationships, independence, occupations), which led to changes in their behavior. However, without the ability to remember the collection of life events that occurred after injury and their behavioral responses to such drastic changes, these individuals were unable to provide accurate and updated depictions of themselves, thus highlighting the interconnectedness between the MTL declarative memory system and the accurate perception of one’s self.
These results differ somewhat from previous findings in single cases. As previously described, patients K. C. (Tulving, 1993), D. B. (Klein et al., 2002), and M. K. (Grilli et al., 2018) gave personality ratings consistent with how their caregivers rated them after brain injury. However, these studies have important limitations. For example, D. B.’s caregiver did not provide retrograde personality ratings, thus limiting conclusions that can be made about whether his ratings are more reflective of his personality before or after injury. Similarly, D. B. was studied only 2 months after his injury, not allowing much time for him to experience and integrate major life changes. Another important consideration when reviewing these prior cases pertains to the distinction between episodic and semantic personal knowledge. These patients had very limited access to personal episodic memory, suggesting that personality ratings can largely be made using semantic knowledge about the self. The current study did not directly examine the differential contributions of episodic and semantic knowledge, although data presented in Table S1 provide a strong case that many aspects of retrograde semantic memory are intact in our patients. The pattern of retrograde episodic memory is less clear. Data from the Iowa Autobiographical Memory Questionnaire suggest varying degrees of retrograde episodic memory loss (see Table S1; Jones et al., 1998), which is corroborated by previous work that has extensively characterized functioning across these domains in one of the patients in this sample (see Feinstein et al., 2010). Understanding how episodic and semantic memories independently contribute to and influence personality ratings in this cohort would be an excellent avenue for future research.
An additional consideration involves the inclusion of an individual with unilateral MTL damage (Patient 2367). Although this patient was included on the basis of their comparable neuropsychological profile, it is worth noting potential differences relative to the bilateral patients. Patient 2367 exhibited similar levels of stability over time (see Table 2); however, they did not follow the pattern of self–other agreement to the same extent as the bilateral cases (see Table S3). In comparison with the rest of the sample, Patient 2367 showed mild levels of self–other agreement at concurrent and retrospective time points. Their caregiver’s ratings did not show any decrease in stability from concurrent to retrospective ratings, suggesting that they may not have exhibited any major shifts in personality after lesion onset. This pattern of findings is consistent with a previously published unilateral case study, M. K., who developed amnesia following a surgical resection of the left anterior temporal lobe (Grilli et al., 2018). M. K. demonstrated stable and accurate (when compared with his wife’s ratings) self-ratings over time. Furthermore, he and his wife reported little change in personality since his surgery (Grilli et al., 2018). Taken together, these findings suggest that left unilateral MTL damage, compared with bilateral damage, may be associated with lesser change in personality following lesion onset.
It should be noted that our findings pertain specifically to memory and the MTL. Other types of cognitive deficits (e.g., dysexecutive syndrome) associated with damage to other brain regions (e.g., ventromedial prefrontal cortex) could demonstrate different patterns regarding the stability of personality ratings and one’s ability to update their sense of self (Barrash et al., 2000, 2018). Additionally, the literature in populations with other forms of brain damage (e.g., TBI, frontotemporal lobar degeneration) has largely focused on the stability of personality traits from the view of the caregiver rather than the patient, with caregivers reporting variable degrees of personality change over time (Kurtz et al., 1998; Mahoney et al., 2011; Tate, 2003). Research on self–other agreement among personality traits has been similarly limited. To our knowledge, there has been only one study that examined self–other consistency on the Big Five personality traits (using the Revised NEO Personality Inventory) in a sample of patients with TBIs and a healthy comparison group (Kurtz & Putnam, 2006). Levels of self–other consistency on personality ratings in the TBI sample were found to be comparable with those of the healthy comparison group (Kurtz & Putnam, 2006). Our amnesic sample had lower concurrent self–other consistency across all five traits than the TBI and healthy groups, suggesting that discrepancies in self–other agreement may not occur to the same extent in other forms of brain injury. Future work should further investigate the specificity of these findings.
There are a number of strengths to the present study, including a relatively large number of amnesic patients with MTL damage; use of a well-validated measure of personality, self-ratings, and caregiver ratings at multiple time points; and assessment of retrospective ratings. There are also some important limitations. Although we know that caregivers were providing their retrospective ratings for the patients on the basis of the year prior to their injury, we did not collect retrospective ratings from the patients themselves. However, given our extensive interactions with these patients, we consider it highly unlikely that they would have rated themselves very differently if they had been asked explicitly to provide retrospective ratings. Furthermore, no studies have investigated self–other agreement on retrospective ratings in normative samples, which further limits our ability to examine the specificity of the current findings. Thus, we really do not know whether the amnesic patients are normal in regard to their ability to accurately report who they were. Rather, we simply know that there is stronger agreement between self and other when the informant is making a retrospective judgment about the amnesic patient. To expand on this work, future studies could systematically have amnesic patients rate their personality from different time periods in life and compare them with parallel ratings from caregivers.
Finally, it is important to consider that although we had seven patients, the sample size was still small for variable-centered analyses, though we provide them here for descriptive purposes. However, person-centered analyses, as presented in this study, are similar to the analyses conducted in prior case studies (Klein et al., 2002, 2003; Tulving, 1993) and are much more robust, in that they take advantage of the many items (44) on the BFI. Despite these limitations, this study provides important new insight into the role of declarative memory in the conceptualization of one’s self.
Supplemental Material
Supplemental material, sj-docx-1-pss-10.1177_09567976211007463 for Who Are You? The Study of Personality in Patients With Anterograde Amnesia by McKenna M. Garland, Jatin G. Vaidya, Daniel Tranel, David Watson and Justin S. Feinstein in Psychological Science
Acknowledgments
We thank Brooke Feinstein for help with data collection and Joel Bruss for help with figure creation. We also thank Hanna Damasio for assistance in lesion identification.
Footnotes
ORCID iD: McKenna M. Garland  https://orcid.org/0000-0002-3148-9967
https://orcid.org/0000-0002-3148-9967
Supplemental Material: Additional supporting information can be found at http://journals.sagepub.com/doi/suppl/10.1177/09567976211007463
Transparency
Action Editor: Karen Rodrigue
Editor: Patricia J. Bauer
Author Contributions
M. M. Garland and J. G. Vaidya contributed equally to this study. J. S. Feinstein and D. Tranel developed the study concept and design. J. S. Feinstein conducted testing and data collection. M. M. Garland analyzed and interpreted the data under the supervision of J. G. Vaidya and J. S. Feinstein. M. M. Garland and J. G. Vaidya drafted the manuscript, and J. S. Feinstein, D. Tranel, and D. Watson provided critical revisions. D. Watson provided the data on normative comparison stability and agreement. All the authors approved the final manuscript for submission.
Declaration of Conflicting Interests: The author(s) declared that there were no conflicts of interest with respect to the authorship or the publication of this article.
Funding: This research was supported by awards from the National Institute of Mental Health (P50 MH094258), the Kiwanis Foundation (to D. Tranel), and the Fraternal Order of Eagles (to J. S. Feinstein).
Open Practices: Data and materials for this study have not been made publicly available. Requests for item-level Big Five Inventory data and materials can be emailed to the Corresponding Author. The design and analysis plan for the study were not preregistered.
References
- Allen J. S., Tranel D., Bruss J., Damasio H. (2006). Correlations between regional brain volumes and memory performance in anoxia. Journal of Clinical and Experimental Neuropsychology, 28, 457–476. 10.1080/13803390590949287 [DOI] [PubMed] [Google Scholar]
- Barrash J., Stuss D. T., Aksan N., Anderson S. W., Jones R. D., Manzel K., Tranel D. (2018). “Frontal lobe syndrome”? Subtypes of acquired personality disturbances in patients with focal brain damage. Cortex, 106, 65–80. 10.1016/j.cortex.2018.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrash J., Tranel D., Anderson S. W. (2000). Acquired personality disturbances associated with bilateral damage to the ventromedial prefrontal region. Developmental Neuropsychology, 18(3), 355–381. 10.1207/S1532694205Barrash [DOI] [PubMed] [Google Scholar]
- Cavaco S., Feinstein J. S., van Twillert H., Tranel D. (2012). Musical memory in a patient with severe anterograde amnesia. Journal of Clinical and Experimental Neuropsychology, 34(10), 1089–1100. https://doi.org/10.1080%2F13803395.2012.728568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway M. A. (2005). Memory and the self. Journal of Memory and Language, 53(4), 594–628. 10.1016/j.jml.2005.08.005 [DOI] [Google Scholar]
- Costello C. K., Srivastava S., Saucier G. (2018). Stability and change in the Big Five and Big Six: New tests of the maturity and cumulative continuity principles. PsyArXiv. 10.31234/osf.io/b36tv [DOI]
- Duff M. C., Wszalek T., Tranel D., Cohen N. J. (2008). Successful life outcome and management of real-world memory demands despite profound anterograde amnesia. Journal of Clinical and Experimental Neuropsychology, 30(8), 931–945. 10.1080/13803390801894681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein J. S., Rudrauf D., Khalsa S. S., Cassell M. D., Bruss J., Grabowski T. J., Tranel D. (2010). Bilateral limbic system destruction in man. Journal of Clinical and Experimental Neuropsychology, 32(1), 88–106. 10.1080/13803390903066873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnambs T. (2014). A meta-analysis of dependability coefficients (test–retest reliabilities) for measures of the Big Five. Journal of Research in Personality, 52, 20–28. 10.1016/j.jrp.2014.06.003 [DOI] [Google Scholar]
- Grilli M. D., Bercel J. J., Wank A. A., Rapcsak S. Z. (2018). The contribution of the left anterior ventrolateral temporal lobe to the retrieval of personal semantics. Neuropsychologia, 117, 178–187. 10.1016/j.neuropsychologia.2018.06.002 [DOI] [PubMed] [Google Scholar]
- John O. P., Naumann L. P., Soto C. J. (2008). Paradigm shift to the integrative Big Five trait taxonomy. In John O. P., Robins R. W., Pervin L. A. (Eds.), Handbook of personality: Theory and research (3rd ed., pp. 114–158). Guilford Press. [Google Scholar]
- John O. P., Srivastava S. (1999). The Big Five trait taxonomy: History, measurement, and theoretical perspectives. In Pervin L. A., John O. P. (Eds.), Handbook of personality: Theory and research (2nd ed., pp. 102–138). Guilford Press. [Google Scholar]
- Jones R. D., Grabowski T. J., Tranel D. (1998). The neural basis of retrograde memory: Evidence from positron emission tomography for the role of non-mesial temporal lobe structures. Neurocase, 4(6), 471–479. 10.1080/13554799808410640 [DOI] [Google Scholar]
- Klein S. B., Cosmides L., Costabile K. A. (2003). Preserved knowledge of self in a case of Alzheimer’s dementia. Social Cognition, 21(2), 157–165. 10.1521/soco.21.2.157.21317 [DOI] [Google Scholar]
- Klein S. B., Gangi C. E. (2010). The multiplicity of self: Neuropsychological evidence and its implications for the self as a construct in psychological research. Annals of the New York Academy of Sciences, 1191, 1–15. 10.1111/j.1749-6632.2010.05441.x [DOI] [PubMed] [Google Scholar]
- Klein S. B., Lax M. L. (2010). The unanticipated resilience of trait self-knowledge in the face of neural damage. Memory, 18(8), 918–948. 10.1080/09658211.2010.524651 [DOI] [PubMed] [Google Scholar]
- Klein S. B., Rozendal K., Cosmides L. (2002). A social-cognitive neuroscience analysis of the self. Social Cognition, 20(2), 105–135. 10.1521/soco.20.2.105.20991 [DOI] [Google Scholar]
- Kurtz J. E., Putnam S. H. (2006). Patient-informant agreement on personality ratings and self-awareness after head injury. The Clinical Neuropsychologist, 20(3), 453–468. 10.1080/13854040590967090 [DOI] [PubMed] [Google Scholar]
- Kurtz J. E., Putnam S. H., Stone C. (1998). Stability of normal personality traits after traumatic brain injury. The Journal of Head Trauma Rehabilitation, 13(3), 1–14. 10.1097/00001199-199806000-00002 [DOI] [PubMed] [Google Scholar]
- Longley S. L., Watson D., Noyes R., Jr. (2005). Assessment of the hypochondriasis domain: The Multidimensional Inventory of Hypochondriacal Traits (MIHT). Psychological Assessment, 17(1), 3–14. 10.1037/1040-3590.17.1.3 [DOI] [PubMed] [Google Scholar]
- Mahoney C. J., Rohrer J. D., Omar R., Rossor M. N., Warren J. D. (2011). Neuroanatomical profiles of personality change in frontotemporal lobar degeneration. The British Journal of Psychiatry, 198(5), 365–372. 10.1192/bjp.bp.110.082677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquine M. J. (2008). Self-knowledge and self-referential processing in memory disorders: Implications for neuropsychological rehabilitation (Publication No. 3315558) [Doctoral dissertation, The University of Arizona]. ProQuest Dissertations and Theses Global.
- Philippi C. L., Feinstein J. S., Khalsa S. S., Damasio A., Tranel D., Landini G., Williford K., Rudrauf D. (2012). Preserved self-awareness following extensive bilateral brain damage to the insula, anterior cingulate, and medial prefrontal cortices. PLOS ONE, 7(8), Article e38413. 10.1371/journal.pone.0038413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathbone C. J., Moulin C. J. A., Conway M. A. (2009). Autobiographical memory and amnesia: Using conceptual knowledge to ground the self. Neurocase: The Neural Basis of Cognition, 15(5), 405–418. 10.1080/13554790902849164 [DOI] [PubMed] [Google Scholar]
- Roberts B. W., DelVecchio W. F. (2000). The rank order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin, 126(1), 3–25. 10.1037//0033-2909.126.1.3 [DOI] [PubMed] [Google Scholar]
- Roberts B. W., Walton K. E., Viechtbauer W. (2006). Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin, 132(1), 1–25. https://doi/org/10.1037/0033-2909.132.1.1 [DOI] [PubMed] [Google Scholar]
- Scoville W. B., Milner B. (1957). Loss of recent memory after bilateral hippocampal lesions. Journal of Neurology, Neurosurgery and Psychiatry, 20(1), 11–21. 10.1136/jnnp.20.1.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldz S., Vaillant G. E. (1999). The Big Five personality traits and the life course: A 45-year longitudinal study. Journal of Research in Personality, 33(2), 208–232. 10.1006/jrpe.1999.2243 [DOI] [Google Scholar]
- Soto C. J. (2019). How replicable are links between personality traits and consequential life outcomes? The Life Outcomes of Personality Replication Project. Psychological Science, 30(5), 711–727. 10.1177/0956797619831612 [DOI] [PubMed] [Google Scholar]
- Soto C. J. [@cjsotomatic]. (2020, November 10). Haven’t published these stats, but in the LOOPR Project (Soto, 2019) four-week retest correlations are .86/80/84/86/83 [Tweet]. Twitter. https://twitter.com/cjsotomatic/status/1326277246395572231 [Google Scholar]
- Soto C. J., John O. P. (2009). Ten facet scales for the Big Five Inventory: Convergence with NEO PI-R facets, self-peer agreement, and discriminant validity. Journal of Research in Personality, 43(1), 84–90. 10.1016/j.jrp.2008.10.002 [DOI] [Google Scholar]
- Soto C. J., John O. P. (2017). The next Big Five Inventory (BFI-2): Developing and assessing a hierarchical model with 15 facets to enhance bandwidth, fidelity, and predictive power. Journal of Personality and Social Psychology, 113(1), 117–143. [DOI] [PubMed] [Google Scholar]
- Tate R. L. (2003). Impact of pre-injury factors on outcome after severe traumatic brain injury: Does post-traumatic personality change represent an exacerbation of premorbid traits? Neuropsychological Rehabilitation, 13(1), 43–64. 10.1080/09602010244000372 [DOI] [PubMed] [Google Scholar]
- Tellegen A. (1988). The analysis of consistency in personality assessment. Journal of Personality, 56(3), 621–663. [Google Scholar]
- Tulving E. (1993). Self-knowledge of an amnesic individual is represented abstractly. In Srull T. K., Wyer R. S., Jr. (Eds.), Advances in social cognition: Vol. 5. The mental representation of trait and autobiographical knowledge about the self (pp. 147–156). Erlbaum. [Google Scholar]
- Turner J. C., Onorato R. S. (1999). Social identity, personality, and the self-concept: A self-categorization perspective. In Tyler T. R., Kramer R. M., John O. P. (Eds.), The psychology of the social self (pp. 11–46). Erlbaum. [Google Scholar]
- Vaidya J. G., Gray E. K., Haig J., Watson D. (2002). On the temporal stability of personality: Evidence for differential stability and the role of life experiences. Journal of Personality and Social Psychology, 83(6), 1469–1484. 10.1037/0022-3514.83.6.1469 [DOI] [PubMed] [Google Scholar]
- Watson D. (2004). Stability versus change, dependability versus error: Issues in the assessment of personality over time. Journal of Research in Personality, 38(4), 319–350. 10.1016/j.jrp.2004.03.001 [DOI] [Google Scholar]
- Watson D., Hubbard B., Wiese D. (2000). Self–other agreement in personality and affectivity: The role of acquaintanceship, trait visibility, and assumed similarity. Journal of Personality and Social Psychology, 78(3), 546–558. 10.1037//0022-3514.78.3.546 [DOI] [PubMed] [Google Scholar]
- Wechsler D. (1997. a). Wechsler Adult Intelligence Scale, Third Edition (WAIS-III). Psychological Corp. [Google Scholar]
- Wechsler D. (1997. b). Wechsler Memory Scale, Third Edition (WMS-III). Psychological Corp. [Google Scholar]
- Wilson T. D. (2009). Know thyself. Perspectives on Psychological Science, 4(4), 384–389. 10.1111/j.1745-6924.2009.01143.x [DOI] [PubMed] [Google Scholar]
- Zola-Morgan S. M., Squire L. R., Amaral D. G. (1986). Human amnesia and the medial temporal region: Enduring memory impairment following a bilateral lesion limited to field CA1 of the hippocampus. The Journal of Neuroscience, 6(10), 2950–2967. 10.1523/JNEUROSCI.06-10-02950.1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pss-10.1177_09567976211007463 for Who Are You? The Study of Personality in Patients With Anterograde Amnesia by McKenna M. Garland, Jatin G. Vaidya, Daniel Tranel, David Watson and Justin S. Feinstein in Psychological Science